Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
3 viewsAssessment Tools Reviewer
Assessment Tools Reviewer
Uploaded by
Taegeuk KimThe document discusses several pediatric assessment tools used to evaluate motor development in infants and young children:
1) The Harris Infant Neurodevelopment Test (HINT) assesses motor behavior, behavioral state, and parent concerns in infants 2.5-12.5 months through observation. Higher scores indicate less mature development.
2) The Alberta Infant Motor Scale (AIMS) evaluates gross motor performance in infants from birth to independent walking through 58 items organized by position. Higher percentiles suggest less likely delay.
3) The Peabody Developmental Motor Scales (PDMS-2) assesses motor skills in children from birth to 6 years through tasks evaluating grasping, visual-motor integration, and object manipulation
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You might also like
- Alberta Infant Motor Scale (AIMS)Document5 pagesAlberta Infant Motor Scale (AIMS)Aditi Desai50% (10)
- Occupational Therapy Assessment ToolsDocument19 pagesOccupational Therapy Assessment ToolsThirdy BullerNo ratings yet
- SINDA: Standardized Infant NeuroDevelopmental AssessmentFrom EverandSINDA: Standardized Infant NeuroDevelopmental AssessmentNo ratings yet
- PBS PrintDocument20 pagesPBS Printlisa ekaNo ratings yet
- Neuro-Sensory Motor Development AssessmentDocument9 pagesNeuro-Sensory Motor Development AssessmentIin PuspariniNo ratings yet
- Cerebral Palsy Factsheets April 17a PDFDocument1 pageCerebral Palsy Factsheets April 17a PDFSuné GreeffNo ratings yet
- Developmental Screening TestDocument23 pagesDevelopmental Screening TestSheron MathewNo ratings yet
- Cerebral PalsyDocument55 pagesCerebral PalsyManish ManiNo ratings yet
- The Motor Control Assessment: An Instrument To Measure Motor Control in Physically Disabled ChildrenDocument5 pagesThe Motor Control Assessment: An Instrument To Measure Motor Control in Physically Disabled Childrennandhini raguNo ratings yet
- Week 3 Readings - Chapter 7 and 8Document48 pagesWeek 3 Readings - Chapter 7 and 8Bethany LongNo ratings yet
- Ni Hms 221860Document24 pagesNi Hms 221860Diego AlejandroNo ratings yet
- Alberta Infant Motor Scale (AIMS)Document5 pagesAlberta Infant Motor Scale (AIMS)Sheila SchneibergNo ratings yet
- Evaluaciones Del Procesamiento Sensorial en Los Lactantes ARTDocument13 pagesEvaluaciones Del Procesamiento Sensorial en Los Lactantes ARTLuisa duenasNo ratings yet
- Zitelli Development Cap 3Document30 pagesZitelli Development Cap 3Marcela HincapiéNo ratings yet
- Tool Validity and ReliabilityDocument9 pagesTool Validity and ReliabilityudupisonyNo ratings yet
- MUUL InglesDocument5 pagesMUUL InglesXimena GuzmanNo ratings yet
- DownloadDocument7 pagesDownloadalvinakemNo ratings yet
- Kinematic Cabeza Pretermino 2015Document6 pagesKinematic Cabeza Pretermino 2015LucyFloresNo ratings yet
- 5a21 PDFDocument15 pages5a21 PDFekaNo ratings yet
- ViewDocument8 pagesViewMatt Keanu CatapiaNo ratings yet
- What Assessments Evaluate Use of Hands in Infants? A Literature ReviewDocument5 pagesWhat Assessments Evaluate Use of Hands in Infants? A Literature ReviewMaria Camila SanabriaNo ratings yet
- Motor Control Motor LearningDocument56 pagesMotor Control Motor LearningJune EpeNo ratings yet
- Cep 2022 00822Document7 pagesCep 2022 00822Knowell CadienteNo ratings yet
- Functional Symmetry Observation Scale, Version 2 .13Document8 pagesFunctional Symmetry Observation Scale, Version 2 .13Manola ValerioNo ratings yet
- Rehabilitation Approach of Children With Cerebral PalsyDocument55 pagesRehabilitation Approach of Children With Cerebral PalsyridaNo ratings yet
- TIMP ImprovmentpdfDocument14 pagesTIMP ImprovmentpdfArtur SalesNo ratings yet
