Professional Documents
Culture Documents
Week 14 Drug Study
Week 14 Drug Study
Uploaded by
Cecilia Micole M. De GulaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Week 14 Drug Study
Week 14 Drug Study
Uploaded by
Cecilia Micole M. De GulaCopyright:
Available Formats
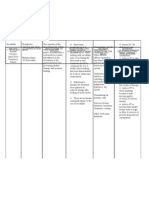
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
ALTRETAMINE Ovarian Cancer Altretamine has CNS: Paresthesias, Hypersensitivity to Monitor blood counts at
o Adult: PO 260 demonstrated hyporeflexia, muscle altretamine, severe bone least monthly and prior to
mg/m2/d for neoplastic activity in weakness, peripheral marrow depression, each course of therapy.
14 or 21 patients resistant to numbness, ataxia, neurologic toxicity, Perform a neurologic
examination regularly;
consecutive d alkylating agents. Parkinson-like tremors. pregnancy (category D),
question patient about the
in a 28-d cycle GI: Nausea, vomiting. lactation.
presence of: paresthesias,
Hematologic: hypoesthesias, muscle
Leukopenia, weakness, peripheral
thrombocytopenia. numbness, ataxia, decreased
Urogenital: Slight sensations, and alterations in
increase in serum mood or consciousness.
creatinine. Withhold medication if
Skin: Alopecia and neurologic symptoms fail to
eczema. resolve with dose reduction.
Notify physician.
Monitor for nausea and
vomiting, which are related
to the cumulative dose of
altretamine. After several
weeks some patients
develop tolerance to the GI
effects. Antiemetics may be
required to control GI
distress.
Taking altretamine after
meals or with food or milk
may decrease nausea.
Report symptoms indicative
of neurotoxicity to physician
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
BUSULFAN Chronic Myelogenous Causes cell death by Hematologic: Major Therapy-resistant chronic Monitor for therapeutic
Leukemia acting toxic effects are related lymphocytic leukemia; effectiveness: Normal
o Adult: PO 4–8 predominantly on to bone marrow failure; lymphoblastic crisis of leukocyte count is usually
slowly proliferating agranulocytosis (rare), chronic myelogenous achieved in about 2 mo.
mg/d until
Monitor the following: Vital
maximal stem cells by pancytopenia, leukemia; bone marrow signs, weight, I&O ratio and
clinical and inducing cross thrombocytopenia, depression, pattern. Urge patient to
hematologic linkage in DNA, thus leukopenia, anemia. immunizations (patient increase fluid intake to 10–
improvement, blocking replication. Urogenital: Flank pain, and household 12 [8 oz] glasses daily (if
allowed) to assure adequate
may use 1–4 Acquired resistance renal calculi, uric acid members), chickenpox
urinary output.
mg/d if may develop, nephropathy, acute (including recent Monitor for and report
remission is probably due to renal failure, exposure), herpetic symptoms suggestive of
shorter than 3 intracellular gynecomastia, testicular infections. Safety during superinfection, particularly
mo inactivation of atrophy, azoospermia, pregnancy (category D) when patient develops
o Child: PO 0.06– busulfan. impotence, sterility in or lactation is not leukopenia.
0.12 mg/kg/d males, ovarian established. Baseline Hgb, Hct, WBC with
or 1.8–4.6 suppression, menstrual differential, platelet count,
mg/m2 changes, amenorrhea liver function, kidney
(potentially irreversible), function, serum uric acid;
repeat at least weekly.
menopausal symptoms.
Avoid invasive procedures
Respiratory: Irreversible
during periods of platelet
pulmonary fibrosis count depression.
("busulfan lung"). Report to physician any of
Skin: Alopecia, the following: Easy bruising
hyperpigmentation. or bleeding, cloudy or pink
Other: Endocardial urine, dark or black stools;
fibrosis, dizziness, sore mouth or throat,
cholestatic jaundice, unusual fatigue, blurred
infections. vision, flank or joint pain,
swelling of lower legs and
feet; yellowing white of eye,
dark urine, light-colored
stools, abdominal
discomfort, or itching
(hepatotoxicity).
Use contraceptive measures
during busulfan therapy and
for at least 3 mo after drug is
withdrawn.
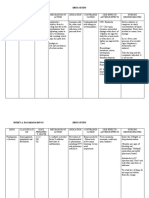
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
CARBOPLATIN Ovarian Cancer Full or partial Body as a Whole: History of severe Monitor closely during first
Adult: IV 360 mg/m2 activity against a Hypersensitivity reactions to carboplatin 15 min of infusion, since
once q4wk. May be variety of cancers reactions. or other platinum allergic reactions have
repeated when resulting in GI: Mild to moderate compounds, severe bone occurred within minutes of
neutrophil count is reduction or nausea and vomiting, marrow depression; carboplatin administration.
at least 2000 mm3 stabilization of anorexia, hypogeusia, significant bleeding; Baseline and periodic CBC
and platelet count is tumor size and dysgeusia, mucositis, impaired renal function; with differential, platelet
count, Hgb and Hct. Monitor
at least 100,000 useful in patients diarrhea, constipation, pregnancy (category D),
periodically kidney function
mm3. If neutrophil with impaired renal elevated liver enzymes. and lactation. with creatinine clearance
and platelet counts function, patients Hematologic: tests and serum electrolytes.
are lower, dose of unable to Thrombocytopenia, Monitor results of peripheral
carboplatin should accommodate high- leukopenia, blood counts. Median nadir
be reduced by 50– volume hydration, neutropenia, anemia. occurs at day 21. Leukopenia,
75% of initial dose. or patients at high Metabolic: Mild neutropenia, and
Alternatively, 400 risk for hyponatremia, thrombocytopenia are dose
mg/m2 as a 24-h neurotoxicity and/or hypomagnesemia, related and may produce
infusion for 2 ototoxicity. hypocalcemia, and dose-limiting toxicity.
Monitor for peripheral
consecutive d can be hypokalemia.
neuropathy (e.g.,
used CNS: Peripheral
paresthesias), ototoxicity,
neuropathy. and visual disturbances.
Head and Neck and Skin: Rash, alopecia. Monitor serum electrolyte
Small Cell Lung Cancer Special Senses: Tinnitus. studies, because carboplatin
o Adult: IV 300–400 Urogenital: has been associated with
mg/m2 q4wk Nephrotoxicity. decreases in sodium,
o Child: IV Up to 560 potassium, calcium, and
mg/m2 once q4wk magnesium. Special
or up to 175 mg/m2 precautions may be
warranted for patients on
q2wk. Other dosage
diuretic therapy.
regimens have been
used for specific
dosing protocols
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
CARMUSTINE Previously Untreated Drug metabolites Hematologic: Delayed History of pulmonary Monitor for nausea and
Patients—Carcinoma thought to be myelosuppression function impairment; vomiting (dose related), which
may occur within 2 h after drug
Adult: IV 150–200 mg/m2 responsible for (dose-related); recent illness with or administration and persist for up
q6wk in one dose or given antineoplastic thrombocytopenia. exposure to chickenpox to 6 h. Prior administration of an
over 2 d activities. Full or CNS: Dizziness, ataxia. or herpes zoster; antiemetic may help to decrease
Child: IV 200–250 mg/m2 partial activity Respiratory: Pulmonary infection, decreased or prevent these adverse effects.
Baseline CBC with differential
q4–6wk as single dose. against a variety of infiltration or fibrosis. circulating platelets,
and platelet count, repeat blood
Doses adjusted based on cancers resulting in Skin: Skin flushing and leukocytes, or studies following infusion at
hematologic parameter reduction or burning pain at injection erythrocytes; pregnancy weekly intervals for at least 6
wk. Baseline and periodic tests
stabilization of site, hyperpigmentation (category D), lactation. of hepatic and renal function.
tumor size and of skin (from contact). Platelet nadir usually occurs
increased survival Special Senses: (with within 4–5 wk, and leukocyte
rates. high doses) Eye nadir within 5–6 wk after
therapy is terminated.
infarctions, retinal
Thrombocytopenia may be more
hemorrhage, suffusion severe than leukopenia; anemia
of conjunctiva. is less severe.
GI: Stomatitis, nausea, Check temperature daily. Avoid
vomiting. use of rectal thermometer to
prevent injury to mucosa. An
elevation of 0.6° F or more
above usual temperature
warrants reporting.
Report symptoms of lung
toxicity (cough, shortness of
breath, fever) to the physician
immediately.
Be alert to signs of hepatic
toxicity (jaundice, dark urine,
pruritus, light-colored stools)
and renal insufficiency (dysuria,
oliguria, hematuria, swelling of
lower legs and feet.)
Report burning sensation
immediately, as carmustine can
cause burning discomfort even
in the absence of extravasation.
Infusion will be discontinued and
restarted in another site. Ice
application over the area may
decrease the discomfort.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
CLORAMBUCIL Malignant Diseases Lymphocytic effect Body as a Whole: Drug Hypersensitivity to Lab tests: CBC, Hgb, total and
is marked, thus it is fever, skin rashes, chlorambucil or to other differential leukocyte counts,
(Lymphomas, Hodgkin's
and serum uric acid initially and
Disease, etc.) effective in papilledema, alopecia, alkylating agents; at least once weekly during
o Adult: PO 0.1– treatment of various peripheral neuropathy, administration within 4 treatment.
0.2 mg/kg/d lymphomas. sterile cystitis, wk of a full course of Leukopenia usually develops
(usual dose 4– pulmonary radiation or after the third week of
treatment; it may continue for
10 mg/d) complications, seizures chemotherapy; full
o Child: PO 0.1– (high doses). dosage if bone marrow is up to 10 d after last dose, then
GI: Low incidence of infiltrated with rapidly return to normal.
0.2 mg/kg/d in
Avoid or reduce to minimum
single or divided gastric discomfort, lymphomatous tissue or injections and other invasive
doses hepatotoxicity. is hypoplastic; smallpox procedures (e.g., rectal
Hematologic: Bone and other vaccines; temperatures, enemas) when
marrow depression: pregnancy (category D), platelet count is low because of
danger of bleeding.
leukopenia, lactation.
Monitor for S&S of skin rashes,
thrombocytopenia, which are rare, but appear to
anemia. show a consistent pattern:
Metabolic: Sterility, pustular eruption on mouth,
hyperuricemia. chin, cheeks; urticarial erythema
on trunk that spreads to legs.
The rash occurs early in
treatment period and lasts
about 10 d after last dose.
Keep appointments with
physician. During treatment it is
dangerous to go longer than 2
wk without a clinical
examination and blood studies.
Notify physician if the following
symptoms occur: unusual
bleeding or bruising, sores on
lips or in mouth; flank, stomach,
or joint pain; fever, chills, or
other signs of infection, sore
throat, cough, dyspnea.
