Professional Documents
Culture Documents
Annals of Clinical Case Reports: Hemolytic Anemia - A Rare Case Report
Annals of Clinical Case Reports: Hemolytic Anemia - A Rare Case Report
Uploaded by
Dumindu PereraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Annals of Clinical Case Reports: Hemolytic Anemia - A Rare Case Report
Annals of Clinical Case Reports: Hemolytic Anemia - A Rare Case Report
Uploaded by
Dumindu PereraCopyright:
Available Formats
Annals of Clinical Case Reports Case Report
Published: 04 Aug, 2020
Mycoplasma pneumoniae Induced Warm Autoimmune
Hemolytic Anemia – A Rare Case Report
Chew WH1*, Zainal Adlishah ZA1, Fann RJ1, Mohamad AZ2, Ong TC2 and Jameela2
1
Department of Internal Medicine, Hospital Canselor Tuanku Muhriz, Malaysia
2
Department of Hematology, Ampang Hospital, Malaysia
Abstract
Mycoplasma infection is commonly associated with subclinical hemolysis. We report a case of
Mycoplasma infection in a 15 year-old young lady who had severe anemia with hemoglobin level of
2.4 on presentations. There was clinical and radiological evidence of pneumonia, as well as elevated
Mycoplasma antibody titer. Peripheral blood film was suggestive of AIHA with active hemolysis and
Coombs test was strongly positive (4+) for IgG and C3d suggestive of warm AIHA. She was treated
with oral Azithromycin, IV methylprednisolone, IV immunoglobulin and blood transfusion. She
was discharged with oral prednisolone and showed a favorable recovery on blood count on follow
up.
Introduction
Mycoplasma pneumoniae is commonly associated with IgM cold agglutinins result in subclinical
hemolysis and mild elevation of reticulocyte count. However, severe hemolysis due to Mycoplasma
infection is extremely rare. We herein report a case of severe warm Autoimmune Hemolytic Anemia
(AIHA) associated with Mycoplasma pneumoniae infection.
Case Presentation
A 15-years-old young lady with no previous medical illness presented to tertiary hospital
with fever, cough and vomiting for 1 week. On examination, she was pale and jaundiced. She was
breathless on minimal exertion and tachycardia at rest. There were crepitations heard bilateral lower
zones upon lungs auscultation. There was no organomegaly or lymphadenopathy. The rest of the
OPEN ACCESS
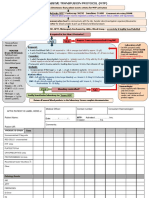
examination was unremarkable. Chest radiography was suggestive of pneumonia with reticulo-
*Correspondence: nodular infiltrates seen over both lungs (Figure 1). Laboratory evaluation showed severe anemia with
Chew WH, Department of Internal hemoglobin level of 2.4 g/dL, leukocytosis with total white count of 36.2 and platelet of 328. Others
Medicine, Hospital Canselor Tuanku laboratory results included: serum total bilirubin 59 mg/dL with predominant indirect bilirubin,
Muhriz (HCTM), Malaysia, serum Lactate Dehydrogenase (LDH) 1761 U/L, serum sodium 135 mmol/L with creatinine level
E-mail: sarahchew5064@gmail.com
of 52 mmol/L. Blood and urine culture were negative. Urgent peripheral blood film was suggestive
of AIHA and active hemolysis. Direct Coombs test was strongly positive (4+) for IgG and C3d
Received Date: 06 Jul 2020
suggestive of warm AIHA. Indirect Coombs test was positive as well but antibody identification
Accepted Date: 01 Aug 2020
revealed non-specific autoantibody IgG. Other autoimmune and virology screening were negative.
Published Date: 04 Aug 2020
The diagnosis of Mycoplasma pneumoniae infection was confirmed on the basis of high mycoplasma
Citation: antibody titer of 1:1280. Further testing showed red cell phenotype was O positive, R1R1, Jka-b+
Chew WH, Zainal Adlishah ZA, Fann and ss. She was treated with intravenous immunoglobulin, intravenous methylprednisolone and
RJ, Mohamad AZ, Ong TC, Jameela. oral azithromycin. 2 pints of least incompatible packed cell were transfused during her stay without
Mycoplasma pneumoniae Induced transfusion reaction. She was discharged after 5 days with oral prednisolone and subsequent follow
Warm Autoimmune Hemolytic Anemia up reviewed normal blood count (Figures 2-4).
