Professional Documents
Culture Documents
Cancer Care Platinum
Cancer Care Platinum
Uploaded by
Star HealthOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cancer Care Platinum
Cancer Care Platinum
Uploaded by
Star HealthCopyright:
Available Formats
ii.
Renewal shall not be denied on the ground that the insured person had made a claim or claims in the preceding
Cancellation table applicable with instalment option of Half-yearly premium payment frequency policy years Schedule of Benefits Premium Chart Excluding Tax
iii. Request for renewal along with requisite premium shall be received by the Company before the end of the policy
Period on risk Rate of premium to be retained Section I : Base Cover
period
Up to 1 Mth 45% of the total premium received iv. At the end of the policy period, the policy shall terminate and can be renewed within the Grace Period of 30 days Is this part of the
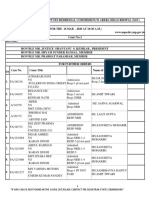
Subject / Sum Insured Premium Per Year (in Rs.)
to maintain continuity of benefits without break in policy. Coverage is not available during the grace period 5 7.5 10 sum insured/In addition
(INR in Lac)
Exceeding one mth up to 4 mths 87.5% of the total premium received to the sum insured
v. No loading shall apply on renewals based on individual claims experience Age Band /
5,00,000 7,50,000 10,00,000
Exceeding 4 mths up to 6 mths 100% of the total premium received Sum Insured (Rs.)
Possibility of Revision of Terms of the Policy lncluding the Premium Rates
Exceeding 6 mths up to 7 mths 65% of the total premium received In-patient Hospitalization Single Standard A/C Room Part of the sum insured 5m-29 14,285 17,995 20,870
The Company, with prior approval of lRDAl, may revise or modify the terms of the policy including the premium rates.
Exceeding 7 mths up to 10 mths 85% of the total premium received The insured person shall be notified three months before the changes are effected. ICU, Doctor Fee, Medicines, 30-39 16,190 20,370 23,605
Covered Part of the sum insured
Tests
Exceeding 10 mths 100% of the total premium received Premium Payment In Instalments 40-49 18,050 22,750 26,340
lf the insured person has opted for Payment of Premium on an instalment basis i.e. Half Yearly or Quarterly as Day Care Procedures Covered Part of the sum insured
Cancellation table applicable with instalment option of Quarterly premium payment frequency mentioned in the policy Schedule/Certificate of Insurance, the following Conditions shall apply (notwithstanding any 50-59 19,875 25,130 29,075
terms contrary elsewhere in the policy);
Period on risk Rate of premium to be retained for one eye - 60-69 24,430 30,845 35,830
i. Grace Period of 7 days would be given to pay the instalment premium due for the policy.
ii. During such grace period, coverage will not be available from the due date of instalment premium till the date of for one eye - 30,000 40,000/- &
Up to 1 Mth 87.5% of the total premium received Cataract Limit (INR) Part of the sum insured Above 69 28,990 36,540 42,385
per policy year - 40,000 per policy
receipt of premium by Company.
year - 60,000 Section II : Lump sum cover for Cancer (Optional Cover)
Exceeding one mth up to 3 mths 100% of the total premium received iii. The insured person will get the accrued continuity benefit in respect of the "Waiting Periods", "Specific Waiting
Periods" in the event of payment of premium within the stipulated grace Period Premium Per Year (in Rs.)
Exceeding 3 mths up to 4 mths 87.5% of the total premium received
iv. No interest will be charged lf the instalment premium is not paid on due date Emergency Road Ambulance Covered Part of the sum insured
Exceeding 4 mths up to 6 mths 100% of the total premium received v. ln case of instalment premium due not received within the grace period, the policy will get cancelled Age Band /
2,50,000 3,75,000 5,00,000
vi. ln the event of a claim, all subsequent premium instalments shall immediately become due and payable Pre Hospitalization Expenses 30 days Part of the sum insured Sum Insured (Rs.)
Exceeding 6 mths up to 7 mths 85% of the total premium received
vii. The company has the right to recover and deduct all the pending installments from the claim amount due under 60 days (up to 2% of the basic 5m-29 10,135 15,200 20,265
Exceeding 7 mths up to 9 mths 100% of the total premium received the policy Post Hospitalization Expenses Part of the sum insured
sum insured per hospitalization)
30-39 10,135 15,200 20,265
Exceeding 9 mths up to 10 mths 85% of the total premium received
Free Look Period Health Check-Up
40-49 10,135 15,200 20,265
Exceeding 10 mths 100% of the total premium received The Free Look Period shall be applicable on new individual health insurance policies and not on renewals or at the time (available for every claim 2,500/- 2,500/- 2,500/- In addition to the sum insured
of porting/migrating the policy. free year) 50-59 10,135 15,200 20,265
Notwithstanding anything contained herein or otherwise, no refunds of premium shall be made in respect of The insured person shall be allowed free look period of fifteen days from date of receipt of the policy document to
Cancellation where, any claim has been admitted or has been lodged or any benefit has been availed by the insured review the terms and conditions of the policy, and to return the same if not acceptable. Medical Second Opinion Available - 60-69 10,135 15,200 20,265
person under the policy. lf the insured has not made any claim during the Free Look Period, the insured shall be entitled to;
5% for every claim free year maximum Above 69 10,135 15,200 20,265
ii. The Company may cancel the policy at any time on grounds of misrepresentation non-disclosure of material i. a refund of the premium paid less any expenses incurred by the Company on medical examination of the insured No Claim Bonus -
facts, fraud by the insured person by giving 15 days' written notice. There would be no refund of premium on up to 50%
person and the stamp duty charges or
cancellation on grounds of misrepresentation, non-disclosure of material facts or fraud ii. where the risk has already commenced and the option of return of the policy is exercised by the insured person, a Diet and Nutrition Program, Weight The information provided in this brochure is only indicative. For more details on the risk factors, terms and
Automatic Expiry deduction towards the proportionate risk premium for period of cover or Management programme and Specialist conditions, please read the policy wordings before concluding a sale.
Wellness Services -
iii. where only a part of the insurance coverage has commenced, such proportionate premium commensurate with Consultation available through
The insurance under this policy with respect to each relevant Insured Person policy shall expire immediately on the Or
Star Tele-Health App
earlier of the following events: the insurance coverage during such period; Visit Website: www.starhealth.in
i. Upon the death of the Insured Person. Rehabilitation &
Enhancement of Sum insured Covered up to 10% of the Sum Insured Part of the sum insured
ii. Upon exhaustion of the Basic sum insured plus bonus under the policy. Pain management
Sum insured once opted cannot be enhanced even on renewal.
Migration Modern Treatments Covered (up to the sub-limits) Part of the sum insured
Withdrawal of the policy
The insured person will have the option to migrate the policy to other health insurance products/plans offered by the
company by applying for migration of the Policy atleast 30 days before the policy renewal date as per IRDAI i. In the likelihood of this product being withdrawn in future, the Company will intimate the insured person about the
Hospice Care Up to 20% of the Basic Sum Insured in life time Part of the sum insured
guidelines on Migration. lf such person is presently covered and has been continuously covered without any lapses same 90 days prior to expiry of the policy.
under any health insurance product/plan offered by the company, the insured person will get the accrued continuity ii. lnsured Person will have the option to migrate to similar health insurance product available with the Company at
the time of renewal with all the accrued continuity benefits such as cumulative bonus, waiver of waiting period. as Optional Cover
benefits in waiting periods as per IRDAI guidelines on migration.
For Detailed Guidelines on migration, kindly refer the link per IRDAI guidelines, provided the policy has been maintained without a break.
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.aspx?page=PageNo3987 Lump-sum benefit for Cancer
Buy this insurance IRDAI IS NOT INVOLVED IN ACTIVITIES LIKE SELLING INSURANCE POLICIES,
Portability (INR in Lac) 2.5 3.75 5 -
Please contact our nearest Branch Office /our Agent or visit our website www.starhealth.in for online purchase ANNOUNCING BONUS OR INVESTMENT OF PREMIUMS. PUBLIC RECEIVING
Insurance is the subject matter of solicitation
(Waiting period 30 months)
The insured person will have the option to port the policy to other insurers by applying to such insurer to port the
entire policy along with all the members of the family, if any, at least 45 days before, but not earlier than 60 days from Tax Benefits SUCH PHONE CALLS ARE REQUESTED TO LODGE A POLICE COMPLAINT
the policy renewal date as per IRDAI guidelines related to portability. lf such person is presently covered and has Payment of premium by any mode other than cash for this insurance is eligible for relief under Section 80D of the
Waiting Period
been continuously covered without any lapses under any health insurance policy with an lndian General/Health Income Tax Act 1961.
insurer, the proposed insured person will get the accrued continuity benefits in waiting periods as per IRDAI
Star Cancer Care Platinum Insurance Policy
guidelines on portability. Prohibition of Rebates Initial waiting period 30 days (except for Accidents) - Unique Identification No.: SHAHLIP22031V022122
BRO / SCCP/ V.1 / 2021
For Detailed Guidelines on portability, kindly refer the link Section 41 of Insurance Act 1938 (Prohibition of rebates): No person shall allow or offer to allow, either directly or
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.aspx?page=PageNo3987 indirectly, as an inducement to any person to take out or renew or continue an insurance in respect of any kind of risk For specific diseases 24 months -
Buy this Insurance Online at www.starhealth.in
relating to lives or property in India, any rebate of the whole or part of the commission payable or any rebate of the
Renewal premium shown on the policy, nor shall any person taking out or renewing or continuing a policy accept any rebate, For Pre-Existing diseases Call Toll-free: 1800-425-2255 / 1800-102-4477,
30 months -
The policy shall ordinarily be renewable except on grounds of fraud, misrepresentation by the Insured Person; except such rebate as may be allowed in accordance with the published prospectuses or tables of the insurer: Any (including Cancer) sms STAR to 56677 « Fax Toll Free No: 1800-425-5522
i. The Company shall endeavor to give notice for renewal. However, the Company is not under obligation to give person making default in complying with the provisions of this section shall be liable for a penalty which may extend to Email : support@starhealth.in
For Hospice Care 12 months -
any notice for renewal ten lakhs rupees. CIN : U66010TN2005PLC056649 « IRDAI Regn. No: 129
6 7 8
· The second opinion should be only for medical reasons and not for medico-legal purposes. B. In case of enhancement of sum insured the exclusion shall apply afresh to the extent of sum insured 3. The member has to be 18 years of age or older and 26. Unconventional, Untested, Experimental therapies - Code Excl 27
STAR CANCER CARE PLATINUM INSURANCE POLICY · Any liability due to any errors or omission or consequences of any action taken in reliance of the second increase. 4. Body Mass Index (BMI); 27. Chondrocyte Implantation, Procedures using Platelet Rich plasma and Intra articular injection therapy -
Unique Identification No.: SHAHLIP22031V022122 opinion provided by the Medical Practitioner is outside the scope of this policy. C. If the Insured Person is continuously covered without any break as defined under the portability norms of a. greater than or equal to 40 or Code Excl 28
· Utilizing this facility alone will not be considered as a claim. the extant IRDAI (Health Insurance) Regulations, then waiting period for the same would be reduced to b. greater than or equal to 35 in conjunction with any of the following severe co-morbidities following
Star Cancer Care Platinum Insurance Policy offers protection for persons diagnosed with Cancer. The policy keeps the the extent of prior coverage. failure of less invasive methods of weight loss: 28. Biologicals, except when administered as an in-patient, when clinically indicated and hospitalization
k) Wellness Service: This program intends to promote, incentivize and to reward the Insured Persons' healthy life
insured financially prepared during their fight against Cancer and provides indemnity coverage for medical expenses D. Coverage under the policy after the expiry of 30 months for any pre-existing disease is subject to the i. Obesity-related cardiomyopathy warranted - Code Excl 29
style through various wellness activities. The Insured Person can avail the following services: (i) Diet and Nutrition
incurred for Cancer and Non-cancer ailments. Program: To strengthen/restore the immune system. (ii) Weight Management Program – To maintain healthy weight same being declared at the time of application and accepted by Insurer. ii. Coronary heart disease 29. All treatment for Priapism and erectile dysfunctions - Code Excl 30
(iii) Specialist Consultation –Available through Star Tele-health app. 2. Specified disease / procedure waiting period - Code Excl 02 iii. Severe Sleep Apnea
Policy Term 30. Inoculation or Vaccination (except for post-bite treatment and for medical treatment for therapeutic reasons) -
l) Rehabilitation and Pain Management: The company will pay the medical expenses for Rehabilitation and Pain A. Expenses related to the treatment of the listed Conditions, surgeries/treatments shall be excluded until iv. Uncontrolled Type2 Diabetes
1 year Code Excl 31
Management up to the sub-limit (or) maximum up to 10% of the basic sum insured whichever is less, per policy year. the expiry of 24 months of continuous coverage after the date of inception of the first policy with us. This 7. Change-of-Gender treatments - Code Excl 07: Expenses related to any treatment, including surgical
Type of Policy (For details please refer website: www.starhealth.in) exclusion shall not be applicable for claims arising due to an accident. management, to change characteristics of the body to those of the opposite sex. 31. Dental treatment or surgery unless necessitated due to accidental injuries and requiring hospitalization.
Individual Note: Company's liability under this benefit shall not exceed 10% of Basic Sum insured B. In case of enhancement of sum insured the exclusion shall apply afresh to the extent of sum insured (Dental implants are not payable) - Code Excl 32
Rehabilitation: The Company will pay the expenses for rehabilitation, if availed at authorized centres as an In- increase. 8. Cosmetic or plastic Surgery - Code Excl 08: Expenses for cosmetic or plastic surgery or any treatment to
Eligibility change appearance unless for reconstruction following an Accident, Burn(s) or Cancer or as part of medically 32. Medical and / or surgical treatment of Sleep apnea, treatment for endocrine disorders - Code Excl 33
patient/Out-patient, and if there is an admissible claim for In-patient hospitalization for an injury, disease or illness C. If any of the specified disease/procedure falls under the waiting period specified for pre-Existing
Persons who have been diagnosed with Cancer, aged between 5 months and 65 years can avail this Insurance. Proposer specified below; necessary treatment to remove a direct and immediate health risk to the insured. For this to be considered a 33. Hospital registration charges, admission charges, telephone charges and such other charges - Code Excl 34
diseases, then the longer of the two waiting periods shall apply. medical necessity, it must be certified by the attending Medical Practitioner.
should be aged 18 years and above. 1. Poly Trauma D. The waiting period for listed conditions shall apply even if contracted after the policy or declared and 34. Cost of spectacles and contact lens, hearing aids, walkers and crutches, wheel chairs, Cochlear implants
Sum Insured Options 2. Head injury accepted without a specific exclusion. 9. Hazardous or Adventure sports - Code Excl 09: Expenses related to any treatment necessitated due to and procedure related hospitalization expenses, CPAP, BIPAP, Continuous Ambulatory Peritoneal Dialysis,
Section I - Rs.5,00,000/-, Rs.7,50,000/- and Rs.10,00,000/- 3. Diseases of the spine participation as a professional in hazardous or adventure sports, including but not limited to, para-jumping, rock
E. If the Insured Person is continuously covered without any break as defined under the applicable norms on infusion pump and such other similar aids - Code Excl 35
4. Stroke climbing, mountaineering, rafting, motor racing, horse racing or scuba diving, hand gliding, sky diving, deep-
Section II - 50% of Section I sum insured.(Sum Insured under Section II cannot vary) portability stipulated by IRDAI, then waiting period for the same would be reduced to the extent of prior
Pain Management: Cover for treatment of pain management subject to the limits sea diving. 35. Any hospitalizations which are not Medically Necessary - Code Excl 36
coverage.
Pre medical Examination 10. Breach of law - Code Excl 10: Expenses for treatment directly arising from or consequent upon any Insured 36. Other Excluded Expenses as detailed in the website www.starhealth.in - Code Excl 37
m) Coverage for Modern Treatment: Expenses are subject to the limits. F. List of specific diseases/procedures
There is no pre medical tests irrespective of age. The previous medical records including details of treatment to be submitted (For details please refer website: www.starhealth.in) 1. Treatment of Cataract and diseases of the anterior and posterior chamber of the Eye, Diseases of Person committing or attempting to commit a breach of law with criminal intent.
along with proposal. 37. Existing disease/s, disclosed by the insured and mentioned in the policy schedule (based on insured's
n) Hospice Care: Payable up to 20% of sum insured at network providers on indemnity basis, payable once in life ENT, Diseases related to Thyroid, Benign diseases of the breast. 11. Excluded Providers - Code Excl 11: Expenses incurred towards treatment in any hospital or by any Medical consent), for specified ICD codes - Code Excl 38
Instalment Facility available time. Available after a waiting period of 12 months from the policy inception. 2. Subcutaneous Benign Lumps, Sebaceous cyst, Dermoid cyst, Mucous cyst lip / cheek, Carpal Practitioner or any other provider specifically excluded by the Insurer and disclosed in its website / notified to
Premium can be paid Quarterly, Half yearly. Premium can also be paid Annually Hospice care in Oncology is a special kind of care that focuses on the quality of life of patients (as well as their Tunnel Syndrome, Trigger Finger, Lipoma, Neurofibroma, Fibroadenoma, Ganglion and similar the policyholders are not admissible. However, in case of life threatening situations or following an accident, 38. Expenses incurred for treatment of diseases/illness/accidental injuries by systems of medicine other than
caregivers) who are experiencing an advanced, life-limiting cancers. pathology expenses up to the stage of stabilization are payable but not the complete claim. allopathy - Code Excl 39
For instalment mode of payment there will be loading as given below;
Hospice care provides compassionate care for cancer patients during their last phases of life so that they can live as 3. All treatments (Conservative, Operative treatment) and all types of intervention for Diseases related
Quarterly - 3% | Half Yearly - 2% 12. Treatment for, Alcoholism, drug or substance abuse or any addictive condition and consequences thereof - 39. Naturopathy - Code Excl 40
fully and comfortably as possible. to Tendon, Ligament, Fascia, Bones and Joint Including Arthroscopy and Arthroplasty / Joint
Note: This loading will be applied on annual premium Replacement [other than caused by accident]. Code Excl 12
o) Copayment: This policy is subject to co-payment of 10% of each and every claim amount for fresh as well as Moratorium Period
Policy Benefits renewal policies for insured persons whose age at the time of entry is 61 years and above 4. All types of treatment for Degenerative disc and Vertebral diseases including Replacement of 13. Treatments received in health hydros, nature cure clinics, spas or similar establishments or private beds After completion of eight continuous years under the policy no look back to be applied. This period of eight years is
Section I Indemnity Cover (Applicable for treatment of Cancer and Non Cancer) bones and joints and Degenerative diseases of the Musculo-skeletal system, Prolapse of registered as a nursing home attached to such establishments or where admission is arranged wholly or partly
Section II Lumpsum Cover for Cancer (Optional Cover Available only if specifically opted on payment of called as moratorium period. The moratorium would be applicable for the sums insured of the first policy and
Intervertebral Disc (other than caused by accident), for domestic reasons - Code Excl 13
a) Room (Single Standard A/C), Boarding, Nursing expenses as provided by the Hospital / Nursing Home. additional premium and shown in the policy schedule) - If during the period stated in the Schedule the insured person subsequently completion of 8 continuous years would be applicable from date of enhancement of sums insured
Note: Hospitalisation expenses which vary based on the room occupied by the insured person will be 5. All treatments (conservative, interventional, laparoscopic and open) related to Hepato-pancreato-
suffers a recurrence, metastasis, and / or a second malignancy unrelated to first cancer, then the Company will pay a lump 14. Dietary supplements and substances that can be purchased without prescription, including but not limited to only on the enhanced limits. After the expiry of Moratorium Period no health insurance claim shall be contestable
considered in proportion to the room category stated in the policy schedule or actuals whichever is less. biliary diseases including Gall bladder and Pancreatic calculi. All types of management for Kidney
sum amount stated in the policy schedule. This benefit is in addition to the sum insured of Indemnity cover under Section I. Vitamins, minerals and organic substances unless prescribed by a medical practitioner as part of except for proven fraud and permanent exclusions specified in the policy contract. The policies would however be
calculi and Genitourinary tract calculi.
