Professional Documents
Culture Documents
Ar11feb 13
Ar11feb 13
Uploaded by
Jenny ConsignadoCopyright:
Available Formats
You might also like
- Informative Formal SpeechDocument3 pagesInformative Formal SpeechAlba Quintanilla100% (1)
- 1 s2.0 S1028455909600802 MainDocument3 pages1 s2.0 S1028455909600802 MainSuminten S. Pd.No ratings yet
- Uterine Inversion: A Life-Threatening Obstetric Emergency: Dawn R. Hostetler, MD, and Michael Bosworth, DODocument4 pagesUterine Inversion: A Life-Threatening Obstetric Emergency: Dawn R. Hostetler, MD, and Michael Bosworth, DOAndi Farras WatyNo ratings yet
- Placenta Increta Causing Um in The 26th Week of Pregnancy 2Document3 pagesPlacenta Increta Causing Um in The 26th Week of Pregnancy 2Kester ApostolNo ratings yet
- Case Report: Postpartum Uterine Wound Dehiscence Leading To Secondary PPH: Unusual SequelaeDocument4 pagesCase Report: Postpartum Uterine Wound Dehiscence Leading To Secondary PPH: Unusual SequelaemelisaberlianNo ratings yet
- Recurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoDocument2 pagesRecurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoeditorijmrhsNo ratings yet
- 1-4 HalamannnnDocument4 pages1-4 HalamannnnJulian Auparai WorabayNo ratings yet
- Case Report: Ruptured Ectopic Pregnancy in Caesarean Section Scar: A Case ReportDocument3 pagesCase Report: Ruptured Ectopic Pregnancy in Caesarean Section Scar: A Case ReportEga MegawatiNo ratings yet
- مرجع 2Document4 pagesمرجع 2Ahmed AnwarNo ratings yet
- Girija BS, Sudha TR: AbstractDocument4 pagesGirija BS, Sudha TR: AbstractALfuNo ratings yet
- Ectopic Pregnancy - StatPearls - NCBI BookshelfDocument9 pagesEctopic Pregnancy - StatPearls - NCBI BookshelfKatherine DavilaNo ratings yet
- Ruptured Ectopic Pregnancy in The Presence of An Intrauterine DeviceDocument5 pagesRuptured Ectopic Pregnancy in The Presence of An Intrauterine DevicePatrick NunsioNo ratings yet
- PEBDocument4 pagesPEBDR RISKA WAHYUNo ratings yet
- Case Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyDocument4 pagesCase Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyChidimma VictoryNo ratings yet
- Uterine Rupture in Nulliparous Woman Without Risk Factors: A Case Report and Literature ReviewDocument6 pagesUterine Rupture in Nulliparous Woman Without Risk Factors: A Case Report and Literature ReviewBOHR International Journal on GynaecologyNo ratings yet
- Cesarean Scar Ectopic Pregnancies: Etiology, Diagnosis, and ManagementDocument9 pagesCesarean Scar Ectopic Pregnancies: Etiology, Diagnosis, and ManagementDinorah MarcelaNo ratings yet
- Primary Ovarian Abscess in Pregnancy: Case ReportDocument3 pagesPrimary Ovarian Abscess in Pregnancy: Case ReportVinnyRevinaAdrianiNo ratings yet
- Ectopic Pregnancy: A ReviewDocument13 pagesEctopic Pregnancy: A ReviewDinorah MarcelaNo ratings yet
- Cesarean Scar Pregnancies and Their ManagementDocument7 pagesCesarean Scar Pregnancies and Their ManagementClinton SitanggangNo ratings yet
- Abrasio PlacentaDocument3 pagesAbrasio Placentamuhammad azamNo ratings yet
- Challenges in The Management of A Case of 2nd Abdominal Pregnancy - OJOG - 2015092815302981Document3 pagesChallenges in The Management of A Case of 2nd Abdominal Pregnancy - OJOG - 2015092815302981Stella Putri WandaNo ratings yet
- Obstetrics 2Document6 pagesObstetrics 2najmulNo ratings yet
- Gynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernDocument3 pagesGynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernIrvin MarcelNo ratings yet
- Ectopic Pregnancy - StatPearls - NCBI BookshelfDocument6 pagesEctopic Pregnancy - StatPearls - NCBI BookshelfLaura valentina ramos mezaNo ratings yet
- Tubalpregnancy DiagnosisandmanagementDocument12 pagesTubalpregnancy DiagnosisandmanagementAndreaAlexandraNo ratings yet
- Uterine Rupture: A Catastrophic Obstetric EmergencyDocument2 pagesUterine Rupture: A Catastrophic Obstetric EmergencyImtihanamiseNo ratings yet
