Professional Documents
Culture Documents
Idiopathic Fascicular Left Ventricular Tachycardia: A Case Report
Idiopathic Fascicular Left Ventricular Tachycardia: A Case Report
Uploaded by
Ade BayunataOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Idiopathic Fascicular Left Ventricular Tachycardia: A Case Report
Idiopathic Fascicular Left Ventricular Tachycardia: A Case Report
Uploaded by
Ade BayunataCopyright:
Available Formats
LAPORAN KASUS
Idiopathic Fascicular Left Ventricular Tachycardia:
A Case Report
Kadek Agus Putra Udayana, I Putu Parwata Jaya
Department of Cardiology, Wangaya Distric Hospital, Denpasar, Bali, Indonesia
Abstract
Idiopathic fascicular left ventricular tachycardia (IFLVT) is the most common idiopathic ventricular tachycardia (IVT) of the left ventricle. ILFVT is
characterized by right bundle branch block and left axis deviation. We report a case of IFLVT in a 34-year-old woman presenting with palpitation.
The ECG revealed a wide QRS complex tachycardia with a right bundle branch block (RBBB) and right axis deviation. Vagal maneuvers were
ineffective. Conversion to sinus rhythm was obtained 10 hours later, with i.v amiodarone. The patient was discharged after 3 days on oral
verapamil.
Keywords: Idiopathic ventricular tachycardia, right bundle branch block complex tachycardia, verapamil
Abstrak
Idiopathic Fascicular Left Ventricular Tachycardia (IFLVT) adalah bentuk paling sering Idiopathic Ventricular Tachycardia (IVT) ventrikel kiri. ILFVT
ditandai dengan blok cabang berkas kanan dan penyimpangan sumbu ke kiri. Kami melaporkan kasus IFLVT pada wanita 34 tahun yang
mengalami palpitasi. EKG menunjukkan takikardi kompleks QRS lebar dengan morfologi blok cabang berkas kanan dan penyimpangan sumbu
ke kanan. Manuver vagal tidak efektif. Konversi ke irama sinus diperoleh 10 jam kemudian dengan amiodaron i.v.. Pasien dipulangkan setelah 3
hari dengan verapamil oral. Kadek Agus Putra Udayana, I Putu Parwata Jaya. Idiopathic Fascicular Left Ventricular Tachycardia: Laporan Kasus
Kata kunci: Blok cabang berkas kanan, idiopathic ventricular tachycardia, verapamil
INTRODUCTION is the most common IVT of the left ventricle The palpitations was not accompanied with
Broad complex tachycardia presents a and represents the 10-15% of all IVT.4 Zipes, et shortness of breath, chest pain nor syncopal
diagnostic and therapeutic challenge to al, first described IFLVT in 1979.5 They reported attack. She is breastfeeding an 8-month child.
the emergency physician. The majority of three VT cases with right bundle branch block She also complained of fever since a day ago.
cases are ventricular tachycardia (VT) with (RBBB) and left axis after atrial pacing. Two She is non-smoker and has no known history
underlying ischaemic heart disease.1 Broad years later, Belhassen, et al,6 described that of any medical illness or drug use; with no
complex tachycardia may also occur as a intravenous verapamil significantly decreased similar previous complaint.
result of a supraventricular tachycardia (SVT) the recurrence rate of IFLVT.
