Professional Documents
Culture Documents
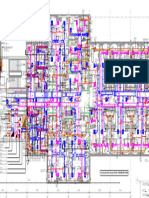
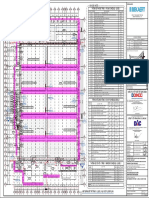
PT Concept Map
PT Concept Map
Uploaded by
api-657741346Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PT Concept Map
PT Concept Map
Uploaded by
api-657741346Copyright:
Available Formats
Labs ND:
Anxiety r/t being discharged too early
AEB pt states "I don't think I'm ready to go home"
(Lippincott Advisor for
Education, n.d.)
Interventions Interventions Interventions
Labs
Administer
Provide care in Provide adequate quiet
prescribed
a calm and reassuring time and decrease
medications and
manner environmental stimuli
monitor their effect
Monitor ABGs
Po2: 59 = low
Pco2: 67 = high
Monitor: Bicarb: 35.5 = high Goal Gaol
pH: 7.33 = low Goal
Glucose, K
BP, PR Monitor:
HR, glucose
Goal:
BP, K
The patient will verbalize
Intervention anxiety, concerns, and
fears by end of shift
Labs Labs Goal was met.
Labs
Labs
Labs
Monitor:
Labs
K, BP, HR
Labs Labs
Other medications:
Monitor:
Labs HR, RR, Alt, Ast
Labs Alprazolam 0.25mg PRN Assessment:
Insulin Albuterol: 3 ml q3h Formoterol 20 mcg bid Education: Pt A&O xs4, rates pain 6 on a scale
Education: Budesonide 0.5 mg bid
Monitor: Glucose: Education: Education: Levalbuterol 1.25 mg bid Seek immediate attention if dizzy, of 10 in left groin area,
Education:
107 Glucose management Teach pt how to use inhaler correctly Do not increase dose Education: light-headed, extreme sleepiness, acetaminophen administered PRN.
Used for acute asthma attacks
A1c: 6.0 = high Injection technique and sites If prescribed more than one
Avoid exposure to chicken pox and
If dose is missed, wait and take next Do not increase prescribed dose slow or difficult breathing, or unresponsive Vital signs: BP-144/89; T- 98; P-95;
Eat w/in 30 min inhale, wait 2 min in b/t puffs sched dose Effects last up to 8 hrs RR- 19; O2- 94% on 6 L of O2.
Labs Do not wash inhaler in water
measles, if exposed notify PCP
Used for acute asthma attacks Do not double dose
Avoid hazardous activites
S/S of hypo/hyperglycemia Opened Respules are good for 2 wks Avoid alcohol PERRLA 3 mm bilaterally, round,
Use bronchodilator before Report of worsening symptoms Report AR of palpations,
Insulin requirements may vary corticosteroids
Edu on good nasal and
Report N/V, shakiness, HA, fast or rapid HR, HA, Smoking will decrease effectiveness reactive, and accommodating to
depending on the severity of illness oral hygiene to reduce light. Mucous membranes pink,
Report if symptoms worsen irregular heartbeat, dizziness, tremor Do not stop abruptly
Do not stop abruptly spread of infection
(Lippincott Advisor for and sleeplessness (Lippincott Advisor for (Lippincott Advisor for moist, and intact. Skin turgor < 3s,
(Lippincott Advisor for
Seek medical attention Education, n.d.) (Lippincott Advisor for Education, n.d.) Education, n.d.) Cap refill < 3s. Skin dry and intact w/
Education, n.d.)
of any AR Education, n.d.) exception of lower legs, skin is dry
Metabolic Panel: (Lippincott Advisor for and flaky. Edema noted 4+. Full
BUN: 51 = high Education, n.d.) ROM. Active bowel sounds Xs 4.
