Professional Documents
Culture Documents
Parathyroid Hormone Metabolism
Parathyroid Hormone Metabolism
Uploaded by
Assault AmphibiansCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Parathyroid Hormone Metabolism
Parathyroid Hormone Metabolism
Uploaded by
Assault AmphibiansCopyright:
Available Formats
mini review www.kidney-international.
org
Parathyroid hormone metabolism and signaling in
health and chronic kidney disease
Pieter Evenepoel1,4, Jordi Bover2,4 and Pablo Ureña Torres3,4
1
KU Leuven, Department of Immunology and Microbiology, Laboratory of Nephrology and University Hospitals Leuven, Department of
Nephrology and Renal Transplantation, B-3000 Leuven, Belgium; 2Fundació Puigvert, Department of Nephrology, IIB Sant Pau, RedinREn,
Barcelona, Catalonia, Spain; 3Ramsay-Générale de Santé, Clinique du Landy, Service de Néphrologie-Dialyse, Saint Ouen, France, INSERM
U1151-CNRS UMR8253 Université Paris Descartes, and Service des Explorations Fonctionnelles, Hôpital Necker-Enfants Malades, Paris,
France; and 4Board member of the ERA-EDTA CKD-MBD Working Group
C
Circulating parathyroid hormone (PTH) shows a complex hronic kidney disease (CKD)–mineral bone disorder is
relationship with hard outcomes in subjects with chronic a systemic disorder that describes the complex bone
kidney disease (CKD). Moreover, intervention studies and mineral abnormalities that occur in CKD. Sec-
directly targeting PTH failed to yield unequivocal results. ondary hyperparathyroidism (SHPT) is an integral compo-
Disturbed PTH metabolism, posttranslational modifications nent of CKD–mineral bone disorder and, if left unchecked,
of PTH, and end-organ hyporesponsiveness to PTH may leads to a worsening of laboratory abnormalities, bone dis-
explain the poor performance of PTH as an outcome ease, and soft-tissue calcification.1 In recent years, insights
biomarker and precise target of therapy in the setting of into the pathogenesis of SHPT have improved, and the ther-
CKD, at least in the gray middle target zone. PTH fragments apeutic armamentarium to tackle this condition has
accumulate in CKD patients and may exert effects that are expanded. However, the relationship between circulating
distinct from, if not opposite to biointact (1-84)PTH. parathyroid hormone (PTH) concentration and outcomes
Posttranslational modification of PTH and especially in CKD patients is complex and rather weak, unless at the
oxidation may alter the interaction of PTH with its receptor. extremes. In this mini review, we discuss factors and mecha-
Its clinical relevance, however, remains a matter of ongoing nisms underlying the disappointing performance of PTH as
debate. Less controversial is the issue of end-organ an outcome biomarker and target of therapy in CKD and
hyporesponsiveness to PTH. This phenomenon, formally therefore focus on the underappreciated role of end-organ
referred to as PTH resistance, has long been recognized in hyporesponsiveness to PTH.
CKD, but factors and mechanisms contributing to it remain
poorly defined. Subsequent evidence identified
PTH METABOLISM AND SIGNALING IN HEALTH
downregulation of the PTH receptor and competing PTH metabolism
downstream signals as underlying pathophysiologic PTH is a single-chain hormone of 84 amino acids that is
mechanisms. End-organ hyporesponsiveness to PTH in mainly produced by chief cells of the parathyroid glands. PTH
CKD, along with important analytical and biological is cleaved from pre-pro–PTH and thereafter stored in secre-
variability, renders defining the PTH target range in CKD tory granules awaiting 1 of 2 fates: circadian and pulsatile
challenging. Although this may still be accomplished at the secretion or intracellular degradation. Synthesis and secretion
population level, it may prove to be very difficult at the of PTH are tightly regulated by extracellular calcium (Ca2þ).
individual level. This is a disillusioning thought in an era of Hypercalcemia not only reduces overall PTH secretion but
personalized medicine. Parallel to the search of a functional also favors release of PTH fragments, whereas hypocalcemia
and readily available assay quantifying PTH signaling tone stimulates overall PTH secretion and favors (1-84)PTH
or sensitivity, additional biomarkers (or a panel of release. After secretion, (1-84)PTH and its fragments are
biomarkers) should be formally evaluated. further metabolized in the kidney and liver.2 The half-life of
Kidney International (2016) 90, 1184–1190; http://dx.doi.org/10.1016/ C-terminal PTH fragments is much longer than the half-life
j.kint.2016.06.041
of (1-84)PTH, being 2 to 4 minutes. Thus, circulating PTH
KEYWORDS: CKD; hyperparathyroidism; mineral metabolism; parathyroid is a heterogeneous mixture of full-length hormone and
hormone
fragments, with (7-84)PTH accounting for as much as 50% of
Copyright ª 2016, International Society of Nephrology. Published by
Elsevier Inc. All rights reserved. overall PTH.3
Increasingly specific PTH assays have been developed over
the years. Second-generation assays are currently the most
Correspondence: P. Evenepoel, Dienst nefrologie, Universitair Ziekenhuis widely implemented. They use a capture antibody that binds
Gasthuisberg, Herestraat 49, B-3000 Leuven, Belgium. E-mail: near the N-terminus and a second solid phase–coupled
Pieter.Evenepoel@uzleuven.be antibody that binds to the C-terminus. Differences in anti-
Received 7 May 2016; revised 24 June 2016; accepted 27 June 2016; body specificities and affinities of the assays translate in
published online 18 September 2016 differing recovery of (1-84)PTH and differing cross-reactivity
1184 Kidney International (2016) 90, 1184–1190
P Evenepoel et al.: PTH hyporesponsiveness in CKG mini review
with (7-84)PTH and other fragments. This may explain, anabolic or catabolic, appears to depend on the duration and
together with the lack of an agreed-on common standard periodicity of PTH exposure. Bone resorption predominates
(calibrator), the large variability that exists among commer- in response to continuous exposure to high circulating PTH
cially available second-generation PTH assays.4 The third- levels, whereas intermittent PTH administration leads to a net
generation assay uses the same capture antibody, but the increase in bone mass. Continuous, as compared with inter-
detection antibody is more specific for the first 4 amino acids mittent, PTH exposure regulates in bone cells different sets of
of PTH, thereby avoiding cross-reactivity with the N-terminal genes or, alternatively, affects the same sets of genes in a
truncated PTH fragments. PTH shows homology with PTH- sustained versus transient manner, the first favoring bone
related peptide (PTHrP), the molecule responsible for most resorption and the second bone formation. PTH1R signaling
humoral hypercalcemia of malignancies; however, PTHrP in osteoblasts and osteocytes can increase the receptor acti-
does not cross-react with PTH in those PTH assays. vator of nuclear factor-kB ligand/osteoprotegerin (RANKL/
OPG) ratio. The OPG-RANKL-RANK pathway appears to be
PTH signaling the main mediator of the catabolic actions of PTH. Moreover,
PTH and PTHrP exert their multiple actions by binding to continuous exposure to PTH causes a sustained upregulation
PTH/PTHrP type 1 receptor (PTH1R). PTH1R is highly of monocyte chemoattractant protein-1, another mediator of
expressed in bone and kidney, but also at lower levels in the bone resorption. The anabolic effect of PTH on bone,
vasculature and in other tissues at various times throughout conversely, seems to be mediated largely through canonical
development. PTH1R is a 7-transmembrane, G protein– Wnt signaling. PTH may increase Wnt signaling both directly
coupled receptor linked to heterotrimeric G proteins Gs and and indirectly (e.g., by repressing the osteocytic expression of
Gq. The activation of PTHR1 by PTH signals through several secreted Wnt antagonist sclerostin5) (Figure 1).