Proportionate deductions are not applied in respect of the hospitals which do not follow differential billing hospitalization claim or day care procedure - Code Excl 14 subject to all limits, sub limits, co-payments, deductibles as per the policy contract.
Note: 6. All types of Hernia,
or for those expenses in respect of which differential billing is not adopted based on the room category. 1. A waiting period of 30 months is applicable for this lump-sum benefit cover. 7. Desmoid Tumor, Umbilical Granuloma, Umbilical Sinus, Umbilical Fistula, 15. Refractive Error - Code Excl 15: Expenses related to the treatment for correction of eye sight due to refractive
b) Surgeon, Anesthetist, Medical Practitioner, Consultants, Specialist Fees Claims Procedure
2. Claim under this benefit is admissible only if treatment for recurrence, metastasis and/or a second malignancy unrelated 8. All treatments (conservative, interventional, laparoscopic and open) related to all Diseases of error less than 7. 5 dioptres.
c) Anesthesia, blood, oxygen, operation theatre charges, ICU Charges, medicines and drugs to first cancer commences after 30 months from first inception of Star Cancer Care Platinum Insurance Policy. · Call the 24 hour help-line for assistance - 1800 425 2255 / 1800 102 4477
Cervix, Uterus, Fallopian tubes, Ovaries, Uterine Bleeding, Pelvic Inflammatory Diseases 16. Unproven Treatments - Code Excl 16: Expenses related to any unproven treatment, services and supplies
d) Emergency Road Ambulance charges, for transportation of the insured person by private ambulance service when 3. On an admissible claim for lump-sum, the coverage under Section II ceases and the policy will continue with Section 9. All Diseases of Prostate, Stricture Urethra, all Obstructive Uropathies, · In case of planned hospitalization, inform 24 hours prior to admission in the hospital
for or in connection with any treatment. Unproven treatments are treatments, procedures or supplies that lack
this is needed for medical reasons to go to hospital for treatment, provided however there is an admissible claim I for the sum insured stated in the policy schedule for the remaining policy period. 10. Benign Tumours of Epididymis, Spermatocele, Varicocele, Hydrocele, significant medical documentation to support their effectiveness. · In case of emergency hospitalization information to be given within 24 hours after hospitalization
under the policy 4. On an admissible claim for lump-sum under Section II, the subsequent renewal, will be for Section I only. 11. Fistula, Fissure in Ano, Hemorrhoids, Pilonidal Sinus and Fistula, Rectal Prolapse, Stress Incontinence · Cashless facility wherever possible in network hospital
e) Pre-hospitalization Expenses: Medical expenses incurred up to 30 days immediately before the insured person 17. Sterility and Infertility - Code Excl 17: Expenses related to sterility and infertility. This includes:
Cumulative Bonus (Applicable for Section I only) 12. Varicose veins and Varicose ulcers i. Any type of contraception, sterilization · In non-network hospitals payment must be made up-front and then reimbursement will be effected on
is hospitalized 13. All types of transplant and related surgeries. submission of documents
The insured person will be eligible for Cumulative bonus calculated at 5% of basic sum insured for each claim free year ii. Assisted Reproduction services including artificial insemination and advanced reproductive technologies
f) Post Hospitalization Expenses: Medical expenses incurred up to 60 days immediately after the insured person is subject to a maximum of 50% of the basic sum insured 14. Congenital Internal disease / defect For Section II
such as IVF, ZIFT, GIFT, ICSI
discharged from the hospital. The amount payable shall be up to 2% of the basic sum insured per hospitalization Special Conditions i. Certificate from the Treating Doctor confirming the Cancer diagnosis
3. 30-day waiting period - Code Excl 03 iii. Gestational Surrogacy
g) All day care procedures are covered 1. The Cumulative bonus will be calculated on the expiring Basic Sum Insured ii. Clinical, Radiological, Histological, Pathological, Histopathological and laboratory reports in support
A. Expenses related to the treatment of any illness within 30 days from the first policy commencement date iv. Reversal of sterilization
h) Cataract treatment: The company will pay the expenses incurred for treatment of cataract up to the limits 2. If the insured opts to reduce the Basic Sum Insured at the subsequent renewal, the limit of indemnity by way of such shall be excluded except claims arising due to an accident, provided the same are covered.
mentioned below; Cumulative bonus shall not exceed such reduced basic sum insured 18. Maternity - Code Excl 18 Disclosure to information norms
B. This exclusion shall not, however, apply if the Insured Person has continuous coverage for more than
3. In the event of a claim resulting in; i. Medical treatment expenses traceable to childbirth (including complicated deliveries and caesarean The policy shall become void and all premium paid thereon shall be forfeited to the Company in the event of mis-
Basic Sum Insured (Rs.) Limit of Cataract Surgery (Rs.) twelve months.
a. Partial utilization of Basic Sum Insured, such cumulative bonus so granted will be reduced at the same rate at sections incurred during hospitalization) except ectopic pregnancy; representation, mis description or non-disclosure of any material fact by the policy holder.
C. The within referred waiting period is made applicable to the enhanced sum insured in the event of
30,000/- per eye per person and not exceeding which it has accrued ii. Expenses towards miscarriage (unless due to an accident) and lawful medical termination of pregnancy
5,00,000/- granting higher sum insured subsequently. Cancellation
40,000/- per person per policy period b. Full utilization of Basic Sum Insured and nil utilization of cumulative bonus accrued, such cumulative bonus so during the policy period.
granted will be reduced at the same rate at which it has accrued 4. Investigation & Evaluation - Code Excl 04 i. The policyholder may cancel this policy by giving 15 days' written notice and in such an event, the Company
40,000/- per eye per person and not exceeding 19. Circumcision(unless necessary for treatment of a disease not excluded under this policy or necessitated due to
7,50,000/- and 10,00,000/- c. Full utilization of Basic Sum Insured and partial utilization of cumulative bonus accrued, the cumulative bonus A. Expenses related to any admission primarily for diagnostics and evaluation purposes only are excluded. shall refund premium for the unexpired policy period as detailed below;
60,000/- per person per policy period an accident), Preputioplasty, Frenuloplasty, Preputial Dilatation and Removal of SMEGMA - Code Excl 19
granted on renewal will be the balance cumulative bonus available and will be reduced at the same rate at B. Any diagnostic expenses which are not related or not incidental to the current diagnosis and treatment are
which it has accrued excluded. 20. Congenital External Condition / Defects / Anomalies - Code Excl 20 Cancellation table applicable without instalment option
i) Cost of Health Checkup: Expenses incurred towards Cost of Health check-up up to Rs.2,500/- for every claim free year.
Note: d. Full utilization of Basic Sum Insured and full utilization of cumulative bonus accrued, the cumulative bonus on 5. Rest Cure, rehabilitation (except to the extent covered under Section I (l)) and respite care - Code Excl 05: 21. Convalescence , general debility, run-down condition, Nutritional deficiency states - Code Excl 21
1. This benefit is payable on renewal and when the renewed policy is in force renewal will be “nil” Period on risk Rate of premium to be retained
Expenses related to any admission primarily for enforced bed rest and not for receiving treatment. This also includes: 22. Intentional self injury - Code Excl 22
2. Payment under this benefit does not form part of the sum insured and will not impact the Bonus. Exclusions 1. Custodial care either at home or in a nursing facility for personal care such as help with activities of daily Up to one mth 22.5% of the policy premium
living such as bathing, dressing, moving around either by skilled nurses or assistant or non-skilled persons. 23. Injury/disease directly or indirectly caused by or arising from or attributable to war, invasion, act of foreign
j) The Insured Person is given the facility of obtaining a Medical Second Opinion from a Doctor in the Company's The Company shall not be liable to make any payments under this policy in respect of any expenses what so ever incurred Exceeding one mth up to 3 mths 37.5% of the policy premium
2. Any services for people who are terminally ill to address physical, social, emotional and spiritual needs. enemy, warlike operations (whether war be declared or not) - Code Excl 24
network of Medical Practitioners. All the medical records provided by the Insured Person will be submitted to the by the insured person in connection with or in respect of;
Doctor either online: e_medicalopinion@starhealth.in or through post/courier 6. Obesity/ Weight Control - Code Excl 06: Expenses related to the surgical treatment of obesity that does not 24. Injury or disease directly or indirectly caused by or contributed to by nuclear weapons/material - Code Excl 25 Exceeding 3 mths up to 6 mths 57.5% of the policy premium
1. Pre-Existing Diseases - Code Excl 01
Subject to the following conditions; A. Expenses related to the treatment of a pre-existing Disease (PED) and its direct complications shall be fulfill all the below conditions: 25. Expenses incurred on Enhanced External Counter Pulsation Therapy and related therapies, Chelation therapy, Exceeding 6 mths up to 9 mths 80% of the policy premium
· This should be specifically requested for by the Insured Person excluded until the expiry 30 months of continuous coverage after the date of inception of the first policy with 1. Surgery to be conducted is upon the advice of the Doctor Hyperbaric Oxygen Therapy, Rotational Field Quantum Magnetic Resonance Therapy, VAX-D, Low level laser
· This opinion is given without examining the patient, based only on the medical records submitted. insurer. 2. The surgery/Procedure conducted should be supported by clinical protocols therapy, Photodynamic therapy and such other therapies - Code Excl 26 Exceeding 9 mths Full of the policy premium
1 2 3 4 5
· The second opinion should be only for medical reasons and not for medico-legal purposes. B. In case of enhancement of sum insured the exclusion shall apply afresh to the extent of sum insured 3. The member has to be 18 years of age or older and 26. Unconventional, Untested, Experimental therapies - Code Excl 27
STAR CANCER CARE PLATINUM INSURANCE POLICY · Any liability due to any errors or omission or consequences of any action taken in reliance of the second increase. 4. Body Mass Index (BMI); 27. Chondrocyte Implantation, Procedures using Platelet Rich plasma and Intra articular injection therapy -
Unique Identification No.: SHAHLIP22031V022122 opinion provided by the Medical Practitioner is outside the scope of this policy. C. If the Insured Person is continuously covered without any break as defined under the portability norms of a. greater than or equal to 40 or Code Excl 28
· Utilizing this facility alone will not be considered as a claim. the extant IRDAI (Health Insurance) Regulations, then waiting period for the same would be reduced to b. greater than or equal to 35 in conjunction with any of the following severe co-morbidities following
Star Cancer Care Platinum Insurance Policy offers protection for persons diagnosed with Cancer. The policy keeps the the extent of prior coverage. failure of less invasive methods of weight loss: 28. Biologicals, except when administered as an in-patient, when clinically indicated and hospitalization
k) Wellness Service: This program intends to promote, incentivize and to reward the Insured Persons' healthy life
insured financially prepared during their fight against Cancer and provides indemnity coverage for medical expenses D. Coverage under the policy after the expiry of 30 months for any pre-existing disease is subject to the i. Obesity-related cardiomyopathy warranted - Code Excl 29
style through various wellness activities. The Insured Person can avail the following services: (i) Diet and Nutrition
incurred for Cancer and Non-cancer ailments. Program: To strengthen/restore the immune system. (ii) Weight Management Program – To maintain healthy weight same being declared at the time of application and accepted by Insurer. ii. Coronary heart disease 29. All treatment for Priapism and erectile dysfunctions - Code Excl 30
(iii) Specialist Consultation –Available through Star Tele-health app. 2. Specified disease / procedure waiting period - Code Excl 02 iii. Severe Sleep Apnea
Policy Term 30. Inoculation or Vaccination (except for post-bite treatment and for medical treatment for therapeutic reasons) -
l) Rehabilitation and Pain Management: The company will pay the medical expenses for Rehabilitation and Pain A. Expenses related to the treatment of the listed Conditions, surgeries/treatments shall be excluded until iv. Uncontrolled Type2 Diabetes
1 year Code Excl 31
Management up to the sub-limit (or) maximum up to 10% of the basic sum insured whichever is less, per policy year. the expiry of 24 months of continuous coverage after the date of inception of the first policy with us. This 7. Change-of-Gender treatments - Code Excl 07: Expenses related to any treatment, including surgical
Type of Policy (For details please refer website: www.starhealth.in) exclusion shall not be applicable for claims arising due to an accident. management, to change characteristics of the body to those of the opposite sex. 31. Dental treatment or surgery unless necessitated due to accidental injuries and requiring hospitalization.
Individual Note: Company's liability under this benefit shall not exceed 10% of Basic Sum insured B. In case of enhancement of sum insured the exclusion shall apply afresh to the extent of sum insured (Dental implants are not payable) - Code Excl 32
Rehabilitation: The Company will pay the expenses for rehabilitation, if availed at authorized centres as an In- increase. 8. Cosmetic or plastic Surgery - Code Excl 08: Expenses for cosmetic or plastic surgery or any treatment to
Eligibility change appearance unless for reconstruction following an Accident, Burn(s) or Cancer or as part of medically 32. Medical and / or surgical treatment of Sleep apnea, treatment for endocrine disorders - Code Excl 33
patient/Out-patient, and if there is an admissible claim for In-patient hospitalization for an injury, disease or illness C. If any of the specified disease/procedure falls under the waiting period specified for pre-Existing
Persons who have been diagnosed with Cancer, aged between 5 months and 65 years can avail this Insurance. Proposer specified below; necessary treatment to remove a direct and immediate health risk to the insured. For this to be considered a 33. Hospital registration charges, admission charges, telephone charges and such other charges - Code Excl 34
diseases, then the longer of the two waiting periods shall apply. medical necessity, it must be certified by the attending Medical Practitioner.
should be aged 18 years and above. 1. Poly Trauma D. The waiting period for listed conditions shall apply even if contracted after the policy or declared and 34. Cost of spectacles and contact lens, hearing aids, walkers and crutches, wheel chairs, Cochlear implants
Sum Insured Options 2. Head injury accepted without a specific exclusion. 9. Hazardous or Adventure sports - Code Excl 09: Expenses related to any treatment necessitated due to and procedure related hospitalization expenses, CPAP, BIPAP, Continuous Ambulatory Peritoneal Dialysis,
Section I - Rs.5,00,000/-, Rs.7,50,000/- and Rs.10,00,000/- 3. Diseases of the spine participation as a professional in hazardous or adventure sports, including but not limited to, para-jumping, rock
E. If the Insured Person is continuously covered without any break as defined under the applicable norms on infusion pump and such other similar aids - Code Excl 35
4. Stroke climbing, mountaineering, rafting, motor racing, horse racing or scuba diving, hand gliding, sky diving, deep-
Section II - 50% of Section I sum insured.(Sum Insured under Section II cannot vary) portability stipulated by IRDAI, then waiting period for the same would be reduced to the extent of prior
Pain Management: Cover for treatment of pain management subject to the limits sea diving. 35. Any hospitalizations which are not Medically Necessary - Code Excl 36
coverage.
Pre medical Examination 10. Breach of law - Code Excl 10: Expenses for treatment directly arising from or consequent upon any Insured 36. Other Excluded Expenses as detailed in the website www.starhealth.in - Code Excl 37
m) Coverage for Modern Treatment: Expenses are subject to the limits. F. List of specific diseases/procedures
There is no pre medical tests irrespective of age. The previous medical records including details of treatment to be submitted (For details please refer website: www.starhealth.in) 1. Treatment of Cataract and diseases of the anterior and posterior chamber of the Eye, Diseases of Person committing or attempting to commit a breach of law with criminal intent.
along with proposal. 37. Existing disease/s, disclosed by the insured and mentioned in the policy schedule (based on insured's
n) Hospice Care: Payable up to 20% of sum insured at network providers on indemnity basis, payable once in life ENT, Diseases related to Thyroid, Benign diseases of the breast. 11. Excluded Providers - Code Excl 11: Expenses incurred towards treatment in any hospital or by any Medical consent), for specified ICD codes - Code Excl 38
Instalment Facility available time. Available after a waiting period of 12 months from the policy inception. 2. Subcutaneous Benign Lumps, Sebaceous cyst, Dermoid cyst, Mucous cyst lip / cheek, Carpal Practitioner or any other provider specifically excluded by the Insurer and disclosed in its website / notified to
Premium can be paid Quarterly, Half yearly. Premium can also be paid Annually Hospice care in Oncology is a special kind of care that focuses on the quality of life of patients (as well as their Tunnel Syndrome, Trigger Finger, Lipoma, Neurofibroma, Fibroadenoma, Ganglion and similar the policyholders are not admissible. However, in case of life threatening situations or following an accident, 38. Expenses incurred for treatment of diseases/illness/accidental injuries by systems of medicine other than
caregivers) who are experiencing an advanced, life-limiting cancers. pathology expenses up to the stage of stabilization are payable but not the complete claim. allopathy - Code Excl 39
For instalment mode of payment there will be loading as given below;
Hospice care provides compassionate care for cancer patients during their last phases of life so that they can live as 3. All treatments (Conservative, Operative treatment) and all types of intervention for Diseases related
Quarterly - 3% | Half Yearly - 2% 12. Treatment for, Alcoholism, drug or substance abuse or any addictive condition and consequences thereof - 39. Naturopathy - Code Excl 40
fully and comfortably as possible. to Tendon, Ligament, Fascia, Bones and Joint Including Arthroscopy and Arthroplasty / Joint
Note: This loading will be applied on annual premium Replacement [other than caused by accident]. Code Excl 12
o) Copayment: This policy is subject to co-payment of 10% of each and every claim amount for fresh as well as Moratorium Period
Policy Benefits renewal policies for insured persons whose age at the time of entry is 61 years and above 4. All types of treatment for Degenerative disc and Vertebral diseases including Replacement of 13. Treatments received in health hydros, nature cure clinics, spas or similar establishments or private beds After completion of eight continuous years under the policy no look back to be applied. This period of eight years is
Section I Indemnity Cover (Applicable for treatment of Cancer and Non Cancer) bones and joints and Degenerative diseases of the Musculo-skeletal system, Prolapse of registered as a nursing home attached to such establishments or where admission is arranged wholly or partly
Section II Lumpsum Cover for Cancer (Optional Cover Available only if specifically opted on payment of called as moratorium period. The moratorium would be applicable for the sums insured of the first policy and
Intervertebral Disc (other than caused by accident), for domestic reasons - Code Excl 13
a) Room (Single Standard A/C), Boarding, Nursing expenses as provided by the Hospital / Nursing Home. additional premium and shown in the policy schedule) - If during the period stated in the Schedule the insured person subsequently completion of 8 continuous years would be applicable from date of enhancement of sums insured
Note: Hospitalisation expenses which vary based on the room occupied by the insured person will be 5. All treatments (conservative, interventional, laparoscopic and open) related to Hepato-pancreato-
suffers a recurrence, metastasis, and / or a second malignancy unrelated to first cancer, then the Company will pay a lump 14. Dietary supplements and substances that can be purchased without prescription, including but not limited to only on the enhanced limits. After the expiry of Moratorium Period no health insurance claim shall be contestable
considered in proportion to the room category stated in the policy schedule or actuals whichever is less. biliary diseases including Gall bladder and Pancreatic calculi. All types of management for Kidney
sum amount stated in the policy schedule. This benefit is in addition to the sum insured of Indemnity cover under Section I. Vitamins, minerals and organic substances unless prescribed by a medical practitioner as part of except for proven fraud and permanent exclusions specified in the policy contract. The policies would however be
calculi and Genitourinary tract calculi.
Proportionate deductions are not applied in respect of the hospitals which do not follow differential billing hospitalization claim or day care procedure - Code Excl 14 subject to all limits, sub limits, co-payments, deductibles as per the policy contract.