Drink at least 10–12 glasses (240
mL [8 oz] each) of fluid per day,
if not contraindicated, and
report to physician if urine
output decreases below normal
amounts.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
AZACITIDINE Myelodysplastic The cytotoxic effects Body as a Whole: Known hypersensitivity Monitor for S&S of drug
Syndrome of azacitidine cause Fever, fatigue, to azacitidine or toxicity in those with renal
o Adult : SC 75 the death of rapidly malaise, weakness, mannitol; advanced insufficiency.
dividing cancer cells asthenia, limb pain, malignant hepatic
mg/m2 once Lab tests: Obtain LFTs and
back pain ,
daily for 7 d that are no longer tumors, myelodysplastic serum creatinine before
lymphadenopathy,
every 4 wk; may responsive to hematoma, night
syndrome with hepatic initiation of therapy;
increase to 100 normal growth impairment; vaccination; monitor CBC with
mg/m2 if no control sweats, cellulitis, active infection; dental differential before each
beneficial mechanisms. lethargy. work; intramuscular treatment cycle and prn.
response is seen CNS: Dizziness, injections, if platelets Withhold drug & notify
after 2 headache, depression, <50,000 mm3; pregnancy physician for S&S of
syncope.
treatment (category D), lactation. hepatic or renal
CV: Chest pain, cardiac
cycles and no Safety and efficacy in insufficiency; lab values
murmur, tachycardia,
toxicity other hypotension. children have not been that indicate leukopenia,
than nausea and GI: Nausea, vomiting, established. neutropenia,
vomiting has diarrhea, constipation, thrombocytopenia, or
occurred anorexia, weight loss, hepatic or renal
abdominal pain, insufficiency; or serum
stomatitis, dyspepsia. bicarbonate levels less
Hematologic: Anemia, than 20 mEq/L.
thrombocytopenia, Promptly report S&S of
leukopenia,
infection or indication of
neutropenia,
ecchymosis, febrile
unusual bleeding
neutropenia . tendencies (e.g., dark,
Metabolic: Peripheral tarry stools and easy
edema . bruising).
Musculoskeletal: Women should avoid
Myalgia, arthralgia , becoming pregnant and
muscle cramps. men should not father a
Respiratory: Cough, child while taking this
dyspnea, pharyngitis, drug.
nasopharyngitis,
pneumonia ,
wheezing, pleural
effusion, rhonchi.
Skin: Injection site
erythema, injection
site reactions, rash,
pruritus, sweating ,
urticaria.
Urogenital: Dysuria,
urinary tract infection
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
FLUOROURACIL Carcinoma Highly toxic, CNS: Euphoria, acute Poor nutritional status; Obtain total and differential
[5- especially to cerebellar syndrome; myelosuppression. Safety leukocyte counts before each
Adult: IV 12
pustular contact dose is administered.
FLUOROURACIL mg/kg/d for 4 proliferative cells in during pregnancy Discontinue drug if leukopenia
(5-FU)] neoplasms, bone hypersensitivity. (category D) or lactation
consecutive days up occurs (WBC <3500/mm3) or if
CV: Cardiotoxicity
to 800 mg or until marrow, and is not established. patient develops
(rare), angina. thrombocytopenia (platelet
toxicity develops or intestinal mucosa.
GI: Anorexia, nausea, count <100,000/mm3). Baseline
12 d therapy, may Low therapeutic vomiting, stomatitis, and periodic checks of Hct and
repeat at 1 mo index with high esophagopharyngitis, liver and kidney function are
intervals; if toxicity potential for severe medicinal taste, also advised.
occurs, 15 mg/kg hematologic diarrhea, proctitis. Use protective isolation of
toxicity. patient during leukopenic period
once weekly can be Hematologic: Anemia,
(WBC <3500/mm3).
given until toxicity leukopenia,
Watch for and report signs of
subsides thrombocytopenia, abnormal bleeding from any
eosinophilia. source during thrombocytopenic
Body as a Whole: period (day 7–17); inspect skin
Actinic and Solar
Hypersensitivity: for ecchymotic and petechial
Keratosis Pustular contact areas. Protect patient from
Adult: Topical Apply eruption, edema of trauma.
cream or solution face, eyes, tongue, Report disorientation or
b.i.d. for 2–4 wk; legs. confusion; drug should be
withdrawn immediately.
apply Carac once Skin: SLE-like
Establish a reference data base
daily dermatitis, alopecia, for body weight, I&O ratio and
photosensitivity, pattern, food preferences and
Superficial Basal Cell erythema, increased dietary habits, bowel habits, and
Carcinoma pigmentation, skin condition of mouth.
dryness and fissuring, Report intractable vomiting to
Adult: Topical Apply physician.
pruritic
5% cream b.i.d. for maculopapular rash. Inspect patient's mouth daily.
3–6 wk [Topical] Local pain, Promptly report cracked lips,
xerostomia, white patches, and
pruritus,
erythema of buccal membranes.
hyperpigmentation,
burning at site of Report development of
maculopapular rash; it usually
application, responds to symptomatic
dermatitis, treatment and is reversible.
suppuration, swelling, Systemic toxicity may follow use
scarring, toxic of topical drug on large
granulation. ulcerated area. Report
symptoms promptly.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
6- Leukemias Delayed GI: Stomatitis, Prior resistance to Monitor CBC with differential,
MERCAPTOPURINE immunosuppressive mercaptopurine; first platelet count, Hgb, Hct, and
o Adult/Child: PO esophagitis,
liver functions closely.
Loading Dose properties and anorexia, nausea, trimester of pregnancy Monitor for S&S of liver damage.
2.5 mg/kg/d, carcinogenic vomiting, diarrhea, (category D); lactation; Hepatic toxicity occurs most
may increase potential. intestinal infections. often when dose exceeds 2.5
up to 5 ulcerations, mg/kg/d. Jaundice signals onset
of hepatic toxicity and may
mg/kg/d after impaired liver
necessitate terminating use.
4 wk if needed function, hepatic Withhold drug and notify
PO necrosis. physician at the first sign of an
Maintenance Hematologic: abnormally large or rapid fall in
Leukopenia, anemia, platelet and leukocyte counts.
Dose 1.25–2.5
Record baseline data related to
mg/kg/d eosinophilia, I&O ratio and pattern and body
pancytopenia, weight.
thrombocytopenia, Check vital signs daily. Report
abnormal bleeding, febrile states promptly.
Protect patient from exposure to
bone marrow
trauma, infections, or other
hypoplasia. stresses (restrict visitors and
Urogenital: personnel who have colds)
Hyperuricemia, during periods of leukopenia.
oliguria, renal Report nausea, vomiting, or
diarrhea. These may signal
impairment. excessive dosage, especially in
Skin: Rash. adults.
Body as a Whole: Watch for signs of abnormal
Drug fever. bleeding (ecchymoses,
petechiae, melena, bleeding
gums) if thrombocytopenia
develops; report immediately.
Increase hydration (10–12
glasses of fluid daily) to reduce
risk of hyperuricemia. Consult
physician about desirable
volume.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
CAPECITABINE Breast Cancer, Colorectal Reduces or Body as a Whole: Hypersensitivity to Monitor periodically CBC
Cancer stabilizes tumor size Fatigue, pyrexia, capecitabine, with differential and liver
o Adult: PO in metastatic breast pain, myalgia. CV: doxifluridine, 5-FU; functions including bilirubin,
2500 cancer. Metastatic Edema. myelosuppression; transaminases, alkaline
breast cancer dihydropyrimidine phosphatase.
mg/m2/d in 2 GI: Severe diarrhea,
Monitor carefully for S&S of
divided doses refractory to other nausea, vomiting, dehydrogenase (DPD)
grade 2 or greater toxicity:
times 2 wk, treatments, stomatitis, deficiency; females of diarrhea >4 BMs/day or at
then 1 wk off. colorectal cancer, abdominal pain, childbearing age; active night; vomiting >1 time/24 h;
Repeat single-agent constipation, infection; jaundice; significant loss of appetite or
adjuvant therapy for dyspepsia, anorexia. severe renal failure or anorexia; stomatitis; hand-
Renal Impairment colon cancer after Hematologic: impairment; pregnancy and-foot syndrome (pain,
o Clcr 30–50 surgery. Neutropenia, (category D); lactation, swelling, erythema,
mL/min thrombocytopenia, children <18 y. desquamation, blistering);
reduce dose anemia, temperature = 100.5° F; and
S&S of infection.
by 25%, <30 lymphopenia .
Withhold drug and
mL/min do Metabolic: immediately report S&S of
not use Dehydration, grade 2 or greater toxicity.
hyperbilirubinemia. Monitor for dehydration and
CNS: Paresthesias, replace fluids as needed.
headache, dizziness, Monitor carefully patients
insomnia. with coronary artery disease
Skin: Hand-and-foot for S&S of cardiotoxicity (e.g.,
syndrome, increasing angina).
dermatitis, nail
disorder.
Special Senses: Eye
irritation.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
CLADRIBINE Hairy Cell Leukemia Cladribine is CNS: Headache, Hypersensitivity to Monitor vital signs during
Adult: IV 0.09 cytotoxic to both dizziness. cladribine; pregnancy and after drug infusion. Fever
mg/kg/d by 7 d actively dividing and GI: Nausea, (category D). (>100° F) is common during
quiescent Use cautiously on the 5th to 7th day in patients
continuous infusion diarrhea.
with hairy cell leukemia, and
lymphocytes and Hematologic: patients with hepatic or
severe fever (>104° F) may
Chronic Lymphocytic monocytes, Myelosuppression renal impairment. develop within the first
Leukemia inhibiting both DNA (neutropenia), Safety and efficacy in month of therapy.
Adult: IV 0.1 mg/kg/d synthesis and repair. anemia, children not established. Lab tests: Frequent
by 7 d continuous thrombocytopenia. hematologic studies; periodic
infusion or 0.028– Metabolic: Fever. serum creatinine and liver
0.14 mg/kg/d as 2 h CNS: Headache, function tests.
infusion for 5 dizziness. Closely monitor hematologic
consecutive d status; myelosuppression is
Urogenital: Elevated
common during the first
serum creatinine. month after starting therapy.
Monitor for and report S&S
of infection. Note that within
the first month, fever may
occur in the absence of
infection.
With high doses of cladribine,
monitor for neurologic
toxicity
(paraparesis/quadriparesis)
and acute nephrotoxicity.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
CLOFARABINE Acute Lymphocytic Cytotoxic to rapidly CNS: Anxiety, depression, Pregnancy (category Monitor vital signs frequently
Leukemia proliferating and dizziness, headache, D); lactation. during infusion of
o Adolescent/Child: quiescent cancer irritability, somnolence. Use Cautiously in clofarabine.
cells. CV: Tachycardia, Monitor closely for S&S of
IV 52 mg/m2/d patients with Renal
pericardial infusion, left capillary leak syndrome or
over 2 h for 5 d or hepatic function
ventricular systolic systemic inflammatory
dysfunction (LSVT). impairment, response syndrome (e.g.,
GI: Vomiting, nausea, and thrombocytopenia, tachypnea, tachycardia,
diarrhea, abdominal pain, neutropenia hypotension, pulmonary
constipation. edema). If either is
Hematologic/Lymphatic: suspected, immediately DC
Anemia, leukopenia, IV, institute supportive
thrombocytopenia, measures and notify
neutropenia, febrile physician.
neutropenia. Monitor I&O rates and
Hepatic: Jaundice, pattern and watch for S&S of
hepatomegaly. Metabolic: dehydration, including
Anorexia, decreased dizziness, lightheadedness,
appetite, edema, fainting spells, or decreased
decreased weight. urine output.
