Professional Documents
Culture Documents
General Principles in Clinical Microbiology Supplemental Notes
General Principles in Clinical Microbiology Supplemental Notes
Uploaded by
Ahnorrei PavlaskaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
General Principles in Clinical Microbiology Supplemental Notes
General Principles in Clinical Microbiology Supplemental Notes
Uploaded by
Ahnorrei PavlaskaCopyright:
Available Formats
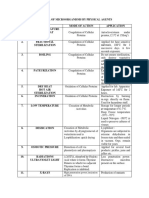
Laboratory Safety
PROTOCOL ACTION APPLICATION AGENTS
used on INANIMATE OBJECTS/FOMITES
Reduces/inhibit
pathogenic
microorganisms but Household bleach,
Cleaning laboratory
not all (prions, phenols (e.g., Lysol),
DISINFECTION viruses, endospores
surfaces, working
glutaraldehyde,
area, bathrooms
etc.); prolonged alcohol
exposure may destroy
bacterial endospores
Ionizing radiation,
Removal of pathogenic Treatment of
halogens, peracetic
DECONTAMINATION organisms for safe infectious waste prior
acid, autoclave,
handling to disposal
incineration
Complete elimination Preparation of
of all vegetative cells surgical equipment Autoclave, biocides,
STERILIZATION including spores and and needles for radiation
viruses injection, etc.
used on SKIN OR LIVING BEINGS
Kills/inhibits Cleaning injured skin
Iodophor, 70% ethyl
ANTISEPSIS multiplication of or in preparation of
alcohol
microorganism surgical procedures
Reduction of
microbial load by Soap and water,
DEGERMING gentle to firm
Handwashing
alcohol
scrubbing
METHOD ACTION APPLICATION DISADVANTAGE CONDITION
DRY HEAT
INCINERATION Dehydrates cell Used to treat Ashes produced are 870°C to
wall; denatures infectious waste; toxic and presence of 980°C
protein burned to ashes at high heavy metals are
temp.; recommended observed
for prions and
infective proteins
DRY HEAT Dehydrates cell Used to sterilize Requires longer 160°C- 180°C
OVEN wall; denatures glassware, oil, exposure time 1-3 hours
protein and petroleum, or powder compared to moist
nucleic acid by heat
disrupting cell
membrane
MOIST HEAT- steam under pressure
AUTOCLAVE Coagulates and Sterilization of 121°C at
*Most denatures biohazardous trash 15psi(atm)
efficient structural and heat-stable objects _ for 30 mins
method* proteins and
Prepared by: coramirez, rmt032023
enzymes
irreversibly
BOILING Denaturation of Used for disinfection Cannot kill 100°C for 15-
protein which kills vegetative endospores 30 mins
bacteria
CHEMICAL
ETHYLENE Blocks DNA For decontamination Lengthy cycles and Used in
OXIDE replication and of rubber, plastic creates potential gaseous form
enzymatic tubes, other heat- hazard production QC: Bacillus
reaction sensitive materials subtilis @
35°C- 37°C
VAPOR-PHASE- Production of Used as sterilant for Cannot penetrate
H2O2 toxic free nonmetal and devices well with large dense -
radicals that that cannot tolerate packaging of
affects lipids, high temperatures material
DNA and other (e.g., HEPA filters)
cell components
of the
microorganism
IRRADIATION
NON-IONIZING Breaks disulfide Used to sterilize rooms Low penetration Greatest
(e.g., UV bond and BSCs rate, antimicrobial
light) microorganisms activity at
must have direct 250-260nm
exposure
IONIZING Damages DNA Used to sterilize rooms
(e.g., X-ray, affecting and disposable
gamma rays, replication, materials (e.g., gloves)
cathode produces free
rays) radicals
FILTRATION
LQUID Removal of Used for sterilizing Uses cellulose
FILTRATION microorganism solutions such as acetate or
with the use of antibiotic solution, cellulose
cellulose acetate protein solution, nitrate
as filter vaccines, etc. medium with
vacuum
AIR Removal of Used to sterilize air in HEPA filter
FILTRATION microorganism Biosafety Cabinets or (>0.3um)
with the use of in rooms ULPA filter
filters <0.3 um
PASTEURIZATION
Destroys milk/food-borne Used for milk/food Heat gently
pathogens without damaging sterilization at 70°C for 30
nutritional content or flavor minutes
Method of Sterilization BIOLOGICAL INDICATOR (for Quality Control)
DRY HEAT Bacillus subtilis var. niger
AUTOCLAVE Bacillus stearothermophilus
IONIZING RADIATION Bacillus pumilis
ETHYLENE OXIDE Bacillus subtilis var. globiji
Chemical sterilant or Biocides are chemicals that kills or destroys all vegetative lifeform.
