Professional Documents
Culture Documents
Depresssion Student PCP - RK Comments - 2020
Depresssion Student PCP - RK Comments - 2020
Uploaded by
Bob Bob0 ratings0% found this document useful (0 votes)
4 views3 pages1) The patient is experiencing depression, insomnia, and forgetting things. He has been missing doses of his medication.
2) His symptoms have been present for a while and he needs counseling and lifestyle changes in addition to medication adjustments. Switching medications could help with side effects.
3) A referral should be made to assess for potential dementia given his symptoms of forgetting things for three years.
Original Description:
Original Title
Depresssion Student PCP_RK comments_2020(1)
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1) The patient is experiencing depression, insomnia, and forgetting things. He has been missing doses of his medication.
2) His symptoms have been present for a while and he needs counseling and lifestyle changes in addition to medication adjustments. Switching medications could help with side effects.
3) A referral should be made to assess for potential dementia given his symptoms of forgetting things for three years.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
4 views3 pagesDepresssion Student PCP - RK Comments - 2020
Depresssion Student PCP - RK Comments - 2020
Uploaded by
Bob Bob1) The patient is experiencing depression, insomnia, and forgetting things. He has been missing doses of his medication.
2) His symptoms have been present for a while and he needs counseling and lifestyle changes in addition to medication adjustments. Switching medications could help with side effects.
3) A referral should be made to assess for potential dementia given his symptoms of forgetting things for three years.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 3
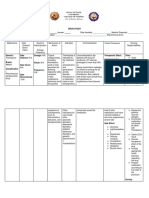
Print Name Student Number
Further Information Required Source of Information
How long exactly have these symptoms been happening? patient
Have you had psychosocial interventions yet Patient
Have you had any thoughts about harming yourself Patient
Have you been drinking – related to INR Patient
General Pharmaceutical Needs/Problems Assessment Action Monitoring
Special Needs: (e.g. visual, learning, auditory disabilities or problems Yes Patient is forgetting to take his Give patient his medication in a Ask the patient if they think it
with dexterity)
No medication NOMAD tray could help
Problems: (e.g. practical supply problems)
Condition/ Aims Assessment A Action (including patient counselling points) Monitoring/
Problem P Follow up
N
depression Manage Aim not being met, A Patient needs to be offered CBT and physical activity normally see them after 2 weeks.
depression patient is starting programmes. His symptoms have been present for a while so See them regularly thereafter, for
according to sertraline, unclear sertraline is a suitable first line treatment, although it example at intervals of 2 to 4
guidance whether hes had CBT. interacts with warfarin, increasing bleeding risk. weeks in the first 3 months, and
Warfarin and sertraline then at longer intervals if response
interact NICE recommends patients on warfarin start taking is good.
mirtazapine – cautioned for use in elderly as increases risk of
falls, that this patient suffers with. There is a major Monitor closely for increased risk
advantage, mirtazapine can make patients sleepy, but this of falls
patient suffers from insomnia so taking mirtazapine will help
with that
A = actual problem, P = potential problem, N = no problem
Not taking his Improve Aim not being met, A Consider giving patient NOMAD tray to improve adherence to Speak to patient next time after
medication/me patients patient is missing doses his medication. Discuss with the patient whether that’s giving NOMAD and see if
dicines adherence of his medication something they think would help adherence has improved
optimisation
Medicine optimisation can also help, the patient hasn’t been
taking his medications. Explore if the patient needs the senna
and oxybutynin, if he doesn’t need them, we can reduce pill
burden, as well as reducing antimuscarinic burden on the
patient, reducing the risk of falls.
Forgetting Manage Aim not being met, Y Patient must be investigated for dementia, as he has been Write to GP and ask for referral to
things patients patient isn’t on any forgetting things since his wifes fall three years ago AD services
symptoms medication
At the initial assessment take a history (including cognitive,
behavioural and psychological symptoms, and the impact
symptoms have on their daily life):
• from the person with suspected dementia and
• if possible, from someone who knows the person well (such as
a family member).
1.2.2 If dementia is still suspected after initial assessment:
• conduct a physical examination and
• undertake appropriate blood and urine tests to exclude
reversible causes of cognitive decline and
• use cognitive testing.
insomnia Help patient Aim not being met y Counsel patient on sleep hygiene Ask patient if sleep improves next
to sleep Offer people with depression advice on sleep hygiene if time he comes to pharmacy
better needed, including:
• establishing regular sleep and wake times
• avoiding excess eating, smoking or drinking alcohol before
sleep
• creating a proper environment for sleep
• taking regular physical exercise.
A = actual problem, P = potential problem, N = no problem
Y Y Y
Legal Problems? Clinical Problems? Will you dispense prescription?