in the presence of aberrant conduction. Physical examination in previous hospital,
Differentiation has important implications It may be difficult to differentiate IFLVT from revealed blood pressure was 110/80 mmHg,
for management and prognosis. If VT is SVT because both are characterized by the pulse rate 222 beats/minute, and body
mistakenly diagnosed as SVT with aberrant absence of structural heart disease and the temperature 38,5 ºC. On cardiac examination,
conduction and treated with calcium channel same ECG based on QRS morphology or S1 and S2 were normal, no murmurs nor
blockers, the patient is likely to become RS interval. Vagal maneuvers, adenosine, additional sounds. The chest was clear on
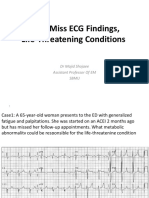
haemodynamically unstable.2 Some clinicians and lidocaine are ineffective in IFLVT; it auscultation. On electrocardiogram (ECG),
therefore advocate assumption that all cases is terminated or suppressed by calcium lead I rhythm showed a broad complex
of broad complex tachycardia are VT.1,2 antagonists.7 tachycardia with QRS duration 120 ms. Lead
II and III rhythms showed an apparent narrow
Idiopathic ventricular tachycardia (IVT) is a CASE QRS complex tachycardia with QRS duration
term used for VT in the absence of clinically A 34-year-old woman was admitted to the 80 ms. Lead V1 showed monophasic R pattern
apparent structural heart disease and accounts emergency department referred from private and R/S in V6 less than 1. A 12-lead ECG
for approximately 10% of all VTs.3 Idiopathic hospital with sudden onset of palpitations. She revealed wide QRS complex tachycardia with
fascicular left ventricular tachycardia (IFLVT) complained palpitations since about 3 hours. a right bundle branch block (RBBB), and right
Presented at Bali Cardiology Update VII 2018
Alamat Korespondensi email: putraudayana91@gmail.com
436 CDK-287/ vol. 47 no. 6 th. 2020
LAPORAN KASUS
axis deviation (Figure 1). Vagal manouver were interval of 60-80 ms).9 Both features can lead includes AV dissociation, capture or fusion
tried but failed to terminate the arrhythmia. to misdiagnosis of aberrant supraventricular beats, negative or positive concordance, and
Cardiology consultation was sought and tachycardia. Capture beats and fusion beats tachycardia QRS narrower than sinus QRS.10,11
a diagnosis of fascicular tachycardia was may be present, suggesting the diagnosis of VT The traditional criteria needs determination
suspected. Intravenous amiodarone was rather than SVT . Physical findings that indicate that the broad complex has a right bundle
administered with a dose of 150 mg in the first the presence of AV dissociation strongly branch block (RBBB)-like or a left bundle
10 minutes and continued with a maintenance suggests VT.2,10 Valsalva maneuver, carotid branch block (LBBB)-like pattern. In RBBB-like
dose of 900 mg in 24 hours. It was successfully sinus massage or adenosine administration pattern, criteria suggesting VT: (i) QRS width
converted to sinus tachycardia 3 hours later may also facilitate the elucidation of >140 ms, (ii) left axis deviation, and (iii) in lead
(Figure 2). Then the patient was referred to a tachycardia mechanism. Termination of V1 found QR, or R, or RSr’ with lead V6, R/S <1
public hospital because of the unavailability of tachycardia using these procedures strongly or QS. Whereas, in LBBB-like pattern, criteria
intensive care. suggests SVT.10 VT due to triggered mechanism suggesting VT: (i) QRS width >160 ms, (ii) right
such as idiopathic outflow tract VT may be axis deviation, and (iii) initial R in V1 >30 ms, or
In the referral hospital, the hemodynamic was terminated as well with these maneuvers.10,11 slurring /notching of the downstroke of the S
stabile, blood pressure 100/70 mmHg, pulse Even if the arrhythmia remains unaffected, wave in V1-2, or begin QRS-nadir S-wave >70
rate 110 beats/minute, respiratory rate 20/ these maneuvers may clarify the mechanism ms in V1-2, with Q in V6.11
minute, and body temperature 38,5ºC. Only of tachycardia by exposing AV dissociation in
intravenous amiodarone was given with a the case of VT.10 In 1991, Brugada, et al, produced simple
maintenance dose of 900 mg in 24 hours. criteria in a stepwise approach irrespective
The traditional ECG criteria favouring VT of the QRS complex morphology.10,11 The
After 10 hours, ECG shows sinus rhythm.
The patient was admitted to the intensive
cardiology care unit where serial ECGs
were done. Laboratory tests only revealed
leukocytosis with neutrophils increase. Acute
mastitis was diagnosed based on examination.