- Elisson Et Al., 1985 Construction of An Infant Neurological InternationalDocument8 pagesElisson Et Al., 1985 Construction of An Infant Neurological InternationalSantiago Gonzalez ArdilaNo ratings yet
- INFANIBDocument8 pagesINFANIBandrea sierraNo ratings yet
- DEVPSYCH 5 - Cognitive Development During The First 3 YearsDocument3 pagesDEVPSYCH 5 - Cognitive Development During The First 3 YearsRedgie G. GabaneNo ratings yet
- Neonatal Neurobehavioral Examination A NDocument7 pagesNeonatal Neurobehavioral Examination A NRheza NarwangsaNo ratings yet
- Functional Assessment TestsDocument17 pagesFunctional Assessment TestsAlessa Dela CruzNo ratings yet
- Evaluation ToolsDocument13 pagesEvaluation ToolsScribdTranslationsNo ratings yet
- Sensory Inputs NeonatesDocument13 pagesSensory Inputs NeonatesValedaboveNo ratings yet
- Kinamatic Analisis Por Video Mov 2016Document7 pagesKinamatic Analisis Por Video Mov 2016LucyFloresNo ratings yet
- Degraafpeters 2007Document10 pagesDegraafpeters 2007silvaines06No ratings yet
- CHN - Study Guide 1 2 - 240227 - 063026Document18 pagesCHN - Study Guide 1 2 - 240227 - 063026Taif SalimNo ratings yet
- Effect of Playdough On Fine Motor Skill Development in Preschool Children Aged 4 To 6 Years at Wachid Hasyim Kindergarten, Surabaya, East JavaDocument8 pagesEffect of Playdough On Fine Motor Skill Development in Preschool Children Aged 4 To 6 Years at Wachid Hasyim Kindergarten, Surabaya, East Javastikesah prodiNo ratings yet
- Iran Rehabil J 2014 12 19 14 17Document4 pagesIran Rehabil J 2014 12 19 14 17PANI78No ratings yet
- Trunk Control TestDocument20 pagesTrunk Control TestSilaghi CiprianNo ratings yet
- Development of Postural Adjustments During Reaching in Infants at Risk For Cerebral Palsy From 4 To 18 MonthsDocument9 pagesDevelopment of Postural Adjustments During Reaching in Infants at Risk For Cerebral Palsy From 4 To 18 MonthsramopavelNo ratings yet
- The Trunk Control Measurement Scale: Reliability and Discriminative Validity in Children and Young People With Neuromotor DisordersDocument7 pagesThe Trunk Control Measurement Scale: Reliability and Discriminative Validity in Children and Young People With Neuromotor DisordersDesak AgungNo ratings yet
- Effectiveness of Sensory Integration Program in Motor Skills in Children With AutismDocument6 pagesEffectiveness of Sensory Integration Program in Motor Skills in Children With AutismLiliann RiveraNo ratings yet
- Validation of The Schutte Self-Report Emotional Intelligence TestDocument5 pagesValidation of The Schutte Self-Report Emotional Intelligence TestSmriti DhakalNo ratings yet
- Pediatric Nursing Sir Guian Maam MadelDocument17 pagesPediatric Nursing Sir Guian Maam MadelAnna Carmela P. MelendezNo ratings yet
- Assessment Gross: Infants: ofDocument7 pagesAssessment Gross: Infants: ofIngrid BarkoNo ratings yet
- Procedure On New Born AssessmentDocument19 pagesProcedure On New Born AssessmentPriya100% (2)
- Weefmi Validada para Evaluar La Funcion Motora y Cognitiva de Niños Turcos Con PciDocument8 pagesWeefmi Validada para Evaluar La Funcion Motora y Cognitiva de Niños Turcos Con PciIngrid BarkoNo ratings yet
- Motor Development: How Inf Get Into The Act: Motor Actions and Psychological FunctionDocument18 pagesMotor Development: How Inf Get Into The Act: Motor Actions and Psychological FunctionGeneracion Diez TfNo ratings yet
- Pediatric Outcome MeasuresDocument40 pagesPediatric Outcome MeasuresMaybelle Anne ZamoraNo ratings yet
- NeuropsicologiaDocument10 pagesNeuropsicologiaMaria Del Mar Marulanda GrizalesNo ratings yet
- Group 2 - Pedia PTDocument34 pagesGroup 2 - Pedia PTvincecarlosbNo ratings yet
- Test of Infant Motor Performance (TIMP)Document6 pagesTest of Infant Motor Performance (TIMP)Juan Pablo NavarroNo ratings yet
