Professional Documents
Culture Documents
Lucy Clooney
Lucy Clooney
Uploaded by
syed danish aliOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lucy Clooney
Lucy Clooney
Uploaded by
syed danish aliCopyright:
Available Formats
Writing Test - Doctor
Time Allow ed - 40 minutes
Read the case notes below and complete the writing task which follows.
Patient'sname : Mrs. Lucy Clooney d.o.b. 18 April 1955
Social History : Bank manager, Heavy smoker ( 20 cigarettes daily for 30
years ), drinks alcohol occasionally
Past Medical History : Mild hypertension, Not taking medication regularly,
moderately overweight
18/8/2009
Subjective : discomfort in upper abdomen, burning sensation at the same
area since her early 20s, difficulty in swallowing solid foods. especially meat &
bread, Liquid- no problem, no nausea, no vomiting, not associated with
hoarseness of voice
Objective : pulse rate- 80/ min, BP- 135/85, no cervical lymph node swelling,
chest & abdomen- unremarkable, not clinically anaemic or jaundiced
Assessment : Dysphagia due to either hiatus hernia or other organic lesions
in oesophagus
Plan : explain the possible diagnosis, advise to stop smoking & to adjust her
life style, to consider further investigations for definitive diagnosis, review in 2
weeks
20/11/2009
Subjective : missed review visit, her symptoms- worsened, increasing
difficulty in swallowing, now regurgitated undigested solid foodstuffs but no
pain on swallowing, concerned about her weight loss ( 5 kg in 3 months ) ,
Antacid taken by self - not effective
Objective : examination - normal, rectal & abdominal - normal, no peripheral
oedema
Assessment : Hiatus hernia or mass in oesophagus
Plan : CXR, ECG, Endoscopy & Biopsy, refer to surgeon if abnormality found
25/11/2009
Subjective ; all symptoms- not improved, cough at night , sometimes being
woken from sleep, productive of clear sputum, not bile or blood stained, no
history of angina, shortness of breath, ankle swelling
Objective ; examination- still normal, no signs of maligancy, CXR- no
evidence of aspiration pneumonia, ECG- normal, Endoscopy- oesophagitis &
stricture at 36cm from incisor teeth showing small hiatus hernia, Biopsy -
consistent with oesophagitis & no malignancy identified
Assessment : Barette's oesophagus
Plan : lifestyle change ( smoking, drinking alcohol & stress ) , Gaviscon 30 ml
& Omeprazole 40 mg daily, repeat endoscopy at 6-8 weeks' time, to undergo
operation if malignancy is detected
23/1/2010
Subjective : now asymptomatic but continue to take regular omeprazole, She
wants to stop therapy , taking on board the lifestyle change , stopped
smoking, worried to take tablets for the rest of life
Objective : no abnormality found
Plan : refer to GI surgeon for assessment for operation ( fundoplication )
Writing Task
Using the information in the case notes, write a letter of referral to Dr. Harry
Smith at the Royal Melbourne Hospital, Flemington Road, Parkville 3050. In
your answer, expand the relevant case notes into complete sentences. Do not
use note form. The body of letter should be approximately 180-200 words.
Use correct letter format.
You might also like
- Esther ParksDocument6 pagesEsther ParksMyrnaivette Pierson63% (19)
- SOAP Note DiabetesDocument16 pagesSOAP Note Diabetesmichael thorn92% (25)
- Case Study On Jaundice With AnswersDocument4 pagesCase Study On Jaundice With Answersabirami pNo ratings yet
- 15casebook in Gastroenterology PDFDocument109 pages15casebook in Gastroenterology PDFKMNo ratings yet
- Nursing Care Planpulmonary TuberculosisDocument20 pagesNursing Care Planpulmonary Tuberculosisgandhialpit100% (5)
- SOAP NoteDocument26 pagesSOAP Noteapi-376765485% (13)
- Health and Fitness: Learner's WorksheetDocument8 pagesHealth and Fitness: Learner's WorksheetMarianelaGomezNo ratings yet
- Growing With The Garden: A Curriculum For Practicing Horticulture With Incarcerated IndividualsDocument179 pagesGrowing With The Garden: A Curriculum For Practicing Horticulture With Incarcerated Individualscalderdavid35No ratings yet
- Six Sigma Black Belt Project ExampleDocument26 pagesSix Sigma Black Belt Project ExampleSelvakumar Raju100% (1)
