Professional Documents
Culture Documents
Standard Treatment: Guidelines 2022
Standard Treatment: Guidelines 2022
Uploaded by
LijoeliyasCopyright:
Available Formats
You might also like
- Running Head: Case Study 1Document6 pagesRunning Head: Case Study 1Benjamin Adet OnyangoNo ratings yet
- Allergic Rhinitis (NCP)Document3 pagesAllergic Rhinitis (NCP)24 PAULINO ALDRIN MUJAR50% (2)
- Color Atlas of Clinical Hematology Hoffbrand PDFDocument2 pagesColor Atlas of Clinical Hematology Hoffbrand PDFSonja50% (2)
- Legal, Ethical, and Political IssuesDocument481 pagesLegal, Ethical, and Political IssuesVanessa Flores86% (7)
- CH 150 Management of Cough in Office PracticeDocument8 pagesCH 150 Management of Cough in Office Practiceroshen02No ratings yet
- CH 146 Management of Fever Without Focus in Office PracticeDocument9 pagesCH 146 Management of Fever Without Focus in Office Practiceroshen02No ratings yet
- App To CHR CoughDocument6 pagesApp To CHR Coughbrajendra singhNo ratings yet
- CH 027 STG BronchiolitisDocument9 pagesCH 027 STG BronchiolitisAkshita JainNo ratings yet
- CH 035 STG Bronchial AsthmaDocument11 pagesCH 035 STG Bronchial AsthmaNosirova ManijaNo ratings yet
- Allergic Rhinitis FinalDocument9 pagesAllergic Rhinitis FinalDrAyushi Aggarwal AshiNo ratings yet
- Pediatric AsthmaDocument79 pagesPediatric AsthmanitshieldNo ratings yet
- TLP RadDocument1 pageTLP RadIqra AsimNo ratings yet
- JPG 1020Document1 pageJPG 1020Ishak FikNo ratings yet
- Common ColdDocument1 pageCommon ColdLalisaM ActivityNo ratings yet
- Cardio&ThoraxDocument92 pagesCardio&Thoraxm.dejesusNo ratings yet
- Session 4-Management of Paediatric COVID19Document24 pagesSession 4-Management of Paediatric COVID19Uncertain NeuronNo ratings yet
- DM 2008Document40 pagesDM 2008Arpita SahaNo ratings yet
- Protracted Bacterial Bronchitis (PBB) in Children: Patient EducationDocument2 pagesProtracted Bacterial Bronchitis (PBB) in Children: Patient EducationAngelaNo ratings yet
- Chapter 14 AsthmaDocument28 pagesChapter 14 AsthmaNat WehrNo ratings yet
- A. Enrichment Activity 1 (Lesson 2: RHU)Document6 pagesA. Enrichment Activity 1 (Lesson 2: RHU)Yam Esor OsomrofNo ratings yet
- Lesson Plan ON BroncitisDocument24 pagesLesson Plan ON Broncitisvani reddyNo ratings yet
- Update: On Allergic RhinitisDocument8 pagesUpdate: On Allergic RhinitisJayantiNo ratings yet
- Ob2 Sas 26Document9 pagesOb2 Sas 26????No ratings yet
- Teaching On Ent DisordersDocument26 pagesTeaching On Ent DisordersMary Menu100% (1)
- Allergic Rhinitis EnglishDocument20 pagesAllergic Rhinitis EnglishAnonymous 1Jbk4GxNo ratings yet
- Acute EpiglottitisDocument12 pagesAcute EpiglottitisDr. Sarthak MishraNo ratings yet
- Bronchiolitis 1 1Document27 pagesBronchiolitis 1 1Raazia AliNo ratings yet
- Management of Children With Community-Acquired PneDocument9 pagesManagement of Children With Community-Acquired PneAthea 88No ratings yet
- Drug Treatments of Childhood Coughs: ManagementDocument5 pagesDrug Treatments of Childhood Coughs: ManagementCristoper PanjaitanNo ratings yet
- Pediatric Resource NursingDocument30 pagesPediatric Resource NursingAddis KusseNo ratings yet
- Hiv and Aids in Children 2,2Document27 pagesHiv and Aids in Children 2,2Kazau FwalangaNo ratings yet
- Bronchiolitis F1533 A5 Col FINAL Mar16Document12 pagesBronchiolitis F1533 A5 Col FINAL Mar16Hassan MohdNo ratings yet
- PlanningDocument13 pagesPlanningErmiyas BeletewNo ratings yet
- Concept Map and OutcomesDocument7 pagesConcept Map and Outcomesapi-663879558No ratings yet
- Communicable Disease ActivityDocument1 pageCommunicable Disease ActivityMadelyn GatdulaNo ratings yet
- Cough, Cold and AllergyDocument32 pagesCough, Cold and AllergyLany GadeNo ratings yet
- CH 084 Oral ThrushDocument7 pagesCH 084 Oral ThrushSavir GuptaNo ratings yet
- Protracted Bacterial BronchitisDocument7 pagesProtracted Bacterial BronchitisDr. Sarthak MishraNo ratings yet
- I-CARE-For-Kids-Summary-2023-02-22Document2 pagesI-CARE-For-Kids-Summary-2023-02-22BugMagnetNo ratings yet
- Topic: Bronchitis: PathophysiologyDocument3 pagesTopic: Bronchitis: PathophysiologyEdson John DemayoNo ratings yet