– A Rare Case Report. Ann Clin Case Discussion
Rep. 2020; 5: 1870.
ISSN: 2474-1655 Subclinical hemolysis is common in Mycoplasma pneumoniae infection but severe warm AIHA
Copyright © 2020 Chew WH. This is requiring intensive treatment and blood transfusion is rare. Our patient demonstrated a severe form
of hemolytic anemia with presentation hemoglobin level of 2.4 g/dl and it showed warm AIHA
an open access article distributed under
suggestive by Direct Antiglobulin Test (DAT), requiring high dose steroid with IV immunoglobulin
the Creative Commons Attribution
and blood transfusion. Although such cases were rare, there have been several case reports reporting
License, which permits unrestricted
similar presentation [1-3].
use, distribution, and reproduction in
any medium, provided the original work AIHA was defined as positive Direct Antiglobulin Test (DAT-positive) after exclusion of
is properly cited. alternatives [4]. Autoantibody or complement fragment deposition on the RBC can be detected
Remedy Publications LLC., | http://anncaserep.com/ 1 2020 | Volume 5 | Article 1870
Chew WH, et al., Annals of Clinical Case Reports - Internal Medicine
Figure 1: Patient’s chest radiography on admission.
Figure 4: The chart showed series hemoglobin level and treatment given.
A: Oral azithromycin; B: Blood transfusion; I: Immunoglobulin; M:
Methylprednisolone
Myco II). Serodia Myco II is an in vitro diagnostic test for detection of
antibodies to Mycoplasma pneumoniae which is manufactured using
artificial gelatins particles sensitized with cell membrane component
of Mycoplasma pneumoniae (Mac strain). In a study conducted in
Malaysia, it concluded that titer of 1: >80 was the most suitable cut-of
titer for diagnosis of Mycoplasma pneumonia in Malaysians. Based
on her clinical and radiological evidence suggestive of pneumonia,
together with high titer of antibody detected, Mycoplasma pneumoniae
Figure 2: Peripheral blood film showed anemia with numerous spherocytes infection was diagnosed. While other causes of hemolysis had been
and polychromasia. excluded, it is strongly suggestive warm AIHA in this patient was
Nucleated RBC also seen. associated with Mycoplasma infection.
Corticosteroid with or without immunoglobulin remain the
mainstay of treatment of warm AIHA. Our case report demonstrated
that severe warm AIHA associated with Mycoplasma pneumoniae can
also be treated with systemic corticosteroid and IV immunoglobulin.
Nevertheless, she should be seen periodically to monitor for relapse
and reemergence of new symptoms that suggest other underlying
causes of warm AIHA [6].
Conclusion
Severe warm autoimmune hemolytic anemia can be associated
with Mycoplasma infection which responded well with antibiotics,
Figure 3: Presence of teardrop-shaped red cells and red cell auto- steroid, immunoglobulin and blood transfusion if indicated.
agglutination.
References
using polyspecific and monospecific DAT. Warm AIHA is caused by 1. Cassimos D, Bezirgiannidou Z, Pantelidou D, Christoforidis A,
autoantibodies that bind red cells optimally in vitro at 37°C leading to Chatzimichae A, Maritinis G. Warm autoimmune hemolytic anemia
destruction of red cells. Warm AIHA comprising mainly in adult cases following recurrent mycoplasma pneumonia infections in a child with
which half of the cases are called primary because unknown etiology. Down syndrome. Pediatr Hematol Oncol. 2008;25(7):693-8.
Secondary warm AIHA such as lymphoproliferative disorder, 2. Wandro C, Dolatshahi L, Blackall D. Severe warm autoimmune hemolytic
autoimmune disease especially systemic lupus erythematosus [5,6], anemia in a 7-month-old infant associated with a mycoplasma pneumoniae
infections mostly viral or drug induced. The autoantibodies in warm infection. J Pediatr Hematol Oncol. 2018;40(7):e439-e41.
AIHA are the IgG in most cases [7]. Complement fragments, most 3. Louie EK, Ault KA, Smith BR, Hardman EL, Quesenberry PJ. IgG-
often C3d combined with IgG happened in 50% of warm AIHA. In mediated haemolysis masquerading as cold agglutinin-induced anemia
other word, warm AIHA can be happened in the presence of DAT complicating severe infection with mycoplasma pneumoniae. Scand J
positive for IgG with or without C3d. C3d may be found in both Haematol. 1985;35(3):264-9.
cold and warm AIHA, hence testing for cold agglutinin in patient is 4. Hill QA, Hill A, Berentsen S. Defining autoimmune hemolytic anemia: A
needed. systematic review of the terminology used for diagnosis and treatment.
