Professional Documents
Culture Documents
Is Lec Immunodeficiency Diseases
Is Lec Immunodeficiency Diseases
Uploaded by
Kez Amolato0 ratings0% found this document useful (0 votes)
21 views9 pagesThere are nine categories of primary immunodeficiencies. Category 1 includes combined immunodeficiencies affecting both B and T cells, such as Severe Combined Immunodeficiency (SCID). Category 2 features combined immunodeficiencies associated with other syndromic features, exemplified by Wiskott-Aldrich Syndrome which involves immunodeficiency, eczema, and low platelet count. Purine-nucleoside phosphorylase (PNP) deficiency is a rare autosomal recessive trait that presents in infancy with recurrent infections and affects T cell mediated immunity through toxic purine metabolite accumulation.
Original Description:
Original Title
IS-LEC-IMMUNODEFICIENCY-DISEASES
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThere are nine categories of primary immunodeficiencies. Category 1 includes combined immunodeficiencies affecting both B and T cells, such as Severe Combined Immunodeficiency (SCID). Category 2 features combined immunodeficiencies associated with other syndromic features, exemplified by Wiskott-Aldrich Syndrome which involves immunodeficiency, eczema, and low platelet count. Purine-nucleoside phosphorylase (PNP) deficiency is a rare autosomal recessive trait that presents in infancy with recurrent infections and affects T cell mediated immunity through toxic purine metabolite accumulation.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
21 views9 pagesIs Lec Immunodeficiency Diseases
Is Lec Immunodeficiency Diseases
Uploaded by
Kez AmolatoThere are nine categories of primary immunodeficiencies. Category 1 includes combined immunodeficiencies affecting both B and T cells, such as Severe Combined Immunodeficiency (SCID). Category 2 features combined immunodeficiencies associated with other syndromic features, exemplified by Wiskott-Aldrich Syndrome which involves immunodeficiency, eczema, and low platelet count. Purine-nucleoside phosphorylase (PNP) deficiency is a rare autosomal recessive trait that presents in infancy with recurrent infections and affects T cell mediated immunity through toxic purine metabolite accumulation.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 9
IMMUNOLOGY AND SEROLOGY
Lecture| finals: Immunodeficiencies
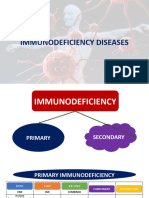
IMMUNODEFICIENCY DISEASES The Nine Categories of Primary
If autoimmune disorders are disorders were the Immunodeficiencies
immune system attacks itself. In Category 1: Combined Immunodeficiencies
immunodeficiency disease these are the Category 2: Combined Immunodeficiencies
disorders in which body’s immune system is not With Associate or Syndromic Features
functioning well because there is something Category 3: Predominantly Antibody
missing or there is a component that is Deficiencies
dysfunctional. People with this condition will Category 4: Diseases of Immune Dysregulation
have a decrease ability to defend themselves Category 5: Congenital Defects of Phagocyte
against infectious organisms and are more Number, Function, or Both
susceptible to developing certain types of Category 6: Defects in Innate Immunity –
cancer. sometimes they overlap because the complement
Evaluating Immunoglobulin Deficiency States deficiencies are also part of the innate immune
In evaluating immunoglobulin deficiency states, system
it is important to remember that blood levels of Category 7: Autoinflammatory Disorders
immunoglobulins change with age. Category 8: Complement Deficiencies
Age Category 9: Phenocopies of Primary
Blood level of IgG at birth = adult level Immunodeficiencies
o The blood level of IgG at birth Category 1: Combined Immunodeficiencies
is about the same as the adult - Contains diseases in which there are
level, reflecting transfer of defects in both humoral which mean
maternal IgG across the there are problems with the B cells and a
placenta. problem with the T cells as well
IgG level declines over the first 6 consequently affecting the cell-mediated
months of life immunity. This deficiencies result from
o The IgG level drops as maternal a mutation that develop that affects the
antibody is catabolized. development of both types of
Levels of IgA and IgM are low at birth lymphocytes or cause defective
o The concentrations of all interaction between the two antigen
immunoglobulins gradually rise specific claims of the adaptive immune
when the infant begins to sysrem.
produce antibodies at a few Severe Combined Immunodeficiency (SCID)
months of age, in response to The most serious of the congenital
environmental stimuli. immune
IgM (1 yr) → Igg (5-6 yrs) → IgA a group of related diseases that all affect
(adolescence) T- and B-cell function but with differing
o IgM reaches normal adult levels causes.