Clinical Check N N
of Prescription N N N
N
Comments Comments Comments
Mirtazapine may be a better option for this patient Discuss the option of switching to mirtazapine
with the prescriber
A = actual problem, P = potential problem, N = no problem
You might also like
- Concept Map - BipolarDocument1 pageConcept Map - BipolarbacnatjoyNo ratings yet
- Risk Assessment For Cross-Contamination in Solid Dosage Form Manufacturing FacilitiesDocument5 pagesRisk Assessment For Cross-Contamination in Solid Dosage Form Manufacturing Facilitiesanandhra2010No ratings yet
- Pre Reg Pharmacists Last MinuteDocument9 pagesPre Reg Pharmacists Last MinuteBob BobNo ratings yet
- The List of Health Conditions or Problems Ranked According To Priorities: Problem Score 4Document25 pagesThe List of Health Conditions or Problems Ranked According To Priorities: Problem Score 4Sytrose Morales100% (2)
- Case 1:: Rule in Rule OutDocument7 pagesCase 1:: Rule in Rule OutAnn CruzNo ratings yet
- NCP Modified Radical MastectomyDocument5 pagesNCP Modified Radical MastectomyIvan Jules P. PALMARESNo ratings yet
- Case Study 6Document4 pagesCase Study 6Mary Hope Bacuta0% (2)
- NCM 105 RLE Case 2Document8 pagesNCM 105 RLE Case 2Maria Charis Anne IndananNo ratings yet
- Nursing Care Plan Assessment Diagnosis Inference Planning Interventio N Rationale EvaluationDocument3 pagesNursing Care Plan Assessment Diagnosis Inference Planning Interventio N Rationale EvaluationDianne100% (2)
- Nursing Care Plan - AnxietyDocument1 pageNursing Care Plan - AnxietyPauPau100% (2)
- Specialties in Pharmacy Practice: Functions & ResponsibilitiesDocument31 pagesSpecialties in Pharmacy Practice: Functions & ResponsibilitiesJessica Denise0% (1)
- Legal Opinion Letter CBD Sold Nationwide Final August 21, 2018Document33 pagesLegal Opinion Letter CBD Sold Nationwide Final August 21, 2018Robert KossackNo ratings yet
- Kathryn Kiser (Eds.) - Oral Anticoagulation Therapy - Cases and Clinical Correlation-Springer International Publishing (2017) PDFDocument293 pagesKathryn Kiser (Eds.) - Oral Anticoagulation Therapy - Cases and Clinical Correlation-Springer International Publishing (2017) PDFAdharaaNo ratings yet
- Gap Analysis Report District Hospital HardoiDocument58 pagesGap Analysis Report District Hospital HardoiDr. Sachendra Raj100% (3)
- Nursing Care PlanDocument3 pagesNursing Care PlanMeryl MarcosNo ratings yet
- ADN Care Plan - DepressionDocument3 pagesADN Care Plan - DepressionDavid PerezNo ratings yet
- Concept Map Mental HealthDocument2 pagesConcept Map Mental HealthRhina FutrellNo ratings yet
- Potential Complications:: Ruston Et Al., 2013)Document11 pagesPotential Complications:: Ruston Et Al., 2013)brianNo ratings yet
- Material, Vincent M. (NCP Seizure, Head Trauma, CVA)Document33 pagesMaterial, Vincent M. (NCP Seizure, Head Trauma, CVA)vincent materialNo ratings yet
- Ch071 - 001-007 Migraine HeadacheDocument7 pagesCh071 - 001-007 Migraine Headached_94100% (1)
- Choosing AntidepressantDocument4 pagesChoosing AntidepressantJorge Luis Ángeles VelázquezNo ratings yet
- Qst. Paul University Philippines: School of Nursing and Allied Health Sciences College of NursingDocument5 pagesQst. Paul University Philippines: School of Nursing and Allied Health Sciences College of NursingChristian UmosoNo ratings yet
- Jall Jsot Dap PresentationDocument13 pagesJall Jsot Dap Presentationapi-383172592No ratings yet
- NCPDocument6 pagesNCPBon BonNo ratings yet
- Assessment Nursing Diagnosis Nursing Inference Nursing Goal Nursing Interventions EvaluationDocument4 pagesAssessment Nursing Diagnosis Nursing Inference Nursing Goal Nursing Interventions EvaluationtrishxianieNo ratings yet
- PASSMEDICINE MCQs-PSYCHIATRYDocument33 pagesPASSMEDICINE MCQs-PSYCHIATRYghanijamali79No ratings yet
