Professional Documents
Culture Documents
KDIGO 2022 Diabetes Guideline Quick Reference Guide
KDIGO 2022 Diabetes Guideline Quick Reference Guide
Uploaded by
Christian Risco QuezadaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
KDIGO 2022 Diabetes Guideline Quick Reference Guide
KDIGO 2022 Diabetes Guideline Quick Reference Guide
Uploaded by
Christian Risco QuezadaCopyright:
Available Formats
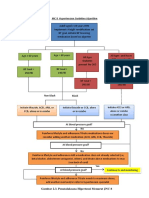
KDIGO DIABETES IN CKD: Chapter 1 Chapter 1 Chapter 1 Chapter 2
QUICK REFERENCE COMPREHENSIVE CARE IN COMPREHENSIVE CARE IN COMPREHENSIVE CARE IN GLYCEMIC MONITORING AND
GUIDE PATIENTS WITH DIABETES AND PATIENTS WITH DIABETES AND PATIENTS WITH DIABETES AND TARGETS IN PATIENTS WITH
CKD - RAS BLOCKADE CKD - SGLT2i CKD - MRA DIABETES AND CKD
This guide presents the recommendation statements from the
KDIGO 2022 Clinical Practice Guideline for Diabetes Management in
Chronic Kidney Disease KEY CONCEPTS KEY CONCEPTS KEY CONCEPTS KEY CONCEPTS
Chapter 1 → ACEi/ARB should be initiated in patients with diabetes, hypertension and → SGLT2i should be initiated in patients with T2D, CKD and eGFR ≥20 ml/ → A nonsteroidal mineralocorticoid receptor antagonist (ns-MRA), finerenone, → HbA1c, glycated hemoglobin, is recommended to monitor glycemic control in
albuminuria and titrated to the maximum tolerated dose. min/1.73 m2. Currently SGLT2i with approved indications for kidney and heart has demonstrated kidney and cardiovascular benefits for patients with T2D, patients with diabetes and CKD. Monitoring twice per year is reasonable and
COMPREHENSIVE CARE IN protection include canagliflozin, dapagliflozin, and empagliflozin. CKD and eGFR ≥25 ml/min/1.73 m2. Its use is suggested in those with normal can be as often as 4 times per year if glycemic target is not met or there is a
→ Monitor for changes in BP, serum creatinine and serum potassium within serum potassium concentration and presence of albuminuria (≥30 mg/g [≥3 change in glucose-lowering therapy.
PATIENTS WITH DIABETES AND 2-4 weeks of ACEi/ARB initiation or dose escalation since RAS blockade can → Once an SGLT2i is initiated, it is reasonable to continue an SGLT2i even if the mg/mmol]) despite maximum tolerated dose of RASi.
induce a transient decrease in the eGFR or a transient increase in serum eGFR falls below 20 ml/min per 1.73 m2, unless it is not tolerated or kidney → Precision and accuracy of HbA1c measurement declines with advanced CKD
CKD creatinine and/or potassium. replacement therapy is initiated. The use of SGLT2i in dialysis and transplant → An ns-MRA can be added to a RASi and an SGLT2i for treatment of T2D and (G4-G5) since inflammatory states and metabolic acidosis can bias towards
patients is currently unsupported. CKD. higher HbA1c while conditions such as anemia and transfusions that affect
→ Patients should be maintained on ACEi or ARB unless serum creatinine rises red blood cell survival or turnover can bias toward lower HbA1c.
