Professional Documents
Culture Documents
Quick Reference Guide Endocrine Hypertension 2 2016 Version
Quick Reference Guide Endocrine Hypertension 2 2016 Version
Uploaded by
Parishan SaeedCopyright:
Available Formats
You might also like
- Pa 1 Persuasive EssayDocument4 pagesPa 1 Persuasive Essayapi-458023500No ratings yet
- E773 FullDocument6 pagesE773 FullanhiramdhaniNo ratings yet
- Aldosteronismo PrimarioDocument23 pagesAldosteronismo PrimarioLuisNo ratings yet
- Joim 12831 PDFDocument23 pagesJoim 12831 PDFnurhidayahNo ratings yet
- Hypertensive EmergencyDocument4 pagesHypertensive EmergencyRara MuuztmuuztmuccuNo ratings yet
- Astra End HipDocument47 pagesAstra End HipIlze KonrādeNo ratings yet
- Evaluationandmanagement Ofprimary Hyperaldosteronism: Frances T. Lee,, Dina ElarajDocument15 pagesEvaluationandmanagement Ofprimary Hyperaldosteronism: Frances T. Lee,, Dina ElarajDiego BallesterosNo ratings yet
- Ardhanari 2015Document11 pagesArdhanari 2015Vivi DeviyanaNo ratings yet
- Primary Hyperaldosteronism - StatPearls - NCBI BookshelfDocument7 pagesPrimary Hyperaldosteronism - StatPearls - NCBI BookshelfCecil-An DalanonNo ratings yet
- Manchester Presentation Final 2Document21 pagesManchester Presentation Final 2api-610233914No ratings yet
- Stopp Start ToolkitDocument22 pagesStopp Start ToolkitRifky IlhamiNo ratings yet
- Crisis HipertensivasDocument17 pagesCrisis HipertensivasJuan C. Moreno BarraganNo ratings yet
- Antihypertensive DrugsDocument52 pagesAntihypertensive Drugsapi-224264169No ratings yet
- 1 Dental Management of Patients With Cardiovascular DiseasesDocument14 pages1 Dental Management of Patients With Cardiovascular Diseasesاحمد سلامNo ratings yet
- HypertensionDocument10 pagesHypertensionaa zzNo ratings yet
- HypertensionDocument5 pagesHypertensiongoinggreen91No ratings yet
- Jama Hta ResistenteDocument9 pagesJama Hta ResistenteMayra Alejandra Prada SerranoNo ratings yet
- Diagnosis and Treatment of Primary AldosteronismDocument17 pagesDiagnosis and Treatment of Primary AldosteronismcastillojessNo ratings yet
- Articles: Spironolactone Management of Resistant HypertensionDocument8 pagesArticles: Spironolactone Management of Resistant HypertensionKatherine America Camac DelgadoNo ratings yet
- HTN EmergenciesDocument7 pagesHTN EmergenciesBarry Tumpal Wouter NapitupuluNo ratings yet
- سريرية نظري٢Document12 pagesسريرية نظري٢مصطفى ابراهيم سعيدNo ratings yet
- 5 HypertensionDocument8 pages5 Hypertensioniraqeana100100No ratings yet
- Managing Hyperkalemia Caused by Inhibitors of The Renin-Angiotensin-Aldosterone SystemDocument8 pagesManaging Hyperkalemia Caused by Inhibitors of The Renin-Angiotensin-Aldosterone SystemMedranoReyesLuisinNo ratings yet
- Ferne HTN Emerg Feldstein 2007 PDFDocument5 pagesFerne HTN Emerg Feldstein 2007 PDFridwan020392No ratings yet
- Case StudiesDocument5 pagesCase Studiespragna novaNo ratings yet
- Hypertension Definition:: Nitric OxideDocument5 pagesHypertension Definition:: Nitric OxideAnonymous bbeAZHxZNo ratings yet
- Drug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansDocument0 pagesDrug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansRajihah JihahNo ratings yet
- Flashcards - QuizletDocument7 pagesFlashcards - QuizletNEsreNo ratings yet
- DBP: Diastolic Blood Pressure SBP: Systolic Blood PressureDocument7 pagesDBP: Diastolic Blood Pressure SBP: Systolic Blood PressureM. JoyceNo ratings yet
- Essential Hypertension Review - USMLE Step 2Document26 pagesEssential Hypertension Review - USMLE Step 2Marc Imhotep Cray, M.D.No ratings yet
- Why Hard To Control Blood Pressure ?: Atma GunawanDocument35 pagesWhy Hard To Control Blood Pressure ?: Atma GunawanLies Pramana SariNo ratings yet
- Anesthetic Management in Conn's Syndrome and PheochromocytomaDocument35 pagesAnesthetic Management in Conn's Syndrome and PheochromocytomaShashikant RamNo ratings yet
- Acquired TTP - Clinical Manifestations and Diagnosis - UpToDateDocument16 pagesAcquired TTP - Clinical Manifestations and Diagnosis - UpToDatepradeep danielNo ratings yet
- Hyperkalemia in Heart Failure: The Present and FutureDocument15 pagesHyperkalemia in Heart Failure: The Present and FutureLizette Galvan GalvanNo ratings yet
- High Yield Board ReviewDocument5 pagesHigh Yield Board ReviewMarcoNo ratings yet
- Lec 3Document13 pagesLec 3fbbqbcht6yNo ratings yet
- HypertensionDocument55 pagesHypertensionSr.Jyothy SABSNo ratings yet
- Sodium Disorders AAFP PDFDocument12 pagesSodium Disorders AAFP PDFIvan Tintaya UrureNo ratings yet
- Hypertensiveemergencies PDFDocument7 pagesHypertensiveemergencies PDFGede AdiNo ratings yet