first, around 1 year of age, Interleukim-2 receptor gamma
followed by IgG at about 5 to 6 (IL2RG) gene
years of age. In some normal o Mutation of this, IL2RG is
children, IgA levels do not reach located on the X chromosome
normal adult values until and considered as the most
adolescence. Therefore, it is common form of the disease
important to compare a child’s approximately accounting for 46
immunoglobulin levels to age- of the cases in the United States.
matched reference ranges. o Patients with SCID generally
present early in infancy with
infection by nearly any type of
organism. Oral candidal
NJES BMLS-3D | RMT 2023 CUTIE 1
IMMUNOLOGY AND SEROLOGY
Lecture| finals: Immunodeficiencies
infections, pneumonia, and About two-thirds of PNP-deficient
diarrhea are the most common patients also have neurological
manifestations. disorders, but no characteristic
o Babies with Severe SCID physical abnormalities have been
should not be given live described. Because of the relatively
vaccines because their immune selective defect in cell-mediated
system is defective, live immunity, PNP deficiency can be
vaccines can actually cause confused with neonatal HIV
them severe illness unless infection. The two conditions can
immune reconstitution can be usually be distinguished by specific
achieved by bone marrow tests for anti-HIV antibody (if the
transplantation or by infant is old enough to be producing
specifically replacing a deficient antibody) and by assays for PNP
enzyme, patients with SCID die activity.
before they reach 2 years of age. o One immunodeficiency state for
Adenosine deaminase (ADA) which a specific enzymatic basis.
deficiency o PNP deficiency is a rare autosomal
o About 15 to 20 percent of the recessive trait. The condition
patients with SCID presents in infancy with recurrent
o leads to T-negative which mean or chronic pulmonary infections,
there is no/negative T cell, B cell, oral or cutaneous candidiasis,
no NK phenotype ; no antiseptic, it diarrhea, skin infections, urinary
doesn’t have any lymphocytes tract infections, and failure to
o Located in chromosome 1 region thrive.
of the long arm of the acute 21 o PNP deficiency affects an enzyme
o Will affect an enzyme involved in involved in the metabolism of
the metabolism of purines, it is purines.
actually had similarities with PNP Category 2: Combined Immunodeficiencies
deficiency. There will be toxic With Associate or Syndromic Features
metabolites of the purines that will - Differs from the category 1 in that the
accumulate in lymphoid cells and diseases in category 2 are characterized
impair their proliferation of Both B by non-immunologic features in addition
and T cells. It is not produce rather to the combined immunodeficiency.
these cells are unable to proliferate Diseases in this category are typically
because they’re being killed by caused by defects in cell mediated
toxic metabolites. immunity which will indirectly lead to
Purine-nucleoside phosphorylase problems with other branches of the
(PNP) deficiency immune responses. Oftentimes, diseases
o Produces moderate to severe defect can result from abnormalities at
in the cell mediated so it is more on different stages of T-cell development.
the T cells with a normal or mildly Wiskott-Aldrich Syndrome (WAS)
impaired humoral immunity. These are abnormalities in both the
o The number of T cells cellular and humoral branches of the
progressively decreases because of immune system, related to a general
the accumulation of defect in antigen processing.
deoxyguanosine triphosphate, a triad of immunodeficiency, eczema
toxic purine metabolite. (inflammation of the skin), and
o The levels of immunoglobulins are thrombocytopenia (low platelet count)
generally normal or increased.
NJES BMLS-3D | RMT 2023 CUTIE 2
IMMUNOLOGY AND SEROLOGY
Lecture| finals: Immunodeficiencies
o Patient will display severe The defect in the third and fourth
deficiency also of naturally pharyngeal pouches will have a severe
occurring IgM antibodies to and persistent decrease in T cell
ABO blood group or numbers.
isohemagglutinins which means o about 20 percent of children
you cannot do a reverse blood decrease in T-cell numbers
typing for the patient with WAS Severely affected children usually
because their anti-A and anti-B present in the neonatal period with
antibodies are very low or tetany (caused by hypocalcemia
almost zero. resulting from hypoparathyroidism) or
Absence of isohemagglutinins manifestations of cardiac defects.
o Absence of isohemagglutinins The immunodeficiency associated with
(IgM antibodies against ABO the DiGeorge anomaly is a quantitative
blood group antigens) is the defect in thymocytes. Not enough
most consistent laboratory mature T cells are made, but those that
finding in WAS and is often are present are functionally normal. The
used diagnostically. immunodeficiency of DiGeorge
o In addition, these patients have syndrome can be treated with fetal
persistently increased levels of thymus transplantation. Bone marrow
serum alpha-fetoprotein, which transplantation has also been successful
can also be a useful diagnostic in some patients, as has administration
feature. of thymic hormones.