The symptoms was relieved after antibiotics
was given. Echocardiography showed a
nondilated left ventricle with normal systolic
and diastolic function. Amiodarone were still
administered intravenously until it run out
within 24 hours. The patient was discharged
after 3 days on oral verapamil 80 mg three times
a day and advised for electrophysiological
study or catheter ablation.
DISCUSSION
ILFVT generally presents in young adults Figure 1. ECG during ventricular tachycardia. ECG shows a monomorphic right bundle branch block
aged 15-40 year-old, mainly affects males tachycardia with a relative narrow QRS duration (narrower than other forms of VT), and right axis deviation
(60%-80%).8 Symptoms typically include
dizziness, palpitations, chest discomfort,
and occasionally syncope. Although most
episodes occur at rest, exercise, infection,
emotional stress and catecholamine infusion
can act as triggers. Triggered activity was at
first postulated as a potential mechanism,5
but later studies showed that IFLVT behaves
electrophysiologically as a reentrant
tachycardia.8
The baseline ECG is normal in most patients;
it may present T-wave inversion immediately
after tachycardia (cardiac memory). Unlike
patients with structural heart disease, IFLVT
usually shows a QRS complex duration inferior
to 140-150 ms and fast initial forces (RS Figure 2. ECG after 2 hour of amiodarone infusion. ECG shows conversion to sinus tachycardia
CDK-287/ vol. 47 no. 6 th. 2020 437
LAPORAN KASUS
algorithm begins with the identification of an Anterior Hemiblock Aberrancy has been was successful as the second line of acute
RS complex in any precordial lead, if negative, reported by Michowitz et al. They found management in 4 children with IFLVT; the VT
the diagnosis of VT is made. If an RS complex criteria were suggestive of VT: (i) atypical V1 slowed down and was finally terminated in 3
is present in one or more precordial leads, morphology, (ii) QRS width ≤ 140 ms, (iii) R/S patients (within 1-48 hours)14 However, unlike
the next step is to measure the longest RS ratio in V6 ≤ 1, and (iv) positive aVR.12 other idiopathic VT, IFLVT usually does not
interval. If an RS interval is longer than 100 ms, respond to vagal maneuvers, adenosine, or
the diagnosis of VT is made. If not, the next The electrocardiographical pattern varies beta blockers.15 This has been attributed to the
step of the algorithm is to consider whether depending on the site of origin of the fact that IFLVT depends on the slow entry of
AV dissociation is present. If positive, the tachycardia. Posterior fascicular VT by calcium in partially depolarized Purkinje fibers
diagnosis of VT is made. If absent, the classical far accounts for the majority of IFLVT, and not the cyclic adenosine monophosphate
morphology criteria for VT are used. If both representing over 90% cases. The surface mediated triggered activity occurring in the
lead V1 and V6 fulfil the criteria for VT, the electrocardiogram demonstrates tachycardia adenosine‑sensitive VT.15
diagnosis of VT is made. If not, the diagnosis with a RBBB pattern and a left superior axis
of SVT with aberrant conduction is made by deviation. Other forms of IFLVT include Verapamil may be helpful in patients with
exclusion of VT.11 anterior fascicular VT presenting with a RBBB mild symptoms.9,13 If symptoms are severe
and right axis deviation as well as the more and pharmacologic treatment is not effective
In 2007, a new algorithm has been proposed rare upper septal fascicular VT which can or is poorly tolerated, catheter ablation is
by Vereckei, et al.10,11 The following criteria present with either a RBBB, left bundle branch recommended.9 Ablation success rates as
were suggestive of VT: (i) AV dissociation; (ii) an block (LBBB), or a normal QRS.6 reported in various series vary between 85
initial R-wave in lead aVR, and (iii) the voltage and 95%, generally higher in posterior IFLVT.
