Professional Documents
Culture Documents
Augmentative and Alternative Communication: Clinical Guideline
Augmentative and Alternative Communication: Clinical Guideline
Uploaded by
Bethany KeilyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Augmentative and Alternative Communication: Clinical Guideline
Augmentative and Alternative Communication: Clinical Guideline
Uploaded by
Bethany KeilyCopyright:
Available Formats
Speech Pathology Australia
Clinical
Guideline
Augmentative and Alternative Communication
Copyright 2012 The Speech Pathology Association of Australia Limited
Disclaimer: To the best of The Speech Pathology Association of Australia Limited’s ("the
Association") knowledge, this information is valid at the time of publication. The Association
makes no warranty or representation in relation to the content or accuracy of the material in
this publication. The Association expressly disclaims any and all liability (including liability for
negligence) in respect of use of the information provided. The Association recommends you
seek independent professional advice prior to making any decision involving matters outlined
in this publication.
Level 2 / 11-19 Bank Place T 61 3 9642 4899 office@speechpathologyaustralia.org.au
Melbourne Victoria 3000 F 61 3 9642 4922 www.speechpathologyaustralia.org.au
Speech Pathology Australia
ACKNOWLEDGEMENTS
This clinical guideline was developed by a dedicated team of experts in the field of
Augmentative and Alternative Communication (AAC). The development of this guideline has
been supported by the valuable contributions of clinical researchers and teachers in the field
of AAC, people who use AAC, representatives of national associations for AAC in Australia,
industry members, international researchers in the field of AAC, and academics in AAC,
speech pathology, special education, psychology, and occupational therapy.
To cite this document:
Speech Pathology Australia (2012). Augmentative and Alternative Communication Clinical
Guideline. Melbourne: Speech Pathology Australia.
Level 2 / 11-19 Bank Place T 61 3 9642 4899 office@speechpathologyaustralia.org.au
Melbourne Victoria 3000 F 61 3 9642 4922 www.speechpathologyaustralia.org.au
Speech Pathology Australia
CONTENTS
ACKNOWLEDGEMENTS ........................................................................................................ 2
SUMMARY .............................................................................................................................. 5
GLOSSARY OF TERMS.......................................................................................................... 6
1. Origins of the Paper ........................................................................................................ 11
2. Overview and Purpose .................................................................................................... 11
3. Introduction ..................................................................................................................... 11
4. Origins and Aims of AAC................................................................................................. 13
5. Client Group .................................................................................................................... 13
6. Research ......................................................................................................................... 14
6.1 Evidence Based Practice .......................................................................................... 14
6.2 Evaluating the Evidence for AAC .............................................................................. 15
6.3 Service Delivery in AAC ............................................................................................ 16
7. Principles in AAC Services .............................................................................................. 16
8. Leadership, Supervision, and Mentoring ......................................................................... 18
9. Legal Issues .................................................................................................................... 18
9.1 Code of ethics ........................................................................................................... 19
9.2 Legislation ................................................................................................................ 19
9.3 Duty of care .............................................................................................................. 19
9.4 ‘Proxy’ interventions .................................................................................................. 19
9.5 Consent for speech pathology involvement .............................................................. 19
9.6 Indemnity Cover and Insurance ................................................................................ 20
9.7 Service guidelines..................................................................................................... 20
9.8 AAC Specific Issues ................................................................................................. 20
10. Education and Training ................................................................................................ 22
11. Assessment ................................................................................................................. 23
11.1 Feature Matching in AAC Assessment .................................................................. 24
12. Intervention .................................................................................................................. 25
12.1 Rationale ............................................................................................................... 25
12.2 Selecting a Suitable Teaching Approach to Establish Competence ...................... 25
12.3 Including the Person with Complex Communication Needs in Decision-Making ... 27
13. Measuring Outcomes ................................................................................................... 28
14. Ethical Considerations ................................................................................................. 30
14.1 Facilitated Communication .................................................................................... 30
14.2 Mobile Technologies.............................................................................................. 31
15. Conclusion ................................................................................................................... 32
Augmentative and Alternative Communication Clinical Guideline 3
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
16. Future Directions .......................................................................................................... 32
17. Review ......................................................................................................................... 33
18. Selected Resources on Augmentative and Alternative Communication ...................... 34
19. References................................................................................................................... 35
Augmentative and Alternative Communication Clinical Guideline 4
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
SUMMARY
• It is the position of Speech Pathology Australia that working in the field of Augmentative
and Alternative Communication (AAC) is within the scope of practice of speech
pathologists (Speech Pathology Australia, 2003).
• It is essential that speech pathologists work collaboratively as part of a team using a
person centred approach in the field of AAC.
• The Association supports an evidence based practice approach to the assessment,
intervention, and outcome measurement in the provision of AAC and other supports for
people with complex communication needs.
• The Association strongly supports speech pathologists providing education and
consultancy services to professionals, the broader community, clients, and carers to
improve the understanding of AAC.
• It is the position of the Association that speech pathologists working in AAC engage in
ongoing professional development and seek professional support and supervision as
required.
• It is recommended that speech pathologists working in the field of AAC be conversant
with legal issues relevant to their state or territory. In particular legal issues related to
consent, validation of AAC users messages, and privacy need to be understood.
Augmentative and Alternative Communication Clinical Guideline 5
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
GLOSSARY OF TERMS
It is strongly advised that the glossary of terms is reviewed prior to reading the body of the
document.
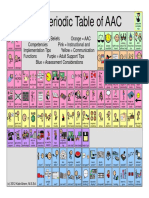
AAC system: An integrated group of components, including the symbols, aids, strategies
and techniques used by individuals to enhance communication. The AAC system serves to
supplement any gestural, spoken, and/or written communication abilities (ASHA, 1991). AAC
includes unaided and aided systems and communication strategies.
Access Techniques: The means of accessing a communication aid including:
Direct selection: The individual independently points to the desired item (e.g. picture,
object, and letter). This technique includes finger pointing, fist pointing, eye pointing,
and the use of a pointer, head stick, or other assistive device; and
Indirect selection: The individual is offered choices of available symbols, pictures,
letters, or words through visual or auditory scanning, and indicates choice by a pre-
determined signal (e.g. blink, nod, gesture, or vocalisation).
Assistive Technology is “any item, piece of equipment, or product, whether it is acquired
commercially, modified, or customized, that is used to increase, maintain, or improve the
functional capabilities of individuals with disabilities” (Assistive Technology Act, 2004).
Assistive technologies pertinent to communication include aids (e.g., hearing aids, visual
aids), computer technologies, speech generating devices, computer laptops, or mobile
technologies (e.g., smart phones or tablet devices) with assistive software, switches, access
devices (e.g., head pointers, styli), and communication books or boards (Beukelman &
Mirenda, 2005).
Augmentative and Alternative Communication (AAC): An area of clinical and educational
practice that provides communication strategies, techniques, and interventions for people
with a range of communication limitations. The term ‘augmentative’ in this context means
supplemental or additional to speech. Augmentative techniques (e.g. gestures, facial
expressions, and items of reference) are commonly used when communicating and
interacting with others. The use of the term ‘alternative’ acknowledges that there are some
individuals whose speech is sufficiently impaired that they must rely completely on strategies,
systems, and techniques which do not augment speech but are alternatives to speech
(Vanderheiden & Yoder, 1996).
Augmentative and Alternative Communication Clinical Guideline 6
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Augmentative and Alternative Communication (AAC) systems include:
Aided AAC: is where an external item is used to aid communication (e.g. object
symbols, communication boards, books, key-ring mini-cards, wallets, speech
generating device, computer, mobile phone, tablet). Aided AAC is often divided into
high technology and low/light technology systems (see below); and
Unaided AAC: Unaided AAC refers to communication techniques that do not require
the use of an external aid. That is, the person uses whatever is available to them
generally using their own body. Examples of unaided AAC include using eye gaze,
facial expression, body language, gesture, and manual sign.
Communication Continuum: Communication develops along a continuum beginning at the
earliest level pre-intentional/unintentional stage. It usually progresses through a series of
stages, to intentional symbolic and then linguistic communication (Coupe-O’Kane & Goldbart,
1998). Most people move through these stages to become functional and independent
communicators. A small percentage of people who have significant intellectual disabilities do
not make this transition and remain dependent upon others interpreting their non-symbolic
communication.
Preintentional / Unintentional Communication: Preintentional or unintentional
communication occurs when a person’s behaviour can be interpreted as
communicative, but lacks the intent to communicate, as demonstrated by directing the
behaviour to another person. The unintentionally communicative behaviour may reflect
the person’s wants and preferences, states (e.g., hunger, pain, discomfort,
contentment, fear, anger, worry, happiness, joy) and/or alertness. The behaviours
observed may include intentional or goal-directed behaviours that are not intentionally
communicative (Iacono, Carter & Hook, 1998). For example, a person demonstrating
challenging behaviours because of a desire to go outside, but who does not direct a
signal - conventional or otherwise, is demonstrating an intentional act, but not an
intentional communicative act. Unintentional communication can be interpreted from
an observation of the person’s affect and behaviours, facial expression, body
movements, and/or vocalisations, and the context of the situation. In any given
context, the communication partner interprets the person’s behaviour and attributes
meaning to it. If the individual is unable to demonstrate symbolic understanding using
non-verbal methods and remains reliant on the communication partner interpreting
facial expression, body language and vocalisations, he or she is considered to be an
unintentional communicator.
Intentional Informal Communication: Intentional informal communication is goal-
directed behaviour, with a communicative signal directed to another person,
demonstrated by co-ordinated gaze between the person and referent. People whose
Augmentative and Alternative Communication Clinical Guideline 7
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
disabilities preclude the demonstration of co-ordinated eye gaze may use other
means, such as body orientation to direct the signal to another person (Iacono, et al.,
1998). The person with a disability is aware of the role of a communication partner in
the interaction and understands that communication first involves having the attention
of a communication partner. Informal behaviours are used intentionally to
communicate, including unconventional signals - such as idiosyncratic body
movements. At this stage, the behaviours are non-symbolic because they do not
involve any sort of symbol, such as spoken words, conventional gestures or manual
sign. The behaviours used include facial expression and simple gesture (e.g., pointing,
hugging, waving use of objects, and vocalisation).
Symbolic Communication: As with intentional informal communication, the person
acts with intent and anticipates a response from the communication partner. Symbolic
communicators are able to use a range of symbolic and non-symbolic behaviours.
Symbolic communication may include pointing to line drawings/photos, manual sign,
speech, and the intentional selection of letters to encode words. The person will also
have a repertoire of non-symbolic intentionally communicative behaviours to
supplement his or her communication (e.g., gesture, facial expression, body language
and non-speech vocalisations).
Communication Disability: A person’s health condition may feature impairments of body
structure and function that combine with environmental and personal factors to impact upon
their activities and participation in society. This is known as a communication disability.
According to the WHO International Classification of Functioning, Disability, and Health (ICF,
WHO, 2001) and the International Classification of Functioning, Disability, and Health –
Children and Youth Version (ICF-CY, WHO, 2007), the disability exists as a result of the
interaction of the various factors and not solely within the individual.
Communication Partners: A communication partner is anyone who is involved in a
communicative interaction with another person. Communication partners are a vital part of
the environment for communication and have impact on the activities and participation of the
person with communication disability (ICF, WHO, 2001; ICF-CY, WHO, 2007).
Communication Strategy: A communication strategy is a specific way of using
augmentative aids, symbols, and techniques more effectively to enhance communication. A
strategy, whether learnt, or taught to an individual, is implemented to improve performance
(ASHA, 1991).
Augmentative and Alternative Communication Clinical Guideline 8
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Communication Technique: A communication technique is a method of transmitting ideas
(e.g. direct selection, scanning, encoding, signing, or gesturing) (ASHA, 1991).
Communication Vulnerability: People with a communication limitation of any aetiology are
considered to be vulnerable to poor communication in a range of settings (Blackstone, 2010).
Complex Communication Needs: People with complex communication needs have
communication problems associated with a wide range of physical, sensory, cognitive and
environmental causes which restrict/limit their ability to participate independently in society.
They and their communication partners may benefit from using AAC methods either
temporarily or permanently (Balandin, 2002).
Gesture: Gesture refers to the use of bodily movement to represent an object, idea, action,
emotion or relationship without the linguistic constraints of manual signs or a formalised
manual sign system.
High Technology System: High technology communication systems utilise computer
components and specialised software. They may have the capacity to provide printed output
as well as voice output (Sigafoos & Iacono, 1993). They are commonly referred to as ‘high
tech’ systems.
Key Word Sign: Key Word Sign (see Key Word Sign, Australia, in Resources) is a formal
means of unaided communication. The principles of Key Word Sign involve the concurrent
use of speech and manual sign with only the key words of the sentence being signed. Key
Word Sign incorporates the use of natural gesture, facial expression, and body language with
simple sign language techniques such as directionality and placement. In Australia, the
manual signs used are from Auslan, the language of the Australian Deaf community.
