Professional Documents
Culture Documents
First Page PDF
First Page PDF
Uploaded by
Bukola Christianah AkinCopyright:
Available Formats
You might also like
- Klebsiella Pneumonia - StatPearls - NCBI BookshelfDocument7 pagesKlebsiella Pneumonia - StatPearls - NCBI BookshelfMariel Siason-OrbisoNo ratings yet
- Samman MSDocument5 pagesSamman MSSamman zakaNo ratings yet
- Review of Known and Unknown Facts of Klebsiella Pneumoniae and Its Relationship With AntibioticsDocument8 pagesReview of Known and Unknown Facts of Klebsiella Pneumoniae and Its Relationship With AntibioticsPhuong NguyenNo ratings yet
- Klebsiella Pneumoniae Pathogenesis: Etiology/BacteriologyDocument4 pagesKlebsiella Pneumoniae Pathogenesis: Etiology/Bacteriologysuper cute100% (1)
- Antibioticoterapia Na Pneumonia Pediátrica 2006Document7 pagesAntibioticoterapia Na Pneumonia Pediátrica 2006Tainah__100% (1)
- Reviews: Population Genomics ofDocument16 pagesReviews: Population Genomics ofRaul MolloNo ratings yet
- Clinical Microbiology Reviews-1998-Podschun-589.fullDocument15 pagesClinical Microbiology Reviews-1998-Podschun-589.fullDorin SaulescuNo ratings yet
- Pneumo Virulence FactorsDocument14 pagesPneumo Virulence FactorsTauseef Asmat MalghaniNo ratings yet
- Tuberculosis: NeurocysticercosisDocument7 pagesTuberculosis: Neurocysticercosismenesesgilbertmd333No ratings yet
- Chlamydophila Abortus Pelvic: Inflammatory DiseaseDocument3 pagesChlamydophila Abortus Pelvic: Inflammatory DiseaseJefri SoniNo ratings yet
- K10 - Important Pathogenic Bacteria During Child (Mikrobiologi)Document42 pagesK10 - Important Pathogenic Bacteria During Child (Mikrobiologi)Juanto Tio VocNo ratings yet
- 2002 23 132 Benjamin Gaston: Pediatr. RevDocument11 pages2002 23 132 Benjamin Gaston: Pediatr. RevDiego DíazNo ratings yet
- 4 Infección Neonatal C. DifficileDocument5 pages4 Infección Neonatal C. DifficileLuis Astudillo MedinaNo ratings yet
- Hypervirulent Klebsiella Pneumoniae Clinical and Molecular PerspectivesDocument18 pagesHypervirulent Klebsiella Pneumoniae Clinical and Molecular PerspectivesMargauxNo ratings yet
- Topic: "Picoronoviruses. Coxsackie. ECHO. Laboratory Diagnostics"Document26 pagesTopic: "Picoronoviruses. Coxsackie. ECHO. Laboratory Diagnostics"deekshit dcNo ratings yet
- 2002 23 132 Benjamin Gaston: Pediatrics in ReviewDocument11 pages2002 23 132 Benjamin Gaston: Pediatrics in ReviewLuis Fernando Rojas ArroyoNo ratings yet
- Final Project VinceDocument21 pagesFinal Project Vincekiss4444f4No ratings yet
- TreatmentDocument3 pagesTreatmentNarasimharao HarnoorNo ratings yet
- Update On Bacterial Pneumonia and Pleuropneumonia in The Adult Horse-2Document16 pagesUpdate On Bacterial Pneumonia and Pleuropneumonia in The Adult Horse-2Laura VillotaNo ratings yet
- Neonatal SepsisDocument39 pagesNeonatal SepsisBryan KernsNo ratings yet
- Neonatal Varicella: PediatricsDocument5 pagesNeonatal Varicella: Pediatricsnoval rafsanjaniNo ratings yet
- KlebDocument14 pagesKlebAzraNo ratings yet
- Research Papers On KlebsiellaDocument8 pagesResearch Papers On Klebsiellagzrvpcvnd100% (1)
- Pneumococcus PneumoniaDocument20 pagesPneumococcus PneumoniaIseoghenaNo ratings yet
- Coxsackievirus: Shandong University School of MedicineDocument26 pagesCoxsackievirus: Shandong University School of MedicineMonRedNo ratings yet
- GetahunLTBINEJM2015 PDFDocument9 pagesGetahunLTBINEJM2015 PDFSharah Stephanie IINo ratings yet
- Current Concepts: C - A P CDocument9 pagesCurrent Concepts: C - A P CMarice Ferrufino SchmidtNo ratings yet
- Catterall 1999Document10 pagesCatterall 1999choklletmrNo ratings yet
- Clinical Findings: A. Specimens, Microscopic Examination, and CultureDocument3 pagesClinical Findings: A. Specimens, Microscopic Examination, and CultureLeah VicenteNo ratings yet
