Professional Documents
Culture Documents
Nursing-Care-Plan - Age
Nursing-Care-Plan - Age
Uploaded by
Panda JocyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing-Care-Plan - Age
Nursing-Care-Plan - Age
Uploaded by
Panda JocyCopyright:
Available Formats
CENTRO ESCOLAR UNIVERSITY
SCHOOL OF NURSING
MANILA*MAKATI*MALOLOS
NURSING CARE PLAN
Igtanloc, Jocely, I.
BSN 2C3 Acute Gastroenteritis
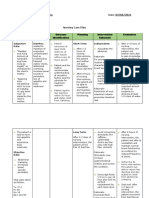
ASSESSMENT NURSING DIAGNOSIS SCIENTIFIC PLANNING INTERVENTIONS SCIENTIFIC EVALUATION
EXPLANATION (IMPLEMENTATION) RATIONALE
Subjective Data: Risk for infection due Acute Gastroenteritis Long term Outcomes: Independent Nursing Action: Independent Nursing Action: Discharge Outcome:
to insufficient is also known as Discharge Outcomes Upon Discharge, the
The baby was reported to knowledge to prevent infectious diarrhea, it 1. Obtain baseline vital 1. Fluid and electrolyte client:
have had 10 watery stools contamination is the inflammation of signs and monitor every imbalances can alter 1. Client has
over the previous 24 hours, (Inappropriate hand the gastrointestinal 1. Client will be 2-4 hours. vital body functions. reduced
during which she became hygiene, and food tract that involves reduced . frequency of
quite unsettled, restless, handling) stomach and small frequency of 2. Observe and record stools.
2. Aids in diagnosis and
irritable, crying a lot, whilst intestine. Sign and stools. stool frequency,
in monitoring the child
drinking half her usual symptoms include characteristics, amount
status
amount of liquids/milk. some combination of 2. Client’s stool and precipitating 2. The patient’s
Vomited for 4 times for the diarrhea, abdominal will able to factors. stool has
last 24 hours was also pain, fever, lack of return to more returned to
3. To avoid intestinal
reported. energy, and normal stool 3. Identify foods and more normal
irritants that can
dehydration. Elevated consistency. fluids that precipitate stool
promote intestinal
Mother claimed that WBC and platelets are diarrhea like milk, consistency.
irritation.
“Alyzzia is still on bottle an indicator of vegetables and fruits.
feeding with powder milk infection and also 3. Client will no 3. The patient has
4. It helps determine the
formula” there is a presence of longer be 4. Monitor Intake and been settled,
character of the stool
E. coli. unsettled, Output. Note character, not restless, or
and indicate fluid
Mother claimed that Alyzzia restless, or and number of stools, irritable.
balance for the client.
cannot “fall to sleep” unless irritable. estimate insensible
finishing 2 bottles with 10 fluid losses.
ounces of milk formula.
Name and Group Number Submitted to:
CENTRO ESCOLAR UNIVERSITY
SCHOOL OF NURSING
MANILA*MAKATI*MALOLOS
NURSING CARE PLAN
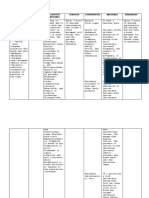
Alyzzia is also into pacifier Reference: Elliott, E. J. Short term Outcome: 5. Wash hands well 5. Helps prevents Short term Outcome:
and always with her is a (2007). Acute After 1 hour of nursing before and after transmission of After 1 hour of nursing
gastroenteritis in
small pillow as her “security intervention the contact with the child. microorganism. intervention the
children. Bmj, 334(7583),
blanket”. 35-40. clients: clients:
Collaborative Nursing Action: Collaborative Nursing Action:
As mentioned by the mother 1. Fever will be 1. Administer prescribed 1. Provides necessary 1. Fever is
Alyzzia received the manageable or oral dehydration and fluids and nutrients to manageable or
following vaccine: “BCG, within normal intravenous solutions the child. within normal
Hepatitis B, pentavalent, range range
oral polio, MMR”
2. Skin turgor, dry 2. Notify the physician if 2. To ensure early 2. Skin turgor, dry
Objective Data: lips and dry diarrhea persists, stool intervention. lips and dry
buccal mucosa characteristics change, buccal mucosa
➢ Medical history will be or other symptoms of has improved.
revealed delivery at improved. dehydration/
term via normal electrolyte imbalance
spontaneous occur
delivery, cephalic
presentation, with a
birth weight of
3910 g.
➢ Apgar score was 7-8
at one and five
minutes,
respectively.
