Professional Documents
Culture Documents
Week 27-COPD PDF
Week 27-COPD PDF
Uploaded by
Jaimie Charlotte Marie LangilleOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Week 27-COPD PDF
Week 27-COPD PDF
Uploaded by
Jaimie Charlotte Marie LangilleCopyright:
Available Formats
Week 27-Ronan Parker-COPD/Emphysema
Gas Exchange
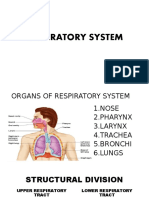
1) External respira@on—gas exchange between Respiratory Histology
alveoli and pulmonary capillary blood. Upper Airway
-O2 diffuses from alveolar air -Nose & pharynx —pseudostra@fied ciliated
(PO2=105mmHg) to pulmonary capillaries Trachea columnar, goblet cells
(PO2 =40mmHg). -Oropharynx & laryngopharynx—nonkera@nized
Main Bronchus
-CO2 diffuses opposite from pulmonary stra@fied squamous epithelium
capillaries (PCO2=45mmHg) to alveolar air Lobar
Lower Airway
Bronchus
(PO2=40mmHg). -Larynx—nonkera@nized stra@fied squamous
-Exchange occurs un@l equal on both sides. (above vocal folds), pseudostra@fied ciliated
Segmental
-Exchange influenced by par@al pressure columnar/goblet (below vocal folds)
Bronchus
gradients, small diffusion distance, large -Trachea & bronchi—pseudostra@fied ciliated
surface area, solubility of gases. Terminal Bronchiole columnar, goblet cells.
-Short membrane distance & large surface -Bronchioles, terminal, & respiratory bronchioles
Respiratory Bronchiole
area=efficient gas exchange. —simple ciliated columnar, goblet, Clara cells
2) Internal respira@on—gas exchange at the Alveolar Duct
-Alveolar ducts/sacs—simple squamous.
@ssue level. Alveolar Sac Alveoli -Alveoli—simple squamous (TI) & cuboidal (TII)
Arterial Hypoxemia from Gas Exchange Failure
Key Symptoms of Respiratory Disease
-Arterial hypoxemia is O2 deficiency in arterial blood.
-Dyspnea—SOB and difficulty breathing.
-4 causes
-Cough & sputum
1) Alveolar hypoven,la,on
-Hemoptysis—coughing up blood/bloody sputum.
-Poor ven@la@on to alveoli from defect along respiratory path, thoracic cage
-Chest pain/@ghtness; **differen@ate from angina**
abnormali@es, or upper airway obstruc@on.
-Expiratory wheeze.
-Nocturanal hypoxemia in COPD=intercostal & accessory muscle inhibi@on with
-Nasal symptoms—runny, blocked nose & sneezing.
shallow breathing during sleep.
Respiratory Failure & Headaches 2) Alveolar Diffusion Defect
-Resp. failure: inadequate gas -Alveolar membrane thickness change (fibrosis)/reduc@on in alveolar surface area
exchange by respiratory system. (emphysema) result in slowing of O2 diffusion into blood; PO2 equilibrium doesn’t
-Morning headaches are occur.
expression of poor ven@la@on 3) Ven,la,on:Perfusion Mismatch
(hypercapnia) during sleep. -Ven@la@on and perfusion in different areas aren’t equal thus inefficient gas transfer.
-Hypercapnia & low O2 in the -High V:Q=lung well ven@lated, aren’t many capillaries supplying blood to area;
brain cause vessel perfusing blood well-oxygenated.
dila@on thus -Low V:Q=good blood supply, but poor ven@la@on; blood perfusing poorly oxygenated.
increased blood 4) Shunt (V:Q ra,o=0)
flow & ICP. -2 types:
-Headache is from a) Anatomical CVS abnormality—mixed venous blood bypasses ven@lated alveoli
nerves, muscles, meninges in passing from RT to LT side of heart
& vessels of head/neck b) Intrapulmonary Defect—mixed venous blood perfuses under ven@lated alveoli.
compressed with increased
cranial volume.