Low/light Technology System: Low and/or light technology communication systems include
any types of communication boards, books, objects boards, and simple technologies for
communication, including single message devices (Sigafoos & Iacono, 1993).
Mobile Technologies: Mobile technologies include smart phones, tablet computers, and
laptops that enable connection to the Internet via wireless or cable connection.
Multimodal Communication: Providing multimodal communication means offering a range
of communication systems and strategies as options to enable the person the greatest
degree of choice in using a preferred modality in any given situation. Multimodal
communication can occur in face-to-face interpersonal contexts and in telecommunication
contexts (i.e., telephone, video conference, and internet: email, sms, and social media, see
Raghavendra et al., 2012; The Newell Network, 2011; and Media Access Australia, 2012). It
is recognised within the AAC field that no one method or technique will fulfil every
communication need in every situation (Beukelman & Mirenda, 2005). Speech pathologists
Augmentative and Alternative Communication Clinical Guideline 9
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
implementing multimodal communication strategies ideally aim to increase the person’s
competence and confidence in not only using multiple modalities for communication, but also
choosing and switching between modalities for different purposes to meet his or her
communication needs across situations. Reliance or proficiency in only one modality for
communication might leave a person vulnerable to breakdowns in communication across a
range of communication contexts.
Participation Model: This model is based on the work of Rosenberg and Beukelman (1987)
and further developed by Beukelman and Mirenda (2005). It provides a framework for
assessment and intervention aimed at functional outcomes that enhance a person's ability to
participate in the community and wellbeing. The outcomes include developing communication
strategies focusing on the individual’s present and future communication needs.
Partner Assisted Strategies: In any partner assisted strategy the communication partner
plays a meaningful part in the production of the message to a greater or lesser extent.
Examples are (a) ‘auditory scanning’, whereby a partner speaks out messages, words, or
letters until the person indicates his or her selection (e.g., head nod, vocalisation, eye-blink);
(b) asking a series of questions; each of which require a yes/no or other response; and (c)
encoding individual elements selected by the person into a meaningful unit, such as
combining selected letters into words. In these situations, the person with complex
communication needs may also be described as ‘partner-dependent’ in communicating using
these strategies (Beukelman & Mirenda, 2005). In these situations, the person with complex
communication needs must be provided the opportunity to confirm or disconfirm the encoding
or other attempts by the communication partner to co-construct meaning.
Sign Language: This refers to the natural sign language of the Deaf community. In Australia
the natural sign language is Auslan. The term does not cover the use of manual signs as a
code for a spoken language (e.g. Australasian sign or Signed English).
Speech Generating Device: A speech generating device is a form of high technology AAC
that produces speech either by digital recording of a person’s voice or synthesized speech. A
speech generating device might either be dedicated to communication (i.e., its primary
purpose and design is as a communication aid) or non-dedicated, with a primary purpose
other than communication (e.g., mobile technologies, computers, laptops, smart phones).
Symbol: Something used or regarded as standing for or representing something else is a
symbol. A symbol can represent an idea or concept using visual, auditory, or tactile
modalities (e.g. gestures, manual sign, pictures, printed word, spoken words, real objects).
Augmentative and Alternative Communication Clinical Guideline 10
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
1. Origins of the Paper
This Clinical Guideline has evolved from the Speech Pathology Australia Position Paper,
Augmentative and Alternative Communication (AAC) (2004). The expansion of evidence
and technology in the field AAC has been the impetus to update the position paper into this
current clinical guideline.
2. Overview and Purpose
This document contains clinical guidelines for speech pathologists assessing, treating, and
supporting clients with complex communication needs who may benefit from Augmentative
and Alternative Communication (AAC). It is evidence based and incorporates recent research
but it is not intended as an exhaustive examination of or an instructional manual on the topic.
In order to achieve the best possible outcomes for people with complex communication
needs, speech pathologists support clients using AAC in collaboration with a multi-
professional (multidisciplinary, interdisciplinary, and trans-disciplinary) team using family and
person-centred approaches. Speech pathologists have a pivotal role to play in the
assessment, implementation, monitoring, and management of clients with complex
communication needs. Furthermore, the speech pathologist may act as clinician, consultant,
team manager, educator, supervisor, mentor, and/or researcher. The extent of involvement
depends on the expertise of the speech pathologist, the nature of the clinical setting, the
support needs of the client, and the context of the referral.
This clinical guideline should be read in conjunction with Speech Pathology Australia core
association documents including; Code of Ethics (2010), Competency Based Occupational
Standards (2011), Principles of Practice (2009) and Scope of Practice (2003).
3. Introduction
AAC is a dynamic area of speech pathology practice that is changing rapidly due to advances
in technology and active international research endeavours. The field of AAC was
established in the late 1970s. Since that time, burgeoning research and clinical interventions
in AAC demonstrate that the need for and range of applications of AAC in clinical practice are
increasing. The importance of this area of practice is now formally recognised by Speech
Pathology Australia, with Multimodal Communication a Range of Practice in the Competency
Based Occupational Standards (CBOS, Speech Pathology Australia, 2011). AAC is a form of
Augmentative and Alternative Communication Clinical Guideline 11
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
multimodal communication and includes oral (speech, vocalisations), manual (sign and
gesture), all forms of aided and unaided systems and strategies, and any other assistive
technologies that support communication (Speech Pathology Australia, 2011). As such, AAC
is integrated within the practice and competencies of graduating speech pathologists across
all populations and groups of people with communication disabilities (ASHA, 2011). Indeed,
most speech pathologists in their working life are likely to encounter individuals who could
benefit from AAC. Although speech pathologists currently graduate with knowledge and skill
in the principles and practices of multimodal communication (Speech Pathology Australia,
2011), Costigan and Light (2010) noted that students are at risk of having limitations in their
expertise owing to many university academics having “minimal expertise in AAC” and
concluded that it was unclear whether pre-service programs equipped professionals for entry-
level AAC practice. Indeed, there are many qualified clinicians who have had limited practice
in and knowledge of the area and as a result might actively avoid introducing AAC
(Sutherland, Gillon, & Yoder, 2005). Despite the relevance of AAC across a range of groups
with communication disorders, and the ever increasing evidence base, research has
indicated that few speech pathologists feel competent in advising on AAC interventions or
developing AAC programs (Sutherland et al., 2005).
It is unlikely that speech pathologists will remain up to date in all areas covered by the
profession due to an expansion of information and a tendency to specialise quite early in their
careers. Nonetheless, communication is a fundamental characteristic of human interaction
(Kaiser, Hester, & McDuffie, 2001) and is recognised as a human right (see UNCRPD 2006,
Articles, 16, 17, 21, 24). Therefore, people with complex communication needs should not be
denied the opportunity to communicate to the best of their ability and in their preferred mode
or modalities that reflect their authentic voice. Consequently, it is important that all speech
pathologists have at least a basic understanding of all forms of AAC and factors affecting the
implementation of any strategies to improve communication. Furthermore, speech
pathologists need to know where they can obtain information, support, and resources to
facilitate their further learning and skill development.
In this Speech Pathology Australia Clinical Guideline, current principles of good practice in
AAC and multimodal communication are outlined and the evidence base highlighted. The
field of AAC continues to grow and expand, with demonstrated relevance to a wide scope of
speech pathology practice. Speech pathologists have a pivotal role on the AAC team and
need the skill and confidence to implement multimodal communication interventions across
the lifespan. People with complex communication needs and their families are vulnerable to
exploitation and exposure to not only treatments that lack a strong evidence base but
treatments known to be harmful (Gorman, Wynn, Morse, & Todd, 2011). Speech pathologists
are well placed to help families know the risks and benefits of treatments that might be
Augmentative and Alternative Communication Clinical Guideline 12
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
selected and to point out flaws in the evidence put forward in support of treatment options
(Lof, 2011). Therefore, clinicians need to adopt a lifelong approach to learning in AAC and
multimodal communication, stay abreast of developments, and critique accompanying
evidence as it becomes available. Speech Pathology Australia encourages continued
research, clinical practice, and professional development in AAC, to enhance and optimise
the communication skills of people for whom speech is not a functional communication mode.
4. Origins and Aims of AAC
Augmentative and Alternative Communication (AAC) is an area of clinical and educational
practice that provides communication interventions for people who have little or no functional
speech or who have complex communication needs. They and their communication partners
are likely to benefit from the use of a range of AAC systems and communication support
strategies to participate fully in all aspects of life. The aims of AAC systems and strategies
and communication support interventions are to:
• support and increase the individual’s ability to participate in all environments with
autonomy, choice, and self-determination; and
• enhance opportunities for community participation and improve quality of life. The
successful use of AAC systems and strategies contributes to personal well-being and
quality of life for people with complex communication needs (Iacono, Lyons, Johnson,
& West, 2012).
5. Client Group
People who potentially benefit from AAC are children and adults with communication
problems associated with either lifelong (developmental) or acquired physical, neurological,
cognitive, and/or sensory disorders that impede communication by speech alone. The
conditions may be temporary or permanent and result in an inability to use functional speech
to meet all communication needs. Candidacy for AAC is based on a person’s unmet
communication needs across all communicative contexts and not upon his or her skills or
capacities (Beukelman & Mirenda, 2005; Beukelman & Mirenda, forthcoming). Because of
the role of communication partners in successful communication using AAC, the client group
includes both the person with little or no functional speech and his or her communication
partners.
Augmentative and Alternative Communication Clinical Guideline 13
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
An estimated 1 in 500 people in Australia have severe communication disabilities or complex
communication needs (Perry, Reilly, Bloomberg & Johnson, 2002). Some populations have a
significantly higher incidence of communication disabilities due to the occurrence of multiple
impairments affecting speech, language, and/or cognition. For example, up to 25% of people
with cerebral palsy have little or no functional speech and will use AAC (Access Economics,
2008; Goldsmith & Novak, 2010). It has been estimated that 17%-25% of children with
Autism Spectrum Disorders fail to develop functional speech (National Research Council,
2001). People with developmental disabilities and complex communication needs have
lifelong conditions, and their communication needs will change according to developmental
processes and transitions. Some people with acquired conditions will also develop complex
communication needs secondary to the condition affecting speech, language and/or cognition
(e.g., motor neuron disease, Parkinson’s disease, stroke, dementia, or traumatic brain
injury) (Beukelman, Garrett, & Yorkston, 2007). Their complex communication needs may
continue through the remaining years of life or may increase over time if the condition is
progressive (Beukelman et al., 2007). Some people may have only temporary complex
communication needs arising from short term conditions or states associated with illness
(e.g., Guillain Barre Disease), injury (e.g., requiring intubation), or surgical interventions
impacting upon speech, language and/or cognition (Beukelman et al., 2007).
6. Research
6.1 Evidence Based Practice
As in all areas of speech pathology practice, speech pathologists are required to follow an
evidence-based practice approach to their provision of AAC services. In relation to AAC, the
influence of the environment and communication partners on the success of an AAC
intervention must be considered within an evidence based framework. In the
Transdisciplinary Model of Evidence Based Practice, Satterfield, et al., (2009) emphasised
the organisational / environmental context in which implementation of evidence occurs and is
suitable in the practice of AAC interventions. When working within the Transdisciplinary
Model of Evidence Based Practice, clinicians:
• source the best available research evidence for the AAC intervention and instructional
method;
• source resources that will be required for each treatment option including the
practitioner’s expertise, the client’s characteristics and needs, values, and
preferences; and
• consider the organisational context in which treatment is to occur.
Taking all of the above into account, the speech pathologist considers all available options for
AAC intervention and adopts an evidence based practice approach towards selecting a range
of appropriate AAC strategies and techniques for intervention.
Augmentative and Alternative Communication Clinical Guideline 14
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
6.2 Evaluating the Evidence for AAC
Speech pathologists need to be able to evaluate the efficacy of AAC interventions and justify
their choice of interventions (Schlosser, 2000; Schlosser & Raghavendra, 2004). Evidence
based practice principles encourage speech pathologists to ask well-built clinical questions
and search the available evidence (Schlosser, Koul, & Costello, 2007), and to integrate
clinical experience with the best available evidence (Reilly, 2004). Evidence is ranked in a
hierarchy from strong evidence found in rigorously conducted systematic reviews and
randomised controlled studies to the weakest form, including anecdotal evidence (e.g.,
anecdotal material appearing on YouTube or blogs or in journal publications that depicts a
personal view or experience) and opinions from committees or experts (Schlosser &
Raghavendra, 2004). In the field of AAC, an increase in the availability of systematic and
narrative reviews and a growing interest in evidence-based practice have resulted in a wider
appreciation of the benefits of AAC across many populations (see Goldsmith & Novak, 2010;
Mostert, 2001; Pennington, Goldbart, & Marshall, 2004; Schlosser & Lee, 2000; Schlosser &
Sigafoos, 2004; Schlosser & Wendt, 2008; Schwartz & Nye, 2006; Wendt, 2009). On the
basis of a review of the AAC evidence base, Iacono (2004) concluded that:
• the evidence in AAC predominantly stems from single case and small group designs;
• research studies have been more numerous in relation to developmental than
acquired disabilities;
• it is difficult to conduct randomised group control studies in the field of AAC due to the
heterogeneity of the AAC population;
• the applicability of randomised control study designs to people with complex
communication needs is questionable; and
• there is a wide range of evidence sufficient to support the application of AAC, with
evidence for some areas of AAC being particularly strong as a result of controlled trials
and availability of systematic reviews.
