Professional Documents
Culture Documents
The Orthopaedic Implications of Diphosphonate Therapy
The Orthopaedic Implications of Diphosphonate Therapy
Uploaded by
Azmi FarhadiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Orthopaedic Implications of Diphosphonate Therapy
The Orthopaedic Implications of Diphosphonate Therapy
Uploaded by
Azmi FarhadiCopyright:
Available Formats
Review Article
The Orthopaedic Implications of
Diphosphonate Therapy
Abstract
Michael J. Weaver, MD Diphosphonates are among the many commonly prescribed drugs
Micah A. Miller, BS for osteoporosis management. These synthetic analogues of
physiologically occurring inorganic pyrophosphate bind to the
Mark S. Vrahas, MD
hydroxyapatite crystals of bone. Diphosphonates act by decreasing
the amount of osteoclast-mediated bone resorption by inducing
apoptosis and disrupting the mevalonate biosynthetic pathway.
Prospective clinical trials have shown that diphosphonates increase
bone mineral density and reduce the risk of fracture.
Diphosphonates are generally well tolerated, with a low incidence
of side effects. They may be administered orally or intravenously;
infusions are the most potent. Few studies have directly studied
the effect of diphosphonates on the rate of fracture or time to
union. Concern exists regarding the long-term safety of
diphosphonates, particularly in patients with osteoporosis. New
evidence suggests that long-term therapy may increase the risk of
fracture of the femoral shaft, with possible morphologic and
prodromal warning signs. Further prospective research into the
consequences of diphosphonate-mediated suppressed bone
turnover is needed to elucidate a safe duration of treatment.
From Partners Orthopaedic Trauma
Service, Brigham and Women’s
D iphosphonates are a class of
drugs widely used in the treat-
ment of such varied conditions as
creasing the amount of osteoclast-
mediated bone resorption. Recent re-
ports have suggested that long-term
Hospital and Massachusetts General
Hospital, Boston, MA. heritable skeletal disorders in chil- diphosphonate use may play a role
Dr. Weaver or an immediate family dren, hypercalcemia, metastatic car- the development of stress fractures of
member has received research or cinoma, multiple myeloma, Paget the femoral shaft.
institutional support from Synthes disease of bone, and osteoporosis.
and Zimmer. Dr. Vrahas or an
Since their initial development for
immediate family member has
received research or institutional clinical use, hundreds of different Pharmacology and
support from Synthes; DePuy, a compounds have been synthesized, Mechanism of Action
Johnson & Johnson company; and dozens have undergone clinical
Zimmer; and AO. Neither Mr. Miller
trials. Diphosphonates are synthetic ana-
nor any immediate family member
Diphosphonates remain among the logues of physiologically occurring
has received anything of value from
or owns stock in a commercial most common drug treatments for inorganic pyrophosphate (PPi), in
company or institution related osteoporosis. Research continues to which the oxygen bridge has been re-
directly or indirectly to the subject of placed with a carbon atom (P-C-P).
this article.
elucidate the exact mechanisms of
action of these medications as well as The carbon center is resistant to heat
J Am Acad Orthop Surg 2010;18: and enzymatic hydrolysis, which al-
367-374
the implication of their long-term use
on bone remodeling, the biomechan- lows the molecules to pass intact to
Copyright 2010 by the American sites of bone resorption without be-
ical properties of bone, and bone
Academy of Orthopaedic Surgeons.
healing. Diphosphonates act by de- ing metabolized. Once in the blood
June 2010, Vol 18, No 6 367
The Orthopaedic Implications of Diphosphonate Therapy
Figure 1 sorption of bone.1 Aminodiphospho-
nates contain an amino group on R2,
with ring-configured amino groups
yielding much greater potency than
simple amino groups. For example,
zoledronate is 20,000 times more
potent per equivalent dose than eti-
dronate, the original non-amino-
diphosphonate. It appears that these
Chemical structure of pyrophosphate (A), simple diphosphonate (B), and two classes of drug affect osteoclastic
aminodiphosphonate (C). The moiety in the place of R1 and R2 determines resorption of bone in different ways.
the specific chemical characteristics of the diphosphonate. The P-C-P portion
Simple diphosphonates act by being
is responsible for the high affinity for the hydroxyapatite in bone. N = amino
metabolized into nonhydrolyzable
adenosine triphosphate analogues.
Figure 2 These metabolites accumulate within
osteoclasts, inhibiting cellular metab-
olism, leading to apoptosis and cell
death1 (Figure 2, A). Aminodiphospho-
nates appear to act primarily by disrupt-
ing the mevalonate biosynthetic path-
way. The mevalonate pathway is
responsible for cholesterol production
and is perhaps best known as a target
for common cholesterol-lowering stat-
ins. Aminodiphosphonates act by inhib-
iting protein prenylation, which causes
loss of the ruffled border and results in
apoptosis2 (Figure 2, B). The primary
target appears to be farnesyl pyro-
phosphate synthase, although other
enzymes may also be affected.
The selectivity of diphosphonates
is a function of their affinity to bone
rather than to their specific intracel-
lular activity. Diphosphonates bind
to hydroxyapatite crystals in bone.3
They are not integrated directly into
hydroxyapatite but rather bind to
the surface of the crystal and are
A, Mechanism of action of simple diphosphonates. Diphosphonates are then trapped as new crystals form.