- Tambimuttu 2015Document2 pagesTambimuttu 2015cristian vivasNo ratings yet
- Hem 2020000139 CDocument5 pagesHem 2020000139 CA.21-AH0602- VINA SHALSABINANo ratings yet
- Anesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaDocument4 pagesAnesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaHanayuki VizureiNo ratings yet
- Ectopic Pregnancy - MedscapeDocument31 pagesEctopic Pregnancy - Medscapeantonio91uNo ratings yet
- Expectatant Management of Cesarean Scar Ectopic PregnancyDocument5 pagesExpectatant Management of Cesarean Scar Ectopic PregnancyEricNo ratings yet
- PlasentaDocument4 pagesPlasentaLois YunikeNo ratings yet
- 9.radha Et Al.Document3 pages9.radha Et Al.International Journal of Clinical and Biomedical Research (IJCBR)No ratings yet
- The Back Alley Revisited: Sepsis After Attempted Self-Induced AbortionDocument3 pagesThe Back Alley Revisited: Sepsis After Attempted Self-Induced Abortionmila nurmalaNo ratings yet
- PIIS0015028219304844Document2 pagesPIIS0015028219304844nighshift serialsleeperNo ratings yet
- Minakshi S. Neglected Puerperal Inversion of The Uterus Ignorance Makes Acute A Chronic FormDocument4 pagesMinakshi S. Neglected Puerperal Inversion of The Uterus Ignorance Makes Acute A Chronic FormJulius Albert SNo ratings yet
- Ovarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014Document4 pagesOvarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014alif bagusNo ratings yet
- Case Report Rare Cesarean Section Scar Ectopic Pregnancy Successfully Treated by Methotrexate: A CaseDocument5 pagesCase Report Rare Cesarean Section Scar Ectopic Pregnancy Successfully Treated by Methotrexate: A Casemustafaali9711No ratings yet
- Anesthesia For Foetal Surgery: Dr. Athira S MadhuDocument98 pagesAnesthesia For Foetal Surgery: Dr. Athira S MadhuAthira S MadhuNo ratings yet
- A Rare Case of Morbidly Adherent Placenta in A Young - 2024 - International JouDocument4 pagesA Rare Case of Morbidly Adherent Placenta in A Young - 2024 - International JouRonald QuezadaNo ratings yet
- Scar Ectopic Case ReportDocument6 pagesScar Ectopic Case ReportMominah MayamNo ratings yet
- Total and Acute Uterine Inversion After Delivery A Case Report PDFDocument4 pagesTotal and Acute Uterine Inversion After Delivery A Case Report PDFatika sgrtNo ratings yet
- 1 s2.0 S0090825804003610 Main PDFDocument3 pages1 s2.0 S0090825804003610 Main PDFRirin WahyuniNo ratings yet
- UC Irvine: Clinical Practice and Cases in Emergency MedicineDocument6 pagesUC Irvine: Clinical Practice and Cases in Emergency MedicinePatrick NunsioNo ratings yet
- Abnormal PlacentationDocument9 pagesAbnormal PlacentationJack BladeNo ratings yet
- Ectopic Pregnancy22Document43 pagesEctopic Pregnancy22Sunil YadavNo ratings yet
- Juhi Abstract QuestDocument2 pagesJuhi Abstract QuestjuhiNo ratings yet
- Ectopic PregnancyDocument39 pagesEctopic PregnancyFecky Fihayatul IchsanNo ratings yet
- Postpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiDocument4 pagesPostpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiAstrit GashiNo ratings yet
- Thesis On Ectopic Pregnancy in IndiaDocument7 pagesThesis On Ectopic Pregnancy in Indiaynwtcpwff100% (2)
- Leong Et Al-2004-BJOG: An International Journal of Obstetrics & GynaecologyDocument2 pagesLeong Et Al-2004-BJOG: An International Journal of Obstetrics & GynaecologyAngie MandeoyaNo ratings yet
- Preservational Procedure of Cervical Pregnancy - 201Document1 pagePreservational Procedure of Cervical Pregnancy - 201online videoNo ratings yet
- Abdominal Pregnancy: A Rare Presentation of Ectopic PregnancyDocument3 pagesAbdominal Pregnancy: A Rare Presentation of Ectopic PregnancynajmulNo ratings yet
- Clinical StudyDocument6 pagesClinical StudyAmelia FebrinaNo ratings yet
- Hetero TopicDocument3 pagesHetero TopicDONNYNo ratings yet