Musculoskeletal: Withhold drug and notify
Arthralgia, back pain, physician if hypotension
myalgia. develops for any reason
Respiratory: Cough, during 5-d period of drug
dyspnea, epistaxis, pleural administration.
effusion, respiratory Baseline and periodic CBC
distress. and platelet counts (more
Skin: Dermatitis, frequent with cytopenias);
contusion, dry skin, frequent LFTs and kidney
erythema, palmar-plantar function test during the 5 d
erythrodysesthesia of clofarabine therapy.
syndrome, pruritus.
Body as a Whole: Increase
risk of infection.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
IRINOTECAN Metastatic Carcinoma By inhibiting Body as a Whole: Previous hypersensitivity Monitor WBC with
o Adult: IV 125 topoisomerase I, Asthenia, fever, pain, to irinotecan, topotecan, differential, Hgb, and platelet
mg/m2 once irinotecan and its chills, edema, or other camptothecin count before each dose;
weekly for 4 wk, active metabolite abdominal analogs; acute infection, monitor closely coagulation
then a 2-wk rest enlargement, back parameters especially with
SN-38 cause double- diarrhea, pregnancy
period (future pain. concurrent use of other
stranded DNA (category D), lactation. drugs which affect these
courses may be CNS: Headache,
adjusted to range damage during the insomnia, dizziness. parameters.
from 50 to 150 synthesis (S) phase CV: Monitor fluid and electrolyte
mg/m2 of DNA. This inhibits Vasodilation/flushing. balance closely during and
depending on both DNA and RNA GI: Diarrhea (early and after periods of diarrhea.
tolerance; see synthesis. late onset), Monitor liver and renal
complete dehydration, nausea, function tests and blood
prescribing vomiting, anorexia, glucose periodically.
information for weight loss, Monitor for acute GI distress,
specific dosage constipation, especially early diarrhea
adjustment abdominal cramping (within 24 h of infusion),
recommendations and pain, flatulence, which may be preceded by
based on toxic stomatitis, dyspepsia, diaphoresis and cramping,
effects) increased alkaline and late diarrhea (>24 h after
phosphatase and AST. infusion).
Hematologic: Notify physician immediately
Leukopenia, when you experience
neutropenia, anemia. diarrhea, vomiting, and S&S
Respiratory: Dyspnea, of infection. Diarrhea
cough, rhinitis. requires prompt treatment
Skin: Alopecia, to prevent serious fluid and
sweating, rash. electrolyte imbalances.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
TOPOTECAN Metastatic Ovarian Permits uncoiling Body as a Whole: Previous hypersensitivity Lab tests: Obtain CBC
Cancer and Small Cell but prevents Asthenia, fever, to topotecan, irinotecan, counts with differential
Lung Cancer recoiling of the two fatigue. or other camptothecin frequently; periodically
o Adult: IV 1.5 strands of DNA, GI: Nausea, analogs; acute infection; monitor ALT.
mg/m2 daily for resulting in a vomiting, diarrhea, pregnancy (category D), Assess for GI distress,
5 d starting on permanent break in constipation, lactation. respiratory distress,
day 1 of a 21 d the DNA strands. abdominal pain, neurosensory symptoms,
course. Four stomatitis, anorexia, and S&S of infection
courses of transient elevations throughout therapy.
therapy in liver function Learn common adverse
recommended. tests. effects and measures to
Subsequent Hematologic: control or minimize when
doses can be Leukopenia, possible. Immediately
adjusted by 0.25 neutropenia , report any distressing
mg/m2 anemia, adverse effects to
depending on thrombocytopenia. physician.
toxicity Respiratory: Avoid pregnancy during
Dyspnea. therapy.
Skin: Alopecia.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
ETOPOSIDE Testicular Carcinoma Antineoplastic effect Body as a Whole: Severe bone marrow Check IV site during and after
Adult: IV 50–100 is due to its ability Hypersensitivity depression; severe infusion. Extravasation can
mg/m2/d for 5 to arrest mitosis (sweating, chills, hepatic or renal cause thrombophlebitis and
(cell division). fever, coryza, impairment; existing or necrosis.
consecutive days
Be prepared to treat an
q3–4wk for 3–4 Treatment of tachycardia; throat, recent viral infection,
anaphylactoid reaction. Stop
courses or 100 refractory testicular back and general bacterial infection;
infusion immediately if the
mg/m2 on days 1, 3, neoplasms, in body pain; intraperitoneal, reaction occurs.
and 5 q3–4wk for 3– patients who have abdominal cramps, intrapleural, or Monitor vital signs during
4 courses PO Twice already received flushing, substernal intrathecal and after infusion. Stop
the IV dose rounded appropriate surgical, chest pain, dyspnea, administration. Safety infusion immediately if
to the nearest 50 chemotherapeutic, bronchospasm, during pregnancy hypotension occurs.
mg and radiation pulmonary edema, (category D), lactation, or Lab tests: Perform baseline
therapy; for anaphylactoid in children is not all prior to and at regular
Small Cell Lung treatment of reaction). established. intervals during therapy, and
Carcinoma choriocarcinoma in CNS: Peripheral before each subsequent
treatment course. Tests
Adult: IV 35 women and small neuropathy,
include: CBC with differential;
mg/m2/d for 4 cell carcinoma of paresthesias, liver and kidney function
consecutive days to the lung. weakness, tests (AST, ALT, serum
50 mg/m2/d for 5 somnolence, bilirubin, LDH, BUN, serum
consecutive days unusual tiredness, creatinine).
q3–4wk PO Twice transient confusion. Withhold therapy when an
the IV dose rounded CV: Transient absolute neutrophil count is
to the nearest 50 hypotension; below 500/mm3 or a platelet
mg thrombophlebitis count below 50,000/mm3.
with extravasation. Make position changes
slowly, particularly from lying
GI: Nausea,
to upright position because
vomiting, dyspepsia, transient hypotension after
anorexia, diarrhea, therapy is possible.
constipation, Inspect mouth daily for
stomatitis. ulcerations and bleeding.
Hematologic: Avoid obvious irritants such
Leukopenia, as hot or spicy foods,
thrombocytopenia, smoking, alcohol.
severe Be alert to evidence of
patient complaints that
myelosuppression,
might suggest development
anemia,
of leukopenia, infection
pancytopenia, (immunosuppression), and
neutropenia. bleeding.
Respiratory: Pleural Protect patient from any
effusion, trauma that might
bronchospasm. precipitate bleeding during
Skin: Reversible period of platelet nadir
alopecia (can particularly. Withhold
progress to total invasive procedures if
possible.
baldness); radiation
recall dermatitis;
necrosis, pain at IV
site.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
MITOXANTRONE Combination Therapy Highly destructive to CV: Arrhythmias, Hypersensitivity to Monitor IV insertion site.
for ANLL rapidly proliferating decreased left mitoxantrone; Transient blue skin
Adult: IV Induction cells in all stages of ventricular function, myelosuppression; discoloration may occur at
cell division. In CHF, tachycardia, pregnancy (category D), site if extravasation has
Therapy: 12
occurred.
mg/m2/d on days 1– combination with ECG changes, MI lactation.
Monitor cardiac functioning
3, may need to other drugs for the (occurs with throughout course of
repeat induction treatment of acute cumulative doses of therapy; report signs and
course. IV nonlymphocytic >80–100 mg/m2), symptoms of CHF or cardiac
Consolidation leukemia (ANLL) in edema, increased arrhythmias.
Therapy: 12 mg/m2 adults, bone pain in risk of Lab tests: Perform liver
on days 1 and 2 advanced prostate cardiotoxicity. function tests prior to and
(max: lifetime dose cancer. Reducing GI: Nausea, during course of treatment.
80–120 mg/m2) neurologic disability vomiting, diarrhea, Monitor serum uric acid
and/or the hepatotoxicity. levels and initiate
Child: IV 8–33
hypouricemic therapy before
mg/m2 q3–4wk frequency of clinical Hematologic:
antileukemic therapy.
relapses in patients Leukopenia, Monitor carefully CBC with
Solid Tumors with secondary thrombocytopenia. differential prior to and
Child: IV 5–8 mg/m2 progressive, Other: Discolors during therapy.
once a week or 18– progressive urine and sclera a Expect urine to turn blue-
20 mg/m2 q3–4wk relapsing, or blue-green color. green for 24 h after drug
worsening Skin: Mild phlebitis, administration; sclera may
relapsing-remitting blue skin also take on a bluish color.
multiple sclerosis. discoloration, Be aware that
stomatitis/mucositis may
alopecia.
occur within 1 wk of therapy.
Do not to risk exposure to
those with known infections
during the periods of
myelosuppression.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
DAUNORUBICIN Neoplasms A potent bone Body as a Whole: Severe Monitor for therapeutic
o Adult: IV As a marrow suppressant Fever. CNS: myelosuppression; effectiveness. A profound
single agent, with Amnesia, anxiety, immunizations (patient, suppression of bone marrow
immunosuppressive ataxia, confusion, family), and preexisting is required to induce a
30–60 mg/m2/d
complete remission. Nadirs
for 3–5 d q3– properties as well as hallucinations, cardiac disease unless
for thrombocytes and
4wk (max: total antineoplastic emotional lability, risk-benefit is evaluated; leukocytes are usually
cumulative dose properties. It tremors. lactation; uncontrolled reached in 10–14 d.
500–600 interferes with DNA CV: Pericarditis, systemic infection. Safe Monitor serum bilirubin;
mg/m2); As and RNA synthesis. myocarditis, use during pregnancy drug dose needs to be
reduced when bilirubin is
combination Induces cardiac arrhythmias, (category D) is not
>1.2 mg/dL.
therapy, 30–45 toxicity and may be peripheral edema, established.
Monitor BP, temperature,
mg/m2/d on mutagenic and CHF, hypertension, pulse, and respiratory
days 1, 2, 3 of carcinogenic tachycardia. function during treatment.
first course and (development of GI: Acute nausea Monitor for S&S of acute
days 1 and 2 of secondary and vomiting (mild), CHF. It can occur suddenly,
subsequent carcinomas). anorexia, stomatitis, especially when total dosage
courses. mucositis, diarrhea exceeds 550 mg/m2, or in
o Child: IV As (occasionally) patients with compromised
combination hemorrhage. heart function because of
previous radiation therapy to
therapy, 2 y, Urogenital: Dysuria,
heart area.
25–45 mg/m2; nocturia, polyuria, Report immediately:
<2 y, calculated dry skin. Breathlessness, orthopnea,
on body weight Hematologic: Bone change in pulse and BP
(mg/kg) rather marrow depression parameters. Early clinical
than body thrombocytopenia, diagnosis of drug-induced
surface area leukopenia, anemia, CHF is essential for successful
Skin: Generalized treatment.
alopecia Report promptly S&S of
superinfections including
(reversible),
elevation of temperature,
transverse
chills, upper respiratory tract
pigmentation of infection, tachycardia,
nails, severe overgrowth with
cellulitis or tissue opportunistic organisms
necrosis at site of because myelosuppression
drug extravasation. imposes risk of
Endocrine: superimposed infection
Hyperuricemia, Protect patient from contact
gonadal with persons with infections.
The most hazardous period is
suppression.
during nadirs of
thrombocytes and
leukocytes.
Control nausea and vomiting
(usually mild) by antiemetic
therapy.
