Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
44 viewsAntimycobacterial Drugs NOTES PDF
Antimycobacterial Drugs NOTES PDF
Uploaded by
Mae Lislie Canonigo - FloresThis document discusses drugs used to treat tuberculosis, including isoniazid. It provides details on isoniazid such as its mechanism of action, inhibiting mycolic acid synthesis; basis for resistance, such as mutations in katG or inhA genes; recommended dosages; and potential adverse reactions like hepatitis. Combination therapy with two or more drugs is emphasized to prevent emergence of drug resistance, as mycobacteria are prone to developing resistance due to their slow growth.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- The APhA Complete Review For Pharmacy, 11th EditionDocument1,707 pagesThe APhA Complete Review For Pharmacy, 11th Editionمحمد حميدان90% (10)
- Case Study AssignmentDocument2 pagesCase Study AssignmentNida Ridzuan100% (2)
- Adult Infectious Disease Bulletpoints HandbookFrom EverandAdult Infectious Disease Bulletpoints HandbookRating: 4.5 out of 5 stars4.5/5 (9)
- Antimycobacterial Drugs: Camille E. Beauduy, Pharmd, & Lisa G. Winston, MDDocument17 pagesAntimycobacterial Drugs: Camille E. Beauduy, Pharmd, & Lisa G. Winston, MDRegine Coeli Menta LansanganNo ratings yet
- IsoniazidDocument2 pagesIsoniazidalmahiraNo ratings yet
- Chemotherapy of TB & LeprosyDocument11 pagesChemotherapy of TB & LeprosyReatul Karim NeetolNo ratings yet
- Anti TB DrugsDocument46 pagesAnti TB DrugsAlvin LaurenceNo ratings yet
- Antitubercular DrugsDocument7 pagesAntitubercular DrugsAhsan IbrahimNo ratings yet
- Antimycobacterial Drugs: Prajogo Wibowo パラジョゴウィボヲ Hang Tuah UniversityDocument48 pagesAntimycobacterial Drugs: Prajogo Wibowo パラジョゴウィボヲ Hang Tuah UniversityRafif AmirNo ratings yet
- Unit - 3Document39 pagesUnit - 3ujjwalNo ratings yet
- Anti TB DrugsDocument46 pagesAnti TB Drugs88AKKNo ratings yet
- DP On AglDocument12 pagesDP On AglDeepikaNo ratings yet
- Notes - Lec 20 - Antimycobacterial AgentsDocument14 pagesNotes - Lec 20 - Antimycobacterial AgentsChesmar MacapalaNo ratings yet
- Antimycobacterial DrugsDocument7 pagesAntimycobacterial Drugsنشط عقلكNo ratings yet
- Antimycobacterial DrugsDocument36 pagesAntimycobacterial Drugsmadhu bonamNo ratings yet
- Antimicrobial Agents - Disinfectants, Antiseptics, SterilantsDocument8 pagesAntimicrobial Agents - Disinfectants, Antiseptics, SterilantsPhilip Ryken YuNo ratings yet
- AminoglycosidesDocument41 pagesAminoglycosidesAshiqul IslamNo ratings yet
- TB TreatmentDocument58 pagesTB TreatmentNdayisaba CorneilleNo ratings yet
- Antibiotics in Veterinary UseDocument83 pagesAntibiotics in Veterinary Usehansmeet100% (1)
- Unit 3 - Cology 3Document25 pagesUnit 3 - Cology 3Shreyas ShreyuNo ratings yet
- Drug Study IsoniazidDocument3 pagesDrug Study IsoniazidJamil Lorca100% (4)
- Drugs Used To Treat: TuberculosisDocument46 pagesDrugs Used To Treat: TuberculosisDR AbidNo ratings yet
- AMINOGLYCOSIDESDocument45 pagesAMINOGLYCOSIDESAbdullah EmadNo ratings yet
- Newer Antibiotics: Guide: DR Saroja A ODocument51 pagesNewer Antibiotics: Guide: DR Saroja A OparahulNo ratings yet
- Antitubercalous AgentsDocument20 pagesAntitubercalous AgentsMaxamed Faarax XaashiNo ratings yet
- Drugs For Giardiasis: Cryptosporidium Parvum, Giardia LambliaDocument7 pagesDrugs For Giardiasis: Cryptosporidium Parvum, Giardia LambliaSmita DabadeNo ratings yet
- Aminoglycosides.: Chapter No. 02 Week # 07Document2 pagesAminoglycosides.: Chapter No. 02 Week # 07Alee Iz HarNo ratings yet
- Anti Tuberculosis DrugsDocument1 pageAnti Tuberculosis Drugsdan singh pimoliNo ratings yet
- Aminoglycosides 23099Document27 pagesAminoglycosides 23099TES SENNo ratings yet
- Recent Advances in The Treatment of SleDocument5 pagesRecent Advances in The Treatment of SleLakshya J BasumataryNo ratings yet
- Anti - TB DrugsupdatedDocument35 pagesAnti - TB DrugsupdatedgNo ratings yet
- Antitubercular DrugsDocument82 pagesAntitubercular Drugstum chrisNo ratings yet
- Reference: Chapter 47. Basic and Clinical Pharmacology - 13th Edition. Katzung and Trevor. Lec GuideDocument8 pagesReference: Chapter 47. Basic and Clinical Pharmacology - 13th Edition. Katzung and Trevor. Lec GuideselflessdoctorNo ratings yet
- Alternative Second-Line Drugs For TuberculosisDocument42 pagesAlternative Second-Line Drugs For TuberculosisAlvin LaurenceNo ratings yet
- AMINOGLYCOSIDEDocument18 pagesAMINOGLYCOSIDEVinayKumarNo ratings yet
- AMINOGLYCOSIDESDocument15 pagesAMINOGLYCOSIDESGareth BaleNo ratings yet
- Inhibitor of Bacterial Protein SynthesisDocument83 pagesInhibitor of Bacterial Protein SynthesisNdayisaba CorneilleNo ratings yet
- Department of Pharmacology: Prof. Dr. Asya RehmanDocument15 pagesDepartment of Pharmacology: Prof. Dr. Asya RehmanGareth BaleNo ratings yet
- PharmacologyDocument8 pagesPharmacologyfileacademicsNo ratings yet
- Anthelmintics PDFDocument26 pagesAnthelmintics PDFalihashebriNo ratings yet
- Anti Mycobacterial DrugsDocument16 pagesAnti Mycobacterial DrugsIqra NaeemNo ratings yet
- AntiviralDocument81 pagesAntiviralDheemanth veerlaNo ratings yet
- Pharma URO AminoglycosidesDocument8 pagesPharma URO AminoglycosidesHussein AlhaddadNo ratings yet
- Antibacterial Drugs: B.K. SatriyasaDocument56 pagesAntibacterial Drugs: B.K. SatriyasaVicNo ratings yet
- AminoglycosideDocument6 pagesAminoglycosidesaqibmunawar550No ratings yet
- College of Nursing: Pharmacological ManagementDocument3 pagesCollege of Nursing: Pharmacological ManagementAnika PleñosNo ratings yet
- AntiTBDocument22 pagesAntiTBvaishnavipillai03No ratings yet
- Antimycobacterial DrugsDocument4 pagesAntimycobacterial DrugsRani SujithNo ratings yet
- 12. Sizar et alDocument6 pages12. Sizar et allitbang.pbperdosri4No ratings yet
- Antibiotics & Analgesics Used in DentistryDocument4 pagesAntibiotics & Analgesics Used in DentistryDominique AbelaNo ratings yet
- Anti TBDocument68 pagesAnti TBGunjan YadavNo ratings yet
- Antifungal AgentsDocument41 pagesAntifungal AgentsSami YGNo ratings yet
- AntifungalsDocument28 pagesAntifungalsnandhini2k23No ratings yet
- Antibiotic RevirwDocument10 pagesAntibiotic RevirwYasser ElashryNo ratings yet