- Refinement, Reliability, and Validity of The Segmental Assessment of Trunk ControlDocument12 pagesRefinement, Reliability, and Validity of The Segmental Assessment of Trunk ControlBeverly IgartuaNo ratings yet
- 4th Lesson Assesing Newborns and InfantsDocument5 pages4th Lesson Assesing Newborns and InfantsdaningdubouzetNo ratings yet
- Comparison of Different Therapy Approaches in Children With Down SyndromeDocument6 pagesComparison of Different Therapy Approaches in Children With Down SyndromeRosy OktaridaNo ratings yet
- Editorial: Developmental Assessment Tests: Scope and LimitationsDocument5 pagesEditorial: Developmental Assessment Tests: Scope and LimitationsMOON RNo ratings yet
- Pain ManagementDocument5 pagesPain ManagementHany ElbarougyNo ratings yet
- Assessing Neuromotor Readiness for Learning: The INPP Developmental Screening Test and School Intervention ProgrammeFrom EverandAssessing Neuromotor Readiness for Learning: The INPP Developmental Screening Test and School Intervention ProgrammeRating: 5 out of 5 stars5/5 (1)
- The Resilient Mind Executive Functions, Emotion Regulation, And Mental Health in Children And AdolescentsFrom EverandThe Resilient Mind Executive Functions, Emotion Regulation, And Mental Health in Children And AdolescentsNo ratings yet
- Psychophysiological assessment of human cognition and its enhancement by a non-invasive methodFrom EverandPsychophysiological assessment of human cognition and its enhancement by a non-invasive methodNo ratings yet
Assessment Tools Reviewer
Assessment Tools Reviewer
Uploaded by
Taegeuk Kim0 ratings0% found this document useful (0 votes)
3 views8 pagesThe document discusses several pediatric assessment tools used to evaluate motor development in infants and young children:
1) The Harris Infant Neurodevelopment Test (HINT) assesses motor behavior, behavioral state, and parent concerns in infants 2.5-12.5 months through observation. Higher scores indicate less mature development.
2) The Alberta Infant Motor Scale (AIMS) evaluates gross motor performance in infants from birth to independent walking through 58 items organized by position. Higher percentiles suggest less likely delay.
3) The Peabody Developmental Motor Scales (PDMS-2) assesses motor skills in children from birth to 6 years through tasks evaluating grasping, visual-motor integration, and object manipulation
Original Description:
Original Title
Assessment-Tools-Reviewer.docx
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses several pediatric assessment tools used to evaluate motor development in infants and young children:
1) The Harris Infant Neurodevelopment Test (HINT) assesses motor behavior, behavioral state, and parent concerns in infants 2.5-12.5 months through observation. Higher scores indicate less mature development.
2) The Alberta Infant Motor Scale (AIMS) evaluates gross motor performance in infants from birth to independent walking through 58 items organized by position. Higher percentiles suggest less likely delay.
3) The Peabody Developmental Motor Scales (PDMS-2) assesses motor skills in children from birth to 6 years through tasks evaluating grasping, visual-motor integration, and object manipulation
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
3 views8 pagesAssessment Tools Reviewer
Assessment Tools Reviewer
Uploaded by
Taegeuk KimThe document discusses several pediatric assessment tools used to evaluate motor development in infants and young children:
1) The Harris Infant Neurodevelopment Test (HINT) assesses motor behavior, behavioral state, and parent concerns in infants 2.5-12.5 months through observation. Higher scores indicate less mature development.
2) The Alberta Infant Motor Scale (AIMS) evaluates gross motor performance in infants from birth to independent walking through 58 items organized by position. Higher percentiles suggest less likely delay.
