Professional Documents
Culture Documents
Clinical Supervision Artifact
Clinical Supervision Artifact
Uploaded by
api-645942287Copyright:
Available Formats
You might also like
- Fatty LiverDocument23 pagesFatty Liverbrijsing67% (3)
- PDP SRosaDocument2 pagesPDP SRosaSarah Ro SaNo ratings yet
- Concept of Faculty Supervisor (Dual) Position: SupervisionDocument6 pagesConcept of Faculty Supervisor (Dual) Position: SupervisionAru Verma100% (2)
- 52 Teen Boy Problems & How To Solve ThemDocument99 pages52 Teen Boy Problems & How To Solve ThemCristiano RochaNo ratings yet
- Functions of Pci in The Hospital SettingDocument4 pagesFunctions of Pci in The Hospital SettingJohn Michael Manlupig PitoyNo ratings yet
- Clinical Teaching MethodDocument16 pagesClinical Teaching Methodanjuhooda1987No ratings yet
- Purpose of Clinical TeachingDocument3 pagesPurpose of Clinical TeachingCharles kevin InesNo ratings yet
- Clinical Teaching PlanDocument5 pagesClinical Teaching Planapi-258524831No ratings yet
- Clinical TeachingDocument48 pagesClinical TeachingAmy Roc100% (3)
- Sample Teaching Philosphy StatementsDocument11 pagesSample Teaching Philosphy StatementsMufaro PfendeNo ratings yet
- SupervisorDocument16 pagesSupervisorshijoantonyNo ratings yet
- Teaching PhilosophyDocument9 pagesTeaching PhilosophyJairo EmarNo ratings yet
- Clinical TeachingDocument31 pagesClinical Teachingabcqwe123No ratings yet
- Womens PetDocument3 pagesWomens Petapi-307931906No ratings yet
- Concept of Faculty SupervisorDocument14 pagesConcept of Faculty SupervisorThilaga Ram0% (1)
- Clinical Teaching MethodDocument23 pagesClinical Teaching MethodRakesh ChoudhryNo ratings yet
- CHAPTER 1 Action ResearchDocument30 pagesCHAPTER 1 Action ResearchmatetbongNo ratings yet
- About Clinical Instructors Evaluating Nursing StudentsDocument22 pagesAbout Clinical Instructors Evaluating Nursing Studentsrex_tubana50% (2)
- Student Nurse CourseworkDocument4 pagesStudent Nurse Courseworkshvfihdjd100% (2)
- Clinical Teaching ProgrammeDocument28 pagesClinical Teaching ProgrammeLamnunnem HaokipNo ratings yet
- Teaching and Learning - Lesson 1Document81 pagesTeaching and Learning - Lesson 1Rtvc RoldanNo ratings yet
- ch1 Summative EvaluationDocument3 pagesch1 Summative Evaluationapi-740209346No ratings yet
- Narrative SummaryDocument5 pagesNarrative Summaryapi-458907281No ratings yet
- Nurse Educator Practicum - Reflective Journal 2Document4 pagesNurse Educator Practicum - Reflective Journal 2api-643881078No ratings yet
- The EssentialsDocument1 pageThe EssentialsWilliam OtienoNo ratings yet
- Learning Plan Nurs 2021Document8 pagesLearning Plan Nurs 2021api-258039684100% (1)
- An Assignment On: Concept of Faculty Supervisor (Dual Role) PositionDocument13 pagesAn Assignment On: Concept of Faculty Supervisor (Dual Role) Positionsoniya josephNo ratings yet
- Clinical Teaching: Health Education BSN-1BDocument25 pagesClinical Teaching: Health Education BSN-1Bmiles sbNo ratings yet
- Psycho Motor SkillsDocument9 pagesPsycho Motor Skillstimoetoamos123100% (1)
- Nurse Educator Practicum - Reflective Journal 4Document3 pagesNurse Educator Practicum - Reflective Journal 4api-643881078No ratings yet
- Nurse Educator Practicum - Reflective Journal 5Document3 pagesNurse Educator Practicum - Reflective Journal 5api-643881078No ratings yet
- Instant Download PDF Conceptual Foundations The Bridge To Professional Nursing Practice 6th Edition Friberg Test Bank Full ChapterDocument37 pagesInstant Download PDF Conceptual Foundations The Bridge To Professional Nursing Practice 6th Edition Friberg Test Bank Full Chapteronterokhawer100% (6)
- Supervision Final PaperDocument10 pagesSupervision Final Paperapi-626497212No ratings yet
- Teaching Philosophy Statement Example #1Document5 pagesTeaching Philosophy Statement Example #1Dilruk GallageNo ratings yet