Note: 6. All types of Hernia,
or for those expenses in respect of which differential billing is not adopted based on the room category. 1. A waiting period of 30 months is applicable for this lump-sum benefit cover. 7. Desmoid Tumor, Umbilical Granuloma, Umbilical Sinus, Umbilical Fistula, 15. Refractive Error - Code Excl 15: Expenses related to the treatment for correction of eye sight due to refractive
b) Surgeon, Anesthetist, Medical Practitioner, Consultants, Specialist Fees Claims Procedure
2. Claim under this benefit is admissible only if treatment for recurrence, metastasis and/or a second malignancy unrelated 8. All treatments (conservative, interventional, laparoscopic and open) related to all Diseases of error less than 7. 5 dioptres.
c) Anesthesia, blood, oxygen, operation theatre charges, ICU Charges, medicines and drugs to first cancer commences after 30 months from first inception of Star Cancer Care Platinum Insurance Policy. · Call the 24 hour help-line for assistance - 1800 425 2255 / 1800 102 4477
Cervix, Uterus, Fallopian tubes, Ovaries, Uterine Bleeding, Pelvic Inflammatory Diseases 16. Unproven Treatments - Code Excl 16: Expenses related to any unproven treatment, services and supplies
d) Emergency Road Ambulance charges, for transportation of the insured person by private ambulance service when 3. On an admissible claim for lump-sum, the coverage under Section II ceases and the policy will continue with Section 9. All Diseases of Prostate, Stricture Urethra, all Obstructive Uropathies, · In case of planned hospitalization, inform 24 hours prior to admission in the hospital
for or in connection with any treatment. Unproven treatments are treatments, procedures or supplies that lack
this is needed for medical reasons to go to hospital for treatment, provided however there is an admissible claim I for the sum insured stated in the policy schedule for the remaining policy period. 10. Benign Tumours of Epididymis, Spermatocele, Varicocele, Hydrocele, significant medical documentation to support their effectiveness. · In case of emergency hospitalization information to be given within 24 hours after hospitalization
under the policy 4. On an admissible claim for lump-sum under Section II, the subsequent renewal, will be for Section I only. 11. Fistula, Fissure in Ano, Hemorrhoids, Pilonidal Sinus and Fistula, Rectal Prolapse, Stress Incontinence · Cashless facility wherever possible in network hospital
e) Pre-hospitalization Expenses: Medical expenses incurred up to 30 days immediately before the insured person 17. Sterility and Infertility - Code Excl 17: Expenses related to sterility and infertility. This includes:
Cumulative Bonus (Applicable for Section I only) 12. Varicose veins and Varicose ulcers i. Any type of contraception, sterilization · In non-network hospitals payment must be made up-front and then reimbursement will be effected on
is hospitalized 13. All types of transplant and related surgeries. submission of documents
The insured person will be eligible for Cumulative bonus calculated at 5% of basic sum insured for each claim free year ii. Assisted Reproduction services including artificial insemination and advanced reproductive technologies
f) Post Hospitalization Expenses: Medical expenses incurred up to 60 days immediately after the insured person is subject to a maximum of 50% of the basic sum insured 14. Congenital Internal disease / defect For Section II
such as IVF, ZIFT, GIFT, ICSI
discharged from the hospital. The amount payable shall be up to 2% of the basic sum insured per hospitalization Special Conditions i. Certificate from the Treating Doctor confirming the Cancer diagnosis
3. 30-day waiting period - Code Excl 03 iii. Gestational Surrogacy
g) All day care procedures are covered 1. The Cumulative bonus will be calculated on the expiring Basic Sum Insured ii. Clinical, Radiological, Histological, Pathological, Histopathological and laboratory reports in support
A. Expenses related to the treatment of any illness within 30 days from the first policy commencement date iv. Reversal of sterilization
h) Cataract treatment: The company will pay the expenses incurred for treatment of cataract up to the limits 2. If the insured opts to reduce the Basic Sum Insured at the subsequent renewal, the limit of indemnity by way of such shall be excluded except claims arising due to an accident, provided the same are covered.
mentioned below; Cumulative bonus shall not exceed such reduced basic sum insured 18. Maternity - Code Excl 18 Disclosure to information norms
B. This exclusion shall not, however, apply if the Insured Person has continuous coverage for more than
3. In the event of a claim resulting in; i. Medical treatment expenses traceable to childbirth (including complicated deliveries and caesarean The policy shall become void and all premium paid thereon shall be forfeited to the Company in the event of mis-
Basic Sum Insured (Rs.) Limit of Cataract Surgery (Rs.) twelve months.
a. Partial utilization of Basic Sum Insured, such cumulative bonus so granted will be reduced at the same rate at sections incurred during hospitalization) except ectopic pregnancy; representation, mis description or non-disclosure of any material fact by the policy holder.
C. The within referred waiting period is made applicable to the enhanced sum insured in the event of
30,000/- per eye per person and not exceeding which it has accrued ii. Expenses towards miscarriage (unless due to an accident) and lawful medical termination of pregnancy
5,00,000/- granting higher sum insured subsequently. Cancellation
40,000/- per person per policy period b. Full utilization of Basic Sum Insured and nil utilization of cumulative bonus accrued, such cumulative bonus so during the policy period.
granted will be reduced at the same rate at which it has accrued 4. Investigation & Evaluation - Code Excl 04 i. The policyholder may cancel this policy by giving 15 days' written notice and in such an event, the Company
40,000/- per eye per person and not exceeding 19. Circumcision(unless necessary for treatment of a disease not excluded under this policy or necessitated due to
7,50,000/- and 10,00,000/- c. Full utilization of Basic Sum Insured and partial utilization of cumulative bonus accrued, the cumulative bonus A. Expenses related to any admission primarily for diagnostics and evaluation purposes only are excluded. shall refund premium for the unexpired policy period as detailed below;
60,000/- per person per policy period an accident), Preputioplasty, Frenuloplasty, Preputial Dilatation and Removal of SMEGMA - Code Excl 19
granted on renewal will be the balance cumulative bonus available and will be reduced at the same rate at B. Any diagnostic expenses which are not related or not incidental to the current diagnosis and treatment are
which it has accrued excluded. 20. Congenital External Condition / Defects / Anomalies - Code Excl 20 Cancellation table applicable without instalment option
i) Cost of Health Checkup: Expenses incurred towards Cost of Health check-up up to Rs.2,500/- for every claim free year.
Note: d. Full utilization of Basic Sum Insured and full utilization of cumulative bonus accrued, the cumulative bonus on 5. Rest Cure, rehabilitation (except to the extent covered under Section I (l)) and respite care - Code Excl 05: 21. Convalescence , general debility, run-down condition, Nutritional deficiency states - Code Excl 21
1. This benefit is payable on renewal and when the renewed policy is in force renewal will be “nil” Period on risk Rate of premium to be retained
Expenses related to any admission primarily for enforced bed rest and not for receiving treatment. This also includes: 22. Intentional self injury - Code Excl 22
2. Payment under this benefit does not form part of the sum insured and will not impact the Bonus. Exclusions 1. Custodial care either at home or in a nursing facility for personal care such as help with activities of daily Up to one mth 22.5% of the policy premium
living such as bathing, dressing, moving around either by skilled nurses or assistant or non-skilled persons. 23. Injury/disease directly or indirectly caused by or arising from or attributable to war, invasion, act of foreign
j) The Insured Person is given the facility of obtaining a Medical Second Opinion from a Doctor in the Company's The Company shall not be liable to make any payments under this policy in respect of any expenses what so ever incurred Exceeding one mth up to 3 mths 37.5% of the policy premium
2. Any services for people who are terminally ill to address physical, social, emotional and spiritual needs. enemy, warlike operations (whether war be declared or not) - Code Excl 24
network of Medical Practitioners. All the medical records provided by the Insured Person will be submitted to the by the insured person in connection with or in respect of;
Doctor either online: e_medicalopinion@starhealth.in or through post/courier 6. Obesity/ Weight Control - Code Excl 06: Expenses related to the surgical treatment of obesity that does not 24. Injury or disease directly or indirectly caused by or contributed to by nuclear weapons/material - Code Excl 25 Exceeding 3 mths up to 6 mths 57.5% of the policy premium
1. Pre-Existing Diseases - Code Excl 01
Subject to the following conditions; A. Expenses related to the treatment of a pre-existing Disease (PED) and its direct complications shall be fulfill all the below conditions: 25. Expenses incurred on Enhanced External Counter Pulsation Therapy and related therapies, Chelation therapy, Exceeding 6 mths up to 9 mths 80% of the policy premium
· This should be specifically requested for by the Insured Person excluded until the expiry 30 months of continuous coverage after the date of inception of the first policy with 1. Surgery to be conducted is upon the advice of the Doctor Hyperbaric Oxygen Therapy, Rotational Field Quantum Magnetic Resonance Therapy, VAX-D, Low level laser
· This opinion is given without examining the patient, based only on the medical records submitted. insurer. 2. The surgery/Procedure conducted should be supported by clinical protocols therapy, Photodynamic therapy and such other therapies - Code Excl 26 Exceeding 9 mths Full of the policy premium
1 2 3 4 5
· The second opinion should be only for medical reasons and not for medico-legal purposes. B. In case of enhancement of sum insured the exclusion shall apply afresh to the extent of sum insured 3. The member has to be 18 years of age or older and 26. Unconventional, Untested, Experimental therapies - Code Excl 27
STAR CANCER CARE PLATINUM INSURANCE POLICY · Any liability due to any errors or omission or consequences of any action taken in reliance of the second increase. 4. Body Mass Index (BMI); 27. Chondrocyte Implantation, Procedures using Platelet Rich plasma and Intra articular injection therapy -
Unique Identification No.: SHAHLIP22031V022122 opinion provided by the Medical Practitioner is outside the scope of this policy. C. If the Insured Person is continuously covered without any break as defined under the portability norms of a. greater than or equal to 40 or Code Excl 28
· Utilizing this facility alone will not be considered as a claim. the extant IRDAI (Health Insurance) Regulations, then waiting period for the same would be reduced to b. greater than or equal to 35 in conjunction with any of the following severe co-morbidities following
Star Cancer Care Platinum Insurance Policy offers protection for persons diagnosed with Cancer. The policy keeps the the extent of prior coverage. failure of less invasive methods of weight loss: 28. Biologicals, except when administered as an in-patient, when clinically indicated and hospitalization
k) Wellness Service: This program intends to promote, incentivize and to reward the Insured Persons' healthy life
insured financially prepared during their fight against Cancer and provides indemnity coverage for medical expenses D. Coverage under the policy after the expiry of 30 months for any pre-existing disease is subject to the i. Obesity-related cardiomyopathy warranted - Code Excl 29
style through various wellness activities. The Insured Person can avail the following services: (i) Diet and Nutrition
incurred for Cancer and Non-cancer ailments. Program: To strengthen/restore the immune system. (ii) Weight Management Program – To maintain healthy weight same being declared at the time of application and accepted by Insurer. ii. Coronary heart disease 29. All treatment for Priapism and erectile dysfunctions - Code Excl 30
(iii) Specialist Consultation –Available through Star Tele-health app. 2. Specified disease / procedure waiting period - Code Excl 02 iii. Severe Sleep Apnea
Policy Term 30. Inoculation or Vaccination (except for post-bite treatment and for medical treatment for therapeutic reasons) -
l) Rehabilitation and Pain Management: The company will pay the medical expenses for Rehabilitation and Pain A. Expenses related to the treatment of the listed Conditions, surgeries/treatments shall be excluded until iv. Uncontrolled Type2 Diabetes
1 year Code Excl 31
Management up to the sub-limit (or) maximum up to 10% of the basic sum insured whichever is less, per policy year. the expiry of 24 months of continuous coverage after the date of inception of the first policy with us. This 7. Change-of-Gender treatments - Code Excl 07: Expenses related to any treatment, including surgical
Type of Policy (For details please refer website: www.starhealth.in) exclusion shall not be applicable for claims arising due to an accident. management, to change characteristics of the body to those of the opposite sex. 31. Dental treatment or surgery unless necessitated due to accidental injuries and requiring hospitalization.
Individual Note: Company's liability under this benefit shall not exceed 10% of Basic Sum insured B. In case of enhancement of sum insured the exclusion shall apply afresh to the extent of sum insured (Dental implants are not payable) - Code Excl 32
Rehabilitation: The Company will pay the expenses for rehabilitation, if availed at authorized centres as an In- increase. 8. Cosmetic or plastic Surgery - Code Excl 08: Expenses for cosmetic or plastic surgery or any treatment to
Eligibility change appearance unless for reconstruction following an Accident, Burn(s) or Cancer or as part of medically 32. Medical and / or surgical treatment of Sleep apnea, treatment for endocrine disorders - Code Excl 33
patient/Out-patient, and if there is an admissible claim for In-patient hospitalization for an injury, disease or illness C. If any of the specified disease/procedure falls under the waiting period specified for pre-Existing
Persons who have been diagnosed with Cancer, aged between 5 months and 65 years can avail this Insurance. Proposer specified below; necessary treatment to remove a direct and immediate health risk to the insured. For this to be considered a 33. Hospital registration charges, admission charges, telephone charges and such other charges - Code Excl 34
diseases, then the longer of the two waiting periods shall apply. medical necessity, it must be certified by the attending Medical Practitioner.
should be aged 18 years and above. 1. Poly Trauma D. The waiting period for listed conditions shall apply even if contracted after the policy or declared and 34. Cost of spectacles and contact lens, hearing aids, walkers and crutches, wheel chairs, Cochlear implants
Sum Insured Options 2. Head injury accepted without a specific exclusion. 9. Hazardous or Adventure sports - Code Excl 09: Expenses related to any treatment necessitated due to and procedure related hospitalization expenses, CPAP, BIPAP, Continuous Ambulatory Peritoneal Dialysis,
Section I - Rs.5,00,000/-, Rs.7,50,000/- and Rs.10,00,000/- 3. Diseases of the spine participation as a professional in hazardous or adventure sports, including but not limited to, para-jumping, rock
E. If the Insured Person is continuously covered without any break as defined under the applicable norms on infusion pump and such other similar aids - Code Excl 35
4. Stroke climbing, mountaineering, rafting, motor racing, horse racing or scuba diving, hand gliding, sky diving, deep-
Section II - 50% of Section I sum insured.(Sum Insured under Section II cannot vary) portability stipulated by IRDAI, then waiting period for the same would be reduced to the extent of prior
Pain Management: Cover for treatment of pain management subject to the limits sea diving. 35. Any hospitalizations which are not Medically Necessary - Code Excl 36
coverage.
Pre medical Examination 10. Breach of law - Code Excl 10: Expenses for treatment directly arising from or consequent upon any Insured 36. Other Excluded Expenses as detailed in the website www.starhealth.in - Code Excl 37
m) Coverage for Modern Treatment: Expenses are subject to the limits. F. List of specific diseases/procedures
There is no pre medical tests irrespective of age. The previous medical records including details of treatment to be submitted (For details please refer website: www.starhealth.in) 1. Treatment of Cataract and diseases of the anterior and posterior chamber of the Eye, Diseases of Person committing or attempting to commit a breach of law with criminal intent.
along with proposal. 37. Existing disease/s, disclosed by the insured and mentioned in the policy schedule (based on insured's
n) Hospice Care: Payable up to 20% of sum insured at network providers on indemnity basis, payable once in life ENT, Diseases related to Thyroid, Benign diseases of the breast. 11. Excluded Providers - Code Excl 11: Expenses incurred towards treatment in any hospital or by any Medical consent), for specified ICD codes - Code Excl 38
Instalment Facility available time. Available after a waiting period of 12 months from the policy inception. 2. Subcutaneous Benign Lumps, Sebaceous cyst, Dermoid cyst, Mucous cyst lip / cheek, Carpal Practitioner or any other provider specifically excluded by the Insurer and disclosed in its website / notified to
Premium can be paid Quarterly, Half yearly. Premium can also be paid Annually Hospice care in Oncology is a special kind of care that focuses on the quality of life of patients (as well as their Tunnel Syndrome, Trigger Finger, Lipoma, Neurofibroma, Fibroadenoma, Ganglion and similar the policyholders are not admissible. However, in case of life threatening situations or following an accident, 38. Expenses incurred for treatment of diseases/illness/accidental injuries by systems of medicine other than
caregivers) who are experiencing an advanced, life-limiting cancers. pathology expenses up to the stage of stabilization are payable but not the complete claim. allopathy - Code Excl 39
For instalment mode of payment there will be loading as given below;
Hospice care provides compassionate care for cancer patients during their last phases of life so that they can live as 3. All treatments (Conservative, Operative treatment) and all types of intervention for Diseases related
Quarterly - 3% | Half Yearly - 2% 12. Treatment for, Alcoholism, drug or substance abuse or any addictive condition and consequences thereof - 39. Naturopathy - Code Excl 40
fully and comfortably as possible. to Tendon, Ligament, Fascia, Bones and Joint Including Arthroscopy and Arthroplasty / Joint
Note: This loading will be applied on annual premium Replacement [other than caused by accident]. Code Excl 12
o) Copayment: This policy is subject to co-payment of 10% of each and every claim amount for fresh as well as Moratorium Period
Policy Benefits renewal policies for insured persons whose age at the time of entry is 61 years and above 4. All types of treatment for Degenerative disc and Vertebral diseases including Replacement of 13. Treatments received in health hydros, nature cure clinics, spas or similar establishments or private beds After completion of eight continuous years under the policy no look back to be applied. This period of eight years is
Section I Indemnity Cover (Applicable for treatment of Cancer and Non Cancer) bones and joints and Degenerative diseases of the Musculo-skeletal system, Prolapse of registered as a nursing home attached to such establishments or where admission is arranged wholly or partly
Section II Lumpsum Cover for Cancer (Optional Cover Available only if specifically opted on payment of called as moratorium period. The moratorium would be applicable for the sums insured of the first policy and
Intervertebral Disc (other than caused by accident), for domestic reasons - Code Excl 13
a) Room (Single Standard A/C), Boarding, Nursing expenses as provided by the Hospital / Nursing Home. additional premium and shown in the policy schedule) - If during the period stated in the Schedule the insured person subsequently completion of 8 continuous years would be applicable from date of enhancement of sums insured
Note: Hospitalisation expenses which vary based on the room occupied by the insured person will be 5. All treatments (conservative, interventional, laparoscopic and open) related to Hepato-pancreato-
suffers a recurrence, metastasis, and / or a second malignancy unrelated to first cancer, then the Company will pay a lump 14. Dietary supplements and substances that can be purchased without prescription, including but not limited to only on the enhanced limits. After the expiry of Moratorium Period no health insurance claim shall be contestable
considered in proportion to the room category stated in the policy schedule or actuals whichever is less. biliary diseases including Gall bladder and Pancreatic calculi. All types of management for Kidney
sum amount stated in the policy schedule. This benefit is in addition to the sum insured of Indemnity cover under Section I. Vitamins, minerals and organic substances unless prescribed by a medical practitioner as part of except for proven fraud and permanent exclusions specified in the policy contract. The policies would however be
calculi and Genitourinary tract calculi.
Proportionate deductions are not applied in respect of the hospitals which do not follow differential billing hospitalization claim or day care procedure - Code Excl 14 subject to all limits, sub limits, co-payments, deductibles as per the policy contract.