taken up by osteoclasts (left), where they are metabolized into Diphosphonates have been shown to
nonhydrolyzable adenosine triphosphate analogues (center). Right,
accumulate at the site of bone re-
Accumulation leads to induction of apoptosis. B, Aminodiphosphonate
mechanism of action within osteoclasts. The mevalonate pathway is blocked, sorption where bone mineral is most
thus inhibiting protein prenylation. Cell morphology is disrupted, leading to exposed.4 As activated osteoclasts re-
loss of the ruffled border and eventual apoptosis. DP = diphosphonate, sorb bone, the deposited diphospho-
HMG-CoA = hydroxymethylgutaryl-coenzyme A, PP = pyrophosphate
nate is released into the local mi-
croenvironment and is preferentially
stream, diphosphonates demonstrate (Figure 1), or first- and second-gen- taken up by osteoclasts. Once inter-
an affinity for bone. eration diphosphonates, respectively. nalized, diphosphonates inhibit bone
Diphosphonates can be classified in Aminodiphosphonates are 10 to 10,000 resorption and eventually induce ap-
two general categories: simple diphos- times more potent than simple diphos- optosis.5,6 Approximately 50% to
phonates and aminodiphosphonates phonates in inhibiting osteoclastic re- 80% of diphosphonates are cleared
368 Journal of the American Academy of Orthopaedic Surgeons
Michael J. Weaver, MD, et al
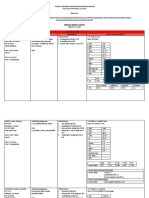
Table 1
Diphosphonates Listed in Order of Increasing Potency With Current Dosing Recommendations9
Drug Daily Weekly Monthly Yearly
Etidronatea (Didronel [Procter & Gam- 5 mg/kg PO — — —
ble Pharmaceuticals, Cincinnati, OH])
Tiludronatea (Skelid, [sanofi-aventis, 400 mg PO — — —
Bridgewater, NJ])
Pamidronatea,b (Aredia [Novartis Phar- — — — 30-90 mg infusion
maceuticals, Basel, Switzerland])
Alendronatea,c (Fosamax, Fosamax 10 mg PO 70 mg PO — —
Plus D [Merck, Whitehouse Station,
NJ])
Ibandronatec (Boniva [Roche Laborato- 2.5 mg PO — 150 mg PO —
ries, Nutley, NJ])
Risedronatea,c (Actonel, Actonel with 5 mg PO 35 mg PO 150 mg PO —
Calcium [Procter & Gamble])
Zoledronic acidb (Reclast, Zometa — — — 4-mg infusion
[Novartis])
a
US FDA approved in the treatment of Paget disease of bone
b
US FDA approved in the treatment of skeletal metastatic disease
c
US FDA approved in the treatment of osteoporosis
from the blood stream by renal ex- esophageal ulcers.10 Symptomatic hy- sis of the jaw bones are poorly un-
cretion, and approximately 1% are pocalcemia has been reported in pa- derstood, but several theories exist.
cleared through biliary excretion.7 tients with hypoparathyroidism and The unique environment of the oral
The remainder of the drug is incor- vitamin D deficiency.11 Ocular side cavity normally facilitates quick and
porated into the crystalline structure effects, including pain, blurred vi- uncomplicated healing after a surgi-
of bone and may persist for the life- sion, scleritis, and uveitis, have also cal insult, such as tooth extraction.
time of the patient, with an esti- been reported with diphosphonate When this environment is disturbed,
mated half-life in bone of 10 years.7 use.12 There are sporadic reports of however, either by loss of vascular-
myalgia and arthralgia in patients on ization of the jawbones from tumori-
Dosage and Side Effects diphosphonate therapy.13 cidal radiation or some other agent
Osteonecrosis of the jaw is a rare or pathology, then minor injury may
Diphosphonates can be administered complication of diphosphonate ther- increase the risk of osteonecrosis and
either orally or intravenously. Oral apy. Reports of “phossy jaw” date as possible secondary osteomyelitis.
bioavailability is poor; only 1% to far back as the mid 19th century in The mandible and maxilla are also
5% of the drug is absorbed.8 Diphos- factory workers exposed to white sites of high bone turnover, so the
phonates should be taken with water phosphorus.14 The incidence of jaw possibility exists that diphospho-
on an empty stomach, and the pa- osteonecrosis is approximately 1 in nates are selectively deposited in jaw-
tient should remain upright for 2 to 50,000 patient-years when oral bones more than in other bony tis-
3 hours to minimize the risk of diphosphonates are taken for os- sues. However, we are unaware of
esophagitis. Dosage and frequency of teoporosis.15 The risk of osteonecro- any study demonstrating selective in-
administration vary by drug, with sis is higher in oncology patients, pa- crease in diphosphonate deposition
daily, weekly, and monthly dosing tients undergoing chemotherapy, and in certain bones, such as the jaws.
schedules. Typical regimens are pre- patients undergoing significant den- Another possibility is that other con-
sented in Table 1. tal procedures.15 This complication comitant medications may exacer-
Diphosphonates are generally well may be dose-specific; oncology pa- bate wound healing problems and
tolerated, with a low incidence of side tients typically receive much higher could be considered to be possible
effects. Upper gastrointestinal side ef- doses of diphosphonates than do cofactors.
fects have been reported, including dys- those treated for osteoporosis. Infusion reactions have been re-
pepsia, dysphagia, esophagitis, and The mechanisms involved in necro- ported with the use of zoledronic
June 2010, Vol 18, No 6 369
The Orthopaedic Implications of Diphosphonate Therapy
acid and pamidronate. Symptoms in- deoxypyridinoline, N-telopeptides of patients in the placebo group sus-
clude low-grade fever, myalgia, ar- type 1 collagen, and C-telopeptides tained vertebral fracture, versus 8%
thralgia, and malaise persisting for of type 1 collagen. Pyridinolines are in the alendronate group—a 47%
24 to 72 hours following drug ad- measured in urine, whereas telopep- lower risk (P = 0.001). Additionally,
ministration. As many as 32% of pa- tides can be measured in urine or se- the incidence of any clinical fracture
tients may experience such symp- rum. The advantage of using bone was lower in the alendronate group
toms following the first infusion, markers instead of BMD to assess than in the placebo group (13.6%
with reduced incidence following bone turnover is that significant versus 18.2%, respectively), and pa-
subsequent infusions.13 Zoledronic changes in bone markers can be ob- tients in the alendronate group had
acid has also been associated with a served at 3 to 6 months after the fewer hip and wrist fractures than
slight increase in the risk of atrial fi- did those in the placebo group. In a
start of therapy, whereas significant
brillation.13 The US FDA issued an 10-year extension of the study pub-
BMD changes may take 18 months
alert in 2008 regarding the asso- lished by Bone et al,26 treatment with
to materialize.
ciation between diphosphonate use 10 mg alendronate daily resulted in a
Currently there is no consensus on
and transient musculoskeletal pain, significant increase in BMD in the
how long to continue diphosphonate
which may occur days, months, or lumbar spine as well as at other skel-
therapy. However, stopping therapy
years after therapy is begun.16 This etal sites. The reduction in fracture
after 5 years may be reasonable for
phenomenon is distinct from acute risk appears to be most pronounced
some patients because there appears
infusion response, whose frequency in patients with osteoporosis.22
to be a residual benefit on BMD and
and contributing risk factors be- Liberman et al23 found that alendro-
fracture prevention for up to 5 years
tween severe musculoskeletal pain nate therapy of 10 mg/d increased
following cessation of therapy. This
and diphosphonate use are currently bone density of the spine and proxi-
was demonstrated in the Fracture In-
unknown. mal femur by 8.8% and 7.8%, re-
tervention Trial Long-Term Exten-
Analysis of human iliac crest biop- spectively, over a 3-year period com-
sion (ie, FLEX), a study involving
sies suggests that microdamage will pared with placebo (P < 0.001).