- Klebsiella Sp. Epidemiology Taxonomy and PatogenicityDocument15 pagesKlebsiella Sp. Epidemiology Taxonomy and PatogenicityDulce MariaNo ratings yet
- CTX-M Paper PDFDocument4 pagesCTX-M Paper PDFTunde OdetoyinNo ratings yet
- Opthalmia UmDocument23 pagesOpthalmia Umnanu-jenuNo ratings yet
- Kingella KingaeDocument7 pagesKingella KingaeChad SilbaNo ratings yet
- Wolbachia Induces Density-Dependent Inhibition To Dengue Virus in Mosquito CellsDocument8 pagesWolbachia Induces Density-Dependent Inhibition To Dengue Virus in Mosquito CellsFebby AuliaNo ratings yet
- Neisseria MeningitidisDocument53 pagesNeisseria MeningitidisPratibha AgarwalNo ratings yet
- Klebsiella Pneumoniae ThesisDocument6 pagesKlebsiella Pneumoniae Thesisaprillaceyjackson100% (1)
- Haemophilus, Bordetella, Brucella,: and FrancisellaDocument29 pagesHaemophilus, Bordetella, Brucella,: and FrancisellaDaniel AtiehNo ratings yet
- Introduction of Klebsiella PneumoniaeDocument189 pagesIntroduction of Klebsiella PneumoniaeAnia sahaNo ratings yet
- Picornaviridae & Adenoviridae - Raja Pardomuan HarahapDocument63 pagesPicornaviridae & Adenoviridae - Raja Pardomuan HarahapM. RamazaliNo ratings yet
- Histopathologic Changes Related To Fibrotic Oviduct Occlusion After Genital Tract Infection Chlamydia MuridarumDocument8 pagesHistopathologic Changes Related To Fibrotic Oviduct Occlusion After Genital Tract Infection Chlamydia MuridarumAgung SentosaNo ratings yet
- Antecedentes INFECTOLOGYDocument40 pagesAntecedentes INFECTOLOGYDr. Claro RichardNo ratings yet
- 10 Atypical PneumoniaDocument4 pages10 Atypical PneumoniaKevinTevesYupanquiNo ratings yet
- Fatal Neonatal Septicaemia and Meningitis Due To Haemophilus Influenzae AcquiredDocument2 pagesFatal Neonatal Septicaemia and Meningitis Due To Haemophilus Influenzae AcquiredEden AparicioNo ratings yet
- Pelvic Infections in Women: Belgian Guidelines: OutlineDocument35 pagesPelvic Infections in Women: Belgian Guidelines: OutlineJose mauricio PalenciaNo ratings yet
- Practice EssentialsDocument6 pagesPractice EssentialsdessydaswarNo ratings yet
- 1 s2.0 S0091674915001876 Main PDFDocument10 pages1 s2.0 S0091674915001876 Main PDFAlirman OdeNo ratings yet
- Papilovasicular Eruption in Pregnanct Woman PDFDocument2 pagesPapilovasicular Eruption in Pregnanct Woman PDFSyed Furqan AliNo ratings yet
- CLERKS Diagnostic Exam Microbiology 2022Document10 pagesCLERKS Diagnostic Exam Microbiology 2022Dey SibalNo ratings yet
- CANDIDIASISDocument18 pagesCANDIDIASISLiz GonzalesNo ratings yet
- Chapter 56Document57 pagesChapter 56Rahmat MuliaNo ratings yet
- Diagnostic Laboratory Tests Epidemiology and Ecology: A. Specimens, Microscopic Examination, and CultureDocument3 pagesDiagnostic Laboratory Tests Epidemiology and Ecology: A. Specimens, Microscopic Examination, and CultureAnggaNo ratings yet
- Subacute MeningitisDocument42 pagesSubacute Meningitisderarataye6No ratings yet
- Group 1Document5 pagesGroup 1Ardesh AbdilleNo ratings yet
- Challenge To Healthcare: Multidrug Resistance in Klebsiella PneumoniaeDocument5 pagesChallenge To Healthcare: Multidrug Resistance in Klebsiella PneumoniaeSutha SaskaraNo ratings yet
- PreventionDocument6 pagesPreventionBipin PatelNo ratings yet
- MICROMIDTERMSLABDocument27 pagesMICROMIDTERMSLABmicaellaabedejosNo ratings yet
- p1761 PDFDocument8 pagesp1761 PDFUtari UbNo ratings yet
- Mycobacterium Tuberculosis: Bañagado, Noreen B. Bs - Medical Technology 2Document4 pagesMycobacterium Tuberculosis: Bañagado, Noreen B. Bs - Medical Technology 2Noreen Bañagado100% (1)
- Raja Sekar An 2013Document14 pagesRaja Sekar An 2013aneu virginaNo ratings yet
- Vaccinated: From Cowpox to mRNA, the Remarkable Story of VaccinesFrom EverandVaccinated: From Cowpox to mRNA, the Remarkable Story of VaccinesRating: 4 out of 5 stars4/5 (39)
