Professional Documents
Culture Documents
Feline Chronic Gingivostomatitis An Update 1671815182
Feline Chronic Gingivostomatitis An Update 1671815182
Uploaded by
Herland HernandezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Feline Chronic Gingivostomatitis An Update 1671815182
Feline Chronic Gingivostomatitis An Update 1671815182
Uploaded by
Herland HernandezCopyright:
Available Formats
FEATURES • PEER REVIEWED
IDENTIFY AND ACT
Early detection of gingivostomatitis in
cats can aid the veterinary team in starting
therapy and working toward remission.
PRESSLAB/shutterstock.com
Abstract
Feline chronic gingivostomatitis (FCGS) affects around 0.7% to 12% of the feline population and is a source of
frustration for the affected pet, pet owner, and veterinary team. The exact etiology of the disease continues to evade
the veterinary community, making it difficult to explain to pet owners. Past and present studies are making progress
toward identifying a link to the exact causality of this disease and have opened the door to multiple therapeutic
modalities. Although surgical intervention in conjunction with medical management is still the gold standard, other
options are now available to veterinary professionals. New modalities are discussed alongside current research
detailing the long history of FCGS in cats today.
64 • WINTER 2023 • todaysveterinarynurse.com
PEER REVIEWED • FEATURES
DENTISTRY
Feline Chronic
Gingivostomatitis:
An Update
Sheena Davis, LVT, VTS (Dentistry), Veterinary Cannabis Counselor
Big Apple LVT Consulting & Education, New York City, New York
F
eline chronic gingivostomatitis (FCGS) is a Many studies are dedicated to the discovery of the
debilitating inflammatory disease affecting true etiology of FCGS. Unfortunately, the exact
the oral cavity of cats. This disease is cause of FCGS is currently unknown, but
marked by severe to chronic inflammation of the thankfully a decade’s worth of investigation has
gingiva, mucosa, and surrounding tissues that line advanced the knowledge and treatment of this
the oral cavity.1 Chronic gingivostomatitis affects debilitating disease.
approximately 0.7% to 12% of the general cat
population.2-4
ETIOLOGY
There is a great deal of frustration regarding the This complex multifactorial condition does not
diagnosis and treatment of this oral inflammatory have a simple etiologic agent. Several studies have
disease. The frustration is due in part to the high found that FCGS is caused by an exaggerated
frequency of inflammatory diseases in the oral immunologic response to antigenic stimulation.6
cavity of cats and veterinary professionals’ limited The causes of this stimulation can be exaggerated
understanding of their etiology.5 by viral diseases such as feline leukemia virus
(FeLV) infection, feline immunodeficiency virus
(FIV) infection, calicivirus infection, feline
Take-Home Points
z The etiology of feline chronic z Environmental stressors z Regenerative therapy (currently in
gingivostomatitis (FCGS) (especially in multicat households) development) shows promise for
is unknown and most likely can play a role in FCGS. management of FCGS.
multifactorial.
z Current treatment options involve z Nutritional support (via a feeding
z FCGS can affect any breed of cat, partial- to full-mouth extractions, tube) may be indicated in severe
regardless of age or sex. with or without medical cases.
management.
z FCGS is an exaggerated immune
response to antigenic stimulation. z Medical management alone is not
acceptable.
todaysveterinarynurse.com • WINTER 2023 • 65
FEATURES • PEER REVIEWED
infectious peritonitis, herpesvirus infection, and influence on the overall diversity and abundance of
panleukopenia virus infection as well as bacterial specific bacteria in the oral microbiome of cats. The
organisms such as Bartonella henselae.6 cats fed an exclusively dry diet had higher bacterial
diversity than the cats fed a wet-food diet. While
The systemic and local consequences of FCGS are differences between the oral microbiome of the cats fed
suggested by the presence of lymphocytes and plasma these exclusive diets were noted, the relationship
cells in affected oral tissues, with fewer neutrophils, between these differences and gingival health remains
Mott cells, and mast cells.7,8 In humans, a known ratio unclear. Further studies are needed to determine the
of low CD4+ to CD8+ T cells is a marker for immune full extent of the “diet factor” and FCGS.
dysfunction and chronic inflammation. Through this,
we can infer a similar pathologic reaction in cats with As for breed predilection, unfortunately this disease can
FCGS that have an increased CD8+ (cytotoxic) T cell affect any breed, regardless of age or sex.16 Until 2007,
count compared with CD4+ (helper) T cell count. it was believed that breeds such as Abyssinian, Burmese,
These cells have been detected locally as well as Himalayan, Persian, and Siamese were mostly
systemically, supporting the theory of an inflammatory affected.16 In a survey of almost 5000 cats in
response, likely a cell-mediated immune response, to 12 practices over a 12-week period, 34 cases of FCGS
antigenic stimulation probably caused by pathogens were noted, with no breed bias identified.2
such as viruses.9-11 Recent studies focused on the
shedding of calicivirus as an active virus in clinical cases A 2019 study noted a possible link between
of FCGS and found no association of viral shedding environmental stressors and FCGS, revealing a higher
with FeLV, FIV, herpesvirus, and Bartonella.12 incidence in multicat households versus single-cat
households; every additional household cat increased
A 2021 study examined the oral microbiome of cats to the odds of FCGS by more than 70%.17 Cats within
determine whether an imbalance of the oral flora this study were indoor-only; therefore, evidence was
played a potential role in FCGS. In this small pilot missing regarding indoor–outdoor cats within a
study, 14 clinically healthy cats and 14 cats affected by multicat home. Further studies focusing on the
FCGS were tested.13 A sterile swab was used to obtain a interaction between cats in a multicat household, with
sample and tested using next-generation DNA access to the outdoors and possible circulation
sequencing. A high number of fungal species, such as (reinfection) of infectious agents between housemates,
Malassezia restricta, Malassezia arunalokei, Cladosporium must be conducted.