Creatinine: 1.5 = high Urine and bowel continent. S1 and
Albumin: 2.9 S2 clear and present. SOB on
exertion. Clear sounds in left lung,
crackles heard in upper lobe of
-Exposure to tobacco Obtain health hx right lung
smoke Assess pulmonary function
-Passive smoking Use of spirometry
Electrolyte: -increased age Monitor PR and RR
K: 4.6 -in/outdoor air pollution Monitor for edema Acetaminophen 650 mg q4h PRN
Na: 144 RT Medication RT Medication RT Medication -Occupational Monitor O2 levels Education:
RT Medication Monitor:
Cl: 101 exposure Monitor ABGs levels High doses over long period of time
BP, HR
Ca: 8.6 Medications (Hinkle, 7/29/19) Assess triggers will cause liver damage
AST, glucose
Mg: 2.5 -Fam Hx Assess respiratory status No more than 2g/day
Labs K, P, Mg
-Obesity (Hinkle, 7/29/19) Teach s/s of liver damage
Albumin
-Age > 45 Stop taking if rash appears or other
H&H, RBC, WBC
Monitor BP -HTN Risk Factors adverse reaction
Plt
Obtain BMI -High HDL (Lippincott Advisor for
CBC: Foot exam -Poor diet Education, n.d.)
Hct: 41.1 Skin exam (Hinkle, 7/29/19) Assessment
Hgb: 13.1 Neuro exam COPD:
WBC: 7k Oral exam People with COPD commonly become symptomatic during the middle adult years, and the
incidence of the disease increases with age. Although certain aspects of lung function normally
Plt: 141k Monitor blood glucose levels decrease with age—for example, vital capacity and forced expiratory volume in 1 second
and A1c Risk Factors (FEV1)—COPD accentuates and accelerates these physiologic changes as described later. In
Diabetes: COPD, the airflow limitation is both progressive and associated with the lungs’ abnormal
(Hinkle, 7/29/19) The two main problems related to insulin in type 2 diabetes are insulin resistance and
impaired insulin secretion. Insulin resistance refers to a decreased tissue sensitivity to insulin.
inflammatory response to noxious particles or gases. The inflammatory response occurs
throughout the proximal and peripheral airways, lung parenchyma, and pulmonary vasculature
Normally, insulin binds to special receptors on cell surfaces and initiates a series of reactions Because of the chronic inflammation and the body’s attempts to repair it, changes and narrowing
involved in glucose metabolism. In type 2 diabetes, these intracellular reactions are occur in the airways. In the proximal airways (trachea and bronchi greater than 2 mm in
diminished, making insulin less effective at stimulating glucose uptake by the tissues and at diameter), changes include increased numbers of goblet cells and enlarged submucosal glands,
regulating glucose release by the liver. The exact mechanisms that lead to insulin resistance both of which lead to hypersecretion of mucus. In the peripheral airways (bronchioles less than 2
Atorvastatin 40 mg daily and impaired insulin secretion in type 2 diabetes are unknown, although genetic factors are mm diameter), inflammation causes thickening of the airway wall, peribronchial fibrosis, exudate
Monitor lipid panel: Education: thought to play a role. in the airway, and overall airway narrowing (obstructive bronchiolitis) (Hinkle, 7/29/19)
To overcome insulin resistance and to prevent the buildup of glucose in the blood, increased
HDL: 86 = high Edu on dietary management, amounts of insulin must be secreted to maintain the glucose level at a normal or slightly
Pantoprazole 40 mg bid
Cholesterol: 149 weight control, and exercise elevated level. If the beta cells cannot keep up with the increased demand for insulin, the Education:
glucose level rises and type 2 diabetes develops. Insulin resistance may also lead to
Triglycerides: 65 Importance of controlling high metabolic syndrome, which is a constellation of symptoms, including hypertension, Take as the same time every day
Urine changes
LDL: 50 Labs fat levels
hypercholesterolemia, abdominal obesity, and other abnormities (Hinkle, 7/29/19)
Take w/ or w/out meals Monitor:
Renal and blood labs
Avoid alcohol Assessment Swallow pill whole, no crushing Labs LFT, Ca
Urinary output
Notify of any AR - muscle spasms, Antacids do not affect absorption HR, BP
Medication Diabetes
malaise, fever Educate s/s of hypo magnesium
Assess for pain
Can be taken at any
Pulmonary edema:
(Lippincott Advisor for
Pulmonary edema is an acute event that results from left ventricular failure. It can occur following acute MI or as
-Increase aged (Hinkle, 7/29/19)
time-of-day w/ or
an exacerbation of chronic HF. When the left ventricle begins to fail, blood backs up into the pulmonary circulation,
causing pulmonary interstitial edema. This may occur quickly in some patients, a condition sometimes called flash
Education, n.d.)