- Efek Samping: Azelaic Acid 20 % Cream: Effects On Quality of Life and Disease Severity in Adult Female Acne PatientsDocument11 pagesEfek Samping: Azelaic Acid 20 % Cream: Effects On Quality of Life and Disease Severity in Adult Female Acne PatientsAlfina RahmaNo ratings yet
- ERICDocument3 pagesERICVivienne IrvingNo ratings yet
- Chapter 55 - Progressive Kidney Disease - It Was Only A Matter of Time Level IIIDocument5 pagesChapter 55 - Progressive Kidney Disease - It Was Only A Matter of Time Level IIIaleksme88No ratings yet
- Diabetes Mellitus: Postpartum Type 2 Diabetes Mellitus Insulin Blood Hyperglycemia DiabetesDocument8 pagesDiabetes Mellitus: Postpartum Type 2 Diabetes Mellitus Insulin Blood Hyperglycemia DiabetesRHUBY ABENOJANo ratings yet
- APA DSM5TR Level2RepetitiveThoughtsAndBehaviorsAdultDocument3 pagesAPA DSM5TR Level2RepetitiveThoughtsAndBehaviorsAdultG. S.No ratings yet
- High Dose Per Fraction, Hypofractionated Treatment Effects in The Clinic (HyTEC) - An OverviewDocument10 pagesHigh Dose Per Fraction, Hypofractionated Treatment Effects in The Clinic (HyTEC) - An OverviewgriloucuraNo ratings yet
- FULL-TEXT - NCLEX-RN Practice Quiz Test Bank 4 - NurseslabsDocument77 pagesFULL-TEXT - NCLEX-RN Practice Quiz Test Bank 4 - NurseslabsRonaldo Matos PerezNo ratings yet
- SGOT (Aspartate Aminotransferase, AST, Glutamic Oxaloacetic Transaminase)Document9 pagesSGOT (Aspartate Aminotransferase, AST, Glutamic Oxaloacetic Transaminase)Reman A. AlingasaNo ratings yet
- (G1) What Triggers ADHDDocument24 pages(G1) What Triggers ADHDhvtvan0702No ratings yet
- Community Based Assessment Checklist (CBAC) FormDocument3 pagesCommunity Based Assessment Checklist (CBAC) FormShubhaDavalgiNo ratings yet
- Test Bank For Goulds Pathophysiology For The Health Professions 6th Edition by HubertDocument6 pagesTest Bank For Goulds Pathophysiology For The Health Professions 6th Edition by HubertFranklin Roberts100% (41)
- 709 WewykubabuDocument3 pages709 WewykubabuJobinNo ratings yet
- Medicolegal DeathDocument13 pagesMedicolegal DeathWASIF ISMAILNo ratings yet
- Psychology 227 HW - 4 (1) ...Document6 pagesPsychology 227 HW - 4 (1) ...Brian ochiengNo ratings yet
- ECmed Eval SheetDocument1 pageECmed Eval SheetSalie GuarinoNo ratings yet
- Management of The Critically Ill PatientDocument36 pagesManagement of The Critically Ill PatientZhi Hao OoiNo ratings yet
- Diagnostic Report: FinalDocument2 pagesDiagnostic Report: FinalRAGHA DIAGNOSTIC CENTRENo ratings yet
- MSN I 20.4.2020 FN TyphoidDocument20 pagesMSN I 20.4.2020 FN TyphoidDr. DhaneshNo ratings yet
- Midterms Psyc LecDocument14 pagesMidterms Psyc LecMiden AlbanoNo ratings yet
- Head and Neck Cancer Awareness Exploratory Survey in Undergraduate StudentsDocument7 pagesHead and Neck Cancer Awareness Exploratory Survey in Undergraduate StudentsSteve GannabanNo ratings yet
- Blue Red LesionDocument14 pagesBlue Red LesionXara Barretto MagadiaNo ratings yet
- AbPsy Practice Exam 1Document15 pagesAbPsy Practice Exam 1janlyn espinosaNo ratings yet
- ALSANGEDY BULLETS FOR PACES Cluster Headache (2nd Edition)Document2 pagesALSANGEDY BULLETS FOR PACES Cluster Headache (2nd Edition)mrcp study notesNo ratings yet
- Cranial Nerve Disorders: Ernest E. WangDocument13 pagesCranial Nerve Disorders: Ernest E. Wangirsyad tsaniNo ratings yet
- Ir Jajad KaokabDocument13 pagesIr Jajad Kaokabdharsa plyNo ratings yet
- Lecture 5 Brachytherapy Implantation - 6-18 FinalDocument10 pagesLecture 5 Brachytherapy Implantation - 6-18 FinalArcrije JerezNo ratings yet
- Emergency NursingDocument15 pagesEmergency NursingAshley Ishika100% (1)
- GRTP Wallet Card FinalDocument2 pagesGRTP Wallet Card FinalIrish FroggyNo ratings yet