KEY CONCEPTS by more than 30% within 4 weeks of initiation or dose escalation. Episodes → A modest drop in eGFR (≤30%) after SGLT2i administration should not prompt → Initiate finerenone at 10 mg for patients with eGFR <60 ml/min/1.73 m2 or
of hyperkalemia can often be effectively managed with various strategies discontinuation of therapy. If decrease is >30%, assess risk for hypovolemia 20 mg for patients with eGFR ≥60 ml/min/1.73 m2 and serum potassium → For individuals in whom HbA1c measurements are not concordant with
below before decreasing the dose or discontinuing RASi therapy. and consider decreasing diuretic dose. SGLT2i may be temporarily withheld ≤4.8 mmol/l. Monitor potassium at 1 month and every 4 months thereafter. directly measured blood glucose or clinical symptoms, continuous glucose
→ Patients with diabetes and CKD are at high risk of CKD progression and during surgery or critical illness. Continue with current dose if serum potassium is 4.9-5.5 mmol/l. If serum monitoring (CGM) can be used to index glycemia.
cardiovascular disease that requires a comprehensive strategy from a → Combined use of ACEi and ARB should be avoided. Similarly, the use of a potassium is >5.5 mmol/l, hold finerenone and adjust diet or medications.
multidisciplinary team of health care professionals. direct renin inhibitor with an ACEi or ARB should be avoided. Resume finerenone only when serum potassium is ≤5.0 mmol/l. → Self-monitoring of blood glucose (SMBG) or the use of CGM can help monitor
for episodes of hypoglycemia. For patients who wish to do neither, glucose-
→ Given the adverse fetal effects of ACEi/ARB, women who are considering PRACTICAL APPROACH TO INITIATING SGLT2i IN → Steroidal MRA can be used in patients with CKD and diabetes who also lowering therapies that pose lower hypoglycemic risks are preferred.
→ This approach should include a foundation of
lifestyle modification and self-management pregnancy or who are pregnant should discontinue the use of these therapies. PATIENTS WITH T2D AND CKD have heart failure, hyperaldosteronism, or refractory hypertension. However,
(maintenance of a healthy plant-based diet, steroidal MRA and ns-MRA should not be combined. If a patient has → HbA1c target ranging from <6.5% to <8.0% is appropriate for patients
proper protein and sodium intake, optimal indications for both but not treated with either, the most clinically pressing with diabetes and CKD (not on dialysis) and should be individualized
weight and exercise; absence of tobacco indication should drive the MRA selection. based on patient preferences, severity of CKD, presence of macrovascular
use), upon which are layered first-line drug complications or comorbidities, life expectancy, hypoglycemia burden, choice
therapies (metformin, SGLT2i, RASi, statins) of glucose-lowering agents, and availability of resources or support system.
according to clinical characteristics.
→ Additional drugs with proven kidney
and heart protection (GLP-1 RA,
ns-MRA, antiplatelets) as guided
by assessments of residual risk
are administered with further
interventions to control risk
factors (glycemia, hypertension,
dyslipidemia) if applicable.
WHAT THE GUIDELINE SAYS:
Recommendation 1.4.1: We suggest a nonsteroidal mineralocorticoid receptor
antagonist with proven kidney or cardiovascular benefit for patients with T2D,
WHAT THE GUIDELINE SAYS:
an eGFR ≥25 ml/min/1.73 m2, normal serum potassium concentration, and
WHAT THE GUIDELINE SAYS: WHAT THE GUIDELINE SAYS: albuminuria (≥30 mg/g [≥3 mg/mmol]) despite maximum tolerated dose of RAS Recommendation 2.1.1: We recommend using hemoglobin A1c (HbA1c) to monitor
inhibitor (RASi) (2A). glycemic control in patients with diabetes and CKD (1C).
Recommendation 1.2.1: We recommend that treatment with an angiotensin- Recommendation 1.3.1: We recommend treating patients with type 2 diabetes Recommendation 2.2.1: We recommend an individualized HbA1c target ranging from
converting enzyme inhibitor (ACEi) or an angiotensin II receptor blocker (ARB) (T2D), CKD, and an eGFR ≥20 ml/min per 1.73 m2 with an SGLT2i (1A). <6.5% to <8.0% in patients with diabetes and CKD not treated with dialysis (1C).
be initiated in patients with diabetes, hypertension, and albuminuria, and that
these medications be titrated to the highest approved dose that is tolerated
(1B).