- Md1projpt1 Cole KDocument13 pagesMd1projpt1 Cole Kapi-742831699No ratings yet
- Seminar On Concept of Faculty Supervisor Position in Nursing (Dual Role)Document8 pagesSeminar On Concept of Faculty Supervisor Position in Nursing (Dual Role)babyNo ratings yet
- Perspective On Teaching and LearningDocument43 pagesPerspective On Teaching and LearningJonalyn Cielito Francisco100% (2)
- Midpoint Analysis AssignmentDocument2 pagesMidpoint Analysis Assignmentapi-346051113No ratings yet
- Nurs 253 Preceptor Evaluation Forms - Den1Document8 pagesNurs 253 Preceptor Evaluation Forms - Den1api-284048628No ratings yet
- Preceptor GuidelinesDocument16 pagesPreceptor GuidelinesAryn Phillips100% (2)
- Nurse Educator Practicum - Reflective Journal 7Document3 pagesNurse Educator Practicum - Reflective Journal 7api-643881078No ratings yet
- Clinical Teaching SeminarDocument63 pagesClinical Teaching SeminarTilarupa Bhattarai100% (1)
- 261 Final EvaluationDocument9 pages261 Final Evaluationapi-283888852No ratings yet
- Nurse Educator Practicum III - Reflective Journal 2Document3 pagesNurse Educator Practicum III - Reflective Journal 2api-643881078No ratings yet
- TeachingphilosophyDocument3 pagesTeachingphilosophyapi-257281037No ratings yet
- Teaching and Learning at The BedsideDocument23 pagesTeaching and Learning at The BedsideJohn SummertonNo ratings yet
- PreceptorshipPurpose PDFDocument2 pagesPreceptorshipPurpose PDFsofieeeeNo ratings yet
- Concept of Faculty Supervisor (Dual) Role: Rajkumari Amrit Kaur College of Nursing Lajpat Nagar, New DelhiDocument8 pagesConcept of Faculty Supervisor (Dual) Role: Rajkumari Amrit Kaur College of Nursing Lajpat Nagar, New DelhiMallika JoonNo ratings yet
- Nurse Educator Practicum - Reflective Journal 6Document3 pagesNurse Educator Practicum - Reflective Journal 6api-643881078No ratings yet
- Final Evaluation Nurs1020Document4 pagesFinal Evaluation Nurs1020api-271855323No ratings yet
- NUR 420 Practicum Midterm Practicum Progress DocumentDocument9 pagesNUR 420 Practicum Midterm Practicum Progress DocumentBrooke GagnonNo ratings yet
- JOB DESCRIPTION OF NURSING TUTOR FinalDocument5 pagesJOB DESCRIPTION OF NURSING TUTOR FinalPatel Amee100% (4)
- Nursing Critical ThinkingDocument8 pagesNursing Critical ThinkingafmohuodeNo ratings yet
- My NLN CompetenciesDocument5 pagesMy NLN Competenciesapi-285244567No ratings yet
- Nurs 253 Student Self Evaluation-Oct23Document8 pagesNurs 253 Student Self Evaluation-Oct23api-283153412No ratings yet
- Nurs 253 Preceptor Feedback For Natasha SinghDocument8 pagesNurs 253 Preceptor Feedback For Natasha Singhapi-283970192No ratings yet
- Rodriguez Evaluation For e PortfolioDocument2 pagesRodriguez Evaluation For e Portfolioapi-739232245No ratings yet
- CONCEPT OF FACULTY SUPERVISOR POSITION IN NURSING - WordDocument8 pagesCONCEPT OF FACULTY SUPERVISOR POSITION IN NURSING - WordSMITHA JOSENo ratings yet
- Self-Designed Experience ProposalDocument8 pagesSelf-Designed Experience Proposalapi-300792588No ratings yet
- Preceptor Evaluation Form Docx CompleteDocument8 pagesPreceptor Evaluation Form Docx Completeapi-279007013No ratings yet
- Final GraphicalDocument5 pagesFinal Graphicalapi-645942287No ratings yet
- Act Cart InterventionDocument21 pagesAct Cart Interventionapi-645942287No ratings yet
- Mbs De-IdentifiedDocument2 pagesMbs De-Identifiedapi-645942287No ratings yet
- De-Identified StudentDocument4 pagesDe-Identified Studentapi-645942287No ratings yet
- Typhon Summary-Report-As of 12-16-2022Document22 pagesTyphon Summary-Report-As of 12-16-2022api-645942287No ratings yet
- Burnout Syndrome - Stress in Health Care Professionals Working To Fight Covid-19 in Public HospitalsDocument14 pagesBurnout Syndrome - Stress in Health Care Professionals Working To Fight Covid-19 in Public HospitalsIJAERS JOURNALNo ratings yet