1,099 postmenopausal women who
accumulate after 5 years of alendro- Recent meta-analyses of both alen-
had previously undergone alendro-
nate therapy, particularly in patients dronate and risedronate therapy in
nate therapy for 5 years.20
with low bone mineral density postmenopausal women demonstrated
(BMD).17 Microdamage is generally a low relative risk of vertebral and non-
defined as matrix failure detectable Reduction in Risk of vertebral fracture.27,28 Zoledronic acid
with light microscopy. This likely be- Osteoporotic Fracture has also been shown to decrease the rate
gins with debonding of the collagen of fragility fracture and mortality com-
fiber matrix, progressing through the Several prospective randomized clini- pared with placebo. In a benchmark
hierarchy of bone architecture until cal trials have shown that diphospho- randomized, double-blind, placebo-
very fine cracks coalesce into dye- nates, including alendronate, rised- controlled trial, 2,127 patients were as-
penetrable cracks that are visible un- ronate, ibandronate, and zoledronic signed to receive yearly zoledronic acid
der a light microscope. The cracks acid, increase BMD and decrease the infusion or placebo. Administration of
may also compound upon one an- risk of fragility fracture.13,20-25 Alen- a single intravenous dose of zoledronic
other, changing the stress state to dronate was the first orally active acid within 90 days following hip frac-
produce more and larger cracks. aminodiphosphonate available in the ture resulted in a 35% reduction in the
Some authors advise checking mark- United States. Its effectiveness in re- incidence of second fracture.24 A
ers of bone metabolism in patients ducing the incidence of osteoporotic 28% reduction in deaths from any
taking diphosphonates and consider- fractures was investigated in the cause was seen in the zoledronic acid
ing a drug holiday if turnover has Fracture Intervention Trial (FIT),21 group, and no cases of osteonecrosis
stopped.18 Markers of bone resorp- which involved 2,027 women with of the jaw or adverse effects on frac-
tion seem to be stronger predictors low BMD in the femoral neck, with ture healing were noted.
of future bone loss than are markers or without vertebral fracture. Pa- These data collectively demonstrate
of bone formation; these markers are tients were randomized to receive the utility of diphosphonate therapy in
correlated more strongly in elderly alendronate or a placebo for 3 years. reducing the risk of osteoporotic frac-
women than in younger women.19 Clinically and radiographically evi- tures and subsequent mortality, most
Currently available markers of bone dent vertebral fractures served as the notably from hip fracture. The signif-
resorption include pyridinoline, primary end point. Fifteen percent of icance of this cannot be overstated,
370 Journal of the American Academy of Orthopaedic Surgeons
Michael J. Weaver, MD, et al
given the very high rate of mortality fol- ther research into the effects of periprosthetic BMD compared with
lowing hip fracture in elderly persons. diphosphonates on primary bone controls. Friedl et al36 randomized
Diphosphonate therapy is a relatively healing is required, although indirect patients undergoing cementless THA
cost-effective intervention that can de- evidence suggests that diphospho- to receive either a single infusion of
monstrably reduce the risk of such a nates are safe to use following surgi- zoledronic acid or placebo. They
common problem in elderly persons cal fixation of fractures. Data from demonstrated a statistically signifi-
and in persons with osteoporosis. animal studies have demonstrated a cant reduction in acetabular compo-
delay in union following spinal fu- nent subsidence (P < 0.05) and a
sion while the animals were on trend for less femoral subsidence in
Diphosphonates and diphosphonates.33 The proper dose patients treated with zoledronic acid.
Fracture Healing and timing of administration during Neither acetabular or femoral failure
There is concern that diphosphonates the postoperative period following of ingrowth was observed.
may hamper the normal healing process fracture or spinal fusion remains to
following fracture; however, there is a be defined.
Diphosphonates and
paucity of studies directly examining the Femoral Shaft Stress
effect of diphosphonates on the rate of Diphosphonates and Total Fracture
or time to union in fracture patients. Joint Arthroplasty
Munns et al29 reported that pamidro- Recent case series have implicated
nate treatment was associated with de- Data regarding the use of diphospho- diphosphonate therapy—specifically,
layed healing after osteotomy but not nates in patients undergoing total hip alendronate—with low-energy frac-
after fracture in children with moder- arthroplasty (THA) and total knee ar- tures of the subtrochanteric region of
ate to severe osteogenesis imperfecta. throplasty (TKA) are limited. Peripros- the femur. The earliest report of frac-
Adult studies are lacking. Animal stud- thetic bone loss after THA and TKA is tures associated with alendronate use
ies have shown that the effect of thought to occur primarily because of was by Odvina et al37 in 2005. They
zoledronic acid on fracture repair is a stress-shielding phenomenon. Bone reported a series of nine spontaneous
characterized by a larger trabecular surrounding the new joint adjusts its fractures of the pelvis, femur, and
bone volume, increased callus size and mineral density and structure to meet sacrum. More recent series focus spe-
bone mineral content, and improved the changed mechanical demands. Lo- cifically on fractures of the femoral
mechanical strength.30,31 However, a cal surgical trauma and immobilization shaft, particularly in the subtrochan-
delay in remodeling of the hard cal- can also negatively affect bone quality. teric region.38,39
lus during endochondral fracture re- Poor bone density and structure around Goh et al38 and Neviaser et al39
pair was observed.30,31 the implant may place the recipients of presented case series of 13 and 70
Recent studies have provided evi- these implants at greater risk of asep- patients, respectively, who sustained
dence that diphosphonates stimulate tic loosening and periprosthetic frac- subtrochanteric femur fractures. A
the proliferation of osteoblasts and ture. There is some evidence that pa- high proportion of patients treated
osteoblast-like cells. They enhance tients on diphosphonate therapy may with alendronate had a cortical beak
the proliferation of bone marrow have a lower incidence of these postop- on the anterolateral aspect of the fe-
stromal cells and promote osteoblas- erative complications after THA or mur (Figure 3). The cause and im-
tic differentiation, primarily medi- TKA. portance of this abnormality is un-
ated through bone morphogenetic In a randomized controlled trial of known. Five of the 13 patients in the
protein-2.32 Diphosphonates may also 19 patients with TKA, patients who study by Goh et al38 recalled prodro-
prevent osteoblast apoptosis through an took alendronate and calcium were mal pain prior to their fractures.