intracellular pathways, including protein kinase A and protein PTH also interacts with skeletal endocrine functions.8
kinase C, although a preference for certain pathways is Again, the dynamics of exposure seem to be of importance.
apparent in each organ and function, which depends on the Whereas short-term (1-34)PTH infusion studies showed
presence or the absence of the sodium-dependent hydrogen suppressed circulating fibroblast growth factor 23 (FGF23)
exchanger regulatory factor-1.3 Termination of PTH1R levels, longer term infusion studies showed a delayed increase
signaling is achieved through negative feedback of PTH in FGF23, most probably in response to the PTH-induced
secretion in response to restoration of Ca2þ levels or by a increase in circulating calcitriol.9
desensitization-internalization process of the receptor.3,5 Kidney. In the kidney, PTH stimulates Ca2þ reabsorption
In addition to PTH1R, a second G protein–coupled PTH in the distal convoluted tubule by activating specific ion
receptor, PTH2R, has been identified. The PTH2R normally channels. It also increases urinary phosphate excretion mainly
responds to tuberoinfundibular peptide 39, but is inhibited by by regulating sodium-phosphate cotransporters in the prox-
PTH and does not interact with PTHrP. PTH2R is expressed imal convolute tubule via both protein kinase A– and protein
in various tissues, but its function is still poorly understood. kinase C–dependent pathways. It also indirectly enhances
Finally, a receptor has been characterized in osteoblasts intestinal Ca2þ and phosphate absorption by stimulating the
and osteocytes with specificity for the C-terminal region of renal production of 1,25-dihydroxy-vitamin D3.3
PTH (C-PTHR).6,7 Although much remains to be learned
about the C-PTH/C-PTHR system, available evidence in- Nonclassic target organs of PTH
dicates that it seems to act antagonistically to the PTH/ PTH1R is expressed in various other tissues, including the
PTH1R system. A major effect of C-PTHR activation could be pancreas, bone marrow, and vasculature. PTH and PTHrP exert
the suppression of osteocytic osteolysis. acute vasodilatory actions through PTH1R activation in
vascular smooth muscle cells and reduce vascular oxidative
Classic target organs of PTH stress and procalcific and profibrotic signals that drive arte-
Bone. PTH plays an important role in maintaining Ca2þ riosclerotic disease.10 These actions may be considered para-
homeostasis and in bone remodeling. PTH pulses and sus- doxical when viewed against the backdrop of the hypertension
tained PTH elevations promote calcium release from the bone and vascular disease arising in the setting of primary hyper-
using various mechanisms with markedly different kinetics. parathyroidism. It is suggested that the vasculopathy of SHPT
PTH-mediated Ca2þ release from a rapid skeletal exchange- may relate to an arterial desensitization to paracrine PTHrP/
able pool and osteocytic osteolysis are thought to underlie the PTH1R-dependent regulation of vascular tone and/or renal
acute (minute-hours) response to hypocalcemia. The slow hemodynamics in addition to direct toxic effects mediated by
response, which takes several days, is driven by bone cells high calcium and/or phosphate levels, often accompanying
involved in the remodeling process. SHPT. Thus strategies that selectively preserve the paracrine
Various paracrine and endocrine signals participate in PTHrP/PTH1R pathway are generally predicted to exert car-
bone remodeling, with PTH playing a central role. Direct diovascular benefits, with reduced calcification, restricted
effects of PTH on osteoblasts and osteocytes and indirect neointimal formation, and appropriate regional tissue perfu-
actions on osteoclasts promote both bone formation and sion in response to physiologic demands reflecting preservation
bone resorption. The final effect on bone mass, either of healthy conduit artery structure and function.10 Diseases or
Kidney International (2016) 90, 1184–1190 1185
mini review P Evenepoel et al.: PTH hyporesponsiveness in CKG
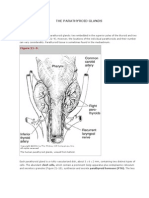
Figure 1 | Parathyroid hormone (PTH) and bone metabolism. PTH elicits bone anabolic and catabolic effects by stimulating both bone
formation and, indirectly, bone resorption. PTH exerts its action by binding to the PTH type 1 receptor (PTH1R) mainly expressed on osteoblasts
and osteocytes. PTH may increase osteoanabolic Wnt signaling both directly and indirectly (e.g., by repressing the osteocytic expression of
secreted Wnt antagonist sclerostin). FZD, frizzled; LRP, low-density lipoprotein receptor; OPG, osteoprotegerin; PKA, protein kinase A; RANKL,
receptor activator of nuclear factor-kB (ligand).