However, if used in shorter period, this may serve as disinfectants.
Prepared by: coramirez, rmt032023
Chemical Sterilant/Biocide Action
Exhibits broad spectrum antimicrobial activity against vegetative
Alcohol bacteria, viruses, and fungi but not sporicidal. Optimal when diluted
with water at 60-90% (ethyl, isopropyl, n-propanol)
For low temperature disinfection and sterilization of endoscopes and
Aldehydes surgical equipment (at 2% conc. sporicidal). (Formaldehyde and
Glutaraldehyde) Not commonly used and are irritant.
Chlorine-releasing agents such as sodium hypochlorite, chlorine
dioxide, and sodium dichloroisocyanurate (oxidizing agents; destroy
Halogens cellular activity of protein, sporicidal at higher concentration)
recommended dilution at 1:10
Broad-spectrum activity against microorganisms. Sporicidal at 10-
Peroxygen 30% of H2O2 and longer contact times. (Commercially available at 3%)
Effective in the presence of organic material, used for sterilization
Peracetic acid of surgical instruments. Cold sterilization is the term used when
peracetic acid and glutaraldehyde are used as sterilant.
Antiseptic, disinfectant, and preservative properties of detergent at
Phenolics 2-5% concentration; used for cleaning bench tops.
Cationic detergents useful as antiseptic and disinfectants; for bench
Quaternary ammonium
tops or lab surfaces. Inactivated by gross contamination of organic
compounds (QUATS/QUACS) material (e.g., blood), limiting its usage; made up of ammonium salts.
refer to book for complete list
Training and practice of aseptic technique.
Interdiction of mouth pipetting.
NO eating, NO drinking, NO smoking inside the laboratory.
Proper use of PPE inside the laboratory and should not be worn outside.
Use of Biosafety Cabinets.
Immunization of employees when vaccines are available.
Adherence to Biosafety Level precautions.
Employee education and orientation
Proper biohazardous waste disposal
Engineering controls and safe work practices
Personal Protective Equipment
Postexposure plan (includes investigation of all accidents and plan to prevent re-occurrence
with proper documentation)
Must adhere with the local regulations and national guidelines.
Biohazard bags and containers must contain biohazard symbols
All materials contaminated with potentially infectious agents must be decontaminated by
waste-treatment method (autoclaving, incineration, etc.).
Do not remove or insert contact lenses inside the laboratory.
Limit access to laboratory personnel only.
Assume all patients are infectious.
Discard sharps in appropriate waste bin.
Never recap needles by hand, use safety devices.
Prepared by: coramirez, rmt032023
Biohazard symbols must be displayed on laboratory doors and equipment that has infectious
materials.
Air movement from lower to higher risk areas must be observes.
Pest control program.
Houseplants are not allowed.
Prepared by: coramirez, rmt032023
Category A: UN 6.2, UN 2814, UN 2900
Category B: UN 3373
Labels include:
Infectious substance (diamond shaped
label or UN 3373 certification mark)
Proper shipping name and UN 2814
certification mark
Shipper and consignee identification
(name, address, and telephone)
Package orientation arrows if
primary receptacle exceeds 50 mL or
more
Prepared by: coramirez, rmt032023
SPECIMEN MANAGEMENT
Collected during the early phase of illness (within 2-3 days for viral infections), and before
medications are administered, if possible.
Collection manuals/instruction are given to clinicians by the microbiologist for optimal
specimen collection and transport information. Manual should include the following:
o Safety considerations
o Selection of the appropriate anatomic site and specimen
o Collection instructions, including the type of swab or
o transport medium
o Transportation instructions, including time and temperature
o constraints
o Labeling instructions, including patient demographic
o information (minimum of two patient identifiers)
o Special instructions, such as patient preparation
o Sterile versus nonsterile collection devices
o Minimal acceptable quality and recommended quantity
Specimen in microbiology should be collected in sterile containers except for stool.
For specimen collected by patients, verbal and written instruction should be given.
Specimen should be transported to the laboratory within 2 hours of collection.
Adverse changes in oxygen, pH, and temperature in the environment can prevent recovery of
certain microorganisms and allows overgrowth of others.
Preservative/Transport
Application
media
Boric acid Urine preservation
Polyvinyl alcohol
Ova, parasite, trophozoites, and cyst
Formalin
Transport media that contains swab and is activated by crushing an
Stuart’s medium ampule
Amie’s medium Modified Stuart’s medium
Sodium polyaenthol
Anticoagulant for blood culture, bone marrow, and synovial fluid
sulfonate
Sodium thioglycolate Maintain viability for up to 72 hours
Cary-Blair medium For stool specimen (enteric pathogens)
Serves as N. Gonorrhea transport medium which contains selective
JEMBEC system agar and CO2 generating tablet.