Name and Group Number Submitted to:
CENTRO ESCOLAR UNIVERSITY
SCHOOL OF NURSING
MANILA*MAKATI*MALOLOS
NURSING CARE PLAN
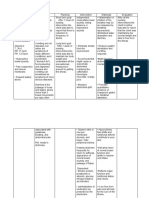
➢ Upon physical
examination
revealed an alert but
irritable and ill-
appearing infant.
Vital Signs:
T: 39.9C
PR: 145 and 160 beats/min
RR: 40 and 50 breaths/min
O2 saturation: 100%
Weight upon admission is
10.8 kg
➢ Skin was pale grey
➢ Tenting skin turgor
➢ Dry lips
➢ Dry buccal mucosa
Sunken eyes and
reduced tears
➢ Capillary refill time of
3 seconds.
➢ Urine output was
also decreased.
➢ Heart and lung
examination were
Name and Group Number Submitted to:
CENTRO ESCOLAR UNIVERSITY
SCHOOL OF NURSING
MANILA*MAKATI*MALOLOS
NURSING CARE PLAN
normal except for
tachycardia
➢ The abdomen was
swollen and slightly
painful on palpation,
no
hepatosplenomegaly.
➢ Abdominal and
thorax radiographs
were normal.
➢ There were no signs
of meningeal
irritation.
➢ Routine stool
specimen tested
positive for E. coli
whilst results for
blood and urine
culture were
negative.
Other Laboratory as follows:
Name and Group Number Submitted to:
CENTRO ESCOLAR UNIVERSITY
SCHOOL OF NURSING
MANILA*MAKATI*MALOLOS
NURSING CARE PLAN
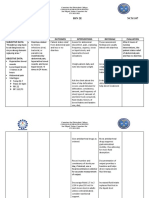
WBC/PMN (*109 /L) Result:
18/7.6
Normal range: 6–17.5/1.0–
8.5
Hb (g/dL)/ Ht (%)
Result: 12.6/ 42.2
Normal range: 11.1–14.1/
31–41
Platelets (*109 /L)
Result: 1085
Normal range: 300–750
CRP (mg/dL)
Result: <0.05
Normal range: <1
pH
Result: 7.21
Normal range: 7.38-7.46
Bicarbonate/base excess
(mEq/L)
Result: 8/-19.3
Normal range: 24-30/(-)3-
(+)3
Name and Group Number Submitted to:
CENTRO ESCOLAR UNIVERSITY
SCHOOL OF NURSING
MANILA*MAKATI*MALOLOS
NURSING CARE PLAN
BUN (mg/dL)
Result: 61
Normal range: 10-50
Na (mEq/L)
Result: 146
Normal range: 129-143
Name and Group Number Submitted to:
CENTRO ESCOLAR UNIVERSITY
SCHOOL OF NURSING
MANILA*MAKATI*MALOLOS
NURSING CARE PLAN
References:
Freedman, S. B., Adler, M., Seshadri, R., & Powell, E. C. (2006). Oral ondansetron for gastroenteritis in a pediatric emergency department. New England Journal of Medicine, 354(16), 1698-1705
Elliott, E. J. (2007). Acute gastroenteritis in children. Bmj, 334(7583), 35-40
GASTROENTERITIS, S. O. A. (1996). Practice parameter: the management of acute gastroenteritis in young children. Pediatrics, 97(3), 424-435
Hartman, S., Brown, E., Loomis, E., & Russell, H. A. (2019). Gastroenteritis in children. American family physician, 99(3), 159-165.
Mushtaq, A., Khan, S., Zeb, F., Ain, Q., Syed, A., & Khattak, F. (2016). Risk factors associated with gastroenteritis in children 2-5 years of age attending Rehman Medical Institute
Peshawar. American Journal of Food Science and Health, 2(5), 94-101.
Burkhart, D. M. (1999). Management of acute gastroenteritis in children. American Family Physician, 60(9), 2555.