Hyperlipidemia: pulmonary edema. Pulmonary edema can also develop slowly, especially when it is caused by noncardiac -Comorbid conditions
w/out meals disorders such as kidney injury and other conditions that cause fluid overload. The pathophysiology is an extreme
Elevated cholesterol and triglycerides associated w/ premature form of that seen in left-sided HF. The left ventricle cannot handle the volume overload, and blood volume and -Pre-existing kidney and
(Lippincott Advisor for coronary disease. (Hinkle, 7/29/19) PMH
Monitor BP
pressure build up in the left atrium. The rapid increase in atrial pressure results in an acute increase in pulmonary
PMH vascular diseases,
Education, n.d.) venous pressure, which produces an increase in hydrostatic pressure that forces fluid out of the pulmonary
Complete Health Hx -Elderly male > 45 yrs capillaries and into the interstitial spaces and alveoli (Hinkle, 7/29/19)
and respiratory failure
-Family Hx
Physical exam (Hinkle, 7/29/19)
-Obesity
Possible organ damage -Poor diet PMH PMH
Lab tests: UA, blood -Sedentary lifestyle
Hypertension:
-Sleep apnea
chemistry, 12 lead tele, -Stress Risk Factors Blood pressure is the product of cardiac output multiplied by peripheral resistance. Cardiac
output is the product of the heart rate multiplied by the stroke volume. Each time the heart Risk Factors
renal labs (Hinkle, 7/29/19)
contracts, pressure is transferred from the contraction of the heart muscle to the blood and
then pressure is exerted by the blood as it flows through the blood vessels. Hypertension can
Retinal exam result from increases in cardiac output, increases in peripheral resistance (constriction of the
74 yr old Caucasian male
(Hinkle, 7/29/19)
blood vessels), or both. Increases in cardiac output are often related to an expansion in
vascular volume. Although no precise cause can be identified for most cases of hypertension, Chief Complaint:
AKI:
Although the pathogenesis of AKI and oliguria is not always known, many times there
Assessment
it is understood that hypertension is a multifactorial condition. Because hypertension can be a Pulmonary edema, fluid
sign, it is most likely to have many causes, just as fever has many causes (Hinkle, 7/29/19)
overload, elevated troponin,
PMH is a specific underlying cause. Some of the factors may be reversible if identified and
treated promptly, before kidney function is impaired. This is true of the following
COPD conditions that reduce blood flow to the kidney and impair kidney function: (1)
PMH hypovolemia; (2) hypotension; (3) reduced cardiac output and heart failure; (4)
obstruction of the kidney or lower urinary tract by tumor, blood clot, or kidney stone; Goal Reference
VS: BP-144/89; T- 98; P-95; and (5) bilateral obstruction of the renal arteries or veins. If these conditions are
Assessment RR- 19; O2- 94% treated and corrected before the kidneys are permanently damaged, the increased
BUN and creatinine levels, oliguria, and other signs may be reversed. (Hinkle, 7/29/19)
Congestion: CHF:
Systolic HF results in decreased blood ejected from the ventricle. The decreased blood flow is sensed by baroreceptors in the Allergies:
Dyspnea aortic and carotid bodies. The sympathetic nervous system is then stimulated to release epinephrine and norepinephrine. The
Penicillin, Iodine
Orthopnea purpose of this initial response is to increase heart rate and contractility and support the failing myocardium, but the continued
response has multiple negative effects. Sympathetic stimulation causes vasoconstriction in the skin, gastrointestinal tract, and
Paroxysmal nocturnal dyspnea kidneys. A decrease in renal perfusion due to low CO and vasoconstriction then causes the release of renin by the kidneys. Renin
Cough (recumbent or exertional) converts the plasma protein angiotensinogen to angiotensin I, which then circulates to the lungs. Angiotensin-converting enzyme - Family Hx Assess thyroid hormone levels
(ACE) in the lumen of pulmonary blood vessels converts angiotensin I to angiotensin II, a potent vasoconstrictor, which then
