Professional Documents
Culture Documents
Hepatitis
Hepatitis
Uploaded by
api-648401824Copyright:
Available Formats
You might also like
- Viral HEPATITIS PPT by ApplemberDocument45 pagesViral HEPATITIS PPT by ApplemberEmpress ApplemberNo ratings yet
- 2018 Hepatitis Viral InfectionDocument51 pages2018 Hepatitis Viral Infectionkomang nickoNo ratings yet
- Hepatitis Viruses: Dr. Muna. M. A. Yousif M.D Clinical MicrobiologyDocument45 pagesHepatitis Viruses: Dr. Muna. M. A. Yousif M.D Clinical MicrobiologyMAxeneNo ratings yet
- Viral HepatitisDocument6 pagesViral Hepatitisadinda sandyaNo ratings yet
- Gastroenterology Handouts Spring 2019Document27 pagesGastroenterology Handouts Spring 2019Sasoo EmadNo ratings yet
- Hepatitis BUMIL, Materi DR - Emil, SP - Pd.Document36 pagesHepatitis BUMIL, Materi DR - Emil, SP - Pd.yuliyanto.efendiNo ratings yet
- Viral Hepatitis COLEDocument73 pagesViral Hepatitis COLERuth SanmooganNo ratings yet
- Acute & Chronic HepatitisDocument65 pagesAcute & Chronic HepatitisMahmoud AjinehNo ratings yet
- Topics For Oral Exam Hep Pneu DengueDocument4 pagesTopics For Oral Exam Hep Pneu DenguePCRMNo ratings yet
- Class 3: Hepatitis Outline I. Hepatitis A Transmission RiskDocument5 pagesClass 3: Hepatitis Outline I. Hepatitis A Transmission RiskTonyNo ratings yet
- Key Slides: Individualizing Treatment Recommendations For Patients With Hepatitis B Based On EASL GuidanceDocument17 pagesKey Slides: Individualizing Treatment Recommendations For Patients With Hepatitis B Based On EASL GuidanceluamsmarinsNo ratings yet
- Gi L17 - HabcdvDocument2 pagesGi L17 - HabcdvIan Evan LeeNo ratings yet
- Acute Viral Hepatitis (Final)Document5 pagesAcute Viral Hepatitis (Final)Kim LompotNo ratings yet
- VIRAL HEPATITIS IN PREGNANCY Copy 1Document48 pagesVIRAL HEPATITIS IN PREGNANCY Copy 1EndaleNo ratings yet
- Hepatitis A-EDocument34 pagesHepatitis A-EVer Garcera TalosigNo ratings yet
- 3.0HEPATIT Lecture 5Document48 pages3.0HEPATIT Lecture 5Jiya MuhammadNo ratings yet
- HIV&HepatitisDocument46 pagesHIV&HepatitisRaja RuzannaNo ratings yet
- Gastroenterology - Viral HepatitisDocument2 pagesGastroenterology - Viral HepatitisEugen MNo ratings yet
- Hepatitis - An Overview: Dr. JayalakshmiDocument77 pagesHepatitis - An Overview: Dr. JayalakshmiNithin SundarNo ratings yet
- Heaptobiliary Disease by Lecturio.Document106 pagesHeaptobiliary Disease by Lecturio.louisegantierNo ratings yet
- Viral Hepatitis (Part I)Document12 pagesViral Hepatitis (Part I)Maarveen RajNo ratings yet
- Hepatitis BDocument23 pagesHepatitis BMarty Asis100% (1)
- HepatitisDocument29 pagesHepatitisRose Anne AbivaNo ratings yet
- Virus Hepatitis - KBKDocument53 pagesVirus Hepatitis - KBKfifi anggraeniNo ratings yet
- He HepatitisDocument4 pagesHe HepatitisMayar JaradNo ratings yet
- Hepatitis and Hepatic Failure: in ChildrenDocument26 pagesHepatitis and Hepatic Failure: in Childrenchilu20No ratings yet
- Acute Hepatitis+alf 678Document37 pagesAcute Hepatitis+alf 678Sheren GamaleldenNo ratings yet
- Hep B VirusDocument20 pagesHep B VirusBhupesh ChandNo ratings yet
- DR Moh AbdalgaderDocument27 pagesDR Moh AbdalgaderAlex SamNo ratings yet
- DR Moh AbdalgaderDocument27 pagesDR Moh AbdalgaderAlex SamNo ratings yet
- Hepatitis B Dan C - PresentasiDocument31 pagesHepatitis B Dan C - PresentasiRatu anisa Fadila balgisNo ratings yet
- LIVERDISEASEDocument82 pagesLIVERDISEASEHervis FantiniNo ratings yet