Note: 6. All types of Hernia,
or for those expenses in respect of which differential billing is not adopted based on the room category. 1. A waiting period of 30 months is applicable for this lump-sum benefit cover. 7. Desmoid Tumor, Umbilical Granuloma, Umbilical Sinus, Umbilical Fistula, 15. Refractive Error - Code Excl 15: Expenses related to the treatment for correction of eye sight due to refractive
b) Surgeon, Anesthetist, Medical Practitioner, Consultants, Specialist Fees Claims Procedure
2. Claim under this benefit is admissible only if treatment for recurrence, metastasis and/or a second malignancy unrelated 8. All treatments (conservative, interventional, laparoscopic and open) related to all Diseases of error less than 7. 5 dioptres.
c) Anesthesia, blood, oxygen, operation theatre charges, ICU Charges, medicines and drugs to first cancer commences after 30 months from first inception of Star Cancer Care Platinum Insurance Policy. · Call the 24 hour help-line for assistance - 1800 425 2255 / 1800 102 4477
Cervix, Uterus, Fallopian tubes, Ovaries, Uterine Bleeding, Pelvic Inflammatory Diseases 16. Unproven Treatments - Code Excl 16: Expenses related to any unproven treatment, services and supplies
d) Emergency Road Ambulance charges, for transportation of the insured person by private ambulance service when 3. On an admissible claim for lump-sum, the coverage under Section II ceases and the policy will continue with Section 9. All Diseases of Prostate, Stricture Urethra, all Obstructive Uropathies, · In case of planned hospitalization, inform 24 hours prior to admission in the hospital
for or in connection with any treatment. Unproven treatments are treatments, procedures or supplies that lack
this is needed for medical reasons to go to hospital for treatment, provided however there is an admissible claim I for the sum insured stated in the policy schedule for the remaining policy period. 10. Benign Tumours of Epididymis, Spermatocele, Varicocele, Hydrocele, significant medical documentation to support their effectiveness. · In case of emergency hospitalization information to be given within 24 hours after hospitalization
under the policy 4. On an admissible claim for lump-sum under Section II, the subsequent renewal, will be for Section I only. 11. Fistula, Fissure in Ano, Hemorrhoids, Pilonidal Sinus and Fistula, Rectal Prolapse, Stress Incontinence · Cashless facility wherever possible in network hospital
e) Pre-hospitalization Expenses: Medical expenses incurred up to 30 days immediately before the insured person 17. Sterility and Infertility - Code Excl 17: Expenses related to sterility and infertility. This includes:
Cumulative Bonus (Applicable for Section I only) 12. Varicose veins and Varicose ulcers i. Any type of contraception, sterilization · In non-network hospitals payment must be made up-front and then reimbursement will be effected on
is hospitalized 13. All types of transplant and related surgeries. submission of documents
The insured person will be eligible for Cumulative bonus calculated at 5% of basic sum insured for each claim free year ii. Assisted Reproduction services including artificial insemination and advanced reproductive technologies
f) Post Hospitalization Expenses: Medical expenses incurred up to 60 days immediately after the insured person is subject to a maximum of 50% of the basic sum insured 14. Congenital Internal disease / defect For Section II
such as IVF, ZIFT, GIFT, ICSI
discharged from the hospital. The amount payable shall be up to 2% of the basic sum insured per hospitalization Special Conditions i. Certificate from the Treating Doctor confirming the Cancer diagnosis
3. 30-day waiting period - Code Excl 03 iii. Gestational Surrogacy
g) All day care procedures are covered 1. The Cumulative bonus will be calculated on the expiring Basic Sum Insured ii. Clinical, Radiological, Histological, Pathological, Histopathological and laboratory reports in support
A. Expenses related to the treatment of any illness within 30 days from the first policy commencement date iv. Reversal of sterilization
h) Cataract treatment: The company will pay the expenses incurred for treatment of cataract up to the limits 2. If the insured opts to reduce the Basic Sum Insured at the subsequent renewal, the limit of indemnity by way of such shall be excluded except claims arising due to an accident, provided the same are covered.
mentioned below; Cumulative bonus shall not exceed such reduced basic sum insured 18. Maternity - Code Excl 18 Disclosure to information norms
B. This exclusion shall not, however, apply if the Insured Person has continuous coverage for more than
3. In the event of a claim resulting in; i. Medical treatment expenses traceable to childbirth (including complicated deliveries and caesarean The policy shall become void and all premium paid thereon shall be forfeited to the Company in the event of mis-
Basic Sum Insured (Rs.) Limit of Cataract Surgery (Rs.) twelve months.
a. Partial utilization of Basic Sum Insured, such cumulative bonus so granted will be reduced at the same rate at sections incurred during hospitalization) except ectopic pregnancy; representation, mis description or non-disclosure of any material fact by the policy holder.
C. The within referred waiting period is made applicable to the enhanced sum insured in the event of
30,000/- per eye per person and not exceeding which it has accrued ii. Expenses towards miscarriage (unless due to an accident) and lawful medical termination of pregnancy
5,00,000/- granting higher sum insured subsequently. Cancellation
40,000/- per person per policy period b. Full utilization of Basic Sum Insured and nil utilization of cumulative bonus accrued, such cumulative bonus so during the policy period.
granted will be reduced at the same rate at which it has accrued 4. Investigation & Evaluation - Code Excl 04 i. The policyholder may cancel this policy by giving 15 days' written notice and in such an event, the Company
40,000/- per eye per person and not exceeding 19. Circumcision(unless necessary for treatment of a disease not excluded under this policy or necessitated due to
7,50,000/- and 10,00,000/- c. Full utilization of Basic Sum Insured and partial utilization of cumulative bonus accrued, the cumulative bonus A. Expenses related to any admission primarily for diagnostics and evaluation purposes only are excluded. shall refund premium for the unexpired policy period as detailed below;
60,000/- per person per policy period an accident), Preputioplasty, Frenuloplasty, Preputial Dilatation and Removal of SMEGMA - Code Excl 19
granted on renewal will be the balance cumulative bonus available and will be reduced at the same rate at B. Any diagnostic expenses which are not related or not incidental to the current diagnosis and treatment are
which it has accrued excluded. 20. Congenital External Condition / Defects / Anomalies - Code Excl 20 Cancellation table applicable without instalment option
i) Cost of Health Checkup: Expenses incurred towards Cost of Health check-up up to Rs.2,500/- for every claim free year.
Note: d. Full utilization of Basic Sum Insured and full utilization of cumulative bonus accrued, the cumulative bonus on 5. Rest Cure, rehabilitation (except to the extent covered under Section I (l)) and respite care - Code Excl 05: 21. Convalescence , general debility, run-down condition, Nutritional deficiency states - Code Excl 21
1. This benefit is payable on renewal and when the renewed policy is in force renewal will be “nil” Period on risk Rate of premium to be retained
Expenses related to any admission primarily for enforced bed rest and not for receiving treatment. This also includes: 22. Intentional self injury - Code Excl 22
2. Payment under this benefit does not form part of the sum insured and will not impact the Bonus. Exclusions 1. Custodial care either at home or in a nursing facility for personal care such as help with activities of daily Up to one mth 22.5% of the policy premium
living such as bathing, dressing, moving around either by skilled nurses or assistant or non-skilled persons. 23. Injury/disease directly or indirectly caused by or arising from or attributable to war, invasion, act of foreign
j) The Insured Person is given the facility of obtaining a Medical Second Opinion from a Doctor in the Company's The Company shall not be liable to make any payments under this policy in respect of any expenses what so ever incurred Exceeding one mth up to 3 mths 37.5% of the policy premium
2. Any services for people who are terminally ill to address physical, social, emotional and spiritual needs. enemy, warlike operations (whether war be declared or not) - Code Excl 24
network of Medical Practitioners. All the medical records provided by the Insured Person will be submitted to the by the insured person in connection with or in respect of;
Doctor either online: e_medicalopinion@starhealth.in or through post/courier 6. Obesity/ Weight Control - Code Excl 06: Expenses related to the surgical treatment of obesity that does not 24. Injury or disease directly or indirectly caused by or contributed to by nuclear weapons/material - Code Excl 25 Exceeding 3 mths up to 6 mths 57.5% of the policy premium
1. Pre-Existing Diseases - Code Excl 01
Subject to the following conditions; A. Expenses related to the treatment of a pre-existing Disease (PED) and its direct complications shall be fulfill all the below conditions: 25. Expenses incurred on Enhanced External Counter Pulsation Therapy and related therapies, Chelation therapy, Exceeding 6 mths up to 9 mths 80% of the policy premium
· This should be specifically requested for by the Insured Person excluded until the expiry 30 months of continuous coverage after the date of inception of the first policy with 1. Surgery to be conducted is upon the advice of the Doctor Hyperbaric Oxygen Therapy, Rotational Field Quantum Magnetic Resonance Therapy, VAX-D, Low level laser
· This opinion is given without examining the patient, based only on the medical records submitted. insurer. 2. The surgery/Procedure conducted should be supported by clinical protocols therapy, Photodynamic therapy and such other therapies - Code Excl 26 Exceeding 9 mths Full of the policy premium
1 2 3 4 5
· The second opinion should be only for medical reasons and not for medico-legal purposes. B. In case of enhancement of sum insured the exclusion shall apply afresh to the extent of sum insured 3. The member has to be 18 years of age or older and 26. Unconventional, Untested, Experimental therapies - Code Excl 27
STAR CANCER CARE PLATINUM INSURANCE POLICY · Any liability due to any errors or omission or consequences of any action taken in reliance of the second increase. 4. Body Mass Index (BMI); 27. Chondrocyte Implantation, Procedures using Platelet Rich plasma and Intra articular injection therapy -
Unique Identification No.: SHAHLIP22031V022122 opinion provided by the Medical Practitioner is outside the scope of this policy. C. If the Insured Person is continuously covered without any break as defined under the portability norms of a. greater than or equal to 40 or Code Excl 28
· Utilizing this facility alone will not be considered as a claim. the extant IRDAI (Health Insurance) Regulations, then waiting period for the same would be reduced to b. greater than or equal to 35 in conjunction with any of the following severe co-morbidities following
Star Cancer Care Platinum Insurance Policy offers protection for persons diagnosed with Cancer. The policy keeps the the extent of prior coverage. failure of less invasive methods of weight loss: 28. Biologicals, except when administered as an in-patient, when clinically indicated and hospitalization
k) Wellness Service: This program intends to promote, incentivize and to reward the Insured Persons' healthy life
insured financially prepared during their fight against Cancer and provides indemnity coverage for medical expenses D. Coverage under the policy after the expiry of 30 months for any pre-existing disease is subject to the i. Obesity-related cardiomyopathy warranted - Code Excl 29
style through various wellness activities. The Insured Person can avail the following services: (i) Diet and Nutrition
incurred for Cancer and Non-cancer ailments. Program: To strengthen/restore the immune system. (ii) Weight Management Program – To maintain healthy weight same being declared at the time of application and accepted by Insurer. ii. Coronary heart disease 29. All treatment for Priapism and erectile dysfunctions - Code Excl 30
(iii) Specialist Consultation –Available through Star Tele-health app. 2. Specified disease / procedure waiting period - Code Excl 02 iii. Severe Sleep Apnea
Policy Term 30. Inoculation or Vaccination (except for post-bite treatment and for medical treatment for therapeutic reasons) -
l) Rehabilitation and Pain Management: The company will pay the medical expenses for Rehabilitation and Pain A. Expenses related to the treatment of the listed Conditions, surgeries/treatments shall be excluded until iv. Uncontrolled Type2 Diabetes
1 year Code Excl 31
Management up to the sub-limit (or) maximum up to 10% of the basic sum insured whichever is less, per policy year. the expiry of 24 months of continuous coverage after the date of inception of the first policy with us. This 7. Change-of-Gender treatments - Code Excl 07: Expenses related to any treatment, including surgical
Type of Policy (For details please refer website: www.starhealth.in) exclusion shall not be applicable for claims arising due to an accident. management, to change characteristics of the body to those of the opposite sex. 31. Dental treatment or surgery unless necessitated due to accidental injuries and requiring hospitalization.
Individual Note: Company's liability under this benefit shall not exceed 10% of Basic Sum insured B. In case of enhancement of sum insured the exclusion shall apply afresh to the extent of sum insured (Dental implants are not payable) - Code Excl 32
Rehabilitation: The Company will pay the expenses for rehabilitation, if availed at authorized centres as an In- increase. 8. Cosmetic or plastic Surgery - Code Excl 08: Expenses for cosmetic or plastic surgery or any treatment to
Eligibility change appearance unless for reconstruction following an Accident, Burn(s) or Cancer or as part of medically 32. Medical and / or surgical treatment of Sleep apnea, treatment for endocrine disorders - Code Excl 33
patient/Out-patient, and if there is an admissible claim for In-patient hospitalization for an injury, disease or illness C. If any of the specified disease/procedure falls under the waiting period specified for pre-Existing
Persons who have been diagnosed with Cancer, aged between 5 months and 65 years can avail this Insurance. Proposer specified below; necessary treatment to remove a direct and immediate health risk to the insured. For this to be considered a 33. Hospital registration charges, admission charges, telephone charges and such other charges - Code Excl 34
diseases, then the longer of the two waiting periods shall apply. medical necessity, it must be certified by the attending Medical Practitioner.
should be aged 18 years and above. 1. Poly Trauma D. The waiting period for listed conditions shall apply even if contracted after the policy or declared and 34. Cost of spectacles and contact lens, hearing aids, walkers and crutches, wheel chairs, Cochlear implants
Sum Insured Options 2. Head injury accepted without a specific exclusion. 9. Hazardous or Adventure sports - Code Excl 09: Expenses related to any treatment necessitated due to and procedure related hospitalization expenses, CPAP, BIPAP, Continuous Ambulatory Peritoneal Dialysis,
Section I - Rs.5,00,000/-, Rs.7,50,000/- and Rs.10,00,000/- 3. Diseases of the spine participation as a professional in hazardous or adventure sports, including but not limited to, para-jumping, rock
E. If the Insured Person is continuously covered without any break as defined under the applicable norms on infusion pump and such other similar aids - Code Excl 35
4. Stroke climbing, mountaineering, rafting, motor racing, horse racing or scuba diving, hand gliding, sky diving, deep-
Section II - 50% of Section I sum insured.(Sum Insured under Section II cannot vary) portability stipulated by IRDAI, then waiting period for the same would be reduced to the extent of prior
Pain Management: Cover for treatment of pain management subject to the limits sea diving. 35. Any hospitalizations which are not Medically Necessary - Code Excl 36
coverage.
Pre medical Examination 10. Breach of law - Code Excl 10: Expenses for treatment directly arising from or consequent upon any Insured 36. Other Excluded Expenses as detailed in the website www.starhealth.in - Code Excl 37
m) Coverage for Modern Treatment: Expenses are subject to the limits. F. List of specific diseases/procedures
There is no pre medical tests irrespective of age. The previous medical records including details of treatment to be submitted (For details please refer website: www.starhealth.in) 1. Treatment of Cataract and diseases of the anterior and posterior chamber of the Eye, Diseases of Person committing or attempting to commit a breach of law with criminal intent.
along with proposal. 37. Existing disease/s, disclosed by the insured and mentioned in the policy schedule (based on insured's
n) Hospice Care: Payable up to 20% of sum insured at network providers on indemnity basis, payable once in life ENT, Diseases related to Thyroid, Benign diseases of the breast. 11. Excluded Providers - Code Excl 11: Expenses incurred towards treatment in any hospital or by any Medical consent), for specified ICD codes - Code Excl 38
Instalment Facility available time. Available after a waiting period of 12 months from the policy inception. 2. Subcutaneous Benign Lumps, Sebaceous cyst, Dermoid cyst, Mucous cyst lip / cheek, Carpal Practitioner or any other provider specifically excluded by the Insurer and disclosed in its website / notified to
Premium can be paid Quarterly, Half yearly. Premium can also be paid Annually Hospice care in Oncology is a special kind of care that focuses on the quality of life of patients (as well as their Tunnel Syndrome, Trigger Finger, Lipoma, Neurofibroma, Fibroadenoma, Ganglion and similar the policyholders are not admissible. However, in case of life threatening situations or following an accident, 38. Expenses incurred for treatment of diseases/illness/accidental injuries by systems of medicine other than
caregivers) who are experiencing an advanced, life-limiting cancers. pathology expenses up to the stage of stabilization are payable but not the complete claim. allopathy - Code Excl 39
For instalment mode of payment there will be loading as given below;
Hospice care provides compassionate care for cancer patients during their last phases of life so that they can live as 3. All treatments (Conservative, Operative treatment) and all types of intervention for Diseases related
Quarterly - 3% | Half Yearly - 2% 12. Treatment for, Alcoholism, drug or substance abuse or any addictive condition and consequences thereof - 39. Naturopathy - Code Excl 40
fully and comfortably as possible. to Tendon, Ligament, Fascia, Bones and Joint Including Arthroscopy and Arthroplasty / Joint
Note: This loading will be applied on annual premium Replacement [other than caused by accident]. Code Excl 12
o) Copayment: This policy is subject to co-payment of 10% of each and every claim amount for fresh as well as Moratorium Period
Policy Benefits renewal policies for insured persons whose age at the time of entry is 61 years and above 4. All types of treatment for Degenerative disc and Vertebral diseases including Replacement of 13. Treatments received in health hydros, nature cure clinics, spas or similar establishments or private beds After completion of eight continuous years under the policy no look back to be applied. This period of eight years is
Section I Indemnity Cover (Applicable for treatment of Cancer and Non Cancer) bones and joints and Degenerative diseases of the Musculo-skeletal system, Prolapse of registered as a nursing home attached to such establishments or where admission is arranged wholly or partly
Section II Lumpsum Cover for Cancer (Optional Cover Available only if specifically opted on payment of called as moratorium period. The moratorium would be applicable for the sums insured of the first policy and
Intervertebral Disc (other than caused by accident), for domestic reasons - Code Excl 13
a) Room (Single Standard A/C), Boarding, Nursing expenses as provided by the Hospital / Nursing Home. additional premium and shown in the policy schedule) - If during the period stated in the Schedule the insured person subsequently completion of 8 continuous years would be applicable from date of enhancement of sums insured
Note: Hospitalisation expenses which vary based on the room occupied by the insured person will be 5. All treatments (conservative, interventional, laparoscopic and open) related to Hepato-pancreato-
suffers a recurrence, metastasis, and / or a second malignancy unrelated to first cancer, then the Company will pay a lump 14. Dietary supplements and substances that can be purchased without prescription, including but not limited to only on the enhanced limits. After the expiry of Moratorium Period no health insurance claim shall be contestable
considered in proportion to the room category stated in the policy schedule or actuals whichever is less. biliary diseases including Gall bladder and Pancreatic calculi. All types of management for Kidney
sum amount stated in the policy schedule. This benefit is in addition to the sum insured of Indemnity cover under Section I. Vitamins, minerals and organic substances unless prescribed by a medical practitioner as part of except for proven fraud and permanent exclusions specified in the policy contract. The policies would however be
calculi and Genitourinary tract calculi.
Proportionate deductions are not applied in respect of the hospitals which do not follow differential billing hospitalization claim or day care procedure - Code Excl 14 subject to all limits, sub limits, co-payments, deductibles as per the policy contract.
