Professional Documents
Culture Documents
Panoramic Radiographs Made Before Complete Removable Dental Prostheses Fabrication A Retrospective Study of Clinical Significance
Panoramic Radiographs Made Before Complete Removable Dental Prostheses Fabrication A Retrospective Study of Clinical Significance
Uploaded by
01 X A.A. Gede Reynata Putra XII MIPA 4Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Panoramic Radiographs Made Before Complete Removable Dental Prostheses Fabrication A Retrospective Study of Clinical Significance
Panoramic Radiographs Made Before Complete Removable Dental Prostheses Fabrication A Retrospective Study of Clinical Significance
Uploaded by
01 X A.A. Gede Reynata Putra XII MIPA 4Copyright:
Available Formats
Cornelini.
qxd 11/17/06 3:00 PM Page 914
Immediate Loading of Implants with 3-unit Fixed
Partial Dentures: A 12-month Clinical Study
Roberto Cornelini, MD, DDS1/Filippo Cangini, DDS, MS2/Ugo Covani, MD, DDS3/
Antonio Barone, DDS, PhD4/Daniel Buser, Prof Dr Med Dent5
Purpose: The aim of the present clinical trial was to evaluate the 12-month success rate of titanium
dental implants placed in the posterior mandible and immediately loaded with 3-unit fixed partial den-
tures. Materials and Methods: Patients with missing mandibular premolars and molars were enrolled
in this study. To be included in the study, the implants had to show good primary stability. Implant sta-
bility was measured with resonance frequency analysis using the Osstell device (Integration Diagnos-
tics). Implants were included in the study when the stability quotient (ISQ) exceeded 62. Clinical mea-
surements, such as width of keratinized tissue, ISQ, and radiographic assessment of peri-implant bone
crest levels, were performed at baseline and at the 12-month follow-up. The comparison between the
baseline and the 12-month visits was performed with the Student t test for paired data (statistically
significant at a level of ␣ = 0.05). Results: Forty implants with a sandblasted, large grit, acid-etched
(SLA) surface (Straumann) were placed in 20 patients. At 12 months, only 1 implant had been lost
because of an acute infection. The remaining 39 implants were successful, resulting in a 1-year suc-
cess rate of 97.5%. Neither peri-implant bone levels, measured radiographically, nor implant stability
changed significantly from baseline to the 12-month follow-up (P > .05). Discussion: The immediate
functional loading of implants placed in this case series study resulted in a satisfactory success rate.
Conclusion: The findings from this clinical study showed that the placement of SLA transmucosal
implants in the mandibular area and their immediate loading with 3-unit fixed partial dentures may be
a safe and successful procedure. (Case Series) INT J ORAL MAXILLOFAC IMPLANTS 2006;21:914–918
Key words: immediate loading, partial edentulism, radiologic examinations, success rates
itanium dental implants have been successfully studies have reported high success rates with non-
T used to restore completely and partially edentu-
lous patients over the past 30 years.1,2 The original
submerged titanium implants.5,6 In the last decade,
advances in implant surface technology and continu-
surgical protocol required the implants to remain sub- ous clinical research have provided clinicians with
merged for a healing period of 3 to 6 months. The clinical procedures to address more demanding clini-
healing period, which was associated with avoidance cal situations. Some of the original prerequisites for
of functional loading, was considered necessary to osseointegration have been reassessed to satisfy
achieve osseointegration.3,4 Over the years, several patient demand for reduced treatment time,
improved esthetic outcomes, and increased comfort
1Assistant during healing. New treatment concepts such as
Professor, University of Genoa, Italy; Private Practice,
Rimini, Italy. immediate implant loading (ie, occlusal loading
2Research Assistant, Department of Oral Biology, State University within 24 hours of implant placement) and early
of New York at Buffalo; Private Practice, Rimini, Italy. implant loading (occlusal loading 6 to 8 weeks after
3Associate Professor, Department of Biophysical, Medical and
implant placement) have been proposed to shorten
Odontostomatological Sciences and Technologies, Medical
the overall treatment time and to allow the patient to
School, University of Genova, Italy.
4Assistant Professor, Department of Biophysical, Medical and receive a fixed implant-supported prosthesis in the
Odontostomatological Sciences and Technologies, Medical shortest time possible after implant placement.7,8
School, University of Genova, Italy. The aim of the present clinical study was to evalu-
5Professor, Department of Oral Surgery and Stomatology, Univer-
ate the 12-month implant success rate of immedi-
sity of Bern, School of Dental Medicine, Bern, Switzerland.
ately loaded titanium dental implants in the poste-
Correspondence to: Dott. Roberto Cornelini, Piazza 3, Martiri 38, rior mandible used to support 3-unit fixed partial
Rimini, Italy. Fax: +39 0541 433386. E-mail: rcornel@libero.it dentures.