- Hepatitis: Hepatitis A Hepatitis B Hepatitis C Sirrosis HepatisDocument48 pagesHepatitis: Hepatitis A Hepatitis B Hepatitis C Sirrosis Hepatisfarah maulida martaNo ratings yet
- Hepatitis: Dr. Amany A. GhazyDocument44 pagesHepatitis: Dr. Amany A. GhazyJosé Luis García GarcíaNo ratings yet
- Vaksinasi Hep BDocument28 pagesVaksinasi Hep BMahasti AndrariniNo ratings yet
- Hepatitis B: Steve HartDocument36 pagesHepatitis B: Steve HartangelinaNo ratings yet
- Askep Viral HepatitisDocument43 pagesAskep Viral HepatitisRahayu NurhayatiNo ratings yet
- Viral Hepatitis: Umar Zein Faculty of Medicine Universitas Islam Sumatera Utara 2021Document23 pagesViral Hepatitis: Umar Zein Faculty of Medicine Universitas Islam Sumatera Utara 2021yuniNo ratings yet
- Hepatitis ADocument21 pagesHepatitis ADownload FilmNo ratings yet
- Hepatitis B The Basics: David Wong University of Toronto March 2005Document36 pagesHepatitis B The Basics: David Wong University of Toronto March 2005Umi MazidahNo ratings yet
- Acute VH Definition:: Diffuse Liver Inflammation Lasting Less Than 6 MonthsDocument22 pagesAcute VH Definition:: Diffuse Liver Inflammation Lasting Less Than 6 Monthsnanda ashriNo ratings yet
- Microbiology: HepatitisDocument11 pagesMicrobiology: HepatitisSivaNo ratings yet
- Hepatitis A - Typhoid Fever - KBKDocument50 pagesHepatitis A - Typhoid Fever - KBKanggunNo ratings yet
- Hepatitis A, B and C VirusDocument46 pagesHepatitis A, B and C VirusChyzhi SylviaNo ratings yet
- Hepatitis Viral - Dr. José Gonzáles BenavidesDocument64 pagesHepatitis Viral - Dr. José Gonzáles BenavidesEfrain Brian SilvaNo ratings yet
- Hepatitis B HardDocument7 pagesHepatitis B HardmartyliciousNo ratings yet
- Hepatology MRCP1Document87 pagesHepatology MRCP1Raouf Ra'fat SolimanNo ratings yet
- Viral Hepatitis: DR - Abiy F. Nov 2019 Arsi UniversityDocument67 pagesViral Hepatitis: DR - Abiy F. Nov 2019 Arsi UniversityWakjira NigusuNo ratings yet
- Hepatologi 1 (CMP)Document61 pagesHepatologi 1 (CMP)Yun ZhaNo ratings yet
- Jaundice and Hepatitis in Children: Dr. MwendwaDocument46 pagesJaundice and Hepatitis in Children: Dr. MwendwaAlvin OmondiNo ratings yet
- Part 2 of Medical VirologyDocument113 pagesPart 2 of Medical Virologygatete samNo ratings yet
- Hepatitis ADocument15 pagesHepatitis Azakariah kamal0% (1)
- Ciroza Si Sindromul de Activitate MezenchimalaDocument29 pagesCiroza Si Sindromul de Activitate MezenchimalaClaudiu ValentinNo ratings yet
- Acute Hepatitis: Dr.G.Indhumathi MD.Document39 pagesAcute Hepatitis: Dr.G.Indhumathi MD.Parthiban AnnaduraiNo ratings yet
- Hepatitis A-E Viruses: An OverviewDocument48 pagesHepatitis A-E Viruses: An OverviewPrajakta TawdeNo ratings yet
- GIT Viral Hepatitis in Children - PPT 93Document22 pagesGIT Viral Hepatitis in Children - PPT 93Dr.P.NatarajanNo ratings yet
- Penny R. Thayer, FNP, BC Gastro/Hepatology NP James H. Quillen, VAMCDocument27 pagesPenny R. Thayer, FNP, BC Gastro/Hepatology NP James H. Quillen, VAMCPatresya LantanNo ratings yet
- Module 7Document8 pagesModule 7soriano2214989No ratings yet
- HepatitisDocument19 pagesHepatitisDayana PrasanthNo ratings yet
- Iptec Taching Portfolio Midpoint ReviewDocument2 pagesIptec Taching Portfolio Midpoint Reviewapi-648401824No ratings yet
- Teaching Evaluation Feedback - Antibiotic DeescalationDocument9 pagesTeaching Evaluation Feedback - Antibiotic Deescalationapi-648401824No ratings yet
- Abx DeescalationDocument44 pagesAbx Deescalationapi-648401824No ratings yet
- Phenobarbital Nursing EducationDocument2 pagesPhenobarbital Nursing Educationapi-648401824No ratings yet