- Three-Dimensional Sonographic Findings of A Cervical PregnancyDocument4 pagesThree-Dimensional Sonographic Findings of A Cervical PregnancyEdwin AtencioNo ratings yet
- Aggressive Intervention of Previable Preterm Premature Rupture of MembranesDocument8 pagesAggressive Intervention of Previable Preterm Premature Rupture of MembranesVanessa Riaño GodoyNo ratings yet
- Ectopic Abdominal Pregnancies: About 2 CasesDocument10 pagesEctopic Abdominal Pregnancies: About 2 CasesIJAR JOURNALNo ratings yet
- Ovarian Pregnancy: Two Case Reports.: Jayeeta Roy, Anindita Sinha BabuDocument5 pagesOvarian Pregnancy: Two Case Reports.: Jayeeta Roy, Anindita Sinha BabuAndriyani MuslimNo ratings yet
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- Hyperemesis Gravidarum: Kelompok 5 Andi Cipta Andi Salma Vadhila Nur Alia Resmi Julita Putri RismayantiDocument7 pagesHyperemesis Gravidarum: Kelompok 5 Andi Cipta Andi Salma Vadhila Nur Alia Resmi Julita Putri RismayantiChayeol ParkNo ratings yet
- Cervical CerclageDocument33 pagesCervical Cerclagenazem photocopyNo ratings yet
- LakshmiDocument164 pagesLakshmiujjwal souravNo ratings yet
- Post-Partum HemorrhageDocument15 pagesPost-Partum Hemorrhageapi-257029163No ratings yet
- Stage of Labor and Nursing ManagementDocument22 pagesStage of Labor and Nursing ManagementFatima SajedNo ratings yet
- SDL 1Document2 pagesSDL 1Duchess Juliane Jose MirambelNo ratings yet
- Immediate Postpartum Insertion of IUDDocument7 pagesImmediate Postpartum Insertion of IUDBmpNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument4 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologySimon ReichNo ratings yet
- Shoulder DystociaDocument28 pagesShoulder DystociaLulano MbasuNo ratings yet
- Primary Goal of MCHN:: Introduction To Maternal and Child Health NursingDocument17 pagesPrimary Goal of MCHN:: Introduction To Maternal and Child Health NursingJOVEMEA LIRAYNo ratings yet
- Pregnancy Test in Urine: Uroscopy, A Nonscientific Method To Evaluate UrineDocument4 pagesPregnancy Test in Urine: Uroscopy, A Nonscientific Method To Evaluate UrineSajjadAhmad_QMCNo ratings yet
- KZ Midwifery Ratio 2014Document71 pagesKZ Midwifery Ratio 2014KZNo ratings yet
- PPIUDDocument16 pagesPPIUDmusicwizardNo ratings yet
- Ramos-2bn NCP Delivery RoomDocument2 pagesRamos-2bn NCP Delivery RoomLouwella RamosNo ratings yet
- 1st Trimester ImagingDocument118 pages1st Trimester ImagingLajja Parikh Patel100% (2)
- Provider Resources Obstetrics Late Preterm Steroids July2016Document10 pagesProvider Resources Obstetrics Late Preterm Steroids July2016Pediatrics SLCM-WHQMNo ratings yet
- Nursing Exam Questions 2023 Part 10Document2 pagesNursing Exam Questions 2023 Part 10Lejo SunnyNo ratings yet
- Journal 1 - Plasenta PreviaDocument5 pagesJournal 1 - Plasenta Previarizky ferdina kevinNo ratings yet
- Caesarean SectionDocument48 pagesCaesarean SectionStaen KisNo ratings yet
- Acute Fatty Liver of Pregnancy - V2.1 - GL780Document5 pagesAcute Fatty Liver of Pregnancy - V2.1 - GL780Ade PurnaNo ratings yet
- B. General Measure, Mgso4 Antihipertensi, C SectionDocument4 pagesB. General Measure, Mgso4 Antihipertensi, C SectionValensia VivianNo ratings yet
- 1labor Video Case PDFDocument15 pages1labor Video Case PDFyahyaNo ratings yet
- Gadar Obsteri Kala 1Document27 pagesGadar Obsteri Kala 1Natasha PriskilaNo ratings yet
- Maternal Fetal AttachmentDocument14 pagesMaternal Fetal AttachmentNida Tsaura SNo ratings yet
- Reff. Maji Natitu To Mb/R/3 TMK, Muhimbili 2021 Majernity: Total .Reff. Janyary 2021. Total Reff. February 2021Document5 pagesReff. Maji Natitu To Mb/R/3 TMK, Muhimbili 2021 Majernity: Total .Reff. Janyary 2021. Total Reff. February 2021EMNY KATAMWANo ratings yet
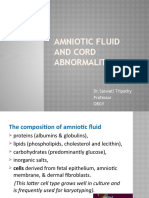