- Hypoglycemia in NewbornDocument10 pagesHypoglycemia in Newbornmaxim tomuNo ratings yet
- Analisa Kuantitatif Dan Kualitatif Ketidaklengkapan Dokumen Rekam Medis Pada Pasien Typoid Di Rsud Kota Semarang Periode Triwulan I Tahun 2014Document10 pagesAnalisa Kuantitatif Dan Kualitatif Ketidaklengkapan Dokumen Rekam Medis Pada Pasien Typoid Di Rsud Kota Semarang Periode Triwulan I Tahun 2014uli shalatiyaNo ratings yet
- Metode PenelitianDocument10 pagesMetode PenelitianL KJNo ratings yet
- Effectiveness of Performance Appraisal System Towards "Dabur India LTD."Document85 pagesEffectiveness of Performance Appraisal System Towards "Dabur India LTD."Ashwani kumarNo ratings yet
- Nirapara Employee Job SatisfactionDocument62 pagesNirapara Employee Job SatisfactionRohit R Pillai50% (2)
- Psychological Adjustment.: in Context of WorkDocument40 pagesPsychological Adjustment.: in Context of Worktarun_sachdevaNo ratings yet
- "A Complete Health App": Designed by New HaircutDocument16 pages"A Complete Health App": Designed by New Haircutmonika sharmaNo ratings yet
- Karakteristik Stirred Yoghurt Mangga Mangifera IndDocument5 pagesKarakteristik Stirred Yoghurt Mangga Mangifera IndAdhy HitachiNo ratings yet
- Tat Hui Foods Pte LTDDocument9 pagesTat Hui Foods Pte LTDSanjoy HasdaNo ratings yet
- CLINICAL GUIDELINES FOR COVID IN MALAYSIA 3rd EDITIONDocument151 pagesCLINICAL GUIDELINES FOR COVID IN MALAYSIA 3rd EDITIONIshak AliNo ratings yet
- Consensus Statement On Vitamin D Status Assessment and Supplementation Whys, Whens, and HowsDocument30 pagesConsensus Statement On Vitamin D Status Assessment and Supplementation Whys, Whens, and HowsChanukya GvNo ratings yet
- Fever of Unknown OriginDocument22 pagesFever of Unknown OriginDonzzkie DonNo ratings yet
- Antimicrobial DrugsDocument24 pagesAntimicrobial DrugsMuh Akbar BaharNo ratings yet
- Cariogram E BookDocument90 pagesCariogram E Bookovy primaNo ratings yet
- Social Work With Drug and Substance Misusers (Transforming Social Work Practice), 2nd Edition - PDF RoomDocument161 pagesSocial Work With Drug and Substance Misusers (Transforming Social Work Practice), 2nd Edition - PDF RoomLe mittzNo ratings yet
- Makita DUR369AZDocument160 pagesMakita DUR369AZAnonymous 4fOfUqNo ratings yet
- CorrosivesDocument25 pagesCorrosivesahmed.farag.ali2020No ratings yet
- Evidence Based Validation of Traditional Medicines 2021Document1,135 pagesEvidence Based Validation of Traditional Medicines 2021shubham panditNo ratings yet
- Key Contacts - Coordination SheetDocument13 pagesKey Contacts - Coordination SheetSoumya RengarajanNo ratings yet
- Second SOC of Guimaras Province (20181205) Smaller Opt PDFDocument226 pagesSecond SOC of Guimaras Province (20181205) Smaller Opt PDFChrister John UyNo ratings yet
- Trial Title: Protocol NumberDocument22 pagesTrial Title: Protocol NumberMilan StojanovićNo ratings yet
- Preprint Not Peer ReviewedDocument9 pagesPreprint Not Peer ReviewedpatrickNo ratings yet
- Coshh Assessment FormDocument6 pagesCoshh Assessment FormAfaan gani InamdarNo ratings yet
- Evaluation of Solid Waste Generation, Categories and Disposal Options in Developing Countries: A Case Study of Nigeria Babayemi, J. O. Dauda, K. TDocument6 pagesEvaluation of Solid Waste Generation, Categories and Disposal Options in Developing Countries: A Case Study of Nigeria Babayemi, J. O. Dauda, K. Trudy yoga lesmanaNo ratings yet
- NatamycinDocument10 pagesNatamycinedwarhannaNo ratings yet
- PHIN Laboratory Result ELR v231Document86 pagesPHIN Laboratory Result ELR v231anujaks_rlbNo ratings yet
- Principle of Good Clinical PracticeDocument39 pagesPrinciple of Good Clinical PracticeVasavi ChittemreddyNo ratings yet
Clinical Supervision Artifact