Inspect oral membranes
daily. Mucositis may occur 3–
7 d after drug is
administered.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
DOXORUBICIN Neoplasm Highly destructive to Body as a Whole: Myelosuppression, Stop infusion, remove IV needle,
o Adult: IV 60– rapidly proliferating Hypersensitivity (red impaired cardiac and notify physician promptly if
flare around injection patient complains of stinging or
75 mg/m2 as cells and slowly function, obstructive burning sensation at the
developing site, erythema, skin jaundice, previous
single dose injection site.
rash, pruritus,
at 21 d carcinomas; treatment with complete Monitor any area of
angioedema, urticaria, extravasation closely for 3–4 wk.
intervals or selectively toxic to eosinophilia, fever,
cumulative doses of
If ulceration begins (usually 1–4
30 mg/m2 cardiac tissue. chills, anaphylactoid doxorubicin or
wk after extravasation), a plastic
on each of 3 reaction). daunorubicin; lactation. surgeon should be consulted.
consecutive CV: Serious, Safe use during Begin a flow chart to establish
days irreversible pregnancy (category D) is baseline data. Include
repeated myocardial toxicity not established. temperature, pulse, respiration,
with delayed CHF, BP, body weight, laboratory
every 4 wk values, and I&O ratio and
(max: total ventricular
pattern.
arrhythmias, acute left
cumulative Lab tests: Baseline and periodic
ventricular failure, hepatic function, renal function,
dose 500–
hypertension, CBC with differential throughout
550 mg/m2) hypotension, and therapy.
o Child: IV 35– cardiomyopathy. Note: The nadir of leukopenia
75 mg/m2 as GI: Stomatitis, (an expected 1000/mm3)
single dose, esophagitis with typically occurs 10–14 d after
repeat at 21- ulcerations; nausea, single dose, with recovery
occurring within 21 d.
d interval, or vomiting, anorexia,
Evaluate cardiac function (ECG)
20–30 inanition, diarrhea.
prior to initiation of therapy, at
mg/m2 once Hematologic: Severe regular intervals, and at end of
myelosuppression; therapy.
weekly
leukopenia, Be alert to and report early signs
thrombocytopenia, of cardiotoxicity. Acute life-
Kaposi's Sarcoma anemia. threatening arrhythmias may
o Adult: IV Skin: occur within a few hours of drug
Doxil 20 Hyperpigmentation of administration.
Report promptly objective signs
mg/m2 nail beds, tongue, and
of hepatic dysfunction (jaundice,
every 3 wk. buccal mucosa
dark urine, pruritus) or kidney
Infuse over (complete alopecia dysfunction (altered I&O ratio
30 min (do (reversible), and pattern, local discomfort
not use in- hyperpigmentation of with voiding).
line filters) dermal creases Promote fastidious oral hygiene,
(especially in especially before and after
children), rash meals. Stomatitis, generally
maximal in second week of
Other: Lacrimation, therapy, frequently begins with
drowsiness, fever, a burning sensation
facial flush with too accompanied by erythema of
rapid IV infusion rate, oral mucosa that may progress
microscopic to ulceration and dysphagia in 2
hematuria, or 3 d.
hyperuricemia, hand- Report signs of superinfection
foot syndrome. With promptly; these may result from
antibiotic therapy during
extravasation: severe
leukopenic period.
cellulitis, vesication,
tissue necrosis,
Avoid rectal medications and
use of rectal thermometer;
lymphangitis, rectal trauma is associated with
phlebosclerosis. bloody diarrhea resulting from
an antiblastic effect on rapidly
growing intestinal mucosal cell.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
EPIRUBICIN Breast Cancer Highly destructive to Body as a Whole: Hypersensitivity to Withhold drug and notify
rapidly proliferating epirubicin and other physician of any of the
o Adult: IV 100– Lethargy, fever.
following: neutrophil count
120 mg/m2 cells. Utilized CV: Asymptomatic related drugs; marked <1500 cells/mm3, recent MI,
infused over 3–5 effectively in the decrease in LVEF, myelosuppression, suspicion of severe myocardial
min on day 1 of treatment of breast CHF. impaired cardiac insufficiency.
a 3–4 wk cycle carcinomas. GI: Nausea, function; previous Obtain baseline and periodic
(before each cycle of therapy)
or 50–60 Indicated by tumor vomiting, mucositis, treatment with maximum
cardiac evaluation: left
mg/m2 on day 1 regression. diarrhea, anorexia. doses of epirubicin, ventricular ejection fraction,
and 8 of a 3–4 Hematologic: doxorubicin, or ECG and ECHO (tests are
wk cycle Leukopenia, daunorubicin; pregnancy recommended especially in the
(category D), lactation. presence of risk factors of
neutropenia,
cardiac toxicity).
anemia, Monitor cardiac status closely
thrombocytopenia, throughout therapy as the risk
AML. of developing severe CHF
Skin: Alopecia, increases rapidly when
cumulative doses approach 900
injection site mg/m2. Report significant ECG
reaction, rash, changes immediately. Report
itching, skin immediately S&S of the
changes. following: tachycardia, gallop
rhythm, pleural effusion,
Other: Amenorrhea,
pulmonary edema, dependent
hot flashes, edema, ascites, or
infection, hepatomegaly.
conjunctivitis/kerati Lab tests: Baseline and periodic
tis, secondary acute (before each cycle of therapy)
CBC with differential, platelet
myelogenous
count, serum total bilirubin, AST,
leukemia (related to serum creatinine.
cumulative dose). Report any of the following to
physician immediately: Pain at
the site of IV infusion, chest
pain, palpitations, shortness of
breath or difficulty breathing,
sudden weight gain, swelling of
hands, feet or legs, or any
unexplained bleeding.
Be aware that your urine may
turn red for 1–2 d after receiving
this drug. This change is
expected and harmless.
Do not take OTC cimetidine or
any other OTC drug without
consulting physician.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
IDARUBICIN Acute Myelogenous Idarubicin exhibits CV: CHF, atrial Myelosuppression, Monitor infusion site closely, as
inhibitory effects on hypersensitivity to extravasation can cause severe
Leukemia (AML) fibrillation, chest
local tissue necrosis. Notify
o Adult: IV 8– DNA and RNA pain, MI. idarubicin or doxorubicin, physician if pain, erythema, or
12 mg/m2 polymerase and, GI: Nausea, pregnancy (category D), edema develops at insertion
daily for 3 d therefore, on vomiting, diarrhea, lactation. site.
injected nucleic acid abdominal pain, Lab tests: Monitor hepatic and
renal function, CBC with
slowly over synthesis. In mucositis. differential and coagulation
10–15 min combination with Hematologic: studies periodically.
other antineoplastic Anemia, leukopenia, Monitor cardiac status closely,
Acute Nonlymphocytic drugs for treatment thrombocytopenia. especially in older adult patients
of AML or those with preexisting cardiac
Leukemia, Acute Other:
disease.
Lymphocytic Leukemia Nephrotoxicity, Monitor hematologic status
o Child: IV 10– hepatotoxicity, carefully; during the period of
12 mg/m2/d alopecia, rash. myelosuppression, patients are
for 3 d at high risk for bleeding and
infection.
Monitor for development of
hyperuricemia secondary to lysis
of leukemic cells.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
VALRUBICIN BCG-Refractory Bladder Valrubicin has Body as a Whole: Hypersensitivity to Therapeutic effectiveness:
Carcinoma in situ higher antitumor Abdominal pain, valrubicin, doxirubicin; Indicated by regression of
o Adult: efficacy and lower asthenia, back pain, patients with a the bladder tumor.
Intravesically toxicity than fever, headache, perforated bladder, Notify physician if bladder
800 mg once doxirubicin. malaise, myalgia. concurrent UTI, active spasms with spontaneous
per wk x 6 wk. Intravesical therapy CNS: Dizziness. infection; severe irritable discharge of valrubicin
of BCG-refractory CV: Vasodilation. bladder symptoms; occur during/shortly after
carcinoma in situ of GI: Diarrhea, severe instillation.
the urinary bladder. flatulence, nausea, myelosuppression; Expect red-tinged urine
vomiting. pregnancy (category C); during the first 24 h after
Urogenital: Urinary lactation. administration.
frequency, urgency, Report prolonged passage
dysuria, bladder of red-colored urine or
spasm, hematuria, prolonged bladder
bladder pain, irritation.
incontinence, Drink plenty of fluids
cystitis, UTI, during 48 h period
nocturia, local following administration.
burning, urethral Use reliable contraception
pain, pelvic pain, during therapy period
gross hematuria, (approximately 6 wk).
urinary retention. Do not breast feed infants
Respiratory: during therapy period
Pneumonia. Skin: (approximately 6 wk).
Rash.
Other: Anemia,
hyperglycemia,
peripheral edema.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
OXACILLIN Staphylococcal Infections In common with Body as a Whole: Hypersensitivity to Ask patient prior to first dose
Adult: PO 250–1000 other isoxazolyl Thrombophlebitis penicillins or about hypersensitivity
mg q4–6h IM/IV 500 penicillins (IV therapy), cephalosporins. Safe use reactions to penicillins,
mg–2 g q4–6h up to (cloxacillin, superinfections, during pregnancy cephalosporins, and other
allergens.
12 g/d dicloxacillin), it is wheezing, sneezing, (category B) is not
Lab tests: periodic liver
Child: PO 50–100 highly active against fever, anaphylaxis. established.
functions, CBC with
mg/kg/d in 4 divided most penicillinase- GI: Nausea, Use cautiously in patients differential, platelet count,
doses IM/IV 50–150 producing vomiting, flatulence, with History of or and urinalysis.
mg/kg/d divided staphylococci, is less diarrhea, suspected atopy or Hepatic dysfunction (possibly
q4–6h potent than hepatocellular allergy (hives, eczema, a hypersensitivity reaction)
Neonate: IV 50–100 penicillin G against dysfunction hay fever, asthma); has been associated with IV
mg/kg/d divided penicillin-sensitive (elevated AST, ALT, premature infants, oxacillin; it is reversible with
q6–12h microorganisms, hepatitis). neonates, lactation (may discontinuation of drug.
and is generally cause infant diarrhea). Symptoms may resemble
Hematologic:
viral hepatitis or general
ineffective against Eosinophilia,
signs of hypersensitivity and
gram-negative leukopenia, should be reported promptly:
bacteria and thrombocytopenia, hives, rash, fever, nausea,
methicillin-resistant granulocytopenia, vomiting, abdominal
staphylococci agranulocytosis; discomfort, anorexia,
(MRSA). neutropenia malaise, jaundice (with dark
(reported in yellow to brown urine, light-
children). colored or clay-colored
Skin: Pruritus, rash, stools, pruritus).