- Dr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFDocument72 pagesDr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFagnesspratiwiNo ratings yet
- Upper Respiratory InfectionDocument7 pagesUpper Respiratory Infectionhazem barhoomNo ratings yet
- Mumps Lesson PlanDocument6 pagesMumps Lesson PlanRajalakshmi67% (3)
- NeonatologyDocument47 pagesNeonatologySoumya K SNo ratings yet
- Take Home Pack Gr.8 Life Orientation T3Document5 pagesTake Home Pack Gr.8 Life Orientation T3Bongisipho Kwarameva NgcoboNo ratings yet
- Pneumonia Article 3Document3 pagesPneumonia Article 3NeniNo ratings yet
- Activity 2.3Document2 pagesActivity 2.3Ganaden yulyNo ratings yet
- Viral Induced Wheeze Consumer Health Information - Paediatric Unit FMCDocument2 pagesViral Induced Wheeze Consumer Health Information - Paediatric Unit FMCAshik MahamudNo ratings yet
- Adenoid Nasal Polyp Homeopathic TreatmentDocument6 pagesAdenoid Nasal Polyp Homeopathic TreatmentsubratNo ratings yet
- Communicable DiseasesDocument4 pagesCommunicable DiseasesMaria Camille CardosaNo ratings yet
- LOTIVIO - CHN 1 RLE Activity 3Document5 pagesLOTIVIO - CHN 1 RLE Activity 3LOTIVIO VIKTORIANo ratings yet
- Covid-19 Management: FAQs by HCWsDocument31 pagesCovid-19 Management: FAQs by HCWsKabirNo ratings yet
- Mouth Breathing Habit: A ReviewDocument7 pagesMouth Breathing Habit: A ReviewMohamed FaizalNo ratings yet
- SC - Nasal CongestionDocument2 pagesSC - Nasal Congestionyushalluuna bektiNo ratings yet
- Covid Home CareDocument23 pagesCovid Home Careangel_sagun_1No ratings yet
- Assessing and Managing Wheezing in Preschool ChildrenDocument8 pagesAssessing and Managing Wheezing in Preschool ChildrenEndy Widya PutrantoNo ratings yet
- q3 HealthDocument54 pagesq3 HealthGenelyn Lucena Hurtada LabindaoNo ratings yet
- Deworming and ImmunizationDocument23 pagesDeworming and ImmunizationKathy Claire BallegaNo ratings yet
- Episode 059 Feb15 BronchiolitisDocument7 pagesEpisode 059 Feb15 BronchiolitisscandNo ratings yet
- NICUDocument14 pagesNICUDanica Yen PagalNo ratings yet
- Seminar On MumpsDocument40 pagesSeminar On Mumpssushmitabiswas052No ratings yet
- Very Update Information About MedicineDocument13 pagesVery Update Information About MedicinetriNo ratings yet
- Long Covid - The Long Covid Book for Clinicians and Sufferers - Away from Despair and Towards UnderstandingFrom EverandLong Covid - The Long Covid Book for Clinicians and Sufferers - Away from Despair and Towards UnderstandingNo ratings yet
- CDC's "Learn The Signs. Act Early." ProgramDocument2 pagesCDC's "Learn The Signs. Act Early." ProgramLijoeliyasNo ratings yet
- Nrich: Under The Auspices of The Iap Action Plan 2023Document7 pagesNrich: Under The Auspices of The Iap Action Plan 2023LijoeliyasNo ratings yet
- Nadler 2015Document13 pagesNadler 2015LijoeliyasNo ratings yet
- Trans-Anal Suture Rectopexy For Haemorrhoids: Madhura M. KilledarDocument2 pagesTrans-Anal Suture Rectopexy For Haemorrhoids: Madhura M. KilledarLijoeliyasNo ratings yet
- Surgical Treatment of Chronic Pancreatitis With Frey Procedure: Current SituationDocument8 pagesSurgical Treatment of Chronic Pancreatitis With Frey Procedure: Current SituationLijoeliyasNo ratings yet
- Information To Upload CME 2018Document2 pagesInformation To Upload CME 2018LijoeliyasNo ratings yet
- Jategaonkar's Modification of Brooke's End-Ileostomy: KeywordsDocument1 pageJategaonkar's Modification of Brooke's End-Ileostomy: KeywordsLijoeliyasNo ratings yet
- കാന്സര്Document60 pagesകാന്സര്LijoeliyasNo ratings yet
- Proforma For Registration of Subject For DissertationDocument12 pagesProforma For Registration of Subject For DissertationLijoeliyasNo ratings yet
- Application ForEquivalency-Recognition CertificateDocument1 pageApplication ForEquivalency-Recognition CertificateLijoeliyasNo ratings yet
- Gme RegulationsDocument99 pagesGme RegulationsLijoeliyasNo ratings yet
- Antibiotic Awareness - Class ScheduleDocument2 pagesAntibiotic Awareness - Class ScheduleLijoeliyasNo ratings yet
- 2017 H1N1 ABC Guidelines For Treatment ManagementDocument4 pages2017 H1N1 ABC Guidelines For Treatment ManagementLijoeliyasNo ratings yet