Clinical Supervision Artifact
Uploaded by
api-645942287Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Supervision Artifact
Clinical Supervision Artifact
Uploaded by
api-645942287Copyright:
Available Formats
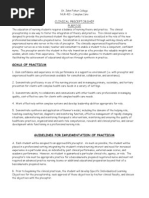
Patrick Massey
Clinical Supervision Artifact
Clinical Supervision
1. List some roles of the clinical supervisor
a. The model for clinical skills based in evidence-based prac:ces.
b. A resource for clinical inquiries
c. A support system for failures and success
d. A guide for professional development
e. A teacher, a mentor, and eventually a peer
2. Why do very busy supervisors with heavy caseloads agree to supervise student
clinicians?
a. This ques:on could have a very personal answer and could be highly dependent
on the disposi:on of the supervisor. The field is in need of SLPs that can work in
demanding heavy caseload environments. It is a service to the field to immerse
students in real world scenarios where they have to face clinical decisions on
how not just to serve all of the clients, but how to serve all clients op#mally. This
may allow a student to see how group interven:ons may be organized and run or
how to iden:fy clients that need one on one sessions. These are clinical decisions
that are not present in our normal University environment and are key learning
opportuni:es to prepare future clinicians for real world scenarios.
b. It is common knowledge that in order to teach or supervise others well one
needs to have their own mastery of content and clinical prac:ce. Supervision is
an opportunity to reinforce best prac:ces in the supervising clinician as well.
c. While this should not be the main mo:va:ng factor to take on students for
supervision, it could provide extra support for the clinician. Caseloads can be
exorbitant, especially in the school seMng. Once a student clinician has gained
more competence and confidence, they should be able to take on more of the
load which could provide extra support for the supervising clinician. With high
caseloads comes more IEPs and increased paperwork. While a student should
never be a replacement for a clinician’s work, once the student is opera:ng more
independently it may relieve some pressure on the supervising clinician that may
allow them to accomplish more work. The caveat here is that supervision should
never be compromised in order to accomplish more work.
3. What are the goals of high-quality supervision?
a. ASHA iden:fies several target goals of clinical supervision
i. Teaching students how to apply academic knowledge in a clinical seMng
ii. Progressing and sequencing a student’s development in an appropriate
way
iii. Crea:ng an environment that allows the student to learn, ask ques:ons,
and engage in difficult clinical conversa:ons
iv. Reinforcing evidence-based founda:ons as a guide for clinical decisions
v. Helping students develop documenta:on competencies with medical
billing, note wri:ng, goal-wri:ng and progress monitoring.
vi. Providing objec:ve feedback to equip a student with prac:cal changes
vii. Iden:fying areas of improvement for the student and providing feedback
in a safe and professional manner.
viii. Encouraging professional communica:on and rela:onship building skills
within the clinical and professional seMng.
ix. Foster personal, clinical, and professional growth of the student
x. Ul:mately, the goal of high-quality supervision is to support a student’s
educa:on and clinical experience with evidence-based founda:ons
through hands on experience that allows the student to gain confidence
and competence in assessments and therapies in a real-world context
with real-:me feedback from a competent clinical professional who is
invested in the growth and development of their student clinicians.