- Amniotic Fluid and Cord Abnormalities: DR - Saswati Tripathy Professor ObgyDocument46 pagesAmniotic Fluid and Cord Abnormalities: DR - Saswati Tripathy Professor ObgySaranya BalamuruganNo ratings yet
- Labor and Delivery: By: Ma. Kizianne Krystel ManioDocument43 pagesLabor and Delivery: By: Ma. Kizianne Krystel ManioJohn Christian LasalitaNo ratings yet
- Definition of Family PlanningDocument4 pagesDefinition of Family PlanningKathryn Arianne CastilloNo ratings yet
- Project Proposal For Buntis Tsek UpDocument5 pagesProject Proposal For Buntis Tsek UpShayne Cabotaje Delos Santos - BorlingNo ratings yet
Ar11feb 13
Ar11feb 13
Uploaded by
Jenny ConsignadoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ar11feb 13
Ar11feb 13
Uploaded by
Jenny ConsignadoCopyright:
Available Formats
IMAJ VOL 13 FEBRUARY 2011
case communications
dilation and curettage: successful treatment for a Heterotopic intrauterine and a twin cervical Pregnancy
Dana Vitner MD, Lior Lowenstein MD MSc, Michael Deutsch MD, Nizar Khatib MD and Zeev Weiner MD
Department of Obstetrics and Gynecology, Rambam Health Care Campus, Haifa, Israel
KeY words: cervical pregnancy, heterotopic pregnancy, dilation and curettage
IMAJ 2011; 13: 115116
orted to be less than 0.1% of all pregnancies [2,4,5]. Possible risk factors for cervical pregnancy are: prior uterine surgery such as cesarean section, dilation and curettage, the use of an intrauterine device, and in vitro fertilization [2,4,5]. Cervical pregnancy is a potentially lifethreatening condition that may present with an unexpected profuse bleeding secondary to the erosion of cervical blood vessels [2]. In the past, cervical pregnancy commonly presented with massive hemorrhage leading to hysterectomy and even death in extreme cases [2-4]. Improvements in ultrasound resolution resulted in earlier detection of such
c type of ectopic pregnancy [1-5], rep-
ervical pregnancy represents a rare
pregnancies, enabling the caregivers to offer conservative treatment. This new approach reduced the morbidity and mortality rate and greatly improved fertility preservation [1,3]. Cervical twin pregnancy is an extremely rare event, with only a few cases reported in the literature. It is reasonable to claim that women with this type of pregnancy are at a higher risk for massive hemorrhage due to the wider implantation area and the increased vascularity [4]. We present the case of a rare event of a triplet pregnancy: a single intrauterine gestation combined with two cervical gestational sacs.
Patient descriPtion A 47 year old primipara woman was referred to the emergency room at 5.5 weeks gestation complaining of vaginal bleeding. Three and a half weeks earlier, the patient underwent an intrauterine transfer of three embryos in an IVF cycle with egg donation due to ovarian failure.
Serum beta-human chorionic gonadotropin level was 10,000 mIU/ml 3 days prior to her admission. On admission, the patients vital signs were stable and the abdomen was soft with no signs of peritoneal irritation. A speculum and bimanual gynecological examination revealed a small amount of cervical bleeding with blood clots, and a normal-size anteverted uterus with normal bilateral adnexae. Transvaginal sonography revealed a single intrauterine gestational sac, irregular in shape, with no embryo or yolk sac [Figure A]. In addition, two gestational sacs were demonstrated in the cervix; one containing an embryo and a fetal heart beat and a second sac with a yolk sac without an embryo [Figure B]. Transvaginal sonography findings were unequivocal; the intrauterine pregnancy looked abnormal. All other laboratory tests were normal. Termination of pregnancy was of course recommended following the ultrasonic findings. After discussion, surgical intervention was preferred considering
[a] Single intrauterine gestational sac. [B] Two cervical gestational sacs. GS1 = gestational sac with an embryo, GS2 = gestational sac with a yolk sac.
