Professional Documents
Culture Documents
Metabolic Alkalosis
Metabolic Alkalosis
Uploaded by
Menna ElesawyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Metabolic Alkalosis
Metabolic Alkalosis
Uploaded by
Menna ElesawyCopyright:
Available Formats
Metabolic alkalosis
Pathophysiology
• Metabolic alkalosis is a simple acid-base disorder that presents as alkalemia
(increased arterial pH) with an increase in plasma bicarbonate.
• It is an extremely common entity in hospitalized patients.
• Under normal circumstances, the kidney is readily able to excrete an alkali load.
Thus, evaluation of patients with metabolic alkalosis must consider two separate
issues:
o Initial process that generates the metabolic alkalosis; and
o Alterations in renal function that maintain the alkalemic state.
• The organ systems involved in metabolic alkalosis are mainly the kidneys and GI
tract.
• The pathogenesis involves two processes:
o Generation of metabolic alkalosis and
o Maintenance of metabolic alkalosis, which usually overlap.
Generation of metabolic alkalosis
Metabolic alkalosis may be generated by one of the following mechanisms:
A. Loss of Hydrogen ions:
• Gastrointestinal Loss of Hydrogen
o Stomach fluids are highly acidic at a pH of approximately 1.5 to
3.5. Hydrogen secretion is accomplished via parietal cells in the gastric
mucosa.
o Therefore, the large volume loss of gastric secretions will correlate as a loss
of hydrogen chloride, an acidic substance, leading to a relative increase in
bicarbonate in the blood, thus driving alkalosis.
o Losses can occur pathologically via vomitus or nasogastric suctioning.
o Most marked with vomiting due to pyloric stenosis or obstruction or bulimia
nervosa because the vomitus is acidic gastric juice only.
• Renal Loss of Hydrogen
o Hydrogen is used within the kidneys are an antiporter energy gradient to
retain a multitude of other elements.
o Of interest here, sodium is reabsorbed through an exchange for hydrogen in
the renal collecting ducts under the influence of aldosterone.
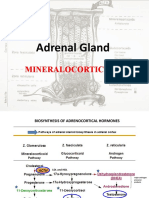
o Therefore, pathologies that increase the levels of mineralocorticoids or
increase the effect of aldosterone, such as Conn’s syndrome will lead to
hypernatremia, hypokalemia, and hydrogen loss in the urine.
1 Dr. Hisham A. Nematalla
o Loop and thiazide diuretics can induce secondary hyperaldosteronism by
increasing sodium and fluid load to the distal nephron, which encourages
the renin-angiotensin-aldosterone system.
o Collecting duct hydrogen ion secretion is stimulated directly by the
increased luminal flow rate and sodium delivery, and indirectly by
intravascular volume contraction, which results in secondary
hyperaldosteronism.
Figure 1: Generation & Maintenance of Metabolic Alkalosis by Diuretics
o In Bartter’s and Gitelman’s syndromes, defects in sodium transport in
the loop of Henle (Bartter’s) or distal convoluted tubule (Gitelman’s) lead
to hypokalemia, secondary hyperaldosteronism, and metabolic alkalosis.
o In Liddle’s syndrome, enhanced sodium reabsorption by the cortical
collecting duct epithelial sodium channel results in a syndrome of
pseudohyperaldosteronism.
o Administration of high doses of penicillins (e.g., ticarcillin) can produce
metabolic alkalosis because they act as non-reabsorbable anions. High
concentrations of poorly reabsorbable anions in the distal renal tubule
increase luminal flow rate and luminal electronegativity, which
enhances the secretion of potassium and hydrogen ion and results in
hypokalemia and metabolic alkalosis.
2 Dr. Hisham A. Nematalla
B. Intracellular Shift of Hydrogen
• Anytime that hydrogen ions are shifted intracellularly, this imbalance in the
buffer system has a relative increase in bicarbonate. Processes that drive
hydrogen intracellularly include hypokalemia.
