Professional Documents
Culture Documents
EASL Clinical Practice Guidelines On Sclerosing Cholangitis Elsevier Enhanced Reader
EASL Clinical Practice Guidelines On Sclerosing Cholangitis Elsevier Enhanced Reader
Uploaded by
chiara valentina luglioOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
EASL Clinical Practice Guidelines On Sclerosing Cholangitis Elsevier Enhanced Reader
EASL Clinical Practice Guidelines On Sclerosing Cholangitis Elsevier Enhanced Reader
Uploaded by
chiara valentina luglioCopyright:
Available Formats
Outline Figures (2) Extras (1)
762 Journal of Hepatology 2022 vol. 77 j 761–806
Table 3. Grades of recommendation. PSC is suspected in the presence of persistently elevated
Grade Wording Criteria serum liver tests in a cholestatic pattern. Most patients are
Strong Must, shall, should, is Evidence, consistency of studies, asymptomatic, but right upper quadrant abdominal pain, jaun-
recommended risk-benefit ratio, patient dice and/or pruritus may be present. Occasionally the initial
Shall not, should not, preferences, ethical obligations, presentation will be an episode of acute cholangitis, with right
is not recommended feasibility
upper quadrant abdominal pain, fever and jaundice. Secondary
Weak or Can, may, is suggested
open May not, is not suggested causes of sclerosing cholangitis should be excluded. Importantly,
50-80% of people with PSC also have IBD. Therefore, elevation in
serum liver tests, especially serum alkaline phosphatase (ALP),
The Delphi Panel agreement on each of the initial recommen- should raise suspicion for PSC and trigger further evaluation
dations is shown in the Appendix. (Fig.
Fig. 1
1). However, some rare patients may present with typical
findings of sclerosing cholangitis on cholangiography but
How is PSC diagnosed in adults? without elevation of serum ALP and gamma-glutamyltransferase
(GGT); such patients need careful follow-up.
Although MRCP can be used as a quick standalone non-
contrast test to diagnose PSC, performing a more complete,
Recommendations high-quality MRI evaluation will also provide information on bile
In adult patients presenting with elevated serum markers of duct thickness and enhancement, the status of hepatic paren-
cholestasis, a diagnosis of large duct PSC should be made in chyma and complications of liver disease including evidence of
the presence of typical findings of sclerosing cholangitis on portal hypertension.25,26
25 26 The classic features of PSC are multi-
high-quality cholangiography and after exclusion of sec- focal strictures and dilatations or ectasias involving the intra-
ondary causes. The preferred diagnostic test is magnetic and/or extrahepatic biliary tree. Other findings include ductal
resonance cholangiopancreaticography (MRCP) (LoE 2, thickening and pruning. In a meta-analysis, the pooled sensi-
strong recommendation, 93% consensus). tivity and specificity of MRCP for the diagnosis of PSC were 86%
and 94%, respectively.2727 Advantages of MRCP over endoscopic
A diagnosis of small duct PSC should be considered in retrograde cholangiopancreaticography (ERCP) include its non-
patients with elevated serum markers of cholestasis of invasive nature, lack of radiation use and lower cost, in addi-
unknown cause, normal high-quality cholangiography, tion to the potential to add MR elastography (MRE) for further
and compatible histology of PSC, particularly in those information on disease staging and prognosis.28,29
28 29 Limitations of
with concomitant inflammatory bowel disease (IBD) (LoE MRCP include poor visualisation of peripheral intrahepatic
3, strong recommendation, 88% consensus). branches, which limits the ability to diagnose very early intra-
Autoantibodies should not be used to diagnose or risk- hepatic PSC, and false-positive findings in cirrhosis of any aeti-
stratify people with PSC (LoE 4, strong recommenda- ology due to tapering and duct distortion.30,31
30 31 In a high-quality
tion, 100% consensus). MRCP, bile ducts up to third order are depicted without arti-
facts over the biliary tree and without motion blurring. For
Elevated ALP + GGT and/or bilirubin
Detailed history, physical examination
Ultrasound Dilated ducts, stones, tumor
Normal
AMA + ANA (sp100, gp210) PBC
Negative
MRCP PSC, SSC
Negative
Liver biopsy Parenchymal or biliary disease
Negative
Genetic analysis ABCB4 deficiency-(ABCB11, ATP8B1, etc.)
Fig. 1. Algorithm of diagnostic measures in chronic cholestasis (derived from20,51). 20 51 Once a positive finding has been achieved (right part of the figure),
additional diagnostic steps should be taken, if needed, according to relevant guidelines. ALP, alkaline phosphatase; AMA, anti-mitochondrial antibody; ANA, anti-
nuclear antibody; GGT, gamma-glutamyltransferase; MRCP, magnetic resonance cholangiopancreaticography; PBC, primary biliary cholangitits; PSC, primary
sclerosing cholangitis; SSC, secondary sclerosing cholangitis.