- Drug Induced Hyperuricemia GoutDocument3 pagesDrug Induced Hyperuricemia GoutAnggun Cahya MertyanaNo ratings yet
- Acute Heart FailureDocument24 pagesAcute Heart FailureTeddy MauriceNo ratings yet
- Diagnostic Tests and ProceduresDocument49 pagesDiagnostic Tests and Procedurespmahi8854No ratings yet
- WJH 5 14Document15 pagesWJH 5 14Elena Borş MorariNo ratings yet
- Art 40Document4 pagesArt 40Francesca BertaccaNo ratings yet
- Farmacos de Hta en EmbarazoDocument5 pagesFarmacos de Hta en EmbarazoДжек ХавокNo ratings yet
- Cardiac Medication LectureDocument23 pagesCardiac Medication LectureilikeedsheeranNo ratings yet
- CVS (HF, HTN) PharmacologyDocument99 pagesCVS (HF, HTN) PharmacologyCherenet TomaNo ratings yet
- Hypertension: 1-Hypertension Is Defined As (BP)Document37 pagesHypertension: 1-Hypertension Is Defined As (BP)hussein alnasryNo ratings yet
- Crisis Hipertensiva CHEST 2007 PDFDocument16 pagesCrisis Hipertensiva CHEST 2007 PDFJenny AlexandraNo ratings yet
- Hypertensive CrisisDocument60 pagesHypertensive CrisisDzikrul Haq KarimullahNo ratings yet
- OmapatrilatDocument3 pagesOmapatrilataislineazpeitia23No ratings yet
- Reviews: Novel Therapeutic Targets For HypertensionDocument11 pagesReviews: Novel Therapeutic Targets For HypertensiongpatwallahNo ratings yet
- LAS 4 Drugs For HypertensionDocument28 pagesLAS 4 Drugs For HypertensionMuhammad Haroon RazaNo ratings yet
- Contraindications To Vasoconstrictors in Dentistry: Part IIDocument5 pagesContraindications To Vasoconstrictors in Dentistry: Part IIBunga Erlita RosaliaNo ratings yet
- Hiperkalemia en ERDocument8 pagesHiperkalemia en ERmjbb1310No ratings yet
- Hyperkalemia Management in The Emergency Department: An Expert Panel ConsensusDocument8 pagesHyperkalemia Management in The Emergency Department: An Expert Panel ConsensusDaniel HeSaNo ratings yet
- Critical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsNo ratings yet
- Hypotensive Syndromes in Geriatric PatientsFrom EverandHypotensive Syndromes in Geriatric PatientsKannayiram AlagiakrishnanNo ratings yet
- Secondary Hypertension: Clinical Presentation, Diagnosis, and TreatmentFrom EverandSecondary Hypertension: Clinical Presentation, Diagnosis, and TreatmentGeorge A. MansoorNo ratings yet
- Conn Syndrome, (Hyper-Aldosteronism) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandConn Syndrome, (Hyper-Aldosteronism) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- 976c5091-5277-4d13-8655-371a2eb3d13fDocument2 pages976c5091-5277-4d13-8655-371a2eb3d13fParishan SaeedNo ratings yet
- Bone Age For Chronological Age Determination - November2018Document4 pagesBone Age For Chronological Age Determination - November2018Parishan SaeedNo ratings yet
- 1 s2.0 S0009912017307178 MainDocument23 pages1 s2.0 S0009912017307178 MainParishan SaeedNo ratings yet
- Decreased Ligand Affinity Rather Than Glucocorticoid Receptor Down-Regulation in Patients With Endogenous Cushing's SyndromeDocument5 pagesDecreased Ligand Affinity Rather Than Glucocorticoid Receptor Down-Regulation in Patients With Endogenous Cushing's SyndromeParishan SaeedNo ratings yet
- Effect of Knowledge of Chronologic Age On The Variability of Pediatric Bone Age Determined Using The Greulich and Pyle StandardsDocument7 pagesEffect of Knowledge of Chronologic Age On The Variability of Pediatric Bone Age Determined Using The Greulich and Pyle StandardsParishan SaeedNo ratings yet
- Cortisol II 2020-03 v6Document5 pagesCortisol II 2020-03 v6Parishan SaeedNo ratings yet
- Guidance Statement: Hormone Supplementation For Pubertal Induction in GirlsDocument21 pagesGuidance Statement: Hormone Supplementation For Pubertal Induction in GirlsParishan SaeedNo ratings yet
- Guideline Treatment of T2DM 2020 ESCDocument1 pageGuideline Treatment of T2DM 2020 ESCParishan SaeedNo ratings yet
- Ece Home 2023 Paag DDocument1 pageEce Home 2023 Paag DParishan SaeedNo ratings yet
- See Full Prescribing Information For Complete Boxed WarningDocument43 pagesSee Full Prescribing Information For Complete Boxed WarningParishan SaeedNo ratings yet
- Glp-1 Receptor Agonists (GLP-1 RA) : Presented By: Nermeen S. Esa (Clinical Pharmacist)Document10 pagesGlp-1 Receptor Agonists (GLP-1 RA) : Presented By: Nermeen S. Esa (Clinical Pharmacist)Parishan SaeedNo ratings yet
- COVID-19 Disease SeverityDocument7 pagesCOVID-19 Disease SeverityParishan SaeedNo ratings yet
- Junior Grade 9 Junior Grade 9Document2 pagesJunior Grade 9 Junior Grade 9Mark Joseph Nepomuceno CometaNo ratings yet