Withhold next drug dose and
urticaria.
report the onset of
Urogenital: hypersensitivity reactions
Interstitial nephritis, and superinfections
transient hematuria, Take oral medication around
albuminuria, the clock, do not miss a dose.
azotemia (newborns Take all of the medication
and infants on high prescribed even if you feel
doses). better, unless otherwise
directed by physician
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
AMPICILLIN Systemic Infections Active against gram- Body as a Whole: Hypersensitivity to Determine previous
Adult: PO 250–500 positive Similar to those for penicillin derivatives; hypersensitivity reactions to
mg q6h IV/IM 250 microorganisms penicillin G. infectious penicillins, cephalosporins,
mg–2 g q6h such as alpha- and Hypersensitivity mononucleosis. and other allergens prior to
Child: PO 25–50 beta-Hemolytic (pruritus, urticaria, Use cautiously in patients therapy.
mg/kg/d divided streptococci, eosinophilia, with History of severe Lab tests: Baseline C&S tests
q6h IV/IM 25–100 Diplococcus hemolytic anemia, reactions to prior to initiation of therapy;
start drug pending results.
mg/kg/d divided pneumoniae, non- interstitial nephritis, cephalosporins;
Baseline and periodic
q6h penicillinase anaphylactoid pregnancy (category B) assessments of renal,
Neonate: IV/IM 7 d producing reaction); or lactation. hepatic, and hematologic
& 2000 g, 50 Staphylococci, and superinfections. functions, particularly during
mg/kg/d divided Listeria. Major CNS: Convulsive prolonged or high-dose
q12h; 7 d & >2000 g, advantage over seizures with high therapy.
75 mg/kg/d divided penicillin G is doses. Inspect skin daily and instruct
q8h; >7 d, 50–100 enhanced action GI: Diarrhea, patient to do the same. The
mg/kg/d divided against most strains nausea, vomiting, appearance of a rash should
of Enterococci and be carefully evaluated to
q6–12h pseudomembranous
differentiate a nonallergenic
several gram- colitis.
ampicillin rash from a
Meningitis negative strains Other: Severe pain hypersensitivity reaction.
Adult/Child: IV 150– including (following IM); Report rash promptly to
200 mg/kg/d Escherichia coli, phlebitis (following physician.
divided q4–6h Neisseria IV). Take medication around the
Neonate: IV/IM 7 d gonorrhoeae, N. Skin: Rash. clock; continue taking
& 2000 g, 100 meningitidis, medication until it is all gone
mg/kg/d divided Haemophilus (usually 10 d) unless
q12h; 7 d & >2000 g, influenzae, Proteus otherwise directed by
mirabilis, Salmonella physician or pharmacist.
150 mg/kg/d
Report diarrhea to physician;
divided q8h; >7 d, (including typhosa),
do not self-medicate. Give a
100–200 mg/kg/d and Shigella.
detailed report to the
divided q6–12h Inactive against physician regarding onset,
Mycoplasma, duration, character of stools,
Gonorrhea rickettsiae, fungi, associated symptoms,
Adult: PO 3.5 g with and viruses. temperature and weight loss
1 g probenecid (if any) to help rule out the
times 1 IV/IM 500 possibility of drug-induced,
mg q8–12h potentially fatal
pseudomembranous colitis
Report S&S of superinfection
(onset of black, hairy tongue;
oral lesions or soreness;
rectal or vaginal itching;
vaginal discharge; loose, foul-
smelling stools; or unusual
odor to urine).
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
TETRACYCLINE Systemic Infection Effective against a CNS: Headache, Hypersensitivity to Administer oral medication
variety of gram- intracranial hypertension tetracyclines or to any on an empty stomach, 1 hr
Adult: PO 250–500
(rare). before or 2–3 hr after meals.
mg b.i.d.–q.i.d. (1–2 positive and gram- Special Senses:
ingredient in the
g/d) IM 250 mg negative bacteria formulation; severe renal Do not give with antacids. If
Pigmentation of
antacids must be used, give
once/d or 300 mg/d and against most conjunctiva due to drug or hepatic impairment,
deposit. them 3 hr after the dose of
in 2–3 divided doses chlamydiae, common bile duct tetracycline.
GI: nausea, vomiting,
Child: PO >8 y, 25– mycoplasmas, obstruction. Use during Culture infection before
epigastric distress,
50 mg/kg/d in 2–4 rickettsiae, and heartburn, diarrhea, tooth development [last beginning drug therapy;
divided doses IM >8 certain protozoa bulky loose stools, half of pregnancy many resistant strains have
y, 15–25 mg/kg/d in (e.g., amebae). steatorrhea, abdominal (category D)], during been identified.
2–3 divided doses Exerts antiacne discomfort, flatulence, infancy and childhood to Do not administer during
dry mouth); dysphagia,
(max: 250 action by the 8th year, or lactation. pregnancy; drug is toxic to
retrosternal pain,
mg/injection) suppressing growth Safety of topical the fetus.
esophagitis, esophageal
of ulceration with oral tetracycline preparations WARNING: Do not use
Propionibacterium administration, foul- in children <8 y is not outdated drugs; degraded
Acne
smelling stools or vaginal drug is highly nephrotoxic
Adult/Child: PO >8 acnes within established.
discharge, stomatitis, and should not be used.
y, 500–1000 mg/d in sebaceous follicles. glossitis; black hairy Arrange for regular renal
4 divided doses tongue (lingua nigra), function tests with long-term
Topical Apply to diarrhea: staphylococcal therapy.
enterocolitis.
cleansed areas twice This drug should not be used
Body as a Whole: Drug
daily fever, angioedema,
during pregnancy; using
serum sickness, barrier contraceptives is
anaphylaxis. advised.
Urogenital: Particularly Report severe cramps,
in patients with kidney watery diarrhea, rash or
disease; increase in itching, difficulty breathing,
BUN/serum creatinine, dark urine or light-colored
renal impairment even stools, yellowing of the skin
with therapeutic doses;
or eyes.
Fanconi-like syndrome;
vulvovaginitis, Take the drug throughout the
Skin: Dermatitis, day for best results. The drug
phototoxicity: should be taken on an empty
discoloration of nails, stomach, 1 hour before or 2–
onycholysis; cheilosis; 3 hours after meals, with a
fixed drug eruptions full glass of water. Do not
particularly on genitalia; take the drug with food,
thrombocytopenic
dairy products, iron
purpura; Urticaria, rash,
exfoliative dermatitis; preparations, or antacids.
Other: Pancreatitis, local
reactions: pain and
irritation (IM site),
Jarisch-Herxheimer
reaction
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
STREPTOMYCIN Tuberculosis Active against a CNS: Paresthesias History of toxic reaction Obtain C&S tests prior to and
Adult: IM 15 mg/kg variety of gram- (peripheral, facial). or hypersensitivity to periodically during course of
up to 1 g/d as single positive, gram- Body as a Whole: aminoglycosides; therapy. In patients with
dose negative, and acid- Hypersensitivity labyrinthine disease; impaired kidney function,
angioedema, drug frequent determinations of
Geriatric: IM 10 fast organisms. myasthenia gravis;
fever, enlarged lymph serum drug concentrations
mg/kg (max: 750 Reportedly, it is the concurrent or sequential and periodic kidney and liver
nodes, anaphylactic
mg/d) least nephrotoxic of shock, headache, use of other neurotoxic function tests are advised
Child: IM 20–40 the inability to or nephrotoxic agents; (serum concentrations
mg/kg/d up to 1 g/d aminoglycosides. concentrate, lassitude, pregnancy (category C); should not exceed 25
as single dose muscular weakness, lactation. mcg/mL in these patients).
Infant: IM 10–15 pain and irritation at Monitor I&O. Report oliguria
mg/kg q12h IM site, or changes in I&O ratio
Neonate: IM 10–20 superinfections, (possible signs of diminishing
neuromuscular kidney function). Sufficient
mg/kg q24h
blockade, fluids to maintain urinary
arachnoiditis. output of 1500 mL/24 h are
Tularemia GI: Stomatitis, generally advised. Consult
Adult: IM 1–2 g/d in hepatotoxicity. physician.
1–2 divided doses Hematologic: Blood Be aware that auditory nerve
for 7–10 d dyscrasias damage is usually preceded
Child: IM 20–40 (leukopenia, by vestibular symptoms and
mg/kg/d divided neutropenia, high-pitched tinnitus, roaring
q6–12h pancytopenia, noises, impaired hearing
hemolytic or aplastic (especially to high-pitched
anemia, eosinophilia). sounds), sense of fullness in
Plague ears. Audiometric test should
Special Senses:
Adult: IM 2 g/d in 2– Labyrinthine damage, be done if these symptoms
4 divided doses auditory damage, appear, and drug should be
Child: IM 30 optic nerve toxicity discontinued. Hearing loss
mg/kg/d divided (scotomas). can be permanent if damage
Urogenital: is extensive. Tinnitus may
q8–12
Nephrotoxicity. persist several days to weeks
CNS: Encephalopathy, after drug is stopped.
CNS depression Report any unusual
syndrome in infants symptoms. Review adverse
(stupor, flaccidity, reactions with physician
coma, paralysis, periodically, especially with
cardiac arrest). prolonged therapy.
Respiratory: Be aware of possibility of
Respiratory ototoxicity and its symptoms
depression.
Skin: Skin rashes,
pruritus, exfoliative
dermatitis.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
NEOMYCIN Intestinal Antisepsis Active against a Body as a Whole: Use of oral drug in Perform audiometric studies
Adult: PO 1 g q1h wide variety of Neuromuscular patients with intestinal twice weekly in patients with
times 4 doses, then gram-negative blockade with obstruction; ulcerative kidney or liver dysfunction
1 g q4h times 5 bacteria, including muscular and bowel lesions; topical receiving extended oral
therapy.
doses Citrobacter, respiratory applications over large
Obtain baseline and daily
Child: PO 10.3 Escherichia coli, paralysis; skin areas; parenteral use
urinalysis for albumin, casts,
mg/kg q4–6h for 3 d Enterobacter, hypersensitivity in patients with kidney and cells; and BUN every
Klebsiella, Proteus reactions. disease or impaired other day. Also, serum drug
Hepatic Coma (including indole- GI: Mild laxative hearing; parkinsonism; levels (toxic levels reportedly
Adult: PO 4–12 g/d positive and indole- effect, diarrhea, myasthenia gravis; range from 8 to 30 mcg/mL,
in 4 divided doses negative strains), nausea, vomiting; pregnancy (category D), although individual variations
for 5–6 d Pseudomonas prolonged therapy: lactation. exist).
Child: PO 437.5– aeruginosa, and malabsorption-like Monitor I&O in patients
Serratia sp. Also syndrome including receiving oral or parenteral
1225 mg/m2 q6h for
therapy. Report oliguria or
5–6 d effective against cyanocobalamin
changes in I&O ratio.
certain gram- (vitamin B12) Inadequate neomycin
Diarrhea positive organisms, deficiency, low excretion results in high
Adult: PO 50 mg/kg particularly, serum cholesterol. serum drug levels and risk of
in 4 divided doses penicillin-sensitive Urogenital: nephrotoxicity and
for 2–3 d IM 1.3–2.6 and some Nephrotoxicity. ototoxicity.
mg/kg q6h methicillin-resistant Special Senses: Stop treatment and consult
Child: PO 8.75 strains of Ototoxicity. physician if irritation occurs
mg/kg q6h for 2–3 d Staphylococcus when you are using topical
Skin: Redness,
neomycin. Allergic dermatitis
aureus (MRSA). scaling, pruritus,
is common.
dermatitis. Report any unusual symptom
related to ears or hearing
Cutaneous Infections (e.g., tinnitus, roaring
Adult: Topical Apply sounds, loss of hearing
1–3 times/d acuity, dizziness).