4. What is ASHA’s recommended percentage of supervision :me?
a. 25% of a student’s total contact with a client at a minimum
b. JMU’s recommended percentage is also a minimum of 25% of total client contact
according to the handbook.
5. What clinical services count as hours?
a. Hours must be direct contact with the client or family either in assessment,
therapy, counseling, or management. Documenta:on hours do not count toward
clinical hours.
6. What are the student clinician’s final achievement goals for clinical competency?
a. For JMU it is expected that the student achieved a skill level of Refining or
Independent in the nine disorder areas of prac:ce. The student must also
complete 400 clinical hours (375 direct pa:ent contact + 25 observa:on).
Pending on the placement there may be extra site-specific competencies or
presenta:ons required.
b. Students must also demonstrate competencies in various professional and
clinical skills such as professionalism, assessment and interven:on skills,
documenta:on, progress monitoring, planning, etc
7. What supervisor supports/behaviors have you found helpful this year?
a. I have found it very helpful when a supervisor engages with my clinical ques:ons
and tries to understand the intent of my ques:on. I also have appreciated when
supervisors have asked where I am struggling and have catered feedback to my
own goals. I have found it very helpful when supervisors acknowledge clinical
competence and engage with the material which helps me reinforce what I do
know and helps me to focus more on what I do not yet know.
8. Where do you think you fall on Anderson’s Con:nuum of Clinical Compentency?
a. As a student I believe I fall close to the self-supervision stage. I feel like I have the
founda:ons and skills to address novel:es in my field, but s:ll feel like I need to
confirm somewhat infrequently with a supervisor to make sure I’m on the right
track and make sure I am doing right by my pa:ent. This may all completely
change if my clientele and work seMng ends up being different from my previous
experiences.
b. As a supervisor, I would love to respond to my student according to their needs.
Everyone responds differently to different teaching styles and modali:es of
feedback. Some need more encouragement and guidance and others may
appreciate more independence. If they need a more direc:ve style, I will gladly
provide that. Ideally, I would like to start in the transi:onal/collabora:ve stage. I
personally learn a lot when I have a chance to fail, but failing with support. I hope
to assume competence in my students and help them find the resources to
problem solve as they would in the real world. I would hope get input from the
student about when they feel like they are at the self-supervision stage
understanding that my opinion may differ from my student on that :ming. Most
importantly I would like to provide an environment where the pa:ent feels safe
to make mistakes, feels encouraged, and is able to bring their personality and
strengths to the table.
You might also like
- Fatty LiverDocument23 pagesFatty Liverbrijsing67% (3)
- PDP SRosaDocument2 pagesPDP SRosaSarah Ro SaNo ratings yet
- Concept of Faculty Supervisor (Dual) Position: SupervisionDocument6 pagesConcept of Faculty Supervisor (Dual) Position: SupervisionAru Verma100% (2)
- 52 Teen Boy Problems & How To Solve ThemDocument99 pages52 Teen Boy Problems & How To Solve ThemCristiano RochaNo ratings yet
- Functions of Pci in The Hospital SettingDocument4 pagesFunctions of Pci in The Hospital SettingJohn Michael Manlupig PitoyNo ratings yet