penidielloides, Cladosporium salinae, and Aspergillus
species, were found and detected in the FCGS group;
the fungi Saccharomyces cerevisiae was found solely in CLINICAL SIGNS
the clinically healthy cat group. “Feline chronic gingivostomatitis” is an umbrella term
used to describe the chronic stomatitis and gingivitis
This pilot study was able to identify the distinct syndrome of cats. This disease can be further classified
differences between the oral microbiome of cats that into types 1 and 218:
were clinically healthy versus those affected by FCGS, ● Type 1 FCGS has a better prognosis and is classified
with a potential biomarker identified as Bergeyella by its clinical characteristic alveolar, labial/buccal
zoohelcum.13 Additional studies are needed to improve mucositis/stomatitis.
the understanding of the oral microbiome of cats, but ● Type 2 FCGS is classified by its characteristic
this study supports the idea of a potential imbalance location along the caudal aspect of the oral cavity,
between the flora of the oral cavity of cats and its with or without alveolar and labial/buccal mucositis/
potential role in FCGS. stomatitis.
Additional studies point to a potential link to Cats affected by FCGS can show various clinical signs,
nutritional disorders and a breed predilection.14 A pilot but the most common are halitosis, dysphagia
study examined the oral microbiome of cats and the (difficulty swallowing), pawing at the mouth,
changes of the microbiome based on provided diets.15 reluctance to eat, anorexia, weight loss, growling/
The cats in this pilot study were divided into 2 groups; crying, drooling, blood-tinged saliva, change in
1 was offered a dry diet and the other a wet-food diet. temperament, enlarged lymph nodes, and a lack of
This study discovered that diet indeed had a significant grooming.19,20
66 • WINTER 2023 • todaysveterinarynurse.com
PEER REVIEWED • FEATURES
It is important to note the difference between gingivitis
and FCGS in cats affected by this disease. Gingivitis is
inflammation of the gingiva and does not extend Gingivitis is inflammation of the
beyond the mucogingival line, whereas true stomatitis gingiva and does not extend
will extend into the alveolar, labial/buccal, lingual, and
caudal aspects of the mouth as well as the palatoglossal
beyond the mucogingival line,
folds.12 Caudal stomatitis is present in 85% of cats whereas true stomatitis will
affected by FCGS.18 extend into the alveolar, labial/
buccal, lingual, and caudal
SIGNALMENT aspects of the mouth as well as
The average age of cats that are presented with FCGS is the palatoglossal folds.12
approximately 7 years.18 A juvenile form of this disease
known as feline juvenile gingivitis/periodontitis
typically presents in cats after the eruption of the adult
teeth, from 3 to 6 months of age. As the patient
matures and eruption is complete, this form of
stomatitis typically resolves around 2 years of age.19,20 the extent of any dental disease, such as periodontal
disease, tooth resorption, retained roots, and missing
teeth—conditions that are often present in conjunction
DIAGNOSTIC WORKUP with FCGS (FIGURE 2).18 These radiographs will also
To determine if a feline patient has FCGS, the assist the veterinarian with extractions and treatment of
veterinary team must obtain a thorough history FCGS (FIGURE 3).
(including nutritional history), perform a physical
exam, and perform diagnostic testing. Any patient that
has suspected FCGS should have a complete blood Histopathology
count, serum biochemical profile, bleeding time test, Because of the proliferative and ulcerative presentation
serology (FIV/FeLV), T4 (thyroxine) test, and urinalysis of FCGS, collecting a biopsy specimen of the mucosa
test performed. and submucosa is advisable and will help the
veterinarian diagnose FCGS. Similar oral lesions, such
The purpose of these tests is to rule out underlying as eosinophilic granulomas, indolent ulcers, and
conditions that can affect anesthesia rather than squamous cell carcinoma, can grossly present as
diagnosing the disease. Testing for calicivirus and FCGS.21 The histopathologic results concurrent with
Bartonella is not recommended because results do not FCGS reveal plasma cells and a diverse number of
change the therapy.18 Although some cats with FCGS
are positive for Bartonella species, a cause-and-effect
relationship has not yet been established, as there is a
high rate of antibody-positive cats within a healthy
population due to flea exposure.18
In a study of 60 cats with FCGS, 7% were positive for
FeLV and 8% were positive for FIV.18 Often,
hyperglobulinemia and increased total protein are
noted on serum biochemical results in patients with
FCGS.12,16 Conversely, neutrophilia is not a
hematologic finding in cats with FCGS.12
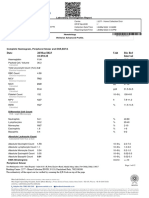
Radiographs
Intraoral radiographs are always warranted and should
be obtained on any patient undergoing a dentistry
FIGURE 1. Oral radiology during a dental examination.
procedure (FIGURE 1). The radiographs help determine
todaysveterinarynurse.com • WINTER 2023 • 67
FEATURES • PEER REVIEWED
of cats will show substantial improvement or resolution
of FCGS, with minimal or no improvement in
Studies have shown that partial- approximately 20% to 30% of cats.18,22-24 Although
mouth (all premolar and surgical intervention yields the best therapeutic results,
it is still important to provide medical management
molar teeth) or full-mouth alongside surgical treatment.