- CPC Case Study NoDocument15 pagesCPC Case Study NoRhaffy Bearneza RapaconNo ratings yet
- H&P FormatDocument7 pagesH&P FormatRaffy Gutman100% (1)
- Chief Complaint: HematocheziaDocument9 pagesChief Complaint: Hematocheziarenne elleNo ratings yet
- Case 9 CPT 3a2Document77 pagesCase 9 CPT 3a2Jack Ortega PuruggananNo ratings yet
- Case Report, General SurgeryDocument36 pagesCase Report, General Surgeryalnoooor38No ratings yet
- Ca Stomach: Under The Guidance of Professor DR J A Jayalal M.SDocument11 pagesCa Stomach: Under The Guidance of Professor DR J A Jayalal M.STheoder RobinsonNo ratings yet
- Ca StomachDocument33 pagesCa StomachAdvaith DevanandNo ratings yet
- Case of Obstructive JaundiceDocument23 pagesCase of Obstructive JaundiceAjay Agrawal100% (1)
- My Notebook - Microsoft OneNote OnlineDocument3 pagesMy Notebook - Microsoft OneNote Onlineatharva sawantNo ratings yet
- Wk7 IhumanDocument8 pagesWk7 IhumanPesh B NimmoNo ratings yet
- Upper Gastro Intestinal BleedingDocument11 pagesUpper Gastro Intestinal BleedingSyima MnnNo ratings yet
- 11.obstructive JaundiceDocument27 pages11.obstructive JaundiceHeng Kai NeoNo ratings yet
- Diagnosticoclinico 1Document11 pagesDiagnosticoclinico 1Kimberlin EliasNo ratings yet
- Wa0008.Document14 pagesWa0008.Mahendra NitharwalNo ratings yet
- Case Write Up Report 5 Umbilical Hernia: SURGERY 1-2022/2023Document6 pagesCase Write Up Report 5 Umbilical Hernia: SURGERY 1-2022/2023RSNo ratings yet
- M1 MET1 SG ACaseofAcuteCholecystitisDocument14 pagesM1 MET1 SG ACaseofAcuteCholecystitisNicholas ReljaNo ratings yet
- Nguyen-L-How Fasting May Have Impacted A Patient With AmyloidosisDocument21 pagesNguyen-L-How Fasting May Have Impacted A Patient With Amyloidosisapi-326828206No ratings yet
- Case StudyDocument4 pagesCase StudyFarjana MalikNo ratings yet
- d2 - Milla Telemed - Written Report 3Document4 pagesd2 - Milla Telemed - Written Report 3Gabriel MillaNo ratings yet
- Surg Week 4Document75 pagesSurg Week 4Casey YanoNo ratings yet
- Case Presentation Lump Right HypochondriumDocument22 pagesCase Presentation Lump Right HypochondriumNANDAN RAINo ratings yet
- Abdominal Case Study CompiledDocument392 pagesAbdominal Case Study CompiledIshak IzharNo ratings yet
- Acute Care Patient Case Example: CC: Hpi: Medical History: Medication History: Allergies: NKDADocument7 pagesAcute Care Patient Case Example: CC: Hpi: Medical History: Medication History: Allergies: NKDAخلودخلودNo ratings yet
- PatientDocument4 pagesPatientParashmani SharanNo ratings yet
- HyperDocument21 pagesHyperayamalkawi204No ratings yet
- Definition and Etiology: PancreatitisDocument24 pagesDefinition and Etiology: PancreatitisAliyah Tofani PawelloiNo ratings yet
- Written Report 3Document4 pagesWritten Report 3Gabriel MillaNo ratings yet
- Wa0001.Document33 pagesWa0001.kmstt780No ratings yet
- A Rather Yellow Looking LadyDocument6 pagesA Rather Yellow Looking LadyMarios GhobrialNo ratings yet
- Transcribed HWDocument2 pagesTranscribed HWnikka aquinoNo ratings yet
- HepatoDocument6 pagesHepatoMohamad MostafaNo ratings yet
- MedicineDocument4 pagesMedicineDianne Camille Ardenaso GasparNo ratings yet
- GI Case Studies-StudentDocument7 pagesGI Case Studies-StudentRhina FutrellNo ratings yet
- Epigastric Pain (Up Date) Masroel GontarDocument52 pagesEpigastric Pain (Up Date) Masroel GontarTaufik Akbar Faried Lubis50% (2)
- PBL Als 02Document7 pagesPBL Als 02Danial MazukiNo ratings yet
- PBL Als 02Document7 pagesPBL Als 02Danial MazukiNo ratings yet
- GASTROINTESTINAL-DISORDER Activity CaseDocument4 pagesGASTROINTESTINAL-DISORDER Activity Casedenebrench23No ratings yet
- Case Illustration: TH THDocument6 pagesCase Illustration: TH THdigimon666No ratings yet
- Esophagus and Stomach NotesDocument15 pagesEsophagus and Stomach Noteslizzy596No ratings yet
- Oldcart - Case #1Document4 pagesOldcart - Case #1BRANDON SANNo ratings yet
- Surgery Case WriteDocument2 pagesSurgery Case WriteDat PhamNo ratings yet
- Clinical CasesDocument12 pagesClinical CasesAndreea HanuNo ratings yet