- gtg60 Cervicalcerclage PDFDocument21 pagesgtg60 Cervicalcerclage PDFLijoeliyas100% (1)
- What Makes Evidence-Based Journal Clubs SucceedDocument3 pagesWhat Makes Evidence-Based Journal Clubs SucceedkemachNo ratings yet
- UNEP Directory July 2019 - 0Document22 pagesUNEP Directory July 2019 - 0Rameez FaroukNo ratings yet
- ADVANCE CDM User Manual and Data Dictionary v3.1 20180521Document170 pagesADVANCE CDM User Manual and Data Dictionary v3.1 20180521xefin78020No ratings yet
- Complementary TherapiesDocument8 pagesComplementary Therapiestj_sweetgirl100% (2)
- Job Description of Nursing OfficerDocument12 pagesJob Description of Nursing OfficerPunam DuwalNo ratings yet
- The OHNEP Interprofessional Oral Health Faculty ToolkitDocument45 pagesThe OHNEP Interprofessional Oral Health Faculty ToolkitMiranda PCNo ratings yet
- 20221106162019college Wise P2Document77 pages20221106162019college Wise P2Harikiran AlwalaNo ratings yet
- Ap PG Display List-2023Document125 pagesAp PG Display List-2023Devi VaraNo ratings yet
- Cleaning Reusable Medical DevicesDocument12 pagesCleaning Reusable Medical DevicesDavid Olamendi ColinNo ratings yet
- TranscriptDocument2 pagesTranscriptapi-308896353No ratings yet
- Cardiology and Cardiothoracic Surgery: DR A CharalampopoulosDocument1 pageCardiology and Cardiothoracic Surgery: DR A Charalampopoulosdeborah priestleyNo ratings yet
- Hiv-Aids Case StudyDocument31 pagesHiv-Aids Case StudyColeen Mae Camarista100% (2)
- Ahhm 19Document100 pagesAhhm 19Joseph Alejandro TrinidadNo ratings yet
- CDMP Examination Preparation GuideDocument28 pagesCDMP Examination Preparation GuideSiti IsmailNo ratings yet
- 5 6275917323719147718 PDFDocument771 pages5 6275917323719147718 PDFKousik AmancharlaNo ratings yet
- Ignou AssignmentsDocument45 pagesIgnou AssignmentshkannurNo ratings yet
- Fast Dissolving Tablets ThesisDocument7 pagesFast Dissolving Tablets Thesisfbyhhh5r100% (2)
- Scenar For Pain Relief DR Prinz-1Document4 pagesScenar For Pain Relief DR Prinz-1rooibergNo ratings yet
- To C Manual of Icu ProceduresDocument9 pagesTo C Manual of Icu ProceduresVitor SandresNo ratings yet
- PresentationDocument8 pagesPresentationShubhamNo ratings yet
- OT VIC 2012 ProgramDocument4 pagesOT VIC 2012 ProgramGray Design GroupNo ratings yet
- SAMU Summary Differentiated ART DeliveryDocument30 pagesSAMU Summary Differentiated ART DeliveryChris TianNo ratings yet
- PQRI - Biosimilar USADocument27 pagesPQRI - Biosimilar USANgoc Sang HuynhNo ratings yet
- Traditional Medicinal Plants in Ethiopia: International Journal of Biology, Physics & MatematicsDocument8 pagesTraditional Medicinal Plants in Ethiopia: International Journal of Biology, Physics & MatematicsadNo ratings yet
- Equivalent Testing Methodology For Agricultural Water PDFDocument2 pagesEquivalent Testing Methodology For Agricultural Water PDFrazanah aulia marhanNo ratings yet
- Cues Nursing Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Planning Intervention Rationale EvaluationBiancaGabatinoAbarcaNo ratings yet
- Principles in Writing A ParagraphDocument6 pagesPrinciples in Writing A Paragraphjannah playlistsNo ratings yet
Standard Treatment: Guidelines 2022
Standard Treatment: Guidelines 2022
Uploaded by
LijoeliyasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Standard Treatment: Guidelines 2022
Standard Treatment: Guidelines 2022
Uploaded by
LijoeliyasCopyright:
Available Formats
Indian Academy of Pediatrics (IAP)
STANDARD
TREATMENT
GUIDELINES 2022
Under
5 Wheeze
Lead Author
Shishir Modak
Co-Authors
Venkatesh Chandrasekaran, Pankaj C Vaidya
Under the Auspices of the IAP Action Plan 2022
Remesh Kumar R
IAP President 2022
Upendra Kinjawadekar Piyush Gupta
IAP President-Elect 2022 IAP President 2021
Vineet Saxena
IAP HSG 2022–2023
039.indd 1 22-04-2022 11:27:38
© Indian Academy of Pediatrics
IAP Standard Treatment Guidelines Committee
Chairperson
Remesh Kumar R
IAP Coordinator
Vineet Saxena
National Coordinators
SS Kamath, Vinod H Ratageri
Member Secretaries
Krishna Mohan R, Vishnu Mohan PT
Members
Santanu Deb, Surender Singh Bisht, Prashant Kariya,
Narmada Ashok, Pawan Kalyan
039.indd 2 22-04-2022 11:27:38
139
Under 5 Wheeze
What is a Wheeze?