interventions impeding paracrine PTHrP/PTH1R signaling, primary hyperparathyroidism, bone and renal phenotypes
conversely, may foster vascular disease. markedly differ. Indeed, patients with primary hyperpara-
The biological actions of PTH thus extend beyond main- thyroidism show high-normal calcitriol levels, hyper-
taining mineral and bone metabolism to include endocrine, calciuria, and high bone turnover. To the contrary, these
immunologic, and cardiovascular effects. Most recently, features are not universally present in CKD patients with
PTHrP/PTH1R signaling has also been demonstrated to fos- SHPT. Thus, high circulating PTH levels in CKD are not
ter wasting and muscle atrophy.11 This further strengthens the necessarily paralleled by increased PTH signaling or at least
notion of PTH as an important uremic toxin. PTH signaling is attenuated. Disturbed PTH metabolism,
posttranslational modifications, and end-organ hypores-
PTH METABOLISM AND SIGNALING IN CKD ponsiveness to PTH probably contribute to the complex
Although data from the CRIC (Chronic Renal Insufficiency relationship between circulating PTH and outcomes in CKD
Cohort) study pointed out that PTH concentrations start to (Figure 2).
increase once the estimated glomerular filtration rate drops
below 45 ml/min per 1.73 m2, more recent data from a Swiss Disturbed PTH metabolism in CKD
population–based cohort study show a steady increase of PTH PTH metabolism is disturbed in CKD,2,13 which results in a
concentrations paralleling the estimated glomerular filtration marked prolongation of the half-life of C-terminal PTH
rate decline and already being significant at an estimated fragments. Clinical data show a proportional increase in C-
glomerular filtration rate of 126 ml/min per 1.73 m2.12 In terminal PTH fragments versus biointact PTH during the
patients with advanced CKD, SHPT is an almost universal progression of CKD. Mounting evidence indicates that
complication. Both enhanced PTH synthesis and secretion C-terminal PTH fragments, by binding to the PTH1R or C-
and increased parathyroid gland mass contribute to the high PTHR, exert biological effects that are distinct if not opposite
circulating PTH levels in CKD. The pathogenesis of SHPT is of (1-84)PTH.9
complex, involving multiple closely interacting factors. These
include Ca2þ, phosphate, calcitriol, FGF23, Klotho, and Posttranslational PTH modification in CKD
uremic toxins. In addition, normal inhibitory feedback Proteins in the human body, in both health and disease, are
mechanisms become deficient in CKD due to downregulation exposed to chemical reactions capable of altering their
of the parathyroid Ca2þ-sensing, vitamin D, and FGF23/ structural and functional properties. Substantial carbamyla-
Klotho receptors. End-organ hyporesponsiveness to the tion or glycation of key proteins (including albumin, eryth-
action of PTH may also contribute to the exacerbation of ropoietin, low-density lipoprotein, and collagen) has been
SHPT in CKD because higher and higher levels of PTH are reported in CKD.14 Although glycation and carbamylation of
progressively needed to maintain Ca2þ homeostasis. PTH have so far not been reported, recent evidence indicates
Despite CKD patients generally present with serum PTH that PTH may be oxidized to a variable extent in patients with
levels that are many times higher than those of patients with CKD.15 Oxidized PTH loses its biological activity as it fails to
1186 Kidney International (2016) 90, 1184–1190
P Evenepoel et al.: PTH hyporesponsiveness in CKG mini review
(–)
(–)
(–)
cAMP
Figure 2 | Impact of chronic kidney disease (CKD) on parathyroid hormone (PTH) metabolism and signaling. CKD has an impact on many
aspects of PTH metabolism and signaling: (i) increased synthesis and secretion, parathyroid cell proliferation, and vitamin D receptor (VDR) and
calcium-sensing receptor (CaSR) downregulation; (ii) accumulation of C-terminal PTH fragments; (iii) posttranslational modification of PTH; (iv)
competitive inhibition between (1-84)PTH and its fragments; (v) PTH type 1 receptor (PTH1R) downregulation; (vi) PTH1R dysfunction; (vii)
inhibitory or competing downstream signals. cAMP: cyclic adenosine monophosphate; FGF23, fibroblast growth factor 23; FGFR1, fibroblast
growth factor receptor 1; LPS, lipopolysaccharide; PhosR, phosphate-sensing receptor.
bind its receptor. Oxidation of methionine residue 8 seems PTH is blunted, but not absent. Other conditions associated
especially crucial in generating conformational changes in with PTH hyporesponsiveness include aging, black race, and
the secondary structure of PTH. A high-resolution liquid diabetes. The concept of PTH hyporesponsiveness in CKD is
chromatography and/or mass spectrometry method was not novel but remains underappreciated in the nephrology
developed (so-called fourth-generation assay) to reliably community. Its pathogenesis, moreover, is complex and only
quantify oxidized PTH in serum samples.15 Although of in- partly understood. Multiple factors are involved including
terest, confirmatory studies are warranted because PTH phosphate loading, calcitriol deficiency, oxidative stress,
oxidation could also occur as an ex vivo artifact. aluminum overload, magnesium deficiency, accumulation of
PTH fragments, and uremic toxins,16 inducing deficiencies in
PTH hyporesponsiveness in CKD trophic factors, excesses of growth inhibitors, or receptor or
The bone and renal responses to the action of PTH are postreceptor defects. Recent evidence points to decreased
progressively impaired in CKD, a condition commonly PTH1R expression and function and competing downstream
referred to as PTH resistance. We consider the term hypo- signals in addition to local environmental factors as
responsiveness more appropriate because the response to contributing mechanisms.