Name and Group Number Submitted to:
You might also like
- Screem-Res Description 1Document4 pagesScreem-Res Description 1Jeanne Marie Vales100% (2)
- Rle Worksheet Nursing ProcessDocument6 pagesRle Worksheet Nursing ProcessMARVIE JOY BALUMA CABIOCNo ratings yet
- Nursing Care Plan (Bowel Elemination)Document8 pagesNursing Care Plan (Bowel Elemination)Rijane Tabonoc Omlang100% (1)
- Nursing Care Plan Diarrhea Assessment Diagnosis Planning Interventions Rationale EvaluationDocument8 pagesNursing Care Plan Diarrhea Assessment Diagnosis Planning Interventions Rationale EvaluationKrah100% (1)
- "Nagsusuka Ang Anak Ko.": Nursing Care ProcessDocument2 pages"Nagsusuka Ang Anak Ko.": Nursing Care Processgeorgia50% (2)
- Gym Business PlanDocument20 pagesGym Business Plany_37860234250% (4)
- Nursing Care Plan 1Document2 pagesNursing Care Plan 1Denise GabatoNo ratings yet
- NCP Nausea and VomitingDocument4 pagesNCP Nausea and VomitingKingJayson Pacman06No ratings yet
- Assessment Nursing Diagnosis Scientific Explanation Planning Nursing Intervention Rationale Evaluation Subjective: IndependentDocument2 pagesAssessment Nursing Diagnosis Scientific Explanation Planning Nursing Intervention Rationale Evaluation Subjective: IndependentgeorgiaNo ratings yet
- DiarrheaDocument3 pagesDiarrheaBert GasalNo ratings yet
- Nursing Care Plan: Cues Nursing Diagnosi S Analysis GOAL and Objectives Intervention Rationale EvaluationDocument5 pagesNursing Care Plan: Cues Nursing Diagnosi S Analysis GOAL and Objectives Intervention Rationale EvaluationMark Allison BuenaventuraNo ratings yet
- NCP Acute GastroenteritisDocument3 pagesNCP Acute GastroenteritisVhiance Czaramae LahuranNo ratings yet
- Diarrhea (AGE)Document2 pagesDiarrhea (AGE)NursesLabs.com100% (1)
- Ate Gabs Nyo Pagod NaDocument3 pagesAte Gabs Nyo Pagod NaGabrielle EvangelistaNo ratings yet
- Nursing Care Plan: Assessment Nursing Diagnosis Rationale Desired Outcome Nursing Intervention Justification EvaluationDocument2 pagesNursing Care Plan: Assessment Nursing Diagnosis Rationale Desired Outcome Nursing Intervention Justification EvaluationDan MandigNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale Evaluation Subjective Data: Short Term: Independent: Short Term: Goal Partially MetDocument3 pagesAssessment Diagnosis Planning Implementation Rationale Evaluation Subjective Data: Short Term: Independent: Short Term: Goal Partially MetPrincess Mildred AbdonNo ratings yet
- Diarrhea Nursing Care PlanDocument2 pagesDiarrhea Nursing Care PlanKrizha Angela NicolasNo ratings yet
- Case Study: Subjective: Objective: General Objective: Independent IndependentDocument10 pagesCase Study: Subjective: Objective: General Objective: Independent IndependentChristine EmanNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermLorie May GuillangNo ratings yet
- NCP BPHDocument1 pageNCP BPHyasiraNo ratings yet
- Borata Nursing Process RleDocument11 pagesBorata Nursing Process Rlefiel borataNo ratings yet
- Care PlanDocument4 pagesCare PlanRapunzel LeanneNo ratings yet
- Fluid Volume Deficit R/T Diarrhea & VomitingDocument4 pagesFluid Volume Deficit R/T Diarrhea & Vomitingjisoo100% (3)
- NCP High Risk PregnancyDocument7 pagesNCP High Risk PregnancyRica ParcasioNo ratings yet
- ACTUAL PROBLEM: Diarrhea Related To Parasitic Infection As Manifested by Loose Liquid Stools 3 Times in 24 HoursDocument4 pagesACTUAL PROBLEM: Diarrhea Related To Parasitic Infection As Manifested by Loose Liquid Stools 3 Times in 24 HoursRal CasingNo ratings yet
- Gonzaga Rlems - NCPDocument3 pagesGonzaga Rlems - NCPShaynne Wencille A. GONZAGANo ratings yet
- Assessment Nursing Diagnosis Plannin G Nursing Intervention Rationale Evaluatio NDocument4 pagesAssessment Nursing Diagnosis Plannin G Nursing Intervention Rationale Evaluatio NMarineth O. LasicNo ratings yet