- University of The CordillerasDocument10 pagesUniversity of The CordillerasLalyn BalasbasNo ratings yet
- Doctor'S Order Date Order Implications ImplicationsDocument2 pagesDoctor'S Order Date Order Implications ImplicationsGan BangNo ratings yet
- BZD TaperDocument2 pagesBZD TaperEduardo AguilarNo ratings yet
- Lampe 2013 Aus Prescriber Drug Treatment AnxietyDocument4 pagesLampe 2013 Aus Prescriber Drug Treatment Anxietyana01210761809No ratings yet
- DepressionDocument24 pagesDepressionIoana VoinaNo ratings yet
- Antidepressant Fact SheetDocument4 pagesAntidepressant Fact Sheetcecile pieNo ratings yet
- Cu7 - Pain 1Document18 pagesCu7 - Pain 1FERMIL PASGALANo ratings yet
- 1-4 Post-Lecture Activity: Ito Ang NURSING MODEL para Sa Yo!Document2 pages1-4 Post-Lecture Activity: Ito Ang NURSING MODEL para Sa Yo!Darwin AndalNo ratings yet
- Pathology of Anxiety Disorders and Identified Signs and SymptomsDocument8 pagesPathology of Anxiety Disorders and Identified Signs and SymptomsChristian Paul ReyesNo ratings yet
- PRIETO - Antipsychotic Drug 3Document4 pagesPRIETO - Antipsychotic Drug 3Stiffany PrietoNo ratings yet
- College of Health Sciences: University of Southern MindanaoDocument2 pagesCollege of Health Sciences: University of Southern MindanaoKervy JuntillaNo ratings yet
- 5219-PRP Support Tool CounsellingDocument10 pages5219-PRP Support Tool CounsellingRodhi AnshariNo ratings yet
- Psych Careplan For PaperDocument18 pagesPsych Careplan For PaperUSMCDOC100% (2)
- GRPD SomaticNCP-1Document2 pagesGRPD SomaticNCP-1Macmac GalabacNo ratings yet
- Psych-Midterm ReviewerDocument12 pagesPsych-Midterm ReviewerPia Rose RoqueNo ratings yet
- Nursing Care Plan: Subjective Cues: Goal/objectiveDocument2 pagesNursing Care Plan: Subjective Cues: Goal/objectiveNikka PelayoNo ratings yet
- 114-116 SavithaDocument3 pages114-116 Savithamavriska.chairunnisaNo ratings yet
- NURSINGCAREPLANDocument5 pagesNURSINGCAREPLANJulius AtencioNo ratings yet
- Disturbed Thought Processes DescribeDocument2 pagesDisturbed Thought Processes DescribePRINCESS LARA CASILAONo ratings yet
- Sample #1 Sample #2 Sample #3: Genre AnalysisDocument4 pagesSample #1 Sample #2 Sample #3: Genre Analysis2bsktccgxyNo ratings yet
- Evaluasi Dan Profilaksis Terapi MigrainDocument53 pagesEvaluasi Dan Profilaksis Terapi Migrainnesya_fanniaNo ratings yet
- DepressionDocument9 pagesDepressionFJ GatdulaNo ratings yet
- Huntingtons Disease NCPDocument4 pagesHuntingtons Disease NCPJerich Mark SalasNo ratings yet
- Module 1a - Nursing ProcessDocument22 pagesModule 1a - Nursing ProcessNathaniel PulidoNo ratings yet
- PsycheDocument4 pagesPsycheclaudine padillonNo ratings yet
- CaseDocument3 pagesCasebLessy_july16No ratings yet
- CP-Rheumatic Heart Disease LandscapeDocument13 pagesCP-Rheumatic Heart Disease Landscapedecebelle alabaNo ratings yet
- The Naturalistic Course of Major Depression N The Absence of Somatic TherapyDocument6 pagesThe Naturalistic Course of Major Depression N The Absence of Somatic TherapyCarlos CostaNo ratings yet
- TB NCPDocument1 pageTB NCPPatricia JuatNo ratings yet
- DepressionDocument47 pagesDepressionJean Pierre FakhouryNo ratings yet
- 121 Full PDFDocument6 pages121 Full PDFMatheus SilvaNo ratings yet
- Assessment Diagnosis Scientific Background Planning Implementation Rationale EvaluationDocument2 pagesAssessment Diagnosis Scientific Background Planning Implementation Rationale EvaluationREOLALAS, Mariane JoyNo ratings yet
- Quizz ClinicDocument3 pagesQuizz ClinicKia MadineNo ratings yet
- Nursing Care Plan: Angeles University Foundation College of NursingDocument2 pagesNursing Care Plan: Angeles University Foundation College of NursingRey Ann PangilinanNo ratings yet
- Nursing Care Plan #1 Mental HealthDocument13 pagesNursing Care Plan #1 Mental HealthNursyNurseNo ratings yet