Specimen Specimen transport Storage before processing
Hair, Nails, or Skin Scrapings (for
Within 72 hours/ RT Indefinitely/RT
fungal culture)
TISSUE <15 min/ RT 24 hours/RT
Blood or Bone Marrow Aspirate Within 2 hours/RT RT/<2 hours
BONE Immediately/RT Plate as soon as received
<24 hours RT
CSF <15 minutes
For viruses 3 days at 4°C
Abscess (also Lesion, Wound, Pustule, Ulcer)
Superficial
<2 hours RT/24 hours
Deep
Prepared by: coramirez, rmt032023
Body Fluids
Amniotic
Ascites
Abdominal <24hours/ RT
Bile
<15 minutes
Synovial
Pleural
<24 hours/ 4°C and for fungal
Pericardial
cultures
Specimen Specimen transport Storage before processing
EAR
Inner <2 hours 24 hours/RT
Outer <2 hours/ RT 24 hours/4°C
EYE
Conjunctiva <2 hours/ RT 24 hours/ RT
Aqueous/Vitreous fluid
<15 min/ RT <24 hours/ RT
Corneal scrapings
FOREIGN BODIES
IUD Plate as soon as received
<15 minutes/ RT Plate as soon as received, if
IV catheters, pins
possible; <2 hours/ 4°C
GI TRACT
<24 hours/ 4°C; neutralized
Gastric aspirate <15 minutes/ RT with sodium bicarbonate
within 1 hour of collection
Gastric biopsy <1 hour/RT <24 hours/ 4°C
Rectal swab <2 hours/ RT <24 hours/ RT
Within 24 hours/ RT in
24 hours/4°C; 48 hours/RT
Stool routine cultures holding media
or 4°C
Unpreserved <1 hour/RT
Fresh non-preserved liquid
Ova & Parasite samples examined within 30 Indefinitely/ RT
minutes of passage
Genital Tract
Bartholin cyst
Cervix
Cul-de-sac
FEMALE <2 hours/ RT 24 hours/RT
Endometrium
Urethra
Vagina
Swab: <2 hours/ RT Swab: 24 hours/ RT
Prostate
Tube: Immediately/RT Tube: Immediately/RT
MALE Swab: 24 hours/ RT
Swab: <2 hours/ RT
Urethra JEMBEC: RT upon receipt in
JEMBEC: Within 2 hours
lab
Urine
Preserved: Within 24 hours/
RT
Clean-voided midstream
Unpreserved <2 hours/RT
24 hours/4°C
<2 hours/RT
Straight catheter (In and out)
Preserved: <24 hours/RT
Suprapubic aspirate Immediately/RT Plate as soon as received
**RT: Room Temperature
Prepared by: coramirez, rmt032023
Mislabeling
Improper transport temperature
condition
Incorrect transport media used
Quantity-not-sufficient
Leakage
Specimen transported beyond expected
time
Use of fixative which kills
microorganism
Incorrect site of collection
Specimen is dried
Processing specimen with questionable
medical value
Areas with blood or mucus must be located and sampled for culture and direct examination.
Note the appearance of specimen being received whether it is blood, cloudy, clotted, etc.
Stool should be examined for evidence of barium (chalky white color), which may preclude
O & P examination.
Serves as quality assessment of specimen, for example the assessment of sputum using
Bartlett’s criteria.
Early indication of infectious agent (e.g., presence of WBC and gram [+] diplococci indicative
S. pneumoniae)
Guide as comparison with result to culture, since both must correlate with each other to the
type of specimen being used. This is to ensure information accuracy.
Can dictate the need for additional testing (e.g., presence of fungal elements for bacterial
culture, this would alert technologist to notify physician to request a fungal culture)
Some specimen does not provide useful information using direct microscopic examination,
such as throat and nasopharyngeal specimen.
Most common bacterial stain GRAM STAIN
Most common direct fungal stains: KOH, Periodic-Acid Schiff, Gorcott’s methenamine silver
stain, and calcofluor white.
Most common direct acid-fast stain: Auramine-rhodamine, Ziehl-Neelsen, Kinyuon
Culture media Description
According to state
Solid media 1.5- 2.0% agar
Semi-solid media 0.5-1.0% agar
Liquid No agar needed
According to use
For isolation; supports growth of non-fastidious organism which
Nutritive/Nonselective support growth of most organisms. (e.g., BAP, CAP)
Prepared by: coramirez, rmt032023
Supports one group of organisms but not another by addition of
antimicrobials, dyes, or alcohol to the medium. (e.g., MAC, CAN,
Selective media MSA, PEA, SSA, HEA, EMB, TCBS, etc.)