C. Retention/Addition of Bicarbonate
• The simplest of which is an overdose of exogenous sodium bicarbonate in a
medical setting: (e.g. iv NaHCO3 infusion, citrate in transfused blood) or from
the infusion of organic anions that are metabolized to bicarbonate, such as
acetate, lactate, and citrate or from an endogenous source (e.g. metabolism of
ketoanions to produce bicarbonate).
• Milk-alkali syndrome is a pathology where the patient consumes excessive
quantities of oral calcium antacids, which leads to hypercalcemia and varying
degrees of renal failure. Additionally, since antacids are neutralizing agents,
they add alkaline substances to the body while reducing acid levels thus
increasing pH.
• Post-hypercapnic metabolic alkalosis
▪ When a patient hypoventilates, CO2 retention occurs in the lungs and
subsequently reduces pH. Over time, the renal system compensates by
retaining bicarbonate to balance pH. This is a slower process. Once the
hypoventilation is corrected, such as with a ventilator-assisted respiratory
failure patient, CO2 levels will quickly decrease, but bicarbonate levels will
lag in reducing.
▪ This causes post-hypercapnia metabolic alkalosis, which is self-correcting.
It is possible to calculate the expected pCO2 in the setting of metabolic
alkalosis to determine if it is a compensatory increase in bicarbonate, or if
there is an underlying pathology driving alkalosis using the following
equation:
▪ Expected pCO2 = 0.7 (HCO3-) + 20 mmHg ± 5.
▪ If the expected pCO2 does not match the measured value, an underlying
metabolic alkalosis is a likely present.
D. Contraction Alkalosis
• This phenomenon occurs when a large volume of sodium-rich, bicarbonate low
fluid is lost from the body.
• This occurs with diuretic use, cystic fibrosis, congenital chloride diarrhea,
among others. The net concentration of bicarbonate increases as a result.
3 Dr. Hisham A. Nematalla
Maintenance of Metabolic Alkalosis
• As long as renal function is maintained, excess bicarbonate is excreted in the urine
fairly rapidly.
• Metabolic alkalosis is predominantly maintained because of an abnormality in
renal function.
• Normally, the kidneys are capable of excreting all the excess bicarbonate presented
to them, even during periods of increased bicarbonate loads.
• As the serum bicarbonate concentration increases, the filtered bicarbonate load
exceeds the maximal rate for bicarbonate reabsorption, and the excess bicarbonate
is excreted in the urine. Under normal circumstances, the excess bicarbonate is
rapidly excreted, and metabolic alkalosis does not occur or is corrected in a matter
of hours.
As a result, metabolic alkalosis will persevere if the ability to eliminate bicarbonate is
impaired due to one of the following causes:
1. Hypovolemia, reduced effective arterial blood volume:
2. Hypokalemia,
3. Hypochloremia
4. Reduced glomerular filtration rate, and/or hyperaldosteronism.
4 Dr. Hisham A. Nematalla
Figure 2: Proximal tubular enhanced Na+ & HCO3- reabsorption
1. Hypovolemia:
• Intravascular volume depletion maintains metabolic alkalosis through several
mechanisms. Decreases in the glomerular filtration rate reduce the filtered
load of bicarbonate at any given serum concentration, thereby decreasing the
kidney’s ability to excrete a bicarbonate load.
• Effective arterial blood volume (EABV) refers to the adequacy of the arterial
blood volume to "fill" the capacity of the arterial vasculature.
• EABV can be reduced, therefore, by factors which reduce actual arterial blood
volume (hemorrhage, dehydration), increase arterial vascular capacitance
(cirrhosis, sepsis) or reduce cardiac output (congestive heart failure).
• Decreased EABV enhances proximal and distal tubular sodium
reabsorption.
• Sodium reabsorption must be coupled with reabsorption of an anion, such as
chloride or bicarbonate, or exchange with a cation, such as potassium or
hydrogen, to maintain charge neutrality.
• In the proximal tubule, increased sodium reabsorption stimulates bicarbonate
reabsorption.