Pulmonary crackles that do not clear with cough PMH -Inadequate TSH
Labs Weight gain (rapid) Medication
increases the blood pressure and afterload. Angiotensin II also stimulates the release of aldosterone from the adrenal cortex,
resulting in sodium and fluid retention by the renal tubules and an increase in blood volume. These mechanisms lead to the fluid Assess medication regimen and serum levels
PMH Hypotyroidism :
(Hinkle, 7/29/19)
Dependent edema
volume overload commonly seen in HF. Angiotensin, aldosterone, and other neurohormones (e.g., endothelin) lead to an increase
in preload and afterload, which increases stress on the ventricular wall, causing an increase in cardiac workload. A counter- Hypothyroidism results from suboptimal levels of thyroid hormone. Thyroid Assess for fatigue
Abdominal bloating or discomfort regulatory mechanism is attempted through the release of natriuretic peptides. Atrial natriuretic peptide (ANP) and B-type
natriuretic peptide (BNP; brain type) are released from the overdistended cardiac chambers. These substances promote
deficiency can affect all body functions and can range from mild, subclinical Reports of hair loss, brittle nails, dry skin,
Ascites
Risk Factors
vasodilation and diuresis. However, their effect is usually not strong enough to overcome the negative effects of the other forms to myxedema (severe deficiency discussed later), an advanced life- numbness and tingling of fingers
Jugular venous distention mechanisms.
threatening form The most common cause of hypothyroidism in adults is
Sleep disturbance (anxiety or air hunger)
As the heart’s workload increases, contractility of the myocardial muscle fibers decreases. Decreased contractility results in an
Risk Factors Assess body temp and pulse rate
increase in end-diastolic blood volume in the ventricle, stretching the myocardial muscle fibers and increasing the size of the autoimmune thyroiditis (Hashimoto disease), in which the immune system
Fatigue -Control of hypertension, ventricle (ventricular dilation). As cardiac cells die and the heart muscle becomes fibrotic, diastolic HF can develop, leading to
attacks the thyroid gland. Symptoms of hyperthyroidism may later be Assess weight changes
further dysfunction. A stiff ventricle resists filling, and less blood in the ventricles causes a further decrease in CO. All of these
Poor Perfusion/Low Cardiac Output: lipids, diabetes, obesity compensatory mechanisms of HF have been referred to as the “vicious cycle of HF” because low CO leads to multiple followed by those of hypothyroidism and myxedema. (Hinkle, 7/29/19) (Hinkle, 7/29/19)
Decreased exercise tolerance (Hinkle, 7/29/19) mechanisms that make the heart work harder, worsening the HF. (Hinkle, 7/29/19)
Muscle wasting or weakness
Anorexia or nausea
Medication
Unexplained weight loss Medication
Lightheadedness or dizziness Assessment
Unexplained confusion or altered mental status Medication
Resting tachycardia
Daytime oliguria with recumbent nocturia
Cool or vasoconstricted extremities
Pallor or cyanosis Medication
(Hinkle, 7/29/19) Medication
Labs
Assessment
Furosemide 40 mg bid Levothyroxine: 75 mcg daily
Education: Education:
Monitor:
Take early in the morning, causes frequent Importance of compliance
HR, BP
urination Therapy is lifelong
BUN, Creatinine Notify AR of OD
If dose is missed, take in early afternoon
Glucose Take w/ plenty of water
Limit alcohol and strenuous exercises in heat to
Plt, WBC, K Do not change brands
prevent worsening symptoms Report bruising or bleeding
Metoprolol 25 mg bid Report AR, such as ringing in ears, severe Notify surgeons of therapy
Labs Aspirin: 81 mg daily Rivaroxciban 20 mg bid
Education:
Education: abdominal pain, sore throat, and fever, this Protect med from light
Education: Monitor pulse rate indicates toxicity and moisture
Eat low sodium diet
Take as directed Do not take if pulse is < 60 bpm Avoid direct sunlight (Lippincott Advisor for
Take w/ food, milk, and large glass of water
Watch for bleeding or bruising Take as prescribed w/ meals Education, n.d.)