High pitched, musical, whistling sound, monophonic, or polyphonic, that occurs when
intrathoracic medium and small airways are narrowed and vibrate due to increased resistance
to the movement of air.
Wheezing occurs in large proportion of children under 5 years of age. It is commonly
associated with viral respiratory tract infections.
First Time Wheezing
When wheezing occurs for the first time in an infant it is usually due to acute viral bronchiolitis.
The diagnosis is mainly clinical. X-ray chest may show hyperinflation with air trapping or
sometimes it may be normal.
Management of first time wheezer (usually acute bronchiolitis):
;; To maintain oxygen saturation and adequate hydration. Oxygen by nasal cannula or hood
is given whenever saturation falls below 92%.
;; Bronchodilators like salbutamol may be given through nebulizer as a trial initially to
assess response in infants who wheeze for the first time, triggered by viral respiratory tract
infections. However, in acute bronchiolitis per se it is not effective and not indicated.
039.indd 3 22-04-2022 11:27:38
Under 5 Wheeze
In a child with recurrent wheezing, detailed history and examination is of paramount
importance. The following questions need to be asked to ascertain a diagnosis of asthma.
;; Onset of cough/wheezing—insidious/sudden
;; Duration of cough—how many days
;; Timing of cough/wheezing—daytime/nocturnal
;; Type of cough—dry/wet
;; Frequency of cough/wheezing—number of days per month
Details of the Symptoms
;; Perennial or seasonal
;; Symptoms—variable or persistent, whether associated with fever?
;; Interval symptoms—symptoms in between the episodes
;; Activity limitation—school absenteeism and restricted play
;; Triggers—viral infections, smoke, exposure to dust, mold, cat, grass/tree pollen, food,
in response to activity/exercise, laughing, crying, etc.
Recurrent Wheezing
;; History of allergy (atopic dermatitis and allergic rhinitis)—in the child/asthma in
parents
Documenting airflow limitation: The presence of wheeze one or more times in the past,
documented by a physician
Documenting reversibility: Response to beta2-agonist inhalation or documented response
to a trial of inhaled corticosteroid (ICS)
The Global Initiative for Asthma (GINA) guideline proposes grouping of recurrently
wheezing patients based on probability of asthma.
039.indd 4 22-04-2022 11:27:38
Under 5 Wheeze
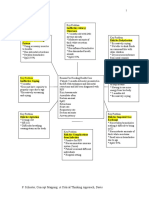
Modified Asthma Predictive Index is an objective tool used to predict the occurrence of asthma
in preschool children.
It is used in children who have 4 or more wheezing episodes in a year. It is said to be positive
when at least one major or two minor criteria are present (Flowchart 1).
Flowchart 1
Modified Asthma Predictive Index
The mAPI has moderate positive predictive value but good negative predictive value (95%) However,
before confirming asthma diagnosis in any child, particularly in this age group it is important to
exclude alternative causes of cough and wheezing.
Clinical features where alternative conditions or asthma mimics are more likely are as following:
;; Onset of wheezing in the neonatal period
;; Wheezing in infants below 6 months of age
;; Nonvariable fixed or persistent signs or symptoms
;; Unilateral signs and localized signs
;; Wet productive cough, presence of high fever
;; Failure to thrive, steatorrhea, and clubbing
;; Multiple system involvement and persistent hypoxia
;; Poor response to bronchodilators
;; Wheezing with dependent edema and/or cardiac murmurs
;; Wheezing accompanied by stridor
039.indd 5 22-04-2022 11:27:38
Under 5 Wheeze
Wheezers below 5 Years of
Differential Diagnosis in
Age—Asthma Mimics
All the conditions mentioned in the figure should be excluded by history, examination,
and, if necessary, by appropriate investigations.