914 Volume 21, Number 6, 2006
COPYRIGHT © 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Cornelini.qxd 11/17/06 3:00 PM Page 915
Cornelini et al
Fig 1 (left) Periapical radiograph obtained
at the time of immediate prosthetic restora-
tion (baseline) in a standardized manner.
Fig 2 (right) Radiograph taken 12 months
following implant placement.
MATERIALS AND METHODS tions. All implants were clinically stable, and the implant
stability was confirmed with the resonance frequency
All the patients were recruited to the study based on analysis (RFA) measurements (Integration Diagnostics,
their need for the restoration of multiple missing Göteborg, Sweden). The Osstell device was used
mandibular posterior teeth (premolars or molars). according to the manufacturer’s recommendations.10,11
Natural teeth adjacent to the area to be restored
were required to have a complete occlusal surface Prosthetic Protocol
and be free from periodontal or endodontic infec- Immediately following implant placement, while the
tion. Additional criteria to enter the study were suffi- patient still under anesthesia, the initial restorative
cient bone quantity (bone height and width) to allow treatment was begun. Two screw-retained transfer
the placement of implants with a diameter of 4.1 mm copings were connected to the implants. Wound clo-
and a length of at least 12 mm or a diameter of 4.8 sure was achieved by suture. Subsequently, an
mm and a length of at least 10 mm, an implant stabil- impression was taken in a customized impression
ity quotient (ISQ) exceeding 62, an occlusal pattern tray. Healing caps were then placed on the implants.
that allowed for bilateral stability, and a signed writ- Within 24 hours of implant placement, a temporary
ten consent form. Exclusion criteria included general screw-retained acrylic resin 3-unit fixed partial den-
health conditions that would jeopardize the bone ture was connected to the implants. Following incor-
healing process (eg, diabetes, osteoporosis, blood dis- poration of the provisional restoration, an individual-
orders), severe maxillomandibular space discrepan- ized acrylic resin template was fabricated for each
cies, parafunctional habits (bruxism or clenching), patient to guarantee radiographic reproducibility for
drug or alcohol abuse, poor oral hygiene, and local the follow-up period. The temporary acrylic resin
peri-implant bone defects requiring simultaneous crown restorations were designed to be placed in
bone augmentation procedures during surgery. occlusal contact. All patients were prescribed 1 g
All patients were referred to a restorative dentist amoxicillin (amoxicillin, Merck Generics, Milan, Italy)
for a complete presurgical evaluation, including twice daily for 5 days and 200 mg ibuprofen (Busco-
waxup and the fabrication of a surgical template. pan, Milan, Italy) as needed. Patients were instructed
Each clinical case was evaluated by examining diag- to rinse twice daily with a chlorhexidine mouthwash
nostic casts for the maxillomandibular relationship, (Eburos; Dentsply, Rome, Italy) twice daily for the fol-
periapical and panoramic radiographs, and comput- lowing 2 weeks. The sutures were removed 7 to 10
erized tomographic scans if needed. days after surgery.
The final implant impression was obtained after 6
Surgical Protocol months. The definitive abutments were connected to
The implants were placed with an atraumatic surgical the implants, and lastly, the definitive metal-ceramic
technique.9 All surgical procedures were performed restoration was cemented.
with the aid of a custom-made template. Every effort
was made to maintain parallelism between the Follow-up Evaluation
implants and the remaining dentition. Standard Strau- All patients were placed on a strict follow-up regi-
mann (4.1 mm wide) or wide-body implants (4.8 mm men until soft tissue healing was complete. The fol-
wide) (Straumann, Waldenburg, Switzerland) with a lowing clinical parameters were evaluated at the
sandblasted, large grit, acid-etched (SLA) surface were time of implant placement (baseline) and at the 12-
placed according to the manufacturer’s recommenda- month follow-up:
The International Journal of Oral & Maxillofacial Implants 915
COPYRIGHT © 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Cornelini.qxd 11/17/06 3:00 PM Page 916
Cornelini et al
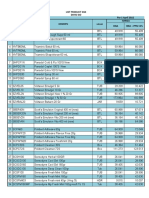
Table 1 Implant Positions and Dimensions Table 2 Changes of Clinical and Radiographic
(n = 40) Parameters Between Baseline and 12-month
Follow-up
Implant position
Implant size
Baseline 12 months
width ⫻ length Premolar (20) Molar (20) Total
Mean SD Mean SD P
4.1 ⫻ 12 mm 16 6 22
4.8 ⫻ 10 mm 3 8 11 DIB
4.8 ⫻ 12 mm 1 6 7 Mesial 2.4 0.4 2.5 0.4 NS
Distal 2.6 0.6 3.1 0.6 NS
Width of keratinized mucosa
Midbuccal 2.0 0.5 2.0 0.5 NS
Midlingual 2.4 0.5 2.2 0.6 NS
ISQ 72.0 5.7 74.5 7.3 NS
• Distance between the implant shoulder and the tion, and all maintained stability. At the 12-month
point of bone-to-implant contact (DIB) mesially examination, 39 implants fulfilled the success criteria
and distally to the implant on periapical radio- proposed by Buser and associates,13 resulting in a
graphs taken in a standardized manner6,12 (Figs 1 short-term success rate of 97.5%.
and 2) Clinical and radiographic parameters such DIB,
• Width of keratinized mucosa at the midbuccal width of keratinized mucosa, and ISQ value (reso-
and midlingual aspects nance frequency analysis) are presented in Table 2.