Chapter 3 Chapter 4 Chapter 4 Chapter 5
2022 DIABETES IN CKD
LIFESTYLE INTERVENTIONS GLUCOSE-LOWERING THERAPIES GLUCOSE-LOWERING THERAPIES APPROACHES TO MANAGEMENT GUIDELINE HIGHLIGHTS
IN PATIENTS WITH DIABETES IN PATIENTS WITH T2D AND CKD IN PATIENTS WITH T2D AND CKD OF PATIENTS WITH DIABETES
AND CKD AND CKD Comprehensive care: Patients with diabetes and CKD have multisystem
disease that requires treatment including a foundation of lifestyle
intervention (healthy diet, exercise, weight management, no smoking) and
drug therapy that improves kidney and cardiovascular outcomes (glucose,
KEY CONCEPTS KEY CONCEPTS KEY CONCEPTS KEY CONCEPTS lipids, blood pressure).
Nutrition intake: Patients should consume a balanced, healthy diet that
→ Patients with diabetes and CKD should adopt a diet high in vegetables, → The treatment algorithm for selecting glucose-lowering therapies for → A long-acting GLP-1 RA is recommended for patients with T2D and CKD → A structured self-management education program is recommended for the is high in vegetables, fruits, whole grains, fiber, legumes, plant-based
fruits, whole grains, etc. and avoid a diet consisting of processed meats, patients with T2D and CKD includes lifestyle therapy, first-line therapy, and who have not achieved glycemic targets despite the use of metformin and care of people with diabetes and CKD, with considerations paid to local proteins, unsaturated fats, and nuts; and lower in processed meats, refined
refined carbohydrates and sweetened beverages. additional drug therapy as needed for glycemic control. SGLT2i. The choice of GLP-1 RA should be guided by agents with documented context, cultures, and availability of resources. carbohydrates, and sweetened beverages. Sodium (<2 g/day) and protein
→ It is suggested that patients with diabetes and CKD not on dialysis maintain cardiovascular benefits (i.e., liraglutide, semaglutide [injectable] and intake (0.8 g/kg/day) in accordance with recommendations for the general
→ Key objectives of effective diabetes self-management education programs include:
a protein intake of 0.8 g/kg (weight)/day while those on dialysis can consume dulaglutide). Listing of available GLP-1 RA is provided below. population should be followed.
between 1.0-1.2 g/kg (weight)/day. → GLP-1 RA should not be combined with DPP-4 (dipeptidyl peptidase-4) inhibitors. SGLT2i: should be initiated for patients with T2D and CKD when eGFR is
→ It is suggested that patients with diabetes and CKD consume <2 g (<90 ≥20 ml/min/1.73 m2 and can be continued after initiation at lower levels of
→ GLP-1 RA has shown to promote intentional weight loss and may be useful in
mmol) sodium/day, which is equivalent to 5 g of salt (NaCl)/day. eGFR. SGLT2i markedly reduce risks of CKD progression, heart failure, and
patients with obesity, T2D and CKD.
atherosclerotic cardiovascular diseases, even when blood glucose is already
→ Patients with diabetes and CKD are advised to perform moderate-intensity controlled.
physical activity for a duration of at least 150 minutes per week. Exercise
intensity should be tailored for those who are frail or are at risk for falls. Metformin: Metformin should be used for patients with T2D and CKD
when eGFR is ≥30 ml/min/1.73 m2. For such patients, metformin is a safe,
→ Sedentary behavior should be avoided and patients with obesity, diabetes effective, and inexpensive drug to control blood glucose and reduce diabetes
and CKD with eGFR ≥30 ml/min/1.73 m2 are encouraged to lose weight. complications.