- Student Evals EtohDocument3 pagesStudent Evals Etohapi-648401824No ratings yet
- Medication BasicsDocument2 pagesMedication Basicsapi-648401824No ratings yet
- Cirrhosis With SBPDocument22 pagesCirrhosis With SBPapi-648401824No ratings yet
- Spring Appe Preceptor FeedbackDocument4 pagesSpring Appe Preceptor Feedbackapi-648401824No ratings yet
- Cardiac ArrestDocument4 pagesCardiac Arrestapi-648401824No ratings yet
- Diabetes Management in The Inpt SettingDocument3 pagesDiabetes Management in The Inpt Settingapi-648401824No ratings yet
- Student Feedback Fall 2022Document4 pagesStudent Feedback Fall 2022api-648401824No ratings yet
- 144-Article Text-566-1-10-20180817Document14 pages144-Article Text-566-1-10-20180817Hekter Gunting KursiNo ratings yet
- KalelDocument2 pagesKalelVanessa Cabales LoberianoNo ratings yet
- CIF-MR 2022 Ver1Document2 pagesCIF-MR 2022 Ver1Ivy marie BonNo ratings yet
- Syphilis Case Study 2013Document4 pagesSyphilis Case Study 2013Ernesto Padron0% (1)
- Needle Stick InjuryDocument6 pagesNeedle Stick InjuryNikitaNo ratings yet
- NASKAH HIV-dikonversiDocument134 pagesNASKAH HIV-dikonversiAPRINo ratings yet
- Ending The StigmaDocument1 pageEnding The StigmaarielNo ratings yet
- 2013 Fluconazole Resistant Candida Albicans.22Document8 pages2013 Fluconazole Resistant Candida Albicans.22Kala SuvarnaNo ratings yet
- Problem Sheet Agr244 - Muhammad Alif Bin Azizan - 2021469618Document3 pagesProblem Sheet Agr244 - Muhammad Alif Bin Azizan - 2021469618szkipper 03100% (1)
- Sys Review Tinea CrurisDocument3 pagesSys Review Tinea CrurisenintakrynNo ratings yet
- Pelvic Inflammatory Disease - Clinical Features - Management - TeachMeObGynDocument4 pagesPelvic Inflammatory Disease - Clinical Features - Management - TeachMeObGynLiridon SopajNo ratings yet
- CRF TyphoidDocument2 pagesCRF TyphoidAndria GuialalNo ratings yet
- Handwashing Facility Turn-Over Ceremony: A Narrative ReportDocument4 pagesHandwashing Facility Turn-Over Ceremony: A Narrative ReportJoy MercadoNo ratings yet
- AAR - Tabletop Simulation Exercise (TTX) For Pandemic Influenza - Rwanda - Aug 2009 - Final - MayiganeLandryNdrikoDocument53 pagesAAR - Tabletop Simulation Exercise (TTX) For Pandemic Influenza - Rwanda - Aug 2009 - Final - MayiganeLandryNdrikoLandry N. MayiganeNo ratings yet
- COVID-19 Rapid Test: Catalogue Number: RAPG-COV-019Document2 pagesCOVID-19 Rapid Test: Catalogue Number: RAPG-COV-019bernarNo ratings yet
- Isolation PrecautionsDocument14 pagesIsolation PrecautionsEm CastilloNo ratings yet
- QLD Immunisation Schedule Under 10Document2 pagesQLD Immunisation Schedule Under 10Anonymous oTObTTNo ratings yet
- SuperDuperUltraMega Micro para Table 1 PDFDocument68 pagesSuperDuperUltraMega Micro para Table 1 PDFThea de la PeñaNo ratings yet
- SalmonellaDocument9 pagesSalmonellaAlyssa Jane MagkalasNo ratings yet
- Augmentin Paed Susp MF gdsv26 Ipiv14 Dated 13 June 2019 24022021Document15 pagesAugmentin Paed Susp MF gdsv26 Ipiv14 Dated 13 June 2019 24022021Phisit PanasophonkulNo ratings yet
- Artigo CientíficoDocument9 pagesArtigo CientíficoBeatriz Souza LimaNo ratings yet
- Clostridia and Bacillus Lecture SlideDocument37 pagesClostridia and Bacillus Lecture SlidePrincewill SeiyefaNo ratings yet
- ESR Verification Form ReviseDocument4 pagesESR Verification Form ReviseRouella DoverteNo ratings yet
- Grade 8 HEALTH Q3 - M1Document17 pagesGrade 8 HEALTH Q3 - M1Virginia IniegoNo ratings yet
- Ch. 23 Infectious DiseasesDocument40 pagesCh. 23 Infectious Diseases吴昊No ratings yet