Blood Adv. 2019;3(12):1897-906.
Serology such as Mycoplasma pneumoniae enzyme-linked
immunosorbent assays for immunoglobulin M and immunoglobin 5. Sallah S, Wan JY, Hanrahan LR. Future development of lymphoproliferative
disorders in patients with autoimmune hemolytic anemia. Clin Cancer
G antibodies are currently widely used. The most convincing
Res. 2001;7(4):791-4.
evidence of ongoing infection is a significant increase in IgG or an
IgG seroconversion in paired sera, collected 3 to 4 weeks part [8]. 6. Roumier M, Loustau V, Guillaud C, Languille L, Mahevas M, Khellaf M, et
In this case, our laboratory used particle agglunation test (Serodia al. Characteristics and outcome of warm autoimmune hemolytic anemia in
Remedy Publications LLC., | http://anncaserep.com/ 2 2020 | Volume 5 | Article 1870
Chew WH, et al., Annals of Clinical Case Reports - Internal Medicine
adults: New insights based on a single-center experience with 60 patients. 8. Nir-Paz R, Michael-Gayego A, Ron M, Block C. Evaluation of eight
Am J Hematol. 2014;89(9):E150-5. commercial tests for Mycoplasma pneumoniae antibodies in the absence
of acute infection. Clin Microbiol Infect. 2006;12(7):685-8.
7. Packman CH. Hemolytic anemia due to warm autoantibodies. Blood Rev.
2008;22(1):17-31.
Remedy Publications LLC., | http://anncaserep.com/ 3 2020 | Volume 5 | Article 1870
You might also like
- Organic Chemistry Board Exam QuestionsDocument10 pagesOrganic Chemistry Board Exam QuestionsRiza Joie Versales100% (1)
- GR10-12 Delphi Cram Notes - Revision1Document20 pagesGR10-12 Delphi Cram Notes - Revision1Adams Adams Sheldon100% (1)
- D75 14Document8 pagesD75 14JorgeCalvoLara100% (2)
- Evan Syndrome A Case ReportDocument3 pagesEvan Syndrome A Case ReportEditor IJTSRDNo ratings yet
- 2761 8144 1 SMDocument6 pages2761 8144 1 SMAnnisa apriliaNo ratings yet
- Fulltext - Hematology v3 Id1118Document3 pagesFulltext - Hematology v3 Id1118Thành Nguyễn VănNo ratings yet
- Servizi SRL: Rapid Diagnosis of Streptococcus Pneumoniae-Induced Haemolytic-Uraemic SyndromeDocument3 pagesServizi SRL: Rapid Diagnosis of Streptococcus Pneumoniae-Induced Haemolytic-Uraemic SyndromeValerii GavrilutaNo ratings yet
- Immune Hemolytic Anemia Modul 4Document10 pagesImmune Hemolytic Anemia Modul 4Dinda SaviraNo ratings yet
- Ofy 038Document5 pagesOfy 038Rosandi AdamNo ratings yet
- Acute Epiglottitis in The Immunocompromised Host: Case Report and Review of The LiteratureDocument5 pagesAcute Epiglottitis in The Immunocompromised Host: Case Report and Review of The Literaturerosandi sabollaNo ratings yet
- Paroxysmal Cold Hemoglobinuria: Donath-Landstiener Screening TestDocument1 pageParoxysmal Cold Hemoglobinuria: Donath-Landstiener Screening TestMichelle San Miguel FeguroNo ratings yet
- Infections in Acute Lymphoblastic Leukaemia: C Y Chong,, A M Tan,, J LouDocument5 pagesInfections in Acute Lymphoblastic Leukaemia: C Y Chong,, A M Tan,, J LouUtari UbNo ratings yet
- Autoimmune Hemolytic Anemia (AIHA) : Becca Greenstein and Rebekah Wood Immunology 2 December 2014Document12 pagesAutoimmune Hemolytic Anemia (AIHA) : Becca Greenstein and Rebekah Wood Immunology 2 December 2014Dewina Dyani Rosari IINo ratings yet
- Cryptococcal Postinfectious Inflammatory Response Syndrome in An Immunocompetent HostDocument3 pagesCryptococcal Postinfectious Inflammatory Response Syndrome in An Immunocompetent HostinfectogoNo ratings yet