3) The Peabody Developmental Motor Scales (PDMS-2) assesses motor skills in children from birth to 6 years through tasks evaluating grasping, visual-motor integration, and object manipulation
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 8
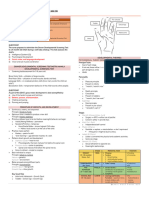
TOPIC: Pediatric Assessment Tool movement against
DATE: 01/31/2023 gravity
SUBJECT: PEDIA PT o Section 4
Tester’s clinical
impression of the
HARRIS INFANT NEUROMOTOR infant’s development
TEST (HINT) Administration:
o 15 to 30 minutes
Target Population: 2.5 to 12.5
o Infant handling is minimal;
months of age
Early screening tool for potential primarily observational
developmental disorders in both Scoring:
high and low risk infants o Total scores are derived from
Higher risk for developmental delay a sum of all scores for each of
= referred for more extensive of the 21 motor behavior items
motor delay Interpretation
Measures: o Lower HINT total scores =
o Infant motor behavior more mature
o Behavioral state o Higher HINT total scores =
o Head circumference less desirable
o Parent/caregiver concerns TEST OF INFANT MOTOR
about the infant’s PERFORMANCE (TIMPS)
development
To assess posture and movement of
Type: Norm-referenced neuromotor,
cognitive, behavioral screening tool infants from 34 weeks
postmenstrual age through 4
Content: Four sections:
months corrected age
o Section 1
For use with infants in intensive care
Infant’s background
nurseries (NICU), developmental
info
follow-up clinics, and early
o Section 2
intervention programs
Five (5) questions Observed scale of 13 dichotomously
assessing caregiver’s scored items used to examine an
perception of the infant’s spontaneous movements
infant’s movement
An elicited scale of 29 items tests the
and play
infant’s movement responses to
o Section 3
various position, sights, and sounds
Twenty-one (21) According to the test authors, the
items assessing the processes tested by the items include
infant’s motor skills the following:
in five positions, o The ability to orient and
muscle tone,
stabilize the head in space
and in response to auditory
and visual stimulation in It was developed to incorporate
supine, prone, side-lying, and components of motor development,
upright positions and during which are deemed essential to the
transitions from one position evaluation and treatment of at-risk
to another infants.
o Body alignment when the Sequential development of postural
head is manipulated control relative to four postural
o Distal selective control of the positions: supine, prone, sitting, and
fingers, wrists, hands, and standing is assessed through
ankles observation.
o Antigravity control of arm The test includes 58 items organized
and leg movements into four positions:
Administration: 25 to 40 minutes o prone, supine, sitting, and
(depending of the child’s abilities, standing.
behavioral state, physiologic, The distribution of these items is as
stability, and level of cooperation) follows: 21 prone, 9 supine, 12
Scoring: 1 present 0 absent sitting, and 16 standing.
o Elicited items are For each item, certain key
administered according to descriptors are identified that must
standardized instructions and be observed for the infant to pass the
involve direct handling of the items.
infant. Responses to these Each item describes three aspects of
items are scored on a 3-, 4-, motor performance:
5-, or 6-point rating scales o weight-bearing
that describe specific o Posture
behaviors to be noted, o antigravity movements
ranging from less mature or Administration
minimal response to mature o Minimal handling
or full response, as defined o Observed and not observed
individually for each test
Interpretation
item.
o The higher the percentile
o Total raw scores range from 0
ranking, the less likely the
to 142.
infant is demonstrating a
ALBERTA INFANT MOTOR SCALE delay in motor development.
(AIMS)
GROSS MOTOR FUNCTION
Assessment of gross motor MEASURE (GMFM)
performance
Clinical measure designed to
Infants from term (40 weeks after
evaluate change in gross motor
conception) through the age of
function in children with Cerebral
independent walking (0 to 18
Palsy
months of age).
5 months to 16 years old.
is appropriate for children whose o Object Manipulation (12
motor skills are at or below those of months and older)
a 5-year-old child without any motor The Fine Motor Scale contains 98
disability. items divided into two subtests:
The test includes 88 items that assess o Grasping (all ages)
motor function in 5 dimensions o Visual-Motor Integration (all
o (1) lying and rolling; ages)
o (2) sitting; Administration
o (3) crawling and kneeling; o 45 to 60 minutes
o (4) standing; o Scored as 0, 1, or 2
o (5) walking, running, and 0 = The child cannot
jumping. or will not attempt the
the test measures whether a child can item, or the attempt
complete the task independently. does not show that the
Administration/Scoring skill is emerging.
o 0 = Does not Initiate 1 = The child’s
o 1 = Initiates (<10% of the performance shows a
task) clear resemblance to
o 2 = partially completes the the item mastery
task (10 to <100% of the criteria but does not
task) fully meet the criteria.
o 3 = task completion (This value allows for
emerging skills.)
o GMFM-88 is 45 to 60
2 = The child
minutes
performs the item
PEABODY DEVELOPMENTAL according to the
MOTOR SCALES – SECOND EDITION criteria specified for
(PDMS-2) mastery.
It was designed to assess motor skills BRUININKS-OSERETSKY TEST OF
in children from birth through 6 MOTOR PROFICIENCY – 2ND ED
years of age.