The evidence base in AAC is strengthened by the conduct of rigorous qualitative studies, well
suited for use in heterogeneous populations, and to gather an understanding the human
experience and views of key stakeholders. In accordance with this, a strong tradition of
rigorous qualitative research is building in the field of AAC and multimodal communication for
understanding of all the factors and complex relationships that might exist in particular life
situations (e.g., Balandin & Goldbart, 2011; Dark, 2010; Dew, Balandin, & Llewellyn, 2011;
Johnson, Douglas, Bigby, & Iacono, 2010; Hemsley, Balandin, & Togher, 2008; Hemsley,
Worrall, & Balandin, 2011; Hines, Balandin, & Togher, 2011; Trembath, Balandin, Stancliffe &
Augmentative and Alternative Communication Clinical Guideline 15
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Togher, 2010). Such rigorously conducted qualitative studies provide evaluations of important
topic areas, inform future qualitative and quantitative research, and guide changes to policy
and practice to improve the lives of people with complex communication needs.
6.3 Service Delivery in AAC
Management of AAC in both children and adults demands a lifespan approach and
consideration of both current and future communication needs. Furthermore, a person’s
transition between life events and life stages must also be considered in design and provision
of AAC systems or strategies (McNaughton & Beukelman, 2010). People with complex
communication needs may require speech pathology and related services in regards to
multimodal communication at a number of points in time throughout their lives, including
episodically. Service delivery includes providing a system for the present (today) while
planning for the system for the future (tomorrow) (Beukelman & Mirenda, 2005). Training for
communication partners is an essential component of intervention.
7. Principles in AAC Services
The Principles of Practice (Speech Pathology Australia, 2001) provides recommendations on
how to facilitate quality service provision for clients. In the field of AAC the following
principles should also be considered:
• Service Model: To maximise efficient and effective intervention, a range of service
delivery approaches may be needed by the person with complex communication
needs and his/her communication partners. To address the person’s communication
needs, interventions include: (i) individual work with the person with complex
communication needs (direct services), (ii) work with a family member, guardian, or
significant other (indirect services), (iii) collaborative consultation, and (iv) education
and training of significant others in the community.
• Team: A multi-professional (multidisciplinary, interdisciplinary, and/or transdisciplinary)
collaborative team approach is required for optimum service delivery. The person with
complex communication needs and his/her significant communication partner(s), as
nominated by the person with disability who can make an informed choice or his/her
proxy, is integral to this team. Other team members include speech pathologists,
speech pathology or allied health assistants, occupational therapists, rehabilitation
engineers, physiotherapists, psychologists, teachers, direct support workers, and
family members. People with complex communication needs will require support to
varying to degrees to enable them to contribute to and direct the team through an
informed choice and decision-making process.
Augmentative and Alternative Communication Clinical Guideline 16
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
• A Dynamic Assessment, Intervention, and Monitoring Cycle: The optimal
processes for assessment, intervention, and monitoring/evaluating outcomes when
providing AAC to people with complex communication needs can be based on
principles drawn from the Participation Model (Beukelman & Mirenda, 2005) and
Dynamic Assessment (Hasson & Joffe, 2007; Iacono & Caithness, 2009). The
Participation Model includes principles for identifying how various AAC systems and
options can address current and future needs of people with complex communication
needs, with a focus on facilitating their participation within their chosen communities.
Dynamic assessment targets the person’s potential for learning rather than the
conduct of a static assessment of current skills, and aligns with the principles and
philosophy of the Participation Model (Beukelman & Mirenda, 2005).
• Natural Settings: Conducting assessment within a person's own environments will
inform intervention that will be relevant to those environments. Consequently,
assessment and intervention may occur across multiple contexts. The ICF (WHO,
2001) and ICF-CY (WHO, 2007) may be used to help guide development of
assessment and intervention goals across contexts, promoting the individual’s
participation in society.
• Duration and Intensity of Treatment or Intervention: Extensive and ongoing
supports may be required in order to establish appropriate and functional
communication. The duration and intensity of support will be determined in part by the
nature of the needs and goals of the individual and his/her communication partners as
well as the communication context/s. Therefore, service administrators and policy
makers need to be integrally involved in designing AAC services that will meet
individual and population needs.
• Training, Mentoring, and Support: Speech pathologists have a responsibility to
ensure that the person has the support to develop their communication skills to the
maximum of ability and that communication partners, including support staff, have
appropriate and adequate training. Training, mentoring, and support is helpful for the
individual with complex communication needs who is using AAC and for each of
his/her regular and/or significant communication partners (Ballin, Balandin, Stancliffe,
& Togher, 2010; Beukelman & Mirenda, 2005). Training is required to prepare for
major transitions, such as entering preschool, primary school, secondary school,
tertiary education/employment, and retirement. Additional support may be required at
Augmentative and Alternative Communication Clinical Guideline 17
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
specific times of transition (e.g. changing classrooms, moving house, death of a
partner or family member, period of hospitalisation, change in support worker) (see
McNaughton & Beukelman, 2010).
• Evidence Based Ethical Practice: Speech pathologists are bound by a code of
ethical practice that impacts upon AAC and all other interventions (Speech Pathology
Australia, 2002; Speech Pathology Australia, forthcoming). Thus, interventions are
selected and delivered on the basis of the evidence demonstrating benefit to the
person with complex communication needs and his/her communication partners, and
minimising harms associated with the selection of one intervention technique or
strategy over another technique or strategy (see Balandin, 2012; Hemsley, 2012).
8. Leadership, Supervision, and Mentoring
Speech pathologists in Australia do not undertake credentialing processes to work in the field
of AAC, provide AAC services, or conduct research in AAC. Supervision in AAC is as
provided for other clinical areas according to workplace policies and procedures. In Australia,
clinicians with expertise in AAC are located in academic institutions, in Government and Non-
Government organisations (including disability, health, and education sectors), profit and
non-profit organisations, and private practice. Experts in AAC take a variety of roles in
relevant associations, including the International Society for Augmentative and Alternative
Communication (ISAAC, www.isaac-online.org), its chapter in Australia - ISAAC-Australia
(www.isaacaustralia.com), The International Association for the Scientific Study of Intellectual &
Developmental Disabilities (IASSIDD, www.iassid.org), the Australasian Society for
Intellectual Disability (ASID, www.asid.asn.au), AGOSCI (www.agosci.org.au), ARATA
(www.arata.org.au) and Speech Pathology Australia (www.speechpathologyaustralia.org).
Mentoring processes are available through many of these organisations.
9. Legal Issues
Speech pathologists should be cognisant of general and specific ethical and legal issues
related to their practice. Section 9.1 to 9.7 outlines general statements related to practice
and section 9.8 discusses specific issues related to practice in the field of AAC and multi-
modal communication.
Augmentative and Alternative Communication Clinical Guideline 18
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
9.1 Code of ethics
Speech pathologists should adhere to the Speech Pathology Australia Code of Ethics (2010)
and to any codes, policies and procedures relevant to their employing body.
9.2 Legislation
It is recommended speech pathologists be conversant with the legislation that applies in the
state or territory in which they practise.
9.3 Duty of care
Duty of care is a legal term describing the relationship, in this case, between the individual
and parent/caregiver and the speech pathologist. The speech pathologist owes a duty of care
to his/her client and parent/caregiver. A breach of duty of care leaves one liable to civil action
for a claim of damages (compensation) if legal action is taken by the individual under care or
the individual’s parent/caregiver(s). A breach of duty of care may result from one or several
specific actions whilst under the care the speech pathologist. For example, a failure to act
when action was required, or a statement made that in the eyes of the law amounts to a
“negligent misstatement.” The duty involves using the same degree of care that a
“reasonable” speech pathologist would exercise in the circumstances. Whether or not there
has been a breach would be determined by what other speech pathologists working in the
same field would have done in the circumstances. Consequently, it is the duty of the speech
pathologist to be aware of recent literature in their field, current practices carried out by
peers, adhering to workplace policies and procedures, and being conversant with the Speech
Pathology Australia Association documents.
9.4 ‘Proxy’ interventions
Where a speech pathologist does not carry out the intervention but instructs and/or
supervises someone else i.e., student speech pathologist carrying out the intervention, the
law would hold the advising/supervising speech pathologist liable just as if they were carrying
out the intervention themselves. The law refers to this as “vicarious liability.” In other words,
the same standard of care would be required if the speech pathologist was holding
him/herself out as the person with the knowledge and skills. The fact that he/she did not
actually carry out the intervention would be irrelevant in the eyes of the law. Therefore it is
necessary for “proxies” to exercise the same standard of care as that required of the speech
pathologist instructing or supervising them, and for all documentation (i.e. Individual
Education Plans, progress notes, negotiated contracts) regarding “proxy” interventions to be
maintained. In addition, the service plans must include adequate time and resources to train
“proxies” and monitor programs.
9.5 Consent for speech pathology involvement
Informed consent refers to the client and/or parent(s)/caregiver(s) being fully informed and
aware regarding the service, assessment, interventions, treatments and role of the speech
pathologist in mental health. For young people who are at an age of being able to consent, if
there is the presence of an intellectual disability or a mental health problem that in the opinion
Augmentative and Alternative Communication Clinical Guideline 19
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
of the speech pathologist does not allow for the ability to consent to services this needs to be
resolved in line with organisational policy/procedure. In such circumstances, the parent(s)
/caregiver(s) may be required to consent. Service provision should not commence without
consent being formally clarified.
Consent requirements vary in different states and territories. A young person may provide
consent depending on the particular state’s laws of age of consent. In some states and
territories the attendance at an appointment is implied as consent.
Situations may arise during the treatment process where verbal consent is requested of the
client or parent(s)/caregiver(s). For example, a case being handed over to another clinician
for a one-off session or a young person’s request that the clinician make contact with their
educational setting without written consent being initially arranged. Ideally, written consent
should be obtained in these instances but where verbal consent has occurred then this
should be documented by the speech pathologist in the individual’s file.
Informed consent for speech pathologists undertaking research requires that the speech
pathologist make contact with the appropriate governing Human Research Ethics Committee
of the service.
9.6 Indemnity Cover and Insurance
It is the responsibility of the speech pathologists to ensure they have appropriate professional
indemnity cover and public liability. Professionals should be aware that there may be
instances where the employing body will not necessarily indemnify them for their actions. It
is recommended that all practicing Speech Pathology Australia members have professional
indemnity insurance.
Speech pathologists should clarify the insurance situation for accidental loss, theft or damage
to resources during transport with their insurer.
9.7 Service guidelines
It is recommended that speech pathologists adhere to the approved guidelines of the
employing body in terms of clinical and service management.
9.8 AAC Specific Issues
Consent: People with complex communication needs must be given the opportunity to
provide informed consent to assessments and interventions either directly or, in situations in
which they have been assessed as lacking capacity for consent, through a proxy (next-of-kin,
primary support person, or legal guardian appointed for the purpose of making relevant
Augmentative and Alternative Communication Clinical Guideline 20
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
decisions). Speech pathologists need the ability to present information about a procedure or
intervention in a way that will maximise the potential for the person with complex
communication needs to understand, and therefore to provide informed consent. In situations
in which a person is judged to lack capacity for informed consent, the person’s assent or
agreement may be determined through (a) direct communication with the person, (b)
observation of the person for any indicators for assent or objection, and/or (c) consultation
with others who are familiar with the person with complex communication needs.
Privacy: Speech pathologists require a working knowledge of Commonwealth and State
privacy laws and/or principles relating to the service within which a person is receiving AAC
assessment and/or intervention. These laws and principles are not meant to interfere with a
person's health care and functioning. As a result, adherence to privacy legislation and
principles does not preclude information about the person and significant others being
included on a communication system, but permission from relevant individuals may be
required.
Providing expert witness: People with little or no functional speech, and those with
disabilities leading to their dependence on other people, are vulnerable to and at risk of
abuse or exploitation (Bryen & Wickman, 2011). Therefore, speech pathologists might also
be called upon to (a) support the person’s communication when interacting with the legal
system, and/or (b) assess an individual’s communicative competence and the validity of
messages delivered through the use of AAC (e.g., by educational or health service
institutions, or legal bodies). The principles and practices of AAC as outlined in these Clinical
Guidelines can be used to help guide such an assessment.
Access to legal rights: It is important that (a) all methods and means of achieving
independently authored messages are assessed to ensure that the person who uses AAC is
afforded the same legal rights as other people; and (b) that the messages created through
the use of AAC, either independently or with assistance, reflect the person’s views.