Low levels of IgM, normal levels of IgA Ataxia-Telangiectasia
and IgG, and increased levels of IgE A rare autosomal recessive syndrome
o The antibody against the ABO characterized by cerebellar ataxia which
blood group which is called is involuntary muscle movements and
isohemagglutinins are naturally telangiectasias where the blood vessels
occurring antibodies against are so fragile, it usually involves
antibodies which are IgM in capillary swelling resulting in red
nature are severely decrease. patches on the skin especially on the
o The gene responsible for the earlobes and conjunctiva.
defect is called the WASp gene,
and it is located on the X
chromosome, region p11. It
actually affects the:
integral membrane protein CD43
DiGeorge Anomaly
developmental abnormality of the
thymus
o The thymus will fail to develop.
Thymus is the exclusive primary
lymphoid organ for the
production, education, and
differentiation of the T-cells Combined defect of both humoral and
is a developmental abnormality of the cellular immunity. Antibody response to
third and fourth pharyngeal pouches that antigens, especially polysaccharides, is
affects thymic development or blunted.
consequently leading to the impaired
development of thymus in the embryo.
NJES BMLS-3D | RMT 2023 CUTIE 3
IMMUNOLOGY AND SEROLOGY
Lecture| finals: Immunodeficiencies
The levels of IgG2, IgA, and IgE are lack of immunoglobulins of all classes.
often low or absent, although the pattern Males exclusive
can be quite variable. Arrested differentiation at the pre-B
Number of circulating T cells is often cell stage
decreased. o No pre-B cells no plasma cells
Category 3: Predominantly Antibody in their lymphoid tissues but
Deficiencies they will still have the T-cells
- This category encompasses conditions in both in normal quantity and
which the main characteristic is low normal quality
levels of serum immunoglobulins term o About half of the patients have a
agammaglobulinemia. The family history of the syndrome.
mechanisms of agammaglobulinemia They develop recurrent bacterial
include genetic defects and B-cell infections beginning in infancy,
maturation or mutations leading to as maternal antibody is cleared.
defective interactions between B and T The underlying genetic mechanism is a
cells. The conditions in this category are deficiency of an enzyme called the
the most common immune deficiencies Bruton tyrosine kinase (Btk) in B-cell
representing about 50% of the primary progenitor cells. Lack of the enzyme
Immunodeficiencies. apparently causes a failure in the
Transient Hypogammaglobulinemia immunoglobulin variable and heavy
All infants experience low levels of (Vh) gene rearrangement. The syndrome
immunoglobulins at approximately 5 to 6 can be differentiated from transient
months of age, but in some babies, the low hypogammaglobulinemia of infancy by
levels persist for a longer time. the absence of CD19 positive B cells in
Low levels of immunoglobulins at the peripheral blood, by the abnormal
infancy with normal numbers of B cells histology of lymphoid tissues, and by its
Severe pyogenic sinopulmonary and persistence beyond 2 years of age.
skin infections *In transient you have low antibodies yet you
o Because these children do not have normal number of B cells. In X-Linked you
begin synthesizing have decrease antibody but you don’t have B
immunoglobulin promptly, they cells.
can experience this as protective Selective IgA Deficiency
maternal IgG is cleared. Most common congenital
9 to 15 months of age immunodeficiency
o Immunoglobulin levels usually Asymptomatic
normalize spontaneously o But those with symptoms
*The mechanism of this transient usually have infections of the
hypogammaglobulinemia is not known. These respiratory and gastrointestinal
patients have normal numbers of circulating tract and an increased tendency
CD19 positive B cells. This condition does not to autoimmune diseases
appear to be X-linked, although it is more (because we know IgA is mostly
common in males. The cause may be related to a found in bodily secretion so the
delayed maturation of one or more components cause of selective IgA
of the immune system, possibly T helper cells. deficiency is impaired
X-linked Bruton’s Tyrosine Kinase (Btk) differentiation of lymphocytes
Deficiency to become IgA producing
lack circulating mature CD19 positive B plasma cells ) such as systemic
cells and exhibit a deficiency lupus erythematosus,
rheumatoid arthritis, celiac
NJES BMLS-3D | RMT 2023 CUTIE 4
IMMUNOLOGY AND SEROLOGY
Lecture| finals: Immunodeficiencies
disease, and thyroiditis. Allergic o That is why transient after 9-15
disorders and malignancy are months of age will be gone; the
also more common. antibody will arise. In CVI, it
< 5 mg/mL : severe will reach 71 years old that has
IgA antibodies in severe state no immunoglobulins because B-
o Anti-IgA antibodies are cells although present they will
produced by 30 to 40 percent of not differentiate into the
patients with severe IgA immunoglobulin producing
deficiency. These antibodies can plasma cells.