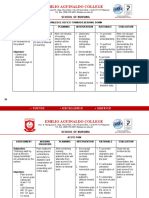
- Emilio Aguinaldo College: School of NursingDocument9 pagesEmilio Aguinaldo College: School of NursingPaullennium Chester MaganaNo ratings yet
- Makalah Temu 10 Bahasa InggrisDocument14 pagesMakalah Temu 10 Bahasa InggrisArhya DutaNo ratings yet
First Page PDF
First Page PDF
Uploaded by
Bukola Christianah AkinOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
First Page PDF
First Page PDF
Uploaded by
Bukola Christianah AkinCopyright:
Available Formats
CHAPTER 115 Klebsiella 1541
C H A P T E R
Klebsiella
115 Randall G. Fisher
Klebsiella is a genus of Enterobacteriaceae, a frequent cause of reported outbreaks of Klebsiella were in neonatal ICUs.54
of nosocomial pediatric infection. Classically described by Outbreaks in newborns continue to occur frequently world-
Friedländer38 as a cause of pneumonia, Klebsiella can cause infec- wide.2,7,24,30,49,90,100 Most outbreaks in newborns have been
tions of the urinary tract, lung, and central venous catheters in associated with K. pneumoniae infection, but scattered outbreaks
high-risk newborns and immunocompromised older children.18 of K. oxytoca infection in nurseries also have been reported.6,112 A
high percentage of infants in ICUs may become colonized with
hospital strains of Klebsiella.46 In one longitudinal study in which
BACTERIOLOGY weekly rectal swabs were cultured, 80 (22%) of 368 neonates in
an ICU harbored extended-spectrum β-lactamase (ESBL)–
Klebsiella organisms were named for Edwin Klebs, the noted producing Klebsiella spp.15 Infecting organisms have been isolated
German bacteriologist.86 Distinguishing features of Klebsiella spp. from care providers and from mothers of colonized infants.24 One
include the absence of motility and the presence of a polysac- report described an outbreak among newborns associated with
charide capsule that gives rise to large mucoid colonies on solid infestation of a neonatal unit by cockroaches colonized with
media. The organisms are oxidase-negative and citrate-positive; infecting Klebsiella strains.25 Klebsiella may spread from newborn
they ferment inositol and hydrolyze urea but do not produce units to adult units; interhospital and international spread of
ornithine decarboxylase or hydrogen sulfide. Acetoin and 2,3- resistant strains has been described.23,30,106
butanediol predominate over acidic end-products during sugar Ribotyping, pulsed field gel electrophoresis, and DNA ampli-
fermentation (positive result on the Voges-Proskauer test). Four fication techniques have proven valuable in characterizing Kleb-
species of Klebsiella commonly are agreed on by microbiologists: siella strains associated with outbreaks.70,108 Different ribotypes
Klebsiella pneumoniae (the most common human pathogen), Kleb- that share plasmids conferring antibiotic resistance can be respon-
siella oxytoca (a less common human pathogen), Klebsiella terrigena, sible for pediatric infections in a particular institution.12 Strains
and Klebsiella planticola. Previously, K. planticola was recovered expressing ESBL may become endemic and may present a
almost exclusively from soil and aquatic environments; reports complex and diverse pattern of production of enzymes with resis-
now suggest that this organism may be a relatively common tance to β-lactamase inhibitors.31,35 Although broad-spectrum
neonatal pathogen in some parts of the world.92,113 K. planticola resistance to β-lactams and carbapenems72 has been described,
may express virulence factors similar to those of K. pneumoniae.93 some longitudinal studies have shown that the frequency of
Organisms are defined serologically by their capsular poly- ESBLs in K. pneumoniae isolates is decreasing.103
saccharide (K antigens) and lipopolysaccharide (O antigens).