Duty of care on determining authenticity: In order to ensure they provide duty of care,
speech pathologists must follow strategies and procedures to determine whether AAC
systems or strategies enable the authentic voice of the person with complex communication
needs. There is a particular need for messages produced through AAC requiring partner
assisted strategies to be validated as originating from the person with complex
communication needs and not the person providing assistance. In situations in which such
assessment fails to provide evidence of authentic communication, and therefore indicate that
the AAC systems and strategies have the potential to result in harm, the speech pathologist
Augmentative and Alternative Communication Clinical Guideline 21
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
has an ethical responsibility to: (a) raise these concerns with relevant parties so that further
actions may be taken to remove harms, and (b) help the person towards appropriate systems
and strategies that enable authentic communication. In such situations, should there be
concern relating to speech pathology practices, the speech pathologist has the further ethical
responsibility to consult with the Speech Pathology Australia ethics committee.
10. Education and Training
The inclusion of multimodal communication as a Range of Practice in the CBOS 2011 has
resulted in the need for incorporating relevant information in professional training. Academics
in speech pathology courses in Australia are working to incorporate all elements of
competence in multimodal communication including both theoretical knowledge and clinical
experience required for practice. Qualified speech pathologists working with clients who
might benefit from AAC systems and strategies may need to engage in activities to actively
update their competencies in this area in light of the growing evidence base and
technological developments that impact on the field. In addition, speech pathologists need to
be aware of the importance of liaising with other professionals (e.g., occupational therapists,
psychologists, teachers, technology experts) involved in working with clients who require
AAC. Clinicians also need to recognise the ongoing need for further education and
consultation with other experienced AAC professionals, such as those with technical
equipment knowledge, including manufacturers and distributors. As for other clinical areas, a
speech pathologist working in the area of AAC acquires knowledge and proficiency in areas
relating to AAC through:
• clinical experience
• supervision and mentoring from experienced clinicians in the field
• participating in special interest groups and online discussion forums (e.g., ACOLUG;
Twitter chat by hashtag usage e.g., #SLPchat #AAC #AugComm), and associations
relevant to working with people with complex communication needs and AAC (e.g.,
ISAAC, ISAAC-Australia, IASSID, ASID, AGOSCI, ARATA, , SPOT on DD)
• sourcing academic websites relating to AAC practice and research
• critical evaluation of current literature and research
• relevant conference and workshop attendance
• postgraduate studies
• providing clinical education to students of speech pathology in the practice of AAC and
multimodal communication.
Augmentative and Alternative Communication Clinical Guideline 22
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Student speech pathologists can be involved in managing people with a complex
presentation under the supervision of a qualified speech pathologist with expertise in AAC.
This will help to ensure that student clinicians have some exposure and experience in the
assessment, management, design, and monitoring of AAC interventions. Factors impacting
upon management that might require further assistance or advice from a more experienced
clinician include management of complex dysphagia, management of challenging
behaviours, and management of autism spectrum disorders. Speech pathologists can consult
current and forthcoming clinical guidelines developed by SPA for these specialised areas. At
all times service providers need to bear in mind:
• that a person with multiple or complex disability’s right to be included in decisions
about healthcare management of other clinical areas (e.g., swallowing, mealtimes,
behaviour) may be impacted by his/her access to communication, including any
necessary AAC systems or strategies; and
• that provision of AAC services ideally proceeds with other interventions as indicated
by a full multi-professional assessment and recommendations within an ethical
decision-making framework.
11. Assessment
Assessment of AAC is a multi-faceted and multiphase process. It includes assessment of a
person with complex communication needs’: (a) cognitive, communicative, motor and
sensory abilities; (b) current and future communication needs; and (c) experiences of
participation barriers within the environments in which he/she participate or desires to
participate (Beukelman & Mirenda, 2005). Assessment must lead to a plan that ensures that
there is a range of solutions for the person with complex communication needs (and his/her
family if appropriate) to consider. Assessment must also lead to functional goal setting and a
follow up/review plan. Individual Education Plans are a typical framework for
assessment/goal setting around AAC needs in school settings and systems and speech
pathologists often contribute to these plans. It is recommended that speech pathologists
involved in the assessment process have the following expertise, in addition to any additional
requirements as set out in CBOS (2011):
• An understanding of the Participation Model of AAC (Beukelman & Mirenda, 2005).
• An understanding of the ICF and ICF-CY, and how these relate to AAC (Fried-Oken &
Granlund, 2012; Pless & Grunland, 2012; see also www.icfcy.org/aac).
• An understanding of the Communication Needs Model (Light, 1989).
• An understanding of the Communicative Competence in AAC Model (Light,
Beukelman, & Reichle, 2003).
Augmentative and Alternative Communication Clinical Guideline 23
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
• An understanding of issues surrounding transition in the lifespan for people who use
AAC (McNaughton & Beukelman, 2010).
• Knowledge of and ability to select appropriate assessment tools and strategies to
determine current and future goals.
• Ability to adapt standardised tests and to understand the ramifications of these
adaptations.
• Ability to interpret and integrate information from informal tests and structured
observation.
• Ability to observe, interpret, and integrate information about the individual’s receptive
and expressive language, visual, auditory and sensory abilities to facilitate: (1) an
increase in natural abilities, (2) utilisation of AAC systems and/or devices, and (3)
appropriate environmental adaptations in collaboration with relevant specialists (e.g.,
occupational therapists, vision specialists, and rehabilitation engineers).
• Ability to conduct an activity/communication needs inventory across environments.
• Ability to determine any available ongoing support available from communication
partners in the person’s immediate environment.
• Ability to conduct formal and informal functional communication assessments across a
range of contexts.
• Ability to evaluate both face-to-face communication skills and literacy abilities.
• Ability to assess opportunity barriers to participation, including those relating to policy,
adopted practices and attitudes, knowledge and skills.
• Ability to prepare any necessary funding applications for AAC systems or strategies
according to the funding body’s requirements.
11.1 Feature Matching in AAC Assessment
Feature matching involves comparing the features (e.g., storage of vocabulary, retrieval of
vocabulary, method of access, modifying voice gender accent pitch and volume, adding
items) of two or more devices according to the person’s needs. Assessing the person’s
performance on at least two AAC systems is necessary to determine the relative benefits of
different features of the system that are best suited to the person’s needs. A full assessment
of the person’s communication needs including direct and in-direct access methods and
feature matching in regards to all AAC options is required. A feature matching assessment
helps to limit the problems associated with basing a decision about the best AAC system or
strategy on selected features to the exclusion of others (e.g., a selection based on price and
portability over access or linguistic considerations). Without a full AAC assessment of
communication needs potential harms include the person not gaining an independent means
to communicate (UNCRPD, 2006) and not having a system that meets their communication
needs (AAC-RERC, 2010).
Augmentative and Alternative Communication Clinical Guideline 24
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
A full feature-matching assessment demands that clinicians consider more than the cost of
devices when making recommendations, even if the cost difference is substantial. It is not
possible to place a monetary value on effective communication. If a person acquires an AAC
system that will not meet his/her current or future communication needs two harms arise: (a)
the possibility that funds will be preferentially allocated to a cheaper but less suitable system
might reduce funds available for more worthwhile interventions, and (b) an AAC system being
purchased and not found to be useful may lead to abandonment of that system and rejection
of future AAC options, as has been found to occur when people are inadequately supported
to program and use their AAC systems (Rackensperger et al., 2005). The provision of funds
for the purchase and support of AAC systems raises ethical concerns given the limited public
funding available (Scope, 2006). Funds available for all persons with disability may not be
sufficient for all requested systems and devices across a population. Speech pathologists
have an important role in (a) ensuring funds allocated to AAC are accessed to the benefit of
person’s who can benefit from AAC, and (b) assisting clients in obtaining funds by advocating
for their needs and providing the necessary assessment data required for funding bodies to
make funding decisions.
12. Intervention
12.1 Rationale
The speech pathologist needs to select a relevant teaching approach for the person with
complex communication needs and his/her communication partners’ to establish confidence
and competence in use of the AAC system and in communicating in a variety of contexts.
The speech pathologist also needs to (a) engage collaboratively with the person with
complex communication needs and, if relevant, the person responsible for making decisions
on their behalf, and (b) adopt an ethical decision making framework in making a
recommendation about AAC interventions. It is recommended that AAC interventions are
developed to address the areas within the Participation Model (Beukelman & Mirenda, 2005)
that have been identified as targets. The rationale for introducing particular AAC systems and
strategies will differ across clients and contexts according to the person’s presenting
condition and communication needs. AAC systems and strategies might not only augment or
be an alternative to speech, but in many instances may facilitate language acquisition and
development (Branson & Demchak, 2009; Schlosser & Wendt, 2008). It is not sufficient
merely to provide a system or to focus only on the design or provision of the tools for
communication. To do so would neglect other factors in the person and the environment that
impact upon successful communication across contexts (Beukelman & Mirenda, 2005; WHO
2001, 2007).
12.2 Selecting a Suitable Teaching Approach to Establish Competence
Teaching strategies for introducing and establishing competence in AAC systems include
aided language stimulation, behavioural interventions, augmenting language, incidental
teaching, naturalistic language paradigms, and peer teaching. The goals of AAC
Augmentative and Alternative Communication Clinical Guideline 25
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
interventions are therefore related to developing not only linguistic competence, but also
strategic, social, and operational competence (Light, 1989). Linguistic competence includes
the acquisition of both spoken and written language skills. The development of literacy skills
in both reading and writing is critical for all individuals, but it is especially important for those
who use AAC with symbolic understanding (see Smith, 2003). The symbols provided in AAC
systems may enable individuals with complex communication needs to communicate a wide
variety of messages, however, the alphabet is the only symbol set that allows precise
communication and unlimited message generation (Erickson & Clendon, 2009). Literacy skills
also provide individuals with the independence to govern their program of interventions and
maintain their own AAC systems. Individuals who use AAC will be at different places on the
continuum of literacy learning (Erickson & CLendon, 2009; Light & McNaughton, 2009).
Some will be emerging in their literacy; others will be able to read and write conventionally.
Interventions should be appropriate for individuals' literacy levels as determined by a
comprehensive assessment. It should also be noted that for individuals who have not
developed literacy will require access to and support in using limited message sets.
The fundamental guiding principle in relation to AAC services must be to address current and
future needs. AAC interventions may be implemented for several reasons: (a) to provide an
interim means of communication, used until speech develops fully, (b) as a supplement to
speech, (c) as an alternative to speech, (d) as a temporary replacement for speech, (e) to
support language development, and/or (f) to support communication after language has
developed in the event of an acquired communication disability (e.g., aphasia following
stroke, primary progressive aphasia, traumatic brain injury, Parkinson’s disease, motor
neuron disease) (Beukelman, Ball, & Fager, 2008; Beukelman et al., 2007). Speech
pathologists must apply what they know about language principles in regards to language
development and interaction. Indeed, AAC is a modality in which speech/language
stimulation can be provided. Multimodal communication helps in this regard, and includes
sign language and key word sign systems (Iacono, 1995).
It is recommended that all speech pathologists working with people with complex
communication needs, including new graduates, possess the following intervention expertise:
• An understanding of the Participation Model and its implications for intervention (e.g.,
the level within the Participation Model that a chosen intervention is targeting).
• An understanding of the ICF and ICF-CY and the rationale for intervention goals
aimed not only at the individual factors but also at environmental factors and personal
factors that impact upon activity and participation (See Rowland et al., 2012 for the
ICF-CY for AAC Profile and Code Set for Children Who Rely on AAC).
Augmentative and Alternative Communication Clinical Guideline 26
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
• Ability to determine functional and meaningful communication goals, in consultation
with the person with complex communication needs, that will increase participation
(see Raghavendra et al., 2011; Rowland et al., 2012).
• Knowledge of the level of evidence for AAC interventions proposed for a person with
complex communication needs (Schlosser & Raghavendra, 2004).
• Knowledge of current unaided and aided AAC systems including symbols, techniques
for message transmission, and strategies for effective use of AAC to support
expression and understanding.
• Knowledge of different vocabulary selection and organisation strategies, and the ability
to implement them according to varied needs.
• Ability to match the person with complex communication needs’ abilities, preferences,
and chosen environments with appropriate aided or unaided AAC, symbols,
techniques, and strategies (feature matching).
• Ability to train others in how to support communicative participation of a person using
AAC (i.e. linguistic and social domains, including through the use of aided language
stimulation techniques).
• Ability to integrate intervention into the person’s environments, including the
involvement and training of a variety of communication partners.
• Ability to determine appropriate goals and strategies for developing communication
skills and literacy, and to work with other members of the educational team to develop
a plan for adapting or modifying the curriculum in these areas.
• Ability to monitor progress and adapt interventions according to response and
changing needs to ensure success over time.
• Awareness that some people with disabilities who exhibit challenging behaviours (e.g.,
physical aggression or property damage) benefit by receiving services from speech
pathologists in regards to behaviours being communicative, and interventions utilising
the full range of AAC systems strategies described in this document (Carr et al., 1994;
Sigafoos, Arthur, & O’Reilly, 2003).