- Clinical Teaching MethodDocument16 pagesClinical Teaching Methodanjuhooda1987No ratings yet
- Purpose of Clinical TeachingDocument3 pagesPurpose of Clinical TeachingCharles kevin InesNo ratings yet
- Clinical Teaching PlanDocument5 pagesClinical Teaching Planapi-258524831No ratings yet
- Clinical TeachingDocument48 pagesClinical TeachingAmy Roc100% (3)
- Sample Teaching Philosphy StatementsDocument11 pagesSample Teaching Philosphy StatementsMufaro PfendeNo ratings yet
- SupervisorDocument16 pagesSupervisorshijoantonyNo ratings yet
- Teaching PhilosophyDocument9 pagesTeaching PhilosophyJairo EmarNo ratings yet
- Clinical TeachingDocument31 pagesClinical Teachingabcqwe123No ratings yet
- Womens PetDocument3 pagesWomens Petapi-307931906No ratings yet
- Concept of Faculty SupervisorDocument14 pagesConcept of Faculty SupervisorThilaga Ram0% (1)
- Clinical Teaching MethodDocument23 pagesClinical Teaching MethodRakesh ChoudhryNo ratings yet
- CHAPTER 1 Action ResearchDocument30 pagesCHAPTER 1 Action ResearchmatetbongNo ratings yet
- About Clinical Instructors Evaluating Nursing StudentsDocument22 pagesAbout Clinical Instructors Evaluating Nursing Studentsrex_tubana50% (2)
- Student Nurse CourseworkDocument4 pagesStudent Nurse Courseworkshvfihdjd100% (2)
- Clinical Teaching ProgrammeDocument28 pagesClinical Teaching ProgrammeLamnunnem HaokipNo ratings yet
- Teaching and Learning - Lesson 1Document81 pagesTeaching and Learning - Lesson 1Rtvc RoldanNo ratings yet
- ch1 Summative EvaluationDocument3 pagesch1 Summative Evaluationapi-740209346No ratings yet
- Narrative SummaryDocument5 pagesNarrative Summaryapi-458907281No ratings yet
- Nurse Educator Practicum - Reflective Journal 2Document4 pagesNurse Educator Practicum - Reflective Journal 2api-643881078No ratings yet
- The EssentialsDocument1 pageThe EssentialsWilliam OtienoNo ratings yet
- Learning Plan Nurs 2021Document8 pagesLearning Plan Nurs 2021api-258039684100% (1)
- An Assignment On: Concept of Faculty Supervisor (Dual Role) PositionDocument13 pagesAn Assignment On: Concept of Faculty Supervisor (Dual Role) Positionsoniya josephNo ratings yet
- Clinical Teaching: Health Education BSN-1BDocument25 pagesClinical Teaching: Health Education BSN-1Bmiles sbNo ratings yet
- Psycho Motor SkillsDocument9 pagesPsycho Motor Skillstimoetoamos123100% (1)
- Nurse Educator Practicum - Reflective Journal 4Document3 pagesNurse Educator Practicum - Reflective Journal 4api-643881078No ratings yet
- Nurse Educator Practicum - Reflective Journal 5Document3 pagesNurse Educator Practicum - Reflective Journal 5api-643881078No ratings yet
- Instant Download PDF Conceptual Foundations The Bridge To Professional Nursing Practice 6th Edition Friberg Test Bank Full ChapterDocument37 pagesInstant Download PDF Conceptual Foundations The Bridge To Professional Nursing Practice 6th Edition Friberg Test Bank Full Chapteronterokhawer100% (6)
- Supervision Final PaperDocument10 pagesSupervision Final Paperapi-626497212No ratings yet
- Teaching Philosophy Statement Example #1Document5 pagesTeaching Philosophy Statement Example #1Dilruk GallageNo ratings yet
- Md1projpt1 Cole KDocument13 pagesMd1projpt1 Cole Kapi-742831699No ratings yet
- Seminar On Concept of Faculty Supervisor Position in Nursing (Dual Role)Document8 pagesSeminar On Concept of Faculty Supervisor Position in Nursing (Dual Role)babyNo ratings yet
- Perspective On Teaching and LearningDocument43 pagesPerspective On Teaching and LearningJonalyn Cielito Francisco100% (2)