- Why Use Real Time RT-PCR?Document4 pagesWhy Use Real Time RT-PCR?Tanzila SiddiquiNo ratings yet
- Order U.S. 144 Cr.P.C. Dt. 24.03.2020-SUB-DIV PARLIAMENT ST. & Vasant KunjDocument3 pagesOrder U.S. 144 Cr.P.C. Dt. 24.03.2020-SUB-DIV PARLIAMENT ST. & Vasant KunjAditya TannuNo ratings yet
- Chickenpox 160531062051 PDFDocument16 pagesChickenpox 160531062051 PDFJu Lie AnnNo ratings yet
- Needle Stick InjuriesDocument24 pagesNeedle Stick InjuriesSarthak LaboratoryNo ratings yet
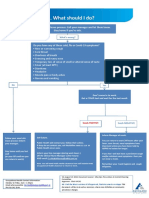
- What To Do If Youre Sick FlowchartDocument1 pageWhat To Do If Youre Sick FlowchartfuckyouNo ratings yet
Hepatitis
Hepatitis
Uploaded by
api-648401824Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hepatitis
Hepatitis
Uploaded by
api-648401824Copyright:
Available Formats
Hepatitis
Characteristics
1. Hepatotropic (systemic infx primarily affect liver), RNA (Hep A & C) or DNA (Hep B) virus
2. Acute illness: Nausea, Anorexia, Fever, Malaise, Abd pain, jaundice or elevated liver enzymes
3. HBV and HCV can produce chronic infection
HAV HBV HCV
Main transmission Fecal-oral Blood, Sexual Blood
Perinatal transmission No Yes Yes
Most common RF Direct contact Born of infected mother Injection drug use
Chronic infection No Yes Yes
Course of infection Acute, then resolved Acute, then sometimes chronic Acute, then usually chronic
Treatment of Chronic infection N/A Yes, not curative Yes, curative
Protective immunity Yes Yes No
Vaccine available Yes Yes Yes
Hep A
1. Acute viral that replicated in liver, excreted in bile, shed in the stool; Incubation period of 28 days
2. Patient group affected is household or close personal contact to person. Fecal-oral, person to person, ingestion of contaminated food or
water
3. Recent HAV outbreaks in persons who use drugs, homeless among men who have sex with men
4. Symptoms
a. Children < 6 yo: asymptomatic
b. Jaundice, fever, fatigue, loss of appetite, diarrhea, joint pain; last < 2 months
5. Diagnosis
a. Either IgM anti-HAV in serum or HAV RNA in serum or stool
6. Treatment – Supportive care
7. Prevention
a. Vaccination – safe in pregnancy (single and combo products)
b. If exposed, post-exposure prophylaxis should be given within 2 weeks
Hep B
1. Virus enters the liver through bloodstream and replicates in the liver
2. Incubation period of 90 days to onset of jaundice and 60 days to onset of abnormal ALTs
3. Symptoms
a. New infected or < 5 yo: asymptomatic
b. Acute symptoms same as Hep A, but no diarrhea 4. Diagnosis
HBsAg Marker of presence of ongoing infection
Anti-HBs Marker of immunity
Total anti-HBc Marker of Exposure
IgM anti-HBc Marker of acute or recently acquired HVC infection
HBeAg Marker of high infectivity in acute or chronic HBV infection
Anti-HBe Marker of loss of viral replication and lower levels of virus
5. Management
a. Acute – supportive care
b. Chronic: therapy goals are sustained suppression, remission of liver disease, prevent cirrhosis, hepatic failure and HCC
c. Phases
i. Patients with…
i HbeAg- (e-) and/or cirrhosis: indefinite therapy
ii HbeAg+ (e+): treatment for at least 12 months OR until HBsAg loss
e+ Immune-tolerant e- Inactive (carrier)
Normal ALT, Elevated HBV DNA Monitor Normal ALT, Low or undetectable Monitor
HBV DNA
e+ Immune-active Treat if ALT > 2xULN, HBV e- Immune reactivation Treat indefinitely if ALT > 2xULN,
Elevated ALT, Elevated HBV DNA DNA > 20,000 IU/mL Elevated ALT, Elevated HBV DNA HBV DNA > 2,000
IU/mL
Otherwise, Monitor
