Professional Documents
Culture Documents
Axelsson 2012
Axelsson 2012
Uploaded by
happyCopyright:
Available Formats
You might also like
- CreativeWriting12 Q1 Module-1Document28 pagesCreativeWriting12 Q1 Module-1Burning Rose89% (140)
- Project Report in JSWDocument44 pagesProject Report in JSWmohd arif khan73% (15)
- O&S April 2009Document134 pagesO&S April 2009Didi Menendez100% (20)
- HHS Public AccessDocument17 pagesHHS Public AccessChika SabaNo ratings yet
- Grothe Et Al., 2013Document13 pagesGrothe Et Al., 2013mackenzie.lacey28No ratings yet
- 2017 Juliaom - PSC PDFDocument10 pages2017 Juliaom - PSC PDFIka Nur AnnisaNo ratings yet
- Dying Means Suffocating, Perceptions of People Living With COPD Facing End of LifeDocument8 pagesDying Means Suffocating, Perceptions of People Living With COPD Facing End of LifetourfrikiNo ratings yet
- Emotional Distress in Patients With Advanced Heart Failure: ReviewDocument11 pagesEmotional Distress in Patients With Advanced Heart Failure: ReviewCândida MineiroNo ratings yet
- Eilertsen BJRK Kirkevold 2010Document11 pagesEilertsen BJRK Kirkevold 2010Anh HuyNo ratings yet
- Determinants of Costs of Care For Patients With Alzheimer's DiseaseDocument11 pagesDeterminants of Costs of Care For Patients With Alzheimer's DiseaseBenny TjanNo ratings yet
- Fpsyg 14 1281878Document10 pagesFpsyg 14 1281878dr.joneidiNo ratings yet
- Lived Through Past Experienced Present Anticipated Future Understanding Existential Loss in The Context of Life Limiting IllnessDocument16 pagesLived Through Past Experienced Present Anticipated Future Understanding Existential Loss in The Context of Life Limiting Illnessfrancheskaam27No ratings yet
- The Effect of Depression On The Quality 0f Life of Patient With Cervical Cancer at Dr. Moewardi Hospital in SurakartaDocument8 pagesThe Effect of Depression On The Quality 0f Life of Patient With Cervical Cancer at Dr. Moewardi Hospital in SurakartaEndahNo ratings yet
- Applied Nursing Research: Mi-Kyoung Cho, PHD, Apn, Gisoo Shin, PHD, RNDocument7 pagesApplied Nursing Research: Mi-Kyoung Cho, PHD, Apn, Gisoo Shin, PHD, RNJoecoNo ratings yet
- The Bodily Presence of Significant Others Intensive Care Patients Experiences in A Situation of Critical IllnessDocument9 pagesThe Bodily Presence of Significant Others Intensive Care Patients Experiences in A Situation of Critical IllnessSara Daniela Benalcazar JaramilloNo ratings yet
- Cardiovascular Risks Associated With Incident and Prevalent Periodontal DiseaseDocument8 pagesCardiovascular Risks Associated With Incident and Prevalent Periodontal DiseaseAlyaefkageNo ratings yet
- 12 Ustundag Orignial 9 3Document8 pages12 Ustundag Orignial 9 3Sanjivi GovekarNo ratings yet
- Barriers To Effective Pain Management in Sickle Cell DiseaseDocument4 pagesBarriers To Effective Pain Management in Sickle Cell DiseaseDr. Smiley JadonandanNo ratings yet
- Pre-Dialysis Patients ' Perceived Autonomy, Self-Esteem and Labor Participation: Associations With Illness Perceptions and Treatment Perceptions. A Cross-Sectional StudyDocument10 pagesPre-Dialysis Patients ' Perceived Autonomy, Self-Esteem and Labor Participation: Associations With Illness Perceptions and Treatment Perceptions. A Cross-Sectional Studyandrada14No ratings yet
- Land Olt 2011Document13 pagesLand Olt 2011Windy TiandiniNo ratings yet
- A Review of EOLDocument33 pagesA Review of EOLinderaaputraaNo ratings yet
- Critical Reviews in Oncology / HematologyDocument18 pagesCritical Reviews in Oncology / HematologyLiterasi MedsosNo ratings yet
- Samson Et Al - Psychosocial Adaptation To Chronic IllnessDocument13 pagesSamson Et Al - Psychosocial Adaptation To Chronic IllnessRaquel PintoNo ratings yet
- Ten Minutes To Midnight: A Narrative Inquiry of People Living With Dying With Advanced Copd and Their Family MembersDocument11 pagesTen Minutes To Midnight: A Narrative Inquiry of People Living With Dying With Advanced Copd and Their Family MembersCeline WongNo ratings yet
- The Effects of Exercise Standards On The Quality of Life To People With Chronic DiseaseDocument18 pagesThe Effects of Exercise Standards On The Quality of Life To People With Chronic DiseaseMario LanzaNo ratings yet
- Mattsson 2011Document12 pagesMattsson 2011oh yuniNo ratings yet
- Concerns of Patients On Dialysis A Research Study PDFDocument15 pagesConcerns of Patients On Dialysis A Research Study PDFProdi S1- 1BNo ratings yet
- Depressive Symptoms and Dietary Adherence in Patients With End-Stage Renal DiseaseDocument10 pagesDepressive Symptoms and Dietary Adherence in Patients With End-Stage Renal Diseasebasti_aka_slimNo ratings yet
- Nurse and Social Worker Palliative Telecare Team and Quality of Life in Patients With COPD, Heart Failure, or Interstitial Lung DiseaseDocument12 pagesNurse and Social Worker Palliative Telecare Team and Quality of Life in Patients With COPD, Heart Failure, or Interstitial Lung DiseasejunhamanoNo ratings yet
- Personality Change Associated With Chronic Diseases: Pooled Analysis of Four Prospective Cohort StudiesDocument13 pagesPersonality Change Associated With Chronic Diseases: Pooled Analysis of Four Prospective Cohort StudiesDebora BergerNo ratings yet
- End of LifeDocument3 pagesEnd of LifeSiti Fatimahtusz07No ratings yet
- Multiple Sclerosis Lancet 2018Document15 pagesMultiple Sclerosis Lancet 2018Sarah Miryam CoffanoNo ratings yet
- Experiences of Psychological FlowerDocument8 pagesExperiences of Psychological Flowerlsj19950128No ratings yet
- Research Article: Turkish Journal of Psychiatry 2021 32 (4) :246-252Document8 pagesResearch Article: Turkish Journal of Psychiatry 2021 32 (4) :246-252Celine WongNo ratings yet
- Background of The Study and SOP - Quali Research2-1Document3 pagesBackground of The Study and SOP - Quali Research2-1Maricris I. AbuanNo ratings yet
- Ho 2013Document6 pagesHo 2013Vera El Sammah SiagianNo ratings yet
- Mia Pruefer - Health Literacy and Elhers-Danlos Syndrome Hypermobility TypeDocument14 pagesMia Pruefer - Health Literacy and Elhers-Danlos Syndrome Hypermobility TypeMia PrueferNo ratings yet
- Living With Advanced Parkinson's Disease: A Constant Struggle With UnpredictabilityDocument10 pagesLiving With Advanced Parkinson's Disease: A Constant Struggle With UnpredictabilityLorenaNo ratings yet
- ContentServer AspDocument8 pagesContentServer Aspstephanie eduarteNo ratings yet
- Birkefeld (2022)Document14 pagesBirkefeld (2022)Nerea AlvarezNo ratings yet
- 480 253 1057 1 10 20190424 PDFDocument8 pages480 253 1057 1 10 20190424 PDFdwiajaNo ratings yet
- Mazujnms v2n2p29 enDocument7 pagesMazujnms v2n2p29 enDoc RuthNo ratings yet
- Pain Neuroscience Education in Older Adults With Chronic Back and or Lower Extremity PainDocument12 pagesPain Neuroscience Education in Older Adults With Chronic Back and or Lower Extremity PainAriadna BarretoNo ratings yet
- Content ServerDocument4 pagesContent ServerEkaSaktiWahyuningtyasNo ratings yet
- End-Of-Life Care in The Icu: Supporting Nurses To Provide High-Quality CareDocument5 pagesEnd-Of-Life Care in The Icu: Supporting Nurses To Provide High-Quality CareSERGIO ANDRES CESPEDES GUERRERONo ratings yet
- Life Review Therapy For Older Adults With Moderate Depressive Symptomatology: A Pragmatic Randomized Controlled TrialDocument12 pagesLife Review Therapy For Older Adults With Moderate Depressive Symptomatology: A Pragmatic Randomized Controlled TrialAstridNo ratings yet
- PIIS1976131710600059Document11 pagesPIIS1976131710600059Marina UlfaNo ratings yet
- Losely Geriatric Paper 325Document7 pagesLosely Geriatric Paper 325api-532850773No ratings yet
- The Perception of Life and Death in Patients With End-Of-Life Stage Cancer: A Systematic Review of Qualitative ResearchDocument13 pagesThe Perception of Life and Death in Patients With End-Of-Life Stage Cancer: A Systematic Review of Qualitative ResearchPedro TavaresNo ratings yet
- Neurobiology of Resilience in Depression Immune and Vascular InsightDocument78 pagesNeurobiology of Resilience in Depression Immune and Vascular InsightMaria BelénNo ratings yet