unknown mechanism, thereby indi- found to maintain distal femoral In a case-control study, Lenart
rectly contributing to the relative in- BMD values close to baseline values, et al40 linked long-term diphosphonate
crease in active cell numbers. whereas patients who received only use with insufficiency fractures of the
Primary bone healing is dependent calcium showed significant bone loss femur in postmenopausal women.
on osteoclast function at the leading at 1-year follow-up.34 Bhandari et Diphosphonate use was observed in 15
edge of cutting cones to cross the al35 conducted a meta-analysis of six of the 41 cases of subtrochanteric/shaft
fracture site. There are no clinical randomized controlled trials and fracture, compared with 9 of the 82
data to support or refute the use of found that diphosphonates have a intertrochanteric/femoral neck controls.
diphosphonates in this setting. Fur- beneficial effect in maintaining The beaking pattern was identified ra-
June 2010, Vol 18, No 6 371
The Orthopaedic Implications of Diphosphonate Therapy
Figure 3 Large-scale randomized controlled
trials demonstrate a decrease in over-
all fracture risk; however, most of
these studies are of <5 years dura-
tion.25 It is possible that longer-term
use of diphosphonates may lead to
an increased risk of fracture. With-
out the extension of previous studies
or the undertaking of a direct obser-
vational study, the nature and mag-
nitude of this potential risk will re-
main unknown.
Summary
Diphosphonates are among the most
Preoperative (A) and postoperative (B) AP radiographs of a 61-year-old commonly prescribed treatments for
woman who sustained a femoral shaft fracture following a ground-level fall.
The patient had been on alendronate therapy for 5 years preinjury. She osteoporosis. They have been shown
reported no prodromal symptoms. The arrows indicate the classic beak to increase BMD over time and re-
appearance of the lateral femur. C, AP radiograph of the contralateral femur duce the rate of fragility fractures. In
demonstrating a stress reaction and beaking (arrow) at the level of the
fracture on the injured side. general, this class of medication is
well tolerated, with few side effects.
Further study is necessary to deter-
mine proper dosing regimens follow-
diographically in 10 of the 15 sub- sue, or advanced glycation end prod- ing surgical fixation of fractures.
trochanteric/shaft cases managed with ucts. Glycation of bone tissue has Diphosphonate use appears to be
a diphosphonate. been shown to make bone more brit- safe in patients undergoing cement-
Animal studies suggest that pro- tle, with a decrease in the deform- less total joint arthroplasty, although
longed diphosphonate use may lead ability of bone before fracture.43 Ani- detailed studies are lacking. Recent
to the accumulation of microdamage mal models suggest that there is an case series suggest a possible associa-
over time and that high doses of accumulation of advanced glycation tion between long-term diphospho-
diphosphonate are associated with end products in cortical and trabecu- nate therapy and the development of
weakened mechanical properties of lar bone with diphosphonate thera- stress fractures of the femoral shaft,
bone.41 Diphosphonate-mediated py.44 Glycation of bone is a common and the optimum duration of ther-
turnover suppression in a canine problem in persons with diabetes apy remains unclear. Direct study
model was associated with a four- to and is one reason for the increased into the mechanism of this associa-
sevenfold increase in microdamage risk of fracture in persons with type tion as well as the magnitude of the
and a 20% to 40% reduction in en- II diabetes, despite normal BMD lev- clinical problem is required to obtain
ergy to fracture.42 However, the nor- els. a clear picture of this emerging con-
mal rate of turnover in the human The aforementioned cases series cern.
femoral shaft is low (<3% per year), have been refuted by a recent study
and it seems implausible that a fur- of the Danish National Hospital
ther reduction in this turnover rate Register.45 Abrahamsen et al45 could References
could be solely responsible for the in- find no data in this large registry
creased fracture risk. study to support the conclusion that Evidence-based Medicine: Levels of
Glycation of bone tissue has also long-term alendronate use was re- evidence are described in the table of
been implicated as a potential cause sponsible for an increase in the rate contents. In this article, references 9,
of femoral shaft fracture. As bone of atypical femur fractures. However, 20-28, 35, and 36 are level I studies.
tissue ages, the bone accumulates this study was based on discharge di- References 10, 19, and 34 are level II
products of processes leading to non- agnoses and did not include direct studies. References 17, 29, and 40
enzymatic glycation of the bone tis- patient or radiographic evaluation. are level III studies. References 11,
372 Journal of the American Academy of Orthopaedic Surgeons
Michael J. Weaver, MD, et al
37-39, and 45 are level IV studies. 14. Marx RE: Uncovering the cause of 25. Tonino RP, Meunier PJ, Emkey R, et al:
“phossy jaw” circa 1858 to 1906: Oral Skeletal benefits of alendronate: 7-year
References 12, 14, 15, and 18 are and maxillofacial surgery closed case treatment of postmenopausal
level V expert opinion. files-case closed. J Oral Maxillofac Surg osteoporotic women. Phase III
2008;66(11):2356-2363. Osteoporosis Treatment Study Group.
Citation numbers printed in bold J Clin Endocrinol Metab 2000;85(9):
15. Khosla S, Burr D, Cauley J, et al:
type indicate references published 3109-3115.