Allows grouping of microorganism based on different
Differential media characteristics demonstrated on the media (e.g., BA, MAC, HEA,
Bile-Esculin agar)
Made together with solid media, so small numbers of organisms
may be detected; allows detection of anaerobes in aerobic culture or
Enrichment/Backup broth organisms damaged by either previous or concurrent antimicrobial
therapy. (e.g., BHIB, thioglycolate, TSB, Selenite broth, Regan Lowe,
etc.)
According to dispensing/distribution
Plated media Preparation: weigh>dissolve>autoclave>dispense
Tubed media Preparation: weigh> dissolve>dispense> autoclave
SELECTION FOR ROUTINE PRIMARY PLATING
Should be based on the specimen type and organism likely to be involved.
Nonselective agar plate for non-fastidious organisms.
Enriched medium for fastidious organisms for normally sterile body fluids or site in which
fastidious organisms are expected.
Selective and differential medium for enteric gram-negative bacilli for most routine bacterial
cultures.
Selective medium for gram-positive organisms for specimens in which mixed gram-positive and
gram-negative bacteria are found.
Additional selective media or enrichment broths for specific pathogens as needed.
Broth medium may be used as a supplement with specimens from sterile body fluids, tissues,
lesions, wounds, and abscesses.
SPECIMEN PREPARATION
Direct inoculation: sterile body fluids, pus, urine, swab, and sputum.
Large volumes of sterile fluid (e.g., ascites or pleural) needs concentration by centrifugation or
filtration. Sediment is inoculated.
Decontamination of respiratory specimen, such as for legionella or mycobacteria.
Swabs may be smeared directly or swab may be suspended into 0.5-1.0 mL of broth and then
vortex-mixed for 10-20 seconds to loosen material and produce even suspension of organisms.
Homogenization for tissue culture is done by mincing or grinding the tissue sample, but this
may destroy fungal elements.
ISOLATION TECHNIQUES
POUR-PLATE METHOD
o Used for obligate and
anaerobic bacteria;
isolation of microbial
colonies by serial
dilutions and counting
colony forming units.
o Before performing,
sample is diluted in series
to bring the microbial
burden within sample
range between 20-300
CFU/mL.
Prepared by: coramirez, rmt032023
STREAK PLATE METHOD
o Semi-quantitative- streaked in four quadrants, which aims for isolation,
microorganisms are successively diluted out as each quadrant is streaked until finally
each morphotype is present as a single colony. Streaked on agar using wire loop.
Grading Interpretation
1 Rare, growth on 1st quadrant only
2 Few or light, growth until 2nd quadrant only
3 Moderate growth until 3rd quadrant only
4 Many, heavy growth on all quadrant
o Quantitative- plates are inoculated for quantitation and are usually streaked using a
1:100 or 1:1000 calibrated loop.
INCUBATION CONDITIONS
Most bacteria grow at 35°- 37° C
Obligate aerobes cannot live without air
Facultative anaerobes are primarily aerobic, but can live in the absence of air.
Aerotolerant anaerobes does not require oxygen, but can tolerate the presence of air.
Microaerophilic grows with reduced O2 (5-10%) and increased CO2 (8% to 10%). Isolated using a
specially designed chamber jars or bags.
Capnophiles grows in an increased concentration of CO2 (5-10%) and ~15% of O2; Candle jar (3%
CO2), CO2 incubator, chamber jar or bag
PANIC VALUES
Certain panic values must be
communicated to the clinician
immediately.
Here is a list of common panic values
in microbiology department:
Prepared by: coramirez, rmt032023
MICROSCOPY
Rapid preliminary organism identification by direct visualization of specimens
Rapid final identification of certain organisms by direct visualization in specimens
Detection of different organisms present in the same specimen
Detection of organisms not easily cultivated in the laboratory
Evaluation of patient specimens for the presence of cells indicative of inflammation (i.e.,
phagocytes) or contamination (i.e., squamous epithelial cells)
Determination of an organism’s clinical significance; bacterial contaminants are not usually
present in patient’s specimen at sufficiently high numbers (3105 cells/mL) to be seen by light
microscopy.
Preculture information about which organisms might be expected to grow so that appropriate
cultivation techniques are used
Determination of which tests and methods should be used for identification and
characterization of cultivated organisms
A method for investigating unusual or unexpected laboratory test results
Most commonly used in microbiology which
consists of ocular and objective lenses.
Principle: visible light is passed through the
specimen and then through a series of lenses
that bend the light in a manner that results
in magnification of the organisms present in
the specimen.