• In the distal nephron, enhanced sodium reabsorption, particularly in the
setting of hypokalemia, stimulates hydrogen ion secretion.
• Most processes that result in a primary metabolic alkalosis also cause fluid loss,
producing a hypovolemia.
5 Dr. Hisham A. Nematalla
• Hypovolemia will stimulate the renin-angiotensin-aldosterone system.
• Angiotensin II promotes hydrogen excretion and bicarbonate retention by
stimulating sodium absorption (with filtered bicarbonate) in the proximal tubule
(by stimulating the luminal sodium/hydrogen antiporter and basolateral
sodium/bicarbonate transporter).
• Aldosterone secretion also promotes renal HCO3– resorption and acid excretion
(H+ loss), since aldosterone promotes the activity of the sodium transporter in
principal cells (absorbs sodium, creating a lumen negative potential, which
facilitates hydrogen excretion in the cortical collecting tubule), V-H+-ATPases
(which excrete hydrogen into the renal tubular lumen)
2. Hypochloremia
• In order for pendrin to secrete bicarbonate, chloride must be reabsorbed.
Thus, sufficient distal tubule chloride delivery is critical for bicarbonate
secretion.
• However, chloride depletion decreases distal chloride delivery, and this
reduces pendrin-mediated bicarbonate secretion (and chloride
reabsorption), thereby “maintaining” metabolic alkalosis.
• The main causes of chloride deficiency metabolic alkalosis, include
urinary salt wasting, excessive loss of salt in the sweat, intestinal chloride
wasting, poor dietary chloride intake & vomiting or sequestration of HCl.
• In the PCT, sodium will be passively resorbed with filtered bicarbonate
(which is in excess in blood and the glomerular filtrate) rather than chloride,
which is depleted.
• Due to chloride depletion, more sodium is delivered to the distal nephron
because less is being absorbed in the loop of Henle, which requires 2x
chloride through the Na-K-2Cl carrier, and early distal tubule (NaCl
transporter).
• Increased sodium delivery to the distal nephron will stimulate the Na
transporter in the distal nephron (which is stimulated by aldosterone and
the increased flow rate due to the excess sodium).
6 Dr. Hisham A. Nematalla
• This transporter absorbs the sodium in exchange for hydrogen (by
stimulating the H+-ATPase in type A intercalated cells) or potassium, via
potassium channels (which, if depleted, promotes aciduria in alkalosis, the
very last thing you want to be happening).
• Decreased filtered chloride is a major stimulus for aldosterone secretion,
because less NaCl is absorbed in the macula densa (reduced salt sensing).
• Aldosterone enhances sodium absorption in the collecting tubules by
stimulating the Na transporter in principal cells at a time when more
sodium is being delivered anyway because of decreased activity of the Na-
K-2Cl and NaCl carriers in the loop of Henle and early distal tubules,
respectively.
• Sodium exchanges for hydrogen, in cortical collecting tubular cells that
have sodium dependent H+-ATPases, and potassium (H+/K+ transporters).
• If potassium is deficient, hydrogen moves out into the lumen instead,
thus increasing renal acid excretion and, HCO3– retention.
• Aldosterone also directly promotes hydrogen excretion via stimulating the
H+-ATPases in the collecting tubules.
• Thus, the best treatment for a chloride-depleted metabolic alkalosis is to
administer chloride as hypertonic NaCl, with supplemental potassium.
• This restores circulating volume (decreasing stimuli for angiotensin II and
aldosterone secretion), provides sodium (so less is absorbed in the
proximal tubules with bicarbonate, allowing the bicarbonate to be filtered)
and provides Cl–, allowing sodium to be resorbed with chloride in the
distal parts of the proximal tubules and the loop of Henle, decreasing distal
sodium delivery, and removing the stimulus for aldosterone secretion
and acid excretion.
7 Dr. Hisham A. Nematalla
• Thus, NaCl is called an “acidifying solution”. Even though not acidic, it
promotes renal hydrogen retention and bicarbonate excretion (thus, it
has an acidifying effect via the kidney).