No alcohol 2 hrs before and 1 hr after (Lippincott Advisor for
Reports any AR, such as SOB
Discard if there is a vinegar smell If dose is missed, Education, n.d.)
Do not stop abruptly, withdrawal gradually,
Encourage soft toothbrush take when remembered, usually takes 1-2 weeks
Ibuprofen interferes w/ absorption, resume normal regimen (Lippincott Advisor for
negating its effects
the next day Education, n.d.) Labs
Keep out of reach of children
(Lippincott Advisor for
(Lippincott Advisor for ND:
Education, n.d.) Education, n.d.) Fluid volume excess r/t compromised renal function and cardiac output
AEB edema in lower and upper extremities (Swearingen, 2012)
Labs
Monitor
Labs Labs Interventions Interventions Interventions
BP, HR, TSH
Monitor:
BP, cholesterol, glucose
Monitor: Ca, Mg, K, Na
Administer prescribed Monitor vital signs Monitor daily weight
Plt, AST, ALT, Monitor BUN, creatinine
medication and monitor
Bilirubin and BP and HR H&H, Plt, WBC
it's effect
GGT
Intervention
Goal
Goal
Goal
IN
Goals:
Edema will be 1+ or
less on a 0-4+ scales
Labs Goal Reference within 24 hrs
Goal being revised
for next 24 hrs
(Swearingen, 2012)
ND:
Impaired gas exchange r/t fluid in airway
AEB O2 saturation of 94% on 6L of O2 via nasal cannula
(Swearingen, 2012)
Intervention Intervention Intervention
Administer prescribed Monitor pulse
Auscultate lung sounds
nebulizer and respiratory oximeter q2hr
q2hr
medications
Goal Goal
Goal
Sources:
Goals:
Key Hinkle, J. L., Cheever, K. H. (19). Lippincott CoursePoint Enhanced for Brunner & Suddarth's Textbook of Medical-Surgical Nursing,
14th Edition. [[VitalSource Bookshelf version]]. Retrieved from vbk://9781975123383 Patient's ABG labs will be
closer to normal
Lippincott. (N.D). Lippincott Advisor for Education. Retrieved from Lippincott Adisvor: https://advisor-edu.lww.com/lna/home.do by discharge
Patient Pathophysiology of Past Risk Factors Assessment Medications Labs Goal is continued to
Information Medical History Nursing Diagnosis Interventions Goals
Swearingen. (2012). All-in-One Care Planning Resource. In Swearingen. St. Louis, Missouri: Elsevier. be monitor
(Swearingen, 2012)
You might also like
- Introduction To Drugs and The Neuroscience of Behavior 1st Edition Adam Prus Test Bank DownloadDocument12 pagesIntroduction To Drugs and The Neuroscience of Behavior 1st Edition Adam Prus Test Bank DownloadBonnie Garza100% (23)
- Pharmacology Mnemonics MNEMOMICSDocument14 pagesPharmacology Mnemonics MNEMOMICSE.R.O100% (1)
- APC Intern Written Examination Practice Paper v1.2013Document67 pagesAPC Intern Written Examination Practice Paper v1.2013Dha21100% (1)
- Zoning MapDocument1 pageZoning MapJoban BrarNo ratings yet
- Sarms 1 - The Ultimate Guide To SarmsDocument4 pagesSarms 1 - The Ultimate Guide To SarmsHumbert Gym ColombinaNo ratings yet
- PCOL3011Document5 pagesPCOL3011Jack AultNo ratings yet
- Dialogue Between Pharmacist and PatientDocument2 pagesDialogue Between Pharmacist and PatientAbid Ali Khan82% (11)
- Plano Upeu GeneralDocument1 pagePlano Upeu GeneralAllisson Arone ValenciaNo ratings yet