Histopathology
Histopathology
-Primarily effects bronchi with mucous gland -Primarily alters acinus (distal to terminal bronchioles)
hypertrophy, hyperplasia, & hypersecre@on. w alveolar wall destruc@on w/o fibrosis (enlarged air
-Goblet cells lining airways increase resul@ng in space).
excessive mucus produc@on. -Permanent bronchiole dila@on & enlargement.
-Too few ciliated cells for proper removal -Loss of alveolar capillaries w/ alveoli loss
contributes to airway obstruc@on. -Deforma@on of terminal and respiratory bronchioles
-Ciliated pseudostra@fied columnar line bronchi;
due to septa loss normally suppor@ng structures.
with smoking, can morph into stra@fied -Elas@c @ssue surrounding alveolar septa lost; reduces
squamous via metaplasia. trac@on of small airways leading to collapse on
Pathogenesis expira@on.
-3 month chronic produc@ve cough in 2 successive Pathogenesis
years when other causes have been excluded. -Permanent airway space enlargement distal to
-Tracheal & bronchi mucous gland hypertrophy Breathing Control terminal bronchioles & alveolar wall destruc@on
Chemoreceptor RegulaTon
induced by air irritants Parts & Func,ons without fibrosis.
-Respiratory system responds to -Inflamma@on & neutrophil accumula@on from toxic
-Mucous hyper-secre@on reflects bronchial 1) Medullary Rhythmicity Centre changes in H+, CO2 and O2
involvement; airway obstruc@on is small airway -Controls inhala@on & exhala@on substance exposure.
levels in CNS
disease & coexis@ng emphysema. -Inhala@on=2 sec; exhala@on=3 sec. -Epithelial injury & ECM proteolysis from neutrophils
-Peripheral chemoreceptors are (release elastase), cytokines (IL-8), & oxidants.
-Impulse in inspiratory centre sent to in aor@c bodies in aor@c arch
COPD Airway ObstrucTon Pathophysiology intercostal muscles/diaphragm s@mula@ng and caro@d bodies in caro@d Cor Pulmonale & COPD
-COPD—chronic recurrent airflow obstruc@on where contrac@on arteries. -Cor pulmonale—RV hypertrophy/dila@on from
airway resistance is increased. -Inhala@on centre inac@ve ader 2 sec. -When PO2 in arterial blood is pulmonary hypertension acributed to primary
-Common cause=cigarece smoking/second-hand smoke. stopping impulse below 100 but above 50 mmHg, disorders of lung parenchyma/pulmonary
-Chronic bronchi@s/emphysema oden coexist (COPD). -Diaphragm and intercostals relax peripheral chemoreceptors are vasculature.
-Dis@nguished from asthma by COPD being irreversible. -Impulses from expiratory centre cause s@mulated. -Acute=dila@on only; chronic=characteris@c RV
abdominal/intercostal muscle contrac@on -Nega@ve feedback responds to (oden RA) hypertrophy.
Pathophysiology (only in forced breathing) increased PCO2, decreased pH Process
-Poor airflow due to lung @ssue breakdown 2) Pneumotaxic Centre (pons) (increased H+), and decreased -Alveolar hypoxia causes increased pulmonary
(emphysema) & small airway disease (bronchioli@s). -Coordinates inhala@on and exhala@on PO2 s@mula@ng increased vascular resistance (PVR) causing pulmonary
-Toxic substance exposure=inflamma@on/epithelial -Sends inhibitory signal to inspiratory centre breathing. hypertension.
injury. -Helps shorten inspira@on @me (more ac@ve, -Acutely—hypoxia causes pulmonary
-Goblet cell metaplasia causes small airway disease more rapid breathing) vasoconstric@on diver@ng blood away from poorly
mucous plugging, inflamma@on, and fibrosis. ven@lated alveoli; acempt to maintain V:Q balance.
-Compensa@on via squamous cell metaplasia (no cilia/ 3) Apneus@c Centre (pon) -Chronic—pulmonary vascular bed structural
goblet cells) due to con@nued cigarece smoke. -Helps coordinate changes (remodelling) induced; muscle hypertrophy
-Smoke inac@vate α1-an@trypsin=elastase breakdown inhala@on and in@mal fibrosis making arteries thicker & less
inhibited and compliant (↑ PVR)
-Limited airflow due to exhala@on. -In COPD, have reduc@on in vasodilator synthesis/
a) loss of elas@city & alveolar acachments in -Sends release & prostacyclin (protect against vascular
emphysema—elas@c recoil reduced & expiratory s@mulatory remodelling).
airway collapse impulses to -RV hypertrophies and dilates due to ↑ PVR.
b) Inflamma@on & scaring narrow small airways. inspiratory for
c) Airways blocked from mucus secre@ons. ac@va@on
-Major blockage due to mucus-secre@ng goblet cells in -Overrides
bronchial mucosa. pneumotaxic
centre.