Journal of Hepatology 2022 vol. 77 j 761–806 763
Clinical Practice Guidelines
details on MRI in PSC and reporting standards please refer to the perinuclear (p-ANCA), targeting another cytoplasmic protein,
recently published position statements.26,32
26 32 myeloperoxidase. A third immunofluorescence pattern is called
A liver biopsy it not mandatory for diagnosis in patients with atypical p-ANCA (perinuclear anti-neutrophil nuclear antibody),
cholangiographic abnormalities compatible with PSC. However, directed against components of the nuclear envelope However,
in roughly 10% of cases, PSC involvement is limited to the pe- these antibodies lack diagnostic specificity. Testing for anti-
ripheral ductules and not visible in MRCP or ERCP images, so- nuclear antibody, smooth muscle antibody and anti-soluble
called small duct PSC.7 7 In these cases, a liver biopsy is required liver antigen is suggested when the diagnosis of overlapping
You might also like
- Multiple Nodul Hepar NcbiDocument6 pagesMultiple Nodul Hepar NcbisyaymaNo ratings yet
- VCE Project Report FinalDocument17 pagesVCE Project Report FinalPuneet Singh Dhani25% (4)
- Disorders of PancreasDocument17 pagesDisorders of PancreasjonasNo ratings yet
- Obstructive Jaundice Aetiological SpectrDocument8 pagesObstructive Jaundice Aetiological Spectrvvwaghmare30No ratings yet
- Imaging in Chronic PancreatitisDocument7 pagesImaging in Chronic Pancreatitisdesy 102017135No ratings yet
- Biliary PancreatitisDocument5 pagesBiliary PancreatitisJuan Francisco SánchezNo ratings yet
- Hepatic Computed Tomography and Cholangiography by Use of Gadoxetic Acid in Healthy CatsDocument11 pagesHepatic Computed Tomography and Cholangiography by Use of Gadoxetic Acid in Healthy CatsAlejandro Estrada RiosNo ratings yet
- CholangiocarcinomaDocument9 pagesCholangiocarcinomaloloalpsheidiNo ratings yet
- The Role of Imaging Methods in Identifying The CausesDocument7 pagesThe Role of Imaging Methods in Identifying The CausesJOSE ERNESTO AGUIRRE ALVAREZNo ratings yet
- AST To Platelet Ratio Index (APRI)Document8 pagesAST To Platelet Ratio Index (APRI)mummy23572No ratings yet
- Weber 2015Document12 pagesWeber 2015Nikos SerifisNo ratings yet
- ACD Ambulatory GI: Liver DiseaseDocument48 pagesACD Ambulatory GI: Liver DiseaseNuthahai SimangernNo ratings yet
- Mcevoy 2013Document17 pagesMcevoy 2013gcallupeNo ratings yet
- Art Scores Usage in Hepatocellular Carcinoma Patients With Tace TherapyDocument31 pagesArt Scores Usage in Hepatocellular Carcinoma Patients With Tace TherapyNadya Meilinar SamsonNo ratings yet
- Urine-Based Tests: UrinalysisDocument31 pagesUrine-Based Tests: Urinalysisshuvam sanatiNo ratings yet
- Article Intervention I Nurul IzatiDocument9 pagesArticle Intervention I Nurul IzatiNurul IzatiNo ratings yet
- Piis0016508507005914 PDFDocument23 pagesPiis0016508507005914 PDFHeidy Bravo RamosNo ratings yet
- Management of Primary Biliary Cirrhosis: Enny EathcoteDocument9 pagesManagement of Primary Biliary Cirrhosis: Enny EathcoteMurat HessesNo ratings yet
- Perspectives in Clinical Gastroenterology and HepatologyDocument16 pagesPerspectives in Clinical Gastroenterology and HepatologyJamie LittleNo ratings yet
- Beyond The Liver Function Tests: A Radiologist's Guide To The Liver Blood TestsDocument18 pagesBeyond The Liver Function Tests: A Radiologist's Guide To The Liver Blood Tests李冠No ratings yet
- Diagnostic Approach To Patients With Cholestatic Jaundice: ReviewDocument11 pagesDiagnostic Approach To Patients With Cholestatic Jaundice: ReviewdanaogreanuNo ratings yet
- CLD 334Document3 pagesCLD 334Joel Antonio García AlvarezNo ratings yet
- Coledocolitiasis CurrentDocument6 pagesColedocolitiasis CurrentvalNo ratings yet
- Perlemakan Hati Non-AlkoholikDocument5 pagesPerlemakan Hati Non-AlkoholikChristinaNo ratings yet
