Professional Documents
Culture Documents
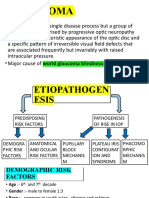
Glaucoma
Glaucoma
Uploaded by
shakyaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Glaucoma
Glaucoma
Uploaded by
shakyaCopyright:
Available Formats
INTRAOCULAR PRESSURE
NORMAL 14-21 mmHg GLAUCOMA
AG
But
Progressive optic neuropathy,
Normal Tension Glaucoma, Ocular with characteristic field defects,
Hypertension, Central Corneal Thickness, most commonly caused by
increased IOP.
Contact tonometry v. non-contact
VISUAL FIELDS
OPTIC DISC CUPPING
Arcuate scotomas, nasal steps, temporal
wedges, paracentral scotomas, NORMAL < 0.5
But
But
Steep learning curve, VA needs to be good, Physiological cupping, Look for symmetry,
rim thickness, ISNT rule, myopes ,
false negatives +positives, fixation losses
tilted discs
DIAGNOSTIC NIGHTMARE!
Complex disease process. IOP and vascular components
Risk Factors: Increasing Age, Race (African-Caribbean more frequent, younger, worse), Family History, NTG more
common with migraine, Raynaud’s, Japanese
Other glaucomas are available! Secondary glaucoma, Pigment dispersion, PXE, Trauma, Congenital malformations,
Rubeosis, Uveitis, Steroid responders, Acute angle closure glaucoma, Chronic angle closure glaucoma…..
TREATMENT
Aim to reduce IOP. Not to cure but to slow down progress. Treat OHT if IOP 28+ as increased risk of POAG
Medical Treatment: prostaglandin analogue, beta blockers, alpha agonists, carbonic anhydrase inhibitors
Laser or surgery: ALT, Trabeculectomy, Tube/shunt procedure
Anne Gobbett 2019 SEI
You might also like
- Hereditary Vitreoretinal DegenerationsDocument11 pagesHereditary Vitreoretinal DegenerationsImtiaz AhmedNo ratings yet
- Papiledema 3Document27 pagesPapiledema 3nellieauthorNo ratings yet
- Glaucoma: DR - Fitratul Ilahi, SPM (K)Document47 pagesGlaucoma: DR - Fitratul Ilahi, SPM (K)nurul ramadhiniNo ratings yet
- Tugas Baca Poag Aao SDDocument36 pagesTugas Baca Poag Aao SDdokumen kuNo ratings yet
- KP 3.4.1.5 Glaukoma 1Document37 pagesKP 3.4.1.5 Glaukoma 1kelsy qoridisa100% (1)
- Globe PathologyDocument13 pagesGlobe PathologyAli 10No ratings yet
- Glaucoma: DR - Yulia Wardany SP.M KJF Ilmu Penyakit MataDocument51 pagesGlaucoma: DR - Yulia Wardany SP.M KJF Ilmu Penyakit MataKwan SiliaNo ratings yet
- Glaucoma: Camille N. LibrandaDocument35 pagesGlaucoma: Camille N. LibrandaCamilleNo ratings yet
- Primary Angle Closure GlaucomaDocument18 pagesPrimary Angle Closure GlaucomaRakshit AgrawalNo ratings yet
- Ophthalmology - GlaucomaDocument13 pagesOphthalmology - GlaucomajbtcmdtjjvNo ratings yet
- Glaukoma Bsolut: Pembimbing: Dr. Anny S., SPMDocument35 pagesGlaukoma Bsolut: Pembimbing: Dr. Anny S., SPMRahma AmaliaNo ratings yet
- Eye 3Document4 pagesEye 3Nadia AbdurasidNo ratings yet
- A Comparison of OpenDocument3 pagesA Comparison of OpenratnafadliNo ratings yet
- Rana Greene Hypertensive IritisDocument34 pagesRana Greene Hypertensive IritisGG INo ratings yet
- Optic Nerve Tumours: Presenter-Dr Adheela Abdulla Moderator - DR Shikha BassiDocument54 pagesOptic Nerve Tumours: Presenter-Dr Adheela Abdulla Moderator - DR Shikha BassiMohammed Jazeel 2549No ratings yet
- Angle Closure GlaucomaDocument21 pagesAngle Closure Glaucomasri sinagaNo ratings yet
- Jurnal Glaukoma EngDocument50 pagesJurnal Glaukoma EngYemimaNo ratings yet
- Ophtha ReviewerDocument3 pagesOphtha ReviewerToni Sy EncinaresNo ratings yet
- Glukoma Primery CareDocument8 pagesGlukoma Primery CareSyarief NurseNo ratings yet
- GlaucomaDocument41 pagesGlaucomaNanda SapitriNo ratings yet
- Bryant's PamphletDocument1 pageBryant's PamphletRenz Bryant BalantadNo ratings yet
- Glaukoma: Dr. Efhandi Nukman SPMDocument56 pagesGlaukoma: Dr. Efhandi Nukman SPMRaja Aulia IndtianyNo ratings yet
- Glaucoma and LensDocument4 pagesGlaucoma and Lenssarguss14No ratings yet
- (Ophtha) Ocular Emergencies .PenguinDocument7 pages(Ophtha) Ocular Emergencies .PenguinPatricia ManaliliNo ratings yet