12.3 Including the Person with Complex Communication Needs in Decision-Making
It order that the person with complex communication’s views are taken into account, speech
pathologists need to ensure that he/she is included at all stages of the AAC assessment,
management decisions, and intervention. Adopting an ethical decision making framework
and a rights-based approach, the speech pathologist takes the views of the person into
account, and may need to provide interim communication supports and other aids to
communication to help the person understand materials included in all phases of AAC
management. Providing information in formats that are accessible to people with
communication difficulty is an ethical imperative according to the World Health Organisation,
Disability Health Report (2011). Communication supports include ‘AAC-friendly’ information
Augmentative and Alternative Communication Clinical Guideline 27
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
sheets and consent forms, information displays, schedules, and the use of appropriate
photographs, pictographs or other symbolic or non-symbolic forms of communication (e.g.,
Watson, 2011), to help the person participate to the extent that they are able in decisions that
affect their lives.
13. Measuring Outcomes
Speech pathologists working in AAC need an understanding of appropriate measures for
determining intervention outcomes. These outcome measures provide information on the
extent to which a person with complex communication needs has achieved participation
across all environments. Speech pathologists require expertise in documenting and
evaluating progress, as set out in CBOS (2011). Outcome measurement in the field of AAC
has, to date, focused primarily upon ‘operational competence’ (i.e., skills in access and use of
an AAC system or strategy) and ‘linguistic competence’ (i.e., skills in receiving language
through the spoken modality and producing language using the AAC system). Unfortunately,
there has been little research that has addressed the ‘social competence’ and ‘strategic
competence’ (Light et al., 2003) that might have positive impacts on communication-related
activities and participation highlighted in the ICF (WHO, 2001). Successful AAC interventions
resulting in better communication can lead to improved personal well-being and quality of life
and reduction in behaviours of concern (Sigafoos et al., 2003). Therefore, it is recommended
that speech pathology practice includes measurement of outcomes. There is also a need to
broaden the scope of measures, in particular, to address the extent to which AAC
interventions lead to improved participation in all aspects of daily life. The following are
specific outcomes that require assessment in relation to evaluating AAC interventions:
• Outcomes measured by tools developed to measure participation as per the ICF
(WHO, 2001): Children's Assessment of Participation and Enjoyment (CAPE) and the
Preferences for Activities of Children (PAC) (King et al., 2004); and the ICF-CY for
AAC Profile and Code Set for Children Who Rely on AAC (Rowland et al., 2012).
• Outcomes as conceptualised by the Participation Model of AAC in relation to
increased opportunities for communication and a reduction in barriers to
communication. Discussion of the various parameters of participation can occur with
the client and communication partners throughout intervention to guide revisions
according to outcomes (see section on criterion referenced outcome measures and
checklists)
• Outcomes according to the Communicative Competence for Individuals who use AAC
(Light, Beukelman, & Reichle, 2003)
• Outcomes on items prioritised by the person with complex communication needs, and
his or her communication partners.
Augmentative and Alternative Communication Clinical Guideline 28
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
• Outcomes that pertain to the usual communication skills and abilities across all
domains (speech, language, fluency, voice) that are the target of any AAC
intervention, including pragmatics, metalinguistics, and literacy.
Criterion referenced outcome measures are a viable and effective alternative to
standardised tests due to the ability to individualise the target outcome according to the
needs, abilities and goals of the person. There are now several evidence-based tools for
measuring and describing outcomes for people who use AAC. These tools can be used in the
assessment, monitoring, and outcome measurement phases of management. The following
list of selected outcome measures illustrates that clinicians need not rely on self-reported or
caregiver-reported outcomes only:
• The Goal Attainment Scale (GAS) (see Hanson, 2007 citing Kiresuk & Sherman,
1967) facilitates the development of individualised goals that can address multiple
factors within the ICF model and multiple domains of the Participation Model. It
involves the selection of an ‘expected level of achievement’ for a functional
communication goal (e.g. may be linguistic, operational, social, environmental) and
then details less than expected and greater than expected outcomes relative to the
abilities of the individual. Goal Attainment Scaling is used widely in many fields
including disability and AAC and it is advisable for speech pathologists to develop
competency with use of this tool or other comparable criterion referenced measures
(Hanson, 2007).
• AAC Profile – A Continuum of Learning (Kovach, 2009) provides information on
functional skills for developing communicative competence using AAC systems and
requires supplemental assessments of communication. The profile is not specific to
disorder, severity, or setting.
• Social Networks (Blackstone & Hunt Berg, 2003) provide a means of describing a
person who uses AAC’s social networks and may be used as a tool at any stage of
management including outcome measures.
• Rowland (2004) developed the Communication Matrix, which is a free online tool and
handbook for assessment of very early communication skills and is also useful for
assessment, review, and outcome measures (see http://communicationmatrix.org).
• An additional free online tool framed around the ICF (WHO, 2001) and a code set
pertinent to AAC (Rowland et al., 2012) will also assist clinicians in development of
functional goals and can be used when determining functional outcomes following
intervention.
Augmentative and Alternative Communication Clinical Guideline 29
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
14. Ethical Considerations
Speech pathologists providing AAC services are bound by their professional Code of Ethics
(Speech Pathology Australia, 2010). The UNCRPD (2006) also underpins decisions relating
to AAC services. Recent publications by Hemsley (in press) and Balandin (in press) outline a
range of ethical issues arising in the expanding field of AAC. As in other areas of clinical
practice, the use of controversial therapies and untested therapies remains an ethical issue
for speech pathologists.
14.1 Facilitated Communication
Facilitated Communication (FC), also referred to as ‘supported typing’ or ‘assisted typing’,
involves a facilitator touching the person with disability’s hand, elbow, shoulder, body,
keyboard or alphabet board (‘rapid prompting’) in order that the person with disability points,
types, or selects messages (see Crossley 1994; Shane, 1994; Todd, in press). In describing
FC, Bara, Bucciarlelli, & Colle (2001) noted: “support initially starts from the child’s wrist and
is gradually moved to the elbow and shoulder until such a touch becomes merely symbolic,
and the facilitator’s hand lightly rests on the child’s leg.” (p. 225). To date, there is no
substantive evidence to support theory argued to underpin FC that the people who use the
method have an underlying movement disorder that warrants facilitation.
The body of peer-reviewed literature reviewing FC research produced in the past decade
helps clinicians in making evidence-based decisions on the technique (Lof, 2011; Mostert,
2001). Substantial evidence now exists, including well-designed controlled trials (see Gorman
et al., 2011, and Mostert, 2001) and two systematic reviews (Simpson, 2005; Wendt, 2009)
that facilitators influence the person’s message, and that they do so consciously and/or
unconsciously. FC has generated controversy as FC users’ communications have
contradicted preconceived beliefs of their abilities and the authorship of messages has been
questioned (Boynton, 2012; Cummins & Prior, 1992; Gorman et al., 2011; Intellectual
Disability Review Panel, IDRP, 1989; Todd, 2012; von Tetzchner, 2012). The continued
research interest in FC remains controversial. There have been recent attempts to use
sophisticated complex analyses (Bernadi & Tuzzi, 2011) and eye-gaze technology (Grayson
et al., 2011), but these have failed to provide a means to authenticate messages. While
proponents argue that FC may lead to independent communication, communication cannot
be considered independent while facilitation or rapid prompting is provided. Anecdotal reports
by people who communicate independently and claim to have previously used FC cannot be
ignored. They provide the lowest level of evidence in that there is no objective means to
substantiate reported benefits, and cannot be taken as generalizable evidence. As a result,
FC remains an approach with little supportive evidence and a preponderance of evidence
that contraindicates its use, and its use is not recommended.
Augmentative and Alternative Communication Clinical Guideline 30
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Speech pathologists need to be aware that the act of using FC to ‘facilitate’ a person to point
to letters, words, or messages might expose the person with complex communication needs
to undue influence, manipulation, and exploitation (Lof, 2011; Gorman et al., 2011). Harms
associated with FC pertain to its potential to remove a person’s communication rights (Todd,
2012; see UNCPRD, 2006), any negative consequences of the constructed messages not
reflecting their own views (see Gorman et al., 2011), and indirect harm by replacing time and
other resources that could be spent on effective interventions (Lof, 2011). The uncertain
authenticity of communication is central to cases involving allegations of abuse (see Boynton,
2012) and disputes over guardianship, or other decisions. In recognition of these
documented harms, professional and non-professional bodies have cautioned people against
the use of FC (e.g., American Academy of Pediatrics, 1998; American Psychological
Association, 1994; The Scottish Intercollegiate Guidelines Network, 2007; VALID, n.d).
Therefore, speech pathologists teaching, recommending, or practicing FC also need to be
aware of their own legal risk and/or liability in relation to potential or actual harms arising from
FC (Todd, 2012).
Speech pathologists have an ethical responsibility to inform their clients and families of the
lack of supportive evidence and evidence of known harms associated with FC in the
literature, including the harms of subconscious facilitator influence and false allegations of
sexual abuse, if FC is discussed (American Speech and Hearing Association, 1995; Todd,
2012). Furthermore, speech pathologists supporting people who use FC cannot assume that
messages communicated by FC are the person’s own messages. Speech pathologists have
an ethical responsibility to: (a) assess whether the communication is the person’s own
communication or has been influenced by the facilitator, and (b) explore all AAC system
access methods (including direct and indirect access) and strategies that allow the person to
communicate independently. In keeping with the principle that AAC includes all and multi-
modal forms of communication, all of the person’s methods of communicating must be taken
into account, including extant forms, such as, facial expression, body movements, and
vocalisations.
14.2 Mobile Technologies
The advent of ‘mobile technologies’ (i.e., touch screen devices that are readily available in
the community for relatively low cost) has been recognised as fundamentally shifting the field
and practice of AAC (AAC-RERC, 2010). Mobile devices are presently limited in both
accessibility and functionality in comparison to dedicated speech generating devices and
computer based software for communication. Research into the benefits of mobile devices
and AAC applications is also in an early phase (e.g., Niemeijer, Donnellan, & Robledo, 2012).
Speech pathologists have an ethical responsibility to explore all available AAC options and to
treat these equally in relation to the feature matching assessment. They also have an ethical
responsibility to (a) work with families who desire these devices and provide unbiased advice
in regards to the potential benefit to the person who uses AAC, and (b) take an evidence
Augmentative and Alternative Communication Clinical Guideline 31
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
based practice approach. Selection of AAC technology must be made with a basic premise of
AAC in mind: that is, that no one mode of communication has universal usefulness across all
people with complex communication needs, and no one technology will meet all of an
individual’s communication needs. Given the limitations of mobile technologies, it is highly
likely that for some populations mobile devices will not provide an appropriate substitute for
dedicated speech generating devices, which offer a range of additional features designed to
promote development of language and integration with other computer systems (AAC-RERC,
2010).
15. Conclusion
Communication touches every aspect of life and people with complex communication needs
may require assistance to fully participate in their chosen communities. Communication
needs and preferences change such that, over a person’s lifetime, different modes and
systems may become appropriate. Interventions need to have functional outcomes and be
delivered in locations that are meaningful for the individual with complex communication
needs, and maximise the potential for positive outcomes. Speech pathologists working with
individuals who would benefit from AAC are part of a team. They must be able to work
collaboratively and ensure that the individual with communication disability and his/her
family/supporters are central to all planning, assessment and intervention. The field of AAC is
expanding rapidly, requiring that speech pathologists are aware of resources, and regularly
reappraise their own skills in order to keep pace with these developments. They need to be
prepared to seek and share information, and adopt a life-long learning approach to this
exciting field.
16. Future Directions
The field of AAC will continue to advance with several factors affecting the roles of speech
pathologists, including: (a) a constantly expanding client group, as people who are ageing
acquire conditions affecting their communication, and as adults with lifelong disabilities age
and acquire conditions associated with ageing and/or experience changes in their social
networks; (b) advances in technology and ways people use computer technologies to
interact, including the expanding use of social media and online or virtual worlds in the field of
AAC; (c) changes in funding arrangements such as those proposed National Disability
Insurance Scheme, potentially impacting upon service models and decisions surrounding
AAC; and (d) the ongoing expansion of the evidence base in the field of AAC and multimodal
communication. In respect of these and other factors, future directions of speech pathologists
are expected to include:
Augmentative and Alternative Communication Clinical Guideline 32
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
• Advising government and industry in the communicative environments in which people
live on how to make local environments more communicatively accessible by the use
of readily available communication technologies.
• Assisting in the transfer of research into practice through actively engaging with
industry in the design and production of AAC, as developers seek expertise and
advice on products to suit a growing market.