You might also like
- Anat102a Notes FinalsDocument12 pagesAnat102a Notes FinalsJianne PulidoNo ratings yet
- Respiratory SystemDocument6 pagesRespiratory Systemshane.surigaoNo ratings yet
- QDQDQDQDQDQWQDDocument17 pagesQDQDQDQDQDQWQDTL GianNo ratings yet
- Medical Surgical Nursing Lecture 234 Pages Pg. 333 566Document189 pagesMedical Surgical Nursing Lecture 234 Pages Pg. 333 566Crystal Ann TadiamonNo ratings yet
- Medical Surgical Nursing Lecture 234 Pages Pg. 333 566Document242 pagesMedical Surgical Nursing Lecture 234 Pages Pg. 333 566ShiraishiNo ratings yet
- Respiratory SystemDocument6 pagesRespiratory SystemChelsie NicoleNo ratings yet
- Chapter 15 Respiratory SystemDocument3 pagesChapter 15 Respiratory SystemRayumaaa100% (1)
- Anatomy Final pt.2Document8 pagesAnatomy Final pt.2Gladys Mae S. BañesNo ratings yet
- Anaphy ReviewerDocument10 pagesAnaphy ReviewerTsukishima RinNo ratings yet
- Respiratory System: AdditionalDocument4 pagesRespiratory System: AdditionalDanielle CapangpanganNo ratings yet
- Anatomy and Physiology Handout # 15 Respiratory System-1Document8 pagesAnatomy and Physiology Handout # 15 Respiratory System-1Jounri Arsted Dimabuyu (Kaiz)No ratings yet
- Respiratory SystemDocument38 pagesRespiratory Systemjsreyes.402No ratings yet
- Gen BioDocument15 pagesGen BioCAMILLE JELLA ALZOLANo ratings yet
- 3 2021 05 1012 46 42 AmDocument43 pages3 2021 05 1012 46 42 Amwardahafif00No ratings yet
- Approach To The Patient With Respiratory Disease PDFDocument6 pagesApproach To The Patient With Respiratory Disease PDFRem AlfelorNo ratings yet
- Respiratory SystemDocument4 pagesRespiratory SystemAlloiza CaguiclaNo ratings yet
- 13 Respiratory SystemDocument8 pages13 Respiratory SystemPauline AñesNo ratings yet
- Airway Management Lec 1Document4 pagesAirway Management Lec 1Lenard SakiliNo ratings yet
- Respiratory SystemDocument40 pagesRespiratory SystemJezebel MolinoNo ratings yet
- Respiratory System ReviewerDocument7 pagesRespiratory System ReviewerVictoria Ellex TiomicoNo ratings yet
- Chapter 43 Physio Respi InsufficiencyDocument3 pagesChapter 43 Physio Respi InsufficiencyAldanna Felicci Garcia CaragNo ratings yet
- Respiratory System LecDocument49 pagesRespiratory System LecStef FieNo ratings yet
- Breathing and Exchange of GasesDocument6 pagesBreathing and Exchange of Gasesadityaaggarwal821No ratings yet
- Respiratory System TransesDocument5 pagesRespiratory System Transesadrielvamos28No ratings yet
- AP - Respiratory SystemDocument3 pagesAP - Respiratory SystemKatalina Estelle LaurierNo ratings yet
- Medsurg RespiDocument38 pagesMedsurg Respij UNo ratings yet
- Respiratory System: LarynxDocument4 pagesRespiratory System: LarynxLouise GermaineNo ratings yet
- Breathing N Gas ExchangeDocument2 pagesBreathing N Gas Exchangemariamfernandes6No ratings yet
- Lesson 13 - Respiratory SystemDocument3 pagesLesson 13 - Respiratory SystemJhana SamsonNo ratings yet
- Review On Respiratory SystemDocument4 pagesReview On Respiratory Systemsecondacvalo123No ratings yet