Other factors in optimizing visualization:
o Resolution, extent to which detail in
the magnified object is maintained.
o Resolving power, closest distance of
two objects that when magnified,
allows the two objects to be
distinguished from each other.
o Contrast, achieved by staining
techniques that highlight organisms
allowing them to be differentiated
from one another and from the
background material/debris.
Gram staining and acid-fast staining are
among the commonly used stain.
Desired resolution with 1000x
magnification is achieved by using immersion oil; oil immersion lens is designed for use with oil.
Direct smear- preparation from primary clinical sample received in the laboratory for
processing; indirect smear- indicates that the primary sample has been processed in culture and
the smear contains organisms obtained after purification or growth on artificial media.
Does not used fixed smear preparation, instead, use wet mount to view organisms and other cells.
Developed to improve contrast differences between cells and the surrounding medium
Principle: uses beams of light passing through the specimen by different densities or thickness
of the microbial cells or cell structures in the specimen. The greater the refractive index of an
object, the more beam of light is slowed which results in decreased light intensity.
Allows observation of viable microorganisms; used to identify medically important fungi grown
in culture.
Formation of dark image on light background.
Prepared by: coramirez, rmt032023
Principle: Fluorophores or fluorochromes, can be raised to a higher energy level after absorbing
ultraviolet (excitation light). When the dye returns to their normal state, they release excess
energy in the form of visible (fluorescent) light.
Photobleaching or fading is the permanent loss of fluorescence as a result of chemical damage to
the fluorochrome. Store in slides in a dark container and refrigerated at 2° to 8°C to decrease loss
of fluorescence over time.
Quenching results from the transfer of light energy to nearby molecules in the sample such as
free radicals, salts of heavy metals, or halogens. May be alleviated by adding chemical
scavengers to the mounting fluid
Fluorochroming a direct chemical interaction occurs between the fluorescent dye of fluorophore
and a component of the bacterial cell; this interaction is the same as occurs with the stains used
in light microscopy, the difference is that it uses fluorescent dye that enhances contrast and
amplifies the observer’s ability to detect stained cells tenfold greater than in light microscopy.
Below are the most common fluorochroming methods used in diagnostic microbiology:
o Acridine orange binds to nucleic acid; used to confirm presence of blood cultures when Gram’s
stain is difficult to interpret or when presence of bacteria is highly suspected but none are
detected using light microscopy; Stains all nucleic acids, thus, it is nonspecific.
o Auramine-Rhodamine high affinity to mycolic acid of mycobacteria; binds to most mycobacteria,
nonspecific.
o Calcofluor White used for direct detection of fungi; cell walls of fungi bind the stain which
enhances its visibility in tissue and other specimen.
Immunofluorescence uses
antibodies labeled with
fluorescent dyes (conjugate) to
specifically stain a particular
bacterial species. These
fluorescent antibodies are then
added to microscope slide
containing a clinical specimen.
The fluorescent antibody will bind to the antigen on the surface of the bacteria, forming antigen-
antibody complex or tagged, it will be detectable by fluorescent microscopy.
o Used to directly examine for bacteria that are difficult or slow to grow (e.g.,Legionella spp.,
Bordetella pertussis, and Chlamydia trachomatis)
o Fluorescein isothiocyanate (FITC) most commonly used fluorochrome for conjugation to
antibodies.
Similar to phase-contrast microscopy that involves alteration of microscopic technique rather
than using dyes/stain.
Principle: special condenser does not allow light to pass directly through the specimen but directs
the light to hit the specimen at an oblique angle. This creates “dark-field” that contrasts against
the highlighted edge of the specimen and results when the oblique rays are reflected from the
edge of the specimen upward into the objective microscope.
All other light that passes through the specimen will miss the objective, thus making the
background a dark field.
Utilized for detecting bacteria with thin dimensions which makes it difficult to be seen using
light microscopy and are difficult to grow in culture. For detection of spirochetes (e.g.,
Treponema pallidum)
Extremely bright object against black field.
Prepared by: coramirez, rmt032023
Uses electrons instead of light to visualize small objects and, instead of lenses, the electrons are
focused by electromagnetic fields and form an image on a fluorescent screen, like a television
screen.
Allows magnifications in excess of 100, 000, 000x.
Two general types of electron microscopes:
o Transmission electron microscope passes electron beam through
objects and allows visualization of internal structures; can
resolve particles 0.001 um
o Scanning electron microscope uses electron beams to scan the
surface of the object and provide three-dimensional views of the
surface structures.
Powerful research tools, many new morphologic features of different
microorganisms have been discovered using electron microscopy.
Not needed for the laboratory diagnosis of most infectious diseases,
only few laboratories employ this method.