during the initial 40 ms (Vi ), the terminal 40 As in other idiopathic ventricular tachycardia, Recurrence rates are also lower in these
ms (Vt), their ratio (Vi /Vt), and that Vi /Vt ≤1 IFLVT diagnosis requires exclusion of structural patients (5% vs. 12.5%).16,17
was suggestive of VT. In 2008, the same group heart disease. It is therefore recommended
presented a simplified algorithm using only to perform echocardiography and coronary CONCLUSION
lead aVR. Using this algorithm, VT can be angiography or computed tomography, A diagnosis of fascicular tachycardia should be
diagnosed if one of these conditions found if deemed necessary depending on the considered if standard methods including vagal
in lead aVR; (i) an initial R-wave, (ii) width of cardiovascular risk profile of the patient.13 maneuvers and adenosine administration fail
an initial r- or q-wave >40 ms, (iii) notching Diagnosis and the mechanism IFLVT can to convert the arrhythmia and the 12-lead
on the initial downstroke of a predominantly be clarified using the electrophysiological ECG shows a right bundle branch block with
negative QRS complex, and (4) Vi /Vt ≤ 1.11 study.3,4,13 left axis deviation. Diagnosis can be clarified
by electrophysiological study. In the acute
ILFVT might be difficult to diagnose using As in other cases of wide QRS tachycardia, setting, first-line pharmacological treatment
these morphological criteria, as most studies the hemodynamic status should evaluated. is verapamil. Catheter ablation is effective
did not include these patients.11 In 2017, a new Electrical cardioversion is emergent in case and is recommended when symptoms are
criteria to differentiate the QRS morphology of of tachycardia intolerance. In stable patients, severe or when pharmacological treatment
Posterior Fascicular Ventricular Tachycardia as its name suggests, first line treatment is ineffective and poorly tolerated or not
from Right Bundle Branch Block and Left is verapamil.6 Intravenous amiodarone preferred by the patient.
REFERENCES
1. Akhtar M, Shenasa M, Jazayeri M, Caceres J, Tchou PJ. Wide QRS complex tachycardia: Reappraisal of a common clinical problem. Ann Intern Med. 1988;109:905–12.
2. Stewart RB, Bardy GH, Greene HL. Wide complex tachycardia: Misdiagnosis and outcome after emergent therapy. Ann Intern Med. 1986;104:766–71.
3. Aliot EM, Stevenson WG, Almendral-Garrote JM, Bogun F, Calkins CH, Delacretaz E, et al. European Heart Rhythm Association/ Heart Rhythm Society expert
consensus on catheter ablation of ventricular arrhythmias. Europace. 2009;11:771-817.
4. Lerman BB, Stein KM, Markowitz SM. Mechanisms of idiopathic left ventricular tachycardia. J Cardiovasc Electrophysiol. 1997;8:571-83.
5. Zipes D, Douglas PR, Troup PJ, Pedersen DHl. Atrial induction of ventricular tachycardia: Reentry versus triggered automaticity. Am J Cardiol. 1979;44:1-8.
6. Belhassen B, Rotmensch HH, Laniado S. Response of recurrent sustained ventricular tachycardia to verapamil. Br Heart J. 1981;46:679-82.
7. Lin FC, Finley CD, Rahimtoola SH, Wu D. Idiopathic paroxysmal ventricular tachycardia with a QRS pattern of right bundle branch block and left axis deviation: A
unique clinical entity with specific properties. Am J Cardiol. 1983;52:95‑100.
8. Nakagawa M, Takahashi N, Nobe S, Ichinose M, Ooie T, Yufu F, et al. Gender differences in various types of idiopathic ventricular tachycardia. J Cardiovasc.
Electrophysiol. 2002;13:633-8.
9. Andrade FR, Eslami M, Elias J, Kinoshita O, Nakazato Y, Marcus FI, et al. Diagnostic clues from the surface ECG to identify idiopathic (fascicular) ventricular tachycardia:
Correlation with electrophysiologic findings. J Cardiovasc Electrophysiol. 1996;7:2‑8.