- "Nagtatae Siya 4 Days Na" As Verbalized by The Mother. Inatake of Causative Agents Irritation of The Stomach Inflammation of The Stomach Increase GI Motility DiarrrheaDocument4 pages"Nagtatae Siya 4 Days Na" As Verbalized by The Mother. Inatake of Causative Agents Irritation of The Stomach Inflammation of The Stomach Increase GI Motility DiarrrheaMelissa MhelNo ratings yet
- Nursing Care Plan: Sex: Wt. On Admission: DateDocument5 pagesNursing Care Plan: Sex: Wt. On Admission: DateAhmed SanadNo ratings yet
- Age NCPDocument3 pagesAge NCPMartin Allen ClaudioNo ratings yet
- Activity 5 NCPDocument5 pagesActivity 5 NCPAl-Mujib TanogNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale Evaluation Subjective Data: Objective Data: Short Term: Independent: Short Term: Goal Partially MetDocument3 pagesAssessment Diagnosis Planning Implementation Rationale Evaluation Subjective Data: Objective Data: Short Term: Independent: Short Term: Goal Partially MetCess YNo ratings yet
- KUSAIN - NCP IN NCM 112 RLE ConstipationDocument2 pagesKUSAIN - NCP IN NCM 112 RLE Constipationjay kusainNo ratings yet
- Diarrhea NCP Pedia WardDocument4 pagesDiarrhea NCP Pedia WardKyle DapulagNo ratings yet
- Group-5 NCM-107 NCPDocument4 pagesGroup-5 NCM-107 NCPbulok netflakes100% (1)
- NCP 1Document3 pagesNCP 1Mary Antonette Adriano EnriquezNo ratings yet
- F. NCP ProperDocument4 pagesF. NCP ProperAle SandraNo ratings yet
- Bert Mao Nani Final Promise HahahaahDocument10 pagesBert Mao Nani Final Promise HahahaahHerbert EstremosNo ratings yet
- Irritable Bowel SyndromeDocument6 pagesIrritable Bowel SyndromeHANNAH MICOLE GAERLANNo ratings yet
- Relos, Kristel Joyce D. Bsn2e - NCPDocument3 pagesRelos, Kristel Joyce D. Bsn2e - NCPKristel Joyce RelosNo ratings yet
- Evaluation of ConstipationDocument8 pagesEvaluation of ConstipationAndrea GallegoNo ratings yet
- NCP Case Analysis GastritisDocument7 pagesNCP Case Analysis GastritisSteffi GolezNo ratings yet
- Diarrhea: University of Santo Tomas-LegazpiDocument4 pagesDiarrhea: University of Santo Tomas-LegazpiJOSHUA DICHOSONo ratings yet
- NCP FinalDocument18 pagesNCP FinalHelen GonzalesNo ratings yet
- Volume 1Document2 pagesVolume 1roxybiscanteNo ratings yet
- Prado NCPDocument4 pagesPrado NCPalleah pradoNo ratings yet
- NCP CholeraDocument2 pagesNCP CholeraMichael Angelo Garcia RafananNo ratings yet
- Risk NCP - PESCADERO 4CDocument1 pageRisk NCP - PESCADERO 4COrlando VillanuevaNo ratings yet
- NCP Urine RetentionDocument4 pagesNCP Urine RetentionKingJayson Pacman06No ratings yet
- Javier, Jomar A. BSN121 Group 83 Nursing Care Plan (Pediatric Patient)Document7 pagesJavier, Jomar A. BSN121 Group 83 Nursing Care Plan (Pediatric Patient)Julie AnnNo ratings yet
- Rabang, Eloisa Janelle (NCP & DRUG STUDY)Document14 pagesRabang, Eloisa Janelle (NCP & DRUG STUDY)Mariam Yiani Aspiras RacelesNo ratings yet
- Assessment Diagnosis Scientific Explanatation Planning Interventions Rationale EvaluationDocument2 pagesAssessment Diagnosis Scientific Explanatation Planning Interventions Rationale EvaluationLatrell GelacioNo ratings yet
- NCP 1. Molar PregnancyDocument2 pagesNCP 1. Molar PregnancyMaria Eliza AgustinoNo ratings yet
- Activity On Care PlanningDocument4 pagesActivity On Care PlanningRichlle CortesNo ratings yet
- Maraming Tubig at Kakain NG Prutas para Makadumi Ako."Document2 pagesMaraming Tubig at Kakain NG Prutas para Makadumi Ako."Cayla Mae CarlosNo ratings yet
- Name: de Guzman, Cameron Josh B. Section: 2Bsn-ADocument3 pagesName: de Guzman, Cameron Josh B. Section: 2Bsn-ACameron De GuzmanNo ratings yet
- Nursing Care Plan Diarrhea Assessment Diagnosis Planning Interventions Rationale EvaluationDocument8 pagesNursing Care Plan Diarrhea Assessment Diagnosis Planning Interventions Rationale EvaluationKrahNo ratings yet