Significant cross-reactivity exists between the capsule of some
pneumococci (e.g., 19F) and Klebsiella.68 The reader is referred to PATHOPHYSIOLOGY
a review by Podschun and Ullman95 for a detailed description of
Klebsiella spp. Pneumonias caused by Klebsiella most commonly arise from colo-
nization of the upper respiratory tract, followed by aspiration of
organisms to the lower respiratory tract. Some degree of gram-
EPIDEMIOLOGY negative oropharyngeal colonization is a normal finding in new-
borns. The oropharynx of nearly one third of healthy newborns
Friedländer38 proposed that K. pneumoniae was the most common is colonized by gram-negative rods, including Klebsiella, by the
cause of community-acquired pneumonia, an observation that time infants reach 1 month of age; colonization rates generally
was refuted by Fraenkel’s36 observations on pneumococcal pneu- are lower in breast-fed infants.9 Antibiotic pressure in high-risk
monia. K. pneumoniae accounts for less than 10 percent of hospi- newborns and older children has been observed to promote over-
talized cases of pneumonia in adults.20 Klebsiella spp. now are in growth of Klebsiella.11,105 Enteric organisms are recovered less
greatest evidence as opportunistic nosocomial pathogens of the frequently from the oropharynx of healthy older children and
urinary tract, respiratory tract, biliary tract, and bloodstream. In adults; oral colonization with gram-negative rods is increased
one survey of the Centers for Disease Control and Prevention, during illness,57 after postoperative viral infections,56,97 and in
the infection rate of nosocomial K. pneumoniae was 16.7 infections debilitated adults.73 Increased adherence of gram-negative rods
per 10,000 patients discharged.54 Hand-carriage generally is to oropharyngeal cells contributes to increased colonization.56
regarded as the common mode of transmission.42 Environmental Elastase made by polymorphonuclear cells contributes to such
sources of Klebsiella spp. include contaminated blood-pressure colonization by reducing the fibronectin coating of sugar recep-
monitoring equipment,98 ventilator traps,42 dialysate,64 ultrasound tors.27 The capsule plays an initial role in interactions of epithelial
coupling gel,40 dextrose solution,66 and hand disinfectant.101 The cells but is not required for an adhesin interaction with the cell
emergence of plasmid-mediated, β-lactamase resistance can be surface.34 Adherence properties may be affected by plasmid
responsible for the rapid spread of resistant organisms to suscep- content29 and may be transferred between E. coli and K.
tible patients in intensive care units (ICUs).10,12 Outbreaks may pneumoniae.53
be complex; patient-to-patient transmission of epidemic strains In animal models of sepsis, capsular polysaccharide (K anti-
containing different plasmids may be interspersed with sporadic, gens) is a virulence factor; monoclonal antibodies to the K anti-
nonepidemic Klebsiella infections.12 Klebsiella spp. are second only gens reduce the severity of illness in mice.67 In a mouse model of
to Escherichia coli as causes of sepsis,41 with the highest rates of urinary tract infection, the K antigens seemed to be more impor-
infection being reported from larger hospitals affiliated with tant in infection than was the lipopolysaccharide (O antigens),
medical schools. and clinical strains deficient in lipopolysaccharide retained viru-
Klebsiella spp. commonly are highlighted as pathogens of lence by resistance of capsule to complement.3,19 In one series of
debilitated adults and alcoholics,60 but by 1985, nearly 50 percent adult patients, capsular type K2 frequently was associated with
You might also like