Ages 4 through 21
The PDMS-2 is divided into two
designed to assess:
components:
o gross and fine motor
o the Gross Motor Scale
functioning in children
o the Fine Motor Scale
o for diagnosis of motor
Gross Motor Scale contains 151
impairments
items divided into four subtests:
o screen for motor deficits
o Reflexes (birth to 11 months)
o assist in educational
o Stationary (all ages),
placement decisions, and can
o Locomotion (all ages)
be used as a means for
planning and evaluating
various motor development Greenspan Social-
curricula Emotional Growth
four motor-area composites Chart: A Screening
o Fine Manual Control Questionnaire for
o Manual Coordination Infants and Young
o Body Coordination Children
o Strength and Agility o Adaptive.
Administration adaptive skill
o 40 to 60 minutes; with an functioning in daily
life based on Adaptive
extra 10 minutes needed to
Behavior Assessment
prepare the testing area.
System, Second
o Two short testing sessions
Edition
are recommended for young
1 month and 42 months of age.
children.
Administration
BAYLEY SCALES OF INFANT AND o For children aged 12 months
TODDLER DEVELOPMENT – 3RD ED and younger, administration
time is approximately 50
identify children with developmental
minutes for the entire battery
delay and provide information for
o For children 13 months and
intervention planning.
older, the total administration
assesses infant and toddler
time is 90 minutes
development across five domains:
o Based on an age-specific start
o Cognitive
point, the child must receive
sensorimotor
a score of 1 on the first three
development,
consecutive items to move
exploration and
forward (basal level). If the
manipulation, object
child scores a 0 on the first
relatedness, concept
age-specific item, the
formation, memory,
examiner goes to previous
and other aspects of
age-specific item and applies
cognitive functioning
the same rule. The test is
o Language
discontinued for the
receptive and
particular scale when the
expressive
child receives scores of 0 for
communication
five consecutive items
o Motor
(ceiling level).
fine motor and gross
motor skills BATTELLE DEVELOPMENTAL
o Social-Emotional INVENTORY – 2ND ED
social and emotional
used to measure development in
milestones in children
children with and without
based on the
disabilities
to screen for children at risk for units within a given
developmental delay activity.
The BDI-2 measures development in o Caregiver Assistance
five domains: measure disability of
o Adaptive children with respect
o Personal-Social to the amount of help
o Communication they need to carry out
o Motor functional activities.
o Cognitive.
The BDI-2 is appropriate for children
from birth to 7 years, 11 months. o Modifications.
Administration provides a frequency
o The BDI-2 contains three count of the type and
extent of
administration procedures:
environmental
structured test, observation,
modifications the
and parent interview.
child depends on to
o The complete BDI-2 can be
support functional
administered in 60 to 90
performance.
minutes, and 10 to 30
minutes for the Screening
Test.
PEDIATRIC EVALUATION OF
DISABILITY INVENTORY
measures both the in three content
domains: FUNCTIONAL INDEPENDENCE
o (1) self-care MEASURE FOR CHILDREN
o (2) mobility
The Functional Independence
o (3) social function
Measure for Children (WeeFIM) is
Functional performance is measured the pediatric adaptation of the
by the level of caregiver assistance Functional Independence Measure
and environmental modifications (FIM) for adults of the Uniform Data
needed to accomplish major System for Medical Rehabilitation.
functional activities.
help monitor children with
The content areas of self-care, disabilities as they grow into adults
mobility, and social function are who function at a maximum level of
assessed through three sets of independence
measurement scales:
The WeeFIM-II system includes the
o Functional Skills
WeeFIM instrument, the WeeFIM
designed to reflect instrument 0–3 Module, and an
meaningful functional Internet-based software
application with a report generator
and quarterly aggregate reports
The latest revision of the WeeFIM
consists of 18 items within three
domains:
o Self-care (8 ITEMS)
o Mobility (5 ITEMS)
o Cognition (5 ITEMS)
designed for use with children
between the ages of 6 months and 7
years, (but may be used with older
children with developmental
disabilities and mental ages less than
SCHOOL FUNCTION ASSESSMENT
7 years.)