extraction provides the best
long-term results. 22-24 For patients that have mild to moderate anorexia due to
FCGS, the placement of a pharyngostomy or
gastrostomy tube is indicated to provide nutritional
support, both before and after surgical intervention, or
until the patient can eat on its own.18
lymphocytes, mast cells, Mott cells, macrophages, and
neutrophils.18 Often, neoplasia can be seen concurrently Antibiotics
with FCGS and should always be ruled out. Antibiotics are recommended only when used in
conjunction with surgery. An antibiotic will decrease
the bacterial load and help the gingiva heal to some
MEDICAL MANAGEMENT VERSUS extent, so that at the time of surgery the veterinarian
SURGICAL INTERVENTION has less friable tissue to work with. The antibiotic of
There are 2 main approaches to treating FCGS: choice for the oral cavity is one that will target both the
medical management and surgical intervention. gram-positive and gram-negative organisms in the
Although medical management is an option, it often mouth.
yields limited and unfavorable outcomes, making
surgical intervention the preferred treatment of choice. The antibiotics that are approved by the U.S. Food and
Depending on the severity of the disease, the option for Drug Administration (FDA) for use in FCGS are
partial-mouth extractions over full-mouth extractions is clindamycin and amoxicillin/clavulanate potassium.18
warranted on a case-by-case basis. Although not approved by the FDA for use in feline
dental disease or infections, metronidazole is another
Studies have shown that partial-mouth (all premolar antibiotic of choice.18 Use of antibiotics alone for
and molar teeth) or full-mouth extraction provides the treatment/management of FCGS is not recommended
best long-term results.22-24 Approximately 70% to 80% and will only increase the likelihood of bacterial
resistance.
FIGURE 3. Radiograph of 407, showing the presence of
FIGURE 2. Gross presentation of dental disease with tooth resorption with moderate periodontal disease (as
moderate localized gingivitis surrounding 407. noted by the >50% bone loss).
68 • WINTER 2023 • todaysveterinarynurse.com
PEER REVIEWED • FEATURES
Anti-inflammatory Medication individual basis.12 It is used to treat retroviral
Although not considered for long-term therapy and infections, with studies reporting that interferon
treatment, a corticosteroid injection will provide some delivered via oral mucosal absorption was as effective as
clinical relief but can decrease a patient’s ability to resist prednisolone in decreasing clinical signs in refractory
the inflammatory process while increasing the chance cases of FCGS.12,25
for diabetes mellitus.18
Prednisolone is often the short-acting steroid of choice Bovine Lactoferrin Therapy
to control inflammation and provide relief for patients Lactoferrin is an antimicrobial and anti-inflammatory
affected by FCGS. Prednisolone is often used on an that helps to decrease the proliferation of mononuclear
as-needed basis for symptomatic treatment on a cells and downregulating inflammation.18 In a study of
tapering dose in patients with refractory FCGS.12,25 13 cats with caudal FCGS, 77% of the clinical signs
were improved with treatment.30 The protocol used was
NSAIDs (nonsteroidal anti-inflammatory drugs) such a combination of piroxicam and bovine lactoferrin
as meloxicam and robenacoxib are often used for spray given once every other day for 4 weeks.
postoperative care, although use in patients with
contraindications such as hepatic or renal disease
should be avoided. Meloxicam is a great short-term Mesenchymal Stem Cell Therapy
NSAID; however, repeated doses of meloxicam over Mesenchymal stem cells (MSCs) are a promising
time has been associated with acute renal failure in cats. therapy for immune-mediated/inflammatory disorders,
Close monitoring and avoidance of long-term use are due to their potent immunomodulatory properties.11
advised.12,18 MSCs inhibit activated T-lymphocyte proliferation.18
In a study of 9 cats affected by refractory FCGS,
Cyclosporine patients were given 2 intravenous injections of
Cyclosporine is an immunosuppressive drug that exerts 20 million autologous adipose-derived MSCs every
its effect through inhibition of T-cell activation, other month. Seven of the 9 cats completed the study,
reducing interleukin-2 expression, and increasing T-cell with 5 cats achieving substantial or complete remission
numbers within the body.26,27 Cyclosporine may have and 2 cats with no clinical response to the treatment.11
an inhibitory effect on B cells as well.28
A follow-up study testing the effects of autologous or
This medication is most often used to decrease allogenic cell fusion given twice a month every other
inflammation in refractory (nonresolving) cases of month resulted in the cure/remission in more than
FCGS after full-mouth extraction. Due to its 60% of the cats affected by refractory FCGS.10
immunosuppressive effects, it should be used solely on
indoor cats because cats that venture outside will be at As promising as these results are, more testing is
a higher risk of infection. The positive effects of needed. Reasearchers at the University of California,
cyclosporine can be noted within 4 weeks of treatment.18 Davis, are conducting ongoing trials with MSCs and cats
Vomiting and diarrhea are the most common side affected by FCGS. The cost of MSC therapy typically
effects seen with patients taking this medication. ranges from $2000 to $4000, with many pet insurance
companies not offering coverage for treatment.31
Interferon
A group of signaling proteins that can interfere with Carbon Dioxide Laser Therapy
viral replication is known as interferons. Recombinant The use of carbon dioxide (CO2) laser therapy for
feline interferon omega (rFeIFN-ω) was the first FCGS has been met with favorable results when
interferon licensed for use in cats in veterinary combined with quality home care. The energy from the
medicine.29 laser decreases pain while enhancing healing through
protein synthesis, cell proliferation, and migration.