- MrsaDocument13 pagesMrsaPaula Grace MorfeNo ratings yet
- Aminoglycoside RevisionDocument33 pagesAminoglycoside Revision418024 LAILA FARIHATIN NISAKNo ratings yet
- 5 AminoglycosidesDocument7 pages5 AminoglycosidesNashat SaadiNo ratings yet
- Antituberculous DrugDocument29 pagesAntituberculous DrugMalueth AnguiNo ratings yet
- Antimicrobial Therapy in Veterinary MedicineFrom EverandAntimicrobial Therapy in Veterinary MedicineSteeve GiguèreRating: 4 out of 5 stars4/5 (1)
- Medicinal Plants: Microbial Interactions, Molecular Techniques and Therapeutic TrendsFrom EverandMedicinal Plants: Microbial Interactions, Molecular Techniques and Therapeutic TrendsNo ratings yet
- Antiviral Agents Notes PDFDocument41 pagesAntiviral Agents Notes PDFMae Lislie Canonigo - FloresNo ratings yet
- Antiviral Agents NotesDocument34 pagesAntiviral Agents NotesMae Lislie Canonigo - FloresNo ratings yet
- Antiprotozoal Drugs Notes PDFDocument26 pagesAntiprotozoal Drugs Notes PDFMae Lislie Canonigo - FloresNo ratings yet
- Antiprotozoal Drugs NotesDocument22 pagesAntiprotozoal Drugs NotesMae Lislie Canonigo - FloresNo ratings yet
- Bacteria MorphologyDocument6 pagesBacteria MorphologyMae Lislie Canonigo - FloresNo ratings yet
- Bacteria UltrastructureDocument7 pagesBacteria UltrastructureMae Lislie Canonigo - FloresNo ratings yet
- Assignment of Sedative HypnoticsDocument6 pagesAssignment of Sedative HypnoticsMae Lislie Canonigo - FloresNo ratings yet
- Seye 3optimization of The Anticonvulsant Activity of 2-Acetamido-N-Benzyl-2 - (5 - Methylfuran-2-Yl) Acetamide Using QSAR Modeling and Molecular Docking TechniquesDocument19 pagesSeye 3optimization of The Anticonvulsant Activity of 2-Acetamido-N-Benzyl-2 - (5 - Methylfuran-2-Yl) Acetamide Using QSAR Modeling and Molecular Docking TechniquesdavidNo ratings yet
- NorepinephrineDocument15 pagesNorepinephrineNTA UGC-NETNo ratings yet
- Energearadionics RatesDocument163 pagesEnergearadionics RatesRoberta & Thomas NormanNo ratings yet
- Code of Pharmaceutical Ethics: Shiva Kant Thakur M.Pharma (Pharmaceutics) 1 YearDocument7 pagesCode of Pharmaceutical Ethics: Shiva Kant Thakur M.Pharma (Pharmaceutics) 1 YearTulasee ReddiNo ratings yet
- Concept of Satvapatana A ReviewDocument2 pagesConcept of Satvapatana A ReviewBala Kiran GaddamNo ratings yet
- (2020) - Bipolar Disorders SeminarDocument16 pages(2020) - Bipolar Disorders SeminarAarón ParedesNo ratings yet
- Formularium Obat IGD 2019Document29 pagesFormularium Obat IGD 2019RaNo ratings yet
- Evaluation of Ophthalmic FormulationDocument15 pagesEvaluation of Ophthalmic FormulationDeepak100% (1)
- Emergency Trolley (Abc) ChecklistDocument64 pagesEmergency Trolley (Abc) ChecklistN.K. Ayu SuksmawatiNo ratings yet
- Drug Chart For PrintDocument1 pageDrug Chart For Printnikitapawar04052000No ratings yet
- Singultus 2Document8 pagesSingultus 2Tika AeNo ratings yet
- Leftover Drug Disposal - Customer Behavior, Pharmacist Recommendations, and Obstacles To Drug Take-Back Box ImplementationDocument10 pagesLeftover Drug Disposal - Customer Behavior, Pharmacist Recommendations, and Obstacles To Drug Take-Back Box ImplementationDenise Yanci DemiarNo ratings yet
- (Drugs and The Pharmaceutical Sciences) Myra L. Weiner and Lois A. Kotkoskie - Excipient Toxicity and Safety-CRC Press (1999) PDFDocument374 pages(Drugs and The Pharmaceutical Sciences) Myra L. Weiner and Lois A. Kotkoskie - Excipient Toxicity and Safety-CRC Press (1999) PDFNguyen TriNo ratings yet
- Pregabalin Hospital PharmacyDocument16 pagesPregabalin Hospital Pharmacyaditya100% (1)
- Assignment 1 Prescription Analysis and InterpretationDocument4 pagesAssignment 1 Prescription Analysis and InterpretationShannen CostoNo ratings yet
- Medical and Pharmacy Abbreviations (Sig Codes) : Abbreviation Meaning(s) CategoryDocument3 pagesMedical and Pharmacy Abbreviations (Sig Codes) : Abbreviation Meaning(s) Categoryscope 3901No ratings yet
- Ejhpharm 2021 002903 Inline Supplementary Material 3Document4 pagesEjhpharm 2021 002903 Inline Supplementary Material 3Putu DananjayaNo ratings yet
- NCM 106 Finals For PrintingDocument13 pagesNCM 106 Finals For PrintingJULIANNAH ATHENA MERCADONo ratings yet
- Botanic Drugs 1917 PDFDocument408 pagesBotanic Drugs 1917 PDFUkefácil Ukelele FacilónNo ratings yet
- Disorders of Na BalanceDocument24 pagesDisorders of Na BalanceElvis obajeNo ratings yet
- Psychosis DraftDocument9 pagesPsychosis DraftCHRISTINE JOY. MOLINANo ratings yet
- Ceftriaxone Product MonographDocument52 pagesCeftriaxone Product MonographSarmadNo ratings yet
- Drug TramadolDocument2 pagesDrug TramadolFlauros Ryu Jabien100% (2)
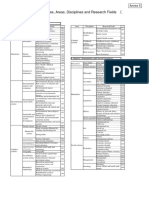
- Attached Table 1 List of Categories, Areas, Disciplines and Research FieldsDocument3 pagesAttached Table 1 List of Categories, Areas, Disciplines and Research FieldsJetro NonanNo ratings yet
- Uronephron Competitors: Product Name Company and Country of Origin Price Weak PointsDocument2 pagesUronephron Competitors: Product Name Company and Country of Origin Price Weak Pointsمصطفى الجبوريNo ratings yet
- Nanoparticulate Drug Delivery System: Mr. Sagar Kishor SavaleDocument101 pagesNanoparticulate Drug Delivery System: Mr. Sagar Kishor SavaleHemin H. MuhammadNo ratings yet
- Anticoagulant TherapyDocument41 pagesAnticoagulant Therapyryan yovanNo ratings yet
- Exogenous Ochronosis: Journal of Dermatological TreatmentDocument7 pagesExogenous Ochronosis: Journal of Dermatological TreatmentStella SunurNo ratings yet
Antimycobacterial Drugs NOTES PDF
Antimycobacterial Drugs NOTES PDF
Uploaded by
Mae Lislie Canonigo - Flores0 ratings0% found this document useful (0 votes)
44 views14 pagesThis document discusses drugs used to treat tuberculosis, including isoniazid. It provides details on isoniazid such as its mechanism of action, inhibiting mycolic acid synthesis; basis for resistance, such as mutations in katG or inhA genes; recommended dosages; and potential adverse reactions like hepatitis. Combination therapy with two or more drugs is emphasized to prevent emergence of drug resistance, as mycobacteria are prone to developing resistance due to their slow growth.