- CR Ingenieros: Limite de ProyectoDocument4 pagesCR Ingenieros: Limite de ProyectoJorge GutierrezNo ratings yet
- Basement LayoutDocument1 pageBasement LayoutKetaki RanalkarNo ratings yet
- Tavevo Lab CabinetsDocument5 pagesTavevo Lab CabinetsRic ReeNo ratings yet
- R2b-P3-206-02-E-Pl-00004 - 1 U-21000 FCC Overall PlanDocument1 pageR2b-P3-206-02-E-Pl-00004 - 1 U-21000 FCC Overall Plan4rc2nq4vwtNo ratings yet
- Áreas y DistanciasDocument9 pagesÁreas y DistanciasKarlixPanNo ratings yet
- PAMPANGA DELTA BRIDGE - TOPO PLAN AND PROFILE B A1Document1 pagePAMPANGA DELTA BRIDGE - TOPO PLAN AND PROFILE B A1Chris Ian MacamNo ratings yet
- PAMPANGA DELTA BRIDGE - TOPO PLAN AND PROFILE B A2Document1 pagePAMPANGA DELTA BRIDGE - TOPO PLAN AND PROFILE B A2Chris Ian MacamNo ratings yet
- 1-PLANTA Y PERFIL-Layout1-Planta Perfil - A1Document1 page1-PLANTA Y PERFIL-Layout1-Planta Perfil - A1Alfredo Villanueva ParedesNo ratings yet
- Project #9Document11 pagesProject #9indyecraftsNo ratings yet
- Registration Policy UrduDocument5 pagesRegistration Policy UrduHuzaifa KhanNo ratings yet
- Reference LevelDocument1 pageReference Level123epcNo ratings yet
- River View South-FinalDocument1 pageRiver View South-FinalAryan MalikNo ratings yet
- Parque Sol. 05-10-21Document8 pagesParque Sol. 05-10-21Kilian ZamboraNo ratings yet
- Project #6Document11 pagesProject #6indyecraftsNo ratings yet
- Niveau Sous Sol - 3: Projet: Hôtel Seybouse Maître D'ouvrage: EGT AnnabaDocument1 pageNiveau Sous Sol - 3: Projet: Hôtel Seybouse Maître D'ouvrage: EGT AnnabaMehieddine AslounNo ratings yet
- Political Risk Map 2017Document1 pagePolitical Risk Map 2017Mahesh ParabNo ratings yet
- Project #2Document14 pagesProject #2indyecraftsNo ratings yet
- Project #1Document15 pagesProject #1indyecraftsNo ratings yet
- Final Drawing - With Coordinates-08-01-2021.-ModelDocument1 pageFinal Drawing - With Coordinates-08-01-2021.-ModelVKT TiwariNo ratings yet
- Pumb & Water Tank Construction Area Fence-Drawing - CommentedDocument3 pagesPumb & Water Tank Construction Area Fence-Drawing - CommentedVinodNo ratings yet
- Aldeinha Lotes 250-ModeloDocument1 pageAldeinha Lotes 250-ModelotelminhopaimNo ratings yet
- Tadikonda Proposed Landuse MapDocument1 pageTadikonda Proposed Landuse MapRamesh BabuNo ratings yet
- Bach Chorales PDFDocument5 pagesBach Chorales PDFLaedson SouzaNo ratings yet
- Combined Utility LayoutDocument1 pageCombined Utility LayoutShahul HameedNo ratings yet
- Av. 450 Años-Model5 PDFDocument1 pageAv. 450 Años-Model5 PDFPablo Helio Mieles PoloNo ratings yet
- System Map Eng 01162024Document2 pagesSystem Map Eng 01162024esk.hpts25No ratings yet
- A - Ward: SCALE 1:6000Document1 pageA - Ward: SCALE 1:6000Somesh MhatreNo ratings yet
- Qfab Yard Layout - Rev A3 - 31may22 - Nfs JKT-NFXP Topside and Subsea StrucDocument45 pagesQfab Yard Layout - Rev A3 - 31may22 - Nfs JKT-NFXP Topside and Subsea StrucSajin Chacko NinanNo ratings yet
- Zoneamento - Amparo (Nov16)Document1 pageZoneamento - Amparo (Nov16)Bruno RochaNo ratings yet