- Neonatal Meningitis: Designed By: Dr. Esraa AlnabilsyDocument19 pagesNeonatal Meningitis: Designed By: Dr. Esraa AlnabilsyAli FalihNo ratings yet
- List of Basic Essential Medicines Ministry of Health Seychelles 2010Document14 pagesList of Basic Essential Medicines Ministry of Health Seychelles 2010portosinNo ratings yet
- Neurology Clerkship UWORLD: Brain TumoursDocument13 pagesNeurology Clerkship UWORLD: Brain TumoursHaadi AliNo ratings yet
- Drugs Influencing Internal Organs Part2Document92 pagesDrugs Influencing Internal Organs Part2Jemi LoriNo ratings yet
- 4 Sitagliptin (Raysiglip)Document200 pages4 Sitagliptin (Raysiglip)Thet Su LwinNo ratings yet
- Polycythemia VeraDocument33 pagesPolycythemia VeramesseeeNo ratings yet
- Loresca - Ratio Mtle - HistopathDocument10 pagesLoresca - Ratio Mtle - HistopathKaycee Gretz LorescaNo ratings yet
- Kawasaki Disease-NcpDocument5 pagesKawasaki Disease-NcpBelen SoleroNo ratings yet
- Muthu HT ReportDocument87 pagesMuthu HT ReportSridharan DNo ratings yet
- Cerebrospinal Fluid - AUBFDocument9 pagesCerebrospinal Fluid - AUBFMitch IbayNo ratings yet
- Medical Diseases in PregnancyDocument37 pagesMedical Diseases in PregnancyAsteway MesfinNo ratings yet
- FMGE JUNE-2109 Questions: AriseDocument20 pagesFMGE JUNE-2109 Questions: AriseSugithaTamilarasanNo ratings yet
- 5 6280832050500993149Document77 pages5 6280832050500993149Nitish AggarwalNo ratings yet
- Clinical Insights: Dr. Wathik M. Thijar MBBCH, Febm, Mrcp-Uk Lecturer of Internal MedicineDocument20 pagesClinical Insights: Dr. Wathik M. Thijar MBBCH, Febm, Mrcp-Uk Lecturer of Internal MedicineYousif AlaaNo ratings yet
- Pancreatic Ductal Adenocarcinoma and Its Variants: Pearls and PerilsDocument20 pagesPancreatic Ductal Adenocarcinoma and Its Variants: Pearls and PerilsGeorge MogaNo ratings yet
- Kode Pintar Icd 10Document60 pagesKode Pintar Icd 10Nur LailaNo ratings yet
- CLIN CHEM: Nonprotein Nitrogen Compounds (NPN) : Topic Outline Urea Uric AcidDocument7 pagesCLIN CHEM: Nonprotein Nitrogen Compounds (NPN) : Topic Outline Urea Uric AcidJezzah Mae CañeteNo ratings yet
- Abnormal PsychologyDocument136 pagesAbnormal PsychologyMary Ye Ariola Magsino100% (3)
- NCM 112 E LEARNING AutosavedDocument7 pagesNCM 112 E LEARNING AutosavedMikko McDonie VeloriaNo ratings yet
- Manual Urinalysis: Lynne PowellDocument37 pagesManual Urinalysis: Lynne PowellAdhya TiaraNo ratings yet
- Anatomy of Human EyeDocument41 pagesAnatomy of Human EyeCarly MelachioNo ratings yet
- Immuno-Serology: Antistreptolysin 0Document13 pagesImmuno-Serology: Antistreptolysin 0Romie SolacitoNo ratings yet
- BLOCK II LMS Quiz AnatomyDocument27 pagesBLOCK II LMS Quiz AnatomyAshley BuchananNo ratings yet
- High Yield Psychiatry: Shelf Exam Review Emma Holliday RamahiDocument71 pagesHigh Yield Psychiatry: Shelf Exam Review Emma Holliday RamahisamNo ratings yet
- Background of The StudyDocument7 pagesBackground of The StudyVern LeStrangeNo ratings yet
- Study Guid Patho 1Document41 pagesStudy Guid Patho 1sturner7887No ratings yet
- Alzheimer Disease EngDocument35 pagesAlzheimer Disease EngAna IantucNo ratings yet
- Basic Brain AnatomyDocument36 pagesBasic Brain Anatomymartha wibawaNo ratings yet
Quick Reference Guide Endocrine Hypertension 2 2016 Version
Quick Reference Guide Endocrine Hypertension 2 2016 Version
Uploaded by
Parishan SaeedOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Quick Reference Guide Endocrine Hypertension 2 2016 Version
Quick Reference Guide Endocrine Hypertension 2 2016 Version
Uploaded by
Parishan SaeedCopyright:
Available Formats
Quick Reference for Residents:
Endocrine Hypertension
Soe Naing, MD, MRCP(UK), FACE
Endocrinologist
Associate Clinical Professor of Medicine
Director of Division of Endocrinology
Medical Director of Community Diabetes Care Center
UCSF-Fresno Medical Education Program
Version: SN/2-10-2016
SN/VERSION 02-10-2016 Page 1
SUMMARY AND RECOMMENDATIONS:
Evaluation: From “Endocrine HTN” available at http://www.endotext.org/
Endocrine Hypertension accounts for about 3% of the secondary forms of hypertension and is a term
assigned to states in which hormonal derangements result in clinically significant hypertension. The most
common causes of endocrine hypertension are
1. primary hyperaldosteronism,
2. pheochromocytoma, and
3. Cushing’s syndrome.
Hypertension in young patients and refractory hypertension should alert the physician to screen for
secondary causes. The first step when evaluating a patient with suspected endocrine-related hypertension
is to exclude other causes of secondary hypertension.