- Klebsiella Pneumonia - StatPearls - NCBI BookshelfDocument7 pagesKlebsiella Pneumonia - StatPearls - NCBI BookshelfMariel Siason-OrbisoNo ratings yet
- Samman MSDocument5 pagesSamman MSSamman zakaNo ratings yet
- Review of Known and Unknown Facts of Klebsiella Pneumoniae and Its Relationship With AntibioticsDocument8 pagesReview of Known and Unknown Facts of Klebsiella Pneumoniae and Its Relationship With AntibioticsPhuong NguyenNo ratings yet
- Klebsiella Pneumoniae Pathogenesis: Etiology/BacteriologyDocument4 pagesKlebsiella Pneumoniae Pathogenesis: Etiology/Bacteriologysuper cute100% (1)
- Antibioticoterapia Na Pneumonia Pediátrica 2006Document7 pagesAntibioticoterapia Na Pneumonia Pediátrica 2006Tainah__100% (1)
- Reviews: Population Genomics ofDocument16 pagesReviews: Population Genomics ofRaul MolloNo ratings yet
- Clinical Microbiology Reviews-1998-Podschun-589.fullDocument15 pagesClinical Microbiology Reviews-1998-Podschun-589.fullDorin SaulescuNo ratings yet
- Pneumo Virulence FactorsDocument14 pagesPneumo Virulence FactorsTauseef Asmat MalghaniNo ratings yet
- Tuberculosis: NeurocysticercosisDocument7 pagesTuberculosis: Neurocysticercosismenesesgilbertmd333No ratings yet
- Chlamydophila Abortus Pelvic: Inflammatory DiseaseDocument3 pagesChlamydophila Abortus Pelvic: Inflammatory DiseaseJefri SoniNo ratings yet
- K10 - Important Pathogenic Bacteria During Child (Mikrobiologi)Document42 pagesK10 - Important Pathogenic Bacteria During Child (Mikrobiologi)Juanto Tio VocNo ratings yet
- 2002 23 132 Benjamin Gaston: Pediatr. RevDocument11 pages2002 23 132 Benjamin Gaston: Pediatr. RevDiego DíazNo ratings yet
- 4 Infección Neonatal C. DifficileDocument5 pages4 Infección Neonatal C. DifficileLuis Astudillo MedinaNo ratings yet
- Hypervirulent Klebsiella Pneumoniae Clinical and Molecular PerspectivesDocument18 pagesHypervirulent Klebsiella Pneumoniae Clinical and Molecular PerspectivesMargauxNo ratings yet
- Topic: "Picoronoviruses. Coxsackie. ECHO. Laboratory Diagnostics"Document26 pagesTopic: "Picoronoviruses. Coxsackie. ECHO. Laboratory Diagnostics"deekshit dcNo ratings yet
- 2002 23 132 Benjamin Gaston: Pediatrics in ReviewDocument11 pages2002 23 132 Benjamin Gaston: Pediatrics in ReviewLuis Fernando Rojas ArroyoNo ratings yet
- Final Project VinceDocument21 pagesFinal Project Vincekiss4444f4No ratings yet
- TreatmentDocument3 pagesTreatmentNarasimharao HarnoorNo ratings yet
- Update On Bacterial Pneumonia and Pleuropneumonia in The Adult Horse-2Document16 pagesUpdate On Bacterial Pneumonia and Pleuropneumonia in The Adult Horse-2Laura VillotaNo ratings yet
- Neonatal SepsisDocument39 pagesNeonatal SepsisBryan KernsNo ratings yet
- Neonatal Varicella: PediatricsDocument5 pagesNeonatal Varicella: Pediatricsnoval rafsanjaniNo ratings yet
- KlebDocument14 pagesKlebAzraNo ratings yet
- Research Papers On KlebsiellaDocument8 pagesResearch Papers On Klebsiellagzrvpcvnd100% (1)
- Pneumococcus PneumoniaDocument20 pagesPneumococcus PneumoniaIseoghenaNo ratings yet
- Coxsackievirus: Shandong University School of MedicineDocument26 pagesCoxsackievirus: Shandong University School of MedicineMonRedNo ratings yet
- GetahunLTBINEJM2015 PDFDocument9 pagesGetahunLTBINEJM2015 PDFSharah Stephanie IINo ratings yet
- Current Concepts: C - A P CDocument9 pagesCurrent Concepts: C - A P CMarice Ferrufino SchmidtNo ratings yet
- Catterall 1999Document10 pagesCatterall 1999choklletmrNo ratings yet
- Clinical Findings: A. Specimens, Microscopic Examination, and CultureDocument3 pagesClinical Findings: A. Specimens, Microscopic Examination, and CultureLeah VicenteNo ratings yet
- Klebsiella Sp. Epidemiology Taxonomy and PatogenicityDocument15 pagesKlebsiella Sp. Epidemiology Taxonomy and PatogenicityDulce MariaNo ratings yet
- CTX-M Paper PDFDocument4 pagesCTX-M Paper PDFTunde OdetoyinNo ratings yet