rFeIFN-ω is available in the United States solely Some veterinarians opt to use CO2 laser therapy at the
through the FDA Expanded Access/Compassionate Use time of initial surgical extraction; CO2 therapy may be
Program.12 This medication is imported on a strict helpful in cases of refractory FCGS as well.18
todaysveterinarynurse.com • WINTER 2023 • 69
FEATURES • PEER REVIEWED
Cannabinoids block. This block will enhance the efficacy and
A 2021 study explored the potential for cannabinoid duration of the local anesthetic but may be associated
use in cats by investigating potential cannabinoid with dose-related adverse effects, such as hypertension
receptors within the oral cavity of healthy cats and cats and bradycardia.33
with FCGS.32 This study focused on the potential
expression of cannabinoid receptors CB1 and CB2, Another intraoral nerve block combination is
GPR55 (G-protein–coupled receptor 55), TRPA1 buprenorphine (0.015 mg/kg) added to bupivacaine
(transient receptor potential ankyrin 1), and 5-HT1A (0.5% solution up to 5 mg).34 The addition of
(serotonin 1A) receptors. Samples were collected from buprenorphine to bupivacaine is known to potentially
8 healthy feline patients and 8 feline patients with extend the duration of analgesia up to 48 to 96 hours
FCGS. Compared to their healthy counterparts, the cats after surgery.34
affected by FCGS presented with markedly upregulated
cannabinoid and cannabinoid-related receptors. For the postoperative phase, oral buprenorphine is a
drug of choice to send home with a patient recovering
Based on the results of this study, there is evidence to from FCGS. In a recent randomized crossover study
support the endocannabinoid system as a potential featuring cats with FCGS, the subjects of the study
therapeutic target for patients affected by FCGS.32 This were given buprenorphine via oral mucosal absorption,
study is the first of its kind, garnering the need for the result being a significant effect on reduced pain
further investigation and the application of a scores in affected cats and a decrease in plasma
cannabinoid-rich product to determine the efficacy of concentration between individuals.35 The subcutaneous
this potential adjunct therapy for cats with FCGS. sustained-release formulation of buprenorphine is
another choice for painful patients after oral surgery
and will provide 24-hour pain relief for up to 3 days.
Opioids
Many of the patients affected by FCGS are in moderate
to severe pain and are typically malnourished. SUMMARY
Managing pain pre-, intra-, and postoperatively is a Although the exact etiology of FCGS remains a
major component to providing quality care. mystery, we have a better understanding of this
condition today thanks to ongoing research and
Using a pure opioid to treat moderate to severe pain in studies. Educating our clients about this debilitating
these patients is a must. Opioids such as morphine, disease is of the utmost importance. Early detection
methadone, hydromorphone, and fentanyl are great and treatment can be the difference between a patient
options for these patients in the perioperative phase. suffering in silence and one that is able to undergo
Constant rate infusions of an opiate are also warranted therapy and achieve remission. Surgical management of
during the intraoperative portion of the procedure. this disease in conjunction with medical management is
still considered the gold standard of care for these
Due to the nature of FCGS, it is understood that there patients. TVN
is a “wind-up effect” from the pain of having an
inflamed mouth for a long time. If not contraindicated,
the administration of a cyclohexylamine such as References
ketamine (1 to 2 mg/kg IV) is recommended and can 1. Gingivostomatitis. Cornell Feline Health Center. Accessed May 28,
2022. https://www.vet.cornell.edu/departments-centers-and-institutes/
be administered during induction or intraoperatively as cornell-feline-health-center/health-information/feline-health-topics/
needed for pain. Ketamine will help reduce the effects gingivostomatitis
of windup, unblock receptors, and create a synergistic 2. Healey KAE, Dawson S, Burrow R, et al. Prevalence of feline chronic
gingivo-stomatitis in first opinion veterinary practice. J Feline Med
analgesic effect. Surg. 2007;9(5):373-81. doi:10.1016/j.jfms.2007.03.003
3. Winer JN, Arzi B, Verstraete FJM. Therapeutic management of feline
chronic gingivostomatitis: a systematic review of the literature. Front
Another major component to pain management is Vet Sci. 2016;3:54. doi:10.3389/fvets.2016.00054
providing intraoral nerve blocks for these patients 4. Girard N, Servet E, Biourge V, Hennet P. Periodontal health
status in a colony of 109 cats. J Vet Dent. 2009;26(3):147-155.
undergoing a comprehensive oral health and assessment doi:10.1177/089875640902600301
treatment plan. If not contraindicated, 5. Pedersen NC. Inflammatory oral cavity diseases of the cat. Vet Clin
dexmedetomidine can be added (1 µg/kg) to North Am Small Anim Pract. 1992;22(6):1323-1345. doi:10.1016/s0195-
5616(92)50130-9
bupivacaine (0.5% solution up to 5 mg) as a nerve
70 • WINTER 2023 • todaysveterinarynurse.com
PEER REVIEWED • FEATURES
6. Williams CA, Aller MS. Gingivitis/stomatitis in cats. Vet Clin North 28. Winslow MM, Gallo EM, Neilson JR, Crabtree GR. The calcineurin
Am Small Anim Pract. 1992;22(6):1361-1383. doi:10.1016/s0195- phosphatase complex modulates immunogenic B cell responses.
5616(92)50132-2 Immunity. 2006;24(2):141-152. doi:10.1016/j.immuni.2005.12.013
7. Arzi B, Murphy B, Cox DP, Vapniarsky N, Kass PH, Verstraete FJM. 29. Leal RO, Gil S. The use of recombinant feline interferon omega
Presence and quantification of mast cells in the gingiva of cats with therapy as an immune-modulator in cats naturally infected with feline
tooth resorption, periodontitis and chronic stomatitis. Arch Oral immunodeficiency virus: new perspectives. Vet Sci. 2016;3(4):32.