- Midpoint Analysis AssignmentDocument2 pagesMidpoint Analysis Assignmentapi-346051113No ratings yet
- Nurs 253 Preceptor Evaluation Forms - Den1Document8 pagesNurs 253 Preceptor Evaluation Forms - Den1api-284048628No ratings yet
- Preceptor GuidelinesDocument16 pagesPreceptor GuidelinesAryn Phillips100% (2)
- Nurse Educator Practicum - Reflective Journal 7Document3 pagesNurse Educator Practicum - Reflective Journal 7api-643881078No ratings yet
- Clinical Teaching SeminarDocument63 pagesClinical Teaching SeminarTilarupa Bhattarai100% (1)
- 261 Final EvaluationDocument9 pages261 Final Evaluationapi-283888852No ratings yet
- Nurse Educator Practicum III - Reflective Journal 2Document3 pagesNurse Educator Practicum III - Reflective Journal 2api-643881078No ratings yet
- TeachingphilosophyDocument3 pagesTeachingphilosophyapi-257281037No ratings yet
- Teaching and Learning at The BedsideDocument23 pagesTeaching and Learning at The BedsideJohn SummertonNo ratings yet
- PreceptorshipPurpose PDFDocument2 pagesPreceptorshipPurpose PDFsofieeeeNo ratings yet
- Concept of Faculty Supervisor (Dual) Role: Rajkumari Amrit Kaur College of Nursing Lajpat Nagar, New DelhiDocument8 pagesConcept of Faculty Supervisor (Dual) Role: Rajkumari Amrit Kaur College of Nursing Lajpat Nagar, New DelhiMallika JoonNo ratings yet
- Nurse Educator Practicum - Reflective Journal 6Document3 pagesNurse Educator Practicum - Reflective Journal 6api-643881078No ratings yet
- Final Evaluation Nurs1020Document4 pagesFinal Evaluation Nurs1020api-271855323No ratings yet
- NUR 420 Practicum Midterm Practicum Progress DocumentDocument9 pagesNUR 420 Practicum Midterm Practicum Progress DocumentBrooke GagnonNo ratings yet
- JOB DESCRIPTION OF NURSING TUTOR FinalDocument5 pagesJOB DESCRIPTION OF NURSING TUTOR FinalPatel Amee100% (4)
- Nursing Critical ThinkingDocument8 pagesNursing Critical ThinkingafmohuodeNo ratings yet
- My NLN CompetenciesDocument5 pagesMy NLN Competenciesapi-285244567No ratings yet
- Nurs 253 Student Self Evaluation-Oct23Document8 pagesNurs 253 Student Self Evaluation-Oct23api-283153412No ratings yet
- Nurs 253 Preceptor Feedback For Natasha SinghDocument8 pagesNurs 253 Preceptor Feedback For Natasha Singhapi-283970192No ratings yet
- Rodriguez Evaluation For e PortfolioDocument2 pagesRodriguez Evaluation For e Portfolioapi-739232245No ratings yet
- CONCEPT OF FACULTY SUPERVISOR POSITION IN NURSING - WordDocument8 pagesCONCEPT OF FACULTY SUPERVISOR POSITION IN NURSING - WordSMITHA JOSENo ratings yet
- Self-Designed Experience ProposalDocument8 pagesSelf-Designed Experience Proposalapi-300792588No ratings yet
- Preceptor Evaluation Form Docx CompleteDocument8 pagesPreceptor Evaluation Form Docx Completeapi-279007013No ratings yet
- Final GraphicalDocument5 pagesFinal Graphicalapi-645942287No ratings yet
- Act Cart InterventionDocument21 pagesAct Cart Interventionapi-645942287No ratings yet
- Mbs De-IdentifiedDocument2 pagesMbs De-Identifiedapi-645942287No ratings yet
- De-Identified StudentDocument4 pagesDe-Identified Studentapi-645942287No ratings yet
- Typhon Summary-Report-As of 12-16-2022Document22 pagesTyphon Summary-Report-As of 12-16-2022api-645942287No ratings yet
- Burnout Syndrome - Stress in Health Care Professionals Working To Fight Covid-19 in Public HospitalsDocument14 pagesBurnout Syndrome - Stress in Health Care Professionals Working To Fight Covid-19 in Public HospitalsIJAERS JOURNALNo ratings yet
- Hypoglycemia in NewbornDocument10 pagesHypoglycemia in Newbornmaxim tomuNo ratings yet