Bisphosphonate-associated osteonecrosis
within the past 5 years. of the jaw: Report of a task force of the 26. Bone HG, Hosking D, Devogelaer JP,
American Society for Bone and Mineral et al: Ten years’ experience with
1. Rodan GA, Fleisch HA: Bisphospho- Research. J Bone Miner Res 2007; alendronate for osteoporosis in
nates: Mechanisms of action. J Clin 22(10):1479-1491. postmenopausal women. N Engl J Med
Invest 1996;97(12):2692-2696. 2004;350(12):1189-1199.
16. US Food and Drug Administration:
2. Luckman SP, Hughes DE, Coxon FP, Information for Healthcare 27. Cranney A, Wells G, Willan A, et al:
Graham R, Russell G, Rogers MJ: Professionals: Bisphosphonates Meta-analyses of therapies for
Nitrogen-containing bisphosphonates (marketed as Actonel, Actonel+Ca, postmenopausal osteoporosis: II. Meta-
inhibit the mevalonate pathway and Aredia, Boniva, Didronel, Fosamax, analysis of alendronate for the treatment
prevent post-translational prenylation of of postmenopausal women. Endocr Rev
Fosamax+D, Reclast, Skelid, and
GTP-binding proteins, including Ras. 2002;23(4):508-516.
Zometa). Available at: http://
J Bone Miner Res 1998;13(4):581-589.
www.fda.gov/Drugs/DrugSafety/
28. Cranney A, Tugwell P, Adachi J, et al:
3. Jung A, Bisaz S, Fleisch H: The binding PostmarketDrugSafetyInformation Meta-analyses of therapies for
of pyrophosphate and two diphospho- forPatientsandProviders/ucm postmenopausal osteoporosis: III. Meta-
nates by hydroxyapatite crystals. Calcif 124165.htm. Accessed March 29, 2010. analysis of risedronate for the treatment
Tissue Res 1973;11(4):269-280. of postmenopausal osteoporosis. Endocr
17. Stepan JJ, Burr DB, Pavo I, et al: Low
4. Kasting GB, Francis MD: Retention of Rev 2002;23(4):517-523.
bone mineral density is associated with
etidronate in human, dog, and rat. bone microdamage accumulation in 29. Munns CF, Rauch F, Zeitlin L, Fassier F,
J Bone Miner Res 1992;7(5):513-522. postmenopausal women with Glorieux FH: Delayed osteotomy but not
5. Sato M, Grasser W, Endo N, et al: osteoporosis. Bone 2007;41(3):378-385. fracture healing in pediatric osteogenesis
Bisphosphonate action: Alendronate imperfecta patients receiving
18. Kuehn BM: Long-term risks of pamidronate. J Bone Miner Res 2004;
localization in rat bone and effects on bisphosphonates probed. JAMA 2009;
osteoclast ultrastructure. J Clin Invest 19(11):1779-1786.
301(7):710-711.
1991;88(6):2095-2105. 30. Matos MA, Araújo FP, Paixão FB: The
19. Cosman F, Nieves J, Wilkinson C, effect of zoledronate on bone remodeling
6. Azuma Y, Sato H, Oue Y, et al: Schnering D, Shen V, Lindsay R: Bone
Alendronate distributed on bone surfaces during the healing process. Acta Cir Bras
density change and biochemical indices 2007;22(2):115-119.
inhibits osteoclastic bone resorption in of skeletal turnover. Calcif Tissue Int
vitro and in experimental hypercalcemia 1996;58(4):236-243. 31. Amanat N, McDonald M, Godfrey C,
models. Bone 1995;16(2):235-245. Bilston L, Little D: Optimal timing of a
20. Black DM, Schwartz AV, Ensrud KE, single dose of zoledronic acid to increase
7. Fleisch H: Pharmacokinetics, in Fleisch et al: Effects of continuing or stopping
H, ed: Bisphosphonates in Bone Disease: strength in rat fracture repair. J Bone
alendronate after 5 years of treatment: Miner Res 2007;22(6):867-876.
From the Laboratory to the Patient. The Fracture Intervention Trial Long-
Berne, Switzerland, University of Berne, term Extension (FLEX). A randomized 32. Im GI, Qureshi SA, Kenney J, Rubash
1993, p 50. trial. JAMA 2006;296(24):2927-2938. HE, Shanbhag AS: Osteoblast
8. Lin JH: Bisphosphonates: A review of proliferation and maturation by
21. Black DM, Cummings SR, Karpf DB, bisphosphonates. Biomaterials 2004;
their pharmacokinetic properties. Bone et al: Randomised trial of effect of
1996;18(2):75-85. 25(18):4105-4115.
alendronate on risk of fracture in women
9. Physicians Desk Reference, ed 63. with existing vertebral fractures: 33. Huang RC, Khan SN, Sandhu HS, et al:
Montvale, NJ, Thomson Healthcare, Fracture Intervention Trial Research Alendronate inhibits spine fusion in a rat
2009. Group. Lancet 1996;348(9041):1535- model. Spine (Phila Pa 1976) 2005;
1541. 30(22):2516-2522.
10. Adami S, Mian M, Gatti P, et al: Effects
of two oral doses of alendronate in the 22. Cummings SR, Black DM, Thompson 34. Soininvaara TA, Jurvelin JS, Miettinen
treatment of Paget’s disease of bone. DE, et al: Effect of alendronate on risk of HJ, Suomalainen OT, Alhava EM,
Bone 1994;15(4):415-417. fracture in women with low bone density Kröger PJ: Effect of alendronate on
but without vertebral fractures: Results periprosthetic bone loss after total knee
11. Schussheim DH, Jacobs TP, Silverberg from the Fracture Intervention Trial. arthroplasty: A one-year, randomized,
SJ: Hypocalcemia associated with JAMA 1998;280(24):2077-2082. controlled trial of 19 patients. Calcif
alendronate. Ann Intern Med 1999; Tissue Int 2002;71(6):472-477.
130(4 pt 1):329. 23. Liberman UA, Weiss SR, Bröll J, et al:
Effect of oral alendronate on bone 35. Bhandari M, Bajammal S, Guyatt GH,
12. Fraunfelder FW, Fraunfelder FT: mineral density and the incidence of et al: Effect of bisphosphonates on
Bisphosphonates and ocular fractures in postmenopausal periprosthetic bone mineral density after
inflammation. N Engl J Med 2003; osteoporosis: The Alendronate Phase III total joint arthroplasty: A meta-analysis.