Uses sophisticated software and unique technology allowing laboratories to acquire microscopic
digital images of Gram stain using a web-based interface.
The interface allows images using fully automated microscope to be viewed on a screen.
Provides opportunity for standardization, cost reductions, and quality improvement of testing.
References:
1. Chapters 4-6, p. 42-85. Bailey & Scott’s Diagnostic Microbiology / Patricia M. Tille, Fourteenth Edition
(2017)
2. Chapter 4,6-7, p.57-87, p104-125. Mahon, Connie R., editor. | Lehman, Donald C., editor: Textbook of
diagnostic microbiology / [edited by] Connie R. Mahon, Donald C, Sixth edition. | St. Louis, Missouri: Elsevier
Saunders, [2019]
Prepared by: coramirez, rmt032023
You might also like
- Angeles Pht413Document3 pagesAngeles Pht413Eduard AngelesNo ratings yet
- Trans Module 3 - Microbial Control and Safety (FKHMR)Document6 pagesTrans Module 3 - Microbial Control and Safety (FKHMR)Faye Kyla Heart ResuelloNo ratings yet
- Principle, Advantages, Disadvantages, Application S of Different Sterilisation Methods and in Process ControlDocument50 pagesPrinciple, Advantages, Disadvantages, Application S of Different Sterilisation Methods and in Process ControlAhmed ImranNo ratings yet
- Term Methods Actions Level of Activity Uses: PhenolsDocument5 pagesTerm Methods Actions Level of Activity Uses: PhenolsJuliana ViteNo ratings yet
- Bio204 Principles of Biochemical EngineeringDocument32 pagesBio204 Principles of Biochemical EngineeringHanifullah JanNo ratings yet
- 3 Lec Notes Sterilization and DisinfectionDocument4 pages3 Lec Notes Sterilization and DisinfectionMacky IbayNo ratings yet
- Sterilization: Sterility TestDocument5 pagesSterilization: Sterility TestSwaroopSinghJakharNo ratings yet
- Sterilization 68Document1 pageSterilization 68Anonymous 9PcFdakHcNo ratings yet
- Sterilization & DisinfectionDocument23 pagesSterilization & Disinfectionemelda sugiartiNo ratings yet
- Sterilization and DisinfectionDocument58 pagesSterilization and DisinfectionBoas Wayne100% (2)
- CONTROLDocument7 pagesCONTROLAbDul RehManNo ratings yet
- FPa 003Document6 pagesFPa 003stepuptoblockNo ratings yet
- Fosroc Nitocote HEX: Constructive SolutionsDocument4 pagesFosroc Nitocote HEX: Constructive SolutionsVJ QatarNo ratings yet
- Week 7 Control of Microbial Growth 2022Document64 pagesWeek 7 Control of Microbial Growth 2022Rivaldi Di CaprioNo ratings yet
- MICRODocument6 pagesMICROShaye Toliao GeligNo ratings yet
- Disinfection Inanimate DisinfectantsDocument36 pagesDisinfection Inanimate DisinfectantsPRASHANT SOLANKINo ratings yet
- Instruments Sterilization-Bansal NotesDocument3 pagesInstruments Sterilization-Bansal NotesGurpremjit SinghNo ratings yet
- Sterlization AsepsisDocument30 pagesSterlization AsepsisVinod BharatiNo ratings yet
- Sterilisation and DisinfectionDocument61 pagesSterilisation and Disinfectionbhoomika kharviNo ratings yet
- Microbiology NotesDocument13 pagesMicrobiology NotesSuchit ChaturvediNo ratings yet
- 5 Decontamination, Decommissioning and Waste Disposal 4.10.23Document59 pages5 Decontamination, Decommissioning and Waste Disposal 4.10.23hamza najmNo ratings yet
- 5 - Control of Microbial GrowthDocument30 pages5 - Control of Microbial GrowthAbdallah MoayadNo ratings yet
- Sterilization and Disinfection of Dental Instrument 7.2Document5 pagesSterilization and Disinfection of Dental Instrument 7.2Khylle Camron LuzzieNo ratings yet
- L4 - Sterilization and DisinfectionDocument23 pagesL4 - Sterilization and DisinfectionArshad AbbasNo ratings yet
- 1-Sterlization and DisinfectionDocument94 pages1-Sterlization and DisinfectionFaaye ZzaaNo ratings yet
- Development of Eye & EarDocument29 pagesDevelopment of Eye & EarSix OneNo ratings yet