10. Vereckei A. Current Algorithms for the diagnosis of wide QRS complex tachycardias. Curr Cardiol Rev. 2014;10:262-76.
11. Alzand BSN, Crijns HJGM. Diagnostic criteria of board QRS complex tachycardia: Decades of evolution. Europace. 2011;13:465-72.
12. Michowitz Y, Tovio Brodie O, Heusler I, Sabbag A, Rahkovich M, Shmueli H, et al. Differentiating the QRS morphology of posterior fascicular ventricular tachycardia
from right bundle branch block and left anterior hemiblock aberrancy. Circ Arrhythm Electrophysiol. 2017;10(9):e005074.
438 CDK-287/ vol. 47 no. 6 th. 2020
LAPORAN KASUS
13. Reviriego SM. Idiopathic fascicular left ventricular tachycardia. e-Journal ESC Council for Cardiology Practice. 2010;9:13-20.
14. Suesaowalak M, Khongphatthanayothin A, Sunsaneewitayakul B, Sirisopikun T, Promphan W, Jariyapongpaiboon Y, et al. Idiopathic left ventricular tachycardia in
children. J Med Assoc Thai. 2008;91(11):1732-8.
15. Lerman BB. Response of nonreentrant catecholamine mediated ventricular tachycardia to endogenous adenosine and acetylcholine. Evidence for myocardial
receptor mediated effects. Circulation. 1993;87:382-90.
16. Peichl P, Wichterle D, Pavlu L, Cihak R, Aldhoon B, Kautzner J. Complications of catheter ablation of ventricular tachycardia: A single center experience. Circ Arrhythm
Electrophysiol. 2014;7:684‑90.
17. Lamberti F, Di Clemente F, Remoli R, Bellini C, De Santis A, Mercurio M, et al. Catheter ablation of idiopathic ventricular tachycardia without the use of fluoroscopy.
Int J Cardiol. 2015;190:338-43.
CDK-287/ vol. 47 no. 6 th. 2020 439
You might also like
- Top 100 ECG CasesDocument212 pagesTop 100 ECG Casessoha.s.tumsa7No ratings yet
- Beast Ebook PDFDocument38 pagesBeast Ebook PDFSteeN100% (1)
- Personal Effectiveness SummativeDocument24 pagesPersonal Effectiveness Summativeisikhuenmhen100% (1)
- GIBS Internship ReportDocument28 pagesGIBS Internship Reportm bilalNo ratings yet
- Idiopathic Fascicular LV Tachycardia Case Report - Kadek Agus Putra - Edit 1Document8 pagesIdiopathic Fascicular LV Tachycardia Case Report - Kadek Agus Putra - Edit 1putra udayanaNo ratings yet
- Can't Miss ECG FindingsDocument61 pagesCan't Miss ECG FindingsVikrantNo ratings yet
- Qara Syifa Fachrani - 2010221030 - Case Report Exercise-Induced Supraventricular Tachycardia in A 16-Year-Old Boy With Tricuspid RegurgitationDocument7 pagesQara Syifa Fachrani - 2010221030 - Case Report Exercise-Induced Supraventricular Tachycardia in A 16-Year-Old Boy With Tricuspid RegurgitationQara Syifa FNo ratings yet
- Differential Diagnosis of Wide QRS TachycardiasDocument6 pagesDifferential Diagnosis of Wide QRS TachycardiasKev Jose Ruiz RojasNo ratings yet
- 2019 WellSpan CV Symposium SVTDocument46 pages2019 WellSpan CV Symposium SVThawaig8No ratings yet
- Dre Sen 2017Document11 pagesDre Sen 2017gino loja villenaNo ratings yet
- Aritmii ECGDocument3 pagesAritmii ECGIlie RoxanaNo ratings yet
- Widecomplex Tachycardia: Mithilesh Kumar Das,, Archana Rajdev,, Vikas KalraDocument13 pagesWidecomplex Tachycardia: Mithilesh Kumar Das,, Archana Rajdev,, Vikas KalraTor JaNo ratings yet