Note: 6. All types of Hernia,
or for those expenses in respect of which differential billing is not adopted based on the room category. 1. A waiting period of 30 months is applicable for this lump-sum benefit cover. 7. Desmoid Tumor, Umbilical Granuloma, Umbilical Sinus, Umbilical Fistula, 15. Refractive Error - Code Excl 15: Expenses related to the treatment for correction of eye sight due to refractive
b) Surgeon, Anesthetist, Medical Practitioner, Consultants, Specialist Fees Claims Procedure
2. Claim under this benefit is admissible only if treatment for recurrence, metastasis and/or a second malignancy unrelated 8. All treatments (conservative, interventional, laparoscopic and open) related to all Diseases of error less than 7. 5 dioptres.
c) Anesthesia, blood, oxygen, operation theatre charges, ICU Charges, medicines and drugs to first cancer commences after 30 months from first inception of Star Cancer Care Platinum Insurance Policy. · Call the 24 hour help-line for assistance - 1800 425 2255 / 1800 102 4477
Cervix, Uterus, Fallopian tubes, Ovaries, Uterine Bleeding, Pelvic Inflammatory Diseases 16. Unproven Treatments - Code Excl 16: Expenses related to any unproven treatment, services and supplies
d) Emergency Road Ambulance charges, for transportation of the insured person by private ambulance service when 3. On an admissible claim for lump-sum, the coverage under Section II ceases and the policy will continue with Section 9. All Diseases of Prostate, Stricture Urethra, all Obstructive Uropathies, · In case of planned hospitalization, inform 24 hours prior to admission in the hospital
for or in connection with any treatment. Unproven treatments are treatments, procedures or supplies that lack
this is needed for medical reasons to go to hospital for treatment, provided however there is an admissible claim I for the sum insured stated in the policy schedule for the remaining policy period. 10. Benign Tumours of Epididymis, Spermatocele, Varicocele, Hydrocele, significant medical documentation to support their effectiveness. · In case of emergency hospitalization information to be given within 24 hours after hospitalization
under the policy 4. On an admissible claim for lump-sum under Section II, the subsequent renewal, will be for Section I only. 11. Fistula, Fissure in Ano, Hemorrhoids, Pilonidal Sinus and Fistula, Rectal Prolapse, Stress Incontinence · Cashless facility wherever possible in network hospital
e) Pre-hospitalization Expenses: Medical expenses incurred up to 30 days immediately before the insured person 17. Sterility and Infertility - Code Excl 17: Expenses related to sterility and infertility. This includes:
Cumulative Bonus (Applicable for Section I only) 12. Varicose veins and Varicose ulcers i. Any type of contraception, sterilization · In non-network hospitals payment must be made up-front and then reimbursement will be effected on
is hospitalized 13. All types of transplant and related surgeries. submission of documents
The insured person will be eligible for Cumulative bonus calculated at 5% of basic sum insured for each claim free year ii. Assisted Reproduction services including artificial insemination and advanced reproductive technologies
f) Post Hospitalization Expenses: Medical expenses incurred up to 60 days immediately after the insured person is subject to a maximum of 50% of the basic sum insured 14. Congenital Internal disease / defect For Section II
such as IVF, ZIFT, GIFT, ICSI
discharged from the hospital. The amount payable shall be up to 2% of the basic sum insured per hospitalization Special Conditions i. Certificate from the Treating Doctor confirming the Cancer diagnosis
3. 30-day waiting period - Code Excl 03 iii. Gestational Surrogacy
g) All day care procedures are covered 1. The Cumulative bonus will be calculated on the expiring Basic Sum Insured ii. Clinical, Radiological, Histological, Pathological, Histopathological and laboratory reports in support
A. Expenses related to the treatment of any illness within 30 days from the first policy commencement date iv. Reversal of sterilization
h) Cataract treatment: The company will pay the expenses incurred for treatment of cataract up to the limits 2. If the insured opts to reduce the Basic Sum Insured at the subsequent renewal, the limit of indemnity by way of such shall be excluded except claims arising due to an accident, provided the same are covered.
mentioned below; Cumulative bonus shall not exceed such reduced basic sum insured 18. Maternity - Code Excl 18 Disclosure to information norms
B. This exclusion shall not, however, apply if the Insured Person has continuous coverage for more than
3. In the event of a claim resulting in; i. Medical treatment expenses traceable to childbirth (including complicated deliveries and caesarean The policy shall become void and all premium paid thereon shall be forfeited to the Company in the event of mis-
Basic Sum Insured (Rs.) Limit of Cataract Surgery (Rs.) twelve months.
a. Partial utilization of Basic Sum Insured, such cumulative bonus so granted will be reduced at the same rate at sections incurred during hospitalization) except ectopic pregnancy; representation, mis description or non-disclosure of any material fact by the policy holder.
C. The within referred waiting period is made applicable to the enhanced sum insured in the event of
30,000/- per eye per person and not exceeding which it has accrued ii. Expenses towards miscarriage (unless due to an accident) and lawful medical termination of pregnancy
5,00,000/- granting higher sum insured subsequently. Cancellation
40,000/- per person per policy period b. Full utilization of Basic Sum Insured and nil utilization of cumulative bonus accrued, such cumulative bonus so during the policy period.
granted will be reduced at the same rate at which it has accrued 4. Investigation & Evaluation - Code Excl 04 i. The policyholder may cancel this policy by giving 15 days' written notice and in such an event, the Company
40,000/- per eye per person and not exceeding 19. Circumcision(unless necessary for treatment of a disease not excluded under this policy or necessitated due to
7,50,000/- and 10,00,000/- c. Full utilization of Basic Sum Insured and partial utilization of cumulative bonus accrued, the cumulative bonus A. Expenses related to any admission primarily for diagnostics and evaluation purposes only are excluded. shall refund premium for the unexpired policy period as detailed below;
60,000/- per person per policy period an accident), Preputioplasty, Frenuloplasty, Preputial Dilatation and Removal of SMEGMA - Code Excl 19
granted on renewal will be the balance cumulative bonus available and will be reduced at the same rate at B. Any diagnostic expenses which are not related or not incidental to the current diagnosis and treatment are
which it has accrued excluded. 20. Congenital External Condition / Defects / Anomalies - Code Excl 20 Cancellation table applicable without instalment option
i) Cost of Health Checkup: Expenses incurred towards Cost of Health check-up up to Rs.2,500/- for every claim free year.
Note: d. Full utilization of Basic Sum Insured and full utilization of cumulative bonus accrued, the cumulative bonus on 5. Rest Cure, rehabilitation (except to the extent covered under Section I (l)) and respite care - Code Excl 05: 21. Convalescence , general debility, run-down condition, Nutritional deficiency states - Code Excl 21
1. This benefit is payable on renewal and when the renewed policy is in force renewal will be “nil” Period on risk Rate of premium to be retained
Expenses related to any admission primarily for enforced bed rest and not for receiving treatment. This also includes: 22. Intentional self injury - Code Excl 22
2. Payment under this benefit does not form part of the sum insured and will not impact the Bonus. Exclusions 1. Custodial care either at home or in a nursing facility for personal care such as help with activities of daily Up to one mth 22.5% of the policy premium
living such as bathing, dressing, moving around either by skilled nurses or assistant or non-skilled persons. 23. Injury/disease directly or indirectly caused by or arising from or attributable to war, invasion, act of foreign
j) The Insured Person is given the facility of obtaining a Medical Second Opinion from a Doctor in the Company's The Company shall not be liable to make any payments under this policy in respect of any expenses what so ever incurred Exceeding one mth up to 3 mths 37.5% of the policy premium
2. Any services for people who are terminally ill to address physical, social, emotional and spiritual needs. enemy, warlike operations (whether war be declared or not) - Code Excl 24
network of Medical Practitioners. All the medical records provided by the Insured Person will be submitted to the by the insured person in connection with or in respect of;
Doctor either online: e_medicalopinion@starhealth.in or through post/courier 6. Obesity/ Weight Control - Code Excl 06: Expenses related to the surgical treatment of obesity that does not 24. Injury or disease directly or indirectly caused by or contributed to by nuclear weapons/material - Code Excl 25 Exceeding 3 mths up to 6 mths 57.5% of the policy premium
1. Pre-Existing Diseases - Code Excl 01
Subject to the following conditions; A. Expenses related to the treatment of a pre-existing Disease (PED) and its direct complications shall be fulfill all the below conditions: 25. Expenses incurred on Enhanced External Counter Pulsation Therapy and related therapies, Chelation therapy, Exceeding 6 mths up to 9 mths 80% of the policy premium
· This should be specifically requested for by the Insured Person excluded until the expiry 30 months of continuous coverage after the date of inception of the first policy with 1. Surgery to be conducted is upon the advice of the Doctor Hyperbaric Oxygen Therapy, Rotational Field Quantum Magnetic Resonance Therapy, VAX-D, Low level laser
· This opinion is given without examining the patient, based only on the medical records submitted. insurer. 2. The surgery/Procedure conducted should be supported by clinical protocols therapy, Photodynamic therapy and such other therapies - Code Excl 26 Exceeding 9 mths Full of the policy premium
1 2 3 4 5
· The second opinion should be only for medical reasons and not for medico-legal purposes. B. In case of enhancement of sum insured the exclusion shall apply afresh to the extent of sum insured 3. The member has to be 18 years of age or older and 26. Unconventional, Untested, Experimental therapies - Code Excl 27
STAR CANCER CARE PLATINUM INSURANCE POLICY · Any liability due to any errors or omission or consequences of any action taken in reliance of the second increase. 4. Body Mass Index (BMI); 27. Chondrocyte Implantation, Procedures using Platelet Rich plasma and Intra articular injection therapy -
Unique Identification No.: SHAHLIP22031V022122 opinion provided by the Medical Practitioner is outside the scope of this policy. C. If the Insured Person is continuously covered without any break as defined under the portability norms of a. greater than or equal to 40 or Code Excl 28
· Utilizing this facility alone will not be considered as a claim. the extant IRDAI (Health Insurance) Regulations, then waiting period for the same would be reduced to b. greater than or equal to 35 in conjunction with any of the following severe co-morbidities following
Star Cancer Care Platinum Insurance Policy offers protection for persons diagnosed with Cancer. The policy keeps the the extent of prior coverage. failure of less invasive methods of weight loss: 28. Biologicals, except when administered as an in-patient, when clinically indicated and hospitalization
k) Wellness Service: This program intends to promote, incentivize and to reward the Insured Persons' healthy life
insured financially prepared during their fight against Cancer and provides indemnity coverage for medical expenses D. Coverage under the policy after the expiry of 30 months for any pre-existing disease is subject to the i. Obesity-related cardiomyopathy warranted - Code Excl 29
style through various wellness activities. The Insured Person can avail the following services: (i) Diet and Nutrition
incurred for Cancer and Non-cancer ailments. Program: To strengthen/restore the immune system. (ii) Weight Management Program – To maintain healthy weight same being declared at the time of application and accepted by Insurer. ii. Coronary heart disease 29. All treatment for Priapism and erectile dysfunctions - Code Excl 30
(iii) Specialist Consultation –Available through Star Tele-health app. 2. Specified disease / procedure waiting period - Code Excl 02 iii. Severe Sleep Apnea
Policy Term 30. Inoculation or Vaccination (except for post-bite treatment and for medical treatment for therapeutic reasons) -
l) Rehabilitation and Pain Management: The company will pay the medical expenses for Rehabilitation and Pain A. Expenses related to the treatment of the listed Conditions, surgeries/treatments shall be excluded until iv. Uncontrolled Type2 Diabetes
1 year Code Excl 31
Management up to the sub-limit (or) maximum up to 10% of the basic sum insured whichever is less, per policy year. the expiry of 24 months of continuous coverage after the date of inception of the first policy with us. This 7. Change-of-Gender treatments - Code Excl 07: Expenses related to any treatment, including surgical
Type of Policy (For details please refer website: www.starhealth.in) exclusion shall not be applicable for claims arising due to an accident. management, to change characteristics of the body to those of the opposite sex. 31. Dental treatment or surgery unless necessitated due to accidental injuries and requiring hospitalization.
Individual Note: Company's liability under this benefit shall not exceed 10% of Basic Sum insured B. In case of enhancement of sum insured the exclusion shall apply afresh to the extent of sum insured (Dental implants are not payable) - Code Excl 32
Rehabilitation: The Company will pay the expenses for rehabilitation, if availed at authorized centres as an In- increase. 8. Cosmetic or plastic Surgery - Code Excl 08: Expenses for cosmetic or plastic surgery or any treatment to
Eligibility change appearance unless for reconstruction following an Accident, Burn(s) or Cancer or as part of medically 32. Medical and / or surgical treatment of Sleep apnea, treatment for endocrine disorders - Code Excl 33
patient/Out-patient, and if there is an admissible claim for In-patient hospitalization for an injury, disease or illness C. If any of the specified disease/procedure falls under the waiting period specified for pre-Existing
Persons who have been diagnosed with Cancer, aged between 5 months and 65 years can avail this Insurance. Proposer specified below; necessary treatment to remove a direct and immediate health risk to the insured. For this to be considered a 33. Hospital registration charges, admission charges, telephone charges and such other charges - Code Excl 34
diseases, then the longer of the two waiting periods shall apply. medical necessity, it must be certified by the attending Medical Practitioner.
should be aged 18 years and above. 1. Poly Trauma D. The waiting period for listed conditions shall apply even if contracted after the policy or declared and 34. Cost of spectacles and contact lens, hearing aids, walkers and crutches, wheel chairs, Cochlear implants
Sum Insured Options 2. Head injury accepted without a specific exclusion. 9. Hazardous or Adventure sports - Code Excl 09: Expenses related to any treatment necessitated due to and procedure related hospitalization expenses, CPAP, BIPAP, Continuous Ambulatory Peritoneal Dialysis,
Section I - Rs.5,00,000/-, Rs.7,50,000/- and Rs.10,00,000/- 3. Diseases of the spine participation as a professional in hazardous or adventure sports, including but not limited to, para-jumping, rock
E. If the Insured Person is continuously covered without any break as defined under the applicable norms on infusion pump and such other similar aids - Code Excl 35
4. Stroke climbing, mountaineering, rafting, motor racing, horse racing or scuba diving, hand gliding, sky diving, deep-
Section II - 50% of Section I sum insured.(Sum Insured under Section II cannot vary) portability stipulated by IRDAI, then waiting period for the same would be reduced to the extent of prior
Pain Management: Cover for treatment of pain management subject to the limits sea diving. 35. Any hospitalizations which are not Medically Necessary - Code Excl 36
coverage.
Pre medical Examination 10. Breach of law - Code Excl 10: Expenses for treatment directly arising from or consequent upon any Insured 36. Other Excluded Expenses as detailed in the website www.starhealth.in - Code Excl 37
m) Coverage for Modern Treatment: Expenses are subject to the limits. F. List of specific diseases/procedures
There is no pre medical tests irrespective of age. The previous medical records including details of treatment to be submitted (For details please refer website: www.starhealth.in) 1. Treatment of Cataract and diseases of the anterior and posterior chamber of the Eye, Diseases of Person committing or attempting to commit a breach of law with criminal intent.
along with proposal. 37. Existing disease/s, disclosed by the insured and mentioned in the policy schedule (based on insured's
n) Hospice Care: Payable up to 20% of sum insured at network providers on indemnity basis, payable once in life ENT, Diseases related to Thyroid, Benign diseases of the breast. 11. Excluded Providers - Code Excl 11: Expenses incurred towards treatment in any hospital or by any Medical consent), for specified ICD codes - Code Excl 38
Instalment Facility available time. Available after a waiting period of 12 months from the policy inception. 2. Subcutaneous Benign Lumps, Sebaceous cyst, Dermoid cyst, Mucous cyst lip / cheek, Carpal Practitioner or any other provider specifically excluded by the Insurer and disclosed in its website / notified to
Premium can be paid Quarterly, Half yearly. Premium can also be paid Annually Hospice care in Oncology is a special kind of care that focuses on the quality of life of patients (as well as their Tunnel Syndrome, Trigger Finger, Lipoma, Neurofibroma, Fibroadenoma, Ganglion and similar the policyholders are not admissible. However, in case of life threatening situations or following an accident, 38. Expenses incurred for treatment of diseases/illness/accidental injuries by systems of medicine other than
caregivers) who are experiencing an advanced, life-limiting cancers. pathology expenses up to the stage of stabilization are payable but not the complete claim. allopathy - Code Excl 39
For instalment mode of payment there will be loading as given below;
Hospice care provides compassionate care for cancer patients during their last phases of life so that they can live as 3. All treatments (Conservative, Operative treatment) and all types of intervention for Diseases related
Quarterly - 3% | Half Yearly - 2% 12. Treatment for, Alcoholism, drug or substance abuse or any addictive condition and consequences thereof - 39. Naturopathy - Code Excl 40
fully and comfortably as possible. to Tendon, Ligament, Fascia, Bones and Joint Including Arthroscopy and Arthroplasty / Joint
Note: This loading will be applied on annual premium Replacement [other than caused by accident]. Code Excl 12
o) Copayment: This policy is subject to co-payment of 10% of each and every claim amount for fresh as well as Moratorium Period
Policy Benefits renewal policies for insured persons whose age at the time of entry is 61 years and above 4. All types of treatment for Degenerative disc and Vertebral diseases including Replacement of 13. Treatments received in health hydros, nature cure clinics, spas or similar establishments or private beds After completion of eight continuous years under the policy no look back to be applied. This period of eight years is
Section I Indemnity Cover (Applicable for treatment of Cancer and Non Cancer) bones and joints and Degenerative diseases of the Musculo-skeletal system, Prolapse of registered as a nursing home attached to such establishments or where admission is arranged wholly or partly
Section II Lumpsum Cover for Cancer (Optional Cover Available only if specifically opted on payment of called as moratorium period. The moratorium would be applicable for the sums insured of the first policy and
Intervertebral Disc (other than caused by accident), for domestic reasons - Code Excl 13
a) Room (Single Standard A/C), Boarding, Nursing expenses as provided by the Hospital / Nursing Home. additional premium and shown in the policy schedule) - If during the period stated in the Schedule the insured person subsequently completion of 8 continuous years would be applicable from date of enhancement of sums insured
Note: Hospitalisation expenses which vary based on the room occupied by the insured person will be 5. All treatments (conservative, interventional, laparoscopic and open) related to Hepato-pancreato-
suffers a recurrence, metastasis, and / or a second malignancy unrelated to first cancer, then the Company will pay a lump 14. Dietary supplements and substances that can be purchased without prescription, including but not limited to only on the enhanced limits. After the expiry of Moratorium Period no health insurance claim shall be contestable
considered in proportion to the room category stated in the policy schedule or actuals whichever is less. biliary diseases including Gall bladder and Pancreatic calculi. All types of management for Kidney
sum amount stated in the policy schedule. This benefit is in addition to the sum insured of Indemnity cover under Section I. Vitamins, minerals and organic substances unless prescribed by a medical practitioner as part of except for proven fraud and permanent exclusions specified in the policy contract. The policies would however be
calculi and Genitourinary tract calculi.
Proportionate deductions are not applied in respect of the hospitals which do not follow differential billing hospitalization claim or day care procedure - Code Excl 14 subject to all limits, sub limits, co-payments, deductibles as per the policy contract.
Note: 6. All types of Hernia,
or for those expenses in respect of which differential billing is not adopted based on the room category. 1. A waiting period of 30 months is applicable for this lump-sum benefit cover. 7. Desmoid Tumor, Umbilical Granuloma, Umbilical Sinus, Umbilical Fistula, 15. Refractive Error - Code Excl 15: Expenses related to the treatment for correction of eye sight due to refractive
b) Surgeon, Anesthetist, Medical Practitioner, Consultants, Specialist Fees Claims Procedure
2. Claim under this benefit is admissible only if treatment for recurrence, metastasis and/or a second malignancy unrelated 8. All treatments (conservative, interventional, laparoscopic and open) related to all Diseases of error less than 7. 5 dioptres.
c) Anesthesia, blood, oxygen, operation theatre charges, ICU Charges, medicines and drugs to first cancer commences after 30 months from first inception of Star Cancer Care Platinum Insurance Policy. · Call the 24 hour help-line for assistance - 1800 425 2255 / 1800 102 4477
Cervix, Uterus, Fallopian tubes, Ovaries, Uterine Bleeding, Pelvic Inflammatory Diseases 16. Unproven Treatments - Code Excl 16: Expenses related to any unproven treatment, services and supplies
d) Emergency Road Ambulance charges, for transportation of the insured person by private ambulance service when 3. On an admissible claim for lump-sum, the coverage under Section II ceases and the policy will continue with Section 9. All Diseases of Prostate, Stricture Urethra, all Obstructive Uropathies, · In case of planned hospitalization, inform 24 hours prior to admission in the hospital
for or in connection with any treatment. Unproven treatments are treatments, procedures or supplies that lack
this is needed for medical reasons to go to hospital for treatment, provided however there is an admissible claim I for the sum insured stated in the policy schedule for the remaining policy period. 10. Benign Tumours of Epididymis, Spermatocele, Varicocele, Hydrocele, significant medical documentation to support their effectiveness. · In case of emergency hospitalization information to be given within 24 hours after hospitalization
under the policy 4. On an admissible claim for lump-sum under Section II, the subsequent renewal, will be for Section I only. 11. Fistula, Fissure in Ano, Hemorrhoids, Pilonidal Sinus and Fistula, Rectal Prolapse, Stress Incontinence · Cashless facility wherever possible in network hospital
e) Pre-hospitalization Expenses: Medical expenses incurred up to 30 days immediately before the insured person 17. Sterility and Infertility - Code Excl 17: Expenses related to sterility and infertility. This includes:
Cumulative Bonus (Applicable for Section I only) 12. Varicose veins and Varicose ulcers i. Any type of contraception, sterilization · In non-network hospitals payment must be made up-front and then reimbursement will be effected on
is hospitalized 13. All types of transplant and related surgeries. submission of documents
The insured person will be eligible for Cumulative bonus calculated at 5% of basic sum insured for each claim free year ii. Assisted Reproduction services including artificial insemination and advanced reproductive technologies
f) Post Hospitalization Expenses: Medical expenses incurred up to 60 days immediately after the insured person is subject to a maximum of 50% of the basic sum insured 14. Congenital Internal disease / defect For Section II
such as IVF, ZIFT, GIFT, ICSI
discharged from the hospital. The amount payable shall be up to 2% of the basic sum insured per hospitalization Special Conditions i. Certificate from the Treating Doctor confirming the Cancer diagnosis
3. 30-day waiting period - Code Excl 03 iii. Gestational Surrogacy
g) All day care procedures are covered 1. The Cumulative bonus will be calculated on the expiring Basic Sum Insured ii. Clinical, Radiological, Histological, Pathological, Histopathological and laboratory reports in support
A. Expenses related to the treatment of any illness within 30 days from the first policy commencement date iv. Reversal of sterilization
h) Cataract treatment: The company will pay the expenses incurred for treatment of cataract up to the limits 2. If the insured opts to reduce the Basic Sum Insured at the subsequent renewal, the limit of indemnity by way of such shall be excluded except claims arising due to an accident, provided the same are covered.
mentioned below; Cumulative bonus shall not exceed such reduced basic sum insured 18. Maternity - Code Excl 18 Disclosure to information norms
B. This exclusion shall not, however, apply if the Insured Person has continuous coverage for more than
3. In the event of a claim resulting in; i. Medical treatment expenses traceable to childbirth (including complicated deliveries and caesarean The policy shall become void and all premium paid thereon shall be forfeited to the Company in the event of mis-
Basic Sum Insured (Rs.) Limit of Cataract Surgery (Rs.) twelve months.
a. Partial utilization of Basic Sum Insured, such cumulative bonus so granted will be reduced at the same rate at sections incurred during hospitalization) except ectopic pregnancy; representation, mis description or non-disclosure of any material fact by the policy holder.