- General Surgery Notes For Dental StudentsDocument128 pagesGeneral Surgery Notes For Dental StudentsMustafa SaßerNo ratings yet
- Micro CH 5 Cheml ControlDocument49 pagesMicro CH 5 Cheml ControlBernadette Joyce PascualNo ratings yet
- Controlling The Growth of MicroorganismsDocument249 pagesControlling The Growth of MicroorganismsthediaberNo ratings yet
- The Control of Microbial GrowthDocument29 pagesThe Control of Microbial GrowthKavisa GhoshNo ratings yet
- Sec.5 SterlizationDocument40 pagesSec.5 Sterlizationفيزيا مهمهNo ratings yet
- Guidance Note 6 DisinfectionDocument9 pagesGuidance Note 6 DisinfectionLum SenioritaNo ratings yet
- Microbiology Casi Lec 1Document5 pagesMicrobiology Casi Lec 1Stevens MacabidangNo ratings yet
- Sterilisation TechniquesDocument4 pagesSterilisation TechniquesmehekNo ratings yet
- Sterilization & DisinfectionDocument27 pagesSterilization & DisinfectionmisdduaaNo ratings yet
- Sterilization - Vs-Disinfection: A Reference Guide To The Difference BetweenDocument9 pagesSterilization - Vs-Disinfection: A Reference Guide To The Difference BetweenyunhungNo ratings yet
- Theme 9 NutritionDocument16 pagesTheme 9 NutritionAmitNo ratings yet
- Nano223 200ml Flyer PDFDocument2 pagesNano223 200ml Flyer PDFBose CatNo ratings yet
- SterilizationDocument6 pagesSterilizationعبدالرحمن عابدNo ratings yet
- Biotech ReviewerDocument5 pagesBiotech ReviewerKristine Ross PelaezNo ratings yet
- Control of Microbial DrugsDocument31 pagesControl of Microbial Drugseyadballas35No ratings yet
- Sterilization and Disinfection - PART IDocument34 pagesSterilization and Disinfection - PART IDr Harender Simar100% (1)
- Asynchronous - Asepsis CaseDocument4 pagesAsynchronous - Asepsis CaseGeorgette FloreanneNo ratings yet
- Bacteriology Lab 1 - Introduction To Bacteriology LaboratoryDocument3 pagesBacteriology Lab 1 - Introduction To Bacteriology LaboratoryJiro Anderson EscañaNo ratings yet
- Hospital Acquired Infections: Polymer Technologies To Manage RiskDocument4 pagesHospital Acquired Infections: Polymer Technologies To Manage RiskVenkadesh SubramanianNo ratings yet
- Dermatologic Pharmacology 2Document8 pagesDermatologic Pharmacology 2Nikko Angelo AlcalaNo ratings yet
- Antiseptics & DisinfectantsDocument53 pagesAntiseptics & DisinfectantselanthamizhmaranNo ratings yet
- Microbio Midterm LectureDocument4 pagesMicrobio Midterm LectureCookie BiscuitsNo ratings yet
- Give The Application and Scenarios Where Chemical and Physical Methods of Sterilization Are Best To UseDocument5 pagesGive The Application and Scenarios Where Chemical and Physical Methods of Sterilization Are Best To UseEarly SaribaNo ratings yet
- DISINFECTION AND DECONTAMINATION OF WORKING AREA For ReflectionDocument4 pagesDISINFECTION AND DECONTAMINATION OF WORKING AREA For ReflectionNick PolesticoNo ratings yet
- Sterilization and DisinfectionDocument67 pagesSterilization and DisinfectionBhoomika Sikri100% (1)
- Physical and Chemical Control of MicroorganismDocument37 pagesPhysical and Chemical Control of Microorganismf20220420No ratings yet
- Biox H ENDocument3 pagesBiox H ENtheglamhavanaNo ratings yet
- Biomedical Waste Management: Isha Thaker Roll No. 142Document14 pagesBiomedical Waste Management: Isha Thaker Roll No. 142TECHNICAL GHOSTNo ratings yet
- SterilizationDocument26 pagesSterilizationGanesh V GaonkarNo ratings yet
- Lezon 2Document2 pagesLezon 2Idk UlitNo ratings yet
- Neo Guard: Life Guard Pharma Pvt. LTDDocument2 pagesNeo Guard: Life Guard Pharma Pvt. LTDRavi MadaanNo ratings yet
- 1 Histopathologic-TechniquesDocument3 pages1 Histopathologic-TechniquesJOUBELLE NUR-NISA NAVALNo ratings yet
- Biochem ProjectDocument1 pageBiochem ProjectSumaira AamirNo ratings yet
- Medical Mycology: Cellular and Molecular TechniquesFrom EverandMedical Mycology: Cellular and Molecular TechniquesKevin KavanaghNo ratings yet