• Implant stability (ISQ)10,11 A comparison of values of DIB, keratinized mucosa
width, and ISQ at baseline and at the 12-month fol-
Data Analysis low-up is shown in Table 2. No statistically significant
Clinical measurements of the 40 implants were cal- differences were found for the parameters measured.
culated for each patient by averaging the readings of All the patients reported that the temporary restora-
each clinical parameter for the implants for each tion was esthetically acceptable. No technical com-
patient, since the intrasubject variation was much plications such as screw loosening, resin fracture, or
lower than the intersubject variation. Subsequently, pain during chewing were registered during the
the means and medians were calculated among the observation period.
means per patient at baseline and 12 months. The
comparison between baseline and 12-month data
was performed with the Student t test for paired DISCUSSION
data and was considered statistically significant at
the ␣ = .05 level. Immediate loading of dental implants offers several
advantages to both the clinician and the patient,
such as reduced number of appointments, reduced
RESULTS healing time, elimination of the need for removable
temporary dentures during healing, and above all
A total of 20 patients (11 men and 9 women) with an increased comfort for the patient with immediate
age ranging from 27 to 59 years (mean, 47.2 years) fixed restorations. The compatibility of immediate
were included in this study. Six patients were smok- and early loading with implant osseointegration and
ers and 14 were nonsmokers. A total of 40 dental long-term success has been investigated in ani-
implants were placed and immediately loaded to mal14–16 and human studies17–19 with positive but
support 20 short-span, 3-unit fixed partial dentures. sometimes controversial results.
Implant positions and dimensions are reported in Deporter and coworkers14 loaded conical cylinder
Table 1. All the implants were free of complications implants immediately after placement; after 4 weeks,
during the healing phase. During the follow-up bone ingrowth without fibrous encapsulation had
period of 12 months, 1 implant was removed 2 reached a certain level, but no further increase was
months after placement because of an acute infec- observed between 4 and 8 weeks. In a histologic
tion at the implant site. The failing implant was study in monkeys, Piattelli and colleagues16 com-
immediately replaced with a new implant, which was pared the amount of bone apposition around screw-
subsequently successful. Throughout the follow-up type implants loaded after 30 days with nonloaded
period of 12 months, none of the 39 remaining implants and reported similar amounts and patterns
implants demonstrated signs of peri-implant infec- of bone apposition. Chiapasco and Gatti18 recently
916 Volume 21, Number 6, 2006
COPYRIGHT © 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Cornelini.qxd 11/17/06 3:00 PM Page 917
Cornelini et al
published a prospective study on 82 patients with In the present study, all implants were placed in the
edentulous mandibles rehabilitated with implant- posterior area of the mandible to replace premolars
supported overdentures delivered immediately after or molars. To evaluate the primary stability of
implant placement. Three hundred twenty-eight implants, resonance frequency analysis was per-
screw-type implants (4 implants per patient) were formed with the Osstell device. This non-invasive,
placed in the interforaminal area of the mental sym- objective, reliable method allows the clinician to mea-
physis. Of 328 implants placed, 296 were followed to sure the primary stability of implants at the time of
62 months. Seven implants were removed; another placement and the continuing stability of the
18 integrated but did not fulfill the success criteria. implants during the different stages of healing.10,11 It
The cumulative sur vival and success rates of has been demonstrated that RFA values are consistent
implants were 96.1% and 88.2%, respectively. with other measurements of primary stability, such as
Glauser and associates20 placed 104 Brånemark manual assessment10 and “true cutting resistance.”29
System MkIV TiUnite implants which were immediate The present study confirmed that transmucosal
occlusally loaded in 38 patients. Of these, 20 were sin- dental implants with good primary stability mea-
gle-tooth restorations, 30 were fixed partial dentures, sured according to the RFA principles can be success-
and 1 was a complete fixed mandibular restoration. fully loaded to support 3-unit dental prostheses. Fur-
The authors reported a cumulative implant success thermore, the immediately loaded implants showed
rate of 97.1% after 1 year of prosthetic loading. The stability of the marginal bone level.
mean marginal bone resorption after 1 year of load- Further clinical trials with larger sample sizes and
ing was 1.2 ± 0.9 mm. Cornelini and associates 21 longer follow-up periods are needed to demonstrate
placed 30 Straumann dental implants with a SLA sur- the long-term success of this clinical approach.