- Opthalmia UmDocument23 pagesOpthalmia Umnanu-jenuNo ratings yet
- Kingella KingaeDocument7 pagesKingella KingaeChad SilbaNo ratings yet
- Wolbachia Induces Density-Dependent Inhibition To Dengue Virus in Mosquito CellsDocument8 pagesWolbachia Induces Density-Dependent Inhibition To Dengue Virus in Mosquito CellsFebby AuliaNo ratings yet
- Neisseria MeningitidisDocument53 pagesNeisseria MeningitidisPratibha AgarwalNo ratings yet
- Klebsiella Pneumoniae ThesisDocument6 pagesKlebsiella Pneumoniae Thesisaprillaceyjackson100% (1)
- Haemophilus, Bordetella, Brucella,: and FrancisellaDocument29 pagesHaemophilus, Bordetella, Brucella,: and FrancisellaDaniel AtiehNo ratings yet
- Introduction of Klebsiella PneumoniaeDocument189 pagesIntroduction of Klebsiella PneumoniaeAnia sahaNo ratings yet
- Picornaviridae & Adenoviridae - Raja Pardomuan HarahapDocument63 pagesPicornaviridae & Adenoviridae - Raja Pardomuan HarahapM. RamazaliNo ratings yet
- Histopathologic Changes Related To Fibrotic Oviduct Occlusion After Genital Tract Infection Chlamydia MuridarumDocument8 pagesHistopathologic Changes Related To Fibrotic Oviduct Occlusion After Genital Tract Infection Chlamydia MuridarumAgung SentosaNo ratings yet
- Antecedentes INFECTOLOGYDocument40 pagesAntecedentes INFECTOLOGYDr. Claro RichardNo ratings yet
- 10 Atypical PneumoniaDocument4 pages10 Atypical PneumoniaKevinTevesYupanquiNo ratings yet
- Fatal Neonatal Septicaemia and Meningitis Due To Haemophilus Influenzae AcquiredDocument2 pagesFatal Neonatal Septicaemia and Meningitis Due To Haemophilus Influenzae AcquiredEden AparicioNo ratings yet
- Pelvic Infections in Women: Belgian Guidelines: OutlineDocument35 pagesPelvic Infections in Women: Belgian Guidelines: OutlineJose mauricio PalenciaNo ratings yet
- Practice EssentialsDocument6 pagesPractice EssentialsdessydaswarNo ratings yet
- 1 s2.0 S0091674915001876 Main PDFDocument10 pages1 s2.0 S0091674915001876 Main PDFAlirman OdeNo ratings yet
- Papilovasicular Eruption in Pregnanct Woman PDFDocument2 pagesPapilovasicular Eruption in Pregnanct Woman PDFSyed Furqan AliNo ratings yet
- CLERKS Diagnostic Exam Microbiology 2022Document10 pagesCLERKS Diagnostic Exam Microbiology 2022Dey SibalNo ratings yet
- CANDIDIASISDocument18 pagesCANDIDIASISLiz GonzalesNo ratings yet
- Chapter 56Document57 pagesChapter 56Rahmat MuliaNo ratings yet
- Diagnostic Laboratory Tests Epidemiology and Ecology: A. Specimens, Microscopic Examination, and CultureDocument3 pagesDiagnostic Laboratory Tests Epidemiology and Ecology: A. Specimens, Microscopic Examination, and CultureAnggaNo ratings yet
- Subacute MeningitisDocument42 pagesSubacute Meningitisderarataye6No ratings yet
- Group 1Document5 pagesGroup 1Ardesh AbdilleNo ratings yet
- Challenge To Healthcare: Multidrug Resistance in Klebsiella PneumoniaeDocument5 pagesChallenge To Healthcare: Multidrug Resistance in Klebsiella PneumoniaeSutha SaskaraNo ratings yet
- PreventionDocument6 pagesPreventionBipin PatelNo ratings yet
- MICROMIDTERMSLABDocument27 pagesMICROMIDTERMSLABmicaellaabedejosNo ratings yet
- p1761 PDFDocument8 pagesp1761 PDFUtari UbNo ratings yet
- Mycobacterium Tuberculosis: Bañagado, Noreen B. Bs - Medical Technology 2Document4 pagesMycobacterium Tuberculosis: Bañagado, Noreen B. Bs - Medical Technology 2Noreen Bañagado100% (1)
- Raja Sekar An 2013Document14 pagesRaja Sekar An 2013aneu virginaNo ratings yet
- Vaccinated: From Cowpox to mRNA, the Remarkable Story of VaccinesFrom EverandVaccinated: From Cowpox to mRNA, the Remarkable Story of VaccinesRating: 4 out of 5 stars4/5 (39)
- Efek Samping: Azelaic Acid 20 % Cream: Effects On Quality of Life and Disease Severity in Adult Female Acne PatientsDocument11 pagesEfek Samping: Azelaic Acid 20 % Cream: Effects On Quality of Life and Disease Severity in Adult Female Acne PatientsAlfina RahmaNo ratings yet