- CHF 5Document8 pagesCHF 5Prameswari ZahidaNo ratings yet
- Tan Burden Distress Qol Informal Caregivers Lung CancerDocument11 pagesTan Burden Distress Qol Informal Caregivers Lung CancerRubí Corona TápiaNo ratings yet
- UncertaintyDocument16 pagesUncertaintymaya permata sariNo ratings yet
- Kaptein-Common-Sense Model-OsteoarthritisDocument9 pagesKaptein-Common-Sense Model-OsteoarthritisZyania MelchyNo ratings yet
- Shao2020 PDFDocument7 pagesShao2020 PDFAndrea ZambranoNo ratings yet
- EUTHADocument10 pagesEUTHAJena WoodsNo ratings yet
- Jurnal CKDDocument8 pagesJurnal CKDRatna Dewi CahyaniNo ratings yet
- Clarifying Dementia Risk Factors: Treading in Murky Waters: CommentaryDocument3 pagesClarifying Dementia Risk Factors: Treading in Murky Waters: CommentaryVazia Rahma HandikaNo ratings yet
- Chochinov - Dignity Therapy - A Feasibility Study of EldersDocument13 pagesChochinov - Dignity Therapy - A Feasibility Study of Eldersjuarezcastellar268No ratings yet
- Acarturk Et Al 2016Document11 pagesAcarturk Et Al 2016290971No ratings yet
- Kart Tune N 2010Document10 pagesKart Tune N 2010AndreiaNo ratings yet
- Orofacial Pain: From Basic Science to Clinical Management, Second EditionFrom EverandOrofacial Pain: From Basic Science to Clinical Management, Second EditionNo ratings yet
- Experiences of Adolescents Living with Type 1 Diabetes Mellitus whilst Negotiating with the Society: Submitted as part of the MSc degree in diabetes University of Surrey, Roehampton, 2003From EverandExperiences of Adolescents Living with Type 1 Diabetes Mellitus whilst Negotiating with the Society: Submitted as part of the MSc degree in diabetes University of Surrey, Roehampton, 2003No ratings yet
- RETREAT Framework Et Al. 2018Document12 pagesRETREAT Framework Et Al. 2018happyNo ratings yet
- Hudson 2005Document13 pagesHudson 2005happyNo ratings yet
- Hendrix 2011Document21 pagesHendrix 2011happyNo ratings yet
- ChecklistDocument2 pagesChecklisthappyNo ratings yet
- Hendrix 2006Document6 pagesHendrix 2006happyNo ratings yet
- He Demand 2011Document9 pagesHe Demand 2011happyNo ratings yet
- Davison Et Al 2006Document5 pagesDavison Et Al 2006happyNo ratings yet
- Leadership Joyce 2016Document7 pagesLeadership Joyce 2016happyNo ratings yet
- Big DataDocument20 pagesBig DataBhavnita NareshNo ratings yet
- Essential Kitchen Bathroom Bedroom - September 2014 UKDocument164 pagesEssential Kitchen Bathroom Bedroom - September 2014 UKfishermantoys100% (1)
- Logic Gate Investigatory PDFDocument12 pagesLogic Gate Investigatory PDFGaurang MathurNo ratings yet
- UNICEF's Work in Public Finance For ChildrenDocument2 pagesUNICEF's Work in Public Finance For ChildrenCr CryptoNo ratings yet
- Bibliografía RazaDocument3 pagesBibliografía RazaJorge Vallejo KazacosNo ratings yet
- Plural of NounsDocument1 pagePlural of NounsStrafalogea Serban100% (2)
- 365DayPan DailyEnglishLessonPlanUPDATED2022Document379 pages365DayPan DailyEnglishLessonPlanUPDATED2022KATIUSCA EVELYN GONZALES RIVERANo ratings yet
- Workshop Living in The Czech Republic: WWW - Expatlegal.czDocument22 pagesWorkshop Living in The Czech Republic: WWW - Expatlegal.czImran ShaNo ratings yet
- Brand Engagement With Brand ExpressionDocument27 pagesBrand Engagement With Brand ExpressionArun KCNo ratings yet
- Le Conditionnel Présent: The Conditional PresentDocument8 pagesLe Conditionnel Présent: The Conditional PresentDeepika DevarajNo ratings yet
- Remunerasi RSDocument39 pagesRemunerasi RSalfanNo ratings yet
- Gate Induced Drain Leakage For Ultra Thin MOSFET Devices Using SilvacoDocument2 pagesGate Induced Drain Leakage For Ultra Thin MOSFET Devices Using Silvacosiddhant gangwalNo ratings yet
- NOTICEDocument126 pagesNOTICEowsaf2No ratings yet
- Count and Non-Count Nous (Plural Form of Nous)Document9 pagesCount and Non-Count Nous (Plural Form of Nous)Kathe TafurNo ratings yet
- 11.29.12 Post Standard, The Word Is Out New Law Protects Overdose Victims and HelpersDocument2 pages11.29.12 Post Standard, The Word Is Out New Law Protects Overdose Victims and Helperswebmaster@drugpolicy.orgNo ratings yet
- QTS AplicationDocument8 pagesQTS Aplicationandreuta23No ratings yet
- Reza Sitinjak CJR COLSDocument5 pagesReza Sitinjak CJR COLSReza Enjelika SitinjakNo ratings yet
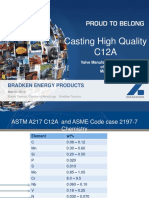
- Casting High Quality C12A: Bradken Energy ProductsDocument37 pagesCasting High Quality C12A: Bradken Energy Productsdelta lab sangliNo ratings yet
- World War IDocument7 pagesWorld War IhzbetulkunNo ratings yet
- English Test-SMA-Kelas-XII-Semester-IDocument4 pagesEnglish Test-SMA-Kelas-XII-Semester-IAru HernalantoNo ratings yet
- Personality and Work Behaviour Exploring The 1996 PDFDocument18 pagesPersonality and Work Behaviour Exploring The 1996 PDFAtif BasaniNo ratings yet
- EstimationDocument106 pagesEstimationasdasdas asdasdasdsadsasddssa0% (1)
- Final For ReviewDocument39 pagesFinal For ReviewMichay CloradoNo ratings yet
- Catholic Ghost Stories of Western PennsylvaniaDocument5 pagesCatholic Ghost Stories of Western PennsylvaniaeclarexeNo ratings yet
- Marketing Research ProcessDocument3 pagesMarketing Research Processadnan saifNo ratings yet
- Novo Nordisk AR 2011 enDocument116 pagesNovo Nordisk AR 2011 enINVESTORNEWNo ratings yet
- Stanford CS193p Developing Applications For iOS Fall 2013-14Document66 pagesStanford CS193p Developing Applications For iOS Fall 2013-14AbstractSoft100% (1)
Axelsson 2012
Axelsson 2012
Uploaded by
happyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Axelsson 2012
Axelsson 2012
Uploaded by
happyCopyright:
Available Formats
E N D O F LI F E A N D P A L L I A T I V E C A R E
Thoughts on death and dying when living with haemodialysis
approaching end of life
Lena Axelsson, Ingrid Randers, Carina Lundh Hagelin, Stefan H Jacobson and Birgitta Klang
Aims and objectives. To describe inner thoughts and feelings relating to death and dying when living with haemodialysis
approaching end of life.
Background. Patients who undergo maintenance haemodialysis suffer a significant symptom burden and an impaired quality of
life. The high mortality rate in these patients indicates that about one-fourth of them are in their last year of life, suggesting the
presence of death and dying in the haemodialysis unit.
Design. A qualitative descriptive design was used.
Methods. A total of 31 qualitative interviews were conducted with eight patients (aged 66–87) over a period of 12 months.
Qualitative content analysis was used to analyse data.
Results. The analysis revealed 10 subthemes that were sorted into three main themes. Being aware that death may be near
comprises being reminded of death and dying by the deteriorating body, by the worsening conditions and deaths of fellow
patients, and by knowing haemodialysis treatment as a border to death. Adapting to approaching death comprises looking upon
death as natural, preparing to face death, hoping for a quick death and repressing thoughts of death and dying. Being alone with
existential thoughts comprises a wish to avoid burdening family, lack of communication with healthcare professionals and
reflections on haemodialysis withdrawal as an hypothetic option.
Conclusions. Living with haemodialysis approaching, the end of life involves significant and complex existential issues and
suffering, and patients are often alone with their existential thoughts.
Relevance to clinical practice. Nurses and other healthcare professionals in haemodialysis settings need to combine technical
and medical abilities with committed listening and communication skills and be open to talking about death and dying, with
sensitivity to individual and changeable needs.
Key words: death, dying, end of life, end-stage renal disease, haemodialysis, qualitative content analysis, qualitative interviews,
serial interviews
Accepted for publication: 26 February 2012
renal transplantation, is increasing worldwide (Eggers 2011).