face in 30 patients with a missing mandibular molar
and immediately restored them. The implants were
included in the study only if the ISQ exceeded 62. At CONCLUSIONS
12 months, only 1 implant had been lost because of
acute infection. Radiographic as well as clinical exami- The results of the present short-term study showed
nation confirmed the clinical success of all remaining that immediate loading of dental implants placed in
implants, resulting in a 12-month success rate of the posterior area of the mandible that achieved pri-
96.7%. Interestingly, implant stability measured with mary stability at a minimum of 62 ISQ can be a suc-
RFA did not increase significantly from baseline to the cessful procedure, if strict inclusion criteria are
12-month follow-up (P > .05) in either that study or respected. This approach has the potential to
the present one. become a valuable alternative to the concept of early
The results of the studies reviewed should be implant loading.
interpreted with caution, since they vary widely with
respect to important determinants of implant suc-
cess such as inclusion/exclusion criteria for patient REFERENCES
selection, area of implant placement (maxilla versus
mandible), and loading protocol. 1. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-
term efficacy of currently used dental implants: A review and
The results of the present study indicated that
proposed criteria of success. Int J Oral Maxillofac Implants
immediate loading of dental implants with 3-unit 1986;1:11–25.
fixed partial dentures in the posterior mandible can 2. Makkonen TA, Holmberg S, Niemi L, Olsson C, Tammisalo T, Pel-
be a safe and predictable procedure. Only 1 implant tola J. A 5-year prospective clinical study of Astra Tech dental
was lost during the study period, whereas 39 of 40 implants supporting fixed bridges or overdentures in the
implants were clinically successful and met the suc- edentulous mandible. Clin Oral Implants Res 1997;8:469–475.
3. Brånemark P-I, Hansson BO, Adell R, et al. Osseointegrated
cess criteria. This resulted in an implant success rate implants in the treatment of the edentulous jaw: Experience
of 97.5% after 12 months of follow-up. The implant from a 10-year period. Scand Plast Reconstr Surg
failure caused prosthesis failure; consequently, the 1977;16(suppl 1):1–132.
prosthesis survival rate was 95%. 4. Adell R, Lekholm U, Rockler B, Brånemark P-I. A 15-year study
of osseointegrated implants in the treatment of the edentu-
These results are in accordance with other studies
lous jaw. Int J Oral Surg 1981;10:387–416.
on the use of immediately loaded implants to sup- 5. Babbush CA. Titanium plasma spray screw implant system for
por t overdentures in completely edentulous reconstruction of the edentulous mandible. Dent Clin North
patients 22–24 and the use of immediately loaded Am 1986;30:117–131.
implants to support single crowns for single tooth 6. Buser D, Weber HP, Bragger U, Balsiger C. Tissue integration of
one-stage ITI implants: 3-year results of a longitudinal study
replacement.25–28
with hollow-cylinder and hollow-screw implants. Int J Oral
Maxillofac Surg 1991;6:405–412.
The International Journal of Oral & Maxillofacial Implants 917
COPYRIGHT © 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Cornelini.qxd 11/17/06 3:00 PM Page 918
Cornelini et al
7. Schnitman PA, Wohrle PS, Rubenstein JE, Da Silva JD, Wang NH. 19. Balshi TJ, Wolfinger GJ. Immediate loading of Brånemark
Ten-year results from Brånemark implants immediately implants in edentulous mandibles: A preliminary report.
loaded with fixed prostheses at implant placement. Int J Oral Implant Dent 1997;6:83–88.
Maxillofac Implants 1997;12:495–503. 20. Glauser R, Lundgren AK, Gottlow J, et al. Immediate occlusal
8. Bornstein MM, Lussi A, Schmid B, Belser UC, Buser D. Early loading of Brånemark TiUnite implants placed predominantly
loading of titanium implants with a sandblasted and acid- in soft bone: 1-year results of a prospective clinical study. Clin
etched (SLA) surface: 3-year results of a prospective study in Implant Dent Relat Res 2003;5(suppl 1):47–56.
partially edentulous patients. Int J Oral Maxillofac Implants 21. Cornelini R, Cangini F, Covani U, Barone A, Buser D. Immediate
2003;18:659–666. restoration of single-tooth implants in mandibular molar sites:
9. Buser D, von Arx T. Surgical procedures in partially edentulous A 12-month preliminary report. Int J Oral Maxillofac Implants
patients with ITI implants. Clin Oral Implants Res 2004;19:855–860.