348(12):1187-1188. Osteoporosis Treatment Study Group. N J Bone Joint Surg Am 2005;87(2):293-
Engl J Med 1995;333(22):1437-1443. 301.
13. Black DM, Delmas PD, Eastell R, et al:
Once-yearly zoledronic acid for 24. Lyles KW, Colón-Emeric CS, Magaziner 36. Friedl G, Radl R, Stihsen C, Rehak P,
treatment of postmenopausal JS, et al: Zoledronic acid and clinical Aigner R, Windhager R: The effect of a
osteoporosis. N Engl J Med 2007; fractures and mortality after hip fracture. single infusion of zoledronic acid on
356(18):1809-1822. N Engl J Med 2007;357(18):1799-1809. early implant migration in total hip
June 2010, Vol 18, No 6 373
The Orthopaedic Implications of Diphosphonate Therapy
arthroplasty: A randomized, double- 40. Lenart BA, Neviaser AS, Lyman S, et al: 43. Vashishth D, Gibson GJ, Khoury JI,
blind, controlled trial. J Bone Joint Surg Association of low-energy femoral Schaffler MB, Kimura J, Fyhrie DP:
Am 2009;91(2):274-281. fractures with prolonged bisphosphonate Influence of nonenzymatic glycation on
use: A case control study. Osteoporos Int biomechanical properties of cortical
37. Odvina CV, Zerwekh JE, Rao DS,
2009;20(8):1353-1362. bone. Bone 2001;28(2):195-201.
Maalouf N, Gottschalk FA, Pak CY:
Severely suppressed bone turnover: A 41. Mashiba T, Hirano T, Turner CH, 44. Tang SY, Allen MR, Phipps R, Burr DB,
potential complication of alendronate Forwood MR, Johnston CC, Burr DB: Vashishth D: Changes in non-enzymatic
therapy. J Clin Endocrinol Metab 2005; Suppressed bone turnover by glycation and its association with altered
90(3):1294-1301.
bisphosphonates increases microdamage mechanical properties following 1-year
38. Goh SK, Yang KY, Koh JS, et al: accumulation and reduces some treatment with risedronate or
Subtrochanteric insufficiency fractures in biomechanical properties in dog rib. alendronate. Osteoporos Int 2009;20(6):
patients on alendronate therapy: A J Bone Miner Res 2000;15(4):613-620. 887-894.
caution. J Bone Joint Surg Br 2007;
89(3):349-353. 42. Allen MR, Iwata K, Phipps R, Burr DB: 45. Abrahamsen B, Eiken P, Eastell R:
Alterations in canine vertebral bone Subtrochanteric and diaphyseal femur
39. Neviaser AS, Lane JM, Lenart BA, turnover, microdamage accumulation, fractures in patients treated with
Edobor-Osula F, Lorich DG: Low-energy and biomechanical properties following alendronate: A register-based national
femoral shaft fractures associated with 1-year treatment with clinical treatment cohort study. J Bone Miner Res 2009;
alendronate use. J Orthop Trauma 2008; doses of risedronate or alendronate. 24(6):1095-1102.
22(5):346-350. Bone 2006;39(4):872-879.
374 Journal of the American Academy of Orthopaedic Surgeons
You might also like
- Oral and Intravenous Bisphosphonate–Induced Osteonecrosis of the Jaws: History, Etiology, Prevention, and Treatment, Second EditionFrom EverandOral and Intravenous Bisphosphonate–Induced Osteonecrosis of the Jaws: History, Etiology, Prevention, and Treatment, Second EditionNo ratings yet
- BiphosphonatesDocument14 pagesBiphosphonatesadrianajg.drNo ratings yet
- Articulo Bifosfonato en InglesDocument6 pagesArticulo Bifosfonato en InglesLeidy Marín SantanaNo ratings yet
- Bisphosphonates Marx OMS ClinicsDocument12 pagesBisphosphonates Marx OMS ClinicsDeb SNo ratings yet
- Katz 2005Document4 pagesKatz 2005Leonardo AmaralNo ratings yet
- Katz 2005Document4 pagesKatz 2005Leonardo AmaralNo ratings yet
- Bisphosphonate-Related Osteonecrosis of The Jaws: A Comprehensive ReviewDocument10 pagesBisphosphonate-Related Osteonecrosis of The Jaws: A Comprehensive Reviewiulian tigauNo ratings yet
- Thirunavukarasu 2015Document4 pagesThirunavukarasu 2015James Alexander Toruño GordonNo ratings yet
- Effects of Drugs in Orthodontic Tooth Movement: A ReviewDocument6 pagesEffects of Drugs in Orthodontic Tooth Movement: A ReviewvprakshaindiaNo ratings yet
- Bone Turnover Markers To Monitor Oral Bisphosphonate TherapyDocument6 pagesBone Turnover Markers To Monitor Oral Bisphosphonate Therapyhossein kasiriNo ratings yet
- University of Miami Division or Oral and Maxillofacial Surgery Position Paper On Drug Induced Osteonecrosis of The Jaws 2014Document26 pagesUniversity of Miami Division or Oral and Maxillofacial Surgery Position Paper On Drug Induced Osteonecrosis of The Jaws 2014Deb SNo ratings yet
- Antirresortivos y Necrosis en Madibula ElsevierDocument15 pagesAntirresortivos y Necrosis en Madibula Elsevierandreaelisa17No ratings yet
- Bisphosphonate Drug HolidayDocument5 pagesBisphosphonate Drug HolidayARNo ratings yet
- Tooth Socket HealingDocument16 pagesTooth Socket HealingluisNo ratings yet
- Bi Pos PhonateDocument24 pagesBi Pos PhonateBudhiNo ratings yet
- Iglesias-Linares Et Al. (2010)Document9 pagesIglesias-Linares Et Al. (2010)Laís C. PoletoNo ratings yet
- Bisphosonatesstatement PDFDocument4 pagesBisphosonatesstatement PDFiulian tigauNo ratings yet
- Long-Term and Sequential Treatment For Osteoporosis: EndocrinologyDocument14 pagesLong-Term and Sequential Treatment For Osteoporosis: EndocrinologyjoaovcfNo ratings yet