If the history is suggestive of typical viral-induced wheezing or that of asthma no investigations
Investigations in Recurrent Wheezers
are necessary. However, in ambiguous cases with suspicion of some alternative condition certain
investigations may be required.
Hemogram
Complete
Eosinophilia may be detected. However, its absence does not rule out possibility
of asthma. X-ray Chest
To rule out alternative conditions in differential diagnosis.
Allergy
These may be useful to document allergen sensitization in those who report allergic
Tests
symptoms on exposure to a particular allergen.
039.indd 6 22-04-2022 11:27:39
Under 5 Wheeze
Recurrent Wheezers
Nitric Oxide
Fraction of
Investigations in
Fraction of nitric oxide (FeNO) in exhaled air may be used to identify those with
eosinophilic inflammation to predict response to corticosteroids.
Spirometry
Spirometry usually cannot be performed reliably by children under the age of 5 years;
other techniques such as forced oscillation technique (FOT) and impulse oscillometry
(IOS) are now available at a few centers which can be used in doubtful cases.
Treatment of Recurrent Wheezers
Inhalation treatment is the mainstay in the treatment of wheezing. Inhaled short-acting beta-
agonist (SABA), usually salbutamol, is used as initial reliever treatment until symptoms subside.
Inhaler Device
;; Till 4 years: Metered-dose inhaler (MDI) + spacer + mask or nebulizer in hospital
Choice of
setting
;; Above 4 years: MDI + spacer with mouth piece. Mask should be removed as soon as
child can breathe through mouthpiece.
Treatment
In children under 5 years of age with recurrent wheezing, the following treatment
Plan
plan is recommended (Flowchart 2).
039.indd 7 22-04-2022 11:27:39
Under 5 Wheeze
Flowchart 2: Treatment plan for children under 5 years of age with recurrent wheezing.
Treatment of Recurrent Wheezers
*In children with severe episode/life-threatening exacerbation in the past, it is important
to continue inhaled corticosteroid (ICS) for a longer period at a minimum dose that can
prevent further exacerbation with periodic monitoring until the child outgrows the
symptoms. If no risk factors for exacerbation are present, ICS should be stopped and child
followed up for symptom recurrence. ICS can be restarted if symptoms recur.
In some children, if symptoms are not well controlled after 3 months of low dose
budesonide and if diagnosis of asthma is certain then higher step of treatment may
be necessary. But before proceeding to higher dose of ICS, the following should be
Step 3 and Step 4 Treatment
checked:
;; Adherence with inhaled medications
;; Technique of device use
;; Comorbidity
;; Ongoing exposure to allergen
If even after correcting all of the above, symptoms persist, then treatment is
stepped up to step 3. ICS dose is doubled, e.g., 200 µg of budesonide twice a day for
next 3 months.
If child is not well-controlled on this double low dose regime after removing all
modifiable risk factors, treatment can be stepped up to step 4. However, such a child
should be referred to asthma specialist for further management.
039.indd 8 22-04-2022 11:27:39
Under 5 Wheeze
Management of Acute exacerbations
Summary of management of flare-up. (BiPAP: bilevel positive airway
pressure; CPAP: continuous positive airway pressure; HFNC: high-flow nasal
cannula; IV: intravenous; MDI: metered-dose inhaler; NIPPV: noninvasive
positive-pressure ventilation; PICU: pediatric intensive care unit)
;; Bush A, Grigg J, Saglani S. Managing wheeze in preschool children. BMJ. 2014;348:1-7.
;; Castro-Rodriguez JA. The Asthma Predictive Index: a very useful tool for predicting asthma in young
children. J Allergy Clin Immunol. 2010;126:212-6.
Further Reading
;; Ducharme FM, Dell SD, Radhakrishnan D, Grad RM, Watson WT, Yang CL, et al. Diagnosis and
management of asthma in preschoolers: a Canadian Thoracic Society and Canadian Paediatric
Society position paper. Can Respir J. 2015;22:135-43.
;; Fakhoury K. (2022). Evaluation of wheezing in infants and children. [online] Available from https://
www.uptodate.com/contents/evaluation-of-wheezing-in-infants-and-children. [Last accessed April,
2022].
;; GINA. (2021). 2021 GINA Report, Global Strategy for Asthma Management and Prevention. [online]
Available from https://ginasthma.org/gina-reports/. [Last accessed April, 2022].
;; Moral L, Vizmanos G, Torres-Borrego J, Praena-Crespo M, Tortajada-Girbés M, Pellegrini FJ, et al.
Asthma diagnosis in infants and preschool children: a systematic review of clinical guidelines.