Otherwise, Monitor
e+ Cirrhosis Treat indefinitely if HBV DNA e- Cirrhosis Treat indefinitely if
Elevated ALT, Elevated HBV > 2,000 IU/mL Elevated ALT, Elevated HBV DNA, HBV DNA > 2,000 IU/mL
DNA, Low albumin/plts Low albumin/plts
Otherwise, Monitor Otherwise, Monitor
Hepatitis
d. First line = Nucleoside analogs
Peg-IFN-2a 180 ug SC weekly for 48 weeks Flu-like symptoms, fatigue, cytopenia, anorexia
Entecavir 0.5-1 mg PO QD Lactic acidosis
Tenofovir Disoproxil Fumarate 300 mg PO QD Nephropathy, Fanconi syndrome, Lactic acidosis
Tenofovir Alafenamide 25 mg PO QD Lactic acidosis
i. Monitoring: immune tolerant ALT Q3-6 months, eAg Q6-12 months or e- inactive patients ALT Q6-12 months
ii. HIV coinfection: three-drug regimen initiated to decrease resistant (Truvada, Descovy)
6. Prevention
a. Vaccination, single and combo products
Hep C
1. Differentiated into 7 genotypes (1-7) and then subtypes [1a, 1b most common in US, followed by 2 and 3]
2. Average times from exposure to symptom onset is 4-12 weeks
3. Symptoms
a. 2/3 of patients are asymptomatic for acute infection, 50% will develop chronic infection
b. Chronic infection: fatigue, depression, nausea, poor appetite, extrahepatic symptoms
4. Diagnosis
a. HCV RNA detectable 1-2 weeks after exposure
5. Management
a. Goal: HCV RNA undetectable 12 weeks after cessation or treatment, prevent complications and death b. Drug classes:
i. NS3/4a protease inhibitors (“-previr”)
1. Potent 3A4 inhibitors, low barrier to resistance
ii. NS5B polymerase inhibitors (“-buvir”)
1. higher barrier of resistance
iii. NS5A replication complex inhibitors (“-asvir”)
1. low barrier of resistance, but very potent
NS3/4a protease inhibitors Grazoprevir (GRZ) ALT elevations (D/C >5xULN); CI Child-Pugh class B or C
Glecaprevir (GLE) HA, Fatigue; Not recommended in Child-Pugh class B, CI in class C
Voxilaprevir (VOX) HA, GI issues, Fatigue; Not recommended in Child-Pugh class B or C
NS5B polymerase Sofosbuvir (SOF) HA, Fatigue; DI with Amiodarone (bradycardia); No hepatic dosing adjustment
inhibitors
NS5A replication complex Ledipasvir (LDV) HA, Fatigue; pH dependent, No hepatic dosing adjustment
inhibitors Elbasvir (ELB) Check for NS5A mutation prior use
Velpatasvir (VEL) Check for NS5A mutation prior use
Pibrentasvir (PIB) HA, Fatigue; Not recommended in Child-Pugh class B, CI in class C
AASLD/IDSA Recommended and Alternative Treatment Recommendations (as of 10/24/22)
HCV GT ELB/GRZ PIB/GLE* VEL/SOF/VOX* LDV/SOF VEL/SOF
Without cirrhosis
1a A P P P
1b P P P P
2 P P
3 P P
With compensated cirrhosis
1a A P P P
1b P P P P
2 P P
3 P Y93H + P Y93H +
Adult Dosing
50 mg/100 mg PO Q 120 mg/300 mg PO QD 100 mg/400 mg/100 90 mg/400 mg PO QD 100 mg/400 mg PO QD
x 12 weeks x 8 weeks mg PO QD x 12 weeks x 8-12 weeks x 12 weeks
* Must take with food, P – Preferred, A – Alternative
6. Prevention
a. Counsel infected patients how to avoid transmission/reinfection, post-exposure prophylaxis for HC personnel
References:
1. Nelson NP, Weng MK, Hofmeister MG, et al. Prevention of hepatitis A virus infection in the United States: recommendations of the Advisory Committee on
Immunization Practices, 2020. MMWR Recomm Rep 2020;69(No. RR-5):1-38.
2. Terrault, NA, Lok, AS.F., McMahon, BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance.
Hepatology 67(4):p1560-1599, April 2018. doi.10.1002/hep.29800
3. AASLD-IDSA. Recommendations for testing, managing, and treating hepatitis C. http://www.hcvguidelines.org. Accessed April 09, 2023.