SN/VERSION 02-10-2016 Page 2
1. Primary Hyperaldosteronism
• Primary aldosteronism (hyperaldosteronism) causes hypertension by an inappropriately high
aldosterone secretion that does not suppress adequately with sodium loading. Primary
aldosteronism is believed to account for 8% of all cases of hypertension and 20% of cases of
resistant hypertension. It should also be suspected with early-onset hypertension or stroke before
age 50 years (or both). It may be difficult to distinguish primary aldosteronism from cases of low
renin essential hypertension, with which it may overlap. Patients of all ages may be affected, but
the peak incidence is between 30 years and 60 years. Excessive aldosterone production increases
sodium retention and suppresses plasma renin. It increases renal potassium excretion, which can
lead to hypokalemia. Cardiovascular events are more prevalent in patients with aldosteronism
(35%) than in those with essential hypertension (11%). Primary aldosteronism may be caused by
an aldosterone-producing adrenal adenoma (Conn syndrome), 40% of which have been found to
have somatic mutations in a gene involved with the potassium channel. Primary aldosteronism is
also commonly caused by unilateral or bilateral adrenal hyperplasia. (from Current Medical Diagnosis &
Treatment 2016)
• This should be suspected in any patient with the triad of:
1. HTN
2. unexplained hypokalemia and
3. metabolic alkalosis.
• The most common subtypes are:
1. Aldosterone-producing adenoma (Conn’s) (APA)
2. idiopathic hyperaldosteronism (IHA)/Bilateral adrenal hyperplasia/ Bilateral micronodular
hyperplasia
• The screening test of choice is “plasma aldosterone to renin ratio or PAC/PRA ratio”.
• Protocol: (please refer to “up-to-date” under the session of "Approach to the patient with hypertension and hypokalemia" for detail)
The test is performed by measuring a morning (preferably 8 AM), ambulatory, paired,
random plasma aldosterone concentration (PAC) and plasma renin activity (PRA) or
plasma renin concentration (PRC). In general, PRA and PRC are undetectable in patients
with primary aldosteronism. In most patients with primary aldosteronism, the PAC is >15
ng/dL; the net effect is a PAC/PRA ratio greater than 20.(Some use a cutoff criteria of 30).
Most antihypertensive medications can be continued and posture stimulation is not
required.
Spironolactone and eplerenone should not be initiated until the evaluation is completed
since these can cause an elevation in PRA. The patients already receiving spironolactone,
therapy should be discontinued for at least six weeks. Other potassium-sparing diuretics,
such as amiloride and triamterene, usually do not interfere with testing unless the patient is
on high doses.
Angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs),
and direct renin inhibitors can falsely lower PAC/PRA ratio, and therefore the test should be
repeated at least 4 weeks after stopping these medications if there is a strong clinical
suspicion of hyperaldosteronism.
SN/VERSION 02-10-2016 Page 3
Table: Effects of Antihypertensive Drugs on the Aldosterone-Renin-Ratio (ARR)
Drug Effect on Renin Effect on Aldosterone Net Effect on ARR
β Blockers ↓ ↑ ↑
α1 Blockers → → →
α2 Sympathomimetics → → →
ACE inhibitors ↑ ↓ ↓
AT1R blockers ↑ ↓ ↓
Calcium antagonists → → →
Diuretics (↑) (↑) →/(↓)
Abbreviations: ACE, angiotensin-converting enzyme; AT1R, angiotensin II receptor type 1.
From Harrison's Principles of Internal Medicine, 19e
SN/VERSION 02-10-2016 Page 4
Treatment
Conn syndrome (unilateral aldosterone-secreting adrenal adenoma) is usually treated by laparoscopic
adrenalectomy, although long-term medical therapy is an option. Bilateral adrenal hyperplasia is best
treated with medical therapy. Medical treatment must include a potassium-sparing diuretic,
particularly spironolactone, eplerenone, or amiloride. Spironolactone also has antiandrogen activity and
men frequently experience breast tenderness, gynecomastia, or reduced libido; it is given at initial doses
of 12.5–25 mg orally once daily; the dose may be titrated upward to 200 mg daily. Spironolactone is
contraindicated in pregnancy and reproductive-age women are cautioned to use contraception during
therapy. Eplerenone is becoming favored for men, since it does not have antiandrogen effects; however, it
has a short half-life and must be taken orally twice daily in doses of 25–50 mg. Another option is amiloride,
which is effective in doses of 10–20 mg/day and is the preferred medication for hyperaldosteronism during
pregnancy. Blood pressure must be monitored daily when beginning these anti-mineralocorticoid
medications; significant drops in blood pressure have occurred when these drugs are added to other
antihypertensives. Other antihypertensive drugs may be required, particularly amlodipine, and ACE
inhibitors or ARBs. (from Current Medical Diagnosis & Treatment 2016)
SN/VERSION 02-10-2016 Page 5
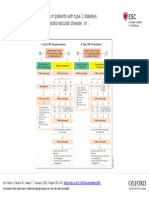
Overview of management of patients with suspected mineralocorticoid excess.
From Harrison's Principles of Internal Medicine, 19e
SN/VERSION 02-10-2016 Page 6
2. Pheochromocytoma
Pheochromocytomas and paragangliomas are catecholamine-producing tumors derived from the
sympathetic or parasympathetic nervous system. These tumors may arise sporadically or be inherited
as features of multiple endocrine neoplasia type 2, von Hippel–Lindau disease, or several other
pheochromocytoma-associated syndromes. The diagnosis of pheochromocytomas identifies a
potentially correctable cause of hypertension, and their removal can prevent hypertensive crises that
can be lethal. The clinical presentation is variable, ranging from an adrenal incidentaloma to a
hypertensive crisis with associated cerebrovascular or cardiac complications.
Pheochromocytoma is estimated to occur in 2–8 of 1 million persons per year, and ∼0.1% of
hypertensive patients harbor a pheochromocytoma. The mean age at diagnosis is ∼40 years, although
the tumors can occur from early childhood until late in life. The classic “rule of tens” for
pheochromocytomas states that ∼10% are bilateral, 10% are extra-adrenal, and 10% are malignant.