B
115
case communications
IMAJ VOL 13 FEBRUARY 2011
the risk of massive hemorrhage following medical abortion. Uterine artery catheterization prior to the D&C was considered, but because of the relatively early gestation and the presumed ease of the surgical procedure, it was declined. The operation was carried out during the day by two senior and experienced surgeons. Before the operation, a senior hematologist was notified and alerted. Novo-7 (Coagulation Factor VII Recombinant, Novo Nordisk, Israel) was prepared along with 4 units of blood for transfusion if required. The patient was given a full and detailed explanation regarding the risks of her condition and the possibility of hysterectomy if circumstances required it, and she signed an informed consent form. Dilatation and curettage of the uterine cavity and the cervical canal were carried out uneventfully under general anesthesia. The material from the uterus and the cervix was sent together without separating them. At the end of the curettage, a single suture of vicryl 0 (Polyglactin 910, Ethicon, Johnson & Johnson, Israel) was placed in the cervix to control bleeding. Transvaginal ultrasound at the end of the procedure confirmed the complete evacuation of the gestational sacs from the cervix and the uterine cavity. The patient was discharged on postoperative day 2 in good condition with no vaginal bleeding. The histopathology report described the products of conception; however,
D&C = dilation and curettage
individual original location could not be identified.
comment Painless vaginal bleeding is the characteristic clinical presentation of cervical pregnancy and the etiology in most cases is unknown. In the past, diagnosis was often delayed, resulting in life-threatening hemorrhage often leading to emergency hysterectomy and even death [1,2,4,5]. Improvements in ultrasound resolution resulted in earlier detection of such pregnancies. This new approach reduced the morbidity and mortality rates and improved fertility preservation [1,3]. To prevent possible complications, termination of cervical pregnancy is recommended as early as possible. Attempts have been made to treat cervical pregnancies using conservative measures such as; intra-amniotic/ cardiac injection of potassium chloride or methotrexate, hypogastric iliac artery ligation, embolization, hysteroscopic resection, intra-amniotic aspiration with placement of cervical sutures, and intraamniotic injection of hypertonic solution [1,5]. In recent years, with the medical treatment (mainly methotrexate) of extrauterine pregnancy gaining popularity, it was also attempted for cervical pregnancy. Although conservative management is preferred in most cases today, the costeffectiveness of this approach compared with the classic surgical approach needs
to be further evaluated [5]. We chose the surgical conservative approach by D&C of the uterine cavity and the cervical canal, estimating that it was the least risky for our patient. Review of the relevant literature demonstrates that the occurrence of a cervical pregnancy combined with an intrauterine pregnancy is quite an exceptional event. To the best of our knowledge this is the first case report describing a heterotopic pregnancy composed of one intrauterine and two cervical pregnancies that were diagnosed and terminated uneventfully by evacuation and curettage at a relatively early stage of pregnancy.
corresponding author:
dr. d. vitner Dept. of Obstetrics and Gynecology, Rambam Health Care Campus, Haifa 31096, Israel Phone: (972-50) 206-4574, (972-77) 549-1310 email: d_vitner@rambam.health.gov.il
references
1. Hirakawa M, Tajima T, Yoshimitsu K, et al. Uterine artery embolization along with the administration of methotrexate for cervical ectopic pregnancy: technical and clinical outcomes. AJR Am J Roentgenol 2009; 192 (6): 1601-7. 2. Agdi M, Tulandi T. Surgical treatment of ectopic pregnancy. Best Pract Res Clin Obstet Gynaecol 2009; 23 (4): 519-27. 3. Majumdar A, Gupta SM, Chawla D. Successful management of post-in-vitro fertilization cervical heterotropic pregnancy. J Hum Reprod Sci 2009; 2 (1): 45-6. 4. Trojano G, Colafiglio G, Saliani N, et al. Successful management of a cervical twin pregnancy: neoadjuvant systemic methotrexate and prophylactic high cervical cerclage before curettage. Fertil Steril 2009; 91 (3): 935.e17-9. 5. Shah AA, Grotegut CA, Likes CE 3rd, et al. Heterotopic cervical pregnancy treated with transvaginal ultrasound-guided aspiration resulting in cervical site varices within the myometrium. Fertil Steril 2009; 91 (3): 934.e19-22.