Original Description:
Original Title
Antimycobacterial Drugs NOTES.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses drugs used to treat tuberculosis, including isoniazid. It provides details on isoniazid such as its mechanism of action, inhibiting mycolic acid synthesis; basis for resistance, such as mutations in katG or inhA genes; recommended dosages; and potential adverse reactions like hepatitis. Combination therapy with two or more drugs is emphasized to prevent emergence of drug resistance, as mycobacteria are prone to developing resistance due to their slow growth.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
44 views14 pagesAntimycobacterial Drugs NOTES PDF
Antimycobacterial Drugs NOTES PDF
Uploaded by
Mae Lislie Canonigo - FloresThis document discusses drugs used to treat tuberculosis, including isoniazid. It provides details on isoniazid such as its mechanism of action, inhibiting mycolic acid synthesis; basis for resistance, such as mutations in katG or inhA genes; recommended dosages; and potential adverse reactions like hepatitis. Combination therapy with two or more drugs is emphasized to prevent emergence of drug resistance, as mycobacteria are prone to developing resistance due to their slow growth.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 14
ANTIMYCOBACTERIAL DRUGS The addition of pyrazinamide to an isoniazid-
rifampin combination for the first 2 months
Mycobacteria are intrinsically resistant to allows the total duration of therapy to be
most antibiotics. reduced to 6 months without loss of efficacy
Because they grow more slowly than other (Table 47–2).
bacteria, antibiotics that are most active In practice, therapy is usually initiated with a
against rapidly growing cells are relatively four-drug regimen of isoniazid, rifampin,
ineffective. pyrazinamide, and ethambutol until
Mycobacterial cells can also be dormant and susceptibility of the clinical isolate has been
thus completely resistant to many drugs or determined.
killed only very slowly. Neither ethambutol nor other drugs such as
The lipid-rich mycobacterial cell wall is streptomycin adds substantially to the
impermeable to many agents. overall activity of the regimen (ie, the
Mycobacterial species are intracellular duration of treatment cannot be further
pathogens, and organisms residing within reduced if another drug is used), but the
macrophages are inaccessible to drugs that fourth drug provides additional coverage if
penetrate these cells poorly. the isolate proves to be resistant to isoniazid,
Finally, mycobacteria are notorious for their rifampin, or both.
ability to develop resistance. The prevalence of isoniazid resistance among
Combinations of two or more drugs are clinical isolates in the United States is
required to overcome these obstacles and to approximately 10%.
prevent emergence of resistance during the Prevalence of resistance to both isoniazid
course of therapy. and rifampin (which is termed multidrug
The response of mycobacterial infections to resistance) is about 3%.
chemotherapy is slow, and treatment must Resistance to rifampin alone is rare.
be administered for months to years,
depending on which drugs are used.
The drugs used to treat tuberculosis, atypical
mycobacterial infections, and leprosy are
described in this chapter.
DRUGS USED IN TUBERCULOSIS
Isoniazid (INH), rifampin (or other rifamycin),
pyrazinamide, ethambutol, and streptomycin
are the traditional five first-line agents for
treatment of tuberculosis (Table 47–1).
Streptomycin is no longer recommended as
first-line therapy in most settings.
Isoniazid and rifampin are the most active
drugs.
An isoniazid-rifampin combination
administered for 9 months will cure 95–98%
of cases of tuberculosis caused by
susceptible strains.
ISONIAZID
Isoniazid is the most active drug for the
treatment of tuberculosis caused by
susceptible strains.
It is a small molecule (MW 137) that is
freely soluble in water. The structural
similarity to pyridoxine is shown below.
In vitro, isoniazid inhibits most tubercle
bacilli at a concentration of 0.2 mcg/mL or
less and is bactericidal for actively growing
tubercle bacilli.
It is less effective against atypical
mycobacterial species.
Isoniazid penetrates into macrophages
and is active against both extracellular and
intracellular organisms.
Mechanism of Action & Basis of Resistance
Isoniazid inhibits synthesis of mycolic
acids, which are essential components of
mycobacterial cell walls.
Isoniazid is a prodrug that is activated by
KatG, the mycobacterial catalase-
peroxidase.
The activated form of isoniazid forms a
covalent complex with an acyl carrier
protein (AcpM) and KasA, a beta-ketoacyl
carrier protein synthetase, which blocks
mycolic acid synthesis.
Resistance to isoniazid is associated with
mutations resulting in overexpression of
inhA, which encodes an NADH-dependent
acyl carrier protein reductase; mutation or
deletion of thekatG gene; promoter
mutations resulting in overexpression of
ahpC, a gene involved in protection of the
cell from oxidative stress; and mutations in
kasA.
Overproducers of inhA express low-level administered as a once-weekly dose or if
isoniazid resistance and cross-resistance there is malabsorption.
to ethionamide. Isoniazid metabolites and a small amount
KatG mutants express high-level isoniazid of unchanged drug are excreted mainly in
resistance and often are not cross-resistant the urine.
to ethionamide. The dosage need not be adjusted in renal
Drug-resistant mutants are normally failure.
present in susceptible mycobacterial Dose adjustment is not well defined in
populations at about 1 bacillus in 10 6 . patients with severe preexisting hepatic
Since tuberculous lesions often contain insufficiency and should be guided by
more than 10 8 tubercle bacilli, resistant serum concentrations if a reduction in
mutants are readily selected if isoniazid or dose is contemplated.
any other drug is given as a single agent. Clinical Uses
The use of two independently acting drugs The typical dosage of isoniazid is 5
in combination is much more effective. mg/kg/d; a typical adult dose is 300 mg
The probability that a bacillus is initially given once daily.
resistant to both drugs is approximately 1 Up to 10 mg/kg/d may be used for serious
in 10 6 × 10 6 , or 1 in 10 12 , several orders infections or if malabsorption is a problem.
of magnitude greater than the number of A 15 mg/kg dose, or 900 mg, may be used
infecting organisms. in a twice-weekly dosing regimen in
Thus, at least two (or more in certain cases) combination with a second
active agents should always be used to antituberculous agent (eg, rifampin, 600
treat active tuberculosis to prevent mg).
emergence of resistance during therapy. Pyridoxine, 25–50 mg/d, is recommended
Pharmacokinetics for those with conditions predisposing to
Isoniazid is readily absorbed from the neuropathy, an adverse effect of isoniazid.
gastrointestinal tract. Isoniazid is usually given by mouth but can
A 300 mg oral dose (5 mg/kg in children) be given parenterally in the same dosage.
achieves peak plasma concentrations of 3– Isoniazid as a single agent is also indicated
5 mcg/mL within 1–2 hours. for treatment of latent tuberculosis.
Isoniazid diffuses readily into all body The dosage is 300 mg/d (5 mg/kg/d) or
fluids and tissues. 900 mg twice weekly, and the duration is
The concentration in the central nervous usually 9 months.
system and cerebrospinal fluid ranges Adverse Reactions
between 20% and 100% of simultaneous The incidence and severity of untoward
serum concentrations. reactions to isoniazid are related to dosage
Metabolism of isoniazid, especially and duration of administration.
acetylation by liver N-acetyltransferase, is A. Immunologic Reactions
genetically determined (see Chapter 4). Fever and skin rashes are occasionally
The average plasma concentration of seen.
isoniazid in rapid acetylators is about one Drug-induced systemic lupus
third to one half of that in slow acetylators, erythematosus has been reported.
and average half-lives are less than 1 hour B. Direct Toxicity
and 3 hours, respectively. Isoniazid-induced hepatitis is the most
More rapid clearance of isoniazid by rapid common major toxic effect.
acetylators is usually of no therapeutic This is distinct from the minor increases in
consequence when appropriate doses are liver aminotransferases (up to three or four
administered daily, but subtherapeutic times normal), which do not require
concentrations may occur if drug is cessation of the drug and which are seen
in 10– 20% of patients, who usually are RIFAMPIN
asymptomatic. Rifampin is a semisynthetic derivative of
Clinical hepatitis with loss of appetite, rifamycin, an antibiotic produced by
nausea, vomiting, jaundice, and right Streptomyces mediterranei.
upper quadrant pain occurs in 1% of It is active in vitro against gram-positive
isoniazid recipients and can be fatal, and gram-negative cocci, some enteric
particularly if the drug is not discontinued bacteria, mycobacteria, and chlamydiae.
promptly. Susceptible organisms are inhibited by less
There is histologic evidence of than 1 mcg/mL.
hepatocellular damage and necrosis. Resistant mutants are present in all
The risk of hepatitis depends on age. It microbial populations at approximately 1
occurs rarely under age 20, in 0.3% of in 10 6 organisms and are rapidly selected
those aged 21–35, 1.2% of those aged 36– out if rifampin is used as a single drug,
50, and 2.3% for those aged 50 and above. especially in a patient with active infection.
The risk of hepatitis is greater in individuals There is no cross-resistance to other
with alcohol dependence and possibly classes of antimicrobial drugs, but there is
during pregnancy and the postpartum cross-resistance to other rifamycin
period. derivatives, eg, rifabutin and rifapentine.