- GlaucomaDocument23 pagesGlaucomasanjivdas100% (2)
- GlaucomaDocument37 pagesGlaucomaEINSTEIN2DNo ratings yet
- GlaucomaDocument5 pagesGlaucomaSudhanshu RajputNo ratings yet
- Ocular Ischemic Syndrome by Dr. Ruksana PDFDocument18 pagesOcular Ischemic Syndrome by Dr. Ruksana PDFsyntacs skNo ratings yet
- Glaucoma PDFDocument42 pagesGlaucoma PDFapi-3740162No ratings yet
- Dr. Md. Yeamli Khan: Mbbs (Dhaka) Do (Du) Fcps (Ophth)Document50 pagesDr. Md. Yeamli Khan: Mbbs (Dhaka) Do (Du) Fcps (Ophth)Kawshik SahaNo ratings yet
- Ocular Emergencies TraumaDocument35 pagesOcular Emergencies TraumaMochaLover100% (2)
- Artigo Management of Ectopia - Neely - 2001Document7 pagesArtigo Management of Ectopia - Neely - 2001Giovanna SoaresNo ratings yet
- Ophthalmology - Optics and RefractionDocument10 pagesOphthalmology - Optics and RefractionjbtcmdtjjvNo ratings yet
- Occular EmergenciesDocument2 pagesOccular EmergenciesAlina PunNo ratings yet
- Vision Impairment 1Document59 pagesVision Impairment 1122ritik goyalNo ratings yet
- GLAUCOMA (Class 7) : Faculty Name Institute NameDocument32 pagesGLAUCOMA (Class 7) : Faculty Name Institute NamePranshu Prajyot 67No ratings yet
- About The Authors: Lai Ling TanDocument12 pagesAbout The Authors: Lai Ling TanStrawberry ShortcakeNo ratings yet
- Vision Disorders - Indd - OsmosisDocument6 pagesVision Disorders - Indd - OsmosisRishi Raj NRNo ratings yet
- Vision DisordersDocument6 pagesVision Disordersgamal attamNo ratings yet
- Geriputri, DR., SP.M: Fakultas Kedokteran Universitas MataramDocument51 pagesGeriputri, DR., SP.M: Fakultas Kedokteran Universitas Mataramzihniyya471No ratings yet
- GLAUCOMADocument7 pagesGLAUCOMAAndrea TamundongNo ratings yet
- Visual Acuity Examination For MNUMS 5th Course StudentsDocument14 pagesVisual Acuity Examination For MNUMS 5th Course Studentsbyambadorj.mbNo ratings yet
- Cataract and PACGDocument26 pagesCataract and PACGR.m. AndriyanNo ratings yet
- GlaucomaDocument28 pagesGlaucomaSarah RahmawatiNo ratings yet
- GLAUKOMADocument47 pagesGLAUKOMARahma GhnNo ratings yet
- Perimetry Aioc 2023Document17 pagesPerimetry Aioc 2023neha midhaNo ratings yet
- Glaucoma: Direct Mechanical Theory - Suggests That HighDocument4 pagesGlaucoma: Direct Mechanical Theory - Suggests That HighMarissa AsimNo ratings yet
- The Acute Painful Red Eye: History of Presenting Complaint - The Time and Speed of OnsetDocument4 pagesThe Acute Painful Red Eye: History of Presenting Complaint - The Time and Speed of Onsetleigh_zaliNo ratings yet
- Ischemic Optic NeuropathyDocument52 pagesIschemic Optic NeuropathySriniwasNo ratings yet
- Pathological MyopiaDocument58 pagesPathological MyopiaMohammad Abdullah BawtagNo ratings yet
- GlaucomaDocument17 pagesGlaucomaSanchi tNo ratings yet
- UveitisDocument1 pageUveitiskaisersosseNo ratings yet
- 2017-09-14 DiopsysDocument37 pages2017-09-14 DiopsyssalsomanoNo ratings yet
- OPTIC NEURITISDocument3 pagesOPTIC NEURITISshreyan.daniNo ratings yet
- Poag UgDocument18 pagesPoag UgSanjeev KrishnanNo ratings yet
- GlaucomaDocument25 pagesGlaucomaAjit ThangeNo ratings yet
- 86 Normal Low Tension Glaucoma PDFDocument4 pages86 Normal Low Tension Glaucoma PDFpoetraNo ratings yet
- 30secondary GlaucomasDocument19 pages30secondary GlaucomasShari' Si WahyuNo ratings yet
- Drug Calculation Exercises Workbook - Student Copy (Campus Week 2)Document15 pagesDrug Calculation Exercises Workbook - Student Copy (Campus Week 2)shakyaNo ratings yet
- Cell Injury and Cell Death HandoutDocument13 pagesCell Injury and Cell Death HandoutshakyaNo ratings yet
- Direct OphthalmosDocument1 pageDirect OphthalmosshakyaNo ratings yet
- Diabetic RetinopathyDocument1 pageDiabetic RetinopathyshakyaNo ratings yet
- Atrial FibrillationDocument1 pageAtrial FibrillationshakyaNo ratings yet
- AuditDocument4 pagesAuditshakyaNo ratings yet