- Reporte de Caso EmbaraoDocument3 pagesReporte de Caso EmbaraoPaola TabaresNo ratings yet
- TMH 0042 0317Document8 pagesTMH 0042 0317Joon RaynerNo ratings yet
- Secondary Hemophagocytic Lymphohistiocytosis: A Rare Case ReportDocument5 pagesSecondary Hemophagocytic Lymphohistiocytosis: A Rare Case ReportivanNo ratings yet
- Entericfever 201810061138061823280Document4 pagesEntericfever 201810061138061823280Cindy HerwitiNo ratings yet
- Hemophagocytic Syndrome Due To Infection by H1N1 Influenza VirusDocument5 pagesHemophagocytic Syndrome Due To Infection by H1N1 Influenza VirusAnonymous zENwrie4No ratings yet
- Plasma Cytokine Profile On Admission Related To Aetiology in Community Acquired PneumoniaDocument9 pagesPlasma Cytokine Profile On Admission Related To Aetiology in Community Acquired Pneumoniahusni gunawanNo ratings yet
- JCM 09 03858Document14 pagesJCM 09 03858MonorachSinNo ratings yet
- Immune Hemolytic AnemiaDocument25 pagesImmune Hemolytic AnemiaMuhammad DaviqNo ratings yet
- Recurrent Aseptic Meningitis in A Child: Case ReportDocument3 pagesRecurrent Aseptic Meningitis in A Child: Case ReportAprimadhansari FarzimNo ratings yet
- CTX-M Paper PDFDocument4 pagesCTX-M Paper PDFTunde OdetoyinNo ratings yet
- TMP FE4 ADocument4 pagesTMP FE4 AFrontiersNo ratings yet
- Asymptomatic Mycoplasma Infection Causing Acute Demyelinating Encephalomyelitis: Case Report and Review of LiteratureDocument4 pagesAsymptomatic Mycoplasma Infection Causing Acute Demyelinating Encephalomyelitis: Case Report and Review of Literatureluisalfredo_montesNo ratings yet
- Dengue Fever With Hepatitis E and Hepatitis A Infection PDFDocument2 pagesDengue Fever With Hepatitis E and Hepatitis A Infection PDFAMENDBENo ratings yet
- 2020 BIO Depth Study Infectious DiseaseDocument8 pages2020 BIO Depth Study Infectious Diseasewhiteprism23No ratings yet
- Genet 1996Document1 pageGenet 1996Araceli Enríquez OvandoNo ratings yet
- Clayton 2016Document2 pagesClayton 2016brakim23No ratings yet
- 148-Article Text-695-1-10-20180529Document5 pages148-Article Text-695-1-10-20180529fio rentiniNo ratings yet
- Asim,+prof +1726Document6 pagesAsim,+prof +1726Zayn HNo ratings yet
- PIIS1198743X14652605Document3 pagesPIIS1198743X14652605Gerald NacoNo ratings yet
- TMP 155 BDocument7 pagesTMP 155 BFrontiersNo ratings yet
- Poster LESDocument6 pagesPoster LESAlejandra LuqueNo ratings yet
- Chronic Spontaneous Urticaria-Status Quo and Future: Susanne Melchers Jan P. NicolayDocument11 pagesChronic Spontaneous Urticaria-Status Quo and Future: Susanne Melchers Jan P. NicolayRizka ZulaikhaNo ratings yet
- Article Koskina ArchDocument8 pagesArticle Koskina ArchElli SymeonidouNo ratings yet
- COVID-19 Related Acute Necrotizing Encephalopathy Presenting in The Early Postoperative PeriodDocument8 pagesCOVID-19 Related Acute Necrotizing Encephalopathy Presenting in The Early Postoperative PeriodElli SymeonidouNo ratings yet
- Atypical MeaslesDocument2 pagesAtypical MeaslesBagusPranataNo ratings yet
- Ajts 15 160Document6 pagesAjts 15 160Khatidja AllyNo ratings yet
- Successful Management of Severe Chronic Autoimmune Hemolytic Anemia With Low Dose Cyclosporine and Prednisone in An InfantDocument4 pagesSuccessful Management of Severe Chronic Autoimmune Hemolytic Anemia With Low Dose Cyclosporine and Prednisone in An InfantFatimatuzzahra ShahabNo ratings yet
- Hemophagocytic Lymphohistiocytosis in A Child With Chro - 2022 - Medical JournalDocument4 pagesHemophagocytic Lymphohistiocytosis in A Child With Chro - 2022 - Medical JournalAnisha RanaNo ratings yet