• Contributing expertise, training, advice, and services in AAC for people in communities
affected by natural disasters, emergency situations, and mass evacuations in Australia
and the Asia-Pacific region. When a community is affected or displaced by a disaster,
demands increase rapidly for those people in the community with complex
communication needs who must get their message across to a range of new
communication partners (e.g., community volunteers, aid workers, emergency
services personnel). In these situations, speech pathologists may be called upon by
various agencies to provide training and population-based interventions to ensure the
safety and wellbeing of people with complex communication needs. Speech
pathologists may be asked to contribute to community disaster response plans, and
may need to be prepared to respond rapidly to requests for AAC support in local or
distant communities.
Across all sectors in the community, future directions of speech pathologists are likely to
include:
• Involvement in the development of AAC training courses and curriculum content for a
range of audiences including students of speech pathology and other professions,
qualified speech pathologists, family members, people with complex communication
needs, and industry members; and
• Input into any organisational, local, State and Federal Government policies and/or
procedures that may affect people with complex communication needs and their
communication partners.
17. Review
This paper should be reviewed five years from the date of ratification by Council.
Augmentative and Alternative Communication Clinical Guideline 33
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
18. Selected Resources on Augmentative and Alternative
Communication
Resources in this list appear in alphabetical order.
• ACOLUG http://aac-rerc.psu.edu/index.php/projects/show/id/18
• AGOSCI all information at www.agosci.org.au (site) www.twitter.com/agosci (Twitter)
• Augmentative and Alternative Communication, The International Journal of ISAAC,
published by Informa Healthcare. www.isaac-online.org/english/publications/aac
• Australian Rehabilitation & Assistive Technology Association (ARATA)
www.arata.org.au
• Australasian Society for Intellectual Disabilities (ASID) www.asid.asn.au
• Assistive Technology Support Services, Cerebral Palsy League, Queensland.
www.cplqld.org.au/services/equipment-technology/atss
• Communication Matrix www.communicationmatrix.org
• CP Tech, The Centre for Cerebral Palsy (TCCP), Western Australia,
www.cptech.com.au/CP_Tech_Home
• EVIDAAC Database of evidence in AAC: www.evidaac.org [forthcoming]
• International Society for Augmentative and Alternative Communication (ISAAC) all
information at www.isaac-online.org
• ISAAC-Australia www.twitter.com/isaacaus (Twitter) www.isaacaustralia.com (blog)
• International Classification of Functioning, Disability, and Health (ICF)
www.who.int/classifications/icf/en/ and ICF Children and Youth Version (ICF-CY)
www.icfcy.org/aac
• Independent Living Centres, Australia (ACT, QLD, NSW, SA, WA, Tasmania, Victoria)
www.ilcaustralia.org/home/default.asp
• Key Word Sign Australia www.newcastle.edu.au/kwsa
• Media Access Australia (www.mediaaccess.org.au)
• Scope Victoria Communication Resource Centre
www.scopevic.org.au/index.php/site/whatweoffer/communicationresourcecentre
• SpeechBITE Database of evidence in speech pathology: www.speechbite.com
• TASC Cerebral Palsy Alliance, NSW www.cerebralpalsy.org.au/our-
services/adults/tasc-technology-solutions-for-computer-access,-seating-and-
communications
• The AAC-RERC on Communication Enhancement http://aac-
rerc.psu.edu/index.php/site/index
• The Newell Network www.newell.org.au
Augmentative and Alternative Communication Clinical Guideline 34
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
19. References
Access Economics (2008). The Economic Impact of Cerebral Palsy in Australia in 2007.
Access Economics. Report by Access Economics Pty Limited for Cerebral Palsy Australia
Retrieved from
http://www.cpaustralia.com.au/index.php/cms/frontend/resource/id/78/name/access_economi
cs_report.pdf
American Academy of Pediatrics (1998) Committee on Children with Disabilities. Auditory
Integration Training and Facilitated Communication for Autism. Retrieved from:
http://pediatrics.aappublications.org/content/102/2/431.full
American Speech-Language-Hearing Association (1991). Augmentative and Alternative
Communication: What is AAC? Retrieved from:
http://www.asha.org/public/speech/disorders/aac.htm
American Speech-Language-Hearing Association (1995, March). Position statement -
facilitated communication. ASHA, 37 (Suppl.14), 22. Retrieved from:
http://www.asha.org/docs/html/ps1995-00089.html
American Psychological Association (1994). Resolution on facilitated communication.
Retrieved from: http://www.apa.org/divisions/div33/fcpolicy.html
Assistive Technology Act. (2004). United States Congress (Public Law 108–364). Retrieved
from: http://resnaprojects.org/nattap/library/laws/pl108-364.pdf
Balandin S. (2002) Message from the president. ISAAC Bulletin 67, February, p.2
Balandin, S. (2012) Dilemmas faced by speech pathologists working with people who use or
need AAC. Logos 65, maj 2012 , 5-8
Augmentative and Alternative Communication Clinical Guideline 35
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Balandin, S., & Goldbart, J. (2011). Qualitative research and AAC: Strong methods and new
topics. Augmentative and Alternative Communication, 27, 227–228.
Ballin, L., Balandin, S., Stancliffe, R. J., & Togher, L. (2010). The views of people who use
speech generating devices on mentoring new learners. Disability and Rehabilitation.
Assistive Technology. DOI: 10.3109/17483107.2011.573438
Bara. B.G, Bucciarlelli, M., & Colle, L. (2001). Communicative abilities in autism: Evidence for
attentional deficits. Brain and Language, 77, 216-240.
Bernardi, L., & Tuzzi, A. (2011). Analyzing written communication in AAC contexts: A
statistical perspective. Augmentative & Alternative Communication, 27, 183-194.
Beukelman, D. R., Ball, L., & Fager, S. (2008). An AAC personnel framework: adults with
acquired complex communication needs. Augmentative and Alternative Communication, 24,
255-267
Beukelman, D. R., Garrett, K., & Yorkston, K. (2007). Augmentative communication
strategies for adults with acute or chronic medical conditions. Baltimore, Maryland: Paul H.
Brookes.
Beukelman, D. R., & Mirenda, P. (2005). Supporting children and adults with complex
communication needs. 3rd Edition. Baltimore, Maryland: Paul H. Brookes.
Beukelman, D. R., & Mirenda, P. (Forthcoming). Supporting children and adults with complex
communication needs. 4th Edition. Baltimore, Maryland: Paul H. Brookes.
Blackstone, S. (2010). Communication access for children: The role of augmentative and
alternative communication technologies and strategies in pediatric rehabilitation. Journal of
Pediatric Rehabilitation Medicine: An Interdisciplinary Approach, 3, 247-250.
Augmentative and Alternative Communication Clinical Guideline 36
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Blackstone, S., & Hunt Berg, M. (2003). Social networks: A communication inventory for
individuals with complex communication needs and their communication partners.
Augmentative Communication Inc.
Boynton, J. (2012). Facilitated Communication—what harm it can do: Confessions of a
former facilitator. Evidence-Based Communication Assessment and Intervention. Available
online early, retrieved from:
http://www.tandfonline.com/doi/abs/10.1080/17489539.2012.674680
Branson, D., & Demchak, M. (2009). The use of augmentative and alternative communication
methods with infants and toddlers with disabilities: a research review. Augmentative and
Alternative Communication, 25, 274-86.
Bryen, D. N. & Wickman, C. H. (2011). Ending the silence of people with little or no functional
speech: Testifying in court. Disability Studies Quarterly. 31(4). Retrieved from: http://dsq-
sds.org/article/view/1711
Carr, E. G., Levin, L., McConnachie, G., Carlson, J. I., Kemp, D. C., & Smith, C. E (1994).
Communication-based intervention for problem behaviour. A user’s guide for producing
positive change. Baltimore: Paul H. Brookes.
Costigan, F. A., & Light, J. (2010) A review of preservice training in augmentative and
alternative communication for speech-language pathologists, special education teachers, and
occupational therapists. Assistive Technology, 22(4), 200-212;
Coupe-O’Kane, J., & Goldbart, J. (1998). Communication before speech: development and
assessment. London: David Fulton Publishers Limited.
Crossley, R (1994). Facilitated communication training. Teachers College Press, New York.
Augmentative and Alternative Communication Clinical Guideline 37
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Cummins, R. & Prior, M. (1992). Autism and assisted communication. A reply to Biklen.
Harvard Educational Review, 62, 228.
Dark, L.,(2010). “My life is getting smaller”: The experiences of loss and grief of older adults
with cerebral palsy and complex communication needs. Doctoral dissertation, The University
of Sydney.
Dew, A., Balandin, S., & Llewellyn, G. (2011). Using a life course approach to explore how
the use of AAC impacts on adult sibling relationships. Augmentative and Alternative
Communication, 27, 245–255.
Erickson, K. A., & Clendon, S. A. (2009). Addressing the literacy demands of the curriculum
for beginning readers and writers. In C. Zangari & G. Soto (Eds). Practically speaking:
Language, literacy, and academic development for students with AAC needs (pp. 195-215).
Baltimore: Paul H. Brookes.
Fried-Oken, M., Granlund, M. (2012).AAC and ICF: A good fit to emphasize outcomes.
Augmentative and Alternative Communication, 28, 1–2.
Goldsmith, S., Novak, I. (2010). What does our future hold?: Prognosis of cerebral palsy
systematic literature review. Developmental Medicine and Child Neurology, 52 (S2): 41
Gorman, B. J., Wynn, C. J., Morse, C. J. & Todd, J. T. (2011). Psychology and law in the
classroom: How the use of clinical fads in the classroom may awaken the educational
malpractice claim. Brigham Young Education and Law Journal, 1, 29-50.
Grayson, A., Emerson, A., Howard-Jones, P., & O'Neil, L. (2011). Hidden communicative
competence: Case study evidence using eye-tracking and video analysis. Autism, 15, 1-16.
Augmentative and Alternative Communication Clinical Guideline 38
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Hanson, E.K. (2007). Documentation in AAC using Goal Attainment Scaling. Perspectives on
Augmentative and Alternative Communication, 16, 6-9.
Hasson & Joffe (2007). The case for Dynamic Assessment in speech and language therapy.
Open access, retrieved from http://clt.sagepub.com/content/23/1/9.full.pdf+html
Hemsley, B. (2012). Ethical issues in augmentative and alternative communication. Journal
of Clinical Practice in Speech Language Pathology, 14(2), 88-92.
Hemsley, B., Balandin, S., & Togher, L. (2008). “We need to be the centrepiece”: Adults with
cerebral palsy and complex communication needs discuss the roles and needs of family
carers in hospital. Disability & Rehabilitation, 30, 1759-1771.
Hemsley, B., Worrall, L., & Balandin, S. (2011). Nursing the patient with complex
communication needs: Time as a barrier and a facilitator to successful communication in
hospital. Journal of Advanced Nursing, 68, 116-126.
Hines, M., Balandin, S., & Togher, L. (2011) Communication and AAC in the lives of adults
with autism: The stories of their older parents. Augmentative and Alternative Communication,
27, 256–266.
Iacono, T. (2004). Augmentative and alternative communitcation. In Reilly, S., Douglas, J. &
Oates, J. (Eds). Evidence based practice in speech pathology. Whurr Publishers, United
Kingdom.
Iacono, T. & Caithness, T. (2009). Assessment issues. In P. Mirenda & T. Iacono (Eds.),
Autism spectrum disorders and AAC (pp. 23-48). Baltimore: Paul H. Brookes.
Augmentative and Alternative Communication Clinical Guideline 39
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Iacono, T., Carter, M., & Hook, J. (1998). The identification of intentional communication in
children with severe and multiple disabilities. Augmentative and Alternative Communication,
14, 102-114.
Iacono, T., Lyon, K., Johnson, H., & West, D. (2012). Experiences of adults with complex
communication needs using low tech systems: An Australian context. Manuscript submitted
for publication.
Intellectual Disability Review Panel (IDRP). (1989). Report to the Director General on the
Reliability and Validity of Assisted Communication. Melbourne, Office of Intellectual Disability
Services.
Johnson, H., Douglas, J., Bigby, C., & Iacono, T. (2010). The pearl in the middle. A case
study of social relationships with an individual with a severe intellectual disability. Journal of
Intellectual and
Developmental Disability, 35 (3), 175-186. DOI: 10.3109/13668250.2010.501026.
Kaiser, A. P., Hester, P. P., & McDuffie, A. S. (2001). Supporting communication in young
children with developmental disabilities. Mental Retardation and Developmental Disabilities,
Research Reviews. 7, 143–150.
King, G., Law, M., King, S., Hurley, P., Rosenbaum, P., Hanna, S., Kertoy, M. & Young, N.
(2004). Children's Assessment of Participation and Enjoyment (CAPE) and Preferences for
Activities of Children (PAC). Pearson.
Kovach, T. M. (2009). Augmentative & Alternative Communication Profile: A Continuum of
Learning. Linguisystems.
Light, J. C. (1989). Towards a definition of communicative competence for individuals using
augmentative and alternative communication systems. Augmentative and Alternative
Communication, 5, 137-144.
Augmentative and Alternative Communication Clinical Guideline 40
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Light, J. C., Beukelman, D. R., & Reichle, J. (2003). Communicative Competence For
Individuals Who Use AAC: From Research To Effective Practice. Baltimore: Paul H. Brookes.