- ERICDocument3 pagesERICVivienne IrvingNo ratings yet
- Chapter 55 - Progressive Kidney Disease - It Was Only A Matter of Time Level IIIDocument5 pagesChapter 55 - Progressive Kidney Disease - It Was Only A Matter of Time Level IIIaleksme88No ratings yet
- Diabetes Mellitus: Postpartum Type 2 Diabetes Mellitus Insulin Blood Hyperglycemia DiabetesDocument8 pagesDiabetes Mellitus: Postpartum Type 2 Diabetes Mellitus Insulin Blood Hyperglycemia DiabetesRHUBY ABENOJANo ratings yet
- APA DSM5TR Level2RepetitiveThoughtsAndBehaviorsAdultDocument3 pagesAPA DSM5TR Level2RepetitiveThoughtsAndBehaviorsAdultG. S.No ratings yet
- High Dose Per Fraction, Hypofractionated Treatment Effects in The Clinic (HyTEC) - An OverviewDocument10 pagesHigh Dose Per Fraction, Hypofractionated Treatment Effects in The Clinic (HyTEC) - An OverviewgriloucuraNo ratings yet
- FULL-TEXT - NCLEX-RN Practice Quiz Test Bank 4 - NurseslabsDocument77 pagesFULL-TEXT - NCLEX-RN Practice Quiz Test Bank 4 - NurseslabsRonaldo Matos PerezNo ratings yet
- SGOT (Aspartate Aminotransferase, AST, Glutamic Oxaloacetic Transaminase)Document9 pagesSGOT (Aspartate Aminotransferase, AST, Glutamic Oxaloacetic Transaminase)Reman A. AlingasaNo ratings yet
- (G1) What Triggers ADHDDocument24 pages(G1) What Triggers ADHDhvtvan0702No ratings yet
- Community Based Assessment Checklist (CBAC) FormDocument3 pagesCommunity Based Assessment Checklist (CBAC) FormShubhaDavalgiNo ratings yet
- Test Bank For Goulds Pathophysiology For The Health Professions 6th Edition by HubertDocument6 pagesTest Bank For Goulds Pathophysiology For The Health Professions 6th Edition by HubertFranklin Roberts100% (41)
- 709 WewykubabuDocument3 pages709 WewykubabuJobinNo ratings yet
- Medicolegal DeathDocument13 pagesMedicolegal DeathWASIF ISMAILNo ratings yet
- Psychology 227 HW - 4 (1) ...Document6 pagesPsychology 227 HW - 4 (1) ...Brian ochiengNo ratings yet
- ECmed Eval SheetDocument1 pageECmed Eval SheetSalie GuarinoNo ratings yet
- Management of The Critically Ill PatientDocument36 pagesManagement of The Critically Ill PatientZhi Hao OoiNo ratings yet
- Diagnostic Report: FinalDocument2 pagesDiagnostic Report: FinalRAGHA DIAGNOSTIC CENTRENo ratings yet
- MSN I 20.4.2020 FN TyphoidDocument20 pagesMSN I 20.4.2020 FN TyphoidDr. DhaneshNo ratings yet
- Midterms Psyc LecDocument14 pagesMidterms Psyc LecMiden AlbanoNo ratings yet
- Head and Neck Cancer Awareness Exploratory Survey in Undergraduate StudentsDocument7 pagesHead and Neck Cancer Awareness Exploratory Survey in Undergraduate StudentsSteve GannabanNo ratings yet
- Blue Red LesionDocument14 pagesBlue Red LesionXara Barretto MagadiaNo ratings yet
- AbPsy Practice Exam 1Document15 pagesAbPsy Practice Exam 1janlyn espinosaNo ratings yet
- ALSANGEDY BULLETS FOR PACES Cluster Headache (2nd Edition)Document2 pagesALSANGEDY BULLETS FOR PACES Cluster Headache (2nd Edition)mrcp study notesNo ratings yet
- Cranial Nerve Disorders: Ernest E. WangDocument13 pagesCranial Nerve Disorders: Ernest E. Wangirsyad tsaniNo ratings yet
- Ir Jajad KaokabDocument13 pagesIr Jajad Kaokabdharsa plyNo ratings yet
- Lecture 5 Brachytherapy Implantation - 6-18 FinalDocument10 pagesLecture 5 Brachytherapy Implantation - 6-18 FinalArcrije JerezNo ratings yet
- Emergency NursingDocument15 pagesEmergency NursingAshley Ishika100% (1)
- GRTP Wallet Card FinalDocument2 pagesGRTP Wallet Card FinalIrish FroggyNo ratings yet
- Emilio Aguinaldo College: School of NursingDocument9 pagesEmilio Aguinaldo College: School of NursingPaullennium Chester MaganaNo ratings yet
- Makalah Temu 10 Bahasa InggrisDocument14 pagesMakalah Temu 10 Bahasa InggrisArhya DutaNo ratings yet