Introduction
The number of patients with ESRD on maintenance hae-
End-stage renal disease (ESRD) (stage 5 chronic kidney modialysis treatment (MHD) is growing in western society.
disease), which requires treatment with lifelong dialysis or Annual mortality rates in these patients are about 20–25%
Authors: Lena Axelsson, RN, Doctoral Student, Sophiahemmet Institutet; Stefan H Jacobson, MD, Professor, Department of
University College and Division of Nursing, Department of Nephrology, Karolinska Institutet and Danderyd University
Neurobiology, Care Sciences and Society, Karolinska Institutet; Hospital; Birgitta Klang, RNT, Associate Professor, Division of
Ingrid Randers, RNT, PhD, Senior Lecturer, Sophiahemmet Nursing, Department of Neurobiology, Care Sciences and Society,
University College and Division of Nursing, Department of Karolinska Institutet, Stockholm, Sweden
Neurobiology, Care Sciences and Society, Karolinska Institutet; Correspondence: Lena Axelsson, Doctoral Student, Sophiahemmet
Carina Lundh Hagelin, RN, PhD, Senior Lecturer, Sophiahemmet University College, Box 5605, Stockholm 11486, Sweden.
University College and Department of Learning, Informatics, Telephone: +46 70 848 93 08.
Management and Ethics, Medical Management Center, Karolinska E-mail: lena.axelsson@shh.se
Ó 2012 Blackwell Publishing Ltd
Journal of Clinical Nursing, 21, 2149–2159, doi: 10.1111/j.1365-2702.2012.04156.x 2149
L Axelsson et al.
(SNR 2010, USRD 2010), indicating that about one-fourth whole person care in their hovering between living in the
of patients on MHD are in their last year of life. This present and worrying about the future, that is facing death
enlightens the presence of death and dying in the haemo- (Axelsson et al. 2012).
dialysis unit. Existential issues have also been described in other studies
of patients’ experiences of MHD. It has been interpreted as a
continuous struggle to maintain hope of a normal life while
Background
dealing with an uncertain future, with questions of meaning
Earlier studies stress the impaired quality of life (Kimmel & and how much time there is left (Gregory et al. 1998). MHD,
Patel 2006, Davison & Jhangri 2010) and significant symp- as a deficient lifeline, has also shown to be a persistent
tom burden (Davison et al. 2006, Saini et al. 2006, Murtagh reminder of a limited lifetime (Hagren et al. 2001). The
et al. 2007) that patients undergoing MHD suffer because of changed life situation experienced by patients undergoing
uraemia and the effects of dialysis. Frequently described MHD, in the dimensions of time and space, has also been
symptoms are lack of energy, decreased appetite, nausea, described as an existential struggle (Hagren et al. 2005), and
pain, pruritus, shortness of breath, sleep disturbances, anx- patients on MHD have been found to fight for personal
iety, muscular cramp and dizziness (Weisbord et al. 2004, preservation while acknowledging the nearness of and
2005). Comorbidities such as diabetes, cardiac disease, awaiting a certain death (Calvin 2004).
cerebrovascular disease and peripheral vascular disease add In the dialysis unit, the nurse cares for patients who have
to the symptom burden and the complexity of the suffering several chronic progressive and life-threatening illnesses and
(Weisbord et al. 2003, 2005). Mortality rates are due largely they suffer from a high symptom burden. Furthermore, these
to comorbidities, with cardiovascular disease causing about severely ill patients maintain life by advanced medical
45% of deaths in patients on MHD (SNR 2010). The mean technology that also raises existential issues. The presence
age of patients undergoing MHD is rising (SNR 2010, USRD of death in the dialysis unit has come forth, and to better
2010), which further decreases life expectancy in this understand and improve care for severely ill patients treated
population. Withdrawal of dialysis treatment precedes about with MHD, we need more knowledge about their experiences
13% (SNR 2010) to 25% (Germain & Cohen 2008) of and increase our understanding of their thoughts and feelings
deaths in patients with MHD and results in an average relating to death and dying when they are approaching end of
remaining survival time of eight days (Cohen et al. 2000a,b). life.
Withholding or initiating withdrawal from dialysis (Cohen
et al. 2000a, Cohen & Germain 2005) has been the focus of
Methods
palliative care for patients with ESRD. However, the ageing
patient population with their complex symptoms and com-
Aim
orbidities has raised awareness of the need to integrate
palliative care approach earlier in nephrology care and for a The aim of this study was to describe inner thoughts and
longer time (Young 2009, Kurella Tamura & Cohen 2010, feelings relating to death and dying when living with
Harrison & Watson 2011). Implementation of the philoso- haemodialysis approaching end of life.
phy of palliative care in the haemodialysis unit, with active
care for the whole person, has also been put forward as many
Design
patients suffer from continuous deterioration (Madar et al.
2007). A qualitative descriptive design with an inductive approach
An earlier study (Axelsson et al. 2012) on the meanings of was used.
being severely ill living with MHD at the approach of end of
life elucidates complexities and intertwined meanings when
Participants and setting
the deteriorating body influences life more and more, and
patients are enduring a restricted and heavy life for the This study is part of an ongoing study intending to increase
possibility of living a bit longer. Being severely ill living with the understanding and knowledge of end-of-life issues in
MHD means facing progressive losses and threats, and severely ill patients living with MHD. In a first study
findings elucidate suffering in physical, psychosocial, emo- (Axelsson et al. 2012), the meanings of being severely ill
tional and existential dimensions. Findings showed the living with haemodialysis were described, while the present
importance of knowing the patients’ own understanding of study seeks for a deeper understanding of thoughts and
their illness and situation and underpin the importance of feelings relating to death and dying.
Ó 2012 Blackwell Publishing Ltd
2150 Journal of Clinical Nursing, 21, 2149–2159
End of life and palliative care Thoughts on death and dying
Eight severely ill adults with ESRD, five men and three tell me your experiences of living with illness and haemod-
women, participated (previously described in Axelsson et al. ialysis’. Open and clarifying questions invited participants to
2012). They were selected with purposive sampling for talk about different dimensions and thereby their thoughts
variation in comorbidities, sex and family situation. The and feelings relating to death and dying. The first author
participants were recruited from four dialysis clinics, two in conducted all 31 interviews on days when the participant was
university hospitals and two smaller dialysis satellites in an free from dialysis. Most interviews (26) took place, according
urban area of Sweden. Participants were clinically assessed as to the participants’ wishes, in the participants’ homes, but
severely ill and therefore possibly in their last year of life, by five were conducted at a nursing home or on a hospital ward.
the nephrology physician and the registered dialysis nurse The interviews (33 hours in total) were audiotaped and
responsible for their dialysis treatments. For this study, we transcribed verbatim.
define this as approaching death. The assessment was based on
the presence of comorbidities, malnutrition and other com-
Data analysis
plications. Inclusion criteria were also to have been treated
with haemodialysis for at least three months, not to be listed Qualitative content analysis was applied when analysing the
for kidney transplantation, and to be able to read, write and data (Graneheim & Lundman 2004). The interview texts
speak Swedish. In addition to kidney disease, the participants were read several times to grasp the overall content.
had a multiplicity of comorbidities, including cardiac disease, ‘Meaning units’ (i.e. parts of sentences, sentences or para-
peripheral vascular disease, previous stroke, diabetes and graphs each containing a meaning) corresponding to the aim
cancer. Most participants had several comorbidities. of the present study were then identified, and the extracted
At the time of inclusion, five participants lived with a text (i.e. meaning units relating to death and dying) was then
spouse and three lived alone. All lived at home and received condensed and coded. The coded units were re-read,
haemodialysis as outpatients. Their ages ranged from compared, interpreted and when appropriate re-combined.
66–87 years (mean = 78). They had received MHD from Thereafter, they were abstracted and sorted into subthemes
15 months to just over seven years. and themes of underlying meaning (Graneheim & Lundman
2004). To gain a deeper understanding during the analysis,
meaning units of all interviews of each participant were both
Ethical considerations
compared over time and analysed as a whole. The analysis
Dialysis nurses gave selected patients a letter about the study process is described as linear, but there was a movement,
including an offer to meet the researcher for additional back and forth, between the described steps of the analysis.
information. Before giving written consent to participation, The software Open Code (2007) was used in the process of
all participants received further information, both written coding to more easily gain an overview of the data through
and verbal, describing the aim of the study, the voluntary printing lists of the coded units.
nature of their participation, their right to discontinue at any
time and the confidential treatment of data. These severely ill
Results
participants narrated their thoughts and feelings, which
required the researcher to be thoughtful and sensitive during When living with MHD and approaching the end of life, the
interviews. The study was approved by the Ethical Review presence of death was multifaceted. Patients’ thoughts and
Board Stockholm, Sweden. feelings about death and dying were complex, and they
fluctuated, both during and between interviews, as existential
issues and needs are intertwined with experiences in physical,
Data collection
social and psychological dimensions.