Light, J C., & McNaughton, D. (2009). Addressing the literacy demands of the curriculum for
conventional and more advanced readers and writers who require AAC. In C. Zangari & G.
Soto (Eds). Practically speaking: Language, literacy, and academic development for students
with AAC needs (pp. 217-245). Baltimore: Brookes.
Lloyd-Smith, W. (1997). EBP and Occupational Therapy. British Journal of Occupational
Therapy, 60, 474-478.
Lof, G.L. (2011). Science-based practice and the speech-language pathologist. International
Journal of Speech-Language Pathology. 13(3), 189-196.
Mostert, M. (2001). Facilitated Communication Since 1995: A review of published studies.
Journal of Autism and Developmental Disorders, Vol. 31, No. 3, 287-313.
McNaughton, D. B., & Beukelman, D. R. (2010). Transition Strategies for Adolescents and
Young Adults Who Use AAC. Baltimore, Maryland: Brookes Publishing.
Media Access Australia. (2012). Sociability: Social Media For People With A Disability. Media
Access Australia. Retrieved from
http://www.mediaaccess.org.au/sites/default/files/files/MAA2657-%20Report-
OnlineVersion.pdf
National Research Council. (2001). Educating children with autism. Washington, DC:
National Academies Press.
Niemeijer, D., Donnellan, M., & Robledo, J. A. (2012). Taking the Pulse of Augmentative and
Alternative Communication on iOS. Amsterdam, Netherlands: Assistive Ware.
Augmentative and Alternative Communication Clinical Guideline 41
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Pennington, L., Goldbart, J., & Marshall, J. (2004). Interaction training for conversational
partners of children with cerebral palsy: A systematic review. International Journal of
Language and Communication Disorders, 39, 151–170.
Perry, A., Reilly S., Bloomberg, K., & Johnson, H. (2002). An analysis of needs for people
with a disability who have complex communication needs. Melbourne, La Trobe University;
School of Human Communication Sciences, Bundoora 3086: 121.
Pless, M., & Granlund, M. (2012). Implementation of the International Classification of
Functioning, Disability and Health (ICF) and the ICF Children and Youth Version (ICF-CY)
Within the Context of Augmentative and Alternative Communication, 28, 11–20.
Rackensperger, T., Krezman, C., McNaughton, D., Williams, M. B., & D’Silva, K. (2005)
“When I first got it, I wanted to throw it off a cliff”: The challenges and benefits of learning
AAC technologies as described by adults who use AAC. Augmentative and Alternative
Communication, 21, 165-186.
Raghavendra, P., Olsson, C., Sampson, J., McInerney, R., & Connell, T. (2012). School
participation and social networks of children with complex communication needs, physical
disabilities and typically developing peers. Augmentative and Alternative Communication, 28,
33-43.
Raghavendra, P., Virgo, R., Olsson, C., Connell, T., & Lane, A. (2011). Activity participation
of children with complex communication need, physical disabilities and typically developing
peers. Developmental Neurorehabilitation, 14, 145-155.
Reilly, S. (2004) The move to evidence based practice in speech pathology. In Reilly, S.,
Douglas, J. & Oates, J. (2004). Evidence Based Practice in Speech Pathology. Whurr
Publishers, United Kingdom.
Augmentative and Alternative Communication Clinical Guideline 42
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Reilly, S., Douglas, J. & Oates, J. (2004). Evidence based practice in speech pathology.
Whurr Publishers, United Kingdom.
Rosengerg, S., & Beukelman, D. (1987). The participation model. In C.A. Coston (Ed.),
Proceedings of the national planners conference on assistive device service delivery (pp.
159-161). Washington DC: The Association for the Advancement of Rehabilitation
Technology.
Rowland, C., Fried-Oken, M., Steiner, S. A. M., Lollar, D., Phelps, R., Simeonsson, R. J., &
Granlund, M. (2012). Developing the ICF-CY for AAC Profile and Code Set for Children Who
Rely on AAC. Augmentative and Alternative Communication, 28, 21–32.
Satterfield, J., Spring, B., Brownson, R., Mullen, E., Newhouse, R., Walker, B., Whitlock, E.
(2009). Toward a transdisciplinary model of evidence-based practice, Milbank Quarterly, 87,
368-390.
Schlosser, R. (2000). The efficacy of augmentative and alternative communication: Towards
evidence based practice. Oxford, UK: Elsevier Science
Schlosser, R. W., Koul, R., & Costello, J. (2007). Asking well-built questions for evidence-
based practice in augmentative and alternative communication. Journal of Communication
Disorders, 40, 225–238.
Schlosser, R. W., & Lee, D. (2000). Promoting generalization and maintenance in
augmentative and alternative communication: A meta-analysis of 20 years of effectiveness
research. Augmentative and Alternative Communication, 16, 208–227.
Schlosser, R. W., & Raghavendra, P. (2004). Evidence-based practice in augmentative and
alternative communication. Augmentative and Alternative Communication, 20, 1-21.
Schlosser, R. W., & Sigafoos, J. (2006). Augmentative and alternative communication
interventions for persons with developmental disabilities: Narrative review of comparative
single-subject experimental studies. Research in Developmental Disabilities, 27, 1–29.
Augmentative and Alternative Communication Clinical Guideline 43
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Schlosser, R. W., & Wendt, O. (2008). Effects of augmentative and alternative
communication intervention on speech production in children with autism: a systematic
review. American Journal of Speech Language Pathology. 17, 212-30.
Schwartz, J. B., & Nye, C. (2006). A systematic review, synthesis, and evaluation of the
evidence for teaching sign language to children with autism. EBP Briefs, 1, 1–17
Scope. (2006). Too little too late: Wait times and cost burden for people with a disability in
seeking equipment funding in Victoria. Melbourne: Scope (Vic). Retrieved from:
http://www.scopevic.org.au/index.php/cms/frontend/resource/id/119
Scottish Intercollegiate Guidelines Network. (2007). Assessment, Diagnosis, and Clinical
Interventions for Children and Young People with Autism: A National Clinical Guideline.
Retrieved from: http://www.sign.ac.uk/pdf/sign98.pdf
Shane, H. C. (Ed.). (1994). Facilitated communication: The clinical and social phenomenon.
San Diego, CA: Singular Publishing.
Sigafoos, J., Arthur, M., & O’Reilly, (2003). Challenging behavior and developmental
disability. Baltimore: Brookes Publishing
Sigafoos, J., & Iacono, T. (1993). Selecting augmentative communication devices for persons
with severe disabilities: Some factors for educational teams to consider. Australia and New
Zealand Journal of Developmental Disabilities, 16, 133-146.
Simpson, R. L. (2005). Evidence-based practices and students with autism spectrum
disorders, Focus on Autism and Other Developmental Disorders, 20, 140-145.
Augmentative and Alternative Communication Clinical Guideline 44
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
Simpson, R. L., & Myles, B. S. (1995). Effectiveness of facilitated communication with
children and youth with autism. Journal of Special Education, 28, 424–439.
Smith, M. (2003). Literacy and Augmentative and Alternative Communication. Elsevier,
Academic Press Inc.
Speech Pathology Australia (forthcoming). Ethics education for Australian speech
pathologists. Melbourne: Speech Pathology Association of Australia.
Speech Pathology Australia (2002) Ethics education for Australian speech pathologists.
Melbourne: Speech Pathology Association of Australia. Retrieved from
http://www.speechpathologyaustralia.org.au/library/Ethics%20Education%20Package.pdf
Speech Pathology Australia (2002, 2009). Principles of Practice. Speech Pathology Australia.
Retrieved from:
http://www.speechpathologyaustralia.org.au/library/policies_and_procedures/11.07%20-
%20Principles%20of%20Practice.pdf
Speech Pathology Australia (2003). Scope of Practice in Speech Pathology. Speech
Pathology Australia. Retrieved from:
http://www.speechpathologyaustralia.org.au/library/Core_Assoc_Doc/Scope_of_Practice.pdf
Speech Pathology Australia (2010). Code of Ethics. Melbourne: Speech Pathology Australia.
Speech Pathology Australia (2011). Competency-Based Occupational Standards (CBOS) for
Speech Pathologists. Melbourne: Speech Pathology Australia.
Sutherland, D. E., Gillon, G. G., & Yoder, D. E. (2005). AAC use and service provision: a
survey of New Zealand speech-language therapists. Augmentative and Alternative
Communication, 21, 295-307
Augmentative and Alternative Communication Clinical Guideline 45
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
The Newell Network (2011). Telecommunication solutions for people with complex
communication needs. A web 2.0 approach to education and awareness www.newell.org.au
Retrieved from http://accan.org.au/files/Reports/The%20Newell%20Network%20-
short%20report.pdf
Todd, J.T. (in press). Rapid prompting. In F. R. Volkmar (Ed.) Encyclopedia of autism
spectrum disorders. London: Springer.
Todd, J. T. (2012). The moral obligation to be empirical: Comments on Boynton's “Facilitated
Communication-what harm can it do: Confessions of a former facilitator”. Evidence-Based
Communication Assessment and Intervention, DOI:10.1080/17489539.2012.704738
Trembath, D., Balandin, S., Stancliffe, R. J., & Togher, L. (2010). The experiences of adults
with complex communication needs who volunteer. Disability & Rehabilitation, 32(11), 875-
884.
UNCPRD (2006) United Nations Convention on the Rights of Persons with Disabilities.
Retrieved from: http://www.un.org/disabilities/default.asp?id=150
VALID (n.d). Position statement on the use of facilitated communication. Retrieved from:
http://valid.org.au/FCPosition/fc_position_statement.pdf
Van der Meer, L., Sigafoos, J., O’Reilly, M. F., & Lancioni, G. E. (2011). Assessing
preferences for AAC options in communication interventions. for individuals with
developmental disabilities: A review of the literature. Research in Developmental Disabilities,
32, 1422–1431.
Vanderheidan G., & Yoder, D. (1986). Overview. In S. Blackstone (Ed.), Augmentative
communication: An introduction. pp.1-28. Rockville, MD: American Speech-Language-
Hearing Association.
Augmentative and Alternative Communication Clinical Guideline 46
Copyright © 2012 The Speech Pathology Association of Australia Ltd
Speech Pathology Australia
von Tetzchner, S. (2012): Understanding facilitated communication: Lessons from a former
facilitator—Comments on Boynton, Evidence-Based Communication Assessment and
Intervention, DOI:10.1080/17489539.2012.699729
Watson, J. (2011). Listening to those rarely heard. Scope, Victoria. Retrieved from:
http://vimeo.com/21176882.
Wendt, O. (2009). The effectiveness of augmentative and alternative communication for
individuals with autism spectrum disorders: A systematic review and meta-analysis.
Dissertation.