2000;11(suppl 1):83–100. 22. Randow K, Ericsson I, Nilner K, Petersson A, Glantz PO. Immedi-
10. Meredith N, Shagaldi F, Alleyne D, Sennerby L, Cawley P. The ate functional loading of Brånemark dental implants. A 18-
application of resonance frequency measurements to study month clinical follow-up study. Clin Oral Implants Res
the stability of titanium implants during healing in the rabbit 1999;10:8–15.
tibia. Clin Oral Implants Res 1997;8:234–243. 23. Ericsson I, Randow K, Nilner K, Peterson A. Early functional
11. Friberg B, Sennerby L, Meredith N, Lekholm U. Stability mea- loading of Brånemark dental implants: 5-year clinical follow-
surements of 1-stage Brånemark implants during healing in up study. Clin Implant Dent Relat Res 2000;2:70–77.
mandibles. A clinical resonance frequency analysis study. Int J 24. Ganeles J, Wismeijer D. Early and immediately restored and
Oral Maxillofac Surg 1999;28:266–272. loaded dental implants for single-tooth and partial-arch appli-
12. Weber HP, Buser D, Fiorellini JP, Williams RC. Radiographic eval- cations. Int J Oral Maxillofac Implants 2004;19:92–102.
uation of crestal bone levels adjacent to nonsubmerged tita- 25. Ericsson I, Nilson H, Lindh T, Nilner K, Randow K. Immediate
nium implants. Clin Oral Implants Res 1992;3:181–188. functional loading of Brånemark single-tooth implants. An 18
13. Buser D, Weber HP, Lang NP. Tissue integration of non-sub- months’ clinical pilot follow-up study. Clin Oral Implants Res
merged implants. 1 year results of a prospective study with 2000;11:26–33.
100 ITI hollow-cylinder and hollow-screw implants. Clin Oral 26. Calandriello R, Tomatis M, Vallone R, Rangert B, Gottlow J.
Implants Res 1990;1:33–40. Immediate occlusal loading of single lower molars using
14. Deporter DA, Watson PA, Pilliar RM, et al. A histological assess- Branemark System Wide-Platform TiUnite implants: An interim
ment of the initial healing response adjacent to porous Ti report of a prospective open-ended clinical multicenter study.
alloy dental implants in dogs. J Dent Res 1986;65:1064–1070. Clin Implant Dent Relat Res 2003;(5 suppl 1):74–80.
15. Hashimoto M, Akagawa Y, Hashimoto M, Nikai H, Tsuru H. Sin- 27. Malò P, Friberg B, Polizzi G, Gualini F, Vighagen T, Rangert B.
gle crystal sapphire endosseous implant loaded with func- Immediate and early function of Brånemark System implants
tional stress: A clinical and histological evaluation of peri- placed in the esthetic zone: A 1-year prospective clinical mul-
implant tissues. J Oral Rehabil 1988;15:65–76. ticenter study. Clin Implant Dent Relat Res 2003;5(suppl
16. Piattelli A, Ruggieri A, Franchi M, Romasco N, Trisi P. A histo- 1):37–46.
logic and histomorphometric study of bone reactions to 28. Glauser R, Ree A, Lundgren A, Gottlow J, Hammerle CH,
unloaded and loaded non-submerged single implants in Scharer P. Immediate occlusal loading of Brånemark implants
monkeys: A pilot study. J Oral Implantol 1993;19:314–320. applied in various jawbone regions: A prospective, 1-year clin-
17. Ledermann PD. Sechsjaehrige klinische Erfahrung mit dem ical study. Clin Implant Dent Relat Res 2001;3:204–213.
titanplasmabeschichteten ITI-Schraubenimlpantat in der 29. Friberg B, Sennerby L, Meredith N, Lekholm U. A comparison
Regio Interforaminalis des Unterkiefers. Schweiz Monatsschr between cutting torque and resonance frequency measure-
Zahnmed 1983;93:1070–1089. ments of maxillary implants. A 20-month clinical study. Int J
18. Chiapasco M, Gatti C, Rossi E, Haefliger W, Markwalder T. Oral Maxillofac Surg 1999;28:297–303.
Implant-retained mandibular overdentures with immediate
loading: Results on 226 consecutive cases. Clin Oral Implants
Res 1997;8:48–57.