Its clinical presentation is so variable that pheochromocytoma has been termed “the great
masquerader”.
Table: Clinical Features Associated with Pheochromocytoma,
Listed by Frequency of Occurrence
1. Headaches 10. Weight loss
2. Profuse sweating 11. Paradoxical response to antihypertensive drugs
3. Palpitations and tachycardia 12. Polyuria and polydipsia
4. Hypertension, sustained or paroxysmal 13. Constipation
5. Anxiety and panic attacks 14. Orthostatic hypotension
6. Pallor 15. Dilated cardiomyopathy
7. Nausea 16. Erythrocytosis
8. Abdominal pain 17. Elevated blood sugar
9. Weakness 18. Hypercalcemia
From Harrison's Principles of Internal Medicine, 19e
This should be suspected in any patient with the triad of:
1. headache,
2. sweating and
3. tachycardia
SN/VERSION 02-10-2016 Page 7
Diagnosis of Pheochromocytoma and Paraganglioma
The screening test of choice is “24-hour urine fractionated catecholamines and metanephrines
and/or plasma fractionated metanephrines”.
Table: Biochemical and Imaging Methods Used for Diagnosis of Pheochromocytoma and Paraganglioma
Diagnostic Method Sensitivity Specificity
24-h urinary tests
Catecholamines +++ +++
Fractionated metanephrines ++++ ++
Total metanephrines +++ ++++
Plasma tests
Catecholamines +++ ++
Free metanephrines ++++ +++
Imaging
CT ++++ +++
MRI ++++ +++
MIBG scintigraphy +++ ++++
Somatostatin receptor scintigraphya ++ ++
Fluoro-DOPA PET/CT
18
+++ ++++
aValues are particularly high in head and neck paragangliomas.
Abbreviations:
MIBG, metaiodobenzylguanidine; PET/CT, positron emission tomography plus CT. For the biochemical tests, the
ratings correspond globally to sensitivity and specificity rates as follows: ++, <85%; +++, 85–
95%; and ++++, >95%.
From Harrison's Principles of Internal Medicine, 19e: Pheochromocytoma
SN/VERSION 02-10-2016 Page 8
SN/VERSION 02-10-2016 Page 9
PHEOCHROMOCYTOMA-ASSOCIATED SYNDROMES
From Harrison's Principles of Internal Medicine, 19e: Pheochromocytoma
About 25–33% of patients with a pheochromocytoma or paraganglioma have an inherited syndrome. At
diagnosis, patients with inherited syndromes are a mean of ∼15 years younger than patients with sporadic
tumors.
Neurofibromatosis type 1 (NF1) was the first described pheochromocytoma-associated syndrome.
The NF1 gene functions as a tumor suppressor by regulating the Ras signaling cascade. Classic features
of neurofibromatosis include multiple neurofibromas, café au lait spots, axillary freckling of the skin, and
Lisch nodules of the iris. Pheochromocytomas occur in only ∼1% of these patients and are located
predominantly in the adrenals. Malignant pheochromocytoma is not uncommon.
Neurofibromatosis. A. MRI of bilateral adrenal pheochromocytoma. B. Cutaneous neurofibromas. C. Lisch
nodules of the iris. D. Axillary freckling.
The best-known pheochromocytoma-associated syndrome is the autosomal dominant disorder multiple
endocrine neoplasia type 2 (MEN2) . Both types of MEN2 (2A and 2B) are caused by mutations
in RET (rearranged during transfection), which encodes a tyrosine kinase. The locations of RET mutations
correlate with the severity of disease and the type of MEN2. MEN2A is characterized by medullary thyroid
carcinoma (MTC), pheochromocytoma, and hyperparathyroidism; MEN2B also includes MTC and
pheochromocytoma as well as multiple mucosal neuromas, marfanoid habitus, and other developmental
disorders, though it typically lacks hyperparathyroidism. MTC is found in virtually all patients with MEN2,
but pheochromocytoma occurs in only ∼50% of these patients. Nearly all pheochromocytomas in MEN2
are benign and located in the adrenals, often bilaterally. Pheochromocytoma may be symptomatic before
MTC. Prophylactic thyroidectomy is being performed in many carriers of RET mutations;
pheochromocytomas should be excluded before any surgery in these patients.
SN/VERSION 02-10-2016 Page 10
Von Hippel–Lindau syndrome (VHL) is an autosomal dominant disorder that predisposes to retinal and
cerebellar hemangioblastomas, which also occur in the brainstem and spinal cord. Other important
features of VHL are clear cell renal carcinomas, pancreatic neuroendocrine tumors, endolymphatic sac
tumors of the inner ear, cystadenomas of the epididymis and broad ligament, and multiple pancreatic or
renal cysts.
Other syndromes are the paraganglioma syndromes (PGLs) and familial pheochromocytoma (FP).
Von Hippel–Lindau disease. A. Retinal angioma. All subsequent panels show findings on MRI: B–
D. Hemangioblastomas of the cerebellum (B) in brainstem (C) and spinal cord (D). E. Bilateral
pheochromocytomas and bilateral renal clear cell carcinomas F. Multiple pancreatic cysts.
SN/VERSION 02-10-2016 Page 11
3. Cushing’s syndrome
From up-to-date and Harrison's Principles of Internal Medicine, 19e
Cushing’s syndrome reflects a constellation of clinical features that result from chronic exposure to
excess glucocorticoids of any etiology. The disorder can be ACTH-dependent (e.g., pituitary
corticotrope adenoma) or ACTH-independent (e.g., adrenocortical adenoma), as well as iatrogenic
(e.g., administration of exogenous glucocorticoids). The term Cushing’s disease refers specifically
to Cushing’s syndrome caused by a pituitary corticotrope adenoma.