You might also like
- Informative Formal SpeechDocument3 pagesInformative Formal SpeechAlba Quintanilla100% (1)
- 1 s2.0 S1028455909600802 MainDocument3 pages1 s2.0 S1028455909600802 MainSuminten S. Pd.No ratings yet
- Uterine Inversion: A Life-Threatening Obstetric Emergency: Dawn R. Hostetler, MD, and Michael Bosworth, DODocument4 pagesUterine Inversion: A Life-Threatening Obstetric Emergency: Dawn R. Hostetler, MD, and Michael Bosworth, DOAndi Farras WatyNo ratings yet
- Placenta Increta Causing Um in The 26th Week of Pregnancy 2Document3 pagesPlacenta Increta Causing Um in The 26th Week of Pregnancy 2Kester ApostolNo ratings yet
- Case Report: Postpartum Uterine Wound Dehiscence Leading To Secondary PPH: Unusual SequelaeDocument4 pagesCase Report: Postpartum Uterine Wound Dehiscence Leading To Secondary PPH: Unusual SequelaemelisaberlianNo ratings yet
- Recurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoDocument2 pagesRecurrent Cornual Ectopic Pregnancy - A Case Report: Article InfoeditorijmrhsNo ratings yet
- 1-4 HalamannnnDocument4 pages1-4 HalamannnnJulian Auparai WorabayNo ratings yet
- Case Report: Ruptured Ectopic Pregnancy in Caesarean Section Scar: A Case ReportDocument3 pagesCase Report: Ruptured Ectopic Pregnancy in Caesarean Section Scar: A Case ReportEga MegawatiNo ratings yet
- مرجع 2Document4 pagesمرجع 2Ahmed AnwarNo ratings yet
- Girija BS, Sudha TR: AbstractDocument4 pagesGirija BS, Sudha TR: AbstractALfuNo ratings yet
- Ectopic Pregnancy - StatPearls - NCBI BookshelfDocument9 pagesEctopic Pregnancy - StatPearls - NCBI BookshelfKatherine DavilaNo ratings yet
- Ruptured Ectopic Pregnancy in The Presence of An Intrauterine DeviceDocument5 pagesRuptured Ectopic Pregnancy in The Presence of An Intrauterine DevicePatrick NunsioNo ratings yet
- PEBDocument4 pagesPEBDR RISKA WAHYUNo ratings yet
- Case Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyDocument4 pagesCase Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyChidimma VictoryNo ratings yet
- Uterine Rupture in Nulliparous Woman Without Risk Factors: A Case Report and Literature ReviewDocument6 pagesUterine Rupture in Nulliparous Woman Without Risk Factors: A Case Report and Literature ReviewBOHR International Journal on GynaecologyNo ratings yet
- Cesarean Scar Ectopic Pregnancies: Etiology, Diagnosis, and ManagementDocument9 pagesCesarean Scar Ectopic Pregnancies: Etiology, Diagnosis, and ManagementDinorah MarcelaNo ratings yet
- Primary Ovarian Abscess in Pregnancy: Case ReportDocument3 pagesPrimary Ovarian Abscess in Pregnancy: Case ReportVinnyRevinaAdrianiNo ratings yet
- Ectopic Pregnancy: A ReviewDocument13 pagesEctopic Pregnancy: A ReviewDinorah MarcelaNo ratings yet
- Cesarean Scar Pregnancies and Their ManagementDocument7 pagesCesarean Scar Pregnancies and Their ManagementClinton SitanggangNo ratings yet
- Abrasio PlacentaDocument3 pagesAbrasio Placentamuhammad azamNo ratings yet
- Challenges in The Management of A Case of 2nd Abdominal Pregnancy - OJOG - 2015092815302981Document3 pagesChallenges in The Management of A Case of 2nd Abdominal Pregnancy - OJOG - 2015092815302981Stella Putri WandaNo ratings yet
- Obstetrics 2Document6 pagesObstetrics 2najmulNo ratings yet
- Gynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernDocument3 pagesGynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernIrvin MarcelNo ratings yet
- Ectopic Pregnancy - StatPearls - NCBI BookshelfDocument6 pagesEctopic Pregnancy - StatPearls - NCBI BookshelfLaura valentina ramos mezaNo ratings yet
- Tubalpregnancy DiagnosisandmanagementDocument12 pagesTubalpregnancy DiagnosisandmanagementAndreaAlexandraNo ratings yet
- Uterine Rupture: A Catastrophic Obstetric EmergencyDocument2 pagesUterine Rupture: A Catastrophic Obstetric EmergencyImtihanamiseNo ratings yet
- Tambimuttu 2015Document2 pagesTambimuttu 2015cristian vivasNo ratings yet
- Hem 2020000139 CDocument5 pagesHem 2020000139 CA.21-AH0602- VINA SHALSABINANo ratings yet
- Anesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaDocument4 pagesAnesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaHanayuki VizureiNo ratings yet
- Ectopic Pregnancy - MedscapeDocument31 pagesEctopic Pregnancy - Medscapeantonio91uNo ratings yet
- Expectatant Management of Cesarean Scar Ectopic PregnancyDocument5 pagesExpectatant Management of Cesarean Scar Ectopic PregnancyEricNo ratings yet
- PlasentaDocument4 pagesPlasentaLois YunikeNo ratings yet
- 9.radha Et Al.Document3 pages9.radha Et Al.International Journal of Clinical and Biomedical Research (IJCBR)No ratings yet
- The Back Alley Revisited: Sepsis After Attempted Self-Induced AbortionDocument3 pagesThe Back Alley Revisited: Sepsis After Attempted Self-Induced Abortionmila nurmalaNo ratings yet
- PIIS0015028219304844Document2 pagesPIIS0015028219304844nighshift serialsleeperNo ratings yet
- Minakshi S. Neglected Puerperal Inversion of The Uterus Ignorance Makes Acute A Chronic FormDocument4 pagesMinakshi S. Neglected Puerperal Inversion of The Uterus Ignorance Makes Acute A Chronic FormJulius Albert SNo ratings yet
- Ovarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014Document4 pagesOvarian Ectopic Pregnancy: A Rare Case: Iran J Reprod Med Vol. 12. No. 4. PP: 281-284, April 2014alif bagusNo ratings yet
- Case Report Rare Cesarean Section Scar Ectopic Pregnancy Successfully Treated by Methotrexate: A CaseDocument5 pagesCase Report Rare Cesarean Section Scar Ectopic Pregnancy Successfully Treated by Methotrexate: A Casemustafaali9711No ratings yet
- Anesthesia For Foetal Surgery: Dr. Athira S MadhuDocument98 pagesAnesthesia For Foetal Surgery: Dr. Athira S MadhuAthira S MadhuNo ratings yet
- A Rare Case of Morbidly Adherent Placenta in A Young - 2024 - International JouDocument4 pagesA Rare Case of Morbidly Adherent Placenta in A Young - 2024 - International JouRonald QuezadaNo ratings yet
- Scar Ectopic Case ReportDocument6 pagesScar Ectopic Case ReportMominah MayamNo ratings yet
- Total and Acute Uterine Inversion After Delivery A Case Report PDFDocument4 pagesTotal and Acute Uterine Inversion After Delivery A Case Report PDFatika sgrtNo ratings yet
- 1 s2.0 S0090825804003610 Main PDFDocument3 pages1 s2.0 S0090825804003610 Main PDFRirin WahyuniNo ratings yet
- UC Irvine: Clinical Practice and Cases in Emergency MedicineDocument6 pagesUC Irvine: Clinical Practice and Cases in Emergency MedicinePatrick NunsioNo ratings yet
- Abnormal PlacentationDocument9 pagesAbnormal PlacentationJack BladeNo ratings yet
- Ectopic Pregnancy22Document43 pagesEctopic Pregnancy22Sunil YadavNo ratings yet
- Juhi Abstract QuestDocument2 pagesJuhi Abstract QuestjuhiNo ratings yet
- Ectopic PregnancyDocument39 pagesEctopic PregnancyFecky Fihayatul IchsanNo ratings yet
- Postpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiDocument4 pagesPostpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiAstrit GashiNo ratings yet
- Thesis On Ectopic Pregnancy in IndiaDocument7 pagesThesis On Ectopic Pregnancy in Indiaynwtcpwff100% (2)
- Leong Et Al-2004-BJOG: An International Journal of Obstetrics & GynaecologyDocument2 pagesLeong Et Al-2004-BJOG: An International Journal of Obstetrics & GynaecologyAngie MandeoyaNo ratings yet
- Preservational Procedure of Cervical Pregnancy - 201Document1 pagePreservational Procedure of Cervical Pregnancy - 201online videoNo ratings yet
- Abdominal Pregnancy: A Rare Presentation of Ectopic PregnancyDocument3 pagesAbdominal Pregnancy: A Rare Presentation of Ectopic PregnancynajmulNo ratings yet
- Clinical StudyDocument6 pagesClinical StudyAmelia FebrinaNo ratings yet
- Hetero TopicDocument3 pagesHetero TopicDONNYNo ratings yet
- Three-Dimensional Sonographic Findings of A Cervical PregnancyDocument4 pagesThree-Dimensional Sonographic Findings of A Cervical PregnancyEdwin AtencioNo ratings yet
- Aggressive Intervention of Previable Preterm Premature Rupture of MembranesDocument8 pagesAggressive Intervention of Previable Preterm Premature Rupture of MembranesVanessa Riaño GodoyNo ratings yet