- Long-Term Outcome of Weekly Bisphosphonates: René Rizzoli, MDDocument5 pagesLong-Term Outcome of Weekly Bisphosphonates: René Rizzoli, MDMatthew PhillipsNo ratings yet
- The Dental Implication of Bisphosphonates RJNDocument10 pagesThe Dental Implication of Bisphosphonates RJNmaxfaxNo ratings yet
- Fluorescent Risedronate Analogue 800CW-PRISDocument17 pagesFluorescent Risedronate Analogue 800CW-PRISPhotios ZervasNo ratings yet
- Oral Osteonecrosis Induced by Drugs in A Multiple Myeloma PatientDocument4 pagesOral Osteonecrosis Induced by Drugs in A Multiple Myeloma Patientbraily_cardenasNo ratings yet
- Bisphosphonates: - Bisphosphonates (Also Called Diphosphonates) Are A Class of Drugs That Prevent The Loss of Bone MassDocument3 pagesBisphosphonates: - Bisphosphonates (Also Called Diphosphonates) Are A Class of Drugs That Prevent The Loss of Bone Massglaire927No ratings yet
- S105 ABSTRACTS / Bone 42 (2008) S17 - S110Document2 pagesS105 ABSTRACTS / Bone 42 (2008) S17 - S110cozcozNo ratings yet
- Dental Complications and Management of Patients On Bisphosphonate Therapy A Review ArticleDocument6 pagesDental Complications and Management of Patients On Bisphosphonate Therapy A Review ArticleyomiboyNo ratings yet
- Jhonatan - The Oncologist-2004-Green-3-13 PDFDocument11 pagesJhonatan - The Oncologist-2004-Green-3-13 PDFYipno Wanhar El MawardiNo ratings yet
- Freeman Hospital, Newcastle Upon Tyne, United KingdomDocument21 pagesFreeman Hospital, Newcastle Upon Tyne, United KingdomcozcozNo ratings yet
- BifosfonatosDocument6 pagesBifosfonatosAna Paulina Marquez LizarragaNo ratings yet
- Heifetz Li2019Document9 pagesHeifetz Li2019Anh KhoaNo ratings yet
- A ColabDocument10 pagesA ColabPopescu MariaNo ratings yet
- BisphosphonateDocument33 pagesBisphosphonatelavate amol bhimraoNo ratings yet
- NSAIDs in Orthodontic Tooth Movement, 2012Document4 pagesNSAIDs in Orthodontic Tooth Movement, 2012Tarif HamshoNo ratings yet
- Nutrients 14 03604 v2Document19 pagesNutrients 14 03604 v2Dr. Asif WaliNo ratings yet
- Cochrane Review Osteoporosis 2011Document9 pagesCochrane Review Osteoporosis 2011Sex & Gender Women's Health CollaborativeNo ratings yet
- Update On Bone Anabolics in Osteoporosis TreatmentDocument16 pagesUpdate On Bone Anabolics in Osteoporosis TreatmentSandra Janneth Perdomo LaraNo ratings yet
- Atypical Fracture With Long-Term Bisphosphonate Therapy Is Associated With Altered Cortical Composition and Reduced Fracture ResistanceDocument6 pagesAtypical Fracture With Long-Term Bisphosphonate Therapy Is Associated With Altered Cortical Composition and Reduced Fracture ResistanceSharan SahotaNo ratings yet
- Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Clinical Practice GuidelineDocument28 pagesPharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Clinical Practice GuidelineÁnh NguyễnNo ratings yet
- Anke 6222s.fullDocument10 pagesAnke 6222s.fullYipno Wanhar El MawardiNo ratings yet
- Revista Española de Cirugía Ortopédica y TraumatologíaDocument13 pagesRevista Española de Cirugía Ortopédica y TraumatologíaLuis socrates Quispe toledoNo ratings yet
- Ghid Tratament in Osteoporoza 2020Document28 pagesGhid Tratament in Osteoporoza 2020Simona ChiricăNo ratings yet
- How To Use BiphosphonatesDocument2 pagesHow To Use BiphosphonatesPablo IgnacioNo ratings yet
- Guia Manejo Osteoporosis 2019Document28 pagesGuia Manejo Osteoporosis 2019SMIBA MedicinaNo ratings yet
- Jper 0584Document11 pagesJper 0584LoredanaNo ratings yet
- The Use of Bisphosphonates in Children. Review of The Literature and Guidelines For Dental ManagementDocument11 pagesThe Use of Bisphosphonates in Children. Review of The Literature and Guidelines For Dental ManagementHemil Dario Rosales MolinaNo ratings yet
- Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Clinical Practice GuidelineDocument28 pagesPharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Clinical Practice GuidelineJulio Manuel Moreno SalcedoNo ratings yet
- Tto de La Osteoporosis - 2020Document16 pagesTto de La Osteoporosis - 2020GilbertoNo ratings yet
- J Oral Maxillofac Surg 2009. American Association of Oral Maxillofacial Surgeons Position Paper PDFDocument11 pagesJ Oral Maxillofac Surg 2009. American Association of Oral Maxillofacial Surgeons Position Paper PDFOctavian BoaruNo ratings yet
- Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Clinical Practice GuidelineDocument28 pagesPharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Clinical Practice GuidelineChon ChiNo ratings yet
- Medication Related Osteonecrosis of The JawDocument26 pagesMedication Related Osteonecrosis of The Jawapi-265532519100% (1)
- Geranylgeraniol in Managing Bisphosphonate-Related OsteonecrosisDocument12 pagesGeranylgeraniol in Managing Bisphosphonate-Related OsteonecrosisPhotios ZervasNo ratings yet
- Understanding Bisphosphonates and Osteonecrosis of The JawDocument9 pagesUnderstanding Bisphosphonates and Osteonecrosis of The JawGabriela OlateNo ratings yet