Do not exceed prescribed
dosage or duration of
therapy.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
ERYTHROMYCIN Moderate to Severe More active against GI: Nausea, Hypersensitivity to Report onset of GI symptoms
Infections gram-positive than vomiting, abdominal erythromycins. History of after PO administration to
physician. These are dose
o Adult: PO 250–500 gram-negative cramping, diarrhea, erythromycin-associated related; if symptoms persist
mg q6h; 333 mg q8h bacteria. heartburn, anorexia. hepatitis; liver after dosage reduction,
o Child: PO 30–50 Effectiveness Body as a Whole: dysfunction; treatment of physician may prescribe drug to
mg/kg/d divided against Chlamydia Fever, eosinophilia, skin disorders such as be given with meals in spite of
impaired absorption.
q6h Topical Apply trachomatis is basis urticaria, skin acne or furunculosis;
Monitor for adverse GI effects.
ointment to infected for its topical use in eruptions, fixed prophylaxis of rheumatic Pseudomembranous
eye 1 or more prophylaxis of drug eruption, fever. enterocolitis, a potentially life-
times/d neonatal inclusion anaphylaxis. threatening condition, may
conjunctivitis. occur during or after antibiotic
o Neonate: PO 7 d, 10 Superinfections by
therapy.
mg/kg q12h; >7 d, nonsusceptible Observe for S&S of
10 mg/kg q8–12h bacteria, yeasts, or superinfection by overgrowth of
Topical 0.5–1 cm in fungi. nonsusceptible bacteria or fungi.
conjunctival sac Special Senses: Emergence of resistant
staphylococcal strains is highly
once Ototoxicity: predictable during prolonged
reversible bilateral therapy.
Chlamydia trachomatis hearing loss, Lab tests: Periodic liver function
Infections tinnitus, vertigo. tests during prolonged therapy.
Digestive: Monitor for S&S of
o Adult: PO 500 mg
hepatotoxicity. Premonitory S&S
q.i.d. or 666 mg q8h Cholestatic hepatitis include: Abdominal pain,
o Child: Topical Apply syndrome. nausea, vomiting, fever,
0.5–1 cm ribbon in Skin: (topical use) leukocytosis, and eosinophilia;
lower conjunctival Erythema, jaundice may or may not be
sacs shortly after desquamation, present. Symptoms may appear
a few days after initiation of
birth burning, tenderness, drug but usually occur after 1–2
dryness or oiliness, wk of continuous therapy.
pruritus. Symptoms are reversible with
prompt discontinuation of
erythromycin.
Monitor for ototoxicity that
appears to develop most
frequently in patients receiving 4
g/d or more, older adults,
female patients, and patients
with kidney or liver dysfunction.
It is reversible with prompt
discontinuation of drug.
DRUG DOSAGE THERAPEUTIC ACTION ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
CHLORAMPHENICOL Serious Infections Effective against a wide Body as a Whole: History of Perform bacterial culture
o Adult: PO/IV 50 variety of gram-negative Hypersensitivity, hypersensitivity or toxic and susceptibility tests prior
mg/kg/d in 4 and gram-positive angioedema, reaction to to first dose and periodically
divided doses. bacteria and most dyspnea, fever, chloramphenicol; thereafter. Baseline CBC,
anaphylaxis, platelets, serum iron, and
Topical 1–2 anaerobic treatment of minor
superinfections, Gray reticulocyte cell counts
drops of microorganisms. syndrome.
infections, prophylactic before initiation of therapy,
ophthalmic GI: Nausea, vomiting, use; typhoid carrier at 48 h intervals during
solution q3–6h or diarrhea, perianal state, history or family therapy, and periodically.
small strip of irritation, history of drug-induced Monitor chloramphenicol
ophthalmic enterocolitis, bone marrow blood levels weekly or more
ointment in glossitis, stomatitis, depression, concomitant frequently with hepatic
lower unpleasant taste, therapy with drugs that dysfunction and in patients
conjunctival sac xerostomia. produce bone marrow receiving therapy for longer
Hematologic: Bone depression; pregnancy than 2 wk.
q3–6h or 2–3
marrow depression Monitor blood studies.
drops of otic (category C); lactation.
(dose-related and Chloramphenicol should be
solution in ear reversible): discontinued upon
t.i.d. reticulocytosis, appearance of leukopenia,
o Neonate: IV 25– leukopenia, reticulocytopenia,
50 mg/kg/d granulocytopenia, thrombocytopenia, or
divided q12–24h thrombocytopenia, anemia.
o Infant/Child: increased plasma Observe the patient closely,
PO/IV 50–75 iron, reduced Hgb, because blood studies are
mg/kg/d divided hypoplastic anemia, not always reliable
hypoprothrombinemi predictors of irreversible
q6h (max: 4 g/d) a. Non-dose-related bone marrow depression.
and irreversible Check temperature at least
Meningitis pancytopenia, q4h. Usually
o Adult: IV 75–100 agranulocytosis, chloramphenicol is
aplastic anemia, discontinued if temperature
mg/kg/d divided
paroxysmal nocturnal remains normal for 48 h.
q6h hemoglobinuria, Monitor I&O ratio or
o Child: IV Same as leukemia. pattern: Report any
for adult CNS: Neurotoxicity: appreciable change.
headache, mental More frequent
depression, determinations of serum
confusion, delirium, glucose are recommended in
digital paresthesias, patients receiving oral
peripheral neuritis. antidiabetic agents.
Skin: Urticaria, Monitor for S&S of Gray
contact dermatitis, syndrome, which has
maculopapular and occurred 2–9 d after
vesicular rashes, initiation of high dose
fixed-drug eruptions. chloramphenicol therapy in
Special Senses: Visual premature infants and
disturbances, optic neonates and in children 2 y.
neuritis, optic nerve Follow dosage and duration
atrophy, contact of therapy as prescribed by
conjunctivitis. physician.
Avoid prolonged or frequent
intermittent use of topical
preparations because
systemic absorption and
toxicity can occur.
DRUG DOSAGE THERAPEUTIC ACTION ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
NOVOBIOCIN S. aureus Infections Active in vitro against GI: Nausea, Contraindicated in Report adverse effects
o Adult: PO 250 mg many gram-positive vomiting, diarrhea, Neonates; during promptly; this drug is an
extremely potent sensitizing
q6h or 500 mg bacteria anorexia, pregnancy (category C), agent.
q12h up to 2 g/d including Staphylococcus abdominal distress, lactation. Be aware that a yellow
o Child: PO 15–45 aureus, Streptococcus jaundice, elevated metabolite of novobiocin can
mg/kg/d in 2–4 pneumoniae, Group serum bilirubin. cause jaundice-like skin
coloration. Differentiation of
divided doses A streptococci, viridans Hematologic: drug-induced effect from frank
streptococci, and against Pancytopenia, jaundice will depend on other
some gram-positive agranulocytosis, signs of liver dysfunction.
bacilli. Enterococci are anemia, Advise patient to report
usually resistant to thrombocytopenia, symptoms promptly.
novobiocin. Also active hemolytic anemia. Lab tests: CBC with differential,
platelet count, Hct and Hgb,
against gram-negative Skin: Urticaria, liver function tests at the first
bacteria maculopapular sign of an adverse response.
including Haemophilus dermatitis, Stevens- Inspect skin for signs of
influenzae and Neisseria Johnson syndrome, thrombocyte dyscrasia:
petechiae, ecchymoses, easy
gonorrhoeae. Resistant erythema
bruising. Promptly report
strains of S. aureus may multiforme, these signs or epistaxis or
develop rapidly during pruritus, bleeding for unexplained
therapy. eosinophilia. reason.
Body as a Whole: Report any reversal in prior
evidence of therapeutic
Dizziness, response to drug therapy.
drowsiness, light- Drug resistance may develop
headedness, rapidly.
swollen joints, Do not stop treatment just
because you feel better.
fever.
Duration of therapy depends
on the infection but it will
continue about 48 h after your
fever is gone or there is no
more evidence of the
infection.
Do not change your treatment
regimen without consulting
physician; sensitivity and
adverse effects may occur as
well as a loss of therapeutic
effects.
Do not use leftover novobiocin
to self-medicate for another
infection.
DRUG DOSAGE THERAPEUTIC ACTION ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
KANAMYCIN Preoperative Intestinal Active against many Body as a Whole: History of Monitor baseline C&S,
Antisepsis gram-negative micro- Eosinophilia, hypersensitivity to urinalysis, and kidney
o Adult: PO 1 g q1h organisms, maculopapular rash, kanamycin or other function prior to initiation
for 4 doses then especially Acinetobacter, pruritus, urticaria, aminoglycosides; history of therapy and periodically
drug fever, thereafter. Monitor serum
q6h for 36–72 h Escherichia coli, of drug-induced
anaphylaxis. sodium, potassium,
Enterobacter aerogenes, ototoxicity, preexisting calcium, and magnesium.
CNS: Dizziness,
Hepatic Coma Klebsiella pneumoniae, circumoral and other hearing loss, vertigo, or Notify physician
o Adult: PO 8–12 Proteus sp, and Serratia paresthesias, optic tinnitus; long-term immediately of signs of
g/d in divided marcescens. Also neuritis, peripheral therapy; PO use in renal irritation:
doses effective against many neuritis, headache, intestinal obstruction or albuminuria, casts, red and
strains of Staphylococcus restlessness, tremors, ulcerative bowel lesions; white cells in urine,
Serious Infection aureus, but it is not the lethargy, convulsions; intraperitoneally to increasing BUN, and serum
neuromuscular creatinine, decreasing
o Adult/Child: IV/IM drug of choice. Inhibits patients under effects of
paralysis, respiratory creatinine clearance,
15 mg/kg/d in growth of Mycobacterium depression (rarely). inhalation anesthetics or oliguria, and edema.
equally divided tuberculosis in vitro. Special Senses: skeletal muscle Monitor peak and trough
doses q8–12h Deafness (can be relaxants. Safety during serum kanamycin
o Adult: irreversible), tinnitus, pregnancy (category D) concentrations: Assess peak
Intraperitoneal vertigo or dizziness, or lactation is not specimen 30–60 min after
500 mg diluted in ataxia, nystagmus. established. IM administration; 30 min
20 mL sterile GI: Nausea, vomiting, after completion of a 30–60
water instilled diarrhea, appetite min IV infusion. Assess
changes, abdominal trough levels just before
through wound
discomfort, the next IM or IV dose.
catheter stomatitis, proctitis, Keep patient well hydrated
Inhalation 250 mg malabsorption to prevent chemical
diluted in 3 mL syndrome (with irritation of renal tubules.
NS administered prolonged oral Monitor I&O. Report
per nebulizer q6– administration). decrease in urine output or
12h Irrigation Hematologic: change in I&O ratio.
0.25% solution Anemia, increased or Determine baseline weight
prn decreased and vital signs and monitor
reticulocytes, at regular intervals during
granulocytopenia, therapy.
agranulocytosis, Report ototoxic symptoms
thrombocytopenia, such as dizziness, hearing
purpura. loss, weakness, or loss of
Urogenital: balance; drug may need to
Nephrotoxicity; be discontinued.
hematuria, urine
casts and cells,
proteinuria; elevated
serum creatinine and
BUN. Other:
Superinfections; local
pain; nodular
formation at injection
site.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
NYSTATIN Candida Infections Fungistatic and GI: Nausea, vomiting, Use of vaginal tablets Monitor oral cavity,
o Adult: PO 500,000– fungicidal activity epigastric distress, during pregnancy especially the tongue, for
1,000,000 U t.i.d.; against a variety of diarrhea (especially with (category C); vaginal signs of improvement.