- Young Lady With Severe Generalized Abdominal Pain (2Document33 pagesYoung Lady With Severe Generalized Abdominal Pain (2najeeb.arbani027No ratings yet
- Rational Drug Used For Gastrointestinal DisorderDocument2 pagesRational Drug Used For Gastrointestinal DisorderZahrosofi AhmadahNo ratings yet
- P Drug Q PostingDocument1 pageP Drug Q PostingRitika AgrawalNo ratings yet
- CFGVDocument28 pagesCFGVmyolie wuNo ratings yet
- ImplementationDocument3 pagesImplementationSittie Hafsah L. MasbodNo ratings yet
- A Case On Periampullary Carcinoma.: Presented by DR Sumaiya Tasnim TanimaDocument34 pagesA Case On Periampullary Carcinoma.: Presented by DR Sumaiya Tasnim TanimaJobaer MahmudNo ratings yet
- GDM With PolyhydramniosDocument4 pagesGDM With PolyhydramniosSure NavyasriNo ratings yet
- 1st Family Medicine Class CasesDocument7 pages1st Family Medicine Class Casesdr.jan.zadigNo ratings yet
- TrammellsoapnoteadultDocument9 pagesTrammellsoapnoteadultapi-284269118No ratings yet
- BJM Mcqs.... 11-09-2023Document14 pagesBJM Mcqs.... 11-09-2023Kiran ShahNo ratings yet
- Case Scenario Peptic UlcerDocument2 pagesCase Scenario Peptic Ulcerchetankumarbhumireddy0% (1)
- World Pumps Volume 1995 Issue 349 1995 (Doi 10.1016/s0262-1762 (99) 81154-7) - Igor J. Karassik (1911-1995) PDFDocument2 pagesWorld Pumps Volume 1995 Issue 349 1995 (Doi 10.1016/s0262-1762 (99) 81154-7) - Igor J. Karassik (1911-1995) PDFvcockscribdNo ratings yet
- p1 SummativeDocument3 pagesp1 Summativeapi-346594405No ratings yet
- Test 6Document16 pagesTest 6Ale FigueroaNo ratings yet
- CC15 Laminar FlowDocument22 pagesCC15 Laminar Flow999impactNo ratings yet
- Nejmoa 2210027Document12 pagesNejmoa 2210027Iris N MNo ratings yet
- Cognitive Processing TherapistDocument219 pagesCognitive Processing Therapistdrorgarbi100% (1)
- WP - Demystifying The Demo Solution LandscapeDocument6 pagesWP - Demystifying The Demo Solution LandscapeJigar VikamseyNo ratings yet
- BBC Knowledge 201506Document98 pagesBBC Knowledge 201506Victor CameronNo ratings yet
- 1 Peter Study GuideDocument38 pages1 Peter Study Guidepastor_steve100% (1)
- BLEACH Charac Part 1.Document53 pagesBLEACH Charac Part 1.Al LanNo ratings yet
- Stories of Sahabah Volume1Document255 pagesStories of Sahabah Volume1shumayounNo ratings yet
- Homework 3 - Solutions: Complex VariablesDocument2 pagesHomework 3 - Solutions: Complex VariablesderlavaiNo ratings yet
- Bài giảng Ngữ âm lý thuyết EHOU Bài 4Document4 pagesBài giảng Ngữ âm lý thuyết EHOU Bài 4tranthanhtambrNo ratings yet
- My MP ThreadDocument52 pagesMy MP ThreadksathisNo ratings yet
- Speech TextDocument4 pagesSpeech Textcici clardianNo ratings yet
- 1964 Constitution of AfghanistanDocument3 pages1964 Constitution of AfghanistanViet EngineeringNo ratings yet
- HE Beauty Care IDocument61 pagesHE Beauty Care IFrancis A. Buenaventura100% (1)
- MSC in Chemical Engineering: WWW - Nottingham.Ac - Uk/ChemenvDocument2 pagesMSC in Chemical Engineering: WWW - Nottingham.Ac - Uk/ChemenvphdzedeNo ratings yet
- Extra Language Practice: TravelDocument3 pagesExtra Language Practice: Travelana maria csalinasNo ratings yet
- Rethinking American Grand Strategy Elizabeth Borgwardt All ChapterDocument67 pagesRethinking American Grand Strategy Elizabeth Borgwardt All Chaptertodd.schrader522100% (19)
- Topic VI PM and ExecutivesDocument30 pagesTopic VI PM and ExecutivesalibabaNo ratings yet
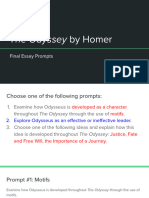
- Student Directions Odyssey - Final Essay PromptsDocument10 pagesStudent Directions Odyssey - Final Essay PromptsJanie MackNo ratings yet
- Philosophy DLLDocument10 pagesPhilosophy DLLGiljohn SoberanoNo ratings yet
- Commercial Bulding Energy Audit PDFDocument33 pagesCommercial Bulding Energy Audit PDFeselco ingenieros100% (1)
- Lecture Notes On Polya's Problem Solving StrategyDocument20 pagesLecture Notes On Polya's Problem Solving StrategyJohn Asher Josh AguinilloNo ratings yet
- Dialog Diabetes B.inggris Kel 5-1Document4 pagesDialog Diabetes B.inggris Kel 5-1Desma LindaNo ratings yet
- PU For Plasticizer PVCDocument22 pagesPU For Plasticizer PVCAnnisa RakhmaNo ratings yet