3. Hypokalemia:
• Potassium is often lost in fluids concurrently with H+ and Cl–. Potassium is low
because it has moved intracellularly in exchange for hydrogen in alkalemic
states.
• Potassium depletion is considered a critical element in sustaining a metabolic
alkalosis.
• A low potassium will exacerbate hypovolemia (inhibits the action of ADH
preventing water from being fully absorbed) and decreases GFR (reducing the
amount of bicarbonate being filtered).
• Low potassium promotes bicarbonate resorption by stimulating the NBC
pump which transports bicarbonate out of the basolateral surface of renal
tubular cells back into blood in the proximal tubule and stimulates renal
ammoniagenesis in the proximal tubules (promoting ammonium chloride or
acid excretion while retaining bicarbonate).
• Low potassium increases sodium delivery to the distal nephron by
decreasing activity of the Na-K-2Cl carrier in the loop of Henle.
• The extra sodium delivered to the distal tubule is resorbed in exchange for
H+ because K+ is low.
• In addition, the sodium absorption drives additional potassium excretion (even
if deficient) by creating a negative lumen potential (just as it drives hydrogen
excretion in cortical collecting tubule cells).
• Since aldosterone is high, sodium is being resorbed in the collecting tubules,
but the low potassium causes hydrogen to move out instead of potassium.
8 Dr. Hisham A. Nematalla
• Thus, a low K+ will potentiate an alkalosis by promoting renal acid excretion
(and bicarbonate retention) in several ways.
Paradoxical Aciduria in Metabolic Alkalosis
Figure 3: These factors result in a paradoxical aciduria.
Vomit-induced Metabolic Alkalosis
9 Dr. Hisham A. Nematalla
Differential Diagnosis of Metabolic Alkalosis
Etiology of metabolic alkalosis
10 Dr. Hisham A. Nematalla
Pathways leading to metabolic alkalosis:
Maintenance factors for metabolic alkalosis
11 Dr. Hisham A. Nematalla
Maintenance factors for metabolic alkalosis: volume contraction
Maintenance factors for metabolic alkalosis: Dyselectrolytemia
12 Dr. Hisham A. Nematalla
Compensation
• The respiratory response to metabolic alkalosis is hypoventilation, which results in
an increased PaCO2.
• Respiratory compensation is initiated within hours when the central and peripheral
chemoreceptors sense an increase in pH.
• The PaCO2 increases 6 to 7 mm Hg for each 10-mEq/L (10 mmol/L) increase in
bicarbonate, up to a PaCO2 of approximately 50 to 60 mm Hg before hypoxia
sensors react to prevent further hypoventilation.
Metabolic alkalosis
• pCO2 increases by 0.6 mmHg for every mmol/l that HCO3- is above 24 mmol/l
within 1-1.5 days (Limit of Compensation pCO2 55-60) mmHg.
Metabolic alkalosis
• pH >7.42 and [HCO3−] >26 mmol per liter
Secondary (respiratory) response:
• PaCO2 = 0.7 × ([HCO3−]-24) + 40±2 mmHg. or
• [HCO3−] + 15 mmHg. or
• 0.7 × [HCO3−] + 20 mmHg
• Complete secondary adaptive response within 24–36 hr.
• Superimposed respiratory acidosis or alkalosis may be diagnosed if the calculated
PaCO2 is greater or less than predicted.
13 Dr. Hisham A. Nematalla
Clinical Presentation
• There are no unique signs or symptoms associated with mild to moderate metabolic
alkalosis, but patients may complain of symptoms related to the underlying cause
of the disorder:
• (e.g., muscle weakness with hypokalemia or postural dizziness with volume
depletion).
• history of vomiting, gastric drainage, or diuretic use, all of which contribute to
the development of metabolic alkalosis.
• Severe alkalemia (blood pH >7.60) has been associated with cardiac arrhythmias,
particularly in patients with heart disease, hyperventilation, and hypoxemia.