Data were collected for the study using qualitative serial The findings were formulated as 10 subthemes and three
interviews during 2007–2008. Six of the participants were themes, which are presented in Table 1 and illustrated in the
followed according to the plan with four interviews over text with representative quotations from the interviews. To
12 months. One participant was interviewed five times, communicate and illuminate the participants’ inner thoughts
because one interview was interrupted. Owing to family and feelings, quotations are presented as poems. The
matters, one participant was interviewed twice. The partic- technique we used means that the words are still presented
ipants were encouraged to talk freely about their experiences verbatim, but the text is divided into lines when semantic
of being ill and living with MHD. The interviews began with features as pauses and hesitation appear (cf. Edvardsson et al.
the open-ended question (Kvale & Brinkmann 2009): ‘Please 2003, Öhlén 2003, Lindqvist et al. 2006, Schuster 2006).
Ó 2012 Blackwell Publishing Ltd
Journal of Clinical Nursing, 21, 2149–2159 2151
L Axelsson et al.
Table 1 Subthemes and themes you think
what will happen to me
Subthemes Themes
what will the end be like
Being reminded of death and dying Being aware that that’s on your mind
by the deteriorating body death may be near
Being reminded of death and dying by the The state of very ill fellow patients had different meanings
worsening conditions and deaths depending on the participant’s own condition. One partici-
of fellow patients
pant described that in comparison with some other patients,
Knowing dialysis treatment as a
border to death
he thought that he himself had managed well, which made
Looking upon death as natural Adapting to him feel stronger. However, later, when he was more ill, he
Preparing to face death approaching death expressed distress about seeing others’ worsening conditions.
Hoping for a quick death The number of deaths among fellow patients raised internal
Repressing thoughts of death and dying questions about what was happening and whose turn would
Wish to avoid burdening family Being alone with
be next. This also contributed to fears about going to hospital
Lack of communication with existential thoughts
healthcare professionals because of an acute condition. One participant described his
Haemodialysis withdrawal as a feelings when a fellow patient had died:
hypothetical option
Death came closer
you know
Being aware that death may be near since I’d come to the dialysis ward two had died
and this was the third one
Being aware that death may be near involved being reminded
so then
of death and dying by the deteriorating body, by the
it sort of reminds you of approaching something
worsening conditions or deaths of fellow patients, and by
I don’t usually think of it
knowing MHD as a border to death.
but when you get this kind of reminder
The participants were aware that death might come soon.
how fast it may go
Their progressively deteriorating bodies reminded them of
then you think it over
their approaching death, and some types of pain seemed
and wonder how long you will last
especially to involve a threat of imminent death. Relief of
pain and other symptoms was comforting and allowed some The closeness of death was also expressed by descriptions of
distance from death, although they were aware that manag- MHD as a border between life and death, sometimes
ing symptoms did not necessarily imply a longer lifetime. Old apparent in the body between dialysis treatments. Some
age in itself also raised awareness of approaching death. participants said that death had become a threat already
when informed of the necessity of MHD, and they had not
Sometimes I think
expected to live as long as they had.
well
is this the so-called final journey
Adapting to approaching death
if I travel by ambulance to the hospital
Adapting to approaching death involved looking upon death
or
as natural and preparing to face it, but also hoping for a
how will it feel
quick death and repressing thoughts of death and dying.
I am also so old
The older participants looked upon death as something
that I know
natural for the old and ill. Thus, death was described as an
that there are many who can’t make it this far
inevitable part of everybody’s life, and that they had lived
The participants described how the worsening conditions and their lives.
deaths of fellow patients at the dialysis clinic reminded them
It is not that strange
of their own vulnerable situation and caused them to wonder
actually
about the end of life and death.
that a person passes away
You see other patients on the dialysis ward who have problems who is ill
you notice how they deteriorate
Feelings of living too long and living a prolonged life were
and
also described, but at the same time, participants wanted to
you hope that it won’t last long
Ó 2012 Blackwell Publishing Ltd
2152 Journal of Clinical Nursing, 21, 2149–2159
End of life and palliative care Thoughts on death and dying
live longer, and thinking of death as normal still involved Moreover, all their children had been present when they
sadness. woke up from unconsciousness, which was also reassuring.
Participants used different ways to prepare to face death.
I have experienced it so I know it
Reading the obituary notices to compare ages emerged as a
what it is like to pass away
way of handling uncertainty through looking for clues, but
so I am not afraid of dying
was also part of reconciling with approaching end of life.
you just fall asleep
Participants reflected on what the cause of death would be
considering all their comorbidities, when and how death Repressing thoughts of death and dying was another way to
would come, and what dying would be like. On the other handle distress and sorrow when approaching the end of life.
hand, participants also said that there was no meaning in Living was easier without the burden of thinking of death,
trying to figure out death. even if death was considered as natural.
Well it isn’t this week anyway No
I think one definitely must not think about it
but that one will die
but sometimes I have to no
I realize that one definitely should not do that
that it will happen one day
I: What is your thinking?
and then I wonder which day
will be the one No
when I can’t walk if I were to go around and think of dying
when I get an infection they can’t find then
when the medicine has no effect then it would be terrible
and then maybe they will lose interest in doing anything no
and I don’t do that
well
Repressing thoughts of dying emerged as a way to distance
I can’t do much about it
and postpone death, not as denial, but as a way to focus on
I hope it won’t be too drawn out
living. Instead, participants turned their thoughts towards the
Participants appeared to fear the end of life more than death good things in life.
itself. Their hopes for a quick death seemed to be connected
to their uncertainty about end of life and dying. They feared a Being alone with existential thoughts
drawn-out end of life totally incapacitated and dependent on Being alone with existential thoughts involved to avoid bur-
others. There was also a sincere wish to live at home until dening family, lack of communication with healthcare pro-
they died a sudden death. fessionals and reflections on MHD withdrawal as a
hypothetical option. Participants found it difficult to talk
That is what I fear the most
about their thoughts and feelings concerning death and dying.
becoming totally dependent on others
They did not want to burden their family additionally with
that is the worst
their existential thoughts. They thought their family did not
yes the best would be to drop dead
want to talk of death, and some described their family as
I think
afraid. Some participants had tried to talk about end of life
A sudden death was acknowledged as more difficult for the and death, but felt that their concerns were pushed away.
family, but one participant reflected that death now would Therefore, they kept existential thoughts to themselves, and
not be sudden in the meaning of unexpected because the everyday life was carried on trying to be as usual. Participants
family must have noticed his weakening condition. Although also described not knowing how to deal with this complex
they hoped for a quick death, the chance of it happening was situation.
also a threat, as hoping for a quick death was not the same as
Well I don’t know if
wanting to die soon.
if maybe one should prepare oneself for
Two participants thought they had already experienced
for the future
what death is like. Therefore, they did not fear the moment of
and perhaps prepare others as well
death, because they now thought of death as falling asleep.
Ó 2012 Blackwell Publishing Ltd
Journal of Clinical Nursing, 21, 2149–2159 2153
L Axelsson et al.
I don’t know because ‘physicians are not allowed to put somebody to
I am not quite sure about how to deal with it death’.
sometimes I think to myself about it Death by MHD withdrawal did not emerge as a real
but alternative for the participants. Some had reflected on the
I probably can’t speak to anyone else about it possibility, as a hypothetical option in a different family
situation or if they became totally dependent on care.
Participants’ need to talk about existential issues, fears and
uncertainties varied over time with complications or critical Sometimes I can reason that if I did not have a wife who is strong and
events. They also described hesitation and uncertainty about able
talking to healthcare professionals about death and dying and and children and grandchildren
found it difficult to bring up existential topics. The impor- if I did not have family and all
tance of trust and continuity was described. The significance then maybe I would have discontinued dialysis
of talking to the right person and of healthcare professionals simply ended
showing interest was emphasised. One participant described
not knowing whether the care professionals were cowards or You want to go to the toilet, take a shower, wash yourself, brush
considerate when they avoided talking of his vulnerable your teeth
illness situation. Participants also thought that the care and all those sorts of things you always do
professionals had other things to attend to. Another reason and if I couldn’t do those things
not to open up was a fear that care professionals would be then that would
careless with thoughts and sentiments revealed in confidence. that would probably be the end
Participants described not having anyone to talk to about and then I could imagine
existential thoughts. Having to manage those thoughts alone I could imagine to discontinue dialysis
was attributed partly to the feeling that nobody would because I don’t want to
understand. I don’t want to be totally dependent on care
When a fellow patient had died, the atmosphere in the
The hypothetical criteria for MHD withdrawal as an option
haemodialysis unit was described as silent. Usually the nurses
changed over time. Also views of withdrawal could change.
answered the direct question of whether a patient had died,
One participant did not consider MHD withdrawal an
but they were reluctant to talk further. The participants said
alternative, as he wanted to hold on as long as possible.
that they understood that the nurses were not allowed to tell
Yet later, as he lost more and more control over his
them about their fellow patients, but still, when they thought
deteriorating body, he reflected on dialysis withdrawal as a
of the dead patient as a friend with whom they had talked
possibility one day. Another participant, who in the first
and laughed during dialysis, it was hard.