- Autoimmune - Hemolytic - Anemia - Mixed - Type-A - Case - Repo 2Document5 pagesAutoimmune - Hemolytic - Anemia - Mixed - Type-A - Case - Repo 2Afsha AnishNo ratings yet
- HellowDocument6 pagesHellowafina rasaki asriNo ratings yet
- Management of HemophagocyticDocument10 pagesManagement of HemophagocyticAlexander CanoNo ratings yet
- Lupus Dupa Interferon AlfaDocument4 pagesLupus Dupa Interferon AlfadeliaNo ratings yet
- PancreatitisDocument5 pagesPancreatitisPanchito2000100% (1)
- Fatal Toxic Shock Syndrome From An Intrauterine DeviceDocument3 pagesFatal Toxic Shock Syndrome From An Intrauterine DeviceSiti Ro'AinunNo ratings yet
- Lee Et Al 2001 Case Report Meningococcal MeningitisDocument3 pagesLee Et Al 2001 Case Report Meningococcal MeningitisAsmae OuissadenNo ratings yet
- Hyperinflammatory Syndrome in A Child With COVID-19 Ind Pediatr 2020Document3 pagesHyperinflammatory Syndrome in A Child With COVID-19 Ind Pediatr 2020Bala RamachandranNo ratings yet
- Role of Intravenous ImmunoglobulinDocument4 pagesRole of Intravenous ImmunoglobulinZamir Eid Paez MojicaNo ratings yet
- Anti NDocument2 pagesAnti NLakhvinder SinghNo ratings yet
- Pakistan - CVID Case Report 27 July 2018Document12 pagesPakistan - CVID Case Report 27 July 2018Aziz Ul QadirNo ratings yet
- A Rare Cause of AA Amyloidosis and End-Stage Kidney Failure: AnswersDocument3 pagesA Rare Cause of AA Amyloidosis and End-Stage Kidney Failure: AnswersSezen YılmazNo ratings yet
- Mjhid 7 1 E2015036Document3 pagesMjhid 7 1 E2015036Admin neuro-usu.idNo ratings yet
- 1 s2.0 S2468124519301184 MainDocument1 page1 s2.0 S2468124519301184 Maindewi sumbangNo ratings yet
- Autoimmune Lymphoproliferative Syndrome (ALPS) : A Rare Cause of Immune CytopeniaDocument3 pagesAutoimmune Lymphoproliferative Syndrome (ALPS) : A Rare Cause of Immune CytopeniaathiraNo ratings yet
- A Young Traveller Presenting With Typhoid Fever After Oral Vaccination: A Case ReportDocument9 pagesA Young Traveller Presenting With Typhoid Fever After Oral Vaccination: A Case ReportMarscha MaryuanaNo ratings yet
- Isoniazid Causing Pleural Effusion: Case ReportDocument2 pagesIsoniazid Causing Pleural Effusion: Case Reporttiti agniNo ratings yet
- Group A Streptococcal Meningitis: Report of A Case and Review of Literature Since 1976Document5 pagesGroup A Streptococcal Meningitis: Report of A Case and Review of Literature Since 1976soledad88No ratings yet
- 1768 PDFDocument2 pages1768 PDFAndhiky Raymonanda MadangsaiNo ratings yet
- A Case Report of Invasive Aspergillosis in A Patient Treated With RuxolitinibDocument3 pagesA Case Report of Invasive Aspergillosis in A Patient Treated With RuxolitinibJongga SiahaanNo ratings yet
- Immune Hematology: Diagnosis and Management of Autoimmune CytopeniasFrom EverandImmune Hematology: Diagnosis and Management of Autoimmune CytopeniasJenny M. DespotovicNo ratings yet
- Adverse Effects: Blood TransfusionDocument43 pagesAdverse Effects: Blood TransfusionDumindu PereraNo ratings yet
- Fpia LS%VD Ixj Ok Moku Chess Development Foundation Rjuq F Mgptpuj JP KD WKDocument3 pagesFpia LS%VD Ixj Ok Moku Chess Development Foundation Rjuq F Mgptpuj JP KD WKDumindu PereraNo ratings yet
- Resolution of ABO Discrepancies: Justin R. Rhees, M.S., MLS (ASCP), SBBDocument41 pagesResolution of ABO Discrepancies: Justin R. Rhees, M.S., MLS (ASCP), SBBDumindu PereraNo ratings yet