Biol. 2010;55(2):148-154. doi:10.1016/j.archoralbio.2009.11.004 doi:10.3390/vetsci3040032
8. Rolim VM, Pavarini SP, Campos FS, et al. Clinical, pathological, 30. Hung YP, Yang YP, Wang HC, et al. Bovine lactoferrin and piroxicam as
immunohistochemical and molecular characterization of feline an adjunct treatment for lymphocytic-plasmacytic gingivitis stomatitis
chronic gingivostomatitis. J Feline Med Surg. 2017;19(4):403-409. in cats. Vet J. 2014;202(1):76-82. doi:10.1016/j.tvjl.2014.06.006
doi:10.1177/1098612X16628578
31. Turner B. Stem cell therapy for cats. Preventive Vet. September
9. Harley R, Gruffydd-Jones TJ, Day MJ. Immunohistochemical 20,2021. Accessed June 6, 2022. https://www.preventivevet.com/cats/
characterization of oral mucosal lesions in cats with chronic stem-cell-therapy-for-cats
gingivostomatitis. J Comp Pathol. 2011;144(4):239-250. doi:10.1016/j. 32. Polidoro G, Galiazzo G, Giancola F, et al. Expression of cannabinoid
jcpa.2010.09.173 and cannabinoid-related receptors in the oral mucosa of healthy
10. Arzi B, Clark KC, Sundaram A, et al. Therapeutic efficacy of fresh, cats and cats with chronic gingivostomatitis. J Feline Med Surg.
allogeneic mesenchymal stem cells for severe refractory feline 2021;23(8):679-691. doi:10.1177/1098612X20970510
chronic gingivostomatitis. Stem Cells Transl Med. 2017;6(8):1710-1722. 33. Pavlica M, Kržan M, Nemec A, Kosjek T, Baš A, Seliškar A.
doi:10.1002/sctm.17-0035 Cardiopulmonary effects and pharmacokinetics of dexmedetomidine
11. Arzi B, Mills-Ko E, Verstraete FJM, et al. Therapeutic efficacy of used as an adjunctive analgesic to regional anesthesia of the oral
fresh, autologous mesenchymal stem cells for severe refractory cavity with levobupivacaine in dogs. Animals (Basel). 2022;12(9):1217.
gingivostomatitis in cats. Stem Cells Transl Med. 2016;5(1):75-86. doi:10.3390/ani12091217
doi:10.5966/sctm.2015-0127 34. Snyder LBC, Snyder CJ, Hetzel S. Effects of buprenorphine added to
12. Greenfield B. Chronic feline gingivostomatitis: proven therapeutic bupivacaine infraorbital nerve blocks on isoflurane minimum alveolar
approaches and new treatment options. Todays Vet Pract. 2017;7(1):26- concentration using a model for acute dental/oral surgical pain in
38. dogs. J Vet Dent. 2016;33(2):90-96. doi:10.1177/0898756416657232
13. Krumbeck JA, Reiter AM, Pohl JC, et al. Characterization of oral 35. Stathopoulou TR, Kouki M, Pypendop BH, Johnston A, Papadimitriou
microbiota in cats: novel insights on the potential role of fungi S, Pelligand L. Evaluation of analgesic effect and absorption of
in feline chronic gingivostomatitis. 2021;10(7):904. doi:10.3390/ buprenorphine after buccal administration in cats with oral disease.
pathogens10070904 J Feline Med Surg. 2018;20(8):704-710. doi:10.1177/1098612X17727234
14. Lyon KF. Gingivostomatitis. Vet Clin North Am Small Anim Pract.
2005;35(4):891-911. doi:10.1016/j.cvsm.2005.02.001
15. Adler CJ, Malik R, Browne GV, Norris JM. Diet may influence the oral
microbiome composition in cats. Microbiome. 2016;4(1):23. doi:10.1186/
s40168-016-0169-y
16. Crawford J, Losey BJ. Feline dentistry. In: Perrone JR, ed. Small Animal
Dental Procedures for Veterinary Technicians and Nurses. 1st ed. Wiley-
Blackwell; 2012:143-160. Sheena Davis
17. Peralta S, Carney PC. Feline chronic gingivostomatitis is more Sheena is the founder and owner of Big Apple LVT
prevalent in shared households and its risk correlates with the Consulting & Education, with more than 16 years
number of cohabiting cats. J Feline Med Surg. 2019;21(12):1165-1171.
doi:10.1177/1098612X18823584 of clinical experience in both specialty and general
18. Oropharyngeal inflammation. In: Bellows J. Feline Dentistry. 2nd ed.
practice. She is a peer-reviewed author, course
Wiley-Blackwell; 2022:253-324. designer for the Veterinary Cannabis Guide Program,
19. Pathology in the pediatric patient. In: Niemiec BA. Small Animal library/media curator for the Veterinary Cannabis
Dental, Oral, & Maxillofacial Disease: A Color Handbook. 2nd ed. CRC Society, and frequent guest lecturer for conferences
Press; 2011:124-125. and events. She achieved dentistry VTS and Veterinary
20. Problems with the gingiva. In: Niemiec BA. Small Animal Dental, Oral, Cannabis Counselor certification in 2020.
& Maxillofacial Disease: A Color Handbook. 2nd ed. CRC Press;
2011:176-181.
21. Reiter AM, Johnston N, Anderson JG, Soltero-Rivera MM, Lobprise
HB. Domestic feline oral and dental diseases. In: Lobprise HB, Dodd
JR, eds. Wiggs’s Veterinary Dentistry: Principles and Practice. 2nd ed.
Wiley-Blackwell; 2019:439-461.
22. Jennings MW, Lewis JR, Soltero-Rivera MM, Brown DC, Reiter AM.
Effect of tooth extraction on stomatitis in cats: 95 cases (2000–2013).