Allergol Immunopathol. 2019;47(2):107-21.
10
039.indd 10 22-04-2022 11:27:39
You might also like
- Running Head: Case Study 1Document6 pagesRunning Head: Case Study 1Benjamin Adet OnyangoNo ratings yet
- Allergic Rhinitis (NCP)Document3 pagesAllergic Rhinitis (NCP)24 PAULINO ALDRIN MUJAR50% (2)
- Color Atlas of Clinical Hematology Hoffbrand PDFDocument2 pagesColor Atlas of Clinical Hematology Hoffbrand PDFSonja50% (2)
- Legal, Ethical, and Political IssuesDocument481 pagesLegal, Ethical, and Political IssuesVanessa Flores86% (7)
- CH 150 Management of Cough in Office PracticeDocument8 pagesCH 150 Management of Cough in Office Practiceroshen02No ratings yet
- CH 146 Management of Fever Without Focus in Office PracticeDocument9 pagesCH 146 Management of Fever Without Focus in Office Practiceroshen02No ratings yet
- App To CHR CoughDocument6 pagesApp To CHR Coughbrajendra singhNo ratings yet
- CH 027 STG BronchiolitisDocument9 pagesCH 027 STG BronchiolitisAkshita JainNo ratings yet
- CH 035 STG Bronchial AsthmaDocument11 pagesCH 035 STG Bronchial AsthmaNosirova ManijaNo ratings yet
- Allergic Rhinitis FinalDocument9 pagesAllergic Rhinitis FinalDrAyushi Aggarwal AshiNo ratings yet
- Pediatric AsthmaDocument79 pagesPediatric AsthmanitshieldNo ratings yet
- TLP RadDocument1 pageTLP RadIqra AsimNo ratings yet
- JPG 1020Document1 pageJPG 1020Ishak FikNo ratings yet
- Common ColdDocument1 pageCommon ColdLalisaM ActivityNo ratings yet
- Cardio&ThoraxDocument92 pagesCardio&Thoraxm.dejesusNo ratings yet
- Session 4-Management of Paediatric COVID19Document24 pagesSession 4-Management of Paediatric COVID19Uncertain NeuronNo ratings yet
- DM 2008Document40 pagesDM 2008Arpita SahaNo ratings yet
- Protracted Bacterial Bronchitis (PBB) in Children: Patient EducationDocument2 pagesProtracted Bacterial Bronchitis (PBB) in Children: Patient EducationAngelaNo ratings yet
- Chapter 14 AsthmaDocument28 pagesChapter 14 AsthmaNat WehrNo ratings yet
- A. Enrichment Activity 1 (Lesson 2: RHU)Document6 pagesA. Enrichment Activity 1 (Lesson 2: RHU)Yam Esor OsomrofNo ratings yet
- Lesson Plan ON BroncitisDocument24 pagesLesson Plan ON Broncitisvani reddyNo ratings yet
- Update: On Allergic RhinitisDocument8 pagesUpdate: On Allergic RhinitisJayantiNo ratings yet
- Ob2 Sas 26Document9 pagesOb2 Sas 26????No ratings yet
- Teaching On Ent DisordersDocument26 pagesTeaching On Ent DisordersMary Menu100% (1)
- Allergic Rhinitis EnglishDocument20 pagesAllergic Rhinitis EnglishAnonymous 1Jbk4GxNo ratings yet
- Acute EpiglottitisDocument12 pagesAcute EpiglottitisDr. Sarthak MishraNo ratings yet
- Bronchiolitis 1 1Document27 pagesBronchiolitis 1 1Raazia AliNo ratings yet
- Management of Children With Community-Acquired PneDocument9 pagesManagement of Children With Community-Acquired PneAthea 88No ratings yet
- Drug Treatments of Childhood Coughs: ManagementDocument5 pagesDrug Treatments of Childhood Coughs: ManagementCristoper PanjaitanNo ratings yet
- Pediatric Resource NursingDocument30 pagesPediatric Resource NursingAddis KusseNo ratings yet
- Hiv and Aids in Children 2,2Document27 pagesHiv and Aids in Children 2,2Kazau FwalangaNo ratings yet
- Bronchiolitis F1533 A5 Col FINAL Mar16Document12 pagesBronchiolitis F1533 A5 Col FINAL Mar16Hassan MohdNo ratings yet
- PlanningDocument13 pagesPlanningErmiyas BeletewNo ratings yet
- Concept Map and OutcomesDocument7 pagesConcept Map and Outcomesapi-663879558No ratings yet
- Communicable Disease ActivityDocument1 pageCommunicable Disease ActivityMadelyn GatdulaNo ratings yet
- Cough, Cold and AllergyDocument32 pagesCough, Cold and AllergyLany GadeNo ratings yet
- CH 084 Oral ThrushDocument7 pagesCH 084 Oral ThrushSavir GuptaNo ratings yet
- Protracted Bacterial BronchitisDocument7 pagesProtracted Bacterial BronchitisDr. Sarthak MishraNo ratings yet