• Neuromuscular irritability can be present, with signs of tetany or hyperactive
reflexes, possibly caused by the decreased ionized calcium concentration that
occurs secondary to the increase in pH. This decrease in ionized calcium may be
caused by a conformational change in the albumin molecules to which the calcium
is bound, resulting in increased binding, or by decreased competition from
hydrogen ions for binding sites on the albumin molecule.
• Mental confusion, muscle cramping, and paresthesia can also occur. Lastly,
patients will be more difficult to liberate from mechanical ventilation.
14 Dr. Hisham A. Nematalla
Management of Metabolic Alkalosis
• Because the body tolerates alkalemia far less well than acidemia, treatment of
metabolic alkalosis is nearly always required and should be aimed at correcting the
factor(s) responsible for the maintenance of the alkalosis.
• For example, vomiting should be treated with antiemetics, gastric losses of
hydrogen ion during nasogastric suction can be modulated by giving histamine
blockers such as ranitidine or proton pump inhibitors such as omeprazole and
reducing or discontinuing diuretic therapy.
• Metabolic alkalosis will persist until the renal mechanism responsible for
maintaining the disorder is corrected, even though the original cause of the
elevated plasma bicarbonate may have resolved.
• For example, hypovolemia should be treated with sodium chloride (i.e., diuretic
abuse or nasogastric suction) to allow excretion of bicarbonate by the kidney.
• However, patients with severely compromised cardiovascular function may not be
able to tolerate this therapeutic approach.
• In situations such as this and/or the presence of life-threatening alkalosis, some
have advocated reduction in pH by control of ventilation.
• Although controlled hypoventilation, sometimes using inspired CO2 with
supplemental oxygen to prevent hypoxia can be life-saving, this approach is not
universally accepted.
• Therapy for metabolic alkalosis can be conceptualized on the basis of the sodium
chloride responsiveness of the disorders.
15 Dr. Hisham A. Nematalla
You might also like
- Clinical Dermatology 5th Ed (2009) - Thomas P Habif PDFDocument14 pagesClinical Dermatology 5th Ed (2009) - Thomas P Habif PDFkikiNo ratings yet
- Teaching Plan: L - LagundiDocument4 pagesTeaching Plan: L - LagundiStiefen WingsingNo ratings yet
- Metabolic Alkalosis (Base Bicarbonate Excess) I. Brief DescriptionDocument3 pagesMetabolic Alkalosis (Base Bicarbonate Excess) I. Brief DescriptionAllyssa MackinnonNo ratings yet
- HYPOKALEMIADocument41 pagesHYPOKALEMIAsamudraandiNo ratings yet
- Metabolic AlkalosisDocument8 pagesMetabolic AlkalosisPauline PerezNo ratings yet
- Disturbances of Acid-Base BalanceDocument3 pagesDisturbances of Acid-Base BalanceDr. NateqNo ratings yet
- Fluid and Electrolyte FinalDocument51 pagesFluid and Electrolyte FinalGeethu SurendranNo ratings yet
- Metabolic AlkalosisDocument54 pagesMetabolic AlkalosispriyankagalhotraNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument15 pagesDr. Ali's Uworld Notes For Step 2 CKBoogy WoogyNo ratings yet
- Acid Base SchwartzDocument13 pagesAcid Base SchwartzRJ TanNo ratings yet