The WeeFIM is a measure of response to the need for an effective
disability, not impairment, and is functional performance measure for
intended to measure what a child children attending elementary
with a disability actually does, not school.
what they ought to be able to do or A reliable and valid assessment tool
might be able to do if circumstances specific to the student’s needs and
were different. abilities and performance within the
Administration/Scoring school environment is necessary for
o direct observation of the child effective evaluation and service
o assessments may be planning.
completed by interviewing Kindergarten through Grade 6.
parents or caregivers who are The SFA consists of three sections:
familiar with the child’s o Participation
everyday activities. general or special
o Each of the 18 items to education classrooms
assess the child’s function is Playground
rated on a seven-level ordinal transportation to/
scale, from (1) total from school
dependence to (7) complete Bathroom
independence. transitions to/from
class
mealtimes.
o Task Supports
Physical Task Support
Assistance
Physical Task Support
Adaptations
Cognitive/Behavioral 7, 8 to 12, and 13 to 18 years of
Task Support– age.
Assistance The Peds-QL contains a pediatric
and self-report for children 5 to 18
Cognitive/Behavioral years and a parent proxy report
Task Support– for children 2 to 18 years.
Adaptations. The Peds-QL contains four
o Activity Performance. multidimensional scales:
Physical Tasks o (1) Physical Functioning (8
Cognitive/Behavioral items)
Tasks o (2) Emotional Functioning (5
items)
o Activity Performance section o (3) Social Functioning (5
is used in measuring items)
performance in school-related o (4) School Functioning (5
functional activities such as items)
following school rules, using And provides three summary scores:
school materials, and o (1) Total Scale Score (23
communicating needs. items)
PEDIATRIC QUALITY-OF-LIFE o (2) Physical Health
INVENTORY Summary Score (8 items)
o (3) Psychosocial
designed to measure health- related Health Summary Score (15
quality of life in healthy children items)
and adolescents and those with
acute and chronic illnesses. PEDIATRIC OUTCOMES DATA-
23-item Peds-Q Generic Core Scales COLLECTION INSTRUMENT
measure core dimensions of health as
comprehensive measure of
delineated by the World Health
musculo-skeletal outcomes
Organization, as well as school
associated with pediatric orthopedic
functioning.
problems.
The Peds-QL Generic Core Scales is
It was created to measure outcomes
a multidimensional questionnaire,
that orthopedic treatment could
measuring health-related quality of
affect:
life pertaining to:
o upper and lower extremity
o Physical
motor skills
o Emotional
o relief of pain
o Social
o restoration of activity.
o school functioning
The PODCI consists of:
Developmentally appropriate forms o an Adolescent Self-Report
are available for children 2 to 4, 5 to
Outcomes Questionnaire
o an Adolescent Parent-Report scales (ranging from 1 to 4, 5,
Outcomes Questionnaire or 6).
o and a Pediatric Outcomes
Questionnaire
The Pediatric Outcomes
Questionnaire is intended to be used
for children 2 to 10 years through
parent report; the Adolescent Parent-
Report Questionnaire is intended for
use in children between 11 and 18
years; and the Adolescent
Self-Report Questionnaire is
intended for youth and children 11
to 18 years who can complete the
form independently.
The Pediatric Outcomes
Questionnaire consists of 8 scales:
o Upper Extremity and
Physical Function Scale
o Transfer and Basic Mobility
Scale
o Sports/Physical Functioning
Scale
o Pain/Comfort Scale
o Treatment Expectations
Scale
o Happiness Scale
o Satisfaction with Symptoms
Scale
o Global Functioning Scale.
The questionnaire contains 86
questions.