→ Metformin should be initiated in patients with T2D, CKD and eGFR ≥30 ml/
→ Patients with diabetes and CKD should avoid consumption of tobacco Glycemic monitoring and targets: HbA1c should be measured regularly.
min/1.73 m2. Most patients would also benefit from concomitant use of
products. Reliability decreases with advanced CKD, particularly for patients treated
SGLT2i . Increase monitoring when eGFR <60 ml/min/1.73 m2 and consider
adjusting dose as needed. When eGFR declines to 30-44 ml/min/1.73 m2, → Self-management education programs should be operated within a with dialysis, and results should be interpreted with caution. CGM or
maximum dose should be halved. Metformin should be discontinued when framework of team-based integrated care promoted by policy-makers and SMBG may also be useful, especially for treatment associated with risk of
eGFR <30 ml/min/1.73 m2. Vitamin B12 deficiency should be monitored in institutional decision-makers that focuses on risk evaluation and patient hypoglycemia. Targets for glycemic control should be individualized, ranging
SUGGESTED APPROACH TO ADDRESS PHYSICAL
those on metformin for more than 4 years. empowerment as part of patients’ comprehensive care. from <6.5% to <8.0%.
INACTIVITY AND SEDENTARY BEHAVIOR
→ Effective team-based integrated care should be supported and delivered by GLP-1 RA: In patients with T2D and CKD who have not achieved individualized
physicians and other allied health professionals such as trained nurses, dieticians, glycemic targets despite use of metformin and SGLT2i, or who are unable to
pharmacists, healthcare assistants, community workers and peer supporters. use those medications, a long-acting GLP-1 RA is recommended as part of
the treatment.
→ If patients still do not meet glycemic targets after lifestyle therapy, RAS blockade: Patients with T1D or T2D, hypertension, and albuminuria
metformin and SGLT2i, GLP-1 RA are generally preferred. Other classes of (persistent ACR ≥30 mg/g [≥3 mg/mmol] should be treated with a RAS
medications can be considered based on patient factors and preferences below: inhibitor (ACEi or ARB), titrated to the maximum approved or highest
tolerated dose. Serum potassium and creatinine should be monitored.
Nonsteroidal mineralocorticoid receptor antagonists (ns-MRA): ns-MRA
reduce risks of CKD progression and cardiovascular events for people with
T2D and residual albuminuria. They are suggested for patients with T2D,
urine ACR ≥30 mg/g [≥3 mg/mmol] and normal serum potassium on other
standard-of-care therapies. Serum potassium and creatinine should be
Starting monitored.
dose
Approaches to management: A team-based and integrated approach to
manage these patients should focus on regular assessment, control of
multiple risk factors, and structured education in self-management to
protect kidney function and reduce risk of complications.
WHAT THE GUIDELINE SAYS:
For more information, please consult:
KDIGO 2022 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease.
Recommendation 1.5.1: We recommend advising patients with diabetes and Monitor
Kidney Int. 2022; 102(5S):S1–S127.
vitamin B12
CKD who use tobacco to quit using tobacco products (1D).
Recommendation 3.1.1: We suggest maintaining a protein intake of 0.8 g protein/ KDIGO Clinical Practice Guidelines are based upon the best information available at the
kg (weight)/d for those with diabetes and CKD not treated with dialysis (2C). Monitor kidney time of publication. This Guideline is designed to provide information and assist decision-
function making. It is not intended to define a standard of care and should not be interpreted as
Recommendation 3.1.2: We suggest that sodium intake be <2 g of sodium per WHAT THE GUIDELINE SAYS: prescribing an exclusive course of management. Variations in practice will inevitably and
day (or <90 mmol of sodium per day, or <5 g of sodium chloride per day) in appropriately occur when clinicians consider the needs of individual patients, available
patients with diabetes and CKD (2C). WHAT THE GUIDELINE SAYS: resources, and limitations unique to an institution or type of practice. Every healthcare
Recommendation 5.1.1: We recommend that a structured self-management professional making use of these recommendations is responsible for evaluating the
Recommendation 3.2.1: We recommend that patients with diabetes and CKD appropriateness of applying them in the setting of any particular clinical situation.
educational program be implemented for care of people with diabetes and CKD (1C).