Development of isoniazid hepatitis Mechanism of Action, Resistance, &
contraindicates further use of the drug. Pharmacokinetics
Peripheral neuropathy is observed in 10– Rifampin binds to the β subunit of bacterial
20% of patients given dosages greater DNA-dependent RNA polymerase and
than 5 mg/kg/d, but it is infrequently seen thereby inhibits RNA synthesis.
with the standard 300 mg adult dose. Resistance results from any one of several
Peripheral neuropathy is more likely to possible point mutations in rpoB, the gene
occur in slow acetylators and patients with for the β subunit of RNA polymerase.
predisposing conditions such as These mutations result in reduced binding
malnutrition, alcoholism, diabetes, AIDS, of rifampin to RNA polymerase.
and uremia. Human RNA polymerase does not bind
Neuropathy is due to a relative pyridoxine rifampin and is not inhibited by it.
deficiency. Rifampin is bactericidal for mycobacteria.
Isoniazid promotes excretion of It readily penetrates most tissues and
pyridoxine, and this toxicity is readily penetrates into phagocytic cells.
reversed by administration of pyridoxine in It can kill organisms that are poorly
a dosage as low as 10 mg/d. accessible to many other drugs, such as
Central nervous system toxicity, which is intracellular organisms and those
less common, includes memory loss, sequestered in abscesses and lung cavities.
psychosis, and seizures. Rifampin is well absorbed after oral
These effects may also respond to administration and excreted mainly
pyridoxine. through the liver into bile.
Miscellaneous other reactions include It then undergoes enterohepatic
hematologic abnormalities, provocation of recirculation, with the bulk excreted as a
pyridoxine deficiency anemia, tinnitus, and deacylated metabolite in feces and a small
gastrointestinal discomfort. amount excreted in the urine.
Isoniazid can reduce the metabolism of Dosage adjustment for renal or hepatic
phenytoin, increasing its blood level and insufficiency is not necessary.
toxicity. Usual doses result in serum levels of 5–7
mcg/mL.
Rifampin is distributed widely in body Rifampin may cause cholestatic jaundice
fluids and tissues. and occasionally hepatitis, and it
The drug is relatively highly protein- commonly causes light-chain proteinuria.
bound, and adequate cerebrospinal fluid If administered less often than twice
concentrations are achieved only in the weekly, rifampin may cause a flu-like
presence of meningeal inflammation. syndrome characterized by fever, chills,
Clinical Uses myalgias, anemia, and thrombocytopenia.
A. Mycobacterial Infections Its use has been associated with acute
Rifampin, usually 600 mg/d (10 mg/kg/d) tubular necrosis.
orally, must be administered with isoniazid Rifampin strongly induces most
or other antituberculous drugs to patients cytochrome P450 isoforms (CYP1A2, 2C9,
with active tuberculosis to prevent 2C19, 2D6, and 3A4), which increases the
emergence of drug-resistant elimination of numerous other drugs
mycobacteria. including methadone, anticoagulants,
In some short-course therapies, 600 mg of cyclosporine, some anticonvulsants,
rifampin is given twice weekly. protease inhibitors, some nonnucleoside
Rifampin, 600 mg daily or twice weekly for reverse transcriptase inhibitors,
6 months, also is effective in combination contraceptives, and a host of others (see
with other agents in some atypical Chapters 4 and 66).
mycobacterial infections and in leprosy. Co-administration of rifampin results in
Rifampin, 600 mg daily for 4 months as a significantly lower serum levels of these
single drug, is an alternative to isoniazid drugs.
for patients with latent tuberculosis who
are unable to take isoniazid or who have
had exposure to a case of active ETHAMBUTOL
tuberculosis caused by an isoniazid- Ethambutol is a synthetic, water-soluble,
resistant, rifampin-susceptible strain. heat-stable compound, the dextro-isomer
B. Other Indications of the structure shown below, dispensed
Rifampin has other uses in bacterial as the dihydrochloride salt.
infections.
An oral dosage of 600 mg twice daily for 2
days can eliminate meningococcal
carriage. Rifampin, 20 mg/kg/d for 4 days,
is used as prophylaxis in contacts of
children with Haemophilus influenzae type
b disease.
Rifampin combined with a second agent is
used to eradicate staphylococcal carriage. Mechanism of Action & Clinical Uses
Rifampin combination therapy is also Susceptible strains of Mycobacterium
indicated for treatment of serious tuberculosis and other mycobacteria are
staphylococcal infections such as inhibited in vitro by ethambutol, 1–5
osteomyelitis and prosthetic valve mcg/mL.
endocarditis. Ethambutol inhibits mycobacterial
Adverse Reactions arabinosyl transferases, which are encoded
Rifampin imparts a harmless orange color by the embCAB operon.
to urine, sweat, and tears (soft contact Arabinosyl transferases are involved in the
lenses may be permanently stained). polymerization reaction of arabinoglycan,
Occasional adverse effects include rashes, an essential component of the
thrombocytopenia, and nephritis. mycobacterial cell wall.
Resistance to ethambutol is due to Ethambutol is relatively contraindicated in
mutations resulting in overexpression of children too young to permit assessment
emb gene products or within the embB of visual acuity and red-green color
structural gene. discrimination.
Ethambutol is well absorbed from the gut.
After ingestion of 25 mg/kg, a blood level
peak of 2–5 mcg/mL is reached in 2–4 PYRAZINAMIDE
hours. Pyrazinamide (PZA) is a relative of
About 20% of the drug is excreted in feces nicotinamide, and it is used only for
and 50% in urine in unchanged form. treatment of tuberculosis.
Ethambutol accumulates in renal failure, It is stable and slightly soluble in water.
and the dose should be reduced by half if It is inactive at neutral pH, but at pH 5.5 it
creatinine clearance is less than 10 inhibits tubercle bacilli at concentrations
mL/min. of approximately 20 mcg/mL.
Ethambutol crosses the blood-brain The drug is taken up by macrophages and
barrier only when the meninges are exerts its activity against mycobacteria
inflamed. residing within the acidic environment of
Concentrations in cerebrospinal fluid are lysosomes.
highly variable, ranging from 4% to 64% of
serum levels in the setting of meningeal
inflammation.
As with all antituberculous drugs,
resistance to ethambutol emerges rapidly
when the drug is used alone.
Therefore, ethambutol is always given in
combination with other antituberculous
drugs.
Ethambutol hydrochloride, 15–25 mg/kg,
is usually given as a single daily dose in
combination with isoniazid or rifampin for
the treatment of active tuberculosis. Mechanism of Action & Clinical Uses
The higher dose may be used for Pyrazinamide is converted to pyrazinoic
treatment of tuberculous meningitis. acid—the active form of the drug—by
The dose of ethambutol is 50 mg/kg when mycobacterial pyrazinamidase, which is
a twice-weekly dosing schedule is used. encoded by pncA.
Adverse Reactions Pyrazinoic acid disrupts mycobacterial cell
Hypersensitivity to ethambutol is rare. membrane metabolism and transport
The most common serious adverse event functions.
is retrobulbar neuritis, resulting in loss of Resistance may be due to impaired uptake
visual acuity and red-green color of pyrazinamide or mutations in pncA that
blindness. impair conversion of PZA to its active form.
This dose-related adverse effect is more Serum concentrations of 30–50 mcg/mL at
likely to occur at dosages of 25 mg/kg/d 1–2 hours after oral administration are
continued for several months. achieved with dosages of 25 mg/kg/d.
At 15 mg/kg/d or less, visual disturbances Pyrazinamide is well absorbed from the
are very rare. gastrointestinal tract and widely
Periodic visual acuity testing is desirable if distributed in body tissues, including
the 25 mg/kg/d dosage is used. inflamed meninges.
The half-life is 8–11 hours.
The parent compound is metabolized by All large populations of tubercle bacilli
the liver, but metabolites are renally contain some streptomycin-resistant
cleared; therefore, PZA should be mutants.
administered at 25–35 mg/kg three times On average, 1 in 10 8 tubercle bacilli can
weekly (not daily) in hemodialysis patients be expected to be resistant to
and those in whom the creatinine streptomycin at levels of 10–100 mcg/mL.
clearance is less than 30 mL/min. Resistance may be due to a point mutation
In patients with normal renal function, a in either the rpsL gene encoding the S12
dose of 40–50 mg/kg is used for thrice- ribosomal protein or the rrs gene
weekly or twice-weekly treatment encoding 16S ribosomal RNA, which alters
regimens. the ribosomal binding site.