918 Volume 21, Number 6, 2006
COPYRIGHT © 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
You might also like
- Twelve-Month Evaluation of A Novel Mineral-Organic Adhesive Material Used To Stabilize Dental Implants Placed in Oversized Osteotomies in Vivo in An Animal ModelDocument14 pagesTwelve-Month Evaluation of A Novel Mineral-Organic Adhesive Material Used To Stabilize Dental Implants Placed in Oversized Osteotomies in Vivo in An Animal ModelAlan PollackNo ratings yet
- Proposed Budget For ClinicDocument5 pagesProposed Budget For ClinicSarah Mae AventuradoNo ratings yet
- Immediate Loading Implants With Mandibular Overdenture: A 48-Month Prospective Follow-Up StudyDocument6 pagesImmediate Loading Implants With Mandibular Overdenture: A 48-Month Prospective Follow-Up StudySung Soon ChangNo ratings yet
- Single ToothReplacementintheAnteriorMaxillaDocument14 pagesSingle ToothReplacementintheAnteriorMaxillaSteffany BernalNo ratings yet
- Telescopic Crowns As Attachments For Implant Supported Restorations A Case SeriesDocument15 pagesTelescopic Crowns As Attachments For Implant Supported Restorations A Case SeriesmaxNo ratings yet
- Carga Inmediata Contra Tardia de Implantes Dentales en Alveolos Frescos Posextraccion en La Zona Estética Maxilar, Un Estudio Clínico ComparativoDocument6 pagesCarga Inmediata Contra Tardia de Implantes Dentales en Alveolos Frescos Posextraccion en La Zona Estética Maxilar, Un Estudio Clínico ComparativoKuro Aranda PlataNo ratings yet
- Koutouzisetal 2013IJOMIAbutmentdisconnectionClinicalDocument8 pagesKoutouzisetal 2013IJOMIAbutmentdisconnectionClinicalKyoko CPNo ratings yet
- A Prospective, Multi Center Study Assessing Early Loading With Short Implants in Posterior Regions. A 3 Year Post Loading Follow Up StudyDocument9 pagesA Prospective, Multi Center Study Assessing Early Loading With Short Implants in Posterior Regions. A 3 Year Post Loading Follow Up StudyBagis Emre GulNo ratings yet
- Immediate Versus Conventional Loading For The Maxilla With Implants Placed Into Fresh and Healed Extraction Sites To Support A Full-Arch Fixed Prosthesis - Nonrandomized Controlled Clinical StudyDocument9 pagesImmediate Versus Conventional Loading For The Maxilla With Implants Placed Into Fresh and Healed Extraction Sites To Support A Full-Arch Fixed Prosthesis - Nonrandomized Controlled Clinical StudySTEPHANIE JARAMILLONo ratings yet
- Arora2017 Implante Imediato Com RogDocument9 pagesArora2017 Implante Imediato Com RogAsafe RheinnickNo ratings yet
- SwithcingDocument6 pagesSwithcingKyoko CPNo ratings yet
- Mozzati 2013Document9 pagesMozzati 2013Larissa RodovalhoNo ratings yet
- Anitua 2016Document7 pagesAnitua 2016IsmaelNo ratings yet
- Immediate Early Loading of Dental Implants. Clinical Documentation and Presentation of A Treatment ConceptDocument23 pagesImmediate Early Loading of Dental Implants. Clinical Documentation and Presentation of A Treatment ConceptDr.SnehalNo ratings yet
- Jap 11 48Document7 pagesJap 11 48Zerelie MaudNo ratings yet
- A One Year Pilot Prospective Multicenter StudyDocument10 pagesA One Year Pilot Prospective Multicenter StudyEly Valentina Contreras ArceoNo ratings yet
- Two-Year Evaluation Oas A Variable-Thread Tapered Implant in Extration Sites. McAllister BS Et AlDocument9 pagesTwo-Year Evaluation Oas A Variable-Thread Tapered Implant in Extration Sites. McAllister BS Et AlDr. Rafael OrroNo ratings yet
- Weinstein 2010Document8 pagesWeinstein 2010gbaez.88No ratings yet
- Schropp Et Al (2005) Immediate Vs Delayed IJOMIDocument9 pagesSchropp Et Al (2005) Immediate Vs Delayed IJOMIAlla MushkeyNo ratings yet
- Schropp Et Al (2005) Immediate Vs Delayed IJOMI PDFDocument9 pagesSchropp Et Al (2005) Immediate Vs Delayed IJOMI PDFAlla MushkeyNo ratings yet
- Correlation Between Placement Torque and Survival of Single-Tooth ImplantsDocument8 pagesCorrelation Between Placement Torque and Survival of Single-Tooth ImplantssheetalNo ratings yet
- 1 s2.0 S0901502714003002 MainDocument9 pages1 s2.0 S0901502714003002 MainMariana RebolledoNo ratings yet
- Two Bilateral Zygomatic Implants Placed and Immediately Loaded A Retrospective Chart Review With Up-To-54-Month Follow-UpDocument5 pagesTwo Bilateral Zygomatic Implants Placed and Immediately Loaded A Retrospective Chart Review With Up-To-54-Month Follow-UpBagis Emre Gul100% (1)