- 10132022-RNG-DTDS-MEC-PLT-001 - 00 - RO - Cable Layout-Layout1Document1 page10132022-RNG-DTDS-MEC-PLT-001 - 00 - RO - Cable Layout-Layout1anaismariaNo ratings yet
- 13TH-18TH Floor As Per New One-2109-Pd-214 1Document1 page13TH-18TH Floor As Per New One-2109-Pd-214 1mohammad JameeluddinNo ratings yet
- Hospital Diogo Layout1Document1 pageHospital Diogo Layout1Leonardo Assis CastilhoNo ratings yet
- Screenshot 2023-11-17 at 7.06.12 PMDocument1 pageScreenshot 2023-11-17 at 7.06.12 PMSamarth ChaturvediNo ratings yet
- Ubicacion y Localización-U-01Document1 pageUbicacion y Localización-U-01rubenNo ratings yet
- General Layout-General Layout and Roads (Area 019) Rev DDocument1 pageGeneral Layout-General Layout and Roads (Area 019) Rev DDean WilyNo ratings yet
- Fuel Tanl ConcDocument1 pageFuel Tanl ConcAyman ZakariaNo ratings yet
- Kertas Kerja NO Nama Akun Neraca AJP NSSD L/R Neraca D K D K D K D K D KDocument3 pagesKertas Kerja NO Nama Akun Neraca AJP NSSD L/R Neraca D K D K D K D K D Kmilad nur fadillahNo ratings yet
- 1.2 Asbuilt Unilineal - Troncal 14 - Nodo VMT-185Document1 page1.2 Asbuilt Unilineal - Troncal 14 - Nodo VMT-185proyectogyga2023No ratings yet
- Goa Castle Rock Kulem Investigation Locations - R1Document1 pageGoa Castle Rock Kulem Investigation Locations - R1Ghulam Quadir KhanNo ratings yet
- DIgSILENT RUM11 PDFDocument1 pageDIgSILENT RUM11 PDFFERDINADNo ratings yet
- Or4100 1 Atnm MM2 SDW 6540601 40Document1 pageOr4100 1 Atnm MM2 SDW 6540601 40Jemuel PinongcosNo ratings yet
- Camino de Vidax - Alto Sax 1Document1 pageCamino de Vidax - Alto Sax 1Fredy Quispe MamaniNo ratings yet
- Eric Marienthal - IshedDocument2 pagesEric Marienthal - IshedRafael Pereira LimaNo ratings yet
- Wycombe-Map-Large Acontinue 7206-4932 eDocument1 pageWycombe-Map-Large Acontinue 7206-4932 eredred121No ratings yet
- L01 MBLC D04 TLM DWG 40la100 Ag Lay100 R01Document1 pageL01 MBLC D04 TLM DWG 40la100 Ag Lay100 R01Nazir HussainNo ratings yet
- As-Built Drawing - Sports CityDocument2 pagesAs-Built Drawing - Sports Cityzubair khanNo ratings yet
- Plans de CoffrageDocument5 pagesPlans de CoffrageHamissa BerisNo ratings yet
- O Espírito de DeusDocument1 pageO Espírito de DeusVagner AraujoNo ratings yet
- Mapa DistritalDocument1 pageMapa Distritalyumpim11100% (1)
- Min-Acm-Prt-Xx-Ax-Dd-90000 (01) Signage Plan & DetailsDocument1 pageMin-Acm-Prt-Xx-Ax-Dd-90000 (01) Signage Plan & Detailsabdullah sahibNo ratings yet
- Ministerio De: Vicente RocafuerteDocument1 pageMinisterio De: Vicente RocafuerteAlex PalaciosNo ratings yet
- DC-BVN-CSA-VO.14 - Drawing PDFDocument7 pagesDC-BVN-CSA-VO.14 - Drawing PDFRevit EdificeNo ratings yet
- Chaplains USMC Team HandbookDocument184 pagesChaplains USMC Team HandbookDocStevens100% (2)
- Đề CK-222-1Document4 pagesĐề CK-222-1namnam21aNo ratings yet
- Pnateamiento General Desague PluvialDocument1 pagePnateamiento General Desague PluvialJJesusNo ratings yet
- Community PaperDocument6 pagesCommunity Paperapi-657741346No ratings yet
- Cover LetterDocument1 pageCover Letterapi-657741346No ratings yet