- Noninvasive Tests in The Assessment of NASH and NAFLD Fibrosis Now and Into The FutureDocument8 pagesNoninvasive Tests in The Assessment of NASH and NAFLD Fibrosis Now and Into The FutureRaeni Dwi PutriNo ratings yet
- Acute PancreatitisDocument9 pagesAcute PancreatitisestefygomezsNo ratings yet
- Management of Pancreatic Calculi An Update PDFDocument8 pagesManagement of Pancreatic Calculi An Update PDFFarid RakhmanNo ratings yet
- Management of Pancreatic Calculi: An Update: ReviewDocument8 pagesManagement of Pancreatic Calculi: An Update: ReviewFarid RakhmanNo ratings yet
- Torbenson 2018Document16 pagesTorbenson 2018Itzas SaLNo ratings yet
- Distal Cholangiocarcinoma (DCC) : Paxton V. Dickson, MD, Stephen W. Behrman, MDDocument57 pagesDistal Cholangiocarcinoma (DCC) : Paxton V. Dickson, MD, Stephen W. Behrman, MDALberta YosheNo ratings yet
- Colangita SclerozantaDocument12 pagesColangita SclerozantaChoi DongYiNo ratings yet
- Acute PancreatitisDocument2 pagesAcute PancreatitisAnonymous ysrxggk21cNo ratings yet
- Polymyalgia Rheumatica and Giant Cell Arteritis 2020Document2 pagesPolymyalgia Rheumatica and Giant Cell Arteritis 2020AnaNo ratings yet
- The Role of Elastography in ClinicallyDocument11 pagesThe Role of Elastography in ClinicallyValentina IorgaNo ratings yet
- Rol de La Endoscopia en La Sospecha de ColedocolitiasisDocument9 pagesRol de La Endoscopia en La Sospecha de ColedocolitiasisGerardo Paul Santana BazalarNo ratings yet
- A Study of Serum Calcium and Serum Albumin Levels in Predicting Severity of Acute PancreatitisDocument11 pagesA Study of Serum Calcium and Serum Albumin Levels in Predicting Severity of Acute PancreatitisIJAR JOURNALNo ratings yet
- Articulo ColedocolitiasisDocument6 pagesArticulo ColedocolitiasisMartha Carolina Hernandez UribeNo ratings yet
- Urofair 2020Document27 pagesUrofair 2020Tong YangaNo ratings yet
- Albumin Ratio As A Novel PDocument6 pagesAlbumin Ratio As A Novel PSara VelezNo ratings yet
- Czaja-2014-Clinical Liver DiseaseDocument4 pagesCzaja-2014-Clinical Liver Diseasecitra mutiarahatiNo ratings yet
- Stadializare HCCDocument12 pagesStadializare HCCIanosi BogdanNo ratings yet
- Clinchem 1263Document7 pagesClinchem 1263NEMESIS NEMESISNo ratings yet
- Liz Thomas AM Report April 25, 2008Document25 pagesLiz Thomas AM Report April 25, 2008lowellaNo ratings yet
- Evaluation of Specific Cytomorphologic Features and CA19-9 LevelsDocument6 pagesEvaluation of Specific Cytomorphologic Features and CA19-9 LevelsТетяна МагасьNo ratings yet
- Del Beke 2004Document7 pagesDel Beke 2004nitsuga oneNo ratings yet
- Clinical Practice Guidelines Slideset Hepatocellular CarcinomaDocument16 pagesClinical Practice Guidelines Slideset Hepatocellular CarcinomaSekre InternaNo ratings yet
- Accuracy of Abbreviated Protocol ofDocument5 pagesAccuracy of Abbreviated Protocol ofBella YulandaNo ratings yet
- 10 1016@j CLD 2014 09 006Document23 pages10 1016@j CLD 2014 09 006Felix camilo GonzálezNo ratings yet
- Marcadores en Cirrosis HepaticaDocument11 pagesMarcadores en Cirrosis HepaticaBelmonte FerNo ratings yet
- Secretin-Enhanced MRCP: Proceed With Cautious OptimismDocument4 pagesSecretin-Enhanced MRCP: Proceed With Cautious OptimismYuda FhunkshyangNo ratings yet
- 1356 FullDocument23 pages1356 FullYamila VicenteNo ratings yet
- Clinical Utility of MRCP in Biliary Disease.2653Document2 pagesClinical Utility of MRCP in Biliary Disease.2653Ilham BelgaNo ratings yet
- 6 Day Pediatric PancreatitisDocument16 pages6 Day Pediatric PancreatitisShreyash Haritwal100% (1)
- Urinary Biomarkers For Acute Kidney Injury in DogsDocument13 pagesUrinary Biomarkers For Acute Kidney Injury in Dogsheidy acostaNo ratings yet
- Epidemio VasculitisDocument9 pagesEpidemio VasculitisAlicia Carrera TorresNo ratings yet