- 10 1067@mpr 2000 107113Document7 pages10 1067@mpr 2000 107113gbaez.88No ratings yet
- 11 B - All On Four Group 01 PDFDocument3 pages11 B - All On Four Group 01 PDFLuis Humberto BorgesNo ratings yet
- 75665e2cfaaaed0e64dc65cd50181d6bDocument7 pages75665e2cfaaaed0e64dc65cd50181d6bNguyen Phuong HangNo ratings yet
- All-On-4 - Immediate-Function Concept ForDocument12 pagesAll-On-4 - Immediate-Function Concept ForAnsaquilo AnsaquiloNo ratings yet
- Agliardi - Immediate Fixed Rehabilitation ofDocument11 pagesAgliardi - Immediate Fixed Rehabilitation ofAnsaquilo AnsaquiloNo ratings yet
- Single Center Retrospective Analisys of 1001 Consecutevely Placed NobelActive Implants BABBUSH Et AlDocument8 pagesSingle Center Retrospective Analisys of 1001 Consecutevely Placed NobelActive Implants BABBUSH Et AlDr. Rafael OrroNo ratings yet
- Chenetal 2009aJOMIDocument33 pagesChenetal 2009aJOMI63127No ratings yet
- Evaluation of Alveolar Process Resorption After Tooth Extraction Using The Socket Shield Technique Without Immediate Installation of Implants: A Randomised Controlled Clinical TrialDocument6 pagesEvaluation of Alveolar Process Resorption After Tooth Extraction Using The Socket Shield Technique Without Immediate Installation of Implants: A Randomised Controlled Clinical TrialPedro PachecoNo ratings yet
- qt2059w9zd NosplashDocument8 pagesqt2059w9zd NosplashCrișu LauraNo ratings yet
- A Multilevel Analysis of Platform-Switching Flapless Implants Placed at Tissue Level: 4-Year Prospective Cohort StudyDocument13 pagesA Multilevel Analysis of Platform-Switching Flapless Implants Placed at Tissue Level: 4-Year Prospective Cohort Studyhkwgt7vskwNo ratings yet
- Primary Loading of Palatal Implants For Orthodontic Anchorage e A Pilot Animal StudyDocument7 pagesPrimary Loading of Palatal Implants For Orthodontic Anchorage e A Pilot Animal StudyPaola LoloNo ratings yet
- Thesis Copy 6 CorrectedDocument54 pagesThesis Copy 6 CorrectedanushiNo ratings yet
- Gallucci (2004) - Immediate Loading With Fixed Screw-Retained Provisional Restorations in Edentulous Jaws, The Pickup Technique.Document10 pagesGallucci (2004) - Immediate Loading With Fixed Screw-Retained Provisional Restorations in Edentulous Jaws, The Pickup Technique.Antonio González Ruiz0% (1)
- CLR 12021Document63 pagesCLR 12021Eliza DNNo ratings yet
- Implant Placement in Fresh Extraction Sockets: Juan Blanco - Cristina Carral - Olalla Argibay - Antonio LiñaresDocument17 pagesImplant Placement in Fresh Extraction Sockets: Juan Blanco - Cristina Carral - Olalla Argibay - Antonio LiñaresBagis Emre GulNo ratings yet
- Simultaneous Sinus Lift and Implant Placement Using Lateral Approach in Atrophic Posterior Maxilla With Residual Bone Height of 5 MM or Less. A Systematic ReviewDocument10 pagesSimultaneous Sinus Lift and Implant Placement Using Lateral Approach in Atrophic Posterior Maxilla With Residual Bone Height of 5 MM or Less. A Systematic ReviewBagis Emre GulNo ratings yet
- Oral & Maxillo ImplantsDocument12 pagesOral & Maxillo ImplantsImen MineneNo ratings yet
- Surgical Extrusion With An Atraumatic Extraction System: A Clinical StudyDocument7 pagesSurgical Extrusion With An Atraumatic Extraction System: A Clinical StudyFebri YolandaNo ratings yet
- 5 PDFDocument8 pages5 PDFoskar ORTIZNo ratings yet
- Rocci 2013Document5 pagesRocci 2013camilaNo ratings yet
- Socket Shield Technique Vs Conventional Immediate Implant Placement With Immediate Temporization. Randomized Clinical TrialDocument10 pagesSocket Shield Technique Vs Conventional Immediate Implant Placement With Immediate Temporization. Randomized Clinical TrialeveraldocruzNo ratings yet
- Outcome of Single Immediate Implants Placed inDocument8 pagesOutcome of Single Immediate Implants Placed injuanita enriquezNo ratings yet
- Abi Nader S, - Plaque Accumulation Beneath Maxillary All-On-4™ Implant-Supported ProsthesesDocument6 pagesAbi Nader S, - Plaque Accumulation Beneath Maxillary All-On-4™ Implant-Supported ProsthesesAnsaquilo AnsaquiloNo ratings yet
- ArticleDocument13 pagesArticlegfernandesNo ratings yet