JAVMA. 2015;246(6):654-660. doi:10.2460/javma.246.6.654
23. Druet I, Hennet P. Relationship between feline calicivirus load, oral
lesions, and outcome in feline chronic gingivostomatitis (caudal
stomatitis): retrospective study in 104 cats. Front Vet Sci. 2017;4:209.
doi:10.3389/fvets.2017.00209
24. Hennet P. Chronic gingivo-stomatitis in cats: long-term follow-up of
30 cases treated by dental extractions. J Vet Dent. 1997;14(1):15-21.
doi:10.1177/08987564970140
25. Lee DB, Verstraete FJM, Arzi B. An update on feline chronic
gingivostomatitis. Vet Clin North Am Small Anim Pract.
2020;50(5):973-982. doi:10.1016/j.cvsm.2020.04.002
26. Robson D. Review of the properties and mechanisms of action of
cyclosporine with an emphasis on dermatological therapy in dogs, cats
and people. Vet Rec. 2003;152(25):768-772. doi:10.1136/vr.152.25.768
27. Matsuda S, Koyasu S. Mechanisms of action of cyclosporine.
Immunopharmacology. 2000;47(2-3):119-125. doi:10.1016/s0162-
3109(00)00192-2
todaysveterinarynurse.com • WINTER 2023 • 71
You might also like
- Neil H. Riordan - Stem Cell Therapy A Rising Tide How Stem Cells Are Disrupting Medicine and Transforming LivesDocument341 pagesNeil H. Riordan - Stem Cell Therapy A Rising Tide How Stem Cells Are Disrupting Medicine and Transforming LivesLuca Dato100% (2)
- The Prevalence of Soil Transmitted Helminthiasis Among Filipino Pregnant Women Determined by FecalysisDocument11 pagesThe Prevalence of Soil Transmitted Helminthiasis Among Filipino Pregnant Women Determined by FecalysisCha GuingabNo ratings yet
- Malt MINI Neuropsychiatric InterviewDocument31 pagesMalt MINI Neuropsychiatric Interviewelvinegunawan50% (2)
- C+F-Physaloptera Infection in Dogs and CatsDocument11 pagesC+F-Physaloptera Infection in Dogs and Catstaner_soysurenNo ratings yet
- Blueprints PsychiatryDocument124 pagesBlueprints Psychiatrymbehar09No ratings yet
- Anupdateonfelinechronic Gingivostomatitis: Da Bin Lee,, Frank J.M. Verstraete,, Boaz ArziDocument10 pagesAnupdateonfelinechronic Gingivostomatitis: Da Bin Lee,, Frank J.M. Verstraete,, Boaz ArziAulia FadliahNo ratings yet
- An Update On Feline Chronic GengivostomatitisDocument11 pagesAn Update On Feline Chronic GengivostomatitisFlávia PinheiroNo ratings yet
- Lyon 2005Document21 pagesLyon 2005Renata StefaniNo ratings yet
- Feline Retroviruses Oral DiseasesDocument4 pagesFeline Retroviruses Oral DiseasesRigel EfNo ratings yet
- Bacteriophage Therapy: An Alternative To Conventional AntibioticsDocument4 pagesBacteriophage Therapy: An Alternative To Conventional AntibioticsAnandNo ratings yet
- Cat Diseases FinaalDocument17 pagesCat Diseases FinaalFaridah MagumparaNo ratings yet
- Shigella 261 FullDocument4 pagesShigella 261 FullDditelmNo ratings yet
- CASE STUDY - H.nanaDocument5 pagesCASE STUDY - H.nanaDr CommissionerNo ratings yet
- Parasitic Infections of The Gut in Children: Paediatrics and International Child HealthDocument9 pagesParasitic Infections of The Gut in Children: Paediatrics and International Child HealthamilyapraditaNo ratings yet
- Feline Chronic Gingivostomatitis VetsDocument4 pagesFeline Chronic Gingivostomatitis VetsnazmlehzaNo ratings yet
- Feline Gastrointestinal Eosinophilic SclerosingDocument16 pagesFeline Gastrointestinal Eosinophilic SclerosingEllen SauresNo ratings yet
- Johnston - Good STM Summary - 2012Document5 pagesJohnston - Good STM Summary - 2012RONALDO CANDRA WIJAYANo ratings yet
- Diarrhea ShelterDocument8 pagesDiarrhea SheltermhmdNo ratings yet
- Assessment of Changes in The Oral Microbiome That Occur in Dogs With Periodontal DiseaseDocument12 pagesAssessment of Changes in The Oral Microbiome That Occur in Dogs With Periodontal DiseaseMaria HernandezNo ratings yet
- IntroductionDocument2 pagesIntroductionapi-3718174No ratings yet
- Assessing Gut Microbiota Perturbations During The Early Phase of Infectious Diarrhea in Vietnamese ChildrenDocument18 pagesAssessing Gut Microbiota Perturbations During The Early Phase of Infectious Diarrhea in Vietnamese ChildrenKavyarani RathodNo ratings yet
- Literature Review On SalmonellaDocument6 pagesLiterature Review On Salmonellac5r9j6zj100% (1)
- Impetigo and Scabies e Disease Burden and Modern Treatment StrategiesDocument7 pagesImpetigo and Scabies e Disease Burden and Modern Treatment StrategiesHandy NugrahaNo ratings yet
- 1 s2.0 S0195561618300263 MainDocument24 pages1 s2.0 S0195561618300263 MainRonaldo Candra WijayaNo ratings yet
- Dipiro 8 ParasitDocument12 pagesDipiro 8 ParasitErik Firman RusdiantoNo ratings yet