Cushing’s syndrome is generally considered a rare disease. It occurs with an incidence of 1–2 per
100,000 population per year. In the overwhelming majority of patients, Cushing’s syndrome is
caused by an ACTH-producing corticotrope adenoma of the pituitary.
This should be suspected in any patient with
1. supraclavicular fat pads,
2. easy bruising/ skin atrophy,
3. wide purplish abdominal striae, and
4. proximal muscle weakness.
The 3 screening tests to establish the diagnosis of Cushing's syndrome or hypercortisolism:
1. 24-hour urinary cortisol,
2. late night salivary cortisol, and
3. low-dose dexamethasone suppression tests.
The tests to establish the cause of Cushing's syndrome:
1. Plasma ACTH concentrations
2. High-dose dexamethasone suppression tests
3. CRH (corticotropin-releasing hormone) stimulation test
4. Petrosal venous sinus catheterization.
SN/VERSION 02-10-2016 Page 12
SN/VERSION 02-10-2016 Page 13
Typical findings in Cushing syndrome. (from Current Medical Diagnosis & Treatment 2016)
Clinical features of Cushing’s syndrome. (From Harrison's Principles of Internal Medicine, 19e)
A. Note central obesity and broad, purple stretch marks (B. close-up). C. Note thin and brittle skin in an elderly patient with
Cushing’s syndrome. D. Hyperpigmentation of the knuckles in a patient with ectopic adrenocorticotropic hormone (ACTH) excess.
SN/VERSION 02-10-2016 Page 14
SN/VERSION 02-10-2016 Page 15
>1.8 mcg/dL
>1.8 mcg/dL
SN/VERSION 02-10-2016 Page 16
You might also like
- Pa 1 Persuasive EssayDocument4 pagesPa 1 Persuasive Essayapi-458023500No ratings yet
- E773 FullDocument6 pagesE773 FullanhiramdhaniNo ratings yet
- Aldosteronismo PrimarioDocument23 pagesAldosteronismo PrimarioLuisNo ratings yet
- Joim 12831 PDFDocument23 pagesJoim 12831 PDFnurhidayahNo ratings yet
- Hypertensive EmergencyDocument4 pagesHypertensive EmergencyRara MuuztmuuztmuccuNo ratings yet
- Astra End HipDocument47 pagesAstra End HipIlze KonrādeNo ratings yet
- Evaluationandmanagement Ofprimary Hyperaldosteronism: Frances T. Lee,, Dina ElarajDocument15 pagesEvaluationandmanagement Ofprimary Hyperaldosteronism: Frances T. Lee,, Dina ElarajDiego BallesterosNo ratings yet
- Ardhanari 2015Document11 pagesArdhanari 2015Vivi DeviyanaNo ratings yet
- Primary Hyperaldosteronism - StatPearls - NCBI BookshelfDocument7 pagesPrimary Hyperaldosteronism - StatPearls - NCBI BookshelfCecil-An DalanonNo ratings yet
- Manchester Presentation Final 2Document21 pagesManchester Presentation Final 2api-610233914No ratings yet
- Stopp Start ToolkitDocument22 pagesStopp Start ToolkitRifky IlhamiNo ratings yet
- Crisis HipertensivasDocument17 pagesCrisis HipertensivasJuan C. Moreno BarraganNo ratings yet
- Antihypertensive DrugsDocument52 pagesAntihypertensive Drugsapi-224264169No ratings yet
- 1 Dental Management of Patients With Cardiovascular DiseasesDocument14 pages1 Dental Management of Patients With Cardiovascular Diseasesاحمد سلامNo ratings yet
- HypertensionDocument10 pagesHypertensionaa zzNo ratings yet
- HypertensionDocument5 pagesHypertensiongoinggreen91No ratings yet
- Jama Hta ResistenteDocument9 pagesJama Hta ResistenteMayra Alejandra Prada SerranoNo ratings yet
- Diagnosis and Treatment of Primary AldosteronismDocument17 pagesDiagnosis and Treatment of Primary AldosteronismcastillojessNo ratings yet
- Articles: Spironolactone Management of Resistant HypertensionDocument8 pagesArticles: Spironolactone Management of Resistant HypertensionKatherine America Camac DelgadoNo ratings yet
- HTN EmergenciesDocument7 pagesHTN EmergenciesBarry Tumpal Wouter NapitupuluNo ratings yet
- سريرية نظري٢Document12 pagesسريرية نظري٢مصطفى ابراهيم سعيدNo ratings yet
- 5 HypertensionDocument8 pages5 Hypertensioniraqeana100100No ratings yet
- Managing Hyperkalemia Caused by Inhibitors of The Renin-Angiotensin-Aldosterone SystemDocument8 pagesManaging Hyperkalemia Caused by Inhibitors of The Renin-Angiotensin-Aldosterone SystemMedranoReyesLuisinNo ratings yet
- Ferne HTN Emerg Feldstein 2007 PDFDocument5 pagesFerne HTN Emerg Feldstein 2007 PDFridwan020392No ratings yet
- Case StudiesDocument5 pagesCase Studiespragna novaNo ratings yet
- Hypertension Definition:: Nitric OxideDocument5 pagesHypertension Definition:: Nitric OxideAnonymous bbeAZHxZNo ratings yet
- Drug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansDocument0 pagesDrug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansRajihah JihahNo ratings yet
- Flashcards - QuizletDocument7 pagesFlashcards - QuizletNEsreNo ratings yet