interview, reflected on withdrawal as a hypothetical option,
Being alone with existential thoughts also involved reflec-
when more ill and closer to death, then instead thought of
tions on MHD withdrawal. Some participants appeared to
MHD withdrawal as suicide. Length of life seemed to have
want to know more about death by withdrawal but feared
more value when he was closer to death, in spite of the
that bringing up the topic might be understood as wanting to
increased dependence he had earlier feared. He did not want
discontinue dialysis treatment. Withdrawal was also de-
to leave this life or his family. On the other hand, even if
scribed as a delicate matter that could be provocative if raised
withdrawal was not considered an option, some participants
by healthcare professionals. One participant described when
reflected on the value of prolonging life vs. maintaining well-
he had tried to talk to a nurse about dialysis withdrawal:
being at the end of life, and postponing death was not always
I asked what will happen if I quit this regarded as crucial. One participant described her agony
he just looked at me when she suffered from restrictions:
you’ll die
The question is whether I draw out a few months more or less
he said and left
of the time that I have left
well that I knew
that is in my condition
I thought to myself
see
Participants had various conceptions about MHD with- I don’t know how to express it but
drawal, including that it involved a death in agony. One but for me it is almost better to die
participant thought that withdrawal was not permitted than to be suffering this way
Ó 2012 Blackwell Publishing Ltd
2154 Journal of Clinical Nursing, 21, 2149–2159
End of life and palliative care Thoughts on death and dying
Narratives revealed ambivalent thoughts and feelings about they were unable to talk about it. Still, even when partici-
life and death in patients suffering from illness and a pants focused on living, death was always nearby. This may
deteriorating body in pain. be interpreted as patients maintain a subtle balance between
recognising approaching death and recognising remaining life
In a way I don’t want to live any longer see
(Hallberg 2004).
with this that I know
The participants’ wish to focus on living was also shown by
that I will not get well again
their reflections on withdrawal of MHD as a hypothetical
but on the other hand
option, but not as a real alternative. Findings indicate that
one doesn’t exactly want to die either
attitudes towards withdrawal and circumstances for consid-
ering it may change over time. This changeability, along with
Discussion
participants’ lack of knowledge and fears of being misread if
This qualitative study focused on the inner thoughts and they ask about withdrawal, highlights the importance and
feelings about death and dying in severely ill patients living challenges of attentive listening and communication with
with MHD approaching end of life. Participants were aware patients.
of their approaching death, but lived with the uncertainty of Participants in the present study did not want to burden
how and when it would happen. While they focused on their family additionally with their existential concerns. Their
living, their narratives reveal that thoughts of death and desire to protect their family by not speaking of their worries
dying were never far away. The presence of death is and fears, however, left them facing the existential loneliness
multifaceted and intertwined with other dimensions of life, also described in patients with other diseases approaching the
and existential thoughts and feelings may fluctuate or change end of life (Sand & Strang 2006, Ek & Ternestedt 2008).
over time. Moreover, the individual perspective, depending Being alone with existential thoughts involved lack of
on experiences, values and age, is vital. communication with healthcare professionals and difficulties
Older participants thought of death as natural and that raising existential topics. Participants’ hesitation is in line
life had to end at some point. Participants feared the with other studies showing that patients often wait for care
uncertain end of life more than death itself. Their evident professionals to initiate talks about death and dying (Davison
fear of a prolonged end of life when being totally dependent 2006, Davison & Simpson 2006). Our findings indicate that
on others agrees with results of other studies of older patients want more communication concerning end of life, as
peoples’ views of death (Hallberg 2004, Ternestedt & shown also by Berzoff et al. (2008).
Franklin 2006, Gott et al. 2008). Participants in the present Unrecognised existential needs have earlier also been
study expressed hopes for a sudden or quick death. This reported in patients with cancer and heart failure (Adelbratt
may be interpreted as a wish to escape progressive losses & Strang 2000, Murray et al. 2004). Obstacles to existential
and suffering as they are facing threats of complications, support were described as healthcare professionals’ stress,
and of losing control, sense of self and dignity (Axelsson fear and lack of knowledge (Strang et al. 2001). This is in line
et al. 2012). Our data indicate that also a worsening with the present findings where participants described care
condition and dying process of fellow patients caused fears professionals’ lack of interest, avoidance and attention to
about the participant’s own end of life. A preference for other priorities in relation to communicating about existen-
sudden death in older people with heart failure was tial issues. Participants also said that it was difficult for others
discussed in terms of maintaining personhood until death to understand their situation, which may be another reason
and avoiding the process of dying, which coincides with not to talk of existential matters.
present findings (Gott et al. 2008). Participants’ thoughts on death show that they lived with
Our findings indicate that adapting to approaching death awareness of that death may be near. Their awareness seemed
and thinking of death as natural also involved repressing to be based on signs and inferences rather than on open
thoughts of death. This seemed a way to distance sorrow and communication with healthcare professionals. Findings illu-
death, to focus on living and to enjoy life, as also described by minate that awareness may be consistent with repressing
Calvin (2004) in a theory of personal preservation in patients thoughts on death to focus on living. Thoughts were also
on MHD treatment. Repressing thoughts of death shows a repressed of consideration to family members or because of
will to live (Gadamer 2003). On the other hand, Hallberg healthcare professionals’ behaviour, which may also obstruct
(2004), in a study of older people, discusses pushing away communication on existential issues and add to patients’
death in relation to a taboo of talking about it. In the present existential loneliness. The significance of the interaction
study, participants also pushed away thoughts of death when between the person approaching end of life and those around
Ó 2012 Blackwell Publishing Ltd
Journal of Clinical Nursing, 21, 2149–2159 2155
L Axelsson et al.
him, both family and professionals, is illuminated by Glaser future is one way to open a conversation that might include
and Strauss (1965) in the theory on awareness of dying. Their existential topics, and it allows the patient to decide the
theory on communication on death and dying, still of clinical appropriate timing. It is also important to create a
relevance (Andrews & Nathaniel 2009), describes the signif- supportive relationship of safety and trust with patients
icance of behaviour and communication for the experience of and to take an interest in their subjective perspective and
end of life (Glaser & Strauss 1965). their whole person. Maintaining life with haemodialysis
The unpredictable course of dying in patients with heart treatment involves a responsibility to aim for the patient’s
failure made nurses in palliative care consider it difficult to well-being when approaching end of life. Thus present
talk about death (Brännström et al. 2005). This may also be findings forward that an integration of the palliative care
an impediment in haemodialysis care as death is often philosophy in haemodialysis units could assist in improving
unpredictable and uncertain. However, this could be a care of these severely ill patients, as the philosophy
challenge rather than an obstacle to nurses in haemodialysis acknowledges death as part of life, while still recognising
units as the individual need of the patient, living with a life and aiming for well-being until life has ended (Saun-
multifaceted presence of death, should direct communication, ders1978, WHO 2002).
and nurses should be attentive to fluctuating needs in their
unpredictable and uncertain course of dying. Findings indi-
Methodological considerations
cate that living with a deteriorating body, a high symptom
burden and dependence on advanced medical technology A weakness of the study may be that participants were
involves existential issues and suffering, and patients are included according to clinical assessments of severe illness,
often alone with their existential thoughts. Difficulties but on the other hand, clinical assessment of patients will also
expressing and sharing their suffering indicate increasing be used to implement the findings in clinical practice. In a
vulnerability in patients with life-threatening illness (Öhlén chronic progressive disease, it may be difficult to know when
2000) whose existential suffering could be alleviated if it were end of life begins but participants’ narratives show that they
acknowledged (Öhlén 2000). thought of life as closing down and of approaching death,
which adds to credibility. The purposive sampling, that is
choosing participants of various gender, family situation and
Conclusion
comorbidities from four different dialysis clinics thus with
Thoughts and feelings relating to death and dying are various experiences, also contributes to credibility. Interviews
significant and complex for persons living with MHD (31) over time yielded richness of data. As the participants
approaching the end of life. Participants lived with the were severely ill with progressive chronic diseases, the
awareness of approaching death but in uncertainty of how longitudinal approach also increased the possibility of iden-
and when. Adapting to approaching death included tifying changes and variations and thus increased the under-
repressing thoughts of death to focus on living the time standing. This strengthens the findings in relation to the
left. Participants were alone with existential issues, which number of participants. Repeated encounters in interviews
varied in intensity as they are intertwined and fluctuate over time facilitated conversations on existential issues,
with other dimensions of life. Findings indicate that it is which also contributed to richness and credibility. Three of
important for these patients to be able to talk about the authors read the interviews, and after open and reflective
existential issues to someone who will listen and that this discussions, we agreed upon subthemes and themes. The
need may vary both with the individual and with circum- authors’ different preunderstandings of the phenomenon
stances over time. under study contributed to critical reflections and analysis,
which add to credibility and thus trustworthiness (Graneheim
& Lundman 2004). The methodological analysis together
Relevance to clinical practice
with representative quotations further contributes to trust-
Healthcare professionals in haemodialysis settings need to worthiness. Presenting the quotations as poems (i.e. we
combine technical and medical abilities with committed divided the verbatim text into lines) (i.e. Edvardsson et al.
listening and communication skills. They need to address 2003, Öhlén 2003, Lindqvist et al. 2006, Schuster 2006) is a
existential thoughts and feelings, as well as physical and method to communicate and read participants’ quotations
psychosocial issues, and offer opportunities to talk about more slowly and thereby more deeply and thus being more
death and dying, with sensitivity to individual and change- sensitive to participants and their narratives as how it is
able needs. Asking patients about their thoughts for the spoken contributes to understanding.