- Metabolic AlkalosisDocument9 pagesMetabolic AlkalosisMohammad Zaki BudimanNo ratings yet
- POTASSIUM HOMEOSTASIS كيمياء سريريةDocument4 pagesPOTASSIUM HOMEOSTASIS كيمياء سريريةMustafa Salah MahdiNo ratings yet
- Acid-Base Disorders NotesDocument10 pagesAcid-Base Disorders NotesLovely100% (1)
- Metabolic AlkalosisDocument2 pagesMetabolic AlkalosisKath ComodaNo ratings yet
- Metabolic Alkalosis: Sign Up For FREE atDocument1 pageMetabolic Alkalosis: Sign Up For FREE atKshirsagar DarshNo ratings yet
- Chloride, Bicarbonate and LactateDocument32 pagesChloride, Bicarbonate and LactateElla OrtegaNo ratings yet
- 7 Acidosis and AlkalosisDocument34 pages7 Acidosis and Alkalosismaria zaheerNo ratings yet
- Chapter 2 Electrolytes and Body Fluid AnalysiDocument103 pagesChapter 2 Electrolytes and Body Fluid AnalysiSanyii MamuyeNo ratings yet
- 02 Genel Cerrahi Notleri 2020Document61 pages02 Genel Cerrahi Notleri 2020Osama E. ShamsNo ratings yet
- Dangerous Rhythms Tachycardia: Potassium Electrolyte HypokalemiaDocument7 pagesDangerous Rhythms Tachycardia: Potassium Electrolyte HypokalemiagorodoeNo ratings yet
- Nephron PhysiologyDocument8 pagesNephron PhysiologyHadeel A. AlkayedNo ratings yet
- SHS.108.Lect-13 Acidosis AlkalosisDocument37 pagesSHS.108.Lect-13 Acidosis AlkalosisAzlan YasirNo ratings yet
- Metabolic AcidosisDocument1 pageMetabolic AcidosisLee June LyngNo ratings yet
- ReferatDocument53 pagesReferatHendri SaputraNo ratings yet
- Metabolic AcidosisDocument1 pageMetabolic AcidosisGlogogeanu Cristina AndreeaNo ratings yet
- Acid Base Disorders MBBSDocument44 pagesAcid Base Disorders MBBSphuyalaryan666No ratings yet
- Seminar RDocument93 pagesSeminar Rmubarak abdulkadirNo ratings yet
- Chloremia (Hypochloremia) & Acute and Chronic Respiratory Alkalosis (Carbonic Acid Deficit)Document4 pagesChloremia (Hypochloremia) & Acute and Chronic Respiratory Alkalosis (Carbonic Acid Deficit)KQarlo Luis Pestaño Maniaol100% (1)
- MetabolicDocument23 pagesMetabolicbtidipNo ratings yet
- 298 - Renal Pathology) Metabolic AlkalosisDocument4 pages298 - Renal Pathology) Metabolic AlkalosisMuhammadR1No ratings yet
- Biochem Blood BuffersDocument4 pagesBiochem Blood BuffersLouis TecsonNo ratings yet
- Chloride Deficit LecDocument2 pagesChloride Deficit Leced123edNo ratings yet
- Dagumbal Fluid and ElectrolyteDocument9 pagesDagumbal Fluid and ElectrolyteAlvin DagumbalNo ratings yet
- Acid-Base Disorders and AbgsDocument46 pagesAcid-Base Disorders and AbgsAlonso Rodriguez EscobedoNo ratings yet
- Diuretics and Dialysis: DR Arpana HazarikaDocument104 pagesDiuretics and Dialysis: DR Arpana HazarikaArpana HazarikaNo ratings yet
- Renal Tubular AcidosisDocument59 pagesRenal Tubular Acidosiskash_buNo ratings yet
- Acute DM ComplicationsDocument34 pagesAcute DM ComplicationsHillary RabinNo ratings yet
- Respiratory and Metabolic Acidosis & AlkalosisDocument34 pagesRespiratory and Metabolic Acidosis & AlkalosisAgus Sudiana NurmansyahNo ratings yet
- Sodium BicarbonateDocument6 pagesSodium BicarbonateBee AarNo ratings yet
- Part 1 - US-Grade 4-BiochemistryDocument34 pagesPart 1 - US-Grade 4-BiochemistryFarah Bashar Al-RawachyNo ratings yet