be advised to undertake moderate-intensity physical activity for a cumulative Recommendation 4.1.1: We recommend treating patients with T2D, CKD, and an eGFR ≥30
This Quick Reference guide was sponsored by the
duration of at least 150 minutes per week, or to a level compatible with their ml/min per 1.73 m2 with metformin (1B). Recommendation 5.2.1: We suggest that policymakers and institutional
Dose Boehringer Ingelheim & Lilly Alliance. KDIGO is solely
cardiovascular and physical tolerance (1D). adjustment Recommendation 4.2.1: In patients with T2D and CKD who have not achieved decision-makers implement team-based, integrated care focused on risk responsible for the content of this Guide.
individualized glycemic targets despite use of metformin and SGLT2i treatment, or who evaluation and patient empowerment to provide comprehensive care in
are unable to use those medications, we recommend a long-acting GLP-1 RA (1B). patients with diabetes and CKD (2B).
You might also like
- Practical Guide To Laboratory Test Interpretation and Differential Diagnosis. Haematology and BiochemistryDocument212 pagesPractical Guide To Laboratory Test Interpretation and Differential Diagnosis. Haematology and BiochemistryAgrovet Don Bosco100% (1)
- Digoxin: Andy Samelson's Drug Cards Andy Samelson's Drug CardsDocument57 pagesDigoxin: Andy Samelson's Drug Cards Andy Samelson's Drug Cardssplendidfender76% (17)
- Case StudyDocument35 pagesCase StudysamanNo ratings yet
- The Pocketbook For PHYSIOTHERAPISTS 2nd Gitesh Amrohit Masud PDFDocument408 pagesThe Pocketbook For PHYSIOTHERAPISTS 2nd Gitesh Amrohit Masud PDFemil100% (1)
- MILVvv 1Document6 pagesMILVvv 1garywall.ukNo ratings yet
- 2019 Diabetic Neuropathy Pontianak PesertaDocument38 pages2019 Diabetic Neuropathy Pontianak Pesertaagung nurcahyoNo ratings yet
- Reno Cardio Protection With Canagliflozin - Endo PerspectiveDocument33 pagesReno Cardio Protection With Canagliflozin - Endo PerspectivedrsantoshkalelearningNo ratings yet
- Jardiance NDRDocument8 pagesJardiance NDRapi-665345625No ratings yet
- PMC4020327-jdi 12214Document11 pagesPMC4020327-jdi 12214anca irinaNo ratings yet
- QuotesDocument41 pagesQuotesTrishenth FonsekaNo ratings yet
- Mounjaro MonographDocument13 pagesMounjaro Monographlu161513No ratings yet
- Diabetic Kidney Disease (DKD)Document39 pagesDiabetic Kidney Disease (DKD)monpyitharNo ratings yet
- ABCD Position On Cardiovascular Impact of Glucose-Lowering Drugs - Independent Professional Body Guideline - GuidelinesDocument6 pagesABCD Position On Cardiovascular Impact of Glucose-Lowering Drugs - Independent Professional Body Guideline - GuidelinesAna MariaNo ratings yet
- Type 2 Diabetes Chronic Kidney Disease: Use of Dipeptidyl Peptidase-4 Inhibitors in Patients WithDocument8 pagesType 2 Diabetes Chronic Kidney Disease: Use of Dipeptidyl Peptidase-4 Inhibitors in Patients WithRahmanu ReztaputraNo ratings yet
- Sec2 Clinical2 (CKD + Answers)Document82 pagesSec2 Clinical2 (CKD + Answers)ahmedmohamed01153159469No ratings yet
- Best Practice For Diabetic Patients On Hemodialysis 2012 (TAD19-S1)Document27 pagesBest Practice For Diabetic Patients On Hemodialysis 2012 (TAD19-S1)Anonymous uuP28GXyNo ratings yet