- Scholarship Agreement 1Document2 pagesScholarship Agreement 1api-657741346No ratings yet
- Concept Map l4 1 2023-03-04 20-19-23Document1 pageConcept Map l4 1 2023-03-04 20-19-23api-657741346No ratings yet
- Concept Map PT 2 UpdatedDocument1 pageConcept Map PT 2 Updatedapi-657741346No ratings yet
- Elizabeth Pope: ExperienceDocument1 pageElizabeth Pope: Experienceapi-657741346No ratings yet
- Healthier U EndowmentDocument2 pagesHealthier U Endowmentapi-657741346No ratings yet
- SSR tsrpt2023Document3 pagesSSR tsrpt2023api-657741346No ratings yet
- BB Cancer A To KDocument49 pagesBB Cancer A To KWaris TriyonoNo ratings yet
- Pharmacology Endocrine DrugsDocument15 pagesPharmacology Endocrine DrugsM Youssif Elkady100% (1)
- Drug InspectorDocument6 pagesDrug InspectorDinkar Pandey100% (1)
- MedicamentosDocument1 pageMedicamentosVictor Manuel Palha SemedoNo ratings yet
- Pharmacology of Metabolic Drugs: Nurlaili SusantiDocument58 pagesPharmacology of Metabolic Drugs: Nurlaili Susantimillennia zulfaNo ratings yet
- Syllabus For Pharmacy (PGQP24) : Pharmaceutics-I (Introduction To Pharmaceutics)Document9 pagesSyllabus For Pharmacy (PGQP24) : Pharmaceutics-I (Introduction To Pharmaceutics)Huba ZehraNo ratings yet
- Immunization ChartDocument1 pageImmunization ChartDesilva ThampiNo ratings yet
- Usp DizolvareDocument168 pagesUsp Dizolvaremelania.irimiaNo ratings yet
- The 10 Most Addictive Pain MedicationsDocument17 pagesThe 10 Most Addictive Pain MedicationslabendetNo ratings yet
- Stock PPG Tangerang Mahakam, Kalbe & Hexpharm 07 Nov 23Document22 pagesStock PPG Tangerang Mahakam, Kalbe & Hexpharm 07 Nov 23rian agustianNo ratings yet
- Adrif Vision List New 11.02.2021Document2 pagesAdrif Vision List New 11.02.2021rahsreeNo ratings yet
- IV To PO Review WorksheetDocument1 pageIV To PO Review WorksheetALberta YosheNo ratings yet
- Satyanand Sahu (Narcotic and Non - Narcotic Analgesic)Document44 pagesSatyanand Sahu (Narcotic and Non - Narcotic Analgesic)Satyanand SahuNo ratings yet
- Ati Medication ListDocument38 pagesAti Medication ListSheldon SloanNo ratings yet
- Twynsta Telmisartan Amlodipine TabletsDocument2 pagesTwynsta Telmisartan Amlodipine TabletsMohamed Omer100% (2)
- Protogyl PDFDocument5 pagesProtogyl PDFpushkar078No ratings yet
- 1.1 Intro To BiopharmDocument32 pages1.1 Intro To BiopharmNeha Dand100% (1)
- JR 1 - 3.8 Tokisitas KloramfenikolDocument7 pagesJR 1 - 3.8 Tokisitas KloramfenikolNursyifa Dewi AfifahNo ratings yet
- Case Report Hydromorphone Precipitating Serotonin SyndromeDocument4 pagesCase Report Hydromorphone Precipitating Serotonin SyndromeMax PowellsNo ratings yet
- Essential Drug List 2020Document61 pagesEssential Drug List 2020felixrobertedwardNo ratings yet
- Gastrointestinal DrugsDocument2 pagesGastrointestinal DrugsKrishna Faith P. DelaraNo ratings yet
- Introduction To CDSCODocument11 pagesIntroduction To CDSCOaadrika negiNo ratings yet
- Denumiri MedicamenteDocument4 pagesDenumiri MedicamenteFlorin PostolacheNo ratings yet
- Inhibition of Cell Wall SynthesisDocument6 pagesInhibition of Cell Wall SynthesisDuaa ShamiehNo ratings yet