- Electrolytes and Arterial Blood Gases: James H. Harrison, JR., M.D., Ph.D. Center For Oncology and Pathology InformaticsDocument30 pagesElectrolytes and Arterial Blood Gases: James H. Harrison, JR., M.D., Ph.D. Center For Oncology and Pathology InformaticsPierre FlorendoNo ratings yet
- BiochemistryDocument33 pagesBiochemistryamhhospital0No ratings yet
- Rangkuman Fisiologi Sistem Kemih ManusiaDocument104 pagesRangkuman Fisiologi Sistem Kemih ManusiaPAP BungsuNo ratings yet
- Lecture 10.2-Laboratory Aspect of Electrolyte and Acid Based, DR Ira Puspitawati, SP - PK (2021)Document76 pagesLecture 10.2-Laboratory Aspect of Electrolyte and Acid Based, DR Ira Puspitawati, SP - PK (2021)NOVITA NUR ROHMA ROHMANo ratings yet
- Electrolytes - HypokalamiaDocument21 pagesElectrolytes - HypokalamiamympomNo ratings yet
- Regulation of Water & Electrolytes Balance: By: Husnil KadriDocument41 pagesRegulation of Water & Electrolytes Balance: By: Husnil KadrimarsyaNo ratings yet
- Rta Final Year 23.2.23Document36 pagesRta Final Year 23.2.23S.ayesh HasanNo ratings yet
- Adrenal Gland by Dr. Rajnee IInd PartDocument30 pagesAdrenal Gland by Dr. Rajnee IInd Part9460106212No ratings yet
- Hyperkalemia: Samir El AnsaryDocument43 pagesHyperkalemia: Samir El AnsaryStrept PneumoniaNo ratings yet
- Medical Surgical NursingDocument57 pagesMedical Surgical NursingLowellyn Grezen VillaflorNo ratings yet
- Kopac M. 2018Document6 pagesKopac M. 2018Jaeline Arleth Macias EscobarNo ratings yet
- c15 Diuretic AgentsDocument13 pagesc15 Diuretic AgentsmohammadNo ratings yet
- DiureticsDocument12 pagesDiureticslandita683No ratings yet
- Definition-Acute Kidney InjuryDocument6 pagesDefinition-Acute Kidney Injuryashi leginNo ratings yet
- The Biliary Tree and Cholestasis: Richard Hinton School of Biological Sciences University of SurreyDocument29 pagesThe Biliary Tree and Cholestasis: Richard Hinton School of Biological Sciences University of SurreynfacmaNo ratings yet
- 01 Lactic AcidosisDocument23 pages01 Lactic Acidosishanady alsnedNo ratings yet
- M5 3 HypokalemiaDocument6 pagesM5 3 HypokalemiaVishal KumarNo ratings yet
- Acid BaseDocument10 pagesAcid BaseOke RinaNo ratings yet
- Mineral, PH, Immunological Markers Plus CaseDocument55 pagesMineral, PH, Immunological Markers Plus CaseVio MincuNo ratings yet
- Introduction To Acid Base Metabolic AcidosisDocument12 pagesIntroduction To Acid Base Metabolic AcidosisKris Sharine Batalla OderoNo ratings yet
- Ascites, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandAscites, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesNo ratings yet
- PEDIA 1 The Pediatric History and Physical Exam HandoutDocument16 pagesPEDIA 1 The Pediatric History and Physical Exam HandoutRyan Loyd MarquezNo ratings yet
- Emedica MRCGP AKT Curriculum ChecklistDocument42 pagesEmedica MRCGP AKT Curriculum ChecklistSana Mustafa100% (1)
- Pediatrics KGMA February 2024Document98 pagesPediatrics KGMA February 2024abhijeets3011No ratings yet
- GDN 5-27 - Metalworking FluidsDocument5 pagesGDN 5-27 - Metalworking Fluidschelios2No ratings yet
- 4 Slaughterhouse Respiratory Check (SRC) and Its Applicability To Defend Ceva S Vaccines - Field Examples PDFDocument27 pages4 Slaughterhouse Respiratory Check (SRC) and Its Applicability To Defend Ceva S Vaccines - Field Examples PDFAnastasia DivaNo ratings yet