C. The within referred waiting period is made applicable to the enhanced sum insured in the event of
30,000/- per eye per person and not exceeding which it has accrued ii. Expenses towards miscarriage (unless due to an accident) and lawful medical termination of pregnancy
5,00,000/- granting higher sum insured subsequently. Cancellation
40,000/- per person per policy period b. Full utilization of Basic Sum Insured and nil utilization of cumulative bonus accrued, such cumulative bonus so during the policy period.
granted will be reduced at the same rate at which it has accrued 4. Investigation & Evaluation - Code Excl 04 i. The policyholder may cancel this policy by giving 15 days' written notice and in such an event, the Company
40,000/- per eye per person and not exceeding 19. Circumcision(unless necessary for treatment of a disease not excluded under this policy or necessitated due to
7,50,000/- and 10,00,000/- c. Full utilization of Basic Sum Insured and partial utilization of cumulative bonus accrued, the cumulative bonus A. Expenses related to any admission primarily for diagnostics and evaluation purposes only are excluded. shall refund premium for the unexpired policy period as detailed below;
60,000/- per person per policy period an accident), Preputioplasty, Frenuloplasty, Preputial Dilatation and Removal of SMEGMA - Code Excl 19
granted on renewal will be the balance cumulative bonus available and will be reduced at the same rate at B. Any diagnostic expenses which are not related or not incidental to the current diagnosis and treatment are
which it has accrued excluded. 20. Congenital External Condition / Defects / Anomalies - Code Excl 20 Cancellation table applicable without instalment option
i) Cost of Health Checkup: Expenses incurred towards Cost of Health check-up up to Rs.2,500/- for every claim free year.
Note: d. Full utilization of Basic Sum Insured and full utilization of cumulative bonus accrued, the cumulative bonus on 5. Rest Cure, rehabilitation (except to the extent covered under Section I (l)) and respite care - Code Excl 05: 21. Convalescence , general debility, run-down condition, Nutritional deficiency states - Code Excl 21
1. This benefit is payable on renewal and when the renewed policy is in force renewal will be “nil” Period on risk Rate of premium to be retained
Expenses related to any admission primarily for enforced bed rest and not for receiving treatment. This also includes: 22. Intentional self injury - Code Excl 22
2. Payment under this benefit does not form part of the sum insured and will not impact the Bonus. Exclusions 1. Custodial care either at home or in a nursing facility for personal care such as help with activities of daily Up to one mth 22.5% of the policy premium
living such as bathing, dressing, moving around either by skilled nurses or assistant or non-skilled persons. 23. Injury/disease directly or indirectly caused by or arising from or attributable to war, invasion, act of foreign
j) The Insured Person is given the facility of obtaining a Medical Second Opinion from a Doctor in the Company's The Company shall not be liable to make any payments under this policy in respect of any expenses what so ever incurred Exceeding one mth up to 3 mths 37.5% of the policy premium
2. Any services for people who are terminally ill to address physical, social, emotional and spiritual needs. enemy, warlike operations (whether war be declared or not) - Code Excl 24
network of Medical Practitioners. All the medical records provided by the Insured Person will be submitted to the by the insured person in connection with or in respect of;
Doctor either online: e_medicalopinion@starhealth.in or through post/courier 6. Obesity/ Weight Control - Code Excl 06: Expenses related to the surgical treatment of obesity that does not 24. Injury or disease directly or indirectly caused by or contributed to by nuclear weapons/material - Code Excl 25 Exceeding 3 mths up to 6 mths 57.5% of the policy premium
1. Pre-Existing Diseases - Code Excl 01
Subject to the following conditions; A. Expenses related to the treatment of a pre-existing Disease (PED) and its direct complications shall be fulfill all the below conditions: 25. Expenses incurred on Enhanced External Counter Pulsation Therapy and related therapies, Chelation therapy, Exceeding 6 mths up to 9 mths 80% of the policy premium
· This should be specifically requested for by the Insured Person excluded until the expiry 30 months of continuous coverage after the date of inception of the first policy with 1. Surgery to be conducted is upon the advice of the Doctor Hyperbaric Oxygen Therapy, Rotational Field Quantum Magnetic Resonance Therapy, VAX-D, Low level laser
· This opinion is given without examining the patient, based only on the medical records submitted. insurer. 2. The surgery/Procedure conducted should be supported by clinical protocols therapy, Photodynamic therapy and such other therapies - Code Excl 26 Exceeding 9 mths Full of the policy premium
1 2 3 4 5
Cancellation table applicable with instalment option of Half-yearly premium payment frequency Possibility of Revision of Terms of the Policy lncluding the Premium Rates
The Company, with prior approval of lRDAl, may revise or modify the terms of the policy including the premium rates. Schedule of Benefits Premium Chart Excluding Tax
Period on risk Rate of premium to be retained The insured person shall be notified three months before the changes are effected.
Up to 1 Mth 45% of the total premium received Section I : Base Cover
Premium Payment In Instalments Is this part of the
Exceeding one mth up to 4 mths 87.5% of the total premium received Subject / Sum Insured Premium Per Year (in Rs.)
lf the insured person has opted for Payment of Premium on an instalment basis i.e. Half Yearly or Quarterly as 5 7.5 10 sum insured/In addition
Exceeding 4 mths up to 6 mths 100% of the total premium received (INR in Lac)
mentioned in the policy Schedule/Certificate of Insurance, the following Conditions shall apply (notwithstanding any to the sum insured
Exceeding 6 mths up to 7 mths 65% of the total premium received terms contrary elsewhere in the policy); Age Band /
5,00,000 7,50,000 10,00,000
i. Grace Period of 7 days would be given to pay the instalment premium due for the policy. Sum Insured (Rs.)
Exceeding 7 mths up to 10 mths 85% of the total premium received
Exceeding 10 mths 100% of the total premium received ii. During such grace period, coverage will not be available from the due date of instalment premium till the date of In-patient Hospitalization Single Standard A/C Room Part of the sum insured 5m-29 14,285 17,995 20,870
receipt of premium by Company.
Cancellation table applicable with instalment option of Quarterly premium payment frequency ICU, Doctor Fee, Medicines, 30-39 16,190 20,370 23,605
iii. The insured person will get the accrued continuity benefit in respect of the "Waiting Periods", "Specific Waiting Covered Part of the sum insured
Periods" in the event of payment of premium within the stipulated grace Period Tests
Period on risk Rate of premium to be retained 40-49 18,050 22,750 26,340
Up to 1 Mth 87.5% of the total premium received iv. No interest will be charged lf the instalment premium is not paid on due date Day Care Procedures Covered Part of the sum insured
Exceeding one mth up to 3 mths 100% of the total premium received v. ln case of instalment premium due not received within the grace period, the policy will get cancelled 50-59 19,875 25,130 29,075
Exceeding 3 mths up to 4 mths 87.5% of the total premium received vi. ln the event of a claim, all subsequent premium instalments shall immediately become due and payable 60-69 24,430 30,845 35,830
for one eye -
Exceeding 4 mths up to 6 mths 100% of the total premium received vii. The company has the right to recover and deduct all the pending installments from the claim amount due under
for one eye - 30,000 40,000/- &
the policy Cataract Limit (INR) Part of the sum insured Above 69 28,990 36,540 42,385
Exceeding 6 mths up to 7 mths 85% of the total premium received per policy year - 40,000 per policy
Exceeding 7 mths up to 9 mths 100% of the total premium received Free Look Period year - 60,000 Section II : Lump sum cover for Cancer (Optional Cover)
Exceeding 9 mths up to 10 mths 85% of the total premium received The Free Look Period shall be applicable on new individual health insurance policies and not on renewals or at the time
of porting/migrating the policy. Premium Per Year (in Rs.)
Exceeding 10 mths 100% of the total premium received Emergency Road Ambulance Covered Part of the sum insured
The insured person shall be allowed free look period of fifteen days from date of receipt of the policy document to Age Band /
Notwithstanding anything contained herein or otherwise, no refunds of premium shall be made in respect of review the terms and conditions of the policy, and to return the same if not acceptable. 2,50,000 3,75,000 5,00,000
Pre Hospitalization Expenses 30 days Part of the sum insured Sum Insured (Rs.)
Cancellation where, any claim has been admitted or has been lodged or any benefit has been availed by the insured lf the insured has not made any claim during the Free Look Period, the insured shall be entitled to;
person under the policy. i. a refund of the premium paid less any expenses incurred by the Company on medical examination of the insured 60 days (up to 2% of the basic 5m-29 10,135 15,200 20,265
ii. The Company may cancel the policy at any time on grounds of misrepresentation non-disclosure of material person and the stamp duty charges or Post Hospitalization Expenses Part of the sum insured
sum insured per hospitalization)
facts, fraud by the insured person by giving 15 days' written notice. There would be no refund of premium on 30-39 10,135 15,200 20,265
ii. where the risk has already commenced and the option of return of the policy is exercised by the insured person, a
cancellation on grounds of misrepresentation, non-disclosure of material facts or fraud deduction towards the proportionate risk premium for period of cover or Health Check-Up
40-49 10,135 15,200 20,265
(available for every claim 2,500/- 2,500/- 2,500/- In addition to the sum insured
Automatic Expiry iii. where only a part of the insurance coverage has commenced, such proportionate premium commensurate with
free year) 50-59 10,135 15,200 20,265
the insurance coverage during such period;
The insurance under this policy with respect to each relevant Insured Person policy shall expire immediately on the
earlier of the following events: Enhancement of Sum insured Medical Second Opinion Available - 60-69 10,135 15,200 20,265
i. Upon the death of the Insured Person. Sum insured once opted cannot be enhanced even on renewal.
5% for every claim free year maximum Above 69 10,135 15,200 20,265
ii. Upon exhaustion of the Basic sum insured plus bonus under the policy. No Claim Bonus -
Withdrawal of the policy up to 50%
Migration i. In the likelihood of this product being withdrawn in future, the Company will intimate the insured person about the
The insured person will have the option to migrate the policy to other health insurance products/plans offered by the Diet and Nutrition Program, Weight The information provided in this brochure is only indicative. For more details on the risk factors, terms and
same 90 days prior to expiry of the policy.
company by applying for migration of the Policy atleast 30 days before the policy renewal date as per IRDAI Management programme and Specialist conditions, please read the policy wordings before concluding a sale.
ii. lnsured Person will have the option to migrate to similar health insurance product available with the Company at Wellness Services -
guidelines on Migration. lf such person is presently covered and has been continuously covered without any lapses Consultation available through
the time of renewal with all the accrued continuity benefits such as cumulative bonus, waiver of waiting period. as Or
Star Tele-Health App
under any health insurance product/plan offered by the company, the insured person will get the accrued continuity per IRDAI guidelines, provided the policy has been maintained without a break. Visit Website: www.starhealth.in
benefits in waiting periods as per IRDAI guidelines on migration. Rehabilitation &
The Company Covered up to 10% of the Sum Insured Part of the sum insured
For Detailed Guidelines on migration, kindly refer the link Pain management
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.aspx?page=PageNo3987 Star Health and Allied Insurance Co. Ltd., commenced its operations in 2006 as India's first Standalone Health
Insurance provider. As an exclusive Health Insurer, the Company is providing sterling services in Health, Personal Modern Treatments Covered (up to the sub-limits) Part of the sum insured
Portability Accident & Overseas Travel Insurance and is committed to setting international benchmarks in service and personal
The insured person will have the option to port the policy to other insurers by applying to such insurer to port the caring.
Hospice Care Up to 20% of the Basic Sum Insured in life time Part of the sum insured
entire policy along with all the members of the family, if any, at least 45 days before, but not earlier than 60 days from
Star Advantages
the policy renewal date as per IRDAI guidelines related to portability. lf such person is presently covered and has
been continuously covered without any lapses under any health insurance policy with an lndian General/Health · No Third Party Administrator, direct in-house claims settlement Optional Cover
insurer, the proposed insured person will get the accrued continuity benefits in waiting periods as per IRDAI · Faster and hassle – free claim settlement
guidelines on portability. · Cashless hospitalization
For Detailed Guidelines on portability, kindly refer the link Lump-sum benefit for Cancer
Buy this insurance (INR in Lac) 2.5 3.75 5 - IRDAI IS NOT INVOLVED IN ACTIVITIES LIKE SELLING INSURANCE POLICIES,
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.aspx?page=PageNo3987
ANNOUNCING BONUS OR INVESTMENT OF PREMIUMS. PUBLIC RECEIVING
Insurance is the subject matter of solicitation
Please contact our nearest Branch Office /our Agent or visit our website www.starhealth.in for online purchase (Waiting period 30 months)
Renewal SUCH PHONE CALLS ARE REQUESTED TO LODGE A POLICE COMPLAINT
The policy shall ordinarily be renewable except on grounds of fraud, misrepresentation by the Insured Person; Tax Benefits
i. The Company shall endeavor to give notice for renewal. However, the Company is not under obligation to give Payment of premium by any mode other than cash for this insurance is eligible for relief under Section 80D of the Waiting Period
any notice for renewal Income Tax Act 1961. Star Cancer Care Platinum Insurance Policy
ii. Renewal shall not be denied on the ground that the insured person had made a claim or claims in the Initial waiting period 30 days (except for Accidents) - Unique Identification No.: SHAHLIP22031V022122
Prohibition of Rebates
BRO / SCCP/ V.2 / 2022
preceding policy years
Section 41 of Insurance Act 1938 (Prohibition of rebates): No person shall allow or offer to allow, either directly or
iii. Request for renewal along with requisite premium shall be received by the Company before the end of the indirectly, as an inducement to any person to take out or renew or continue an insurance in respect of any kind of risk For specific diseases 24 months -
policy period Buy this Insurance Online at www.starhealth.in
relating to lives or property in India, any rebate of the whole or part of the commission payable or any rebate of the For Pre-Existing diseases Call Toll-free: 1800-425-2255 / 1800-102-4477,
iv. At the end of the policy period, the policy shall terminate and can be renewed within the Grace Period of 30 premium shown on the policy, nor shall any person taking out or renewing or continuing a policy accept any rebate, 30 months -
days to maintain continuity of benefits without break in policy. Coverage is not available during the grace (including Cancer) sms STAR to 56677 « Fax Toll Free No: 1800-425-5522
except such rebate as may be allowed in accordance with the published prospectuses or tables of the insurer: Any
period person making default in complying with the provisions of this section shall be liable for a penalty which may extend to For Hospice Care 12 months - Email : support@starhealth.in
v. No loading shall apply on renewals based on individual claims experience ten lakhs rupees. CIN : L66010TN2005PLC056649 « IRDAI Regn. No: 129
6 7 8
Cancellation table applicable with instalment option of Half-yearly premium payment frequency Possibility of Revision of Terms of the Policy lncluding the Premium Rates
The Company, with prior approval of lRDAl, may revise or modify the terms of the policy including the premium rates. Schedule of Benefits Premium Chart Excluding Tax
Period on risk Rate of premium to be retained The insured person shall be notified three months before the changes are effected.
Up to 1 Mth 45% of the total premium received Section I : Base Cover
Premium Payment In Instalments Is this part of the
Exceeding one mth up to 4 mths 87.5% of the total premium received Subject / Sum Insured Premium Per Year (in Rs.)
lf the insured person has opted for Payment of Premium on an instalment basis i.e. Half Yearly or Quarterly as 5 7.5 10 sum insured/In addition
Exceeding 4 mths up to 6 mths 100% of the total premium received (INR in Lac)
mentioned in the policy Schedule/Certificate of Insurance, the following Conditions shall apply (notwithstanding any to the sum insured
Exceeding 6 mths up to 7 mths 65% of the total premium received terms contrary elsewhere in the policy); Age Band /
5,00,000 7,50,000 10,00,000
i. Grace Period of 7 days would be given to pay the instalment premium due for the policy. Sum Insured (Rs.)
Exceeding 7 mths up to 10 mths 85% of the total premium received
Exceeding 10 mths 100% of the total premium received ii. During such grace period, coverage will not be available from the due date of instalment premium till the date of In-patient Hospitalization Single Standard A/C Room Part of the sum insured 5m-29 14,285 17,995 20,870
receipt of premium by Company.
Cancellation table applicable with instalment option of Quarterly premium payment frequency ICU, Doctor Fee, Medicines, 30-39 16,190 20,370 23,605
iii. The insured person will get the accrued continuity benefit in respect of the "Waiting Periods", "Specific Waiting Covered Part of the sum insured
Periods" in the event of payment of premium within the stipulated grace Period Tests
Period on risk Rate of premium to be retained 40-49 18,050 22,750 26,340
Up to 1 Mth 87.5% of the total premium received iv. No interest will be charged lf the instalment premium is not paid on due date Day Care Procedures Covered Part of the sum insured
Exceeding one mth up to 3 mths 100% of the total premium received v. ln case of instalment premium due not received within the grace period, the policy will get cancelled 50-59 19,875 25,130 29,075
Exceeding 3 mths up to 4 mths 87.5% of the total premium received vi. ln the event of a claim, all subsequent premium instalments shall immediately become due and payable 60-69 24,430 30,845 35,830
for one eye -
Exceeding 4 mths up to 6 mths 100% of the total premium received vii. The company has the right to recover and deduct all the pending installments from the claim amount due under
for one eye - 30,000 40,000/- &
the policy Cataract Limit (INR) Part of the sum insured Above 69 28,990 36,540 42,385
Exceeding 6 mths up to 7 mths 85% of the total premium received per policy year - 40,000 per policy
Exceeding 7 mths up to 9 mths 100% of the total premium received Free Look Period year - 60,000 Section II : Lump sum cover for Cancer (Optional Cover)
Exceeding 9 mths up to 10 mths 85% of the total premium received The Free Look Period shall be applicable on new individual health insurance policies and not on renewals or at the time
of porting/migrating the policy. Premium Per Year (in Rs.)
Exceeding 10 mths 100% of the total premium received Emergency Road Ambulance Covered Part of the sum insured
The insured person shall be allowed free look period of fifteen days from date of receipt of the policy document to Age Band /
Notwithstanding anything contained herein or otherwise, no refunds of premium shall be made in respect of review the terms and conditions of the policy, and to return the same if not acceptable. 2,50,000 3,75,000 5,00,000
Pre Hospitalization Expenses 30 days Part of the sum insured Sum Insured (Rs.)