cause anaphylactic reactions CVI is often a diagnosis of exclusion,
when blood products containing where an immunodeficiency is present
IgA are transfused. Because with no specific genetic defect defined
many patients with severe IgA Isolated IgG Subclass Deficiency
deficiency have no other Usually diagnosed by having level of
symptoms, the IgA deficiency one or more of the IgG subclasses is
may not be detected until the more than two standard deviations
patient experiences a transfusion below the mean age-appropriate level.
reaction resulting from the The most common subclass deficiency
presence of anti-IgA antibodies. is IgG4, with IgG1 deficiency being the
Products for transfusion to least common yet more clinical
known IgA-deficient patients significant, although IgG4 subclass
should be collected from IgA- deficiency may have the least clinical
deficient donors, or cellular significance.
products should be washed to IgG1 or IgG3 : reduced response
remove as much donor plasma capability to protein antigens such as
as possible toxins, while selective deficiencies of
Common Variable Immunodeficiency (CVI) IgG2: impaired responses to
most common primary immune polysaccharide antigens, which cause
deficiency (PID) with a severe clinical recurrent infections with
syndrome polysaccharide-encapsulated bacteria
Is a heterogeneous group of disorders such as Streptococcus pneumoniae and
with a prevalence of about 1 in 25,000. Haemophilus influenza. These include
Patients usually begin to have symptoms heavy chain gene deletions and
in their 20s and 30s, but age at onset transcriptional defects.
ranges from 7 to 71 years of age.
hypogammaglobulinemia that leads to
recurrent bacterial infections,
particularly sinusitis and pneumonia.
low serum IgG level IN patients with
recurrent bacterial infections
In contrast to X-linked
agammaglobulinemia, most patients
with CVI have normal numbers of
mature B cells. However, these B cells
do not differentiate normally into
immunoglobulin-producing plasma
cells.
NJES BMLS-3D | RMT 2023 CUTIE 5
IMMUNOLOGY AND SEROLOGY
Lecture| finals: Immunodeficiencies
Category 4: Diseases of Immune Category 5: Congenital Defects of Phagocyte
Dysregulation Number, Function, or Both
- These are diseases with normal numbers - These are primary immune deficiencies
of T or B cells but we just control over where there is an abnormality in the
their functions; less on quantitative but phagocytic cell.
more on qualitative and they would have Chronic Granulomatous Disease (CGD)
usually normal numbers of T and B The most common and the best characterized of
cells. all the neutrophil abnormalities, this is a genetic
Autoimmune lymphoproliferative defect in any of the several components of
syndrome NADPH oxidative system that can result in
o Many of the diseases in this CGD phenotype by making the neutrophil
category will also have features of incapable of generating an oxidative burst.
autoimmunity the outlet of Remember: For phagocyte, part of the process
autoimmune lymphoproliferative of phagocytosis is bacterial killing through the
syndrome which involves mutation production of reactive oxygen species- hydrogen
in genes coding for caspases that is peroxide that will kill the bacteria. This
involved in apoptosis. Once there is phenomenon is called as the oxidative burst. If
defective apoptosis in the thymus the oxidative burst does not happen the bacteria
this will lead to autoreactive cells in will not be killed and thus they will be choke,
the circulation so that will cause can’t digest eventually that will kill also the
autoimmune lymphoproliferative neutrophils if it was from the inside. Typically
syndrome catalyst positive organisms such as
Defective apoptosis Staphylococcus aureus, Burkholderia cepacia
CD25 deficiency Chromobacterium violaceum are involved in
o Manifested by a lack of T-reg cells. addition to fungi such as aspergillus and
No T-reg cells which leads to nocardia. The infection would usually begin
reparation and autoimmunity before 1 year of age and the syndrome is often
because T-reg cells are like the fatal in childhood.