- DBP: Diastolic Blood Pressure SBP: Systolic Blood PressureDocument7 pagesDBP: Diastolic Blood Pressure SBP: Systolic Blood PressureM. JoyceNo ratings yet
- Essential Hypertension Review - USMLE Step 2Document26 pagesEssential Hypertension Review - USMLE Step 2Marc Imhotep Cray, M.D.No ratings yet
- Why Hard To Control Blood Pressure ?: Atma GunawanDocument35 pagesWhy Hard To Control Blood Pressure ?: Atma GunawanLies Pramana SariNo ratings yet
- Anesthetic Management in Conn's Syndrome and PheochromocytomaDocument35 pagesAnesthetic Management in Conn's Syndrome and PheochromocytomaShashikant RamNo ratings yet
- Acquired TTP - Clinical Manifestations and Diagnosis - UpToDateDocument16 pagesAcquired TTP - Clinical Manifestations and Diagnosis - UpToDatepradeep danielNo ratings yet
- Hyperkalemia in Heart Failure: The Present and FutureDocument15 pagesHyperkalemia in Heart Failure: The Present and FutureLizette Galvan GalvanNo ratings yet
- High Yield Board ReviewDocument5 pagesHigh Yield Board ReviewMarcoNo ratings yet
- Lec 3Document13 pagesLec 3fbbqbcht6yNo ratings yet
- HypertensionDocument55 pagesHypertensionSr.Jyothy SABSNo ratings yet
- Sodium Disorders AAFP PDFDocument12 pagesSodium Disorders AAFP PDFIvan Tintaya UrureNo ratings yet
- Hypertensiveemergencies PDFDocument7 pagesHypertensiveemergencies PDFGede AdiNo ratings yet
- Drug Induced Hyperuricemia GoutDocument3 pagesDrug Induced Hyperuricemia GoutAnggun Cahya MertyanaNo ratings yet
- Acute Heart FailureDocument24 pagesAcute Heart FailureTeddy MauriceNo ratings yet
- Diagnostic Tests and ProceduresDocument49 pagesDiagnostic Tests and Procedurespmahi8854No ratings yet
- WJH 5 14Document15 pagesWJH 5 14Elena Borş MorariNo ratings yet
- Art 40Document4 pagesArt 40Francesca BertaccaNo ratings yet
- Farmacos de Hta en EmbarazoDocument5 pagesFarmacos de Hta en EmbarazoДжек ХавокNo ratings yet
- Cardiac Medication LectureDocument23 pagesCardiac Medication LectureilikeedsheeranNo ratings yet
- CVS (HF, HTN) PharmacologyDocument99 pagesCVS (HF, HTN) PharmacologyCherenet TomaNo ratings yet
- Hypertension: 1-Hypertension Is Defined As (BP)Document37 pagesHypertension: 1-Hypertension Is Defined As (BP)hussein alnasryNo ratings yet
- Crisis Hipertensiva CHEST 2007 PDFDocument16 pagesCrisis Hipertensiva CHEST 2007 PDFJenny AlexandraNo ratings yet
- Hypertensive CrisisDocument60 pagesHypertensive CrisisDzikrul Haq KarimullahNo ratings yet
- OmapatrilatDocument3 pagesOmapatrilataislineazpeitia23No ratings yet
- Reviews: Novel Therapeutic Targets For HypertensionDocument11 pagesReviews: Novel Therapeutic Targets For HypertensiongpatwallahNo ratings yet
- LAS 4 Drugs For HypertensionDocument28 pagesLAS 4 Drugs For HypertensionMuhammad Haroon RazaNo ratings yet
- Contraindications To Vasoconstrictors in Dentistry: Part IIDocument5 pagesContraindications To Vasoconstrictors in Dentistry: Part IIBunga Erlita RosaliaNo ratings yet
- Hiperkalemia en ERDocument8 pagesHiperkalemia en ERmjbb1310No ratings yet
- Hyperkalemia Management in The Emergency Department: An Expert Panel ConsensusDocument8 pagesHyperkalemia Management in The Emergency Department: An Expert Panel ConsensusDaniel HeSaNo ratings yet
- Critical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsFrom EverandCritical Care Medications: Vasopressors, Inotropes and Anti-Hypertensives Study Guide: Critical Care EssentialsNo ratings yet
- Hypotensive Syndromes in Geriatric PatientsFrom EverandHypotensive Syndromes in Geriatric PatientsKannayiram AlagiakrishnanNo ratings yet
- Secondary Hypertension: Clinical Presentation, Diagnosis, and TreatmentFrom EverandSecondary Hypertension: Clinical Presentation, Diagnosis, and TreatmentGeorge A. MansoorNo ratings yet
- Conn Syndrome, (Hyper-Aldosteronism) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandConn Syndrome, (Hyper-Aldosteronism) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- 976c5091-5277-4d13-8655-371a2eb3d13fDocument2 pages976c5091-5277-4d13-8655-371a2eb3d13fParishan SaeedNo ratings yet
- Bone Age For Chronological Age Determination - November2018Document4 pagesBone Age For Chronological Age Determination - November2018Parishan SaeedNo ratings yet
- 1 s2.0 S0009912017307178 MainDocument23 pages1 s2.0 S0009912017307178 MainParishan SaeedNo ratings yet
- Decreased Ligand Affinity Rather Than Glucocorticoid Receptor Down-Regulation in Patients With Endogenous Cushing's SyndromeDocument5 pagesDecreased Ligand Affinity Rather Than Glucocorticoid Receptor Down-Regulation in Patients With Endogenous Cushing's SyndromeParishan SaeedNo ratings yet