Cancellation where, any claim has been admitted or has been lodged or any benefit has been availed by the insured lf the insured has not made any claim during the Free Look Period, the insured shall be entitled to;
person under the policy. i. a refund of the premium paid less any expenses incurred by the Company on medical examination of the insured 60 days (up to 2% of the basic 5m-29 10,135 15,200 20,265
ii. The Company may cancel the policy at any time on grounds of misrepresentation non-disclosure of material person and the stamp duty charges or Post Hospitalization Expenses Part of the sum insured
sum insured per hospitalization)
facts, fraud by the insured person by giving 15 days' written notice. There would be no refund of premium on 30-39 10,135 15,200 20,265
ii. where the risk has already commenced and the option of return of the policy is exercised by the insured person, a
cancellation on grounds of misrepresentation, non-disclosure of material facts or fraud deduction towards the proportionate risk premium for period of cover or Health Check-Up
40-49 10,135 15,200 20,265
(available for every claim 2,500/- 2,500/- 2,500/- In addition to the sum insured
Automatic Expiry iii. where only a part of the insurance coverage has commenced, such proportionate premium commensurate with
free year) 50-59 10,135 15,200 20,265
the insurance coverage during such period;
The insurance under this policy with respect to each relevant Insured Person policy shall expire immediately on the
earlier of the following events: Enhancement of Sum insured Medical Second Opinion Available - 60-69 10,135 15,200 20,265
i. Upon the death of the Insured Person. Sum insured once opted cannot be enhanced even on renewal.
5% for every claim free year maximum Above 69 10,135 15,200 20,265
ii. Upon exhaustion of the Basic sum insured plus bonus under the policy. No Claim Bonus -
Withdrawal of the policy up to 50%
Migration i. In the likelihood of this product being withdrawn in future, the Company will intimate the insured person about the
The insured person will have the option to migrate the policy to other health insurance products/plans offered by the Diet and Nutrition Program, Weight The information provided in this brochure is only indicative. For more details on the risk factors, terms and
same 90 days prior to expiry of the policy.
company by applying for migration of the Policy atleast 30 days before the policy renewal date as per IRDAI Management programme and Specialist conditions, please read the policy wordings before concluding a sale.
ii. lnsured Person will have the option to migrate to similar health insurance product available with the Company at Wellness Services -
guidelines on Migration. lf such person is presently covered and has been continuously covered without any lapses Consultation available through
the time of renewal with all the accrued continuity benefits such as cumulative bonus, waiver of waiting period. as Or
Star Tele-Health App
under any health insurance product/plan offered by the company, the insured person will get the accrued continuity per IRDAI guidelines, provided the policy has been maintained without a break. Visit Website: www.starhealth.in
benefits in waiting periods as per IRDAI guidelines on migration. Rehabilitation &
The Company Covered up to 10% of the Sum Insured Part of the sum insured
For Detailed Guidelines on migration, kindly refer the link Pain management
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.aspx?page=PageNo3987 Star Health and Allied Insurance Co. Ltd., commenced its operations in 2006 as India's first Standalone Health
Insurance provider. As an exclusive Health Insurer, the Company is providing sterling services in Health, Personal Modern Treatments Covered (up to the sub-limits) Part of the sum insured
Portability Accident & Overseas Travel Insurance and is committed to setting international benchmarks in service and personal
The insured person will have the option to port the policy to other insurers by applying to such insurer to port the caring.
Hospice Care Up to 20% of the Basic Sum Insured in life time Part of the sum insured
entire policy along with all the members of the family, if any, at least 45 days before, but not earlier than 60 days from
Star Advantages
the policy renewal date as per IRDAI guidelines related to portability. lf such person is presently covered and has
been continuously covered without any lapses under any health insurance policy with an lndian General/Health · No Third Party Administrator, direct in-house claims settlement Optional Cover
insurer, the proposed insured person will get the accrued continuity benefits in waiting periods as per IRDAI · Faster and hassle – free claim settlement
guidelines on portability. · Cashless hospitalization
For Detailed Guidelines on portability, kindly refer the link Lump-sum benefit for Cancer
Buy this insurance (INR in Lac) 2.5 3.75 5 - IRDAI IS NOT INVOLVED IN ACTIVITIES LIKE SELLING INSURANCE POLICIES,
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.aspx?page=PageNo3987
ANNOUNCING BONUS OR INVESTMENT OF PREMIUMS. PUBLIC RECEIVING
Insurance is the subject matter of solicitation
Please contact our nearest Branch Office /our Agent or visit our website www.starhealth.in for online purchase (Waiting period 30 months)
Renewal SUCH PHONE CALLS ARE REQUESTED TO LODGE A POLICE COMPLAINT
The policy shall ordinarily be renewable except on grounds of fraud, misrepresentation by the Insured Person; Tax Benefits
i. The Company shall endeavor to give notice for renewal. However, the Company is not under obligation to give Payment of premium by any mode other than cash for this insurance is eligible for relief under Section 80D of the Waiting Period
any notice for renewal Income Tax Act 1961. Star Cancer Care Platinum Insurance Policy
ii. Renewal shall not be denied on the ground that the insured person had made a claim or claims in the Initial waiting period 30 days (except for Accidents) - Unique Identification No.: SHAHLIP22031V022122
Prohibition of Rebates
BRO / SCCP/ V.2 / 2022
preceding policy years
Section 41 of Insurance Act 1938 (Prohibition of rebates): No person shall allow or offer to allow, either directly or
iii. Request for renewal along with requisite premium shall be received by the Company before the end of the indirectly, as an inducement to any person to take out or renew or continue an insurance in respect of any kind of risk For specific diseases 24 months -
policy period Buy this Insurance Online at www.starhealth.in
relating to lives or property in India, any rebate of the whole or part of the commission payable or any rebate of the For Pre-Existing diseases Call Toll-free: 1800-425-2255 / 1800-102-4477,
iv. At the end of the policy period, the policy shall terminate and can be renewed within the Grace Period of 30 premium shown on the policy, nor shall any person taking out or renewing or continuing a policy accept any rebate, 30 months -
days to maintain continuity of benefits without break in policy. Coverage is not available during the grace (including Cancer) sms STAR to 56677 « Fax Toll Free No: 1800-425-5522
except such rebate as may be allowed in accordance with the published prospectuses or tables of the insurer: Any
period person making default in complying with the provisions of this section shall be liable for a penalty which may extend to For Hospice Care 12 months - Email : support@starhealth.in
v. No loading shall apply on renewals based on individual claims experience ten lakhs rupees. CIN : L66010TN2005PLC056649 « IRDAI Regn. No: 129
6 7 8
ii. Renewal shall not be denied on the ground that the insured person had made a claim or claims in the preceding
Cancellation table applicable with instalment option of Half-yearly premium payment frequency policy years Schedule of Benefits Premium Chart Excluding Tax
iii. Request for renewal along with requisite premium shall be received by the Company before the end of the policy
Period on risk Rate of premium to be retained Section I : Base Cover
period
Up to 1 Mth 45% of the total premium received iv. At the end of the policy period, the policy shall terminate and can be renewed within the Grace Period of 30 days Is this part of the
Subject / Sum Insured Premium Per Year (in Rs.)
to maintain continuity of benefits without break in policy. Coverage is not available during the grace period 5 7.5 10 sum insured/In addition
(INR in Lac)
Exceeding one mth up to 4 mths 87.5% of the total premium received to the sum insured
v. No loading shall apply on renewals based on individual claims experience Age Band /
5,00,000 7,50,000 10,00,000
Exceeding 4 mths up to 6 mths 100% of the total premium received Sum Insured (Rs.)
Possibility of Revision of Terms of the Policy lncluding the Premium Rates
Exceeding 6 mths up to 7 mths 65% of the total premium received In-patient Hospitalization Single Standard A/C Room Part of the sum insured 5m-29 14,285 17,995 20,870
The Company, with prior approval of lRDAl, may revise or modify the terms of the policy including the premium rates.
Exceeding 7 mths up to 10 mths 85% of the total premium received The insured person shall be notified three months before the changes are effected. ICU, Doctor Fee, Medicines, 30-39 16,190 20,370 23,605
Covered Part of the sum insured
Tests
Exceeding 10 mths 100% of the total premium received Premium Payment In Instalments 40-49 18,050 22,750 26,340
lf the insured person has opted for Payment of Premium on an instalment basis i.e. Half Yearly or Quarterly as Day Care Procedures Covered Part of the sum insured
Cancellation table applicable with instalment option of Quarterly premium payment frequency mentioned in the policy Schedule/Certificate of Insurance, the following Conditions shall apply (notwithstanding any 50-59 19,875 25,130 29,075
terms contrary elsewhere in the policy);
Period on risk Rate of premium to be retained for one eye - 60-69 24,430 30,845 35,830
i. Grace Period of 7 days would be given to pay the instalment premium due for the policy.
ii. During such grace period, coverage will not be available from the due date of instalment premium till the date of for one eye - 30,000 40,000/- &
Up to 1 Mth 87.5% of the total premium received Cataract Limit (INR) Part of the sum insured Above 69 28,990 36,540 42,385
per policy year - 40,000 per policy
receipt of premium by Company.
year - 60,000 Section II : Lump sum cover for Cancer (Optional Cover)
Exceeding one mth up to 3 mths 100% of the total premium received iii. The insured person will get the accrued continuity benefit in respect of the "Waiting Periods", "Specific Waiting
Periods" in the event of payment of premium within the stipulated grace Period Premium Per Year (in Rs.)
Exceeding 3 mths up to 4 mths 87.5% of the total premium received
iv. No interest will be charged lf the instalment premium is not paid on due date Emergency Road Ambulance Covered Part of the sum insured
Exceeding 4 mths up to 6 mths 100% of the total premium received v. ln case of instalment premium due not received within the grace period, the policy will get cancelled Age Band /
2,50,000 3,75,000 5,00,000
vi. ln the event of a claim, all subsequent premium instalments shall immediately become due and payable Pre Hospitalization Expenses 30 days Part of the sum insured Sum Insured (Rs.)
Exceeding 6 mths up to 7 mths 85% of the total premium received
vii. The company has the right to recover and deduct all the pending installments from the claim amount due under 60 days (up to 2% of the basic 5m-29 10,135 15,200 20,265
Exceeding 7 mths up to 9 mths 100% of the total premium received the policy Post Hospitalization Expenses Part of the sum insured
sum insured per hospitalization)
30-39 10,135 15,200 20,265
Exceeding 9 mths up to 10 mths 85% of the total premium received
Free Look Period Health Check-Up
40-49 10,135 15,200 20,265
Exceeding 10 mths 100% of the total premium received The Free Look Period shall be applicable on new individual health insurance policies and not on renewals or at the time (available for every claim 2,500/- 2,500/- 2,500/- In addition to the sum insured
of porting/migrating the policy. free year) 50-59 10,135 15,200 20,265
Notwithstanding anything contained herein or otherwise, no refunds of premium shall be made in respect of The insured person shall be allowed free look period of fifteen days from date of receipt of the policy document to
Cancellation where, any claim has been admitted or has been lodged or any benefit has been availed by the insured review the terms and conditions of the policy, and to return the same if not acceptable. Medical Second Opinion Available - 60-69 10,135 15,200 20,265
person under the policy. lf the insured has not made any claim during the Free Look Period, the insured shall be entitled to;
5% for every claim free year maximum Above 69 10,135 15,200 20,265
ii. The Company may cancel the policy at any time on grounds of misrepresentation non-disclosure of material i. a refund of the premium paid less any expenses incurred by the Company on medical examination of the insured No Claim Bonus -
facts, fraud by the insured person by giving 15 days' written notice. There would be no refund of premium on up to 50%
person and the stamp duty charges or
cancellation on grounds of misrepresentation, non-disclosure of material facts or fraud ii. where the risk has already commenced and the option of return of the policy is exercised by the insured person, a Diet and Nutrition Program, Weight The information provided in this brochure is only indicative. For more details on the risk factors, terms and
Automatic Expiry deduction towards the proportionate risk premium for period of cover or Management programme and Specialist conditions, please read the policy wordings before concluding a sale.
Wellness Services -
iii. where only a part of the insurance coverage has commenced, such proportionate premium commensurate with Consultation available through
The insurance under this policy with respect to each relevant Insured Person policy shall expire immediately on the Or
Star Tele-Health App
earlier of the following events: the insurance coverage during such period; Visit Website: www.starhealth.in
i. Upon the death of the Insured Person. Rehabilitation &
Enhancement of Sum insured Covered up to 10% of the Sum Insured Part of the sum insured
ii. Upon exhaustion of the Basic sum insured plus bonus under the policy. Pain management
Sum insured once opted cannot be enhanced even on renewal.
Migration Modern Treatments Covered (up to the sub-limits) Part of the sum insured
Withdrawal of the policy
The insured person will have the option to migrate the policy to other health insurance products/plans offered by the
company by applying for migration of the Policy atleast 30 days before the policy renewal date as per IRDAI i. In the likelihood of this product being withdrawn in future, the Company will intimate the insured person about the
Hospice Care Up to 20% of the Basic Sum Insured in life time Part of the sum insured
guidelines on Migration. lf such person is presently covered and has been continuously covered without any lapses same 90 days prior to expiry of the policy.
under any health insurance product/plan offered by the company, the insured person will get the accrued continuity ii. lnsured Person will have the option to migrate to similar health insurance product available with the Company at
the time of renewal with all the accrued continuity benefits such as cumulative bonus, waiver of waiting period. as Optional Cover
benefits in waiting periods as per IRDAI guidelines on migration.
For Detailed Guidelines on migration, kindly refer the link per IRDAI guidelines, provided the policy has been maintained without a break.
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.aspx?page=PageNo3987 Lump-sum benefit for Cancer
Buy this insurance IRDAI IS NOT INVOLVED IN ACTIVITIES LIKE SELLING INSURANCE POLICIES,
Portability (INR in Lac) 2.5 3.75 5 -
Please contact our nearest Branch Office /our Agent or visit our website www.starhealth.in for online purchase ANNOUNCING BONUS OR INVESTMENT OF PREMIUMS. PUBLIC RECEIVING
Insurance is the subject matter of solicitation
(Waiting period 30 months)
The insured person will have the option to port the policy to other insurers by applying to such insurer to port the
entire policy along with all the members of the family, if any, at least 45 days before, but not earlier than 60 days from Tax Benefits SUCH PHONE CALLS ARE REQUESTED TO LODGE A POLICE COMPLAINT
the policy renewal date as per IRDAI guidelines related to portability. lf such person is presently covered and has Payment of premium by any mode other than cash for this insurance is eligible for relief under Section 80D of the
Waiting Period
been continuously covered without any lapses under any health insurance policy with an lndian General/Health Income Tax Act 1961.
insurer, the proposed insured person will get the accrued continuity benefits in waiting periods as per IRDAI
Star Cancer Care Platinum Insurance Policy
guidelines on portability. Prohibition of Rebates Initial waiting period 30 days (except for Accidents) - Unique Identification No.: SHAHLIP22031V022122
BRO / SCCP/ V.1 / 2021
For Detailed Guidelines on portability, kindly refer the link Section 41 of Insurance Act 1938 (Prohibition of rebates): No person shall allow or offer to allow, either directly or
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.aspx?page=PageNo3987 indirectly, as an inducement to any person to take out or renew or continue an insurance in respect of any kind of risk For specific diseases 24 months -
Buy this Insurance Online at www.starhealth.in
relating to lives or property in India, any rebate of the whole or part of the commission payable or any rebate of the
Renewal premium shown on the policy, nor shall any person taking out or renewing or continuing a policy accept any rebate, For Pre-Existing diseases Call Toll-free: 1800-425-2255 / 1800-102-4477,
30 months -
The policy shall ordinarily be renewable except on grounds of fraud, misrepresentation by the Insured Person; except such rebate as may be allowed in accordance with the published prospectuses or tables of the insurer: Any (including Cancer) sms STAR to 56677 « Fax Toll Free No: 1800-425-5522
i. The Company shall endeavor to give notice for renewal. However, the Company is not under obligation to give person making default in complying with the provisions of this section shall be liable for a penalty which may extend to Email : support@starhealth.in
For Hospice Care 12 months -
any notice for renewal ten lakhs rupees. CIN : U66010TN2005PLC056649 « IRDAI Regn. No: 129
6 7 8
Cancellation table applicable with instalment option of Half-yearly premium payment frequency Possibility of Revision of Terms of the Policy lncluding the Premium Rates
The Company, with prior approval of lRDAl, may revise or modify the terms of the policy including the premium rates. Schedule of Benefits Premium Chart Excluding Tax
Period on risk Rate of premium to be retained The insured person shall be notified three months before the changes are effected.
Up to 1 Mth 45% of the total premium received Section I : Base Cover
Premium Payment In Instalments Is this part of the
Exceeding one mth up to 4 mths 87.5% of the total premium received Subject / Sum Insured Premium Per Year (in Rs.)
lf the insured person has opted for Payment of Premium on an instalment basis i.e. Half Yearly or Quarterly as 5 7.5 10 sum insured/In addition
Exceeding 4 mths up to 6 mths 100% of the total premium received (INR in Lac)
mentioned in the policy Schedule/Certificate of Insurance, the following Conditions shall apply (notwithstanding any to the sum insured
Exceeding 6 mths up to 7 mths 65% of the total premium received terms contrary elsewhere in the policy); Age Band /
5,00,000 7,50,000 10,00,000
i. Grace Period of 7 days would be given to pay the instalment premium due for the policy. Sum Insured (Rs.)
Exceeding 7 mths up to 10 mths 85% of the total premium received
Exceeding 10 mths 100% of the total premium received ii. During such grace period, coverage will not be available from the due date of instalment premium till the date of In-patient Hospitalization Single Standard A/C Room Part of the sum insured 5m-29 14,285 17,995 20,870
receipt of premium by Company.
Cancellation table applicable with instalment option of Quarterly premium payment frequency ICU, Doctor Fee, Medicines, 30-39 16,190 20,370 23,605
iii. The insured person will get the accrued continuity benefit in respect of the "Waiting Periods", "Specific Waiting Covered Part of the sum insured
Periods" in the event of payment of premium within the stipulated grace Period Tests
Period on risk Rate of premium to be retained 40-49 18,050 22,750 26,340
Up to 1 Mth 87.5% of the total premium received iv. No interest will be charged lf the instalment premium is not paid on due date Day Care Procedures Covered Part of the sum insured
Exceeding one mth up to 3 mths 100% of the total premium received v. ln case of instalment premium due not received within the grace period, the policy will get cancelled 50-59 19,875 25,130 29,075
Exceeding 3 mths up to 4 mths 87.5% of the total premium received vi. ln the event of a claim, all subsequent premium instalments shall immediately become due and payable 60-69 24,430 30,845 35,830
for one eye -
Exceeding 4 mths up to 6 mths 100% of the total premium received vii. The company has the right to recover and deduct all the pending installments from the claim amount due under
for one eye - 30,000 40,000/- &
the policy Cataract Limit (INR) Part of the sum insured Above 69 28,990 36,540 42,385
Exceeding 6 mths up to 7 mths 85% of the total premium received per policy year - 40,000 per policy
Exceeding 7 mths up to 9 mths 100% of the total premium received Free Look Period year - 60,000 Section II : Lump sum cover for Cancer (Optional Cover)
Exceeding 9 mths up to 10 mths 85% of the total premium received The Free Look Period shall be applicable on new individual health insurance policies and not on renewals or at the time
of porting/migrating the policy. Premium Per Year (in Rs.)
Exceeding 10 mths 100% of the total premium received Emergency Road Ambulance Covered Part of the sum insured
The insured person shall be allowed free look period of fifteen days from date of receipt of the policy document to Age Band /
Notwithstanding anything contained herein or otherwise, no refunds of premium shall be made in respect of review the terms and conditions of the policy, and to return the same if not acceptable. 2,50,000 3,75,000 5,00,000
Pre Hospitalization Expenses 30 days Part of the sum insured Sum Insured (Rs.)