- Analisa Kuantitatif Dan Kualitatif Ketidaklengkapan Dokumen Rekam Medis Pada Pasien Typoid Di Rsud Kota Semarang Periode Triwulan I Tahun 2014Document10 pagesAnalisa Kuantitatif Dan Kualitatif Ketidaklengkapan Dokumen Rekam Medis Pada Pasien Typoid Di Rsud Kota Semarang Periode Triwulan I Tahun 2014uli shalatiyaNo ratings yet
- Metode PenelitianDocument10 pagesMetode PenelitianL KJNo ratings yet
- Effectiveness of Performance Appraisal System Towards "Dabur India LTD."Document85 pagesEffectiveness of Performance Appraisal System Towards "Dabur India LTD."Ashwani kumarNo ratings yet
- Nirapara Employee Job SatisfactionDocument62 pagesNirapara Employee Job SatisfactionRohit R Pillai50% (2)
- Psychological Adjustment.: in Context of WorkDocument40 pagesPsychological Adjustment.: in Context of Worktarun_sachdevaNo ratings yet
- "A Complete Health App": Designed by New HaircutDocument16 pages"A Complete Health App": Designed by New Haircutmonika sharmaNo ratings yet
- Karakteristik Stirred Yoghurt Mangga Mangifera IndDocument5 pagesKarakteristik Stirred Yoghurt Mangga Mangifera IndAdhy HitachiNo ratings yet
- Tat Hui Foods Pte LTDDocument9 pagesTat Hui Foods Pte LTDSanjoy HasdaNo ratings yet
- CLINICAL GUIDELINES FOR COVID IN MALAYSIA 3rd EDITIONDocument151 pagesCLINICAL GUIDELINES FOR COVID IN MALAYSIA 3rd EDITIONIshak AliNo ratings yet
- Consensus Statement On Vitamin D Status Assessment and Supplementation Whys, Whens, and HowsDocument30 pagesConsensus Statement On Vitamin D Status Assessment and Supplementation Whys, Whens, and HowsChanukya GvNo ratings yet
- Fever of Unknown OriginDocument22 pagesFever of Unknown OriginDonzzkie DonNo ratings yet
- Antimicrobial DrugsDocument24 pagesAntimicrobial DrugsMuh Akbar BaharNo ratings yet
- Cariogram E BookDocument90 pagesCariogram E Bookovy primaNo ratings yet
- Social Work With Drug and Substance Misusers (Transforming Social Work Practice), 2nd Edition - PDF RoomDocument161 pagesSocial Work With Drug and Substance Misusers (Transforming Social Work Practice), 2nd Edition - PDF RoomLe mittzNo ratings yet
- Makita DUR369AZDocument160 pagesMakita DUR369AZAnonymous 4fOfUqNo ratings yet
- CorrosivesDocument25 pagesCorrosivesahmed.farag.ali2020No ratings yet
- Evidence Based Validation of Traditional Medicines 2021Document1,135 pagesEvidence Based Validation of Traditional Medicines 2021shubham panditNo ratings yet
- Key Contacts - Coordination SheetDocument13 pagesKey Contacts - Coordination SheetSoumya RengarajanNo ratings yet
- Second SOC of Guimaras Province (20181205) Smaller Opt PDFDocument226 pagesSecond SOC of Guimaras Province (20181205) Smaller Opt PDFChrister John UyNo ratings yet
- Trial Title: Protocol NumberDocument22 pagesTrial Title: Protocol NumberMilan StojanovićNo ratings yet
- Preprint Not Peer ReviewedDocument9 pagesPreprint Not Peer ReviewedpatrickNo ratings yet
- Coshh Assessment FormDocument6 pagesCoshh Assessment FormAfaan gani InamdarNo ratings yet
- Evaluation of Solid Waste Generation, Categories and Disposal Options in Developing Countries: A Case Study of Nigeria Babayemi, J. O. Dauda, K. TDocument6 pagesEvaluation of Solid Waste Generation, Categories and Disposal Options in Developing Countries: A Case Study of Nigeria Babayemi, J. O. Dauda, K. Trudy yoga lesmanaNo ratings yet
- NatamycinDocument10 pagesNatamycinedwarhannaNo ratings yet
- PHIN Laboratory Result ELR v231Document86 pagesPHIN Laboratory Result ELR v231anujaks_rlbNo ratings yet
- Principle of Good Clinical PracticeDocument39 pagesPrinciple of Good Clinical PracticeVasavi ChittemreddyNo ratings yet