- Pie 2018Document5 pagesPie 2018Tina HerreraNo ratings yet
- HepatomaDocument33 pagesHepatomaRozen RyuhaNo ratings yet
- CushDocument9 pagesCushHilalyNo ratings yet
- Adult Bile Duct StricturesDocument23 pagesAdult Bile Duct Stricturessica_17_steaua6519No ratings yet
- White-Paper USAT FinalDocument11 pagesWhite-Paper USAT FinalmicropocketfilmsNo ratings yet
- Fast Facts: Cholangiocarcinoma: Diagnostic and therapeutic advances are improving outcomesFrom EverandFast Facts: Cholangiocarcinoma: Diagnostic and therapeutic advances are improving outcomesNo ratings yet
- Champschicken Com Seocheck 2020 12 17Document17 pagesChampschicken Com Seocheck 2020 12 17Dayanand baraNo ratings yet
- Steel Material Table PDFDocument1 pageSteel Material Table PDFNathanNo ratings yet
- Cerebrospinal CSFDocument31 pagesCerebrospinal CSFRashid MohamedNo ratings yet
- Perfetti Van MelleDocument24 pagesPerfetti Van MelleYahya Niazi100% (1)
- Msds Promois W-32u 120808Document3 pagesMsds Promois W-32u 120808tia_utami23No ratings yet
- DDP Prithla 2021 Exp NoteDocument22 pagesDDP Prithla 2021 Exp Notelalit singhNo ratings yet
- Thesis Ethical HackingDocument6 pagesThesis Ethical Hackingshannonsandbillings100% (2)
- Ep English Teachers GuideDocument180 pagesEp English Teachers GuideJessy ChrisNo ratings yet
- List - Parts of Bahay Na Bato - Filipiniana 101Document7 pagesList - Parts of Bahay Na Bato - Filipiniana 101Eriellynn Liza100% (1)
- Jemal Yahyaa Software Project Managemant Case Study PrintDocument30 pagesJemal Yahyaa Software Project Managemant Case Study Printjemal yahyaaNo ratings yet
- 125 FINAL PDF Agile UX Research PDFDocument55 pages125 FINAL PDF Agile UX Research PDFMiranda Rogers100% (1)
- Lab 27Document3 pagesLab 27api-239505062No ratings yet
- Fevo 10 828503 1Document10 pagesFevo 10 828503 1keilazache2780No ratings yet
- 02 Cafe Bistro Coffeehouse Business PlanDocument21 pages02 Cafe Bistro Coffeehouse Business PlanBerihun Engda0% (1)
- CTA Pocket CardDocument2 pagesCTA Pocket CardBreitbart News100% (1)
- Einstein Hilbert Action With TorsionDocument19 pagesEinstein Hilbert Action With TorsionLillyOpenMindNo ratings yet
- Brief Hydrogeological Studies of Watershed MR-03 (37) in Context of Groundwater Estimation, Washi, Osmanabad, Maharashtra, IndiaDocument13 pagesBrief Hydrogeological Studies of Watershed MR-03 (37) in Context of Groundwater Estimation, Washi, Osmanabad, Maharashtra, IndiaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Honda CQ Eh8160akDocument37 pagesHonda CQ Eh8160aklondon335No ratings yet
- The Kinston Waterfront Now!Document46 pagesThe Kinston Waterfront Now!Kofi BooneNo ratings yet
- SHC English BulletinDocument1 pageSHC English BulletinMarcus Yee XiangNo ratings yet
- Activity Proposal For Capacity Building For TeachersLNHS 2021Document4 pagesActivity Proposal For Capacity Building For TeachersLNHS 2021ian100% (2)
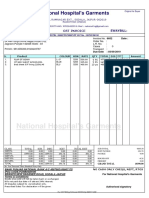
- National Hospital's GarmentsDocument1 pageNational Hospital's GarmentsShekhar GuptaNo ratings yet
- Base Institute - Namakkal - PH: 900 37 111 66: - Mock - Ibpsguide.in - 1Document288 pagesBase Institute - Namakkal - PH: 900 37 111 66: - Mock - Ibpsguide.in - 1Kartik MaheshwariNo ratings yet
- SRS Template ExampleDocument16 pagesSRS Template ExampleabcNo ratings yet
- Washing MachineDocument6 pagesWashing MachineianNo ratings yet
- Compaction of Soils 2013Document9 pagesCompaction of Soils 2013Nature NatureNo ratings yet
- Présentation XanLite 2020 ENDocument18 pagesPrésentation XanLite 2020 ENJ.DoeNo ratings yet
- The Importance of Soft Skills To A Construction ProjectDocument9 pagesThe Importance of Soft Skills To A Construction ProjectJay SayNo ratings yet
- PHP Security CPanelDocument5 pagesPHP Security CPanelManiMegalaiNo ratings yet