1–4 troches 4–5 yeasts and fungi; high oral doses). infections caused by Avoid occlusive dressings or
applications of ointment
times/d; not appreciably Gardnerella vaginalis or
preparation to moist, dark
Suspension: active against Trichomonas sp.
areas of body because they
400,000–600,000 U bacteria, viruses, or favor growth of yeast.
q.i.d. Intravaginal 1– protozoa. Take for oral candidiasis
2 tablets daily for 2 (thrush) treatment after
wk meals and at bedtime.
o Child: PO Dissolve troche in mouth
Suspension: (about 30 min). Do not chew
400,000–600,000 U or swallow. Avoid food and
q.i.d. drink during period of
dissolving and for 30 min
o Infant: PO 100,000–
after treatment.
200,000 U q.i.d. Dust shoes and stockings, as
well as feet, with nystatin
dusting powder.
Gently clean infected areas
with tepid water before each
application of topical
preparation.
Continue medication for
vulvovaginal candidiasis
during menstruation.
Use vaginal tablets up to 6
wk before term to prevent
thrush in the newborn.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
VANCOMYCIN Systemic Infections Active against many Special Senses: Known hypersensitivity Monitor BP and heart rate
o Adult: IV 500 mg gram-positive Ototoxicity to vancomycin, allergy to continuously through period
q6h or 1 g q12h, organisms, including (auditory portion of corn or corn products, of drug administration.
infuse over 60–90 group A beta- eighth cranial previous hearing loss, Lab tests: Monitor urinalysis,
kidney & liver functions, and
min hemolytic nerve). concurrent or sequential
hematologic studies
o Child: IV 40 mg/kg/d Streptococci, Urogenital: use of other ototoxic or
periodically.
divided q6h, infuse Staphylococci, Nephrotoxicity nephrotoxic agents, IM Monitor serial tests of
over 60–90 min Pneumococci, leading to uremia. administration. vancomycin blood levels
o Neonate: IV 10 Enterococci, Body as a Whole: (peak and trough) in patients
mg/kg/d divided Clostridia, and Hypersensitivity with borderline kidney
function, in infants and
q8–12h, infuse over Corynebacteria. reactions (chills,
neonates, and in patients >60
60–90 min Gram-negative fever, skin rash, y.
organisms, urticaria, shock-like Assess hearing. Drug may
Clostridium difficile Colitis mycobacteria, and state), cause damage to auditory
o Adult: PO 125–500 fungi are highly anaphylactoid branch (not vestibular
mg q6h resistant. reaction with branch) of eighth cranial
o Child: PO 40 vascular collapse, nerve, with consequent
mg/kg/d divided superinfections, deafness, which may be
q6h (max: 2 g/d) severe pain, permanent.
thrombophlebitis at Be aware that serum levels of
60–80 mcg/mL are
injection site,
associated with ototoxicity.
generalized tingling Tinnitus and high-tone
following rapid IV hearing loss may precede
infusion. deafness, which may
Hematologic: progress even after drug is
Transient withdrawn. Older adults and
leukopenia, those on high doses are
eosinophilia. especially susceptible.
GI: Nausea, warmth. Monitor I&O: Report changes
Other: Injection in I&O ratio and pattern.
Oliguria or cloudy or pink
reaction that
urine may be a sign of
includes nephrotoxicity (also
hypotension manifested by transient
accompanied by elevations in BUN, albumin,
flushing and and hyaline and granular
erythematous rash casts in urine).
on face and upper
body ("red-neck
syndrome")
following rapid IV
infusion.
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
BACITRACIN Systemic Infections Active against many GI: Anorexia, Toxic reaction or renal Baseline C&S tests prior to
o Child: IM <2.5 kg up gram-positive nausea, vomiting, dysfunction associated initiation of therapy; start
to 900 U/kg/24 h organisms including diarrhea, rectal with bacitracin; impaired drug pending results.
divided q8–12h; Streptococci, itching and burning. renal function; atopic Determine BUN and
nonprotein nitrogen (NPN);
>2.5 kg up to 1000 Staphylococci, Hematologic: individuals; pregnancy
examine urine for albumin,
U/kg/24h divided Pneumococci, Systemic use: Bone (category C).
casts, and cellular elements,
q8–12h Corynebacteria, marrow depression, before systemic therapy is
Clostridia, Neisseria, blood dyscrasias; started. Monitor renal
Skin Infections Haemophilus eosinophilia. function daily throughout
o Adult: Topical Apply influenzae, and Body as a Whole: therapy.
thin layer of Treponema Hypersensitivity Watch for signs of local
ointment b.i.d., pallidum. Also active (erythema, allergic reaction (itching,
t.i.d., as solution of against Gonococci anaphylaxis). burning, redness) with
and Meningococci; topical skin applications.
250–1000 U/mL in Urogenital:
Local reactions have
wet dressing ineffective against Nephrotoxicity,
preceded life-threatening
most other gram- dose related: anaphylactic episodes.
negative organisms. Increased BUN, Monitor I&O during
uremia, renal parenteral therapy.
tubular and Adequate urinary output is
glomerular necrosis. important to reduce
Special Senses: possibility of renal toxicity. If
Tinnitus. fluid intake is inadequate or
Other: Pain and urinary output decreases,
report to physician.
inflammation at
Inspect urine for turbidity
injection site, fever,
and hematuria, and watch
superinfection, for other S&S of urinary tract
neuromuscular dysfunction. Report any
blockade with changes in urination pattern
respiratory (e.g., oliguria, urinary
depression. frequency, nocturia).
DRUG DOSAGE THERAPEUTIC ADVERSE EFFECT CONTRAINDICATIONS NURSING CONSIDERATIONS
ACTION
CYCLOSERINE Tuberculosis Effective against CV: Arrhythmias, Epilepsy; depression, Lab tests: Culture and
o Adult: PO 250 mg gram-positive and CHF. severe anxiety, history of susceptibility tests should be
q12h for 2 wk, may gram-negative Hematologic: psychoses; severe renal performed before initiation
bacteria and insufficiency; chronic of therapy and periodically
increase to 500 mg Vitamin B12 and
thereafter to detect possible
q12h (max: 1 g/d) Mycobacterium folic acid deficiency, alcoholism; pregnancy
bacterial resistance. Monitor
tuberculosis by megaloblastic or (category C), lactation. plasma drug levels weekly
Urinary Tract Infection competitively sideroblastic Safe use in children not and hematologic, renal, and
o Adult: PO 250 mg interfering with the anemia. established. hepatic function at regular
incorporation of D- intervals.
q12h for 2 wk CNS: Drowsiness,
Maintenance of blood-drug
alanine into the anxiety, headache,
level below 30 mg/mL
bacterial cell wall. tremors, myoclonic considerably reduces
jerking, convulsions, incidence of neurotoxicity.
vertigo, visual Possibility of neurotoxicity
disturbances, increases when dose is 500
speech difficulties mg or more or when renal
(dysarthria), clearance is inadequate.
lethargy, Observe patient carefully for
depression, signs of hypersensitivity and
disorientation with neurologic effects.
Neurotoxicity generally
loss of memory,
appears within first 2 wk of
confusion, therapy and disappears after
nervousness, drug is discontinued.
psychoses, tic Drug should be withheld and
episodes, character physician notified or dosage
changes, reduced if symptoms of CNS
hyperirritability, toxicity or hypersensitivity
aggression, reaction develop.
hyperreflexia, Take cycloserine after meals
peripheral to prevent GI irritation.
Notify physician immediately
neuropathy,
of the onset of skin rash and
paresthesias,
early signs of CNS toxicity.
paresis, dyskinesias. Avoid potentially hazardous
Skin: Dermatitis, tasks such as driving until
photosensitivity. reaction to cycloserine has
Special Senses: Eye been determined.
pain (optic neuritis), Take drug precisely as
photophobia. prescribed and to keep
follow-up appointments.
Continuous therapy may
extend into months or years.