- 105 Brucellosis: Etiology/Pathophysiology EpidemiologyDocument3 pages105 Brucellosis: Etiology/Pathophysiology EpidemiologyDamián ContrerasNo ratings yet
- Otita StaphyloDocument5 pagesOtita StaphylolastarelNo ratings yet
- Aggregating Resistant Hypocoagulability, Hyperfibrinolysis, Phagocytosis, and Neutrophil, Monocyte, and Lymphocyte Binding in Canine Whole BloodDocument15 pagesAggregating Resistant Hypocoagulability, Hyperfibrinolysis, Phagocytosis, and Neutrophil, Monocyte, and Lymphocyte Binding in Canine Whole BloodFabricio CamargoNo ratings yet
- Period Ontology JournalDocument12 pagesPeriod Ontology JournalOpeyemi IdaeworNo ratings yet
- Enteritis and Colitis in HorsesDocument44 pagesEnteritis and Colitis in HorsesANDRE LEONARD FARFAN SUAREZNo ratings yet
- Characterization of The Otic Bacterial Microbiota in DogsDocument10 pagesCharacterization of The Otic Bacterial Microbiota in Dogscecy loNo ratings yet
- Pet Ownership in Innmunocompromised ChildrenDocument11 pagesPet Ownership in Innmunocompromised ChildrenMicaPastineNo ratings yet
- Common and Emerging InfectiousDocument14 pagesCommon and Emerging InfectiousRachel AutranNo ratings yet
- Lom Mer 2013Document17 pagesLom Mer 2013M ElmanavieanNo ratings yet
- DiagnosisiofcattlhlmnthsDocument7 pagesDiagnosisiofcattlhlmnthsMarvelous SungiraiNo ratings yet
- Ochoa 2004Document8 pagesOchoa 2004Syarifah Maryam AlydrusNo ratings yet
- Feline Infectious Peritonitis ABCD Guidelines On PDocument12 pagesFeline Infectious Peritonitis ABCD Guidelines On Pxn5q8nckvkNo ratings yet
- An Update On Feline Infectious Peritonitis - Diagnostics and TherapeuticsDocument9 pagesAn Update On Feline Infectious Peritonitis - Diagnostics and TherapeuticsRhagaraRhaNo ratings yet
- The Pathology of Gastric and Duodenal Polyps: Current ConceptsDocument19 pagesThe Pathology of Gastric and Duodenal Polyps: Current Conceptsaccess pathologicNo ratings yet
- Associations Among Water, Sanitation, and Hygiene, and Food Exposures and Typhoid Fever in Case - Control Studies: A Systematic Review and Meta-AnalysisDocument12 pagesAssociations Among Water, Sanitation, and Hygiene, and Food Exposures and Typhoid Fever in Case - Control Studies: A Systematic Review and Meta-AnalysisKartikaa YantiiNo ratings yet
- Metagenomic Sequencing Identified Specific Phage Signature Discriminating Between Healthy and Diarrheal Neonatal PigletsDocument14 pagesMetagenomic Sequencing Identified Specific Phage Signature Discriminating Between Healthy and Diarrheal Neonatal PigletsGuadalupE Ortiz LópezNo ratings yet
- Ajg 2009 524Document10 pagesAjg 2009 524Alex Cristian IonutNo ratings yet
- Salmonellosis Research PaperDocument5 pagesSalmonellosis Research PaperxkcwaaqlgNo ratings yet
- E000679 FullDocument7 pagesE000679 FullKeysha AbigailNo ratings yet
- Salmonella, The Host and Disease: A Brief ReviewDocument8 pagesSalmonella, The Host and Disease: A Brief ReviewPedro Albán MNo ratings yet
- Veterinary Microbiology: S.C. BishopDocument6 pagesVeterinary Microbiology: S.C. BishopMuralidhar MettaNo ratings yet
- Jcad 13 6 48Document6 pagesJcad 13 6 48neetika guptaNo ratings yet
- J Smallrumres 2007 01 006Document12 pagesJ Smallrumres 2007 01 006Ali KareemNo ratings yet
- K Pneumoniae-Induced Infections - Case-Series Study in 697 Animals - BJMDocument10 pagesK Pneumoniae-Induced Infections - Case-Series Study in 697 Animals - BJMANGELA YULEIDY RIVERA VILLARREALNo ratings yet
- Growth and The Microbiome - Integrating Global Health With Basic ScienceDocument3 pagesGrowth and The Microbiome - Integrating Global Health With Basic ScienceTania ItovaNo ratings yet
- Veterinary Clinical Pathology Clerkship ProgramDocument46 pagesVeterinary Clinical Pathology Clerkship ProgramDrVijayata ChoudharyNo ratings yet
- Jurnal Patogenesis AmoebiasisDocument12 pagesJurnal Patogenesis AmoebiasisAngga NuralamNo ratings yet
- Research Paper On SalmonellosisDocument9 pagesResearch Paper On Salmonellosisukldyebkf100% (1)
- Transcriptomic Profiling of High-Density Giardia Foci Encysting in The Murine Proximal IntestineDocument17 pagesTranscriptomic Profiling of High-Density Giardia Foci Encysting in The Murine Proximal IntestineBrieNo ratings yet
- tmp6986 TMPDocument5 pagestmp6986 TMPFrontiersNo ratings yet
- Module 4-VMED 5335Document28 pagesModule 4-VMED 5335PETJSNVENo ratings yet
- Intestinal Phages Interact With Bacteria and Are Involved in Human DiseasesDocument24 pagesIntestinal Phages Interact With Bacteria and Are Involved in Human DiseasesafyyynyhNo ratings yet