Pyrazinamide is an important front-line Streptomycin penetrates into cells poorly
drug used in conjunction with isoniazid and is active mainly against extracellular
and rifampin in short-course (ie, 6- month) tubercle bacilli.
regimens as a “sterilizing” agent active The drug crosses the blood-brain barrier
against residual intracellular organisms and achieves therapeutic concentrations
that may cause relapse. with inflamed meninges.
Tubercle bacilli develop resistance to Clinical Use in Tuberculosis
pyrazinamide fairly readily, but there is no Streptomycin sulfate is used when an
cross-resistance with isoniazid or other injectable drug is needed or desirable and
antimycobacterial drugs. in the treatment of infections resistant to
Adverse Reactions other drugs.
Major adverse effects of PZA include The usual dosage is 15 mg/kg/d
hepatotoxicity (in 1–5% of patients), intramuscularly or intravenously daily for
nausea, vomiting, drug fever, and adults (20–40 mg/kg/d, not to exceed 1–
hyperuricemia. 1.5 g for children) for several weeks,
The latter occurs uniformly and is not a followed by 1–1.5 g two or three times
reason to halt therapy. weekly for several months.
Hyperuricemia may provoke acute gouty Serum concentrations of approximately 40
arthritis. mcg/mL are achieved 30–60 minutes after
intramuscular injection of a 15 mg/kg
dose.
STREPTOMYCIN Other drugs are always given in
The mechanism of action and other combination to prevent emergence of
pharmacologic features of streptomycin resistance.
are discussed in Chapter 45. Adverse Reactions
The typical adult dosage is 1 g/d (15 Streptomycin is ototoxic and nephrotoxic.
mg/kg/d). Vertigo and hearing loss are the most
If the creatinine clearance is less than 30 common adverse effects and may be
mL/min or the patient is on hemodialysis, permanent.
the dosage is 15 mg/kg two or three times Toxicity is dose-related, and the risk is
per week. increased in the elderly.
Most tubercle bacilli are inhibited by As with all aminoglycosides, the dose must
streptomycin, 1–10 mcg/mL, in vitro. be adjusted according to renal function
Nontuberculosis species of mycobacteria (see Chapter 45).
other than Mycobacterium avium complex Toxicity can be reduced by limiting therapy
(MAC) andMycobacterium kansasii are to no more than 6 months whenever
resistant. possible.
SECOND-LINE DRUGS FOR TUBERCULOSIS
The alternative drugs listed below are usually
considered only
(1) in case of resistance to first-line agents;
(2) in case of failure of clinical response to
conventional therapy; and
(3) in case of serious treatment-limiting
adverse drug reactions.
Expert guidance to deal with the toxic effects
of these second-line drugs is desirable.
For many drugs listed in the following text,
the dosage, emergence of resistance, and
long-term toxicity have not been fully
established.
Capreomycin
Ethionamide Capreomycin is a peptide protein synthesis
Ethionamide is chemically related to inhibitor antibiotic obtained
isoniazid and similarly blocks the synthesis fromStreptomyces capreolus.
of mycolic acids. Daily injection of 1 g intramuscularly
It is poorly water soluble and available only results in blood levels of 10 mcg/mL or
in oral form. It is metabolized by the liver. more.
Most tubercle bacilli are inhibited in vitro Such concentrations in vitro are inhibitory
by ethionamide, 2.5 mcg/mL or less. for many mycobacteria, including
Some other species of mycobacteria also multidrug-resistant strains of M
are inhibited by ethionamide, 10 mcg/mL. tuberculosis.
Serum concentrations in plasma and Capreomycin (15 mg/kg/d) is an important
tissues of approximately 20 mcg/mL are injectable agent for treatment of drug-
achieved by a dosage of 1 g/d. resistant tuberculosis.
Cerebrospinal fluid concentrations are Strains ofM tuberculosis that are resistant
equal to those in serum. to streptomycin or amikacin usually are
Ethionamide is administered at an initial susceptible to capreomycin.
dose of 250 mg once daily, which is Resistance to this drug, when it occurs,
increased in 250-mg increments to the may be due to an rrs mutation.
recommended dosage of 1 g/d (or 15 Capreomycin is nephrotoxic and ototoxic.
mg/kg/d), if possible. Tinnitus, deafness, and vestibular
The 1 g/d dosage, though theoretically disturbances occur.
desirable, is poorly tolerated because of The injection causes significant local pain,
gastric irritation and neurologic and sterile abscesses may develop.
symptoms, often limiting the tolerable Dosing of capreomycin is the same as that
daily dose to 500–750 mg. of streptomycin.
Ethionamide is also hepatotoxic. Toxicity is reduced if 1 g is given two or
Neurologic symptoms may be alleviated three times weekly after an initial response
by pyridoxine. has been achieved with a daily dosing
Resistance to ethionamide as a single schedule.
agent develops rapidly in vitro and in vivo.
There can be low-level cross-resistance
between isoniazid and ethionamide.
Cycloserine as the acetylated compound and other
Cycloserine is an inhibitor of cell wall metabolic products.
synthesis and is discussed in Chapter 43. Very high concentrations of aminosalicylic
Concentrations of 15–20 mcg/mL inhibit acid are reached in the urine, which can
many strains of M tuberculosis. result in crystalluria.
The dosage of cycloserine in tuberculosis Aminosalicylic acid is used infrequently
is 0.5–1 g/d in two divided oral doses. because other oral drugs are better
This drug is cleared renally, and the dose tolerated.
should be reduced by half if creatinine Gastrointestinal symptoms are common
clearance is less than 50 mL/min. and may be diminished by giving the drug
The most serious toxic effects are with meals and with antacids.
peripheral neuropathy and central nervous Peptic ulceration and hemorrhage may
system dysfunction, including depression occur.
and psychotic reactions. Hypersensitivity reactions manifested by
Pyridoxine, 150 mg/d, should be given fever, joint pains, skin rashes,
with cycloserine because this ameliorates hepatosplenomegaly, hepatitis,
neurologic toxicity. adenopathy, and granulocytopenia often
Adverse effects, which are most common occur after 3–8 weeks of PAS therapy,
during the first 2 weeks of therapy, occur making it necessary to stop administration
in 25% or more of patients, especially at temporarily or permanently.
higher doses.
Adverse effects can be minimized by
monitoring peak serum concentrations.
The peak concentration is reached 2–4
hours after dosing.
The recommended range of peak
concentrations is 20–40 mcg/Ml.
Aminosalicylic Acid (PAS)
Aminosalicylic acid is a folate synthesis
antagonist that is active almost exclusively
against M tuberculosis.
It is structurally similar to p-amino-benzoic
acid (PABA) and to the sulfonamides (see Kanamycin & Amikacin
Chapter 46). The aminoglycoside antibiotics are
Tubercle bacilli are usually inhibited in discussed inChapter 45.
vitro by aminosalicylic acid, 1–5 mcg/mL. Kanamycin had been used for treatment of
Aminosalicylic acid is readily absorbed tuberculosis caused by streptomycin-
from the gastrointestinal tract. resistant strains, but the availability of less
Serum levels are 50 mcg/mL or more after toxic alternatives (eg, capreomycin and
a 4 g oral dose. amikacin) has rendered it obsolete.
The dosage is 8–12 g/d orally for adults Amikacin is playing a greater role in the
and 300 mg/kg/d for children. treatment of tuberculosis due to the
The drug is widely distributed in tissues prevalence of multidrug-resistant strains.
and body fluids except the cerebrospinal Prevalence of amikacin-resistant strains is
fluid. low (< 5%), and most multidrug-resistant
Aminosalicylic acid is rapidly excreted in strains remain amikacin-susceptible.
the urine, in part as active PAS and in part
M tuberculosis is inhibited at fluoroquinolone is used as a single agent;
concentrations of 1 mcg/mL or less. thus, the drug must be used in
Amikacin is also active against atypical combination with two or more other active
mycobacteria. agents.
There is no cross-resistance between The standard dosage of ciprofloxacin is
streptomycin and amikacin, but kanamycin 750 mg orally twice a day.
resistance often indicates resistance to The dosage of levofloxacin is 500–750 mg
amikacin as well. once a day.
Serum concentrations of 30–50 mcg/mL The dosage of moxifloxacin is 400 mg once
are achieved 30–60 minutes after a 15 a day.
mg/kg intravenous infusion.