You might also like
- BPS Oncology Pharmacy Practice ExamDocument11 pagesBPS Oncology Pharmacy Practice Examiman100% (3)
- CITICOLINE, Drugs in MedicalDocument10 pagesCITICOLINE, Drugs in MedicalInosanto May AnnNo ratings yet
- Drug Study (Ranitidine, Metoclopramide, Ketorolac, and Omeprazole)Document8 pagesDrug Study (Ranitidine, Metoclopramide, Ketorolac, and Omeprazole)Akisan0% (1)
- Drug Study - EsomeprazoleDocument1 pageDrug Study - Esomeprazolechriscustodio100% (1)
- Case Study Colorectal CancerDocument23 pagesCase Study Colorectal CancerLeogalvez BedanoNo ratings yet
- Cancer #1 Case Study - Coreweek OneDocument2 pagesCancer #1 Case Study - Coreweek OneDragan Djordjevic100% (4)
- Alkylating and AntimetabolitesDocument38 pagesAlkylating and AntimetabolitesRebecca Chen0% (1)
- Drugs 2Document6 pagesDrugs 2Elyse Ann ReyesNo ratings yet
- Drug Classification & Indication Dose, Route & Frequency Mechanism of Action Contraindication Side Effects Nursing ResponsibilitiesDocument3 pagesDrug Classification & Indication Dose, Route & Frequency Mechanism of Action Contraindication Side Effects Nursing Responsibilitiestristanpaul100% (1)
- Drug Classification & Indication Dose, Route & Frequency Mechanism of Action Contraindication Side Effects Nursing ResponsibilitiesDocument3 pagesDrug Classification & Indication Dose, Route & Frequency Mechanism of Action Contraindication Side Effects Nursing ResponsibilitiestristanpaulNo ratings yet
- Make A Drug Study On The Medications Given To JaneDocument2 pagesMake A Drug Study On The Medications Given To JaneYoko Mae YanoNo ratings yet
- Drug Sudy CamvilleDocument4 pagesDrug Sudy CamvilleJoshua MendozaNo ratings yet
- Drug Study CHDCDocument1 pageDrug Study CHDCIannBlancoNo ratings yet
- Pharmacological Sheet Patient Name: BALDESTOY, Benedict Age: 19 Years Old Sex: Male Diagnosis: Hepatoma CAP-MRDocument5 pagesPharmacological Sheet Patient Name: BALDESTOY, Benedict Age: 19 Years Old Sex: Male Diagnosis: Hepatoma CAP-MRIngrid NicolasNo ratings yet
- Drug Mechanism of Action Indication Contraindication Adverse Effects Nursing Responsibility BetahistineDocument16 pagesDrug Mechanism of Action Indication Contraindication Adverse Effects Nursing Responsibility Betahistineclydell joyce masiarNo ratings yet
- General Class and Family Enumerate and Underscore Specific Indication IllustrateDocument5 pagesGeneral Class and Family Enumerate and Underscore Specific Indication IllustrateAlvin DagumbalNo ratings yet
- Drug StudyDocument27 pagesDrug StudyAbie Jewel Joy RoqueNo ratings yet
- Case Study Final LandscapeDocument3 pagesCase Study Final LandscapeZhy CaluzaNo ratings yet
- Drug Ana LaraDocument2 pagesDrug Ana LaralarapaulineNo ratings yet
- Drug Study For Multiple Sclerosis (Betaseron)Document4 pagesDrug Study For Multiple Sclerosis (Betaseron)Leslie Lagat PaguioNo ratings yet
- GCP Cs DrugsDocument13 pagesGCP Cs DrugsBel CortezNo ratings yet
- Drug Name Drug Class Mechanism of Action Indications Contra-Indications Side Effects/ Adverse Effects Nursing ConsiderationDocument7 pagesDrug Name Drug Class Mechanism of Action Indications Contra-Indications Side Effects/ Adverse Effects Nursing ConsiderationJhucyl Mae GalvezNo ratings yet
- Drug Name Drug Class Mechanism of Action Indications Contraindications Side Effects/ Adverse Effects Nursing ConsiderationDocument3 pagesDrug Name Drug Class Mechanism of Action Indications Contraindications Side Effects/ Adverse Effects Nursing ConsiderationKim SunooNo ratings yet
- Drug StudyDocument4 pagesDrug StudyMelody Forca FranciscoNo ratings yet
- Name of DrugDocument2 pagesName of DrugNOT AVAILABLENo ratings yet
- DS PantoprazoleDocument2 pagesDS PantoprazoleMatt Reyes Del CastilloNo ratings yet
- Name of Drug Dosage, Frequency, Route, Timing Mechanism of Action Indication Contraindication Adverse Effect Nursing ResponsibilitiesDocument13 pagesName of Drug Dosage, Frequency, Route, Timing Mechanism of Action Indication Contraindication Adverse Effect Nursing Responsibilitieskev mondaNo ratings yet
- PrimidoneDocument6 pagesPrimidoneKim SunooNo ratings yet
- Drug StudyDocument1 pageDrug StudyCuttie Anne GalangNo ratings yet
- Drug Study (Omeprazole)Document2 pagesDrug Study (Omeprazole)Baji ۦۦNo ratings yet
- Fluphenazine Drug Study - DoxDocument3 pagesFluphenazine Drug Study - Doxan naNo ratings yet
- Galantine HBRDocument5 pagesGalantine HBRArone SebastianNo ratings yet
- TELMISARTANDocument8 pagesTELMISARTANCidny CalimagNo ratings yet
- Drug Name Mechanism of Action Contra-Indications Route/Dosage Side Effects Nursing Considerations Alkylating AgentsDocument2 pagesDrug Name Mechanism of Action Contra-Indications Route/Dosage Side Effects Nursing Considerations Alkylating AgentsSave The Day SuppliesNo ratings yet
- Drug Study NCP Appendicitis Medix CADocument3 pagesDrug Study NCP Appendicitis Medix CABel CortezNo ratings yet
- Drug Study CSDocument7 pagesDrug Study CSFrancis MendozaNo ratings yet
- NLM Drug StudyDocument2 pagesNLM Drug Studyamal abdulrahmanNo ratings yet
- Generic Name: Mebeverine Hydrochloride Mechanism of Action Side Effects/ Adverse Reaction Nursing Responsibility Assessment & Drug EffectsDocument4 pagesGeneric Name: Mebeverine Hydrochloride Mechanism of Action Side Effects/ Adverse Reaction Nursing Responsibility Assessment & Drug EffectsNiziu BearsNo ratings yet
- MetoclopramideDocument1 pageMetoclopramideYanejoulce SacanleNo ratings yet
- DRUG STUDY For SrugeryDocument5 pagesDRUG STUDY For SrugeryZheyrille A. ArevaloNo ratings yet
- Azathioprine - Frequent:: Anti-Inflammatory Immunosuppressive That Can Decrease Joint Damage and DisabilityDocument3 pagesAzathioprine - Frequent:: Anti-Inflammatory Immunosuppressive That Can Decrease Joint Damage and DisabilityJordz PlaciNo ratings yet
- Drug Study (CHF)Document9 pagesDrug Study (CHF)Ericka VillanuevaNo ratings yet
- Ryrey A. Pacamana BSN 3C Drug StudyDocument8 pagesRyrey A. Pacamana BSN 3C Drug StudyRyrey Abraham PacamanaNo ratings yet
- Drug Study TableDocument4 pagesDrug Study TableSheena Friales Dorin100% (2)
- Drug StudyDocument9 pagesDrug Studywarlocke100% (2)
- Drug StudyDocument2 pagesDrug StudyJEWEL DEEN VILLARMENTE OQUIANANo ratings yet
- Drug StudyDocument16 pagesDrug StudyManuel PascualNo ratings yet
- Drug Study Surgical WardDocument11 pagesDrug Study Surgical WardpotchistroberriNo ratings yet
- Mfe, Ferrous Sulfate, Calcium Drug StudyDocument3 pagesMfe, Ferrous Sulfate, Calcium Drug StudyMary Shane MoraldeNo ratings yet
- Drugs Study - 3rdrotationDocument15 pagesDrugs Study - 3rdrotationDette CorpuzNo ratings yet
- Drug StudyDocument1 pageDrug Studyjasper pachingelNo ratings yet
- Drug For H-MoleDocument5 pagesDrug For H-MolesAm_30No ratings yet
- OMEPRAZOLEDocument2 pagesOMEPRAZOLERea LynNo ratings yet
- Drug StudyDocument7 pagesDrug StudyDummy AccountNo ratings yet
- LopezBSN3C Medical InterventionDocument5 pagesLopezBSN3C Medical InterventionJoyce Kathreen Ebio LopezNo ratings yet
- Cefuroxime Drug Study ChanDocument5 pagesCefuroxime Drug Study Chanczeremar chanNo ratings yet
- Drug StudyDocument5 pagesDrug StudyMay Dianne Mansia Bautista100% (1)
- Benztrop, Congentin: Drug StudyDocument4 pagesBenztrop, Congentin: Drug StudyHamimah Bint AliNo ratings yet
- Bicalutamide (Casodex) Drug StudyDocument2 pagesBicalutamide (Casodex) Drug StudyAtteya Mogote AbdullahNo ratings yet
- Drug Study NCMHDocument5 pagesDrug Study NCMHnhyceNo ratings yet
- Myasthenia Gravis, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandMyasthenia Gravis, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- The Complete Guide to Chronic Constipation: Symptoms, Risks, Treatments & CuresFrom EverandThe Complete Guide to Chronic Constipation: Symptoms, Risks, Treatments & CuresNo ratings yet
- CNS Drug StudyDocument19 pagesCNS Drug StudyCecilia Micole M. De GulaNo ratings yet
- Cardiovascular Drugs (Drug Study)Document77 pagesCardiovascular Drugs (Drug Study)Cecilia Micole M. De GulaNo ratings yet
- Treaty of ParisDocument2 pagesTreaty of ParisCecilia Micole M. De GulaNo ratings yet
- Pharma Genitourinary TransesDocument15 pagesPharma Genitourinary TransesCecilia Micole M. De GulaNo ratings yet
- Week 15 Drug StudyDocument15 pagesWeek 15 Drug StudyCecilia Micole M. De GulaNo ratings yet
- JC Oncology55211005Document32 pagesJC Oncology55211005Neenuch ManeenuchNo ratings yet
- A05 001Document59 pagesA05 001jaimeNo ratings yet
- Biomonitoring of 5 Flourouracil - AnyDocument23 pagesBiomonitoring of 5 Flourouracil - AnyAgus TianyNo ratings yet
- Curs VII - Terapii SistemiceDocument229 pagesCurs VII - Terapii SistemiceHucay EduardNo ratings yet
- 5 Fluorouracil en Queratoquiste 2017Document11 pages5 Fluorouracil en Queratoquiste 2017arisnicole5No ratings yet
- Cancer Case StudyDocument3 pagesCancer Case Studyapi-311163159No ratings yet
- Folfiri+cetu Gi Col PDocument12 pagesFolfiri+cetu Gi Col PJayelle2No ratings yet
- Fluoracil Drug StudyDocument3 pagesFluoracil Drug StudyNicole Louize CaloraNo ratings yet
- Chemotherapeutic Agents: A. Acred, L. Blake, S. Brodine, M. Devineni, B. Harris, B. Hatchell, C. JamesDocument75 pagesChemotherapeutic Agents: A. Acred, L. Blake, S. Brodine, M. Devineni, B. Harris, B. Hatchell, C. JamesSarah BrodineNo ratings yet
- CancerTreatmentConventionalITO13 1Document627 pagesCancerTreatmentConventionalITO13 1auradelrosarioNo ratings yet
- Anti-Cancer DrugsDocument78 pagesAnti-Cancer DrugsLaghari Jamil100% (1)
- ColorectalCancer - Case StudyDocument28 pagesColorectalCancer - Case StudyColeen Mae CamaristaNo ratings yet
- Anticancer DrugsDocument26 pagesAnticancer DrugsNeha Chugh100% (1)
- RTOG 0529 IMRT Anal CancerDocument57 pagesRTOG 0529 IMRT Anal CancergammasharkNo ratings yet
- Chemo Practice ProblemsDocument12 pagesChemo Practice ProblemsSamNo ratings yet
- 03-Anti-Cancer Drugs - FST PDFDocument77 pages03-Anti-Cancer Drugs - FST PDFRyan RachmawanNo ratings yet
- CAPIRI Capecitabine-Irinotecan (COLORECTAL CANCER)Document5 pagesCAPIRI Capecitabine-Irinotecan (COLORECTAL CANCER)Sindu SankarNo ratings yet
- Our Lady of Fatima University - Valenzuela Campus College of NursingDocument9 pagesOur Lady of Fatima University - Valenzuela Campus College of NursingKhristine Mae RoqueNo ratings yet
- Cortejoso2016 Cost-Effectiveness of Screening For DPYD Polymorphisms To Prevent NeutropeniaDocument6 pagesCortejoso2016 Cost-Effectiveness of Screening For DPYD Polymorphisms To Prevent NeutropeniaSandra KneževićNo ratings yet
- Accumulation of Alpha-Fluoro-Beta-Alanine and Fluoro Mono Acetate in A Patient With 5-Fluorouracil-Associated HyperammonemiaDocument5 pagesAccumulation of Alpha-Fluoro-Beta-Alanine and Fluoro Mono Acetate in A Patient With 5-Fluorouracil-Associated HyperammonemiaJana NgNo ratings yet
- Oxaliplatin Monograph 1dec2016Document9 pagesOxaliplatin Monograph 1dec2016Nadial UzmahNo ratings yet
- Drug Name Mechanism of Action Indication Contraindication Side Effects/Adverse Reaction Nursing Responsibility CNS-malaiseDocument3 pagesDrug Name Mechanism of Action Indication Contraindication Side Effects/Adverse Reaction Nursing Responsibility CNS-malaisekristel_nicole18yahoNo ratings yet
- Anti Cancer Drug Mechanism of ActionDocument8 pagesAnti Cancer Drug Mechanism of ActionayushiNo ratings yet
- FOLFOXDocument4 pagesFOLFOXpkjunaid313No ratings yet
- Xeloda Tablets Description:: BioactivationDocument19 pagesXeloda Tablets Description:: BioactivationDrogoman MarianNo ratings yet
- Verruca Vulgaris JurnalDocument22 pagesVerruca Vulgaris JurnalAndikazaki 74OKNo ratings yet