- Cognitive Psychology JournalDocument3 pagesCognitive Psychology JournalMcKayla ChurchNo ratings yet
- As An Airborne DiseaseDocument3 pagesAs An Airborne DiseaseGabby CabanesNo ratings yet
- What Do During Pandemic ExplanationDocument5 pagesWhat Do During Pandemic Explanationshiella mae baltazarNo ratings yet
- Diagnosis e Manegement Fo Dental ErosionDocument17 pagesDiagnosis e Manegement Fo Dental ErosionEvandro OenningNo ratings yet
- Treatment of Idiopathic Nephrotic Syndrome in Children - UpToDateDocument31 pagesTreatment of Idiopathic Nephrotic Syndrome in Children - UpToDateChetra ColaNo ratings yet
- To Heal The World - Catechesis On The PandemicDocument99 pagesTo Heal The World - Catechesis On The PandemicjL scribdNo ratings yet
- Proposal Form Proposal No:: For Office Use OnlyDocument14 pagesProposal Form Proposal No:: For Office Use OnlyPooja MishraNo ratings yet
- Abrar DMC Medicine OSPEDocument77 pagesAbrar DMC Medicine OSPEmfshihab3352No ratings yet
- Vector Control Interventions To Prevent Dengue IndiaDocument7 pagesVector Control Interventions To Prevent Dengue IndiaShadows BlameNo ratings yet
- Mary MallonDocument3 pagesMary Mallonapi-506588080No ratings yet
- Pneumonia Case Study FinalllDocument56 pagesPneumonia Case Study Finalllbethrice melegritoNo ratings yet
- Module 6 - Laboratory Investigation: Foodborne Disease Outbreak Investigation Team TrainingDocument44 pagesModule 6 - Laboratory Investigation: Foodborne Disease Outbreak Investigation Team TrainingrepyNo ratings yet
- INFEKSI HIV DAN HSV PADA OBSTETRI GINEKOLOGI - DR - Edi Wibowo A, SP - OG (K)Document24 pagesINFEKSI HIV DAN HSV PADA OBSTETRI GINEKOLOGI - DR - Edi Wibowo A, SP - OG (K)Rahayu AyuNo ratings yet
- Sumit SIP REPORT 18-20Document53 pagesSumit SIP REPORT 18-20Nikhil KharodeNo ratings yet
- Surgery in Elderly 2Document41 pagesSurgery in Elderly 2Zeba NaveedNo ratings yet
- Zoology 9th Edition Miller Test BankDocument14 pagesZoology 9th Edition Miller Test Bankthuygladys5x0100% (27)
- Module 2 Physical and Motor Development of Children and AdolescentDocument13 pagesModule 2 Physical and Motor Development of Children and Adolescentjaz bazNo ratings yet
- SCRIPT For SOCLEGDocument7 pagesSCRIPT For SOCLEGKaren Ryl Lozada BritoNo ratings yet
- Tubulointerstitial Nephritis - 161269200418Document12 pagesTubulointerstitial Nephritis - 161269200418ተሣለነ ወልድNo ratings yet
- Psychoeducation in Psychiatric DisorderDocument23 pagesPsychoeducation in Psychiatric Disorderishita aggarwal100% (1)
- Discharge Planning ProjectDocument5 pagesDischarge Planning Projectapi-325271731No ratings yet
- Controversies in The Management of Functional Constipation in ChildrenDocument8 pagesControversies in The Management of Functional Constipation in ChildrenDaniela Rodríguez MartínezNo ratings yet
- 1156 The Effects of Acupuncture Versus Sham Acupuncture in The Treatment of Fibromyalgia A Randomized Controlled Clinical Trial FileDocument6 pages1156 The Effects of Acupuncture Versus Sham Acupuncture in The Treatment of Fibromyalgia A Randomized Controlled Clinical Trial FileValdemar Caumo JuniorNo ratings yet