World Health Organisation (2001). International Classification of Functioning, Disability, and
Health (ICF). World Health Organisation: Geneva. Retrieved from: http://www.who.int/icidh/
Augmentative and Alternative Communication Clinical Guideline 47
Copyright © 2012 The Speech Pathology Association of Australia Ltd
You might also like
- Triple CDocument2 pagesTriple CBethany Keily100% (1)
- A National Guideline For The Assessment and Diagnosis of Autism Spectrum Disorders in AustraliaDocument78 pagesA National Guideline For The Assessment and Diagnosis of Autism Spectrum Disorders in AustraliaCristinaNo ratings yet
- (P78, P80, P90, R50, P58, R30, R50-M, R100) API Programming (V1.2.5)Document196 pages(P78, P80, P90, R50, P58, R30, R50-M, R100) API Programming (V1.2.5)1234567890No ratings yet
- FINAL Parameters of PracticeDocument38 pagesFINAL Parameters of PracticeNathalia Dos ReisNo ratings yet
- Traquestomia PDFDocument25 pagesTraquestomia PDFFonoaudiólogaRancaguaNo ratings yet
- Infection Prevention and Control Guidelines For Audiology: March 2010Document35 pagesInfection Prevention and Control Guidelines For Audiology: March 2010Tamizaje Auditivo Luz FigueroaNo ratings yet
- Tracheostomy ManagementDocument25 pagesTracheostomy ManagementlogoioanninaNo ratings yet
- 3 041RS - Enhancing Capacity of Individuals With Autism To Use Public Transport - Final ReportDocument25 pages3 041RS - Enhancing Capacity of Individuals With Autism To Use Public Transport - Final ReportMimi RikNo ratings yet
- Speech Pathology in Mental Health Services: Clinical GuidelineDocument34 pagesSpeech Pathology in Mental Health Services: Clinical GuidelineDayannaNo ratings yet
- LG Podiatric AssessDocument73 pagesLG Podiatric AssessDarryl SetiawanNo ratings yet
- M I S P: Edical Nterpreting Tandards of RacticeDocument49 pagesM I S P: Edical Nterpreting Tandards of Racticejorge marinNo ratings yet
- Childhood Apraxsia of Speech Draft Position Paper 2023 - For ConsultationDocument34 pagesChildhood Apraxsia of Speech Draft Position Paper 2023 - For ConsultationeulavictoriawatsonNo ratings yet
- Restraints BPGDocument152 pagesRestraints BPGDicsy NithinNo ratings yet
- Mental Health Practice Standards For Nurses in Australian GeneralDocument32 pagesMental Health Practice Standards For Nurses in Australian GeneralHellen NaisangaNo ratings yet
- Practice Standards AND Guidelines For Dysphagia Intervention by Speech-Language PathologistsDocument38 pagesPractice Standards AND Guidelines For Dysphagia Intervention by Speech-Language PathologistsAlejandra Quezada GodoyNo ratings yet
- Clinical LaboratoryDocument24 pagesClinical Laboratorymoonfire2009100% (2)
- Enabling Clinical Supervision Skills (ECSS) : NSW North Coast ICTNDocument52 pagesEnabling Clinical Supervision Skills (ECSS) : NSW North Coast ICTNFransiscus RivaldyNo ratings yet
- Adnet Memory and Cognition Clinic GuidelinesDocument78 pagesAdnet Memory and Cognition Clinic GuidelinessalahouchenesalahNo ratings yet
- Dysphagia - Management in Adults and Children (Speech Pathology)Document22 pagesDysphagia - Management in Adults and Children (Speech Pathology)Valentina Jara Calderón100% (1)
- HVxTscc8wsoaj3FX Rk9whUXvjON1dzMq-National Guideline Response To Consultation Public SubmissionsDocument450 pagesHVxTscc8wsoaj3FX Rk9whUXvjON1dzMq-National Guideline Response To Consultation Public Submissionsannaota2021No ratings yet
- HWA Speech Pathologists in FocusDocument49 pagesHWA Speech Pathologists in Focuslinm@kilvington.vic.edu.auNo ratings yet
- B1639 Cinical Guide To Dentistry September 2023Document35 pagesB1639 Cinical Guide To Dentistry September 2023Michael WallNo ratings yet
- Iodinated Contrast Media GuidelineDocument41 pagesIodinated Contrast Media GuidelineN Aa100% (1)
- Ban or Restrict Mercury Amalgam Use To Safeguard Children Health in PakistanDocument112 pagesBan or Restrict Mercury Amalgam Use To Safeguard Children Health in PakistanQazi KamalNo ratings yet
- Australian Open Disclosure Framework Guide For ManagersDocument44 pagesAustralian Open Disclosure Framework Guide For Managersanita theresiaNo ratings yet
- Pastoral CareDocument92 pagesPastoral CareChy BuzzyNo ratings yet
- Coding For Lab SvcsDocument54 pagesCoding For Lab SvcsTintinNo ratings yet
- Pi Is 0161642016313781Document24 pagesPi Is 0161642016313781Jean PertiwiNo ratings yet
- Rational Use of Medicines in The ASEAN RegionDocument44 pagesRational Use of Medicines in The ASEAN RegionfredrickbryanbelandresNo ratings yet
- SmisedDocument143 pagesSmisedTaklu Marama M. BaatiiNo ratings yet
- Non-Surgical Rhinoplasty (Dario Bertossi, Riccardo Nocini, Ali Pirayesh) (Z-Library)Document164 pagesNon-Surgical Rhinoplasty (Dario Bertossi, Riccardo Nocini, Ali Pirayesh) (Z-Library)ALZAHRA AlkhutariNo ratings yet
- Autism NZ-Diagnostic-Practices Final-Report 2021Document152 pagesAutism NZ-Diagnostic-Practices Final-Report 2021Salar AmiriNo ratings yet
- CBOS 2011 Revised ATSI Content (Web 8 1)Document47 pagesCBOS 2011 Revised ATSI Content (Web 8 1)hms15No ratings yet
- Birhanu 1Document39 pagesBirhanu 1Birhanu AyenewNo ratings yet
- Standards For Sonographic Education v2.1 11-22Document70 pagesStandards For Sonographic Education v2.1 11-22Nisa HasanovaNo ratings yet
- SIGN 131 - Management of Schizophrenia: A National Clinical Guideline March 2013Document71 pagesSIGN 131 - Management of Schizophrenia: A National Clinical Guideline March 2013Septia Widya PratamaNo ratings yet
- Dysphagia GeneralDocument36 pagesDysphagia Generaljavi_marchiNo ratings yet
- Adha Standards08Document16 pagesAdha Standards08anasofiakNo ratings yet
- Review of The Research Report 2011 0Document170 pagesReview of The Research Report 2011 0Angel1331331No ratings yet
- Appearances - of - Power - Part 1Document216 pagesAppearances - of - Power - Part 1أحمد شوقيNo ratings yet
- Preventing and Mitigating Nurse Fatigue in Health Care BPGDocument67 pagesPreventing and Mitigating Nurse Fatigue in Health Care BPGleanneNo ratings yet
- 2000 2008 Oral Health Adult Public SectorDocument45 pages2000 2008 Oral Health Adult Public SectorIsra tanveerNo ratings yet
- Implementing The Australian Open Disclosure Framework in Small PracticesDocument39 pagesImplementing The Australian Open Disclosure Framework in Small Practicesfernandestainara234No ratings yet
- AIOH Position Paper Occupational Noise and Its Potential for Health IssuesDocument15 pagesAIOH Position Paper Occupational Noise and Its Potential for Health Issuesrobertgolec3No ratings yet
- Secure Rooms and Seclusion Standards and Guidelines:: A Literature and Evidence ReviewDocument59 pagesSecure Rooms and Seclusion Standards and Guidelines:: A Literature and Evidence ReviewRoegie LeppagoNo ratings yet
- Kirankumarkrishanappa 2018Document28 pagesKirankumarkrishanappa 2018Nur WahyuniNo ratings yet
- GPR English Language 2014Document33 pagesGPR English Language 2014brendaNo ratings yet
- Speech Pathology Workforce Analysis Report 2023Document28 pagesSpeech Pathology Workforce Analysis Report 2023ramp275No ratings yet
- UCAT UK HandbookDocument118 pagesUCAT UK Handbookjczy4zkkwdNo ratings yet
- Dementia Clinical Network ReportDocument11 pagesDementia Clinical Network ReportZekel HealthcareNo ratings yet
- SG3 SpeechDocument57 pagesSG3 SpeechDian SariNo ratings yet
- UCAT HandbookDocument128 pagesUCAT HandbookWISE EducationNo ratings yet
- OD Standard 2008Document48 pagesOD Standard 2008Ronny BudimanNo ratings yet
- ClinhovrlitrevDocument40 pagesClinhovrlitrevNoviarta TokNo ratings yet
- Code of Conduct For NursesDocument21 pagesCode of Conduct For Nursespaul.ubudNo ratings yet
- CDC Infection Prevention Practices 2016Document44 pagesCDC Infection Prevention Practices 2016Hayes MaineNo ratings yet
- CDC Infection Prevention Practices 2016Document44 pagesCDC Infection Prevention Practices 2016Hayes MaineNo ratings yet
- Australian Feldenkrais GuildDocument90 pagesAustralian Feldenkrais Guildatste100% (1)
- TENA GuíaDocument45 pagesTENA Guíadra aidaduaguirreNo ratings yet
- Basic Guide to Dental InstrumentsFrom EverandBasic Guide to Dental InstrumentsRating: 2.5 out of 5 stars2.5/5 (3)
- We Were Just Kind of Handed It and Then It Was Smoke Bombed by EveryoneDocument11 pagesWe Were Just Kind of Handed It and Then It Was Smoke Bombed by EveryoneBethany KeilyNo ratings yet
- Yes - No Gayle PorterDocument8 pagesYes - No Gayle PorterBethany KeilyNo ratings yet
- I've Had A Love Hate I Mean Mostly Hate Relationship With These PODD Books Parent Perceptions of How They and Their Child Contributed To AACDocument12 pagesI've Had A Love Hate I Mean Mostly Hate Relationship With These PODD Books Parent Perceptions of How They and Their Child Contributed To AACBethany KeilyNo ratings yet
- Ipad Apps For Complex Communication Support NeedsDocument1 pageIpad Apps For Complex Communication Support NeedsBethany KeilyNo ratings yet
- Participation Model For Augmentative and Alternative CommunicationDocument1 pageParticipation Model For Augmentative and Alternative CommunicationBethany KeilyNo ratings yet
- Periodic Table of AacDocument1 pagePeriodic Table of AacBethany KeilyNo ratings yet
- Choosing A Communication Device: Considerations and Feature MatchingDocument5 pagesChoosing A Communication Device: Considerations and Feature MatchingBethany KeilyNo ratings yet
- Recommendation For BSP AwardsDocument7 pagesRecommendation For BSP AwardsNerlie CruzNo ratings yet
- Factors Influencing Child DevelopmentDocument17 pagesFactors Influencing Child DevelopmentMuhammad Zulfadhli0% (1)
- Daily RoutinesDocument8 pagesDaily RoutinesMaría LuisaNo ratings yet
- 1º Teste 10.1D Correction V2Document3 pages1º Teste 10.1D Correction V2Duarte PereiraNo ratings yet
- Snapshot Chapter 5 Mother's DayDocument7 pagesSnapshot Chapter 5 Mother's Dayprateekm698No ratings yet
- Math g5 m4 Mid Module AssessmentDocument11 pagesMath g5 m4 Mid Module AssessmentTimNo ratings yet
- Student Development TheoryDocument9 pagesStudent Development Theoryapi-326536311No ratings yet
- Joven, Angelica P. - The Nature of Reading SkillsDocument38 pagesJoven, Angelica P. - The Nature of Reading SkillsAlec Palcon JovenNo ratings yet
- Cassandra Dyson Benchmark Reviving The Professional Culture 02142024Document9 pagesCassandra Dyson Benchmark Reviving The Professional Culture 02142024api-683979133No ratings yet
- 4O02601Document3 pages4O02601Faraz AnsariNo ratings yet
- Indian School of ActingDocument10 pagesIndian School of ActingAshwani AhujaNo ratings yet
- PMAI Sample ReportDocument6 pagesPMAI Sample ReportchidambaraNo ratings yet
- Margherita Spagnuolo Lobb, Pietro Andrea Cavaleri - Psychopathology of The Situation in Gestalt Therapy - A Field-Oriented Approach-Routledge (2023)Document317 pagesMargherita Spagnuolo Lobb, Pietro Andrea Cavaleri - Psychopathology of The Situation in Gestalt Therapy - A Field-Oriented Approach-Routledge (2023)mariammatchavariani9No ratings yet
- Solving Multi-Step Word Problems With Rounding and Assessing The Reasonableness of The AnswersDocument8 pagesSolving Multi-Step Word Problems With Rounding and Assessing The Reasonableness of The Answersapi-378876175No ratings yet
- 2nd Quarter Full DLLDocument44 pages2nd Quarter Full DLLAnonymous b0U0Mj2GNZNo ratings yet
- Field Site VisitsDocument11 pagesField Site Visitsapi-700032483No ratings yet
- Intrinsic vs. Extrinsic Motivational Orientations and The Volunteer ProcessDocument6 pagesIntrinsic vs. Extrinsic Motivational Orientations and The Volunteer ProcessClaudia BNo ratings yet
- The Life and Works of Dr. Jose P3Document2 pagesThe Life and Works of Dr. Jose P3Jaytone HernandezNo ratings yet
- Maths Circle Theorem HWDocument16 pagesMaths Circle Theorem HWwcv2rs255j100% (1)
- A 7-Level Single DC Source Cascaded H-Bridge Multilevel Inverter Control Using Hibrid ModulationDocument6 pagesA 7-Level Single DC Source Cascaded H-Bridge Multilevel Inverter Control Using Hibrid ModulationYeisson MuñozNo ratings yet
- New B.pharm 2017 18 OnwardsDocument112 pagesNew B.pharm 2017 18 OnwardsHenna TkNo ratings yet
- 1 2020 General Prospectus With CoverDocument271 pages1 2020 General Prospectus With CoverChris WebbNo ratings yet
- Discrete MathematicsDocument3 pagesDiscrete MathematicsMohd Shahril100% (1)
- Rapid Interpretation of EKG Sixth E Dition by by Dale Dubin: Direct DownloadDocument4 pagesRapid Interpretation of EKG Sixth E Dition by by Dale Dubin: Direct DownloadAlex HirschNo ratings yet
- Mathematics STD 7A RAHAT MARTUZA RAFINDocument4 pagesMathematics STD 7A RAHAT MARTUZA RAFINAkhlak HossainNo ratings yet
- An Integrated Rectangular Dielectric Resonator AntennaDocument4 pagesAn Integrated Rectangular Dielectric Resonator AntennaThiripurasundari DNo ratings yet
- IdiomaticityDocument85 pagesIdiomaticityIrina Bicescu100% (1)
- Social LearningDocument6 pagesSocial LearningMariel IliganNo ratings yet
- UGC NET Career ScopeDocument12 pagesUGC NET Career ScopeKadamb SachdevaNo ratings yet