Kidney International (2016) 90, 1184–1190 1187
mini review P Evenepoel et al.: PTH hyporesponsiveness in CKG
PTH1R downregulation. Renal failure in rodents is asso- CLINICAL RELEVANCE OF PTH HYPORESPONSIVENESS
ciated with a decreased expression of PTH1R (at least at the Linear (simple) associations have been reported between
mRNA level) in various tissues and on cells, including circulating PTH levels and bone outcomes (bone turnover,
bone17–19 and renal tubular cells.20 Human data are less bone loss, fractures) in patients with primary hyperparathy-
consistent, with some investigators demonstrating decreased roidism. Conversely, the association between circulating PTH
expression21 and others reporting increased expression22 of levels and outcomes in CKD patients is complex, often
PTH1R in uremic conditions. This apparent discrepancy reported as curvilinear and overall rather weak.32,33 CKD-
remains to be explained. Both analytical issues and case mix induced changes in PTH metabolism and signaling substan-
may be involved. Although the mechanisms responsible for tially and distinctly affect the relationship between PTH and
the (putative) desensitization or downregulation of PTH1R in hard outcomes (i.e., bone disease, vascular calcification, sur-
CKD remain poorly defined, several lines of evidence impli- vival). PTH hyporesponsiveness is as much an integral
cated C-terminal PTH fragments and cellular oxidative stress. component of CKD mineral bone disorder as elevated
PTH fragments. PTH fragments may suppress PTH circulating PTH levels.
signaling by promoting PTH1R downregulation in both bone Regarding bone, not only the accumulation of PTH frag-
and kidney cells.23 Additionally, PTH fragments may oppose ments but also the multifactorial desensitization of the
PTH signaling by both acting as competitive inhibitors of PTH1R may explain why low-turnover bone disease is very
bioactive PTH and activating the C-PTHR.7 (7-84)PTH is prevalent in contemporary CKD patients, although these
suggested to be a component of a feedback mechanism at the patients often demonstrate circulating PTH levels far above
level of the parathyroid gland, bone, or both.9,24 According to the upper normal limit.30,34 Cohort studies clearly showed
this reasoning, increased bioactive PTH may, in addition to that only at the extremes is PTH able to predict the bone-
increasing bone turnover, foster the secretion of (7-84)PTH turnover status with acceptable sensitivity/specificity.1
by the parathyroid gland, which in turn limits the actions of There is close interaction between bone and vasculature in
the bioactive molecule on bone. CKD, commonly referred to as the bone-vascular axis. Low-
Cellular oxidative stress. A diminished calcemic response to turnover bone disease is closely associated with vascular dis-
the infusion of bioactive PTH and/or downregulation of the ease, especially calcification. The underlying pathophysiologic
skeletal and renal PTH1R has been observed in para- mechanisms are complex and incompletely understood. In a
thyroidectomized uremic rats and in uremic rats with PTH recent cross-sectional study, peripheral artery disease was
levels maintained within the normal range.16 This indicates the found to be associated with significant reductions in the
involvement of factors beyond PTH fragments in the patho- skeletal anabolic response to PTH.35 Thus, PTH hypores-
genesis of PTH hyporesponsiveness in uremia.25 Subsequent ponsiveness may be the common soil for low-turnover bone
experimental studies pointed to a circulating factor,26 most disease and vascular disease and might indeed explain the
likely uremic toxins triggering cellular oxidative stress, such as coincidence of these diseases in CKD.
indoxyl sulfate and inflammatory bioactive lipids (e.g., ox-
LDL), as the most likely culprit.27,28 Increased oxidative CONCLUSIONS AND FUTURE DIRECTIONS
stress, a common condition in CKD, may thus be in the causal Monitoring PTH is routine clinical practice in nephrology
pathway between CKD and PTH hyporesponsiveness. care. Much has been inferred from increased PTH values,
Dysfunctional PTH1R. A recent study suggested that solu- both in terms of skeletal integrity and fractures and in terms
ble Klotho might interact with the PTH1R on renal tubular of clinical outcomes for patients. However, recent data from
cells and thereby prevent binding of bioactive PTH. As FGF23 epidemiologic and intervention studies questioned the val-
increases the release of soluble Klotho, it may thus be idity of PTH as a consistent outcome biomarker and target of
hypothesized that part of the effect of FGF23 in lowering therapy in CKD. Altered PTH metabolism and PTH hypo-
calcitriol is mediated by impairing PTH signaling.29 responsiveness along with a high biological variability may
explain why a circulating PTH level, unless at the extremes,
Competing downstream PTHR1 signals and local performs poorly as biomarker.
environmental factors Although defining an optimal PTH range may be chal-
The downstream effects of PTH may be offset by competing lenging but accomplishable at the population level, this
and/or inhibitory paracrine and endocrine signals, mediated might be a very difficult task at the patient level. This is a
by, for example, high sclerostin and osteoprotegerin, low bone disillusioning thought in an era of personalized medicine.
morphogenetic protein 7, and Klotho, in addition to local Some even hastily advocated that given its many limitations,
environmental factors (e.g., acid base disturbances, inflam- the time has come to abandon PTH as an outcome
mation).30 Increased osteocytic sclerostin expression has biomarker and target of therapy in CKD.36 It should be
indeed been observed in early-stage CKD.31 Of note, circulating emphasized that no biomarker so far clearly proved to be
osteoprotegerin and sclerostin levels are many times higher in superior to PTH in predicting bone metabolism in CKD.
advanced CKD than counterparts with normal kidney func- More research is needed. Meanwhile, more frequent PTH
tion. To what extent circulating sclerostin levels reflect bone testing, enabling PTH trends to be captured accurately, rather
expression and affect local signaling remains to be investigated. than abandoning PTH monitoring should remain the motto.
1188 Kidney International (2016) 90, 1184–1190
P Evenepoel et al.: PTH hyporesponsiveness in CKG mini review
The striking increase in low bone turnover disease in patients 9. Wesseling-Perry K, Harkins GC, Wang HJ, et al. The calcemic response to
continuous parathyroid hormone (PTH)(1-34) infusion in end-stage
with end-stage renal disease in recent decades clearly points kidney disease varies according to bone turnover: a potential role for
to overtreatment of secondary hyperparathyroidism. Better PTH(7-84). J Clin Endocrinol Metab. 2010;95:2772–2780.
knowledge of the issue of PTH hyporesponsiveness may help 10. Cheng SL, Shao JS, Halstead LR, et al. Activation of vascular smooth
muscle parathyroid hormone receptor inhibits Wnt/beta-catenin
to turn the tide. Obviously, PTH levels less than 2 times the signaling and aortic fibrosis in diabetic arteriosclerosis. Circ Res. 2010;107:
upper normal limit should be avoided in patients with 271–282.
advanced CKD. 11. Kir S, Komaba H, Garcia AP, et al. PTH/PTHrP Receptor Mediates Cachexia
in Models of Kidney Failure and Cancer. Cell Metab. 2016;23:315–323.