Amikacin is indicated for treatment of
tuberculosis suspected or known to be Linezolid
caused by streptomycin-resistant or Linezolid (discussed inChapter 44) inhibits
multidrug-resistant strains. strains of M tuberculosis in vitro at
This drug must be used in combination concentrations of 4–8 mcg/mL.
with at least one and preferably two or It achieves good intracellular
three other drugs to which the isolate is concentrations, and it is active in murine
susceptible for treatment of drug-resistant models of tuberculosis.
cases. Linezolid has been used in combination
The recommended dosages are the same with other second- and third-line drugs to
as those for streptomycin. treat patients with tuberculosis caused by
multidrug-resistant strains.
Conversion of sputum cultures to negative
was associated with linezolid use in these
cases.
Fluoroquinolones Significant adverse effects, including bone
In addition to their activity against many marrow suppression and irreversible
gram-positive and gram-negative bacteria
peripheral and optic neuropathy, have
(discussed in Chapter 46), ciprofloxacin, been reported with the prolonged courses
levofloxacin, gatifloxacin, and moxifloxacin of therapy that are necessary for treatment
inhibit strains of M tuberculosis at of tuberculosis.
concentrations less than 2 mcg/mL. A 600 mg (adult) dose administered once
They are also active against atypical a day (half of that used for treatment of
mycobacteria. other bacterial infections) seems to be
Moxifloxacin is the most active againstM sufficient and may limit the occurrence of
tuberculosis in vitro. these adverse effects.
Levofloxacin tends to be slightly more Although linezolid may prove to be an
active than ciprofloxacin against M important new agent for treatment of
tuberculosis, whereas ciprofloxacin is tuberculosis, at this point it should only be
slightly more active against atypical used for multidrug-resistant strains that
mycobacteria. also are resistant to several other first- and
Fluoroquinolones are an important second-line agents.
addition to the drugs available for
tuberculosis, especially for strains that are
resistant to first-line agents. Rifabutin
Resistance, which may result from one of Rifabutin is derived from rifamycin and is
several single point mutations in the related to rifampin.
gyrase A subunit, develops rapidly if a
It has significant activity againstM susceptible strains during the continuation
tuberculosis, MAC, and Mycobacterium phase only (ie, after the first 2 months of
fortuitum (see below). therapy and ideally after conversion of
Its activity is similar to that of rifampin, and sputum cultures to negative).
cross-resistance with rifampin is virtually Rifapentine should not be used to treat
complete. patients with HIV infection because of an
Some rifampin-resistant strains may unacceptably high relapse rate with
appear susceptible to rifabutin in vitro, but rifampin-resistant organisms.
a clinical response is unlikely because the Rifapentine, given once weekly for 3
molecular basis of resistance, rpoB months in combination with isoniazid, is
mutation, is the same. an effective short course treatment for
Rifabutin is both substrate and inducer of latent tuberculosis infection.
cytochrome P450 enzymes.
Because it is a less potent inducer, rifabutin
is indicated in place of rifampin for Bedaquiline
treatment of tuberculosis in patients with Bedaquiline, a diarylquinoline, is the first
HIV infection who are receiving drug with a novel mechanism of action
antiretroviral therapy with a protease against M tuberculosis to be approved
inhibitor or a nonnucleoside reverse since 1971.
transcriptase inhibitor (eg, efavirenz), Bedaquiline inhibits adenosine 5′-
drugs that also are cytochrome P450 triphosphate (ATP) synthase in
substrates. mycobacteria, has in vitro activity against
The typical dosage of rifabutin is 300 mg/d both replicating and nonreplicating bacilli,
unless the patient is receiving a protease and has bactericidal and sterilizing activity
inhibitor, in which case the dosage should in the murine model of tuberculosis.
be reduced. No cross-resistance has been found
If efavirenz (also a cytochrome P450 between bedaquiline and other
inducer) is used, the recommended medications used to treat tuberculosis.
dosage of rifabutin is 450 mg/d. Peak plasma concentration and plasma
exposure of bedaquiline increase
approximately twofold when administered
Rifapentine with high-fat food.
Rifapentine is an analog of rifampin. Bedaquiline is highly protein-bound (>
It is active against bothM tuberculosis and 99%), is metabolized chiefly through the
MAC. cytochrome P450 system, and is excreted
As with all rifamycins, it is a bacterial RNA primarily via the feces.
polymerase inhibitor, and cross-resistance The mean terminal half-life of bedaquiline
between rifampin and rifapentine is and its major metabolite (M2), which is
complete. four to six times less active in terms of
Like rifampin, rifapentine is a potent antimycobacterial potency, is
inducer of cytochrome P450 enzymes, and approximately 5.5 months.
it has the same drug interaction profile. This long elimination phase probably
Toxicity is similar to that of rifampin. reflects slow release of bedaquiline and
Rifapentine and its microbiologically active M2 from peripheral tissues.
metabolite, 25-desacetylrifapentine, have CYP3A4 is the major isoenzyme involved in
an elimination half-life of 13 hours. the metabolism of bedaquiline and potent
Rifapentine, 600 mg (10 mg/kg) once or inhibitors or inducers of this enzyme cause
twice weekly, is indicated for treatment of clinically significant drug interactions.
tuberculosis caused by rifampin-
Current recommendations state that A three-drug combination of isoniazid,
bedaquiline, in combination with at least rifampin, and ethambutol is the conventional
three other active medications, may be treatment for M kansasii infection.
used for 24 weeks of treatment in adults A few representative pathogens, with the
with laboratory-confirmed pulmonary clinical presentation and the drugs to which
tuberculosis if the isolate is resistant to they are often susceptible, are given in Table
both isoniazid and rifampin.
47–3.
The recommended dosage for bedaquiline
M avium complex (MAC), which includes
is 400 mg once daily orally for 2 weeks,
bothM avium and M intracellulare, is an
followed by 200 mg three times a week for
22 weeks taken orally with food in order to important and common cause of
maximize absorption. disseminated disease in late stages of AIDS
Bedaquiline has been associated with both (CD4 counts < 50/μL).
hepatotoxicity and cardiac toxicity MAC is much less susceptible thanM
(prolongation of the QTc interval), so tuberculosis to most antituberculous drugs.
patients must be closely monitored during Combinations of agents are required to
treatment. suppress the infection.
Azithromycin, 500 mg once daily, or
DRUGS ACTIVE AGAINST ATYPICAL clarithromycin, 500 mg twice daily, plus
MYCOBACTERIA ethambutol, 15–25 mg/kg/d, is an effective
and well-tolerated regimen for treatment of
Many mycobacterial infections seen in disseminated disease.
clinical practice in the United States are Some authorities recommend use of a third
caused by nontuberculous or “atypical” agent, especially rifabutin, 300 mg once daily.
mycobacteria. Other agents that may be useful are listed in
These organisms have distinctive laboratory Table 47–3.
characteristics, are present in the Azithromycin and clarithromycin are the
environment, and are generally not prophylactic drugs of choice for preventing
communicable from person to person. disseminated MAC in AIDS patients with CD4
As a rule, these mycobacterial species are less cell counts less than 50/μL.
susceptible than M tuberculosis to Rifabutin in a single daily dose of 300 mg has
antituberculous drugs. been shown to reduce the incidence of MAC
On the other hand, agents such as bacteremia but is less effective than
macrolides, sulfonamides, and tetracyclines, macrolides.
which are not active against M tuberculosis,
may be effective for infections caused by
atypical mycobacteria.
Emergence of resistance during therapy is
also a problem with these mycobacterial
species, and active infection should be
treated with combinations of drugs.
M kansasii is susceptible to rifampin and
DRUGS USED IN LEPROSY
ethambutol, partially susceptible to isoniazid,
and completely resistant to pyrazinamide.
Mycobacterium leprae has never been grown
in vitro, but animal models, such as growth in
injected mouse footpads, have permitted The usual adult dosage in leprosy is
laboratory evaluation of drugs. 100 mg daily.
Only those drugs with the widest clinical use For children, the dose is
are presented here. proportionately less, depending on
Because of increasing reports of dapsone weight.
resistance, treatment of leprosy with Dapsone is usually well tolerated.
Many patients develop some
combinations of the drugs listed below is
hemolysis, particularly if they have
recommended.
glucose-6- phosphate dehydrogenase
DAPSONE & OTHER SULFONES deficiency.