You might also like
- Viral HEPATITIS PPT by ApplemberDocument45 pagesViral HEPATITIS PPT by ApplemberEmpress ApplemberNo ratings yet
- 2018 Hepatitis Viral InfectionDocument51 pages2018 Hepatitis Viral Infectionkomang nickoNo ratings yet
- Hepatitis Viruses: Dr. Muna. M. A. Yousif M.D Clinical MicrobiologyDocument45 pagesHepatitis Viruses: Dr. Muna. M. A. Yousif M.D Clinical MicrobiologyMAxeneNo ratings yet
- Viral HepatitisDocument6 pagesViral Hepatitisadinda sandyaNo ratings yet
- Gastroenterology Handouts Spring 2019Document27 pagesGastroenterology Handouts Spring 2019Sasoo EmadNo ratings yet
- Hepatitis BUMIL, Materi DR - Emil, SP - Pd.Document36 pagesHepatitis BUMIL, Materi DR - Emil, SP - Pd.yuliyanto.efendiNo ratings yet
- Viral Hepatitis COLEDocument73 pagesViral Hepatitis COLERuth SanmooganNo ratings yet
- Acute & Chronic HepatitisDocument65 pagesAcute & Chronic HepatitisMahmoud AjinehNo ratings yet
- Topics For Oral Exam Hep Pneu DengueDocument4 pagesTopics For Oral Exam Hep Pneu DenguePCRMNo ratings yet
- Class 3: Hepatitis Outline I. Hepatitis A Transmission RiskDocument5 pagesClass 3: Hepatitis Outline I. Hepatitis A Transmission RiskTonyNo ratings yet
- Key Slides: Individualizing Treatment Recommendations For Patients With Hepatitis B Based On EASL GuidanceDocument17 pagesKey Slides: Individualizing Treatment Recommendations For Patients With Hepatitis B Based On EASL GuidanceluamsmarinsNo ratings yet
- Gi L17 - HabcdvDocument2 pagesGi L17 - HabcdvIan Evan LeeNo ratings yet
- Acute Viral Hepatitis (Final)Document5 pagesAcute Viral Hepatitis (Final)Kim LompotNo ratings yet
- VIRAL HEPATITIS IN PREGNANCY Copy 1Document48 pagesVIRAL HEPATITIS IN PREGNANCY Copy 1EndaleNo ratings yet
- Hepatitis A-EDocument34 pagesHepatitis A-EVer Garcera TalosigNo ratings yet
- 3.0HEPATIT Lecture 5Document48 pages3.0HEPATIT Lecture 5Jiya MuhammadNo ratings yet
- HIV&HepatitisDocument46 pagesHIV&HepatitisRaja RuzannaNo ratings yet
- Gastroenterology - Viral HepatitisDocument2 pagesGastroenterology - Viral HepatitisEugen MNo ratings yet
- Hepatitis - An Overview: Dr. JayalakshmiDocument77 pagesHepatitis - An Overview: Dr. JayalakshmiNithin SundarNo ratings yet
- Heaptobiliary Disease by Lecturio.Document106 pagesHeaptobiliary Disease by Lecturio.louisegantierNo ratings yet
- Viral Hepatitis (Part I)Document12 pagesViral Hepatitis (Part I)Maarveen RajNo ratings yet
- Hepatitis BDocument23 pagesHepatitis BMarty Asis100% (1)
- HepatitisDocument29 pagesHepatitisRose Anne AbivaNo ratings yet
- Virus Hepatitis - KBKDocument53 pagesVirus Hepatitis - KBKfifi anggraeniNo ratings yet
- He HepatitisDocument4 pagesHe HepatitisMayar JaradNo ratings yet
- Hepatitis and Hepatic Failure: in ChildrenDocument26 pagesHepatitis and Hepatic Failure: in Childrenchilu20No ratings yet
- Acute Hepatitis+alf 678Document37 pagesAcute Hepatitis+alf 678Sheren GamaleldenNo ratings yet
- Hep B VirusDocument20 pagesHep B VirusBhupesh ChandNo ratings yet
- DR Moh AbdalgaderDocument27 pagesDR Moh AbdalgaderAlex SamNo ratings yet
- DR Moh AbdalgaderDocument27 pagesDR Moh AbdalgaderAlex SamNo ratings yet
- Hepatitis B Dan C - PresentasiDocument31 pagesHepatitis B Dan C - PresentasiRatu anisa Fadila balgisNo ratings yet
- LIVERDISEASEDocument82 pagesLIVERDISEASEHervis FantiniNo ratings yet
- Hepatitis: Hepatitis A Hepatitis B Hepatitis C Sirrosis HepatisDocument48 pagesHepatitis: Hepatitis A Hepatitis B Hepatitis C Sirrosis Hepatisfarah maulida martaNo ratings yet
- Hepatitis: Dr. Amany A. GhazyDocument44 pagesHepatitis: Dr. Amany A. GhazyJosé Luis García GarcíaNo ratings yet
- Vaksinasi Hep BDocument28 pagesVaksinasi Hep BMahasti AndrariniNo ratings yet