Additional efforts are mandatory to improve diagnostics. A 12. Dhayat N, Ackermann D, Pruijm M, et al. Fibroblast growth factor 23 and
functional and readily available assay quantifying PTH1R markers of mineral metabolism in indviduals with preserved renal
signaling tone or sensitivity would be a great step forward. function. Kidney Int. 2016;90:648–657.
13. Brossard JH, Yamamoto LN, D’Amour P. Parathyroid hormone
Parallel to the development of such an assay, the performance metabolites in renal failure: bioactivity and clinical implications. Semin
of more specific biomarkers (or a panel of biomarkers) Dial. 2002;15:196–201.
should be tested, if possible, against the gold standard (e.g., a 14. Gajjala PR, Fliser D, Speer T, et al. Emerging role of post-translational
modifications in chronic kidney disease and cardiovascular disease.
bone biopsy when evaluating bone integrity). An increasing
Nephrol Dial Transplant. 2015;30:1814–1824.
body of evidence points to (bone-specific) alkaline phos- 15. Hocher B, Armbruster FP, Stoeva S, et al. Measuring parathyroid
phatase as a promising adjunct to PTH. Because no hormone (PTH) in patients with oxidative stress–do we need a fourth
generation parathyroid hormone assay? PLoS One. 2012;7:e40242.
biomarker is free of limitations (renal clearance and meta-
16. Llach F, Bover J. Renal osteodystrophies. In: Brenner BM, ed. The Kidney,
bolism, high biological variability), bone biopsies may still be 6th ed. Philadelphia, PA: W.B. Saunders; 2000:2103–2186.
needed in some conditions. Recent technical advances 17. Iwasaki-Ishizuka Y, Yamato H, Nii-Kono T, et al. Downregulation of
reduced morbidity and may help to lower the threshold for parathyroid hormone receptor gene expression and osteoblastic
dysfunction associated with skeletal resistance to parathyroid hormone
this diagnostic procedure, allowing a better understanding in in a rat model of renal failure with low turnover bone. Nephrol Dial
the future of the narrow link between circulating PTH con- Transplant. 2005;20:1904–1911.
centration, PTH-hyporesponsiveness, and hard outcomes. 18. Urena P, Mannstadt M, Hruby M, et al. Parathyroidectomy does not
prevent the renal PTH/PTHrP receptor down-regulation in uremic rats.
Kidney Int. 1995;47:1797–1805.
DISCLOSURE 19. Urena P, Ferreira A, Morieux C, et al. PTH/PTHrP receptor mRNA is down-
All the authors declared no competing interests. regulated in epiphyseal cartilage growth plate of uraemic rats. Nephrol
Dial Transplant. 1996;11:2008–2016.
20. Urena P, Kubrusly M, Mannstadt M, et al. The renal PTH/PTHrP receptor is
down-regulated in rats with chronic renal failure. Kidney Int. 1994;45:
ACKNOWLEDGMENTS
605–611.
PE has received speaker’s and advisory board honoraria from Amgen,
21. Picton ML, Moore PR, Mawer EB, et al. Down-regulation of human
Shire, Sanofi-Genzyme, and Vifor-Fresenius and research grants from osteoblast PTH/PTHrP receptor mRNA in end-stage renal failure. Kidney
Amgen, Sanofi-Genzyme, and Tecomedical. JB declares having Int. 2000;58:1440–1449.
received speaker’s and/or advisory board honoraria from Abbvie, 22. Pereira RC, Delany AM, Khouzam NM, et al. Primary osteoblast-like cells
Amgen, Sanofi-Genzyme, Shire, Vifor/Fresenius-Pharma, Medice, and from patients with end-stage kidney disease reflect gene expression,
Chugai. proliferation, and mineralization characteristics ex vivo. Kidney Int.
PUT has received speaker’s honoraria, clinical trial studies 2015;87:593–601.
honoraria, and advisory board honoraria from Amgen, Shire, Astellas, 23. Alonso V, Magyar CE, Wang B, et al. Ubiquitination-deubiquitination
Hemotech, and Vifor-Fresenius. balance dictates ligand-stimulated PTHR sorting. J Bone Miner Res.
2011;26:2923–2934.
24. Huan J, Olgaard K, Nielsen LB, Lewin E. Parathyroid hormone 7-84
REFERENCES induces hypocalcemia and inhibits the parathyroid hormone 1-84
1. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work secretory response to hypocalcemia in rats with intact parathyroid
Group. KDIGO clinical practice guideline for the diagnosis, evaluation, glands. J Am Soc Nephrol. 2006;17:1923–1930.
prevention, and treatment of Chronic Kidney Disease-Mineral and Bone 25. Bover J, Jara A, Trinidad P, et al. The calcemic response to PTH in the rat:
Disorder (CKD-MBD). Kidney Int Suppl. 2009;113:S1–S130. effect of elevated PTH levels and uremia. Kidney Int. 1994;46:310–317.
2. Hruska KA, Korkor A, Martin K, Slatopolsky E. Peripheral metabolism of 26. Disthabanchong S, Hassan H, McConkey CL, et al. Regulation of PTH1
intact parathyroid hormone. Role of liver and kidney and the effect of receptor expression by uremic ultrafiltrate in UMR 106-01 osteoblast-like
chronic renal failure. J Clin Invest. 1981;67:885–892. cells. Kidney Int. 2004;65:897–903.