- Simpo 3 - Dr. Bowo SP - pd-kEMD - How TPatients With Co-Formulation InsulinDocument35 pagesSimpo 3 - Dr. Bowo SP - pd-kEMD - How TPatients With Co-Formulation InsulinAgnes Irene ZagotoNo ratings yet
- Diabetic Kidney Disease New Clinical and Therapeutic Issues Joint Position StatementDocument4 pagesDiabetic Kidney Disease New Clinical and Therapeutic Issues Joint Position StatementSiddiq MohammedNo ratings yet
- Vyldagliptin + Dapagliflozin + Metformin Combination in Treatment of T2DMDocument37 pagesVyldagliptin + Dapagliflozin + Metformin Combination in Treatment of T2DMAditya GautamNo ratings yet
- SGLT 2Document11 pagesSGLT 2Macarena SainzNo ratings yet
- BMJDRC 2023 003666Document6 pagesBMJDRC 2023 003666josimarNo ratings yet
- Dermody Grand Rounds May 2023 Circle City Submission - FinalDocument55 pagesDermody Grand Rounds May 2023 Circle City Submission - Finalapi-668510785No ratings yet
- COvID Front Door v1.0Document3 pagesCOvID Front Door v1.0Florin StanciuNo ratings yet
- Prescribing SGLT2 Inhibitors in Patients With CKD Expanding Indications and Practical ConsiderationsDocument14 pagesPrescribing SGLT2 Inhibitors in Patients With CKD Expanding Indications and Practical ConsiderationsJorge Alejandro SañudoNo ratings yet
- DM in CKD Core Curriculum 2022Document9 pagesDM in CKD Core Curriculum 2022Di KlauNo ratings yet
- Chronic Kidney Disease: Table 74-1Document14 pagesChronic Kidney Disease: Table 74-1Ren PastelNo ratings yet
- Chapter 3 Management of Progression and Compl 2013 Kidney International SupDocument18 pagesChapter 3 Management of Progression and Compl 2013 Kidney International SupwardaninurindahNo ratings yet
- CKD Kdigo 2012Document27 pagesCKD Kdigo 2012giggs_libraNo ratings yet
- 2 Modern Sulfonylureas - A Balanced Perspective - 15!09!2022Document30 pages2 Modern Sulfonylureas - A Balanced Perspective - 15!09!2022Lalrin ChhanaNo ratings yet
- Glycaemic Control and Blood Glucose Lowering AgentDocument23 pagesGlycaemic Control and Blood Glucose Lowering AgentIrsa SevenfoldismNo ratings yet
- NENC Regional SGLT2 Top Tips v1.2 NTAG Approved March 2023Document5 pagesNENC Regional SGLT2 Top Tips v1.2 NTAG Approved March 2023Nehal ElnagarNo ratings yet
- Abridged Standards of Care 2021: 7. Diabetes TechnologyDocument1 pageAbridged Standards of Care 2021: 7. Diabetes TechnologyShefira TashaNo ratings yet
- JAPI0078 p74-82Document9 pagesJAPI0078 p74-82ShefaNo ratings yet
- Euglycemic Diabetic KetoacidosisDocument4 pagesEuglycemic Diabetic KetoacidosisThao LamNo ratings yet
- Diabetes in CKDDocument20 pagesDiabetes in CKDdr_iswahyudhiNo ratings yet
- Palmer 1993Document34 pagesPalmer 1993Hindun MaritaNo ratings yet
- Cme PresentationDocument56 pagesCme Presentationapi-439712011No ratings yet
- SGLTi - OrthostaticDocument8 pagesSGLTi - OrthostaticdipanNo ratings yet
- Chronic Kidney Disease: PathophysiologyDocument19 pagesChronic Kidney Disease: PathophysiologyAnastasia Gaudensia Wewe WNo ratings yet
- Skugor TreatmentofdiabetesmellitusDocument5 pagesSkugor TreatmentofdiabetesmellitusyomiboyNo ratings yet
- An Overview of DapagliflozinDocument4 pagesAn Overview of DapagliflozinInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Chronic Kidney Disease:: The Canary in The Coal MineDocument13 pagesChronic Kidney Disease:: The Canary in The Coal MinedhearawrsNo ratings yet