regulatory cells they control the Inability of the patient’s neutrophils to
length or the duration of the produce the reactive forms of oxygen
immune response, without them necessary for normal bacterial killing
there is a tendency of hyper Nitroblue tetrazolium (NBT) reaction
proliferation and eventually o Before, to diagnose CGD we
autoimmunity will happen. employed this. The neutrophil
Mutation in the fox53 gene is of the patients are evaluated on
required for direct differentiation so their ability to reduce the natural
they may show a similar clinical blue tetrazolium dye. NBT
presentation. reduction is caused by the
Chediak-Higashi syndrome production of hydrogen
o Immune deficiency that is peroxide and other reactive
associated that has forms of oxygen. In other
hypopigmentation (albino) that words, the NBT dye will be
is caused by mutation in the IST used by the neutrophil. The
gene. There is a reduced number neutrophil will reduce NBT dye
of NK cells and neutrophils but into a blue precipitate. The
an increased production of reduction will supposed to
inflammatory proteins. produce H2O (WATER) they
will reduce the NBT. The
reduction will cause the NBT to
NJES BMLS-3D | RMT 2023 CUTIE 6
IMMUNOLOGY AND SEROLOGY
Lecture| finals: Immunodeficiencies
happen and there will be no An inability to generate enough NADPH
color. If it reduce because no to supply reducing equivalents to the
H2O production it will become NADPH oxidase system.
blue and it is a positive. o This leads to a defect in
hydrogen peroxide production
and a clinical picture similar to
that of CGD.
Myeloperoxidase deficiency
Recurrent candidal infections.
o Is relatively common, occurring
in about 1 in 3000 persons in the
United States. Deficient patients
may have this.
o Defects of neutrophil secondary
granules have also been
described. However, the
molecular nature of the defects
is unknown.
Dihydrorhodamine (DHR) Leukocyte Adhesion Deficiency (LAD)
o The methodology is more of a free Not on phagocyte killing but on the problem in
flow cytometric assay which involves the adhesion of neutrophils and even on your
the labeling of the neutrophils with monocytes
DHR .DHR will fluoresce when it is CD18- LAD is a deficiency in this
reduced. The neutrophils are then protein.
activated using PHORBOL o Component of adhesion
MYRISTATE ACETATE OR receptors on neutrophils and
PMA which is mitogenic for monocytes (with CD11b or
neutrophils. The resultant oxidative CD11c) and on T cells (with
burst will reduce the DHR resulting CD11a) is defective.
in fluorescence that may be o The CD18 deficiency is
quantitated on the flow cytometer. transmitted with autosomal
Neutrophils from CGD patients will recessive inheritance and has
be unable to undergo the oxidative variable expression. This defect
burst and will show less leads to abnormal adhesion,
fluorescence, less confusing than motility, aggregation,
normal neutrophils. This technique is chemotaxis, and endocytosis by
more objective and quantitative than the affected leukocytes.
the traditional NBT technique. The Delayed wound healing, chronic skin
fluorescence us directly proportional infections, intestinal and respiratory
to the amount/ ability of the tract infections, and periodontitis.
neutrophil to do and to produce an Decreased amount of the CD11/18
oxidative burst so low fluorescence
antigen on patient leukocytes by flow
means no sedative burst. High
cytometry
fluorescence means normal and
o defect in CD18 can be
functional killing of neutrophil. diagnosed by detecting this
Neutrophil Glucose-6-Phosphate
Category 6: Defects in Innate Immunity
Dehydrogenase Deficiency
mutations in Toll-like receptors (TLRs)
o TLR 3 specific deficiency will
result in herpes simplex
NJES BMLS-3D | RMT 2023 CUTIE 7
IMMUNOLOGY AND SEROLOGY
Lecture| finals: Immunodeficiencies
encephalitis, defect in TLRs o Tumor necrosis factor (TNF)
signaling pathways example is receptor-associated periodic
IRAK4 deficiency can also syndrome (TRAPS) – Is caused by a
happen and cause herpes mutation in TNF -Tumor Necrosis
encephalitis. Factor receptor associated is TNFR-
o The diagnosis for category 6 SF1A gene. TNFRSF1A gene codes
involves more on clinical for the TNF receptor and my result in
presentation and would lead to recurrent fevers as well as ocular
molecular analysis to identify endpoint inflammation in the ;
the specific gene mutation. o Early onset inflammatory bowel
Category 7: Autoinflammatory Disorders disease – another non-inflammatory
Can be subdivided into two classifications those disorder under the category 7 is
involving the inflammasome and non- caused by imitation in genes coding
inflammasome. for IL-10 and its receptor.