- VT IndoDocument37 pagesVT IndotyaraNo ratings yet
- Normal Ecg, Infarction & Arrhythmias: Iqbal Lahmadi Departement of Internal Medicine Sintang - 2013Document98 pagesNormal Ecg, Infarction & Arrhythmias: Iqbal Lahmadi Departement of Internal Medicine Sintang - 2013Maylisa ManurungNo ratings yet
- Normal Ecg, Infarction & Arrhythmia SDocument98 pagesNormal Ecg, Infarction & Arrhythmia SAdinda GupitaNo ratings yet
- Diagnosis of Acute Myocardial InfarctDocument5 pagesDiagnosis of Acute Myocardial InfarctOscar SanNo ratings yet
- Supraventricular TachycardiDocument8 pagesSupraventricular TachycardiHairunisa 0049No ratings yet
- Broad Complex Tachycardia-LatestDocument96 pagesBroad Complex Tachycardia-LatestEsayas KebedeNo ratings yet
- Ventricular Arrhythmia - VT: Braghmandaru A.BDocument113 pagesVentricular Arrhythmia - VT: Braghmandaru A.BFaisol SiddiqNo ratings yet
- 12 - Lead ECG Interpretation Case StudiesDocument19 pages12 - Lead ECG Interpretation Case StudiessharenNo ratings yet
- Wide Qrs Tachy 2Document6 pagesWide Qrs Tachy 2Mohit TandonNo ratings yet
- Sixth Problem: Group 5Document51 pagesSixth Problem: Group 5Monica PramanaNo ratings yet
- Sudden Asystole During Radiofrequency Ablationa Case Report and Literature ReviewDocument5 pagesSudden Asystole During Radiofrequency Ablationa Case Report and Literature ReviewRizkaSafitriNo ratings yet
- Im 2Document3 pagesIm 2neni budiNo ratings yet
- Introduction To Interpretation V10.0 (2017-2018)Document91 pagesIntroduction To Interpretation V10.0 (2017-2018)Muhammad AsrudinNo ratings yet
- Unusual Features of Right and Left IdiopDocument5 pagesUnusual Features of Right and Left IdiopRicardo MingireanovNo ratings yet
- Kamis 10 September 2015 - IPD 2 - Kuliah-Ekg-Blok-KegawatdaruratanDocument118 pagesKamis 10 September 2015 - IPD 2 - Kuliah-Ekg-Blok-KegawatdaruratanIrfanArifZulfikarNo ratings yet
- Top100 ECG CasesDocument212 pagesTop100 ECG CaseszahraNo ratings yet
- Idiopathic Fascicular Left Ventricular Tachycardia: Linear Ablation Lesion Strategy For Noninducible or Nonsustained TachycardiaDocument6 pagesIdiopathic Fascicular Left Ventricular Tachycardia: Linear Ablation Lesion Strategy For Noninducible or Nonsustained TachycardiaRahmi SyuadzahNo ratings yet
- Ipd Kuliah Ekg Blok KegawatdaruratanDocument118 pagesIpd Kuliah Ekg Blok Kegawatdaruratansiti solikhaNo ratings yet
- ECG Lecture 4Document44 pagesECG Lecture 4asdasdasdasNo ratings yet
- Abstract Avrtcad2vd MuhammadakhiruddinDocument2 pagesAbstract Avrtcad2vd MuhammadakhiruddinNanank Akhiruddin SyamsaNo ratings yet
- 1 s2.0 S0972629216300213 MainDocument4 pages1 s2.0 S0972629216300213 Mainmaengkiw7No ratings yet
- ECG ModuleDocument40 pagesECG ModuleSHAFIUL ISLAMNo ratings yet
- Arrhythmias: M. Lacombe Mdfmr/Unecom July 22, 2009Document210 pagesArrhythmias: M. Lacombe Mdfmr/Unecom July 22, 2009Kent MaravillosaNo ratings yet
- G7pfe7Document5 pagesG7pfe7Carmen Cuadros BeigesNo ratings yet
- ECG - Complete Heart BlockDocument2 pagesECG - Complete Heart BlockCsilla DobrescuNo ratings yet