- Bisphosphonates ChildrenDocument17 pagesBisphosphonates Childrensheyla alegreNo ratings yet
- 2998-Article Text-8874-1-10-20190629Document3 pages2998-Article Text-8874-1-10-20190629Indra DhootNo ratings yet
- Is Dental Implant Placement Compatible in Patients Treated With BiphosphonatesDocument5 pagesIs Dental Implant Placement Compatible in Patients Treated With BiphosphonatesosiglesiNo ratings yet
- Managing Metastatic Bone Pain: The Role of Bisphosphonates: Review ArticleDocument11 pagesManaging Metastatic Bone Pain: The Role of Bisphosphonates: Review ArticlezainurhafizNo ratings yet
- Jco 19 02192Document11 pagesJco 19 02192giovanni nuñez nuñezNo ratings yet
- BifosfonatosyortodonciaDocument8 pagesBifosfonatosyortodonciavivigaitanNo ratings yet
- Drug Therapy in OrthodonticsDocument4 pagesDrug Therapy in OrthodonticsRicha AhlawatNo ratings yet
- Drug Treatment of Oral Sub Mucous Fibrosis - A Review PDFDocument3 pagesDrug Treatment of Oral Sub Mucous Fibrosis - A Review PDFAnamika AttrishiNo ratings yet
- Osteoporosis 2019Document28 pagesOsteoporosis 2019Diana Parra CárdenasNo ratings yet
- Neurology 2017 Feigin 2160 1Document3 pagesNeurology 2017 Feigin 2160 1royNo ratings yet
- IbandronatedrugscomDocument25 pagesIbandronatedrugscomroyNo ratings yet
- S 009 LBLDocument17 pagesS 009 LBLroyNo ratings yet
- Pal 2011Document6 pagesPal 2011royNo ratings yet
- IndianJPain33125-8620702 235647Document6 pagesIndianJPain33125-8620702 235647royNo ratings yet
- Bronko DilatorDocument30 pagesBronko DilatorroyNo ratings yet
- Movement DisordersDocument18 pagesMovement DisordersFaisal BudisasmitaNo ratings yet
- Breast MassDocument3 pagesBreast MassalhassanmohamedNo ratings yet
- Argireline Technical InformationDocument16 pagesArgireline Technical InformationAnonymous vfb5kkyJNo ratings yet
- Valvular Heart Disease: Bekele T. (MD)Document47 pagesValvular Heart Disease: Bekele T. (MD)alehegn beleteNo ratings yet
- Lesson 22: Diabetes Mellitus, Part 1 (Lesson Information) : Reading AssignmentDocument14 pagesLesson 22: Diabetes Mellitus, Part 1 (Lesson Information) : Reading AssignmentadaezeNo ratings yet
- Research Proposal - ICMR STS 2019 1. Title: Thyroid Auto-Immune Response in Pregnant Women With Gestational Diabetes Mellitus 2. ObjectiveDocument4 pagesResearch Proposal - ICMR STS 2019 1. Title: Thyroid Auto-Immune Response in Pregnant Women With Gestational Diabetes Mellitus 2. Objectivesiddarth reddyNo ratings yet
- DNA ReplicationDocument2 pagesDNA ReplicationFrancoise AngeliqueNo ratings yet
- Osmosis: Major Fluid CompartmentDocument9 pagesOsmosis: Major Fluid CompartmentMarielle ChuaNo ratings yet
- Spondylosis Cervical and LumbarDocument9 pagesSpondylosis Cervical and LumbarDr Aamir Yousuf AhangarNo ratings yet
- Memory Dysfunction.9Document14 pagesMemory Dysfunction.9Luis Antonio Cespedes HernandezNo ratings yet
- CT and MRI Contrast MediaDocument14 pagesCT and MRI Contrast MediadregleavNo ratings yet
- EtiologyEpilepsy2011ExpertRevNeur (Recovered)Document17 pagesEtiologyEpilepsy2011ExpertRevNeur (Recovered)ArwatiKilwowD'ctzGreenNo ratings yet
- Risperidone Drug StudyDocument2 pagesRisperidone Drug StudyBasema HashhashNo ratings yet
- Approach To Dyspepsia: Dr. Ghalia Abu MohsenDocument60 pagesApproach To Dyspepsia: Dr. Ghalia Abu MohsenMohammedNo ratings yet
- Successful Aging Puzzle PacketDocument36 pagesSuccessful Aging Puzzle Packetjudit19No ratings yet
- Retdem 1Document13 pagesRetdem 1Ryah Ryll MacuaNo ratings yet
- WCS 014 - Fever and Purulent Sputum - by DR JCM HoDocument47 pagesWCS 014 - Fever and Purulent Sputum - by DR JCM HoRachelMokNo ratings yet
- Paragonimus WestermaniDocument3 pagesParagonimus WestermaniHanisha EricaNo ratings yet
- Vasculitis SyndromesDocument56 pagesVasculitis SyndromesHengki Permana PutraNo ratings yet
- Optha Samplex and Recalls All inDocument51 pagesOptha Samplex and Recalls All inDey SibalNo ratings yet
- Endocrine Physio D& R AgamDocument76 pagesEndocrine Physio D& R Agamashrithapabba2850% (2)
- Acute Perforated AppendicitisDocument7 pagesAcute Perforated AppendicitisS3V4_9154No ratings yet
- Medical Ward 1 Service 2 CensusDocument13 pagesMedical Ward 1 Service 2 CensusJayricDepalobosNo ratings yet
- Parathyroid GlandDocument3 pagesParathyroid GlandElla OrtegaNo ratings yet
- Scalp Tumors: CME ArticleDocument3 pagesScalp Tumors: CME Articlenailatul fadhilaNo ratings yet
- Paritonitis PDFDocument21 pagesParitonitis PDFSidraNo ratings yet
- (OPHTHA) 7.1-Pediatric Ophthalmology-Strabismus and Amblyopia - Dr. AtienzaDocument14 pages(OPHTHA) 7.1-Pediatric Ophthalmology-Strabismus and Amblyopia - Dr. AtienzaMaria Gracia YamsonNo ratings yet
- Wa0007.Document47 pagesWa0007.KARLA JOHANNA TARIRA BARROSONo ratings yet
- Failure To Thrive (FTT) Atau: Gagal TumbuhDocument25 pagesFailure To Thrive (FTT) Atau: Gagal TumbuhSuryani MalikNo ratings yet
- Peripheral NeuropathyDocument16 pagesPeripheral NeuropathyKhaled OssamaNo ratings yet