Several drugs closely related to the Methemoglobinemia is common but
sulfonamides have been used usually is not a problem clinically.
effectively in the long-term treatment Gastrointestinal intolerance, fever,
of leprosy. pruritus, and various rashes occur.
The most widely used is dapsone During dapsone therapy of
(diaminodiphenylsulfone). Like the lepromatous leprosy, erythema
sulfonamides, it inhibits folate nodosum leprosum often develops.
synthesis. It is sometimes difficult to distinguish
Resistance can emerge in large reactions to dapsone from
populations of M leprae, eg, in manifestations of the underlying
lepromatous leprosy, particularly if low illness.
doses are given. Erythema nodosum leprosum may be
Therefore, the combination of suppressed by thalidomide (see
dapsone, rifampin, and clofazimine is Chapter 55).
recommended for initial therapy of
lepromatous leprosy.
A combination of dapsone plus
rifampin is commonly used for leprosy
with a lower organism burden.
Dapsone may also be used to prevent
and treat Pneumocystis jiroveci
pneumonia in AIDS patients.
Sulfones are well absorbed from the
gut and widely distributed throughout
body fluids and tissues. RIFAMPIN
Dapsone’s half-life is 1–2 days, and Rifampin (see earlier discussion) in a
drug tends to be retained in skin, dosage of 600 mg daily is highly effective
muscle, liver, and kidney. in leprosy and is given with at least one
Skin heavily infected with M leprae other drug to prevent emergence of
may contain several times more drug resistance.
than normal skin. Even a dose of 600 mg per month may be
Sulfones are excreted into bile and beneficial in combination therapy.
reabsorbed in the intestine.
Excretion into urine is variable, and
CLOFAZIMINE
most excreted drug is acetylated.
Clofazimine is a phenazine dye used in the
In renal failure, the dose may have to
treatment of multibacillary leprosy, which
be adjusted.
is defined as having a positive smear from
any site of infection.
Its mechanism of action has not been
clearly established.
Absorption of clofazimine from the gut is
variable, and a major portion of the drug is
excreted in feces.
Clofazimine is stored widely in
reticuloendothelial tissues and skin, and its
crystals can be seen inside phagocytic
reticuloendothelial cells.
It is slowly released from these deposits, so
the serum half-life may be 2 months.
A common dosage of clofazimine is 100
mg/d orally.
The most prominent untoward effect is
discoloration of the skin and conjunctivae.
Gastrointestinal side effects are also
common.
You might also like
- The APhA Complete Review For Pharmacy, 11th EditionDocument1,707 pagesThe APhA Complete Review For Pharmacy, 11th Editionمحمد حميدان90% (10)
- Case Study AssignmentDocument2 pagesCase Study AssignmentNida Ridzuan100% (2)
- Adult Infectious Disease Bulletpoints HandbookFrom EverandAdult Infectious Disease Bulletpoints HandbookRating: 4.5 out of 5 stars4.5/5 (9)
- Antimycobacterial Drugs: Camille E. Beauduy, Pharmd, & Lisa G. Winston, MDDocument17 pagesAntimycobacterial Drugs: Camille E. Beauduy, Pharmd, & Lisa G. Winston, MDRegine Coeli Menta LansanganNo ratings yet
- IsoniazidDocument2 pagesIsoniazidalmahiraNo ratings yet
- Chemotherapy of TB & LeprosyDocument11 pagesChemotherapy of TB & LeprosyReatul Karim NeetolNo ratings yet
- Anti TB DrugsDocument46 pagesAnti TB DrugsAlvin LaurenceNo ratings yet
- Antitubercular DrugsDocument7 pagesAntitubercular DrugsAhsan IbrahimNo ratings yet
- Antimycobacterial Drugs: Prajogo Wibowo パラジョゴウィボヲ Hang Tuah UniversityDocument48 pagesAntimycobacterial Drugs: Prajogo Wibowo パラジョゴウィボヲ Hang Tuah UniversityRafif AmirNo ratings yet
- Unit - 3Document39 pagesUnit - 3ujjwalNo ratings yet
- Anti TB DrugsDocument46 pagesAnti TB Drugs88AKKNo ratings yet
- DP On AglDocument12 pagesDP On AglDeepikaNo ratings yet
- Notes - Lec 20 - Antimycobacterial AgentsDocument14 pagesNotes - Lec 20 - Antimycobacterial AgentsChesmar MacapalaNo ratings yet
- Antimycobacterial DrugsDocument7 pagesAntimycobacterial Drugsنشط عقلكNo ratings yet
- Antimycobacterial DrugsDocument36 pagesAntimycobacterial Drugsmadhu bonamNo ratings yet
- Antimicrobial Agents - Disinfectants, Antiseptics, SterilantsDocument8 pagesAntimicrobial Agents - Disinfectants, Antiseptics, SterilantsPhilip Ryken YuNo ratings yet
- AminoglycosidesDocument41 pagesAminoglycosidesAshiqul IslamNo ratings yet
- TB TreatmentDocument58 pagesTB TreatmentNdayisaba CorneilleNo ratings yet
- Antibiotics in Veterinary UseDocument83 pagesAntibiotics in Veterinary Usehansmeet100% (1)
- Unit 3 - Cology 3Document25 pagesUnit 3 - Cology 3Shreyas ShreyuNo ratings yet
- Drug Study IsoniazidDocument3 pagesDrug Study IsoniazidJamil Lorca100% (4)
- Drugs Used To Treat: TuberculosisDocument46 pagesDrugs Used To Treat: TuberculosisDR AbidNo ratings yet
- AMINOGLYCOSIDESDocument45 pagesAMINOGLYCOSIDESAbdullah EmadNo ratings yet
- Newer Antibiotics: Guide: DR Saroja A ODocument51 pagesNewer Antibiotics: Guide: DR Saroja A OparahulNo ratings yet
- Antitubercalous AgentsDocument20 pagesAntitubercalous AgentsMaxamed Faarax XaashiNo ratings yet
- Drugs For Giardiasis: Cryptosporidium Parvum, Giardia LambliaDocument7 pagesDrugs For Giardiasis: Cryptosporidium Parvum, Giardia LambliaSmita DabadeNo ratings yet
- Aminoglycosides.: Chapter No. 02 Week # 07Document2 pagesAminoglycosides.: Chapter No. 02 Week # 07Alee Iz HarNo ratings yet
- Anti Tuberculosis DrugsDocument1 pageAnti Tuberculosis Drugsdan singh pimoliNo ratings yet
- Aminoglycosides 23099Document27 pagesAminoglycosides 23099TES SENNo ratings yet
- Recent Advances in The Treatment of SleDocument5 pagesRecent Advances in The Treatment of SleLakshya J BasumataryNo ratings yet
- Anti - TB DrugsupdatedDocument35 pagesAnti - TB DrugsupdatedgNo ratings yet
- Antitubercular DrugsDocument82 pagesAntitubercular Drugstum chrisNo ratings yet
- Reference: Chapter 47. Basic and Clinical Pharmacology - 13th Edition. Katzung and Trevor. Lec GuideDocument8 pagesReference: Chapter 47. Basic and Clinical Pharmacology - 13th Edition. Katzung and Trevor. Lec GuideselflessdoctorNo ratings yet
- Alternative Second-Line Drugs For TuberculosisDocument42 pagesAlternative Second-Line Drugs For TuberculosisAlvin LaurenceNo ratings yet
- AMINOGLYCOSIDEDocument18 pagesAMINOGLYCOSIDEVinayKumarNo ratings yet
- AMINOGLYCOSIDESDocument15 pagesAMINOGLYCOSIDESGareth BaleNo ratings yet
- Inhibitor of Bacterial Protein SynthesisDocument83 pagesInhibitor of Bacterial Protein SynthesisNdayisaba CorneilleNo ratings yet
- Department of Pharmacology: Prof. Dr. Asya RehmanDocument15 pagesDepartment of Pharmacology: Prof. Dr. Asya RehmanGareth BaleNo ratings yet
- PharmacologyDocument8 pagesPharmacologyfileacademicsNo ratings yet