Administration
o The Pediatric Outcomes
Questionnaire is completed
by a parent/guardian who has
knowledge of the child’s
condition with approximate
completion time of 10 to 20
minutes. Responses to
questions are rated on various
You might also like
- Alberta Infant Motor Scale (AIMS)Document5 pagesAlberta Infant Motor Scale (AIMS)Aditi Desai50% (10)
- Occupational Therapy Assessment ToolsDocument19 pagesOccupational Therapy Assessment ToolsThirdy BullerNo ratings yet
- SINDA: Standardized Infant NeuroDevelopmental AssessmentFrom EverandSINDA: Standardized Infant NeuroDevelopmental AssessmentNo ratings yet
- PBS PrintDocument20 pagesPBS Printlisa ekaNo ratings yet
- Neuro-Sensory Motor Development AssessmentDocument9 pagesNeuro-Sensory Motor Development AssessmentIin PuspariniNo ratings yet
- Cerebral Palsy Factsheets April 17a PDFDocument1 pageCerebral Palsy Factsheets April 17a PDFSuné GreeffNo ratings yet
- Developmental Screening TestDocument23 pagesDevelopmental Screening TestSheron MathewNo ratings yet
- Cerebral PalsyDocument55 pagesCerebral PalsyManish ManiNo ratings yet
- The Motor Control Assessment: An Instrument To Measure Motor Control in Physically Disabled ChildrenDocument5 pagesThe Motor Control Assessment: An Instrument To Measure Motor Control in Physically Disabled Childrennandhini raguNo ratings yet
- Week 3 Readings - Chapter 7 and 8Document48 pagesWeek 3 Readings - Chapter 7 and 8Bethany LongNo ratings yet
- Ni Hms 221860Document24 pagesNi Hms 221860Diego AlejandroNo ratings yet
- Alberta Infant Motor Scale (AIMS)Document5 pagesAlberta Infant Motor Scale (AIMS)Sheila SchneibergNo ratings yet
- Evaluaciones Del Procesamiento Sensorial en Los Lactantes ARTDocument13 pagesEvaluaciones Del Procesamiento Sensorial en Los Lactantes ARTLuisa duenasNo ratings yet
- Zitelli Development Cap 3Document30 pagesZitelli Development Cap 3Marcela HincapiéNo ratings yet
- Tool Validity and ReliabilityDocument9 pagesTool Validity and ReliabilityudupisonyNo ratings yet
- MUUL InglesDocument5 pagesMUUL InglesXimena GuzmanNo ratings yet
- DownloadDocument7 pagesDownloadalvinakemNo ratings yet
- Kinematic Cabeza Pretermino 2015Document6 pagesKinematic Cabeza Pretermino 2015LucyFloresNo ratings yet
- 5a21 PDFDocument15 pages5a21 PDFekaNo ratings yet
- ViewDocument8 pagesViewMatt Keanu CatapiaNo ratings yet
- What Assessments Evaluate Use of Hands in Infants? A Literature ReviewDocument5 pagesWhat Assessments Evaluate Use of Hands in Infants? A Literature ReviewMaria Camila SanabriaNo ratings yet
- Motor Control Motor LearningDocument56 pagesMotor Control Motor LearningJune EpeNo ratings yet
- Cep 2022 00822Document7 pagesCep 2022 00822Knowell CadienteNo ratings yet
- Functional Symmetry Observation Scale, Version 2 .13Document8 pagesFunctional Symmetry Observation Scale, Version 2 .13Manola ValerioNo ratings yet
- Rehabilitation Approach of Children With Cerebral PalsyDocument55 pagesRehabilitation Approach of Children With Cerebral PalsyridaNo ratings yet
- TIMP ImprovmentpdfDocument14 pagesTIMP ImprovmentpdfArtur SalesNo ratings yet
- Elisson Et Al., 1985 Construction of An Infant Neurological InternationalDocument8 pagesElisson Et Al., 1985 Construction of An Infant Neurological InternationalSantiago Gonzalez ArdilaNo ratings yet
- INFANIBDocument8 pagesINFANIBandrea sierraNo ratings yet
- DEVPSYCH 5 - Cognitive Development During The First 3 YearsDocument3 pagesDEVPSYCH 5 - Cognitive Development During The First 3 YearsRedgie G. GabaneNo ratings yet
- Neonatal Neurobehavioral Examination A NDocument7 pagesNeonatal Neurobehavioral Examination A NRheza NarwangsaNo ratings yet
- Functional Assessment TestsDocument17 pagesFunctional Assessment TestsAlessa Dela CruzNo ratings yet
- Evaluation ToolsDocument13 pagesEvaluation ToolsScribdTranslationsNo ratings yet
- Sensory Inputs NeonatesDocument13 pagesSensory Inputs NeonatesValedaboveNo ratings yet
- Kinamatic Analisis Por Video Mov 2016Document7 pagesKinamatic Analisis Por Video Mov 2016LucyFloresNo ratings yet
- Degraafpeters 2007Document10 pagesDegraafpeters 2007silvaines06No ratings yet
- CHN - Study Guide 1 2 - 240227 - 063026Document18 pagesCHN - Study Guide 1 2 - 240227 - 063026Taif SalimNo ratings yet