3. Lee M, Partridge NC. Parathyroid hormone signaling in bone and kidney. 27. Sage AP, Lu J, Atti E, et al. Hyperlipidemia induces resistance to PTH
Curr Opin Nephrol Hypertens. 2009;18:298–302. bone anabolism in mice via oxidized lipids. J Bone Miner Res. 2011;26:
4. Souberbielle JC, Roth H, Fouque DP. Parathyroid hormone measurement 1197–1206.
in CKD. Kidney Int. 2009;77:93–100. 28. Nii-Kono T, Iwasaki Y, Uchida M, et al. Indoxyl sulfate induces skeletal
5. Silva BC, Bilezikian JP. Parathyroid hormone: anabolic and catabolic resistance to parathyroid hormone in cultured osteoblastic cells. Kidney
actions on the skeleton. Curr Opin Pharmacol. 2015;22:41–50. Int. 2007;71:738–743.
6. Murray TM, Rao LG, Divieti P, Bringhurst FR. Parathyroid hormone 29. Takenaka T, Inoue T, Miyazaki T, et al. Xeno-Klotho inhibits parathyroid
secretion and action: evidence for discrete receptors for the carboxyl- hormone signaling. J Bone Miner Res. 2016;31:455–462.
terminal region and related biological actions of carboxyl-terminal 30. Drueke TB, Massy ZA. Changing bone patterns with progression of
ligands. Endocr Rev. 2005;26:78–113. chronic kidney disease. Kidney Int. 2016;89:289–302.
7. Divieti P, John MR, Juppner H, Bringhurst FR. Human PTH-(7-84) inhibits 31. Sabbagh Y, Graciolli FG, O’Brien S, et al. Repression of osteocyte Wnt/
bone resorption in vitro via actions independent of the type 1 PTH/ beta-catenin signaling is an early event in the progression of renal
PTHrP receptor. Endocrinology. 2002;143:171–176. osteodystrophy. J Bone Miner Res. 2012;27:1757–1772.
8. Vervloet MG, Massy ZA, Brandenburg VM, et al. Bone: a new endocrine 32. Floege J, Kim J, Ireland E, et al. Serum iPTH, calcium and phosphate, and
organ at the heart of chronic kidney disease and mineral and bone the risk of mortality in a European haemodialysis population. Nephrol
disorders. Lancet Diabetes Endocrinol. 2014;2:427–436. Dial Transplant. 2011;26:1948–1955.
Kidney International (2016) 90, 1184–1190 1189
mini review P Evenepoel et al.: PTH hyporesponsiveness in CKG
33. Fishbane S, Hazzan AD, Jhaveri KD, et al. Bone parameters and risk of hip 35. London GM, Marchais SJ, Guerin AP, de Vernejoul MC. Ankle-brachial
and femur fractures in patients on hemodialysis. Clin J Am Soc Nephrol. index and bone turnover in patients on dialysis. J Am Soc Nephrol.
2016;11:1063–1072. 2015;26:476–483.
34. Sprague SM, Bellorin-Font E, Jorgetti V, et al. Diagnostic accuracy of bone 36. Garrett G, Sardiwal S, Lamb EJ, Goldsmith DJ. PTH–a particularly tricky
turnover markers and bone histology in patients with CKD treated by hormone: why measure it at all in kidney patients? Clin J Am Soc Nephrol.
dialysis. Am J Kidney Dis. 2016;67:559–566. 2013;8:299–312.
1190 Kidney International (2016) 90, 1184–1190
You might also like
- Dokumen - Tips - Autism 2018 Klinghardt Institute Autism 2018 Dietrich Klinghardt MD PHD LondonDocument33 pagesDokumen - Tips - Autism 2018 Klinghardt Institute Autism 2018 Dietrich Klinghardt MD PHD LondonakiniramNo ratings yet
- Experiment 4 PCR and Cloning of Alpha-Amylase Gene in E. ColiDocument12 pagesExperiment 4 PCR and Cloning of Alpha-Amylase Gene in E. ColiJiaying ChenNo ratings yet
- The Immunology of Human ReproductionDocument171 pagesThe Immunology of Human ReproductionEkanita Desiani100% (1)
- Silva 2015Document10 pagesSilva 2015Jia-PeiWuNo ratings yet
- Critical Governance Issue of Parathyroid Hormone ADocument9 pagesCritical Governance Issue of Parathyroid Hormone AnikhilmajethiaNo ratings yet
- Parathyroid HormoneDocument17 pagesParathyroid HormoneВладимир ДружининNo ratings yet
- Elecsys PTH (1-84) : Cobas e 801 English System InformationDocument5 pagesElecsys PTH (1-84) : Cobas e 801 English System Informationsyafiq_82No ratings yet
- Short ReportDocument4 pagesShort ReportMWNo ratings yet
- Pathophysiology Primary HyperparathyroidismDocument3 pagesPathophysiology Primary HyperparathyroidismIronic SunNo ratings yet
- Hormonul PTHDocument12 pagesHormonul PTHMonica MonikaNo ratings yet
- Comparison Between Whole and Intact Parathyroid Hormone AssaysDocument8 pagesComparison Between Whole and Intact Parathyroid Hormone AssaysElise BalloNo ratings yet
- Receptors For Parathyroid Hormone (PTH) and PTH-Related PeptideDocument25 pagesReceptors For Parathyroid Hormone (PTH) and PTH-Related PeptideAnonymous qBsWolDnoNo ratings yet
- Clinical Guidelines and PTH Measurement: Does Assay Generation Matter?Document13 pagesClinical Guidelines and PTH Measurement: Does Assay Generation Matter?Elise BalloNo ratings yet
- Ma 2001Document8 pagesMa 2001Jia-PeiWuNo ratings yet
- Leptin Is Produced by Parathyroid Glands and Stimulates Parathyroid Hormone SecretionDocument9 pagesLeptin Is Produced by Parathyroid Glands and Stimulates Parathyroid Hormone Secretionadi suputraNo ratings yet
- PHP2018Document25 pagesPHP2018radu nicolaeNo ratings yet
- 5 Parathyroid Hormone5Document58 pages5 Parathyroid Hormone5Rawbeena RamtelNo ratings yet