Ó 2012 Blackwell Publishing Ltd
2156 Journal of Clinical Nursing, 21, 2149–2159
End of life and palliative care Thoughts on death and dying
We consider findings to be transferable to similar contexts
Contributions
and of value also in the care of other groups of patients in the
haemodialysis unit, and the detailed description of partici- Study design: LA, IR, SHJ, BK; data collection: LA; data
pants and context facilitates judgements of transferability. analysis: LA, IR, BK and manuscript preparation: LA, IR,
CLH, SHJ, BK.
Acknowledgement
Conflict of interest
This research was supported by Sophiahemmet Foundation,
Stockholm. The authors declare to have no conflict of interests.
References
Adelbratt S & Strang P (2000) Death anxiety stage renal disease: the patient tion. Advances in Chronic Kidney Dis-
in brain tumour patients and their perspective. Clinical Journal of the ease 15, 133–139.
spouses. Palliative Medicine 14, 499– American Society of Nephrology 1, Glaser BG & Strauss AL (1965) Awareness
507. 1023–1028. of Dying. Aldine, Chicago, IL.
Andrews T & Nathaniel AK (2009) Davison SN & Jhangri GS (2010) Impact of Gott M, Small N, Barnes S, Payne S &
Awareness of dying revisited. Journal of pain and symptom burden on the Seamark D (2008) Older people’s views
Nursing Care Quality 24, 189–193. health-related quality of life of hemod- of a good death in heart failure: impli-
Axelsson L, Randers I, Jacobson SH & ialysis patients. Journal of Pain and cations for palliative care provision.
Klang B (2012) Living with haemodia- Symptom Management 39, 477–485. Social Science & Medicine 67, 1113–
lysis when nearing end of life. Scandi- Davison SN & Simpson C (2006) Hope and 1121.
navian Journal of Caring Sciences 26, advance care planning in patients with Graneheim UH & Lundman B (2004)
45–52. end stage renal disease: qualitative Qualitative content analysis in nursing
Berzoff J, Swantkowski J & Cohen LM interview study. British Medical Jour- research: concepts, procedures and
(2008) Developing a renal supportive nal 333, 886. measures to achieve trustworthiness.
care team from the voices of patients, Davison SN, Jhangri GS & Johnson JA Nurse Education Today 24, 105–112.
families, and palliative care staff. (2006) Cross-sectional validity of a Gregory DM, Way CY, Hutchinson TA,
Palliative and Supportive Care 6, 133– modified Edmonton symptom assess- Barrett BJ & Parfrey PS (1998) Patients’
139. ment system in dialysis patients: a perceptions of their experiences with
Brännström M, Brulin C, Norberg A, simple assessment of symptom bur- ESRD and hemodialysis treatment.
Boman K & Strandberg G (2005) Being den. Kidney International 69, 1621– Qualitative Health Research 8, 764–
a palliative nurse for persons with 1625. 783.
severe congestive heart failure in Edvardsson D, Rasmussen BH & Riessman Hagren B, Pettersen IM, Severinsson E,
advanced home care. European Journal CK (2003) Ward atmospheres of horror Lutzen K & Clyne N (2001) The hae-
of Cardiovascular Nursing 4, 314–323. and healing: a comparative analysis of modialysis machine as a lifeline: expe-
Calvin AO (2004) Haemodialysis patients narrative. Health: An Interdisciplinary riences of suffering from end-stage
and end-of-life decisions: a theory of Journal for the Social Study of Health, renal disease. Journal of Advanced
personal preservation. Journal of Ad- Illness and Medicine 7, 377–396. Nursing 34, 196–202.
vanced Nursing 46, 558–566. Eggers PW (2011) Has the incidence of end- Hagren B, Pettersen IM, Severinsson E,
Cohen LM & Germain MJ (2005) The stage renal disease in the USA and other Lutzen K & Clyne N (2005) Mainte-
psychiatric landscape of withdrawal. countries stabilized? Current Opinion nance haemodialysis: patients’ experi-
Seminars in Dialysis 18, 147–153. in Nephrology and Hypertension 20, ences of their life situation. Journal of
Cohen LM, Germain M, Poppel DM, 241–245. Clinical Nursing 14, 294–300.
Woods A & Kjellstrand CM (2000a) Ek K & Ternestedt BM (2008) Living with Hallberg IR (2004) Death and dying from
Dialysis discontinuation and palliative chronic obstructive pulmonary disease old people’s point of view. A literature
care. American Journal of Kidney Dis- at the end of life: a phenomenological review. Aging Clinical and Experimen-
eases 36, 140–144. study. Journal of Advanced Nursing 62, tal Research 16, 87–103.
Cohen LM, Germain MJ, Poppel DM, 470–478. Harrison K & Watson S (2011) Palliative
Woods AL, Pekow PS & Kjellstrand Gadamer H-G (2003) Den gåtfulla hälsan: care in advanced kidney disease: a
CM (2000b) Dying well after discon- essäer och föredrag (On the Mystery of nurse-led joint renal and specialist pal-
tinuing the life-support treatment of Health: Essays and Lectures). Dualis liative care clinic. International Journal
dialysis. Archives of Internal Medicine Förlag, Ludvika, Sweden. of Palliative Nursing 17, 42–46.
160, 2513–2518. Germain MJ & Cohen LM (2008) Main- Kimmel PL & Patel SS (2006) Quality of
Davison SN (2006) Facilitating advance taining quality of life at the end of life life in patients with chronic kidney dis-
care planning for patients with end- in the end-stage renal disease popula- ease: focus on end-stage renal disease
Ó 2012 Blackwell Publishing Ltd
Journal of Clinical Nursing, 21, 2149–2159 2157
L Axelsson et al.
treated with hemodialysis. Seminars in ratives in empirical phenomenological Disease in the United States. National
Nephrology 26, 68–79. inquiry into human suffering. Quali- Institutes of Health, National Institute
Kurella Tamura M & Cohen LM (2010) tative Health Research 13, 557–566. of Diabetes and Digestive and Kidney
Should there be an expanded role for Open Code (2007) UMDAC and Epidemi- Diseases, Bethesda, MD.
palliative care in end-stage renal dis- ology, Version 3.4. Department of Weisbord SD, Carmody SS, Bruns FJ, Rot-
ease? Current Opinion in Nephrology Public Health and Clinical Medicine, ondi AJ, Cohen LM, Zeidel ML &
and Hypertension 19, 556–560. University of Umeå, Umeå. Arnold RM (2003) Symptom burden,
Kvale S & Brinkmann S (2009) Interviews: Saini T, Murtagh FE, Dupont PJ, McKin- quality of life, advance care planning
Learning the Craft of Qualitative Re- non PM, Hatfield P & Saunders Y and the potential value of palliative care
search Interviewing. Sage Publications, (2006) Comparative pilot study of in severely ill haemodialysis patients.
Thousand Oaks, CA. symptoms and quality of life in cancer Nephrology Dialysis Transplantation
Lindqvist O, Widmark A & Rasmussen BH patients and patients with end stage 18, 1345–1352.
(2006) Reclaiming wellness – living renal disease. Palliative Medicine 20, Weisbord SD, Fried LF, Arnold RM, Rot-
with bodily problems, as narrated by 631–636. ondi AJ, Fine MJ, Levenson DJ &
men with advanced prostate cancer. Sand L & Strang P (2006) Existential lone- Switzer GE (2004) Development of a
Cancer Nursing 29, 327–337. liness in a palliative home care setting. symptom assessment instrument for
Madar H, Gilad G, Elenhoren E & Sch- Journal of Palliative Medicine 9, 1376– chronic hemodialysis patients: the
warz L (2007) Dialysis nurses for pal- 1387. Dialysis Symptom Index. Journal of
liative care. Journal of Renal Care 33, Saunders C (1978) The philosophy of ter- Pain and Symptom Management 27,
35–38. minal care. In The Management of 226–240.