- AR Yang Komplikasi Menjadi Gagal Jantung PDFDocument5 pagesAR Yang Komplikasi Menjadi Gagal Jantung PDFFitriani AlawiyahNo ratings yet
- EKG Self Study GuideDocument40 pagesEKG Self Study GuideArgee AlonsabeNo ratings yet
- Ecg PDFDocument87 pagesEcg PDFSabir KhanNo ratings yet
- Case Series: Radiofrequency Cathether Ablation of Atrioventricular Nodal Reentrant Tachycardia in OctogeneriansDocument5 pagesCase Series: Radiofrequency Cathether Ablation of Atrioventricular Nodal Reentrant Tachycardia in OctogeneriansAttilio Del RossoNo ratings yet
- Marathon-Related ECG ExasperationDocument24 pagesMarathon-Related ECG ExasperationmohamedsmnNo ratings yet
- Spring 2014 NewsletterDocument5 pagesSpring 2014 Newsletterapi-236445988No ratings yet
- EKG Interpretation: UNS Cardiovascular Dept Medical Student Lecture SeriesDocument85 pagesEKG Interpretation: UNS Cardiovascular Dept Medical Student Lecture Seriesandina rosmalianti100% (1)
- Case Presentation: DR - Ahmad Wali, Resident CardiologyDocument31 pagesCase Presentation: DR - Ahmad Wali, Resident CardiologyAhmad WaliNo ratings yet
- Ventricular Sense ResponseDocument3 pagesVentricular Sense ResponseDaniel Banina AguerreNo ratings yet
- (03241750 - Acta Medica Bulgarica) Multiple Congenital Heart AbnormalitiesDocument4 pages(03241750 - Acta Medica Bulgarica) Multiple Congenital Heart AbnormalitiesTeodorNo ratings yet
- Crite RiosDocument8 pagesCrite RiosNilson Morales CordobaNo ratings yet
- Chest PainDocument3 pagesChest PainDelia DeNo ratings yet
- Supraventricular Tachycardia - Life in The Fast Lane ECG LibraryDocument29 pagesSupraventricular Tachycardia - Life in The Fast Lane ECG LibraryYehuda Agus SantosoNo ratings yet
- TSV Con Aberrancia o TVDocument7 pagesTSV Con Aberrancia o TVOliverVasconcelosNo ratings yet
- Atrioventricular Nodal Reentrant Tachycardia With 21 Atrioventricular Block.Document5 pagesAtrioventricular Nodal Reentrant Tachycardia With 21 Atrioventricular Block.Raul OrtegaNo ratings yet
- P Wave AbnormalitiesDocument20 pagesP Wave AbnormalitiesToufiqurRahmanNo ratings yet
- Answer NDocument1 pageAnswer NJ tanieeNo ratings yet
- Common ECG With Management For Family Medicine ResidentsDocument19 pagesCommon ECG With Management For Family Medicine ResidentsdrhassanashrafeNo ratings yet
- Avnrt AvrtDocument21 pagesAvnrt AvrtRima Rovanne Wenas100% (1)
- ECG and ArrhythmiasDocument25 pagesECG and ArrhythmiasRashed ShatnawiNo ratings yet
- Tachycardia Approach and ManagementDocument41 pagesTachycardia Approach and ManagementChadi Alraies100% (5)
- Year 4 Clinical Pathophysiology Revision + ANSWERSDocument120 pagesYear 4 Clinical Pathophysiology Revision + ANSWERSChristopher TakiNo ratings yet
- ECG - Dilated HypertrophiedDocument19 pagesECG - Dilated Hypertrophiedyusuf fathoniNo ratings yet
- Jurnal Kampurui SiskawatiDocument6 pagesJurnal Kampurui SiskawatiTiansi Hidayati PakayaNo ratings yet
- FDA-Circular-2021-017 List of Class ADocument32 pagesFDA-Circular-2021-017 List of Class Ajennalyn miraflorNo ratings yet