- Anthelmintics PDFDocument26 pagesAnthelmintics PDFalihashebriNo ratings yet
- Anti Mycobacterial DrugsDocument16 pagesAnti Mycobacterial DrugsIqra NaeemNo ratings yet
- AntiviralDocument81 pagesAntiviralDheemanth veerlaNo ratings yet
- Pharma URO AminoglycosidesDocument8 pagesPharma URO AminoglycosidesHussein AlhaddadNo ratings yet
- Antibacterial Drugs: B.K. SatriyasaDocument56 pagesAntibacterial Drugs: B.K. SatriyasaVicNo ratings yet
- AminoglycosideDocument6 pagesAminoglycosidesaqibmunawar550No ratings yet
- College of Nursing: Pharmacological ManagementDocument3 pagesCollege of Nursing: Pharmacological ManagementAnika PleñosNo ratings yet
- AntiTBDocument22 pagesAntiTBvaishnavipillai03No ratings yet
- Antimycobacterial DrugsDocument4 pagesAntimycobacterial DrugsRani SujithNo ratings yet
- 12. Sizar et alDocument6 pages12. Sizar et allitbang.pbperdosri4No ratings yet
- Antibiotics & Analgesics Used in DentistryDocument4 pagesAntibiotics & Analgesics Used in DentistryDominique AbelaNo ratings yet
- Anti TBDocument68 pagesAnti TBGunjan YadavNo ratings yet
- Antifungal AgentsDocument41 pagesAntifungal AgentsSami YGNo ratings yet
- AntifungalsDocument28 pagesAntifungalsnandhini2k23No ratings yet
- Antibiotic RevirwDocument10 pagesAntibiotic RevirwYasser ElashryNo ratings yet
- MrsaDocument13 pagesMrsaPaula Grace MorfeNo ratings yet
- Aminoglycoside RevisionDocument33 pagesAminoglycoside Revision418024 LAILA FARIHATIN NISAKNo ratings yet
- 5 AminoglycosidesDocument7 pages5 AminoglycosidesNashat SaadiNo ratings yet
- Antituberculous DrugDocument29 pagesAntituberculous DrugMalueth AnguiNo ratings yet
- Antimicrobial Therapy in Veterinary MedicineFrom EverandAntimicrobial Therapy in Veterinary MedicineSteeve GiguèreRating: 4 out of 5 stars4/5 (1)
- Medicinal Plants: Microbial Interactions, Molecular Techniques and Therapeutic TrendsFrom EverandMedicinal Plants: Microbial Interactions, Molecular Techniques and Therapeutic TrendsNo ratings yet
- Antiviral Agents Notes PDFDocument41 pagesAntiviral Agents Notes PDFMae Lislie Canonigo - FloresNo ratings yet
- Antiviral Agents NotesDocument34 pagesAntiviral Agents NotesMae Lislie Canonigo - FloresNo ratings yet
- Antiprotozoal Drugs Notes PDFDocument26 pagesAntiprotozoal Drugs Notes PDFMae Lislie Canonigo - FloresNo ratings yet
- Antiprotozoal Drugs NotesDocument22 pagesAntiprotozoal Drugs NotesMae Lislie Canonigo - FloresNo ratings yet
- Bacteria MorphologyDocument6 pagesBacteria MorphologyMae Lislie Canonigo - FloresNo ratings yet
- Bacteria UltrastructureDocument7 pagesBacteria UltrastructureMae Lislie Canonigo - FloresNo ratings yet
- Assignment of Sedative HypnoticsDocument6 pagesAssignment of Sedative HypnoticsMae Lislie Canonigo - FloresNo ratings yet
- Seye 3optimization of The Anticonvulsant Activity of 2-Acetamido-N-Benzyl-2 - (5 - Methylfuran-2-Yl) Acetamide Using QSAR Modeling and Molecular Docking TechniquesDocument19 pagesSeye 3optimization of The Anticonvulsant Activity of 2-Acetamido-N-Benzyl-2 - (5 - Methylfuran-2-Yl) Acetamide Using QSAR Modeling and Molecular Docking TechniquesdavidNo ratings yet
- NorepinephrineDocument15 pagesNorepinephrineNTA UGC-NETNo ratings yet
- Energearadionics RatesDocument163 pagesEnergearadionics RatesRoberta & Thomas NormanNo ratings yet
- Code of Pharmaceutical Ethics: Shiva Kant Thakur M.Pharma (Pharmaceutics) 1 YearDocument7 pagesCode of Pharmaceutical Ethics: Shiva Kant Thakur M.Pharma (Pharmaceutics) 1 YearTulasee ReddiNo ratings yet
- Concept of Satvapatana A ReviewDocument2 pagesConcept of Satvapatana A ReviewBala Kiran GaddamNo ratings yet
- (2020) - Bipolar Disorders SeminarDocument16 pages(2020) - Bipolar Disorders SeminarAarón ParedesNo ratings yet
- Formularium Obat IGD 2019Document29 pagesFormularium Obat IGD 2019RaNo ratings yet
- Evaluation of Ophthalmic FormulationDocument15 pagesEvaluation of Ophthalmic FormulationDeepak100% (1)
- Emergency Trolley (Abc) ChecklistDocument64 pagesEmergency Trolley (Abc) ChecklistN.K. Ayu SuksmawatiNo ratings yet
- Drug Chart For PrintDocument1 pageDrug Chart For Printnikitapawar04052000No ratings yet
- Singultus 2Document8 pagesSingultus 2Tika AeNo ratings yet
- Leftover Drug Disposal - Customer Behavior, Pharmacist Recommendations, and Obstacles To Drug Take-Back Box ImplementationDocument10 pagesLeftover Drug Disposal - Customer Behavior, Pharmacist Recommendations, and Obstacles To Drug Take-Back Box ImplementationDenise Yanci DemiarNo ratings yet
- (Drugs and The Pharmaceutical Sciences) Myra L. Weiner and Lois A. Kotkoskie - Excipient Toxicity and Safety-CRC Press (1999) PDFDocument374 pages(Drugs and The Pharmaceutical Sciences) Myra L. Weiner and Lois A. Kotkoskie - Excipient Toxicity and Safety-CRC Press (1999) PDFNguyen TriNo ratings yet
- Pregabalin Hospital PharmacyDocument16 pagesPregabalin Hospital Pharmacyaditya100% (1)
- Assignment 1 Prescription Analysis and InterpretationDocument4 pagesAssignment 1 Prescription Analysis and InterpretationShannen CostoNo ratings yet
- Medical and Pharmacy Abbreviations (Sig Codes) : Abbreviation Meaning(s) CategoryDocument3 pagesMedical and Pharmacy Abbreviations (Sig Codes) : Abbreviation Meaning(s) Categoryscope 3901No ratings yet
- Ejhpharm 2021 002903 Inline Supplementary Material 3Document4 pagesEjhpharm 2021 002903 Inline Supplementary Material 3Putu DananjayaNo ratings yet
- NCM 106 Finals For PrintingDocument13 pagesNCM 106 Finals For PrintingJULIANNAH ATHENA MERCADONo ratings yet
- Botanic Drugs 1917 PDFDocument408 pagesBotanic Drugs 1917 PDFUkefácil Ukelele FacilónNo ratings yet
- Disorders of Na BalanceDocument24 pagesDisorders of Na BalanceElvis obajeNo ratings yet
- Psychosis DraftDocument9 pagesPsychosis DraftCHRISTINE JOY. MOLINANo ratings yet
- Ceftriaxone Product MonographDocument52 pagesCeftriaxone Product MonographSarmadNo ratings yet
- Drug TramadolDocument2 pagesDrug TramadolFlauros Ryu Jabien100% (2)
- Attached Table 1 List of Categories, Areas, Disciplines and Research FieldsDocument3 pagesAttached Table 1 List of Categories, Areas, Disciplines and Research FieldsJetro NonanNo ratings yet
- Uronephron Competitors: Product Name Company and Country of Origin Price Weak PointsDocument2 pagesUronephron Competitors: Product Name Company and Country of Origin Price Weak Pointsمصطفى الجبوريNo ratings yet
- Nanoparticulate Drug Delivery System: Mr. Sagar Kishor SavaleDocument101 pagesNanoparticulate Drug Delivery System: Mr. Sagar Kishor SavaleHemin H. MuhammadNo ratings yet
- Anticoagulant TherapyDocument41 pagesAnticoagulant Therapyryan yovanNo ratings yet
- Exogenous Ochronosis: Journal of Dermatological TreatmentDocument7 pagesExogenous Ochronosis: Journal of Dermatological TreatmentStella SunurNo ratings yet