- Baseline:: Notify Transfusion Laboratory To: Activate MTP'. Footscray: 56292 Sunshine: 51480 Allocate Team RolesDocument2 pagesBaseline:: Notify Transfusion Laboratory To: Activate MTP'. Footscray: 56292 Sunshine: 51480 Allocate Team RolesDumindu PereraNo ratings yet
- Full Data AnalysisDocument627 pagesFull Data AnalysisMyMinecrafter97No ratings yet
- Chapter 7-Managing Quality: 07/20/2022 1 Arsi University Om Mba-2020Document33 pagesChapter 7-Managing Quality: 07/20/2022 1 Arsi University Om Mba-2020temesgen yohannesNo ratings yet
- CascadeTEK Vacuum Oven ManualDocument49 pagesCascadeTEK Vacuum Oven ManualCascade TEKNo ratings yet
- Complete Using ConditionalsDocument2 pagesComplete Using ConditionalsicecrisNo ratings yet
- The "Write" Way: A Judicial Clerk's Guide To Writing For The CourtDocument92 pagesThe "Write" Way: A Judicial Clerk's Guide To Writing For The Courtunknown07blackstarNo ratings yet
- Willis, John Ral - Slaves and Slavery in Muslin Africa - The Servuile State PDFDocument211 pagesWillis, John Ral - Slaves and Slavery in Muslin Africa - The Servuile State PDFTheCremaNo ratings yet
- Emerging Global Trends in Iot: (Internet of Things)Document28 pagesEmerging Global Trends in Iot: (Internet of Things)EkoPandaraNo ratings yet
- Feasibility Study Project Proposal RequirementsDocument2 pagesFeasibility Study Project Proposal RequirementsErick NgosiaNo ratings yet
- Epe 2013111515302022Document5 pagesEpe 2013111515302022qais652002No ratings yet
- Principal 5svbk8Document56 pagesPrincipal 5svbk8badillojdNo ratings yet
- 7 Furious Prayers For July 2023 by ElishaDocument1 page7 Furious Prayers For July 2023 by Elishaiyayi2006No ratings yet
- People Vs OandasanDocument2 pagesPeople Vs OandasanAdoha Lei T Blanco100% (1)
- Semi Detailed Lesson PlanDocument2 pagesSemi Detailed Lesson Planrey ramirezNo ratings yet
- General Definition of Sag and Tension in Electrical Transmission LinesDocument11 pagesGeneral Definition of Sag and Tension in Electrical Transmission Linesdskymaximus67% (3)
- UGEB2362 Course Outline 2023-24Document5 pagesUGEB2362 Course Outline 2023-24Suki PunNo ratings yet
- METRIX AUTOCOMP - Company ProfileDocument2 pagesMETRIX AUTOCOMP - Company ProfileVaibhav AggarwalNo ratings yet
- PhilosophyDocument4 pagesPhilosophyJudalineNo ratings yet
- Checklist Information Security Policy ImplementationDocument18 pagesChecklist Information Security Policy Implementationbaye omar SoceNo ratings yet
- Cabbash Vms BrochureDocument22 pagesCabbash Vms BrochureOghosa OsahenrhumwenNo ratings yet
- Research GR 2 Pinaka Final 1Document36 pagesResearch GR 2 Pinaka Final 1Richeille JoshNo ratings yet
- Practice Quiz - Managing CollaborationDocument2 pagesPractice Quiz - Managing CollaborationMohamed RahalNo ratings yet
- ReadmeDocument1 pageReadmedan maliwatNo ratings yet
- Technical InstructionsDocument6 pagesTechnical InstructionsSadinjana LakshanNo ratings yet
- Using Powerpoint Effectively in Your PresentationDocument5 pagesUsing Powerpoint Effectively in Your PresentationEl Habib BidahNo ratings yet
- Psycholinguistics: What It Is? - Language, Speech and Communication.Document4 pagesPsycholinguistics: What It Is? - Language, Speech and Communication.Edo PrasetiaNo ratings yet
- ISBB CompilationDocument6 pagesISBB CompilationElla SalesNo ratings yet
- Carroll Solo Bed - Technical ManualDocument42 pagesCarroll Solo Bed - Technical Manualtaioba2010No ratings yet