- NCP 2Document7 pagesNCP 2Janina Kirsten DevezaNo ratings yet
- The STAR D Study: Treating Depression in The Real World: Interpreting Key TrialsDocument10 pagesThe STAR D Study: Treating Depression in The Real World: Interpreting Key TrialsPaula Vergara MenesesNo ratings yet
- Print 10Document4 pagesPrint 10FARAH MOHAMMEDNo ratings yet
- Treating PTSD During The COVID-19 Virus OutbreakDocument50 pagesTreating PTSD During The COVID-19 Virus OutbreakmniosoNo ratings yet
- Doac PCP Week 8 Answer 4Document6 pagesDoac PCP Week 8 Answer 4Bob BobNo ratings yet
- Apixaban PCP Answer 2Document4 pagesApixaban PCP Answer 2Bob BobNo ratings yet
- Romeo FakeDocument1 pageRomeo FakeBob BobNo ratings yet
- DexamethasoneDocument3 pagesDexamethasoneWina Siska Purnama BurmanNo ratings yet
- Business Mumbai Mba Pharma Curriculum PDFDocument4 pagesBusiness Mumbai Mba Pharma Curriculum PDFTech WizardNo ratings yet
- DR - Khan Clinical Pharmacy OrientationDocument55 pagesDR - Khan Clinical Pharmacy OrientationIram CHNo ratings yet
- Subject 4. - Product Design OCW PDFDocument33 pagesSubject 4. - Product Design OCW PDFJose Luis BarradasNo ratings yet
- Zakiyatul Mahmudah-1Document2 pagesZakiyatul Mahmudah-1beauty asriNo ratings yet
- Evaluation of Validation Content Uniformity Test Results Using Lower Probability Bound Distribution ChartsDocument77 pagesEvaluation of Validation Content Uniformity Test Results Using Lower Probability Bound Distribution ChartssakurabaNo ratings yet
- Pediatrics Intensive Care Unit: Presented By: Ms. Sandeep KaurDocument52 pagesPediatrics Intensive Care Unit: Presented By: Ms. Sandeep KaurArchanaNo ratings yet
- Cardiac Drugs 2nd Edition 2015 PDFDocument550 pagesCardiac Drugs 2nd Edition 2015 PDFditairinaNo ratings yet
- Quiz 5Document28 pagesQuiz 5YNo ratings yet
- FTX TB Annex D - Pers Kit ListDocument2 pagesFTX TB Annex D - Pers Kit ListBrodie MooreNo ratings yet
- Ma Huang (Ephedrae Herba) : Setting The Record StraightDocument14 pagesMa Huang (Ephedrae Herba) : Setting The Record StraightInfohoggNo ratings yet
- Watan Qassim Pharmaceutical Manufacturing Plant Saudi Arabia - Profile - 070222Document5 pagesWatan Qassim Pharmaceutical Manufacturing Plant Saudi Arabia - Profile - 070222salman KhanNo ratings yet
- Methods For Isolation of Marine-Derived Endophytic Fungi and Their Bioactive Secondary ProductsDocument12 pagesMethods For Isolation of Marine-Derived Endophytic Fungi and Their Bioactive Secondary ProductsIswan NadiarNo ratings yet
- Reduction Cost ManufactureDocument21 pagesReduction Cost ManufactureAnonymous d1Cgf1n9INo ratings yet
- Undangan Sepsis 24 Nov 2018 1st AnnDocument2 pagesUndangan Sepsis 24 Nov 2018 1st AnnAtik Marfu'ahNo ratings yet
- Fludarabine PhosphateDocument3 pagesFludarabine PhosphateMulayam Singh YadavNo ratings yet
- JIMENEZKaycelyn-Drus StudyDocument11 pagesJIMENEZKaycelyn-Drus Studykaycelyn jimenezNo ratings yet
- RVS JournalDocument39 pagesRVS JournalZikuyNo ratings yet
- Exhibit 1 18 Presents Common Size Income Statements and Balance Sheets ForDocument1 pageExhibit 1 18 Presents Common Size Income Statements and Balance Sheets ForTaimur TechnologistNo ratings yet
- Top 20 Chemists in Churchgate, Mumbai - Best Medical Drug Stores - JustdialDocument7 pagesTop 20 Chemists in Churchgate, Mumbai - Best Medical Drug Stores - JustdialTal subuNo ratings yet
- Thu Oc Chong Loann HipDocument36 pagesThu Oc Chong Loann HipBạch MãNo ratings yet
- Pharmacy 101Document48 pagesPharmacy 101api-381827675No ratings yet
- Ra 10918 BsaDocument19 pagesRa 10918 BsarimNo ratings yet
- 1794 Dmac15 PDFDocument8 pages1794 Dmac15 PDFSGPConsultoresNo ratings yet
- Compendial Approvals Usp36-Nf31Document18 pagesCompendial Approvals Usp36-Nf31Leopoldo AndradeNo ratings yet