Inflammasome Category 8: Complement Deficiencies
o Is a protein oligomer that contains C1q, C4 and C2: lupuslike syndrome
caspase enzymes and other proteins o C2 is most common but least
associated with apoptosis. Caspase important
= apoptosis. Located primarily in C3: lupuslike syndrome but recurrent
myeloid cells and may be activated infectionwith encapsulated organisms
by various microbial substances. C5-C9 : Neisseria meningitides
Once activated the inflammasome infections
stimulates the production of the C1 esterase inhibitor: hereditary
pro-inflammatory cytokines IL-1 neuroangioedema
and IL-18. Basically it is called Category 9: Phenocopies of Primary
inflammatory because you are Immunodeficiencies
producing a protein that will Chronic mucocutaneous candidiasis – a
activate stimulation of production disease that was classifies as a cell
of the pro-inflammatory cytokines mediated deficiency now transferred to
that is harmful to your immune category 9. This disease is induced by a
system that is like genetic mutation in the AIRE gene a
autoinflammatory. It is like an gene involved in the production of the
autoimmune disease for the antibodies or either IL-17 and IL-22.
immune system that leads to an Screening Tests
immunodeficiency Before you all these tests always bear in mind
o Hyper IgD syndrome- caused by a that you always have to start with patient
deficiency of mevalonate kinase an history. Why? Think about it and answer this
enzyme that involved in steroid question on the exam.
synthesis pathway which is the Complete blood count (CBC) and white
syndrome has been seen primarily blood cell (WBC) differentials
in Northern European population Levels of serum IgG, IgM, and IgA and
o Muckle-Wells syndrome – caused by levels of the subclasses of IgG
mutation in CIAS1 gene coding for
Assay for isohemagglutinins
cryopyrin a component of the
CH50 assay
inflammasome. The patients here
Flow cytometric assay – esp. for more
will present with urticarial (sige
problem on the quantitative defect
pangatol) and amyloidosis.
Non-inflammasome
NJES BMLS-3D | RMT 2023 CUTIE 8
IMMUNOLOGY AND SEROLOGY
Lecture| finals: Immunodeficiencies
NJES BMLS-3D | RMT 2023 CUTIE 9
You might also like
- AOM IVIG Comparison Chart 0124 13Document1 pageAOM IVIG Comparison Chart 0124 13Heba_Al_KhozaeNo ratings yet
- Disorders of The Immune System ImmunityDocument7 pagesDisorders of The Immune System ImmunityMarinelle TumanguilNo ratings yet
- Immunodeficiency DisordersDocument8 pagesImmunodeficiency DisordersMutya XDNo ratings yet
- 2019 Immunodeficiency DisordersDocument14 pages2019 Immunodeficiency DisordersamallullaNo ratings yet
- Szczawinska Poplonyk2009 PDFDocument12 pagesSzczawinska Poplonyk2009 PDFFernando CruzNo ratings yet
- Lab ApproachDocument8 pagesLab ApproachMuhammad ShaikhNo ratings yet
- Immunode Ficiency Disorders: Education GapsDocument16 pagesImmunode Ficiency Disorders: Education GapsNadejda MarcovaNo ratings yet
- Finals Lesson 2Document6 pagesFinals Lesson 2Kevin Vincent AquinoNo ratings yet
- Immunodeficiency DisorderDocument14 pagesImmunodeficiency DisorderAaryan PatelNo ratings yet
- Immunodeficiency Diseases: Presented byDocument46 pagesImmunodeficiency Diseases: Presented byMayank TiwariNo ratings yet
- The Evolving Landscape of Primary Immunodeficiencies: EditorialDocument2 pagesThe Evolving Landscape of Primary Immunodeficiencies: EditorialEnrico Emilio LatorracaNo ratings yet
- Immunodeficiency Syndromes - Hiv/Aids Infection: DR O.O. WilliamsDocument35 pagesImmunodeficiency Syndromes - Hiv/Aids Infection: DR O.O. Williamsseun williamsNo ratings yet
- 492-Article Text-1094-1-10-20220501Document13 pages492-Article Text-1094-1-10-20220501Suwai Batul Aslamiyah A Md KepNo ratings yet