- NCP PediatricDocument5 pagesNCP PediatricSL Hanna NebridaNo ratings yet
- Nursing Care Plan: Diarrhea R/T Infectious Scientific: Goal: IndependentDocument4 pagesNursing Care Plan: Diarrhea R/T Infectious Scientific: Goal: IndependentKingJayson Pacman06No ratings yet
- BSN2 C Ihps NCP FinalDocument7 pagesBSN2 C Ihps NCP FinalAdrian DecolongonNo ratings yet
- Intestinal Failure: Diagnosis, Management and TransplantationFrom EverandIntestinal Failure: Diagnosis, Management and TransplantationAlan LangnasNo ratings yet
- 11 BurnDocument31 pages11 Burnjitendra magarNo ratings yet
- Factors of Care During Pregnancy, ScreeningsDocument38 pagesFactors of Care During Pregnancy, ScreeningssabhyaNo ratings yet
- The Perfect 24 Hour Meal PlanDocument7 pagesThe Perfect 24 Hour Meal PlanZX LeeNo ratings yet
- Page 1 of 908Document1,510 pagesPage 1 of 908dominicgonzalesrsNo ratings yet
- Experiment 5 LipidsDocument13 pagesExperiment 5 LipidsClemence Marie FuentesNo ratings yet
- Healthcare SymbolsDocument66 pagesHealthcare SymbolsHosam GomaaNo ratings yet
- Baaleman 2021 CHP - 10.1007 - 978 3 030 80068 0 - 21 Ver PDFDocument26 pagesBaaleman 2021 CHP - 10.1007 - 978 3 030 80068 0 - 21 Ver PDFcLAUDIANo ratings yet
- Optimistic Thinking: Educator GuideDocument33 pagesOptimistic Thinking: Educator GuideRaluca RaluNo ratings yet
- Health Economic GrowthDocument25 pagesHealth Economic GrowthCarmen Ulloa MéndezNo ratings yet
- Justice and Experimentalism PDFDocument29 pagesJustice and Experimentalism PDFRobert ChapmanNo ratings yet
- Compliance Checklist For Garment IndustryDocument9 pagesCompliance Checklist For Garment Industryprasadbpotdar100% (1)
- Demncia Frontotemporal ContinumDocument25 pagesDemncia Frontotemporal ContinumcositaamorNo ratings yet
- Health Education and Health Promotion - OkanegaraDocument40 pagesHealth Education and Health Promotion - OkanegaraKristian Dwi CahyaNo ratings yet
- Funcional Properties of Bioctive Peptides Derived From MeatDocument22 pagesFuncional Properties of Bioctive Peptides Derived From MeatJohanna RomeroNo ratings yet
- Case Study: John Woodbury: More Information Later That Will Most Likely Change Your Hypothesis)Document11 pagesCase Study: John Woodbury: More Information Later That Will Most Likely Change Your Hypothesis)Rld AndreiNo ratings yet
- Fire Incident Report: Complete and and Fax One Copy To The Appropriate Agency Field Office (See Fax Numbers At: HTTPDocument2 pagesFire Incident Report: Complete and and Fax One Copy To The Appropriate Agency Field Office (See Fax Numbers At: HTTPbenonNo ratings yet
- Passport Appointment ScheduleDocument3 pagesPassport Appointment ScheduleSonia ShinoharaNo ratings yet
- Sample Project ProposalDocument4 pagesSample Project ProposalAlyssa Mae AzarconNo ratings yet
- Marlboro Brand AuditDocument17 pagesMarlboro Brand AuditScott HurleyNo ratings yet
- OutliningDocument6 pagesOutliningOREJOLA, IRISH VAN C.No ratings yet
- DMSCO Log Book Vol.50 1972Document57 pagesDMSCO Log Book Vol.50 1972Des Moines University Archives and Rare Book RoomNo ratings yet
- BETA VitaHop CaseSty R2Document1 pageBETA VitaHop CaseSty R2ALEJANDRO AstudilloNo ratings yet
- Combining CareersDocument1 pageCombining CareersManoj PurohitNo ratings yet
- Daftar Obat Floorstock RuanganDocument3 pagesDaftar Obat Floorstock Ruangandini mahdianiNo ratings yet
- Coblation in ENTDocument45 pagesCoblation in ENTDr. T. BalasubramanianNo ratings yet
- Rguhs Thesis Topics in PeriodontologyDocument4 pagesRguhs Thesis Topics in Periodontologyjennifernultonevansville100% (2)
- CRANIOTOMYDocument5 pagesCRANIOTOMYJesha PlatigueNo ratings yet
- 8 - Blood Banking and SerologyDocument4 pages8 - Blood Banking and SerologyRanndolf Javier80% (5)