- Ectopic Abdominal Pregnancies: About 2 CasesDocument10 pagesEctopic Abdominal Pregnancies: About 2 CasesIJAR JOURNALNo ratings yet
- Ovarian Pregnancy: Two Case Reports.: Jayeeta Roy, Anindita Sinha BabuDocument5 pagesOvarian Pregnancy: Two Case Reports.: Jayeeta Roy, Anindita Sinha BabuAndriyani MuslimNo ratings yet
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- Hyperemesis Gravidarum: Kelompok 5 Andi Cipta Andi Salma Vadhila Nur Alia Resmi Julita Putri RismayantiDocument7 pagesHyperemesis Gravidarum: Kelompok 5 Andi Cipta Andi Salma Vadhila Nur Alia Resmi Julita Putri RismayantiChayeol ParkNo ratings yet
- Cervical CerclageDocument33 pagesCervical Cerclagenazem photocopyNo ratings yet
- LakshmiDocument164 pagesLakshmiujjwal souravNo ratings yet
- Post-Partum HemorrhageDocument15 pagesPost-Partum Hemorrhageapi-257029163No ratings yet
- Stage of Labor and Nursing ManagementDocument22 pagesStage of Labor and Nursing ManagementFatima SajedNo ratings yet
- SDL 1Document2 pagesSDL 1Duchess Juliane Jose MirambelNo ratings yet
- Immediate Postpartum Insertion of IUDDocument7 pagesImmediate Postpartum Insertion of IUDBmpNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument4 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologySimon ReichNo ratings yet
- Shoulder DystociaDocument28 pagesShoulder DystociaLulano MbasuNo ratings yet
- Primary Goal of MCHN:: Introduction To Maternal and Child Health NursingDocument17 pagesPrimary Goal of MCHN:: Introduction To Maternal and Child Health NursingJOVEMEA LIRAYNo ratings yet
- Pregnancy Test in Urine: Uroscopy, A Nonscientific Method To Evaluate UrineDocument4 pagesPregnancy Test in Urine: Uroscopy, A Nonscientific Method To Evaluate UrineSajjadAhmad_QMCNo ratings yet
- KZ Midwifery Ratio 2014Document71 pagesKZ Midwifery Ratio 2014KZNo ratings yet
- PPIUDDocument16 pagesPPIUDmusicwizardNo ratings yet
- Ramos-2bn NCP Delivery RoomDocument2 pagesRamos-2bn NCP Delivery RoomLouwella RamosNo ratings yet
- 1st Trimester ImagingDocument118 pages1st Trimester ImagingLajja Parikh Patel100% (2)
- Provider Resources Obstetrics Late Preterm Steroids July2016Document10 pagesProvider Resources Obstetrics Late Preterm Steroids July2016Pediatrics SLCM-WHQMNo ratings yet
- Nursing Exam Questions 2023 Part 10Document2 pagesNursing Exam Questions 2023 Part 10Lejo SunnyNo ratings yet
- Journal 1 - Plasenta PreviaDocument5 pagesJournal 1 - Plasenta Previarizky ferdina kevinNo ratings yet
- Caesarean SectionDocument48 pagesCaesarean SectionStaen KisNo ratings yet
- Acute Fatty Liver of Pregnancy - V2.1 - GL780Document5 pagesAcute Fatty Liver of Pregnancy - V2.1 - GL780Ade PurnaNo ratings yet
- B. General Measure, Mgso4 Antihipertensi, C SectionDocument4 pagesB. General Measure, Mgso4 Antihipertensi, C SectionValensia VivianNo ratings yet
- 1labor Video Case PDFDocument15 pages1labor Video Case PDFyahyaNo ratings yet
- Gadar Obsteri Kala 1Document27 pagesGadar Obsteri Kala 1Natasha PriskilaNo ratings yet
- Maternal Fetal AttachmentDocument14 pagesMaternal Fetal AttachmentNida Tsaura SNo ratings yet
- Reff. Maji Natitu To Mb/R/3 TMK, Muhimbili 2021 Majernity: Total .Reff. Janyary 2021. Total Reff. February 2021Document5 pagesReff. Maji Natitu To Mb/R/3 TMK, Muhimbili 2021 Majernity: Total .Reff. Janyary 2021. Total Reff. February 2021EMNY KATAMWANo ratings yet
- Amniotic Fluid and Cord Abnormalities: DR - Saswati Tripathy Professor ObgyDocument46 pagesAmniotic Fluid and Cord Abnormalities: DR - Saswati Tripathy Professor ObgySaranya BalamuruganNo ratings yet
- Labor and Delivery: By: Ma. Kizianne Krystel ManioDocument43 pagesLabor and Delivery: By: Ma. Kizianne Krystel ManioJohn Christian LasalitaNo ratings yet
- Definition of Family PlanningDocument4 pagesDefinition of Family PlanningKathryn Arianne CastilloNo ratings yet
- Project Proposal For Buntis Tsek UpDocument5 pagesProject Proposal For Buntis Tsek UpShayne Cabotaje Delos Santos - BorlingNo ratings yet