- Histopathology - 2021 - Kővári - The Pathology of Gastric and Duodenal Polyps Current ConceptsDocument19 pagesHistopathology - 2021 - Kővári - The Pathology of Gastric and Duodenal Polyps Current Conceptsfa.anselmo89No ratings yet
- Pyometrainsmallanimals: Ragnvi HagmanDocument23 pagesPyometrainsmallanimals: Ragnvi HagmansalomonNo ratings yet
- Gmic 3 332Document13 pagesGmic 3 332Ema Emanuela SarcaNo ratings yet
- Biomarcadores Parvo 2013Document7 pagesBiomarcadores Parvo 2013María JesúsNo ratings yet
- Arch Dis Child 1998 Ladhani 85 8Document5 pagesArch Dis Child 1998 Ladhani 85 8Dian Ayu Permata SandiNo ratings yet
- Feline Immunodeficiency Virus: From Diagnosis to Well-being for Cats with FIVFrom EverandFeline Immunodeficiency Virus: From Diagnosis to Well-being for Cats with FIVNo ratings yet
- PB - Principles of InsuranceDocument4 pagesPB - Principles of InsurancePriyam BiswasNo ratings yet
- Bartonella Neuroretinitis: Images in Clinical MedicineDocument1 pageBartonella Neuroretinitis: Images in Clinical MedicineBalla ElkhiderNo ratings yet
- Pontiac Schools Pandemic Continuity Plan V - ParentDocument14 pagesPontiac Schools Pandemic Continuity Plan V - ParentAnalyn CanlasNo ratings yet
- Houser2007 Nariz VaciaDocument6 pagesHouser2007 Nariz VaciaFabian Camelo OtorrinoNo ratings yet
- Antituberculous Therapy in Special SituationsDocument8 pagesAntituberculous Therapy in Special SituationsMobeen Raza100% (1)
- Beclometasone-Formoterol As Maintenance and Reliever Treatment in Patients With Asthma: A Double-Blind, Randomised Controlled TrialDocument9 pagesBeclometasone-Formoterol As Maintenance and Reliever Treatment in Patients With Asthma: A Double-Blind, Randomised Controlled TrialArief WibowoNo ratings yet
- Geriatric Physiology and The Frailty SyndromeDocument22 pagesGeriatric Physiology and The Frailty SyndromeJoe Polanco100% (1)
- Kushal A, Gupta SK, Mehta M, Singh MMDocument3 pagesKushal A, Gupta SK, Mehta M, Singh MMJohnnel Acosido PrietosNo ratings yet
- Uworld Study-Guide 2020Document1,007 pagesUworld Study-Guide 2020Ramnath Rajbanshi100% (1)
- 3rd Periodical Mapeh 10Document5 pages3rd Periodical Mapeh 10Peter John Chavez RosellNo ratings yet
- Lecture 1. Sources of Microorganisms in FoodDocument23 pagesLecture 1. Sources of Microorganisms in FoodAnégria GahimbareNo ratings yet
- Isoko TuDocument3 pagesIsoko TuMhedo Bolarinwa AkanniNo ratings yet
- Outer Ear Infection (Swimmer's Ear)Document2 pagesOuter Ear Infection (Swimmer's Ear)ScraaaaNo ratings yet
- Surgery OspeDocument129 pagesSurgery Ospeudvash2024No ratings yet
- Date 28/mar/2023 10:09AM Unit Bio Ref Interval: Laboratory Investigation ReportDocument12 pagesDate 28/mar/2023 10:09AM Unit Bio Ref Interval: Laboratory Investigation ReportChauhanNo ratings yet
- Case Analysis Tool (CAT) Worksheet: Student's NameDocument7 pagesCase Analysis Tool (CAT) Worksheet: Student's NameDina KristevaNo ratings yet
- Hirschsprung DiseaseDocument21 pagesHirschsprung Diseaseeatingchoice100% (1)
- Vitamin CDocument5 pagesVitamin CsitapuNo ratings yet
- General Form No 86 Health ExaminationDocument1 pageGeneral Form No 86 Health ExaminationArminda Annabelle Bangks86% (22)
- Repetitive Strain Injuries, Prevention and Promotion - Wilson VegaDocument5 pagesRepetitive Strain Injuries, Prevention and Promotion - Wilson VegaWiilsoonvegaNo ratings yet
- Ivan P. Casserly MB BCH, Ravish Sachar MD, Jay S. Yadav MD - Practical Peripheral Vascular Intervention-LWW (2011)Document478 pagesIvan P. Casserly MB BCH, Ravish Sachar MD, Jay S. Yadav MD - Practical Peripheral Vascular Intervention-LWW (2011)Xunyao LuNo ratings yet
- Advanced Meridian Study For Yin Yoga Teachers: The Meridians: A Universe WithinDocument20 pagesAdvanced Meridian Study For Yin Yoga Teachers: The Meridians: A Universe Withinfey100% (1)
- (The European Society of Cardiology Series) Jose Luis Zamorano, Jeroen Bax, Juhani Knuuti, Patrizio Lancellotti, Fausto Pinto, Bogdan A. Popescu, Udo Sechtem - The ESC Textbook of Cardiovascular ImagiDocument865 pages(The European Society of Cardiology Series) Jose Luis Zamorano, Jeroen Bax, Juhani Knuuti, Patrizio Lancellotti, Fausto Pinto, Bogdan A. Popescu, Udo Sechtem - The ESC Textbook of Cardiovascular ImagiEdu MartinsNo ratings yet
- General: 6 Go-To Reads For Overcoming TraumaDocument3 pagesGeneral: 6 Go-To Reads For Overcoming Traumamysticalady100% (1)
- Advisory For Corona Virus: AyushDocument3 pagesAdvisory For Corona Virus: AyushPathu JellyNo ratings yet
- UMC Health Anxiety Inventory HAIDocument2 pagesUMC Health Anxiety Inventory HAIeemanfatima1261444No ratings yet
- Medical History FormatDocument5 pagesMedical History Formatkrzia TehNo ratings yet