- I-CARE-For-Kids-Summary-2023-02-22Document2 pagesI-CARE-For-Kids-Summary-2023-02-22BugMagnetNo ratings yet
- Topic: Bronchitis: PathophysiologyDocument3 pagesTopic: Bronchitis: PathophysiologyEdson John DemayoNo ratings yet
- Dr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFDocument72 pagesDr. Nastiti K - Manajemen Asma Pada Anak 2018 PDFagnesspratiwiNo ratings yet
- Upper Respiratory InfectionDocument7 pagesUpper Respiratory Infectionhazem barhoomNo ratings yet
- Mumps Lesson PlanDocument6 pagesMumps Lesson PlanRajalakshmi67% (3)
- NeonatologyDocument47 pagesNeonatologySoumya K SNo ratings yet
- Take Home Pack Gr.8 Life Orientation T3Document5 pagesTake Home Pack Gr.8 Life Orientation T3Bongisipho Kwarameva NgcoboNo ratings yet
- Pneumonia Article 3Document3 pagesPneumonia Article 3NeniNo ratings yet
- Activity 2.3Document2 pagesActivity 2.3Ganaden yulyNo ratings yet
- Viral Induced Wheeze Consumer Health Information - Paediatric Unit FMCDocument2 pagesViral Induced Wheeze Consumer Health Information - Paediatric Unit FMCAshik MahamudNo ratings yet
- Adenoid Nasal Polyp Homeopathic TreatmentDocument6 pagesAdenoid Nasal Polyp Homeopathic TreatmentsubratNo ratings yet
- Communicable DiseasesDocument4 pagesCommunicable DiseasesMaria Camille CardosaNo ratings yet
- LOTIVIO - CHN 1 RLE Activity 3Document5 pagesLOTIVIO - CHN 1 RLE Activity 3LOTIVIO VIKTORIANo ratings yet
- Covid-19 Management: FAQs by HCWsDocument31 pagesCovid-19 Management: FAQs by HCWsKabirNo ratings yet
- Mouth Breathing Habit: A ReviewDocument7 pagesMouth Breathing Habit: A ReviewMohamed FaizalNo ratings yet
- SC - Nasal CongestionDocument2 pagesSC - Nasal Congestionyushalluuna bektiNo ratings yet
- Covid Home CareDocument23 pagesCovid Home Careangel_sagun_1No ratings yet
- Assessing and Managing Wheezing in Preschool ChildrenDocument8 pagesAssessing and Managing Wheezing in Preschool ChildrenEndy Widya PutrantoNo ratings yet
- q3 HealthDocument54 pagesq3 HealthGenelyn Lucena Hurtada LabindaoNo ratings yet
- Deworming and ImmunizationDocument23 pagesDeworming and ImmunizationKathy Claire BallegaNo ratings yet
- Episode 059 Feb15 BronchiolitisDocument7 pagesEpisode 059 Feb15 BronchiolitisscandNo ratings yet
- NICUDocument14 pagesNICUDanica Yen PagalNo ratings yet
- Seminar On MumpsDocument40 pagesSeminar On Mumpssushmitabiswas052No ratings yet
- Very Update Information About MedicineDocument13 pagesVery Update Information About MedicinetriNo ratings yet
- Long Covid - The Long Covid Book for Clinicians and Sufferers - Away from Despair and Towards UnderstandingFrom EverandLong Covid - The Long Covid Book for Clinicians and Sufferers - Away from Despair and Towards UnderstandingNo ratings yet
- CDC's "Learn The Signs. Act Early." ProgramDocument2 pagesCDC's "Learn The Signs. Act Early." ProgramLijoeliyasNo ratings yet
- Nrich: Under The Auspices of The Iap Action Plan 2023Document7 pagesNrich: Under The Auspices of The Iap Action Plan 2023LijoeliyasNo ratings yet
- Nadler 2015Document13 pagesNadler 2015LijoeliyasNo ratings yet
- Trans-Anal Suture Rectopexy For Haemorrhoids: Madhura M. KilledarDocument2 pagesTrans-Anal Suture Rectopexy For Haemorrhoids: Madhura M. KilledarLijoeliyasNo ratings yet
- Surgical Treatment of Chronic Pancreatitis With Frey Procedure: Current SituationDocument8 pagesSurgical Treatment of Chronic Pancreatitis With Frey Procedure: Current SituationLijoeliyasNo ratings yet
- Information To Upload CME 2018Document2 pagesInformation To Upload CME 2018LijoeliyasNo ratings yet
- Jategaonkar's Modification of Brooke's End-Ileostomy: KeywordsDocument1 pageJategaonkar's Modification of Brooke's End-Ileostomy: KeywordsLijoeliyasNo ratings yet
- കാന്സര്Document60 pagesകാന്സര്LijoeliyasNo ratings yet