- HTTPSWWW - Moh.gov - mymohresourcesPenerbitanCPGEndocrineQR T2DM 6th Edition QR Guide Digital PDFDocument8 pagesHTTPSWWW - Moh.gov - mymohresourcesPenerbitanCPGEndocrineQR T2DM 6th Edition QR Guide Digital PDFFiqa KusrinNo ratings yet
- Jdi 13126Document9 pagesJdi 13126Nirmal AliNo ratings yet
- Ajhp 140168Document12 pagesAjhp 140168cherrygems99No ratings yet
- Co-Formulations As The First Injectable in Type 2 Diabetes A Review of Efficacy, Safety, and Implications in Clinical PracticeDocument13 pagesCo-Formulations As The First Injectable in Type 2 Diabetes A Review of Efficacy, Safety, and Implications in Clinical PracticeRIKANo ratings yet
- Oral Antidiabetics in Specific ConditionsDocument3 pagesOral Antidiabetics in Specific Conditionsbelahan jiwaNo ratings yet
- VildagliptinDocument7 pagesVildagliptinwanburyNo ratings yet
- The Emerging Pillars of Chronic Kidney Disease No Longer A Bystander in Metabolic MedicinDocument5 pagesThe Emerging Pillars of Chronic Kidney Disease No Longer A Bystander in Metabolic MedicinAlfredo CruzNo ratings yet
- The Kaohsiung J of Med Scie - 2024 - Chong - Recent Advances in The Treatment of Type 2 Diabetes Mellitus Using New DrugDocument9 pagesThe Kaohsiung J of Med Scie - 2024 - Chong - Recent Advances in The Treatment of Type 2 Diabetes Mellitus Using New DrugAnanda SalmaNo ratings yet
- WJD 12 514Document11 pagesWJD 12 514josimarNo ratings yet
- Chap128 Terapi GNA PDFDocument4 pagesChap128 Terapi GNA PDFnovaNo ratings yet
- Screenshot 2023-03-17 at 12.37.03 AMDocument1 pageScreenshot 2023-03-17 at 12.37.03 AMRenad AlharbiNo ratings yet
- ADS ADEA ANZCA NZSSD - DKA - SGLT2i - Alert - Ver July 2022Document3 pagesADS ADEA ANZCA NZSSD - DKA - SGLT2i - Alert - Ver July 2022tom.condon.02No ratings yet
- Diabetes Type 2 Treatment AlgorithmDocument26 pagesDiabetes Type 2 Treatment AlgorithmLokesh KhuranaNo ratings yet
- Guidelines For The Management of Diabetic Ketoacidosis (DKA) in AdultsDocument21 pagesGuidelines For The Management of Diabetic Ketoacidosis (DKA) in AdultsCristina BadarauNo ratings yet
- Penanganan Diabetes Pada Pasien DM Selama Menjalani Puasa Dibulan Suci RamadhanDocument28 pagesPenanganan Diabetes Pada Pasien DM Selama Menjalani Puasa Dibulan Suci Ramadhanidham shadiqNo ratings yet
- Diabetes Type 2 PharmacotherapyDocument37 pagesDiabetes Type 2 Pharmacotherapyali khanNo ratings yet
- 2020 - Diabetes PharmacotherapyDocument68 pages2020 - Diabetes PharmacotherapyAmal HijaziNo ratings yet
- Chronic Kidney Disease: For The Primary Care PhysicianDocument54 pagesChronic Kidney Disease: For The Primary Care PhysicianFlavia PolodeanuNo ratings yet
- Diabetic Kidney Disease - DynaMedDocument117 pagesDiabetic Kidney Disease - DynaMedElisa ChinchillaNo ratings yet
- Gliclazide MR, An Efficacy and Safety: For T2DM Patients During RamadanDocument28 pagesGliclazide MR, An Efficacy and Safety: For T2DM Patients During RamadanLeonora KomboyNo ratings yet
- Comparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic PatientsDocument5 pagesComparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic Patientsthomas albertNo ratings yet