- Microscopy Hand NotesDocument10 pagesMicroscopy Hand NotesAmeeraNo ratings yet
- Histopathology Laboratory OverviewDocument31 pagesHistopathology Laboratory OverviewaliNo ratings yet
- Basic Organization: Diagnostic Microbiology LaboratoryDocument33 pagesBasic Organization: Diagnostic Microbiology Laboratorytummalapalli venkateswara raoNo ratings yet
- Diferenciacion de Hematogonias y LinfoblastosDocument6 pagesDiferenciacion de Hematogonias y LinfoblastosSusan RamosNo ratings yet
- Diagnosis of Viral Infection (2021-2022)Document21 pagesDiagnosis of Viral Infection (2021-2022)Fahim JaniNo ratings yet
- Beautiful Science Cell Image Coloring BookDocument38 pagesBeautiful Science Cell Image Coloring BookOanaNo ratings yet
- Highly Multiplexed Immunofluorescence Imaging of Human Tissues and Tumors Using T-CyCIF and Conventional Optical MicroscopesDocument46 pagesHighly Multiplexed Immunofluorescence Imaging of Human Tissues and Tumors Using T-CyCIF and Conventional Optical MicroscopesCavin PengNo ratings yet
- A. Unit y Diversity 2. CellsDocument66 pagesA. Unit y Diversity 2. CellshzunigaNo ratings yet
- Dsa 281Document319 pagesDsa 281Nabil ChoukNo ratings yet
- Protocol For Cell Cycle Analysis Using Flow CytometryDocument6 pagesProtocol For Cell Cycle Analysis Using Flow CytometryNeeraj Kalyan GandholiNo ratings yet
- ELISADocument18 pagesELISAmukulpjrNo ratings yet
- Prerequisites For Immunoelectron MicrosDocument3 pagesPrerequisites For Immunoelectron Microsacr3656No ratings yet
- Methods For The Assessment of NET Formation: From Neutrophil Biology To Translational ResearchDocument16 pagesMethods For The Assessment of NET Formation: From Neutrophil Biology To Translational ResearchSzyszka TropinosNo ratings yet
- Isolation of Lymphoid Cells: - Antigen-Antibody Interactions - Antigen-Antibody Based ExperimentsDocument111 pagesIsolation of Lymphoid Cells: - Antigen-Antibody Interactions - Antigen-Antibody Based ExperimentsSivarama KrishnanNo ratings yet
- Cappel Primary and Secondary AntibodiesDocument47 pagesCappel Primary and Secondary Antibodiesjohn chinNo ratings yet
- HistologyDocument423 pagesHistologydorina0101100% (1)
- 16-17 2011 Lecture 1 Handout VersionDocument23 pages16-17 2011 Lecture 1 Handout Versionjeny mathewNo ratings yet
- Rapid Antigen-Specific T Cell Enrichment (Rapid ARTE) - All Protocols - Applications - Miltenyi Biotec - DeutschlandDocument11 pagesRapid Antigen-Specific T Cell Enrichment (Rapid ARTE) - All Protocols - Applications - Miltenyi Biotec - Deutschlandzixu wangNo ratings yet
- Light MicrosDocument39 pagesLight MicrosNabanita ChatterjeeNo ratings yet
- The Wd40 Protein Bamb Mediates Coupling of Bam Complexes Into Assembly Precincts in The Bacterial Outer MembraneDocument14 pagesThe Wd40 Protein Bamb Mediates Coupling of Bam Complexes Into Assembly Precincts in The Bacterial Outer MembraneAMMAR RAZANo ratings yet
- UprgenyDocument9 pagesUprgenyJose Rafael Villafan BernalNo ratings yet
- Immunofluorescence Handbook 1601971Document80 pagesImmunofluorescence Handbook 1601971Ray KuoNo ratings yet
- QIAexpress Detection and Assay HandbookDocument104 pagesQIAexpress Detection and Assay HandbookghadbaneNo ratings yet
- Fluorescent Immunoassay (Autosaved)Document13 pagesFluorescent Immunoassay (Autosaved)Matt McAndrew GarciaNo ratings yet
- Lesson 03 PDFDocument4 pagesLesson 03 PDFLaura B.No ratings yet
- Gen Micro Micro D&R AgamDocument157 pagesGen Micro Micro D&R AgamNirosha Arul100% (1)
- Promotie Toamna 1.09 - 01.11.2020Document1 pagePromotie Toamna 1.09 - 01.11.2020Maria BoldureanuNo ratings yet
- Immuno FluorescenceDocument2 pagesImmuno FluorescenceEstiak RonyNo ratings yet
- Fluorescence DyesDocument48 pagesFluorescence DyesJuan CubasNo ratings yet