Cancellation where, any claim has been admitted or has been lodged or any benefit has been availed by the insured lf the insured has not made any claim during the Free Look Period, the insured shall be entitled to;
person under the policy. i. a refund of the premium paid less any expenses incurred by the Company on medical examination of the insured 60 days (up to 2% of the basic 5m-29 10,135 15,200 20,265
ii. The Company may cancel the policy at any time on grounds of misrepresentation non-disclosure of material person and the stamp duty charges or Post Hospitalization Expenses Part of the sum insured
sum insured per hospitalization)
facts, fraud by the insured person by giving 15 days' written notice. There would be no refund of premium on 30-39 10,135 15,200 20,265
ii. where the risk has already commenced and the option of return of the policy is exercised by the insured person, a
cancellation on grounds of misrepresentation, non-disclosure of material facts or fraud deduction towards the proportionate risk premium for period of cover or Health Check-Up
40-49 10,135 15,200 20,265
(available for every claim 2,500/- 2,500/- 2,500/- In addition to the sum insured
Automatic Expiry iii. where only a part of the insurance coverage has commenced, such proportionate premium commensurate with
free year) 50-59 10,135 15,200 20,265
the insurance coverage during such period;
The insurance under this policy with respect to each relevant Insured Person policy shall expire immediately on the
earlier of the following events: Enhancement of Sum insured Medical Second Opinion Available - 60-69 10,135 15,200 20,265
i. Upon the death of the Insured Person. Sum insured once opted cannot be enhanced even on renewal.
5% for every claim free year maximum Above 69 10,135 15,200 20,265
ii. Upon exhaustion of the Basic sum insured plus bonus under the policy. No Claim Bonus -
Withdrawal of the policy up to 50%
Migration i. In the likelihood of this product being withdrawn in future, the Company will intimate the insured person about the
The insured person will have the option to migrate the policy to other health insurance products/plans offered by the Diet and Nutrition Program, Weight The information provided in this brochure is only indicative. For more details on the risk factors, terms and
same 90 days prior to expiry of the policy.
company by applying for migration of the Policy atleast 30 days before the policy renewal date as per IRDAI Management programme and Specialist conditions, please read the policy wordings before concluding a sale.
ii. lnsured Person will have the option to migrate to similar health insurance product available with the Company at Wellness Services -
guidelines on Migration. lf such person is presently covered and has been continuously covered without any lapses Consultation available through
the time of renewal with all the accrued continuity benefits such as cumulative bonus, waiver of waiting period. as Or
Star Tele-Health App
under any health insurance product/plan offered by the company, the insured person will get the accrued continuity per IRDAI guidelines, provided the policy has been maintained without a break. Visit Website: www.starhealth.in
benefits in waiting periods as per IRDAI guidelines on migration. Rehabilitation &
The Company Covered up to 10% of the Sum Insured Part of the sum insured
For Detailed Guidelines on migration, kindly refer the link Pain management
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.aspx?page=PageNo3987 Star Health and Allied Insurance Co. Ltd., commenced its operations in 2006 as India's first Standalone Health
Insurance provider. As an exclusive Health Insurer, the Company is providing sterling services in Health, Personal Modern Treatments Covered (up to the sub-limits) Part of the sum insured
Portability Accident & Overseas Travel Insurance and is committed to setting international benchmarks in service and personal
The insured person will have the option to port the policy to other insurers by applying to such insurer to port the caring.
Hospice Care Up to 20% of the Basic Sum Insured in life time Part of the sum insured
entire policy along with all the members of the family, if any, at least 45 days before, but not earlier than 60 days from
Star Advantages
the policy renewal date as per IRDAI guidelines related to portability. lf such person is presently covered and has
been continuously covered without any lapses under any health insurance policy with an lndian General/Health · No Third Party Administrator, direct in-house claims settlement Optional Cover
insurer, the proposed insured person will get the accrued continuity benefits in waiting periods as per IRDAI · Faster and hassle – free claim settlement
guidelines on portability. · Cashless hospitalization
For Detailed Guidelines on portability, kindly refer the link Lump-sum benefit for Cancer
Buy this insurance (INR in Lac) 2.5 3.75 5 - IRDAI IS NOT INVOLVED IN ACTIVITIES LIKE SELLING INSURANCE POLICIES,
https://www.irdai.gov.in/ADMINCMS/cms/frmGuidelines_Layout.aspx?page=PageNo3987
ANNOUNCING BONUS OR INVESTMENT OF PREMIUMS. PUBLIC RECEIVING
Insurance is the subject matter of solicitation
Please contact our nearest Branch Office /our Agent or visit our website www.starhealth.in for online purchase (Waiting period 30 months)
Renewal SUCH PHONE CALLS ARE REQUESTED TO LODGE A POLICE COMPLAINT
The policy shall ordinarily be renewable except on grounds of fraud, misrepresentation by the Insured Person; Tax Benefits
i. The Company shall endeavor to give notice for renewal. However, the Company is not under obligation to give Payment of premium by any mode other than cash for this insurance is eligible for relief under Section 80D of the Waiting Period
any notice for renewal Income Tax Act 1961. Star Cancer Care Platinum Insurance Policy
ii. Renewal shall not be denied on the ground that the insured person had made a claim or claims in the Initial waiting period 30 days (except for Accidents) - Unique Identification No.: SHAHLIP22031V022122
Prohibition of Rebates
BRO / SCCP/ V.2 / 2022
preceding policy years
Section 41 of Insurance Act 1938 (Prohibition of rebates): No person shall allow or offer to allow, either directly or
iii. Request for renewal along with requisite premium shall be received by the Company before the end of the indirectly, as an inducement to any person to take out or renew or continue an insurance in respect of any kind of risk For specific diseases 24 months -
policy period Buy this Insurance Online at www.starhealth.in
relating to lives or property in India, any rebate of the whole or part of the commission payable or any rebate of the For Pre-Existing diseases Call Toll-free: 1800-425-2255 / 1800-102-4477,
iv. At the end of the policy period, the policy shall terminate and can be renewed within the Grace Period of 30 premium shown on the policy, nor shall any person taking out or renewing or continuing a policy accept any rebate, 30 months -
days to maintain continuity of benefits without break in policy. Coverage is not available during the grace (including Cancer) sms STAR to 56677 « Fax Toll Free No: 1800-425-5522
except such rebate as may be allowed in accordance with the published prospectuses or tables of the insurer: Any
period person making default in complying with the provisions of this section shall be liable for a penalty which may extend to For Hospice Care 12 months - Email : support@starhealth.in
v. No loading shall apply on renewals based on individual claims experience ten lakhs rupees. CIN : L66010TN2005PLC056649 « IRDAI Regn. No: 129
6 7 8
You might also like
- Internship Project Report Shriram Life InsuranceDocument57 pagesInternship Project Report Shriram Life InsuranceAKSHIT VERMA100% (2)
- Your Insurance Cards: FusionDocument4 pagesYour Insurance Cards: FusionDawn Lamb UmikerNo ratings yet
- Premium Chart Excluding Tax Schedule of BenefitsDocument10 pagesPremium Chart Excluding Tax Schedule of BenefitsPrashant kiniNo ratings yet
- Star Cardiac Care Brochure PlatinumDocument8 pagesStar Cardiac Care Brochure PlatinumyankiNo ratings yet
- STAR HEALTH - Senior-Citizen-Red-Carpet-BrochureDocument7 pagesSTAR HEALTH - Senior-Citizen-Red-Carpet-BrochureTam AwNo ratings yet
- Senior Citizen Red Carpet BrochureDocument7 pagesSenior Citizen Red Carpet Brochureprasad_vjtiNo ratings yet
- Family Health Optima Insurance Plan NewDocument13 pagesFamily Health Optima Insurance Plan NewgmaniNo ratings yet
- Senior Citizen Red Carpet BrochureDocument7 pagesSenior Citizen Red Carpet BrochureMadhu Gowda HRNo ratings yet
- Star Cardiac Care Brochure PlatinumDocument8 pagesStar Cardiac Care Brochure PlatinumAbhishek GuptaNo ratings yet
- Women Care Insurance Policy BrochureDocument14 pagesWomen Care Insurance Policy Brochuresanjay4u4allNo ratings yet
- Women Care Insurance Policy BrochureDocument14 pagesWomen Care Insurance Policy BrochureD T K & CO.No ratings yet
- Women Care Insurance Policy BrochureDocument14 pagesWomen Care Insurance Policy BrochureRohit ChekuriNo ratings yet
- Women Care BrochureDocument14 pagesWomen Care BrochurelovingbabiluNo ratings yet
- Senior Citizen Red Carpet BrochureDocument7 pagesSenior Citizen Red Carpet BrochureMujaffar ShaikhNo ratings yet
- Women Care Insurance Policy BrochureDocument14 pagesWomen Care Insurance Policy Brochuremishradeepak99662No ratings yet
- Brochure Star Women Care Insurance Policy V 5 Web 10 1f319a50baDocument14 pagesBrochure Star Women Care Insurance Policy V 5 Web 10 1f319a50baRupayan DuttaNo ratings yet
- Super Surplus IndividualDocument12 pagesSuper Surplus IndividualsrivennelaassociatesNo ratings yet
- Diabetes Safe BrochureDocument9 pagesDiabetes Safe Brochurepsivakumar menakamillsNo ratings yet
- Your Health Is Our Mission: Mediclassic Insurance Policy (Individual)Document11 pagesYour Health Is Our Mission: Mediclassic Insurance Policy (Individual)deepakNo ratings yet
- Personalized Proposal For Securing Your Goals: FatherDocument7 pagesPersonalized Proposal For Securing Your Goals: FatherAbcNo ratings yet
- GUARANTEEDPENSIONPLANDocument2 pagesGUARANTEEDPENSIONPLANSatyajeet AnandNo ratings yet
- Affordable Health Cover For The Entire Family: Premium Rating in Rs. Excluding TaxDocument5 pagesAffordable Health Cover For The Entire Family: Premium Rating in Rs. Excluding TaxSIMON DSOUZANo ratings yet
- Health Premier Insurance Policy BrochureDocument14 pagesHealth Premier Insurance Policy BrochurePulokesh GhoshNo ratings yet
- Star Super Surplus Floater BrochureDocument18 pagesStar Super Surplus Floater BrochureDinu MrcogNo ratings yet
- Super Surplus Insurance PolicyDocument12 pagesSuper Surplus Insurance PolicyashuriyaNo ratings yet
- Star Critical Illness Multipay Insurance BrochureDocument7 pagesStar Critical Illness Multipay Insurance Brochuresanjay4u4allNo ratings yet
- Brochure Young Star Insurance PolicyDocument15 pagesBrochure Young Star Insurance PolicyANIMESH NEOGNo ratings yet
- Brochure Young Star Insurance PolicyDocument15 pagesBrochure Young Star Insurance PolicyahcharyaNo ratings yet
- Brochure Young Star Insurance PolicyDocument15 pagesBrochure Young Star Insurance PolicyMohan MaheshwarINo ratings yet
- Brochure Young Star Insurance PolicyDocument15 pagesBrochure Young Star Insurance PolicyPrithvi DistributorsNo ratings yet
- Brochure Young Star Insurance PolicyDocument15 pagesBrochure Young Star Insurance PolicyAbhishek ANo ratings yet
- Health Premier Insurance Policy BrochureDocument14 pagesHealth Premier Insurance Policy BrochureMUKUL JANGIDNo ratings yet
- KFD New29112023095424701 UW3Document8 pagesKFD New29112023095424701 UW3Mayur NagdiveNo ratings yet
- Diabetes Safe BrochureDocument8 pagesDiabetes Safe Brochureshobana dineshNo ratings yet
- Saral Suraksha Bima BrochureDocument6 pagesSaral Suraksha Bima Brochurehlasdu sdhNo ratings yet
- Candidate 1Document2 pagesCandidate 1Fascino WhiteNo ratings yet
- LifeStage Assure - LeafletDocument2 pagesLifeStage Assure - Leafletvincent cervoniNo ratings yet
- Corona Rakshak Insurance BrochureDocument4 pagesCorona Rakshak Insurance BrochureAlvin SangmaNo ratings yet
- Term Life Insurance - Compare & Buy Life Insurance OnlineDocument2 pagesTerm Life Insurance - Compare & Buy Life Insurance Onlineabinash771315No ratings yet
- Senior Citizen Red Carpet BrochureDocument7 pagesSenior Citizen Red Carpet BrochureAnish PradeepNo ratings yet
- Diabetes Safe BrochureDocument13 pagesDiabetes Safe BrochureNaga RajanNo ratings yet
- Activ Health Platinum Z FoldDocument2 pagesActiv Health Platinum Z FoldVARUNNo ratings yet
- SMART PLAN SAVINGS T AND CsDocument4 pagesSMART PLAN SAVINGS T AND CsemmanuelNo ratings yet
- Bharti Axa Life Monthly Income Plan +: Toll Free Helpline: 1800-22-6465 WWW - Bluechipindia.co - inDocument6 pagesBharti Axa Life Monthly Income Plan +: Toll Free Helpline: 1800-22-6465 WWW - Bluechipindia.co - inOnline YogeshNo ratings yet
- Os19611729 EbiDocument4 pagesOs19611729 EbiSoumya SwainNo ratings yet
- KFD New E36Document6 pagesKFD New E36vishalNo ratings yet
- Features of ICICI Pru Signature: How Does This Plan Work?Document6 pagesFeatures of ICICI Pru Signature: How Does This Plan Work?Sneha Abhash SinghNo ratings yet
- Icici Lakshya - 10kDocument5 pagesIcici Lakshya - 10kManjunath RNo ratings yet
- General Rules & Regulations: 1. Sum InsuredDocument19 pagesGeneral Rules & Regulations: 1. Sum InsuredYogesh KhemaniNo ratings yet
- Features of ICICI Pru1 Wealth: How Does This Plan Work?Document5 pagesFeatures of ICICI Pru1 Wealth: How Does This Plan Work?rajinigopi1906No ratings yet
- Star Cancer Care Gold BrochureDocument5 pagesStar Cancer Care Gold Brochuresanjay4u4all100% (1)
- Annexure 3 Compensation FeeDocument3 pagesAnnexure 3 Compensation FeeTech TipsNo ratings yet
- Smart Platinum 2lacDocument8 pagesSmart Platinum 2lacRajkumaar UtcNo ratings yet
- Surrender Retention Form New VV - 240517 - 130434Document3 pagesSurrender Retention Form New VV - 240517 - 130434naveen naveenNo ratings yet
- SmartSampoornaRaksha BrochureDocument16 pagesSmartSampoornaRaksha BrochureSuraj DubeyNo ratings yet
- Policy Details ChangeDocument1 pagePolicy Details ChangeKim Espart CastilloNo ratings yet
- 302 InsuranceDocument15 pages302 InsuranceManoj PundirNo ratings yet
- Job Offer-CEC-Relationship Manager-VRM-BRANCH BANKING-VRMDocument3 pagesJob Offer-CEC-Relationship Manager-VRM-BRANCH BANKING-VRMDnyanada NarvekarNo ratings yet
- Job Offer-Management Trainee-CONSTRUCTION EQUIPMENT (CE) - Marketing Branches OperationsDocument3 pagesJob Offer-Management Trainee-CONSTRUCTION EQUIPMENT (CE) - Marketing Branches Operationsaditi guliaNo ratings yet
- Circular No 089-2020Document12 pagesCircular No 089-2020Tan KSNo ratings yet
- AMENDMENTDocument1 pageAMENDMENTjohn paul manaloNo ratings yet
- Financial Model of ManufakturaDocument25 pagesFinancial Model of ManufakturaAravind MadhusudhananNo ratings yet
- Hon'Ble Mr. Justice Shantanu S. Kemkar, President Hon'Ble Mr. Shyam Sunder Bansal, Member Hon'Ble Mr. Prabhat Parashar, MemberDocument9 pagesHon'Ble Mr. Justice Shantanu S. Kemkar, President Hon'Ble Mr. Shyam Sunder Bansal, Member Hon'Ble Mr. Prabhat Parashar, MemberAnand ShahaniNo ratings yet
- Bobby & BettyDocument6 pagesBobby & BettySimon KingNo ratings yet
- Customer Guide Cover: Policy RulesDocument19 pagesCustomer Guide Cover: Policy RulesBertrandNo ratings yet
- Car Auto Repair Research QuestionsDocument5 pagesCar Auto Repair Research QuestionsFatima SethiNo ratings yet
- INSURANCEDocument7 pagesINSURANCELarah BuhaweNo ratings yet
- Summer Training CertificateDocument1 pageSummer Training CertificateuditasinhaNo ratings yet
- 06 Aufenthaltsbewilligung Student-Erklaerung en 20190823Document10 pages06 Aufenthaltsbewilligung Student-Erklaerung en 20190823Omar AliNo ratings yet
- Brochures Business Guard Commercial Package Policy f1619bfbd6Document2 pagesBrochures Business Guard Commercial Package Policy f1619bfbd6HARMAN SINGHNo ratings yet
- ZMP19278 - Fragata Uniao - Mil-Tek 102HD PDFDocument6 pagesZMP19278 - Fragata Uniao - Mil-Tek 102HD PDFLeandro_BarjonasNo ratings yet
- Lecture 11 - Business Interruption Insurance and BCPDocument24 pagesLecture 11 - Business Interruption Insurance and BCPnatasha muunganirwaNo ratings yet
- Investment AvenuesDocument37 pagesInvestment AvenuesSri HarshaNo ratings yet
- Dallas City Attorney Memo On IndemnificationDocument8 pagesDallas City Attorney Memo On IndemnificationTristan HallmanNo ratings yet
- ICICI - Claim FormDocument5 pagesICICI - Claim FormRaja RamanNo ratings yet
- IFRS 17 Insurance Contracts Why Annual Cohorts 1588124015Document6 pagesIFRS 17 Insurance Contracts Why Annual Cohorts 1588124015Grace MoraesNo ratings yet
- Insurance Case Digest Gaisano CagayanDocument3 pagesInsurance Case Digest Gaisano Cagayandempearl2315No ratings yet
- Site Security Service StateDocument2 pagesSite Security Service StateDesire KouadioNo ratings yet
- Insurance Financial and Actuarial AnalysisDocument12 pagesInsurance Financial and Actuarial AnalysisKamal UddinNo ratings yet
- Acme Billing Agreement TemplateDocument4 pagesAcme Billing Agreement TemplateSiddhant SinghNo ratings yet
- Traveleasy LTD Management Accounts Profit and Loss StatementDocument5 pagesTraveleasy LTD Management Accounts Profit and Loss StatementSitakanta AcharyaNo ratings yet
- IDBI Federal AR 2019-20 FINAL FILE PDFDocument220 pagesIDBI Federal AR 2019-20 FINAL FILE PDFpramod_kmr73No ratings yet
- A Project On Insurance and Pension: by KuldeepDocument26 pagesA Project On Insurance and Pension: by KuldeepdhimankuldeepNo ratings yet
- Wesco Financial Corporation: Letter To Shareholders To Our ShareholdersDocument8 pagesWesco Financial Corporation: Letter To Shareholders To Our ShareholdersChidananda SahuNo ratings yet
- Individual Report - How Is Takaful Different From Other Insurance - (Nor Khairiyatul Wafa Binti Rosdi)Document10 pagesIndividual Report - How Is Takaful Different From Other Insurance - (Nor Khairiyatul Wafa Binti Rosdi)Nor KhairiyatulNo ratings yet
- Wica Guide 2020Document40 pagesWica Guide 2020Arthur LimNo ratings yet
- 1today Is WednesdayDocument26 pages1today Is WednesdayGabriel EmersonNo ratings yet
- Linda Mckeon: Your Offer of A PlaceDocument7 pagesLinda Mckeon: Your Offer of A Placefashionmk05No ratings yet
- Cigna SmartCare Helpful GuideDocument42 pagesCigna SmartCare Helpful GuideFasihNo ratings yet