- Hepatitis B: Steve HartDocument36 pagesHepatitis B: Steve HartangelinaNo ratings yet
- Askep Viral HepatitisDocument43 pagesAskep Viral HepatitisRahayu NurhayatiNo ratings yet
- Viral Hepatitis: Umar Zein Faculty of Medicine Universitas Islam Sumatera Utara 2021Document23 pagesViral Hepatitis: Umar Zein Faculty of Medicine Universitas Islam Sumatera Utara 2021yuniNo ratings yet
- Hepatitis ADocument21 pagesHepatitis ADownload FilmNo ratings yet
- Hepatitis B The Basics: David Wong University of Toronto March 2005Document36 pagesHepatitis B The Basics: David Wong University of Toronto March 2005Umi MazidahNo ratings yet
- Acute VH Definition:: Diffuse Liver Inflammation Lasting Less Than 6 MonthsDocument22 pagesAcute VH Definition:: Diffuse Liver Inflammation Lasting Less Than 6 Monthsnanda ashriNo ratings yet
- Microbiology: HepatitisDocument11 pagesMicrobiology: HepatitisSivaNo ratings yet
- Hepatitis A - Typhoid Fever - KBKDocument50 pagesHepatitis A - Typhoid Fever - KBKanggunNo ratings yet
- Hepatitis A, B and C VirusDocument46 pagesHepatitis A, B and C VirusChyzhi SylviaNo ratings yet
- Hepatitis Viral - Dr. José Gonzáles BenavidesDocument64 pagesHepatitis Viral - Dr. José Gonzáles BenavidesEfrain Brian SilvaNo ratings yet
- Hepatitis B HardDocument7 pagesHepatitis B HardmartyliciousNo ratings yet
- Hepatology MRCP1Document87 pagesHepatology MRCP1Raouf Ra'fat SolimanNo ratings yet
- Viral Hepatitis: DR - Abiy F. Nov 2019 Arsi UniversityDocument67 pagesViral Hepatitis: DR - Abiy F. Nov 2019 Arsi UniversityWakjira NigusuNo ratings yet
- Hepatologi 1 (CMP)Document61 pagesHepatologi 1 (CMP)Yun ZhaNo ratings yet
- Jaundice and Hepatitis in Children: Dr. MwendwaDocument46 pagesJaundice and Hepatitis in Children: Dr. MwendwaAlvin OmondiNo ratings yet
- Part 2 of Medical VirologyDocument113 pagesPart 2 of Medical Virologygatete samNo ratings yet
- Hepatitis ADocument15 pagesHepatitis Azakariah kamal0% (1)
- Ciroza Si Sindromul de Activitate MezenchimalaDocument29 pagesCiroza Si Sindromul de Activitate MezenchimalaClaudiu ValentinNo ratings yet
- Acute Hepatitis: Dr.G.Indhumathi MD.Document39 pagesAcute Hepatitis: Dr.G.Indhumathi MD.Parthiban AnnaduraiNo ratings yet
- Hepatitis A-E Viruses: An OverviewDocument48 pagesHepatitis A-E Viruses: An OverviewPrajakta TawdeNo ratings yet
- GIT Viral Hepatitis in Children - PPT 93Document22 pagesGIT Viral Hepatitis in Children - PPT 93Dr.P.NatarajanNo ratings yet
- Penny R. Thayer, FNP, BC Gastro/Hepatology NP James H. Quillen, VAMCDocument27 pagesPenny R. Thayer, FNP, BC Gastro/Hepatology NP James H. Quillen, VAMCPatresya LantanNo ratings yet
- Module 7Document8 pagesModule 7soriano2214989No ratings yet
- HepatitisDocument19 pagesHepatitisDayana PrasanthNo ratings yet
- Iptec Taching Portfolio Midpoint ReviewDocument2 pagesIptec Taching Portfolio Midpoint Reviewapi-648401824No ratings yet
- Teaching Evaluation Feedback - Antibiotic DeescalationDocument9 pagesTeaching Evaluation Feedback - Antibiotic Deescalationapi-648401824No ratings yet
- Abx DeescalationDocument44 pagesAbx Deescalationapi-648401824No ratings yet
- Phenobarbital Nursing EducationDocument2 pagesPhenobarbital Nursing Educationapi-648401824No ratings yet
- Student Evals EtohDocument3 pagesStudent Evals Etohapi-648401824No ratings yet
- Medication BasicsDocument2 pagesMedication Basicsapi-648401824No ratings yet
- Cirrhosis With SBPDocument22 pagesCirrhosis With SBPapi-648401824No ratings yet
- Spring Appe Preceptor FeedbackDocument4 pagesSpring Appe Preceptor Feedbackapi-648401824No ratings yet
- Cardiac ArrestDocument4 pagesCardiac Arrestapi-648401824No ratings yet