- Chapter 15: Respiratory System MC 1Document6 pagesChapter 15: Respiratory System MC 1guadalupedeamargaretNo ratings yet
- ANPH Wk13 - Pulmonary SystemDocument12 pagesANPH Wk13 - Pulmonary SystemSin I GangNo ratings yet
- Pharma Finals NotesDocument18 pagesPharma Finals NotesAj MacotoNo ratings yet
- The Respiratory SystemDocument6 pagesThe Respiratory SystemApril Jeannelyn FenizaNo ratings yet
- HCM 2 QuarterDocument7 pagesHCM 2 QuarterIGP PilienNo ratings yet
- Repiratory System Concept Rna NotesDocument21 pagesRepiratory System Concept Rna NotesArpan BhadrawalNo ratings yet
- Respiratory SystemDocument3 pagesRespiratory SystemJenneive ArellanoNo ratings yet
- ARDS With PathophysiologyDocument79 pagesARDS With Pathophysiologymabec pagaduan95% (19)
- Poe 4Document5 pagesPoe 4martinrestrepobateroNo ratings yet
- Ncma113 Lec Lab FinalDocument24 pagesNcma113 Lec Lab FinalJulla GalangNo ratings yet
- Respiratory PhysiologyDocument16 pagesRespiratory PhysiologyYsabel Salvador Dychinco100% (1)
- Anaphy Lab ReviewerDocument12 pagesAnaphy Lab ReviewerCamille ParedesNo ratings yet
- Dont BreathDocument43 pagesDont BreathDhruv GoswamiNo ratings yet
- Medical Surgical Nursing Module 11Document26 pagesMedical Surgical Nursing Module 11weissNo ratings yet
- Allows You To Talk and Make Sounds When Air Moves in and OutDocument3 pagesAllows You To Talk and Make Sounds When Air Moves in and OutchelliNo ratings yet
- 6 - Respiratory SystemDocument16 pages6 - Respiratory SystemB AuNo ratings yet
- Respiratory SystemDocument192 pagesRespiratory SystemQuolette Constante100% (1)
- 09 Principios en Ventilacion MecanicaDocument35 pages09 Principios en Ventilacion Mecanicadalialm1944No ratings yet
- Dr. Fachrul Jamal, Span Kic: SMF Anestesiologi & Icu Fk-Unsyiah/Bpk Rsuza Banda AcehDocument62 pagesDr. Fachrul Jamal, Span Kic: SMF Anestesiologi & Icu Fk-Unsyiah/Bpk Rsuza Banda AcehSayed Saiful WajirNo ratings yet
- NCM 112 NotesDocument6 pagesNCM 112 NotesKatrina Jhane MercadoNo ratings yet
- 12 Respiratory System - ATFDocument43 pages12 Respiratory System - ATFLucas BarbosaNo ratings yet
- Ms Lec 2 Respiratory SystemDocument11 pagesMs Lec 2 Respiratory SystemLabinnah MoresNo ratings yet
- Physiology Of: RespirationDocument51 pagesPhysiology Of: RespirationDr. R. PeriasamyNo ratings yet
- Ha SemifinalsDocument25 pagesHa Semifinalsericamaeabellanosa22No ratings yet
- Respiratory DisordersDocument15 pagesRespiratory Disordersmnlstr100% (5)
- Anaphy Week4 Respiratory-SystemDocument13 pagesAnaphy Week4 Respiratory-SystemMarc QuireNo ratings yet
- Chapter 2 - Respiratory SystemDocument43 pagesChapter 2 - Respiratory SystemSYAZWANINo ratings yet
- Respiratory MedicineDocument49 pagesRespiratory MedicinemuhamedNo ratings yet
- Respiratory System: Larynx EpiglottisDocument12 pagesRespiratory System: Larynx Epiglottisangel sychingNo ratings yet
- Encyclopaedia Britannica, 11th Edition, Volume 13, Slice 2 "Hearing" to "Helmond"From EverandEncyclopaedia Britannica, 11th Edition, Volume 13, Slice 2 "Hearing" to "Helmond"No ratings yet