- Effect of Knowledge of Chronologic Age On The Variability of Pediatric Bone Age Determined Using The Greulich and Pyle StandardsDocument7 pagesEffect of Knowledge of Chronologic Age On The Variability of Pediatric Bone Age Determined Using The Greulich and Pyle StandardsParishan SaeedNo ratings yet
- Cortisol II 2020-03 v6Document5 pagesCortisol II 2020-03 v6Parishan SaeedNo ratings yet
- Guidance Statement: Hormone Supplementation For Pubertal Induction in GirlsDocument21 pagesGuidance Statement: Hormone Supplementation For Pubertal Induction in GirlsParishan SaeedNo ratings yet
- Guideline Treatment of T2DM 2020 ESCDocument1 pageGuideline Treatment of T2DM 2020 ESCParishan SaeedNo ratings yet
- Ece Home 2023 Paag DDocument1 pageEce Home 2023 Paag DParishan SaeedNo ratings yet
- See Full Prescribing Information For Complete Boxed WarningDocument43 pagesSee Full Prescribing Information For Complete Boxed WarningParishan SaeedNo ratings yet
- Glp-1 Receptor Agonists (GLP-1 RA) : Presented By: Nermeen S. Esa (Clinical Pharmacist)Document10 pagesGlp-1 Receptor Agonists (GLP-1 RA) : Presented By: Nermeen S. Esa (Clinical Pharmacist)Parishan SaeedNo ratings yet
- COVID-19 Disease SeverityDocument7 pagesCOVID-19 Disease SeverityParishan SaeedNo ratings yet
- Junior Grade 9 Junior Grade 9Document2 pagesJunior Grade 9 Junior Grade 9Mark Joseph Nepomuceno CometaNo ratings yet
- Neonatal Meningitis: Designed By: Dr. Esraa AlnabilsyDocument19 pagesNeonatal Meningitis: Designed By: Dr. Esraa AlnabilsyAli FalihNo ratings yet
- List of Basic Essential Medicines Ministry of Health Seychelles 2010Document14 pagesList of Basic Essential Medicines Ministry of Health Seychelles 2010portosinNo ratings yet
- Neurology Clerkship UWORLD: Brain TumoursDocument13 pagesNeurology Clerkship UWORLD: Brain TumoursHaadi AliNo ratings yet
- Drugs Influencing Internal Organs Part2Document92 pagesDrugs Influencing Internal Organs Part2Jemi LoriNo ratings yet
- 4 Sitagliptin (Raysiglip)Document200 pages4 Sitagliptin (Raysiglip)Thet Su LwinNo ratings yet
- Polycythemia VeraDocument33 pagesPolycythemia VeramesseeeNo ratings yet
- Loresca - Ratio Mtle - HistopathDocument10 pagesLoresca - Ratio Mtle - HistopathKaycee Gretz LorescaNo ratings yet
- Kawasaki Disease-NcpDocument5 pagesKawasaki Disease-NcpBelen SoleroNo ratings yet
- Muthu HT ReportDocument87 pagesMuthu HT ReportSridharan DNo ratings yet
- Cerebrospinal Fluid - AUBFDocument9 pagesCerebrospinal Fluid - AUBFMitch IbayNo ratings yet
- Medical Diseases in PregnancyDocument37 pagesMedical Diseases in PregnancyAsteway MesfinNo ratings yet
- FMGE JUNE-2109 Questions: AriseDocument20 pagesFMGE JUNE-2109 Questions: AriseSugithaTamilarasanNo ratings yet
- 5 6280832050500993149Document77 pages5 6280832050500993149Nitish AggarwalNo ratings yet
- Clinical Insights: Dr. Wathik M. Thijar MBBCH, Febm, Mrcp-Uk Lecturer of Internal MedicineDocument20 pagesClinical Insights: Dr. Wathik M. Thijar MBBCH, Febm, Mrcp-Uk Lecturer of Internal MedicineYousif AlaaNo ratings yet
- Pancreatic Ductal Adenocarcinoma and Its Variants: Pearls and PerilsDocument20 pagesPancreatic Ductal Adenocarcinoma and Its Variants: Pearls and PerilsGeorge MogaNo ratings yet
- Kode Pintar Icd 10Document60 pagesKode Pintar Icd 10Nur LailaNo ratings yet
- CLIN CHEM: Nonprotein Nitrogen Compounds (NPN) : Topic Outline Urea Uric AcidDocument7 pagesCLIN CHEM: Nonprotein Nitrogen Compounds (NPN) : Topic Outline Urea Uric AcidJezzah Mae CañeteNo ratings yet
- Abnormal PsychologyDocument136 pagesAbnormal PsychologyMary Ye Ariola Magsino100% (3)
- NCM 112 E LEARNING AutosavedDocument7 pagesNCM 112 E LEARNING AutosavedMikko McDonie VeloriaNo ratings yet
- Manual Urinalysis: Lynne PowellDocument37 pagesManual Urinalysis: Lynne PowellAdhya TiaraNo ratings yet
- Anatomy of Human EyeDocument41 pagesAnatomy of Human EyeCarly MelachioNo ratings yet
- Immuno-Serology: Antistreptolysin 0Document13 pagesImmuno-Serology: Antistreptolysin 0Romie SolacitoNo ratings yet
- BLOCK II LMS Quiz AnatomyDocument27 pagesBLOCK II LMS Quiz AnatomyAshley BuchananNo ratings yet
- High Yield Psychiatry: Shelf Exam Review Emma Holliday RamahiDocument71 pagesHigh Yield Psychiatry: Shelf Exam Review Emma Holliday RamahisamNo ratings yet
- Background of The StudyDocument7 pagesBackground of The StudyVern LeStrangeNo ratings yet
- Study Guid Patho 1Document41 pagesStudy Guid Patho 1sturner7887No ratings yet
- Alzheimer Disease EngDocument35 pagesAlzheimer Disease EngAna IantucNo ratings yet
- Basic Brain AnatomyDocument36 pagesBasic Brain Anatomymartha wibawaNo ratings yet