- Mayo Clinic HypertensionDocument13 pagesMayo Clinic HypertensionshanuddinNo ratings yet
- DrugsDocument7 pagesDrugsEloisa Abarintos RacalNo ratings yet
- Drug of Today.1998.full PDFDocument956 pagesDrug of Today.1998.full PDFCesar CeNo ratings yet
- 2016 ESC Guidelines For The Diagnosis and Treatment of Acute and Chronic Heart FailureDocument85 pages2016 ESC Guidelines For The Diagnosis and Treatment of Acute and Chronic Heart FailureaaronNo ratings yet
- Gestational Hypertension Medical TherapyDocument9 pagesGestational Hypertension Medical TherapydedeNo ratings yet
- Algoritma Tatalaksana HTDocument2 pagesAlgoritma Tatalaksana HTUswatun Hasanah RINo ratings yet
- Hyperkalemia: Dr. K. K. Gupta Associate Prof. Department of Medicine, KgmuDocument23 pagesHyperkalemia: Dr. K. K. Gupta Associate Prof. Department of Medicine, KgmuPrass Ekasetia PoetraNo ratings yet
- Lisinopril VS Ramipril in CoughDocument8 pagesLisinopril VS Ramipril in CoughFreidlander PangestuNo ratings yet
- Diuretics and Drugs Affecting Renal Function, Water, and Electrolyte MetabolismDocument4 pagesDiuretics and Drugs Affecting Renal Function, Water, and Electrolyte MetabolismWaqar HassanNo ratings yet
- Congestive Heart Failure: Dr. J. SaravananDocument31 pagesCongestive Heart Failure: Dr. J. Saravananpetervazhayil100% (1)
- New Scoring System APACHE HF For PredictDocument9 pagesNew Scoring System APACHE HF For PredictAdi PriyatnaNo ratings yet
- Pharmacological and Pharmaceutical Profile of Valsartan: A ReviewDocument8 pagesPharmacological and Pharmaceutical Profile of Valsartan: A ReviewRatna HarefaNo ratings yet
- Heart Failure PharmacyDocument47 pagesHeart Failure PharmacyKhashayar MastooriNo ratings yet
- West Bengal - Hypertension ProtocolDocument1 pageWest Bengal - Hypertension ProtocolDebanjan Basak100% (1)
- Terapi Farmakologi Gagal Jantung - Sept - 2020Document58 pagesTerapi Farmakologi Gagal Jantung - Sept - 2020FAUZAN ILHAM PRATAMANo ratings yet
- Hypertensi S2PDFDocument69 pagesHypertensi S2PDFrisma sakti pNo ratings yet
- New Drug HypertensionDocument23 pagesNew Drug Hypertensiondwi kartikasariNo ratings yet
- Pharmacotherapeutics PDFDocument30 pagesPharmacotherapeutics PDFprazol shresthaNo ratings yet
- Pharmacological and Pharmaceutical Profile of Valsartan: A ReviewDocument8 pagesPharmacological and Pharmaceutical Profile of Valsartan: A ReviewWisnu Dwi AntaraNo ratings yet
- Ehy340 PDFDocument83 pagesEhy340 PDFghufran adnanNo ratings yet
- Hipertensi KebidananDocument77 pagesHipertensi KebidananNINING ALKOMAHNo ratings yet
- 2022 AHA/ACC/HFSA Guideline For The Management of Heart Failure: Executive SummaryDocument24 pages2022 AHA/ACC/HFSA Guideline For The Management of Heart Failure: Executive SummaryAna RuizNo ratings yet
- HypertensionDocument53 pagesHypertensionKate Lynne CamonayanNo ratings yet
- Side Effects of Drugs - Annual 33 - J. Aronson (Elsevier, 2011) WWDocument1,122 pagesSide Effects of Drugs - Annual 33 - J. Aronson (Elsevier, 2011) WWAndrei E. HawayNo ratings yet
- Guias Hipertension 2023 Esc BDocument14 pagesGuias Hipertension 2023 Esc Bmiguel contrerasNo ratings yet
- Amaryl M PI - May 2018marylDocument11 pagesAmaryl M PI - May 2018marylvicky upretiNo ratings yet