Murray SA, Kendall M, Boyd K, Worth A & Terminal Disease (Saunders C ed.). Weisbord SD, Fried LF, Arnold RM, Fine
Benton TF (2004) Exploring the spiritual Edward Arnold, London, pp. 193–202. MJ, Levenson DJ, Peterson RA &
needs of people dying of lung cancer or Schuster M (2006) Profession och existens Switzer GE (2005) Prevalence, severity,
heart failure: a prospective qualitative (Profession and Existence). Daidalos, and importance of physical and
interview study of patients and their ca- Gothenburg (In Swedish). emotional symptoms in chronic he-
rers. Palliative Medicine 18, 39–45. SNR (2010) Svenskt njurregister (Swedish modialysis patients. Journal of the
Murtagh FE, Addington-Hall J & Higginson Renal Registry) Annual Data Report, American Society of Nephrology 16,
IJ (2007) The prevalence of symptoms Jönköping. 2487–2494.
in end-stage renal disease: a systematic Strang S, Strang P & Ternestedt BM (2001) WHO (2002) World Health Organization
review. Advances in Chronic Kidney Existential support in brain tumour DefinitionofPalliativeCare.Availableat:
Disease 14, 82–99. patients and their spouses. Supportive http://www.who.int/cancer/palliative/
Öhlén J (2000) Att vara i en fristad, berät- Care in Cancer 9, 625–633. definition/en/ (accessed 12 May 2011).
telser om lindrat lidande inom palliativ Ternestedt BM & Franklin LL (2006) Ways Young S (2009) Rethinking and integrating
vård (Being in a Lived Retreat: Narra- of relating to death: views of older nephrology palliative care: a nephrol-
tives of Alleviated Suffering Within people resident in nursing homes. ogy nursing perspective. Journal of the
Palliative Care). University of Gothen- International Journal of Palliative Canadian Association of Nephrology
burg, Gothenburg (In Swedish) (Sum- Nursing 12, 334–340. Nurses and Technicians 19, 36–44.
mary in English). USRD (2010) US Renal Data System
Öhlén J (2003) Evocation of meaning Annual Data Report: Atlas of Chronic
through poetic condensation of nar- Kidney Disease and End-Stage Renal
Ó 2012 Blackwell Publishing Ltd
2158 Journal of Clinical Nursing, 21, 2149–2159
End of life and palliative care Thoughts on death and dying
The Journal of Clinical Nursing (JCN) is an international, peer reviewed journal that aims to promote a high standard of
clinically related scholarship which supports the practice and discipline of nursing.
For further information and full author guidelines, please visit JCN on the Wiley Online Library website: http://
wileyonlinelibrary.com/journal/jocn
Reasons to submit your paper to JCN:
High-impact forum: one of the world’s most cited nursing journals and with an impact factor of 1Æ228 – ranked 23 of 85
within Thomson Reuters Journal Citation Report (Social Science – Nursing) in 2009.
One of the most read nursing journals in the world: over 1 million articles downloaded online per year and accessible in over
7000 libraries worldwide (including over 4000 in developing countries with free or low cost access).
Fast and easy online submission: online submission at http://mc.manuscriptcentral.com/jcnur.
Early View: rapid online publication (with doi for referencing) for accepted articles in final form, and fully citable.
Positive publishing experience: rapid double-blind peer review with constructive feedback.
Online Open: the option to make your article freely and openly accessible to non-subscribers upon publication in Wiley
Online Library, as well as the option to deposit the article in your preferred archive.
Ó 2012 Blackwell Publishing Ltd
Journal of Clinical Nursing, 21, 2149–2159 2159
You might also like
- CreativeWriting12 Q1 Module-1Document28 pagesCreativeWriting12 Q1 Module-1Burning Rose89% (140)
- Project Report in JSWDocument44 pagesProject Report in JSWmohd arif khan73% (15)
- O&S April 2009Document134 pagesO&S April 2009Didi Menendez100% (20)
- HHS Public AccessDocument17 pagesHHS Public AccessChika SabaNo ratings yet
- Grothe Et Al., 2013Document13 pagesGrothe Et Al., 2013mackenzie.lacey28No ratings yet
- 2017 Juliaom - PSC PDFDocument10 pages2017 Juliaom - PSC PDFIka Nur AnnisaNo ratings yet
- Dying Means Suffocating, Perceptions of People Living With COPD Facing End of LifeDocument8 pagesDying Means Suffocating, Perceptions of People Living With COPD Facing End of LifetourfrikiNo ratings yet
- Emotional Distress in Patients With Advanced Heart Failure: ReviewDocument11 pagesEmotional Distress in Patients With Advanced Heart Failure: ReviewCândida MineiroNo ratings yet
- Eilertsen BJRK Kirkevold 2010Document11 pagesEilertsen BJRK Kirkevold 2010Anh HuyNo ratings yet
- Determinants of Costs of Care For Patients With Alzheimer's DiseaseDocument11 pagesDeterminants of Costs of Care For Patients With Alzheimer's DiseaseBenny TjanNo ratings yet
- Fpsyg 14 1281878Document10 pagesFpsyg 14 1281878dr.joneidiNo ratings yet
- Lived Through Past Experienced Present Anticipated Future Understanding Existential Loss in The Context of Life Limiting IllnessDocument16 pagesLived Through Past Experienced Present Anticipated Future Understanding Existential Loss in The Context of Life Limiting Illnessfrancheskaam27No ratings yet
- The Effect of Depression On The Quality 0f Life of Patient With Cervical Cancer at Dr. Moewardi Hospital in SurakartaDocument8 pagesThe Effect of Depression On The Quality 0f Life of Patient With Cervical Cancer at Dr. Moewardi Hospital in SurakartaEndahNo ratings yet
- Applied Nursing Research: Mi-Kyoung Cho, PHD, Apn, Gisoo Shin, PHD, RNDocument7 pagesApplied Nursing Research: Mi-Kyoung Cho, PHD, Apn, Gisoo Shin, PHD, RNJoecoNo ratings yet
- The Bodily Presence of Significant Others Intensive Care Patients Experiences in A Situation of Critical IllnessDocument9 pagesThe Bodily Presence of Significant Others Intensive Care Patients Experiences in A Situation of Critical IllnessSara Daniela Benalcazar JaramilloNo ratings yet
- Cardiovascular Risks Associated With Incident and Prevalent Periodontal DiseaseDocument8 pagesCardiovascular Risks Associated With Incident and Prevalent Periodontal DiseaseAlyaefkageNo ratings yet
- 12 Ustundag Orignial 9 3Document8 pages12 Ustundag Orignial 9 3Sanjivi GovekarNo ratings yet
- Barriers To Effective Pain Management in Sickle Cell DiseaseDocument4 pagesBarriers To Effective Pain Management in Sickle Cell DiseaseDr. Smiley JadonandanNo ratings yet
- Pre-Dialysis Patients ' Perceived Autonomy, Self-Esteem and Labor Participation: Associations With Illness Perceptions and Treatment Perceptions. A Cross-Sectional StudyDocument10 pagesPre-Dialysis Patients ' Perceived Autonomy, Self-Esteem and Labor Participation: Associations With Illness Perceptions and Treatment Perceptions. A Cross-Sectional Studyandrada14No ratings yet
- Land Olt 2011Document13 pagesLand Olt 2011Windy TiandiniNo ratings yet
- A Review of EOLDocument33 pagesA Review of EOLinderaaputraaNo ratings yet
- Critical Reviews in Oncology / HematologyDocument18 pagesCritical Reviews in Oncology / HematologyLiterasi MedsosNo ratings yet
- Samson Et Al - Psychosocial Adaptation To Chronic IllnessDocument13 pagesSamson Et Al - Psychosocial Adaptation To Chronic IllnessRaquel PintoNo ratings yet
- Ten Minutes To Midnight: A Narrative Inquiry of People Living With Dying With Advanced Copd and Their Family MembersDocument11 pagesTen Minutes To Midnight: A Narrative Inquiry of People Living With Dying With Advanced Copd and Their Family MembersCeline WongNo ratings yet
- The Effects of Exercise Standards On The Quality of Life To People With Chronic DiseaseDocument18 pagesThe Effects of Exercise Standards On The Quality of Life To People With Chronic DiseaseMario LanzaNo ratings yet
- Mattsson 2011Document12 pagesMattsson 2011oh yuniNo ratings yet
- Concerns of Patients On Dialysis A Research Study PDFDocument15 pagesConcerns of Patients On Dialysis A Research Study PDFProdi S1- 1BNo ratings yet
- Depressive Symptoms and Dietary Adherence in Patients With End-Stage Renal DiseaseDocument10 pagesDepressive Symptoms and Dietary Adherence in Patients With End-Stage Renal Diseasebasti_aka_slimNo ratings yet
- Nurse and Social Worker Palliative Telecare Team and Quality of Life in Patients With COPD, Heart Failure, or Interstitial Lung DiseaseDocument12 pagesNurse and Social Worker Palliative Telecare Team and Quality of Life in Patients With COPD, Heart Failure, or Interstitial Lung DiseasejunhamanoNo ratings yet