- Proforma For Registration of Subject For DissertationDocument12 pagesProforma For Registration of Subject For DissertationLijoeliyasNo ratings yet
- Application ForEquivalency-Recognition CertificateDocument1 pageApplication ForEquivalency-Recognition CertificateLijoeliyasNo ratings yet
- Gme RegulationsDocument99 pagesGme RegulationsLijoeliyasNo ratings yet
- Antibiotic Awareness - Class ScheduleDocument2 pagesAntibiotic Awareness - Class ScheduleLijoeliyasNo ratings yet
- 2017 H1N1 ABC Guidelines For Treatment ManagementDocument4 pages2017 H1N1 ABC Guidelines For Treatment ManagementLijoeliyasNo ratings yet
- gtg60 Cervicalcerclage PDFDocument21 pagesgtg60 Cervicalcerclage PDFLijoeliyas100% (1)
- What Makes Evidence-Based Journal Clubs SucceedDocument3 pagesWhat Makes Evidence-Based Journal Clubs SucceedkemachNo ratings yet
- UNEP Directory July 2019 - 0Document22 pagesUNEP Directory July 2019 - 0Rameez FaroukNo ratings yet
- ADVANCE CDM User Manual and Data Dictionary v3.1 20180521Document170 pagesADVANCE CDM User Manual and Data Dictionary v3.1 20180521xefin78020No ratings yet
- Complementary TherapiesDocument8 pagesComplementary Therapiestj_sweetgirl100% (2)
- Job Description of Nursing OfficerDocument12 pagesJob Description of Nursing OfficerPunam DuwalNo ratings yet
- The OHNEP Interprofessional Oral Health Faculty ToolkitDocument45 pagesThe OHNEP Interprofessional Oral Health Faculty ToolkitMiranda PCNo ratings yet
- 20221106162019college Wise P2Document77 pages20221106162019college Wise P2Harikiran AlwalaNo ratings yet
- Ap PG Display List-2023Document125 pagesAp PG Display List-2023Devi VaraNo ratings yet
- Cleaning Reusable Medical DevicesDocument12 pagesCleaning Reusable Medical DevicesDavid Olamendi ColinNo ratings yet
- TranscriptDocument2 pagesTranscriptapi-308896353No ratings yet
- Cardiology and Cardiothoracic Surgery: DR A CharalampopoulosDocument1 pageCardiology and Cardiothoracic Surgery: DR A Charalampopoulosdeborah priestleyNo ratings yet
- Hiv-Aids Case StudyDocument31 pagesHiv-Aids Case StudyColeen Mae Camarista100% (2)
- Ahhm 19Document100 pagesAhhm 19Joseph Alejandro TrinidadNo ratings yet
- CDMP Examination Preparation GuideDocument28 pagesCDMP Examination Preparation GuideSiti IsmailNo ratings yet
- 5 6275917323719147718 PDFDocument771 pages5 6275917323719147718 PDFKousik AmancharlaNo ratings yet
- Ignou AssignmentsDocument45 pagesIgnou AssignmentshkannurNo ratings yet
- Fast Dissolving Tablets ThesisDocument7 pagesFast Dissolving Tablets Thesisfbyhhh5r100% (2)
- Scenar For Pain Relief DR Prinz-1Document4 pagesScenar For Pain Relief DR Prinz-1rooibergNo ratings yet
- To C Manual of Icu ProceduresDocument9 pagesTo C Manual of Icu ProceduresVitor SandresNo ratings yet
- PresentationDocument8 pagesPresentationShubhamNo ratings yet
- OT VIC 2012 ProgramDocument4 pagesOT VIC 2012 ProgramGray Design GroupNo ratings yet
- SAMU Summary Differentiated ART DeliveryDocument30 pagesSAMU Summary Differentiated ART DeliveryChris TianNo ratings yet
- PQRI - Biosimilar USADocument27 pagesPQRI - Biosimilar USANgoc Sang HuynhNo ratings yet
- Traditional Medicinal Plants in Ethiopia: International Journal of Biology, Physics & MatematicsDocument8 pagesTraditional Medicinal Plants in Ethiopia: International Journal of Biology, Physics & MatematicsadNo ratings yet
- Equivalent Testing Methodology For Agricultural Water PDFDocument2 pagesEquivalent Testing Methodology For Agricultural Water PDFrazanah aulia marhanNo ratings yet
- Cues Nursing Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Planning Intervention Rationale EvaluationBiancaGabatinoAbarcaNo ratings yet
- Principles in Writing A ParagraphDocument6 pagesPrinciples in Writing A Paragraphjannah playlistsNo ratings yet