- Thesis Topics On Total Knee ReplacementDocument5 pagesThesis Topics On Total Knee Replacementsheilaguyfargo100% (2)
- Ai Laboratory and Boarstud SectionDocument63 pagesAi Laboratory and Boarstud SectionrsuertoNo ratings yet
- Psy 1100 Signature Assignment 1Document4 pagesPsy 1100 Signature Assignment 1api-301742190No ratings yet
- Emotional Health BrochureDocument14 pagesEmotional Health Brochureapi-546569844No ratings yet
- FBS BASIC Participate in Workplace CommunicationDocument79 pagesFBS BASIC Participate in Workplace CommunicationCherry joy u BoteNo ratings yet
- Development of The Perceived Physical Literacy Que - 2023 - Journal of ExerciseDocument10 pagesDevelopment of The Perceived Physical Literacy Que - 2023 - Journal of ExerciseSherriNo ratings yet
- A Caregiver's Guide To Urinary Catheter - Jaga-MeDocument6 pagesA Caregiver's Guide To Urinary Catheter - Jaga-MeAMINo ratings yet
- Hygiene PolicyDocument4 pagesHygiene Policyprettyy chauhanNo ratings yet
- Raman 4 Cue CardDocument4 pagesRaman 4 Cue Cardprajapatiparth9011No ratings yet
- Industrial Ventilation and Heat StressDocument47 pagesIndustrial Ventilation and Heat StressbhargavNo ratings yet
- Design of Welding Armrest Based On Ergonomics AnalDocument6 pagesDesign of Welding Armrest Based On Ergonomics AnalgiaphubinhNo ratings yet
- None 7860047eDocument7 pagesNone 7860047esampoernadanjayaNo ratings yet
- Stress and Adaptation Crisis and Its InterventionDocument27 pagesStress and Adaptation Crisis and Its InterventionPuy Puy ChhangteNo ratings yet
- The Problem and Its BackgroundDocument12 pagesThe Problem and Its BackgroundRobinhood Jevons Martirez100% (1)
- Anger Management Workshop Group Counseling 4Document43 pagesAnger Management Workshop Group Counseling 4api-553169681No ratings yet
- GoutDocument6 pagesGoutNader Smadi100% (1)
- Knowledge of Mothers in Management of Diarrhea in Under-Five Children, in Kashan, IranDocument6 pagesKnowledge of Mothers in Management of Diarrhea in Under-Five Children, in Kashan, IrannurlainiNo ratings yet
- Uts ScriptDocument4 pagesUts ScriptErnest VincentNo ratings yet
- Miss Supranational Philippines 2023 Application FormDocument3 pagesMiss Supranational Philippines 2023 Application FormpaoloplopenioNo ratings yet
- Jacc HemodynamicsDocument12 pagesJacc HemodynamicsMZ FachriyanNo ratings yet
- Untitled Document CHAP 1-5 FINALDocument105 pagesUntitled Document CHAP 1-5 FINALDanica Kaye DavidNo ratings yet
- XII PRACTICAL EX ASSIGNMENT1 To XDocument26 pagesXII PRACTICAL EX ASSIGNMENT1 To XDhruv MirchandaniNo ratings yet
- "37 Secrets About Women and Sex": Part of The Outrageous Orgasms SeriesDocument16 pages"37 Secrets About Women and Sex": Part of The Outrageous Orgasms Seriesvigneshwaran sNo ratings yet
- Teaching Essay Writing To High School StudentsDocument8 pagesTeaching Essay Writing To High School Studentsafibavcbdyeqsx100% (2)
- EU Novel Food Regulation - DHA and EPA Ethyl Esters Oil From Schizochytrium Sp. MicroalgaDocument2 pagesEU Novel Food Regulation - DHA and EPA Ethyl Esters Oil From Schizochytrium Sp. MicroalgaDanielaLópezNo ratings yet