- Immuno Defi Ice NcyDocument22 pagesImmuno Defi Ice Ncysara11224466No ratings yet
- Pediatrics - ImmunodeficiencyDocument3 pagesPediatrics - ImmunodeficiencyJasmine KangNo ratings yet
- Immunodeficiency Diseases: Professor Shahenaz M.HussienDocument17 pagesImmunodeficiency Diseases: Professor Shahenaz M.HussienVINAY KUMAR DHAWANNo ratings yet
- Immune DeficiencyDocument18 pagesImmune DeficiencyDr anas AbdullahNo ratings yet
- Jurnal 2Document8 pagesJurnal 2tasya tazkia regita zahraNo ratings yet
- Ims Finals Complete Copy 1st Sem, Sy21-22Document322 pagesIms Finals Complete Copy 1st Sem, Sy21-22hersey miayoNo ratings yet
- Severe Combined Immunodeficiency: Submitted To: DR Amber Submitted By: Mahnoor Khawaja Course: ImmunologyDocument16 pagesSevere Combined Immunodeficiency: Submitted To: DR Amber Submitted By: Mahnoor Khawaja Course: ImmunologyManisanthosh KumarNo ratings yet
- Reviewofprimary ImmunodeficiencydiseasesDocument58 pagesReviewofprimary Immunodeficiencydiseasespriti adsulNo ratings yet
- Primary Immunodeficiency - PMCDocument1 pagePrimary Immunodeficiency - PMCfaniNo ratings yet
- Immunodeficiency BriefingDocument4 pagesImmunodeficiency BriefingAldiyanzah Lukman100% (1)
- Sepsis Neonatorum UpdatedDocument87 pagesSepsis Neonatorum Updated'Eduard Laab AlcantaraNo ratings yet
- Guillain - Barré Syndrome, Transverse Myelitis and Infectious DiseasesDocument16 pagesGuillain - Barré Syndrome, Transverse Myelitis and Infectious DiseasesAdy De La RosaNo ratings yet
- Immunodeficiency DiseasesDocument59 pagesImmunodeficiency DiseasesJkgamerzNo ratings yet
- Example of Immunoglobulin Effect of Excess/Deficiency Brief ExplanationDocument5 pagesExample of Immunoglobulin Effect of Excess/Deficiency Brief ExplanationJayrelle D. SafranNo ratings yet
- Immunodeficiency SyndromesDocument124 pagesImmunodeficiency SyndromesDrSwati Prakash Poddar100% (1)
- bt302 Mid & Final Term NotesDocument58 pagesbt302 Mid & Final Term NotesFarogh e HaqNo ratings yet
- Unbalanced Immune System Immunodeficiencies and AutoimmunityDocument9 pagesUnbalanced Immune System Immunodeficiencies and Autoimmunitycruz98No ratings yet
- Overview InmunodeficienciaDocument25 pagesOverview InmunodeficienciaLuisa AlandeteNo ratings yet
- Immunodeficiency DisordersDocument3 pagesImmunodeficiency DisordersMohan VamsiNo ratings yet
- Study Stack - Immunology Final Table Review PDFDocument8 pagesStudy Stack - Immunology Final Table Review PDF장주연No ratings yet
- Equine Immunodeficiency DisordersDocument12 pagesEquine Immunodeficiency DisordersValentina SuescunNo ratings yet
- Tinjauan Kepustakaan: Imunodefisiensi PrimerDocument16 pagesTinjauan Kepustakaan: Imunodefisiensi PrimerBayu Prawira PutraNo ratings yet
- Aspergilosis InvasivaDocument3 pagesAspergilosis InvasivaEduardo RuizNo ratings yet
- IMMUNODEFICIENCYDocument36 pagesIMMUNODEFICIENCYgfb22wdbbrNo ratings yet
- MS Semifinals Complete NotesDocument59 pagesMS Semifinals Complete NotesMarvie TorralbaNo ratings yet
- Primary ImmunodeficienciesDocument4 pagesPrimary Immunodeficienciesnayd dsNo ratings yet
- Kuby5 19 ImmunoDefsDocument31 pagesKuby5 19 ImmunoDefsDenisa EugeniaNo ratings yet
- 6 - Immune Deficiency Diseases 2Document8 pages6 - Immune Deficiency Diseases 2Belle Galao GepteNo ratings yet
- ImmunodeficiencyDocument33 pagesImmunodeficiencyIqra ShaheenNo ratings yet
- Severe Combined Immunodeficiency 06-02-08Document11 pagesSevere Combined Immunodeficiency 06-02-08Manisanthosh KumarNo ratings yet
- Management of Patients With Immune Deficiency DisordersDocument11 pagesManagement of Patients With Immune Deficiency DisordersmasheennavirgoNo ratings yet
- Immune Deficincies - SarahDocument10 pagesImmune Deficincies - SarahkhaledNo ratings yet