- Personality Change Associated With Chronic Diseases: Pooled Analysis of Four Prospective Cohort StudiesDocument13 pagesPersonality Change Associated With Chronic Diseases: Pooled Analysis of Four Prospective Cohort StudiesDebora BergerNo ratings yet
- End of LifeDocument3 pagesEnd of LifeSiti Fatimahtusz07No ratings yet
- Multiple Sclerosis Lancet 2018Document15 pagesMultiple Sclerosis Lancet 2018Sarah Miryam CoffanoNo ratings yet
- Experiences of Psychological FlowerDocument8 pagesExperiences of Psychological Flowerlsj19950128No ratings yet
- Research Article: Turkish Journal of Psychiatry 2021 32 (4) :246-252Document8 pagesResearch Article: Turkish Journal of Psychiatry 2021 32 (4) :246-252Celine WongNo ratings yet
- Background of The Study and SOP - Quali Research2-1Document3 pagesBackground of The Study and SOP - Quali Research2-1Maricris I. AbuanNo ratings yet
- Ho 2013Document6 pagesHo 2013Vera El Sammah SiagianNo ratings yet
- Mia Pruefer - Health Literacy and Elhers-Danlos Syndrome Hypermobility TypeDocument14 pagesMia Pruefer - Health Literacy and Elhers-Danlos Syndrome Hypermobility TypeMia PrueferNo ratings yet
- Living With Advanced Parkinson's Disease: A Constant Struggle With UnpredictabilityDocument10 pagesLiving With Advanced Parkinson's Disease: A Constant Struggle With UnpredictabilityLorenaNo ratings yet
- ContentServer AspDocument8 pagesContentServer Aspstephanie eduarteNo ratings yet
- Birkefeld (2022)Document14 pagesBirkefeld (2022)Nerea AlvarezNo ratings yet
- 480 253 1057 1 10 20190424 PDFDocument8 pages480 253 1057 1 10 20190424 PDFdwiajaNo ratings yet
- Mazujnms v2n2p29 enDocument7 pagesMazujnms v2n2p29 enDoc RuthNo ratings yet
- Pain Neuroscience Education in Older Adults With Chronic Back and or Lower Extremity PainDocument12 pagesPain Neuroscience Education in Older Adults With Chronic Back and or Lower Extremity PainAriadna BarretoNo ratings yet
- Content ServerDocument4 pagesContent ServerEkaSaktiWahyuningtyasNo ratings yet
- End-Of-Life Care in The Icu: Supporting Nurses To Provide High-Quality CareDocument5 pagesEnd-Of-Life Care in The Icu: Supporting Nurses To Provide High-Quality CareSERGIO ANDRES CESPEDES GUERRERONo ratings yet
- Life Review Therapy For Older Adults With Moderate Depressive Symptomatology: A Pragmatic Randomized Controlled TrialDocument12 pagesLife Review Therapy For Older Adults With Moderate Depressive Symptomatology: A Pragmatic Randomized Controlled TrialAstridNo ratings yet
- PIIS1976131710600059Document11 pagesPIIS1976131710600059Marina UlfaNo ratings yet
- Losely Geriatric Paper 325Document7 pagesLosely Geriatric Paper 325api-532850773No ratings yet
- The Perception of Life and Death in Patients With End-Of-Life Stage Cancer: A Systematic Review of Qualitative ResearchDocument13 pagesThe Perception of Life and Death in Patients With End-Of-Life Stage Cancer: A Systematic Review of Qualitative ResearchPedro TavaresNo ratings yet
- Neurobiology of Resilience in Depression Immune and Vascular InsightDocument78 pagesNeurobiology of Resilience in Depression Immune and Vascular InsightMaria BelénNo ratings yet
- CHF 5Document8 pagesCHF 5Prameswari ZahidaNo ratings yet
- Tan Burden Distress Qol Informal Caregivers Lung CancerDocument11 pagesTan Burden Distress Qol Informal Caregivers Lung CancerRubí Corona TápiaNo ratings yet
- UncertaintyDocument16 pagesUncertaintymaya permata sariNo ratings yet
- Kaptein-Common-Sense Model-OsteoarthritisDocument9 pagesKaptein-Common-Sense Model-OsteoarthritisZyania MelchyNo ratings yet
- Shao2020 PDFDocument7 pagesShao2020 PDFAndrea ZambranoNo ratings yet
- EUTHADocument10 pagesEUTHAJena WoodsNo ratings yet
- Jurnal CKDDocument8 pagesJurnal CKDRatna Dewi CahyaniNo ratings yet
- Clarifying Dementia Risk Factors: Treading in Murky Waters: CommentaryDocument3 pagesClarifying Dementia Risk Factors: Treading in Murky Waters: CommentaryVazia Rahma HandikaNo ratings yet
- Chochinov - Dignity Therapy - A Feasibility Study of EldersDocument13 pagesChochinov - Dignity Therapy - A Feasibility Study of Eldersjuarezcastellar268No ratings yet
- Acarturk Et Al 2016Document11 pagesAcarturk Et Al 2016290971No ratings yet
- Kart Tune N 2010Document10 pagesKart Tune N 2010AndreiaNo ratings yet
- Orofacial Pain: From Basic Science to Clinical Management, Second EditionFrom EverandOrofacial Pain: From Basic Science to Clinical Management, Second EditionNo ratings yet
- Experiences of Adolescents Living with Type 1 Diabetes Mellitus whilst Negotiating with the Society: Submitted as part of the MSc degree in diabetes University of Surrey, Roehampton, 2003From EverandExperiences of Adolescents Living with Type 1 Diabetes Mellitus whilst Negotiating with the Society: Submitted as part of the MSc degree in diabetes University of Surrey, Roehampton, 2003No ratings yet
- RETREAT Framework Et Al. 2018Document12 pagesRETREAT Framework Et Al. 2018happyNo ratings yet
- Hudson 2005Document13 pagesHudson 2005happyNo ratings yet
- Hendrix 2011Document21 pagesHendrix 2011happyNo ratings yet
- ChecklistDocument2 pagesChecklisthappyNo ratings yet
- Hendrix 2006Document6 pagesHendrix 2006happyNo ratings yet
- He Demand 2011Document9 pagesHe Demand 2011happyNo ratings yet
- Davison Et Al 2006Document5 pagesDavison Et Al 2006happyNo ratings yet
- Leadership Joyce 2016Document7 pagesLeadership Joyce 2016happyNo ratings yet
- Big DataDocument20 pagesBig DataBhavnita NareshNo ratings yet
- Essential Kitchen Bathroom Bedroom - September 2014 UKDocument164 pagesEssential Kitchen Bathroom Bedroom - September 2014 UKfishermantoys100% (1)
- Logic Gate Investigatory PDFDocument12 pagesLogic Gate Investigatory PDFGaurang MathurNo ratings yet
- UNICEF's Work in Public Finance For ChildrenDocument2 pagesUNICEF's Work in Public Finance For ChildrenCr CryptoNo ratings yet
- Bibliografía RazaDocument3 pagesBibliografía RazaJorge Vallejo KazacosNo ratings yet
- Plural of NounsDocument1 pagePlural of NounsStrafalogea Serban100% (2)
- 365DayPan DailyEnglishLessonPlanUPDATED2022Document379 pages365DayPan DailyEnglishLessonPlanUPDATED2022KATIUSCA EVELYN GONZALES RIVERANo ratings yet
- Workshop Living in The Czech Republic: WWW - Expatlegal.czDocument22 pagesWorkshop Living in The Czech Republic: WWW - Expatlegal.czImran ShaNo ratings yet
- Brand Engagement With Brand ExpressionDocument27 pagesBrand Engagement With Brand ExpressionArun KCNo ratings yet
- Le Conditionnel Présent: The Conditional PresentDocument8 pagesLe Conditionnel Présent: The Conditional PresentDeepika DevarajNo ratings yet
- Remunerasi RSDocument39 pagesRemunerasi RSalfanNo ratings yet
- Gate Induced Drain Leakage For Ultra Thin MOSFET Devices Using SilvacoDocument2 pagesGate Induced Drain Leakage For Ultra Thin MOSFET Devices Using Silvacosiddhant gangwalNo ratings yet
- NOTICEDocument126 pagesNOTICEowsaf2No ratings yet
- Count and Non-Count Nous (Plural Form of Nous)Document9 pagesCount and Non-Count Nous (Plural Form of Nous)Kathe TafurNo ratings yet
- 11.29.12 Post Standard, The Word Is Out New Law Protects Overdose Victims and HelpersDocument2 pages11.29.12 Post Standard, The Word Is Out New Law Protects Overdose Victims and Helperswebmaster@drugpolicy.orgNo ratings yet
- QTS AplicationDocument8 pagesQTS Aplicationandreuta23No ratings yet
- Reza Sitinjak CJR COLSDocument5 pagesReza Sitinjak CJR COLSReza Enjelika SitinjakNo ratings yet
- Casting High Quality C12A: Bradken Energy ProductsDocument37 pagesCasting High Quality C12A: Bradken Energy Productsdelta lab sangliNo ratings yet
- World War IDocument7 pagesWorld War IhzbetulkunNo ratings yet
- English Test-SMA-Kelas-XII-Semester-IDocument4 pagesEnglish Test-SMA-Kelas-XII-Semester-IAru HernalantoNo ratings yet
- Personality and Work Behaviour Exploring The 1996 PDFDocument18 pagesPersonality and Work Behaviour Exploring The 1996 PDFAtif BasaniNo ratings yet
- EstimationDocument106 pagesEstimationasdasdas asdasdasdsadsasddssa0% (1)
- Final For ReviewDocument39 pagesFinal For ReviewMichay CloradoNo ratings yet
- Catholic Ghost Stories of Western PennsylvaniaDocument5 pagesCatholic Ghost Stories of Western PennsylvaniaeclarexeNo ratings yet
- Marketing Research ProcessDocument3 pagesMarketing Research Processadnan saifNo ratings yet
- Novo Nordisk AR 2011 enDocument116 pagesNovo Nordisk AR 2011 enINVESTORNEWNo ratings yet
- Stanford CS193p Developing Applications For iOS Fall 2013-14Document66 pagesStanford CS193p Developing Applications For iOS Fall 2013-14AbstractSoft100% (1)