- Diabetes Management in The Inpt SettingDocument3 pagesDiabetes Management in The Inpt Settingapi-648401824No ratings yet
- Student Feedback Fall 2022Document4 pagesStudent Feedback Fall 2022api-648401824No ratings yet
- 144-Article Text-566-1-10-20180817Document14 pages144-Article Text-566-1-10-20180817Hekter Gunting KursiNo ratings yet
- KalelDocument2 pagesKalelVanessa Cabales LoberianoNo ratings yet
- CIF-MR 2022 Ver1Document2 pagesCIF-MR 2022 Ver1Ivy marie BonNo ratings yet
- Syphilis Case Study 2013Document4 pagesSyphilis Case Study 2013Ernesto Padron0% (1)
- Needle Stick InjuryDocument6 pagesNeedle Stick InjuryNikitaNo ratings yet
- NASKAH HIV-dikonversiDocument134 pagesNASKAH HIV-dikonversiAPRINo ratings yet
- Ending The StigmaDocument1 pageEnding The StigmaarielNo ratings yet
- 2013 Fluconazole Resistant Candida Albicans.22Document8 pages2013 Fluconazole Resistant Candida Albicans.22Kala SuvarnaNo ratings yet
- Problem Sheet Agr244 - Muhammad Alif Bin Azizan - 2021469618Document3 pagesProblem Sheet Agr244 - Muhammad Alif Bin Azizan - 2021469618szkipper 03100% (1)
- Sys Review Tinea CrurisDocument3 pagesSys Review Tinea CrurisenintakrynNo ratings yet
- Pelvic Inflammatory Disease - Clinical Features - Management - TeachMeObGynDocument4 pagesPelvic Inflammatory Disease - Clinical Features - Management - TeachMeObGynLiridon SopajNo ratings yet
- CRF TyphoidDocument2 pagesCRF TyphoidAndria GuialalNo ratings yet
- Handwashing Facility Turn-Over Ceremony: A Narrative ReportDocument4 pagesHandwashing Facility Turn-Over Ceremony: A Narrative ReportJoy MercadoNo ratings yet
- AAR - Tabletop Simulation Exercise (TTX) For Pandemic Influenza - Rwanda - Aug 2009 - Final - MayiganeLandryNdrikoDocument53 pagesAAR - Tabletop Simulation Exercise (TTX) For Pandemic Influenza - Rwanda - Aug 2009 - Final - MayiganeLandryNdrikoLandry N. MayiganeNo ratings yet
- COVID-19 Rapid Test: Catalogue Number: RAPG-COV-019Document2 pagesCOVID-19 Rapid Test: Catalogue Number: RAPG-COV-019bernarNo ratings yet
- Isolation PrecautionsDocument14 pagesIsolation PrecautionsEm CastilloNo ratings yet
- QLD Immunisation Schedule Under 10Document2 pagesQLD Immunisation Schedule Under 10Anonymous oTObTTNo ratings yet
- SuperDuperUltraMega Micro para Table 1 PDFDocument68 pagesSuperDuperUltraMega Micro para Table 1 PDFThea de la PeñaNo ratings yet
- SalmonellaDocument9 pagesSalmonellaAlyssa Jane MagkalasNo ratings yet
- Augmentin Paed Susp MF gdsv26 Ipiv14 Dated 13 June 2019 24022021Document15 pagesAugmentin Paed Susp MF gdsv26 Ipiv14 Dated 13 June 2019 24022021Phisit PanasophonkulNo ratings yet
- Artigo CientíficoDocument9 pagesArtigo CientíficoBeatriz Souza LimaNo ratings yet
- Clostridia and Bacillus Lecture SlideDocument37 pagesClostridia and Bacillus Lecture SlidePrincewill SeiyefaNo ratings yet
- ESR Verification Form ReviseDocument4 pagesESR Verification Form ReviseRouella DoverteNo ratings yet
- Grade 8 HEALTH Q3 - M1Document17 pagesGrade 8 HEALTH Q3 - M1Virginia IniegoNo ratings yet
- Ch. 23 Infectious DiseasesDocument40 pagesCh. 23 Infectious Diseases吴昊No ratings yet
- Why Use Real Time RT-PCR?Document4 pagesWhy Use Real Time RT-PCR?Tanzila SiddiquiNo ratings yet
- Order U.S. 144 Cr.P.C. Dt. 24.03.2020-SUB-DIV PARLIAMENT ST. & Vasant KunjDocument3 pagesOrder U.S. 144 Cr.P.C. Dt. 24.03.2020-SUB-DIV PARLIAMENT ST. & Vasant KunjAditya TannuNo ratings yet
- Chickenpox 160531062051 PDFDocument16 pagesChickenpox 160531062051 PDFJu Lie AnnNo ratings yet
- Needle Stick InjuriesDocument24 pagesNeedle Stick InjuriesSarthak LaboratoryNo ratings yet
- What To Do If Youre Sick FlowchartDocument1 pageWhat To Do If Youre Sick FlowchartfuckyouNo ratings yet