- Journal Reading BiomarkerDocument17 pagesJournal Reading BiomarkerjoganksNo ratings yet
- Literatur Internasional 3Document18 pagesLiteratur Internasional 3MegaUtariNo ratings yet
- Searching For Light in Long Tunnel: PID Care in Indonesia: Dina MuktiartiDocument33 pagesSearching For Light in Long Tunnel: PID Care in Indonesia: Dina MuktiartiRoberto SoehartonoNo ratings yet
- Guillain-Barré Syndrome Pediatrico 2018Document4 pagesGuillain-Barré Syndrome Pediatrico 2018Mariam Plata100% (1)
- Defisiensi Imun S2Document43 pagesDefisiensi Imun S2fathoni_00No ratings yet
- Neuro-Inflammatory DisordersDocument7 pagesNeuro-Inflammatory DisordersInes StrenjaNo ratings yet
- Immunodeficiency DisordersDocument67 pagesImmunodeficiency DisordersAkbar SaleemNo ratings yet
- IMS - Immunomodulation & ImmunodeficienciesDocument3 pagesIMS - Immunomodulation & ImmunodeficienciesJeanne RodiñoNo ratings yet
- B. 11 Situation - Care of Client With Problems in Inflammatory & Immunologic ResponseDocument4 pagesB. 11 Situation - Care of Client With Problems in Inflammatory & Immunologic ResponseSOLEIL LOUISE LACSON MARBAS100% (1)
- Peds in Review - Immunodeficiency DisordersDocument14 pagesPeds in Review - Immunodeficiency DisordersNICU LEVELNo ratings yet
- Role of Immunoglobulins in Neonatal SepsisDocument6 pagesRole of Immunoglobulins in Neonatal SepsisMuhar RandiNo ratings yet
- MiltonOzorio CynthiaCardoso Etal IOC 2006Document14 pagesMiltonOzorio CynthiaCardoso Etal IOC 2006kaiomelcNo ratings yet
- Autoinmunidad e InmunodeficienciaDocument9 pagesAutoinmunidad e InmunodeficienciaJorge Verdugo MuñozNo ratings yet
- 1 & 2 - Body - S - Defenses - Failures - 2021Document41 pages1 & 2 - Body - S - Defenses - Failures - 2021RayNo ratings yet
- Pediatric Immunology: A Case-Based Collection with MCQs, Volume 2From EverandPediatric Immunology: A Case-Based Collection with MCQs, Volume 2No ratings yet
- Immunodeficiency DisordersDocument67 pagesImmunodeficiency DisordersAkbar SaleemNo ratings yet
- Immunology Mcqs-4: InstructionsDocument22 pagesImmunology Mcqs-4: InstructionsadehkordiNo ratings yet
- 7 - MRCP - Part One - Past-Papers - Jan 2017Document274 pages7 - MRCP - Part One - Past-Papers - Jan 2017zgjybbzNo ratings yet
- Allergic Transfusion Reactions: William J. Savage, MD, PHDDocument4 pagesAllergic Transfusion Reactions: William J. Savage, MD, PHDNausheenNo ratings yet
- Ijms 21 05223 PDFDocument42 pagesIjms 21 05223 PDFrohailNo ratings yet
- Immuno2008, Vol.28, Issues 4, Intravenous Immunoglobulin Treatment of ImmunodeficiencyDocument187 pagesImmuno2008, Vol.28, Issues 4, Intravenous Immunoglobulin Treatment of ImmunodeficiencydudapaskasNo ratings yet
- Immunology FirecrackerDocument45 pagesImmunology FirecrackerMariam A. KarimNo ratings yet
- Circulating Complexes, Iga: Precipitins, Immune and DeficiencyDocument3 pagesCirculating Complexes, Iga: Precipitins, Immune and Deficiencyroopaljain123No ratings yet
- Ministry of Education and Science of Ukraine V.N. Karazin Kharkiv National UniversityDocument44 pagesMinistry of Education and Science of Ukraine V.N. Karazin Kharkiv National UniversityDrTushar GoswamiNo ratings yet
- Immunodeficiency: Abdul Ghaffar, Ph.D. E-Mail: Ghaffar@med - Sc.eduDocument10 pagesImmunodeficiency: Abdul Ghaffar, Ph.D. E-Mail: Ghaffar@med - Sc.eduAhmed Goma'aNo ratings yet
- Celiac Disease Diagnostic Testing AlgorithmDocument1 pageCeliac Disease Diagnostic Testing AlgorithmtarogiosdrakNo ratings yet
- Current Approach To Primary Immunodeficiency Diseases: March 2019Document9 pagesCurrent Approach To Primary Immunodeficiency Diseases: March 2019Ryan ProxyNo ratings yet
- Washed Red Cells: Theory and Practice: Review ArticleDocument11 pagesWashed Red Cells: Theory and Practice: Review Articlemy accountNo ratings yet