- Effect of Playdough On Fine Motor Skill Development in Preschool Children Aged 4 To 6 Years at Wachid Hasyim Kindergarten, Surabaya, East JavaDocument8 pagesEffect of Playdough On Fine Motor Skill Development in Preschool Children Aged 4 To 6 Years at Wachid Hasyim Kindergarten, Surabaya, East Javastikesah prodiNo ratings yet
- Iran Rehabil J 2014 12 19 14 17Document4 pagesIran Rehabil J 2014 12 19 14 17PANI78No ratings yet
- Trunk Control TestDocument20 pagesTrunk Control TestSilaghi CiprianNo ratings yet
- Development of Postural Adjustments During Reaching in Infants at Risk For Cerebral Palsy From 4 To 18 MonthsDocument9 pagesDevelopment of Postural Adjustments During Reaching in Infants at Risk For Cerebral Palsy From 4 To 18 MonthsramopavelNo ratings yet
- The Trunk Control Measurement Scale: Reliability and Discriminative Validity in Children and Young People With Neuromotor DisordersDocument7 pagesThe Trunk Control Measurement Scale: Reliability and Discriminative Validity in Children and Young People With Neuromotor DisordersDesak AgungNo ratings yet
- Effectiveness of Sensory Integration Program in Motor Skills in Children With AutismDocument6 pagesEffectiveness of Sensory Integration Program in Motor Skills in Children With AutismLiliann RiveraNo ratings yet
- Validation of The Schutte Self-Report Emotional Intelligence TestDocument5 pagesValidation of The Schutte Self-Report Emotional Intelligence TestSmriti DhakalNo ratings yet
- Pediatric Nursing Sir Guian Maam MadelDocument17 pagesPediatric Nursing Sir Guian Maam MadelAnna Carmela P. MelendezNo ratings yet
- Assessment Gross: Infants: ofDocument7 pagesAssessment Gross: Infants: ofIngrid BarkoNo ratings yet
- Procedure On New Born AssessmentDocument19 pagesProcedure On New Born AssessmentPriya100% (2)
- Weefmi Validada para Evaluar La Funcion Motora y Cognitiva de Niños Turcos Con PciDocument8 pagesWeefmi Validada para Evaluar La Funcion Motora y Cognitiva de Niños Turcos Con PciIngrid BarkoNo ratings yet
- Motor Development: How Inf Get Into The Act: Motor Actions and Psychological FunctionDocument18 pagesMotor Development: How Inf Get Into The Act: Motor Actions and Psychological FunctionGeneracion Diez TfNo ratings yet
- Pediatric Outcome MeasuresDocument40 pagesPediatric Outcome MeasuresMaybelle Anne ZamoraNo ratings yet
- NeuropsicologiaDocument10 pagesNeuropsicologiaMaria Del Mar Marulanda GrizalesNo ratings yet
- Group 2 - Pedia PTDocument34 pagesGroup 2 - Pedia PTvincecarlosbNo ratings yet
- Test of Infant Motor Performance (TIMP)Document6 pagesTest of Infant Motor Performance (TIMP)Juan Pablo NavarroNo ratings yet
- Refinement, Reliability, and Validity of The Segmental Assessment of Trunk ControlDocument12 pagesRefinement, Reliability, and Validity of The Segmental Assessment of Trunk ControlBeverly IgartuaNo ratings yet
- 4th Lesson Assesing Newborns and InfantsDocument5 pages4th Lesson Assesing Newborns and InfantsdaningdubouzetNo ratings yet
- Comparison of Different Therapy Approaches in Children With Down SyndromeDocument6 pagesComparison of Different Therapy Approaches in Children With Down SyndromeRosy OktaridaNo ratings yet
- Editorial: Developmental Assessment Tests: Scope and LimitationsDocument5 pagesEditorial: Developmental Assessment Tests: Scope and LimitationsMOON RNo ratings yet
- Pain ManagementDocument5 pagesPain ManagementHany ElbarougyNo ratings yet
- Assessing Neuromotor Readiness for Learning: The INPP Developmental Screening Test and School Intervention ProgrammeFrom EverandAssessing Neuromotor Readiness for Learning: The INPP Developmental Screening Test and School Intervention ProgrammeRating: 5 out of 5 stars5/5 (1)
- The Resilient Mind Executive Functions, Emotion Regulation, And Mental Health in Children And AdolescentsFrom EverandThe Resilient Mind Executive Functions, Emotion Regulation, And Mental Health in Children And AdolescentsNo ratings yet
- Psychophysiological assessment of human cognition and its enhancement by a non-invasive methodFrom EverandPsychophysiological assessment of human cognition and its enhancement by a non-invasive methodNo ratings yet