- tmp9CE3 TMPDocument10 pagestmp9CE3 TMPFrontiersNo ratings yet
- Cellular Mechanisms of Renal Osteodystrophy: J A. H and M L. PDocument6 pagesCellular Mechanisms of Renal Osteodystrophy: J A. H and M L. PTaha Hussian AlfairesNo ratings yet
- The Parathyroid GlandsDocument7 pagesThe Parathyroid GlandsRuth AlooNo ratings yet
- Joint Bone SpineDocument6 pagesJoint Bone Spineyayan_adiutama98No ratings yet
- Beyond The Fixed Setpoint of The Hypothalamus-Pituitary-Thyroid AxisDocument12 pagesBeyond The Fixed Setpoint of The Hypothalamus-Pituitary-Thyroid AxisJuliany AscanioNo ratings yet
- Pseudohypoparathyroidism-Literature Update 2018Document8 pagesPseudohypoparathyroidism-Literature Update 2018radu nicolaeNo ratings yet
- Pathophysiology of Primary HyperparathyroidismDocument9 pagesPathophysiology of Primary HyperparathyroidismMuhamad ZulfiqarNo ratings yet
- Thyroid Hormone Research PaperDocument8 pagesThyroid Hormone Research Paperjtbowtgkf100% (1)
- J of Bone Mineral Res - 2022 - Khan - Efficacy and Safety of Parathyroid Hormone Replacement With TransCon PTH inDocument12 pagesJ of Bone Mineral Res - 2022 - Khan - Efficacy and Safety of Parathyroid Hormone Replacement With TransCon PTH insiskaNo ratings yet
- Degortari 2020Document8 pagesDegortari 2020Sergio Guillermo Cuevas CarbonellNo ratings yet
- 10 1002@jbm4 10479Document6 pages10 1002@jbm4 10479Wev LimaNo ratings yet
- Cancers Prostate ScreeningDocument12 pagesCancers Prostate ScreeningMed. TrackNo ratings yet
- Journal of Internal Medicine - 2018 - Nilsson - Primary Hyperparathyroidism Should Surgery Be Performed On All PatientsDocument16 pagesJournal of Internal Medicine - 2018 - Nilsson - Primary Hyperparathyroidism Should Surgery Be Performed On All PatientsPryangka Viana MartinsNo ratings yet
- Normal PTH Levels in Primary Hyperparathyroidism: Still The Same Disease?Document6 pagesNormal PTH Levels in Primary Hyperparathyroidism: Still The Same Disease?ritvikNo ratings yet
- Hungry Bone Syndrome After Parathyroidectomy For Primary Hyperthyroidism 2161 1076 4 168Document5 pagesHungry Bone Syndrome After Parathyroidectomy For Primary Hyperthyroidism 2161 1076 4 168oki harisandiNo ratings yet
- Accepted Manuscript: Mechanisms of Ageing and DevelopmentDocument30 pagesAccepted Manuscript: Mechanisms of Ageing and DevelopmentIvi VenturiNo ratings yet
- Glicerofosfato de Sodio Vs InogarnicoDocument8 pagesGlicerofosfato de Sodio Vs InogarnicojhonNo ratings yet
- Primary Hyperparathyroidism (PHPT) in Children: Two Case Reports and Review of The LiteratureDocument6 pagesPrimary Hyperparathyroidism (PHPT) in Children: Two Case Reports and Review of The LiteratureTimothy supitNo ratings yet
- PTH and PTH Antagonist Induce Different Conformational Changes in The PTHR1 ReceptorDocument10 pagesPTH and PTH Antagonist Induce Different Conformational Changes in The PTHR1 ReceptorMiguel Angel Aguilar LuisNo ratings yet
- Https:/mdpi Res - Com/d Attachment/ijms/ijms 20 04976/article Deploy/iDocument15 pagesHttps:/mdpi Res - Com/d Attachment/ijms/ijms 20 04976/article Deploy/iRajan JattNo ratings yet
- Management of Secondary HyperparathyroidismDocument9 pagesManagement of Secondary HyperparathyroidismStephen MasengiNo ratings yet
- Central Hypothyroidism: Pathogenic, Diagnostic, and Therapeutic ChallengesDocument11 pagesCentral Hypothyroidism: Pathogenic, Diagnostic, and Therapeutic ChallengesCroitort53No ratings yet
- 16 Long TermDocument16 pages16 Long TermsiskaNo ratings yet
- Management of Normocalcemic Primary HyperparathyroidismDocument19 pagesManagement of Normocalcemic Primary HyperparathyroidismErika AvilaNo ratings yet
- 756 FullDocument9 pages756 FullNindi CeyNo ratings yet
- Funcional Analysis of PTHIR Variants Found in Primary Failure of EruptionDocument8 pagesFuncional Analysis of PTHIR Variants Found in Primary Failure of EruptionvivgaitanNo ratings yet
- Atomoxetine Research PapersDocument4 pagesAtomoxetine Research Papersfalk_leeNo ratings yet
- Tryptophan Metabolism and Gut-Brain HomeostasisDocument23 pagesTryptophan Metabolism and Gut-Brain HomeostasisLuísa OliveiraNo ratings yet
- tmpE99B TMPDocument16 pagestmpE99B TMPFrontiersNo ratings yet
- HyperparathyroidismDocument15 pagesHyperparathyroidismMuhamad ZulfiqarNo ratings yet
- 2011 - Hutchenson, Et Al - Serotonin Receptors and Valve Heart Disease - It Was Meant 2BDocument29 pages2011 - Hutchenson, Et Al - Serotonin Receptors and Valve Heart Disease - It Was Meant 2Bcolompar80No ratings yet
- Physiology, Parathyroid Hormone (PTH) : Statpearls (Internet)Document10 pagesPhysiology, Parathyroid Hormone (PTH) : Statpearls (Internet)chafeb febiNo ratings yet
- BJP6 v. 170Document24 pagesBJP6 v. 170LourdesNo ratings yet
- Veterinaria 3 2019 Lunetta ENGDocument8 pagesVeterinaria 3 2019 Lunetta ENGlaisuniforNo ratings yet
- Secondary Hyperparathyroidism - Pathogenesis, Disease Progression, and Therapeutic OptionsDocument9 pagesSecondary Hyperparathyroidism - Pathogenesis, Disease Progression, and Therapeutic OptionsJuanita GonzálezNo ratings yet
- Eje 257Document15 pagesEje 257Sam SoeteNo ratings yet
- Lazcano Et Al Ethanol 2012Document10 pagesLazcano Et Al Ethanol 2012lazcanoivan7No ratings yet
- Direct Action of The Parathyroid Hormone-Like Human Hypercalcemic FactorDocument5 pagesDirect Action of The Parathyroid Hormone-Like Human Hypercalcemic FactorRo KohnNo ratings yet
- Hyperserotonemia in Autism: The Potential Role of 5HT-related Gene VariantsDocument6 pagesHyperserotonemia in Autism: The Potential Role of 5HT-related Gene VariantsWesley MuhammadNo ratings yet
- Rhythms in The Endocrine System of Fish: A Review: ArticleDocument34 pagesRhythms in The Endocrine System of Fish: A Review: ArticleBagas Lantip PrakasaNo ratings yet
- Serum Testosterone Levels in Male Hypogonadism - Why and When To Check-A Review 2017Document9 pagesSerum Testosterone Levels in Male Hypogonadism - Why and When To Check-A Review 2017Sara Velásquez JNo ratings yet
- Bone CaseDocument36 pagesBone Caseroquiyabegum1611No ratings yet
- Pharmacokinetics of L-Triiodothyronine in Patients Undergoing Thyroid Hormone Therapy WithdrawalDocument9 pagesPharmacokinetics of L-Triiodothyronine in Patients Undergoing Thyroid Hormone Therapy Withdrawalletycia469No ratings yet
- Pathogenesis and Treatment of Renal Osteodystrophy: Eduardo Slatopolsky Esther Gonzalez Kevin MartinDocument9 pagesPathogenesis and Treatment of Renal Osteodystrophy: Eduardo Slatopolsky Esther Gonzalez Kevin Martinmohammed makkiNo ratings yet
- Tyroid 10Document6 pagesTyroid 10Anonymous UTUWFODCEYNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 17: OncologyFrom EverandComplementary and Alternative Medical Lab Testing Part 17: OncologyNo ratings yet
- 1.05 Qualitative 0 Quantitative Platelet DisordersDocument9 pages1.05 Qualitative 0 Quantitative Platelet DisordersShiena ArchividoNo ratings yet
- UntitledDocument57 pagesUntitledAkram chaudaryNo ratings yet
- IndianJClinExpOphthalmol 6-4-497 500Document4 pagesIndianJClinExpOphthalmol 6-4-497 500Yogesh SinghNo ratings yet
- Development of DNA Barcode For Magnoliopsida and LDocument9 pagesDevelopment of DNA Barcode For Magnoliopsida and LarisNo ratings yet
- Introduction To OncologyDocument199 pagesIntroduction To Oncologyshivangi khatriNo ratings yet
- Molecular Characterisation of A Novel and Highly Divergent Passerine Adenovirus 1Document16 pagesMolecular Characterisation of A Novel and Highly Divergent Passerine Adenovirus 1Abdul jNo ratings yet
- Midbio14 ExamDocument32 pagesMidbio14 ExamEren SevinceNo ratings yet
- Cell Cycle and Division: 11.1 ChromosomesDocument10 pagesCell Cycle and Division: 11.1 ChromosomesEstee ChowNo ratings yet
- ModuleIII Advanced META-ANALYSIS RevisedDocument92 pagesModuleIII Advanced META-ANALYSIS RevisedRajendra LamsalNo ratings yet
- Traits Parent Offspring: - Genetics - Study of How Are Passed From ToDocument17 pagesTraits Parent Offspring: - Genetics - Study of How Are Passed From ToJohn Dexter JumalonNo ratings yet
- Nitrogenase - WikipediaDocument8 pagesNitrogenase - WikipediafoonganNo ratings yet
- What Is Natural SelectionDocument3 pagesWhat Is Natural SelectionAli RazaNo ratings yet
- (Acero) Week 4 PT - Research Report On Immunotherapy and Its AdvancementsDocument3 pages(Acero) Week 4 PT - Research Report On Immunotherapy and Its AdvancementsPaul AceroNo ratings yet
- Jurnal Internasional Giardia LambliaDocument4 pagesJurnal Internasional Giardia LambliaAhmad FirdausNo ratings yet
- The Limb Girdle Muscular Dystrophies and The 15Document24 pagesThe Limb Girdle Muscular Dystrophies and The 15Mazin Al-TahirNo ratings yet
- AnaPhy Reviewer PrelimsDocument7 pagesAnaPhy Reviewer Prelimsysa hernandezNo ratings yet
- Biochemistry and Molecular Biology 6Th Edition Snape Full ChapterDocument67 pagesBiochemistry and Molecular Biology 6Th Edition Snape Full Chapterebony.blanchard211100% (4)
- New Microsoft Word DocumentDocument13 pagesNew Microsoft Word Documentskchakraborty9143No ratings yet
- Unit 2 Vocab List-TAGDocument2 pagesUnit 2 Vocab List-TAGmymle1No ratings yet
- Lecture 1 CarbohydrateDocument58 pagesLecture 1 CarbohydrateDAVIE MATIASNo ratings yet
- Food MicrobiologyDocument7 pagesFood MicrobiologyJuan Jose Escobar P.No ratings yet
- NCERT Solutions For Class 11 Biology Chapter 8 - Cell The Unit of Life - .Document10 pagesNCERT Solutions For Class 11 Biology Chapter 8 - Cell The Unit of Life - .susilmaji92No ratings yet
- IMAT Humanitas 2015Document36 pagesIMAT Humanitas 2015niloofarNo ratings yet
- Curriculum Vitae: Parvez Singh SlathiaDocument3 pagesCurriculum Vitae: Parvez Singh SlathiaJohn DoeNo ratings yet
- 0610 s19 QP 41 PDFDocument20 pages0610 s19 QP 41 PDFrachitNo ratings yet
- Pedigree Analysis Online I 2 I 3 MYPDocument32 pagesPedigree Analysis Online I 2 I 3 MYPMedinaNo ratings yet
- Full Chapter Immunology An Illustrated Outline 6Th Edition David Male PDFDocument53 pagesFull Chapter Immunology An Illustrated Outline 6Th Edition David Male PDFmitchell.wasmund863100% (5)