- Tissue ManagementDocument16 pagesTissue ManagementSaleh AlsadiNo ratings yet
- Associated Short and Regular Implants For Complete Denture Retention in An Atrophic Mandible: Clinical Follow-UpDocument15 pagesAssociated Short and Regular Implants For Complete Denture Retention in An Atrophic Mandible: Clinical Follow-UpTarsila LopesNo ratings yet
- Cap 10087Document13 pagesCap 10087snkidNo ratings yet
- Implant Placement in Ridge SplitDocument10 pagesImplant Placement in Ridge SplitQuang Bui100% (1)
- Tent-Pole in Regeneration TechniqueDocument4 pagesTent-Pole in Regeneration TechniqueangelicapgarciacastilloNo ratings yet
- 1548 1336 (2004) 30 162:apvfii 2.0.co 2Document9 pages1548 1336 (2004) 30 162:apvfii 2.0.co 2Rajat GuptaNo ratings yet
- Furhauser 2017Document10 pagesFurhauser 2017jhon HanselNo ratings yet
- CroniconDocument9 pagesCroniconAhmed BadrNo ratings yet
- Long-termSurvival Rates of Implants Supporting OverdentureDocument5 pagesLong-termSurvival Rates of Implants Supporting OverdentureTao LinksNo ratings yet
- Krebs Et Al-2015-Clinical Implant Dentistry and Related ResearchDocument12 pagesKrebs Et Al-2015-Clinical Implant Dentistry and Related ResearchthganooNo ratings yet
- Cid 13008Document10 pagesCid 13008snkidNo ratings yet
- Practice-Based Clinical Evaluation of Zirconia PDFDocument12 pagesPractice-Based Clinical Evaluation of Zirconia PDFDiego Alejandro Cortés LinaresNo ratings yet
- Cambios Histológicos Asociados A La Extracción DentalDocument10 pagesCambios Histológicos Asociados A La Extracción DentalAle ZuzaNo ratings yet
- Short ImplantsFrom EverandShort ImplantsBoyd J. TomasettiNo ratings yet
- Oil Pulling and Importance of Traditional Medicine in Oral Health MaintenanceDocument6 pagesOil Pulling and Importance of Traditional Medicine in Oral Health MaintenanceTasha FarahNo ratings yet
- CS346 Midterm 6Document6 pagesCS346 Midterm 6Faux BiteNo ratings yet
- Biophysics 102 Lecture 3 1Document13 pagesBiophysics 102 Lecture 3 1Nada Atef KoraitemNo ratings yet
- 2nd Quarter - School Health Services Accomplishment ReportDocument4 pages2nd Quarter - School Health Services Accomplishment ReportJimmellee EllenNo ratings yet
- Grade3 Science Set2pdfDocument3 pagesGrade3 Science Set2pdfDushyant PradhanNo ratings yet
- Ceramic Laminate Veneers: Clinical Procedures With A Multidisciplinary ApproachDocument23 pagesCeramic Laminate Veneers: Clinical Procedures With A Multidisciplinary ApproachBenjiNo ratings yet
- An Overview of Orthodontic Wires: Trends in Biomaterials and Artificial Organs March 2014Document6 pagesAn Overview of Orthodontic Wires: Trends in Biomaterials and Artificial Organs March 2014DrRohan DasNo ratings yet
- Fundamentals of Cavity PreparationsDocument31 pagesFundamentals of Cavity PreparationsaakritiNo ratings yet
- Management of The Developing Dentition and Occlusion in Pediatric DentistryDocument18 pagesManagement of The Developing Dentition and Occlusion in Pediatric DentistryPAULA ANDREA RAMIREZ ALARCONNo ratings yet
- On Preventive Dentistry: The Axelsson SeriesDocument10 pagesOn Preventive Dentistry: The Axelsson SeriesHoàng Kiều DiễmNo ratings yet
- Minitornillos (02 03)Document2 pagesMinitornillos (02 03)Dikita ZamaNo ratings yet
- Ex Vivo Evaluation of The Ability of Four Different ElectronicDocument5 pagesEx Vivo Evaluation of The Ability of Four Different ElectronicJing XueNo ratings yet
- Dental Caries Prevention and TreatmentDocument7 pagesDental Caries Prevention and TreatmentJOHN HAROLD CABRADILLANo ratings yet
- Clinical S - : Dr. K. S KumarDocument10 pagesClinical S - : Dr. K. S KumarDr. Neesu KumbhatNo ratings yet
- Recommendations For Implant-Supported Full-Arch Rehabilitations in Edentulous Patients: The Oral Reconstruction Foundation Consensus ReportDocument13 pagesRecommendations For Implant-Supported Full-Arch Rehabilitations in Edentulous Patients: The Oral Reconstruction Foundation Consensus Reportsergio bernardesNo ratings yet
- Anagement of Space Problems in The Primary and Mixed DentitionsDocument10 pagesAnagement of Space Problems in The Primary and Mixed Dentitionsjing.zhao222No ratings yet
- Managment of Condylar Fracture LaskinDocument4 pagesManagment of Condylar Fracture LaskinMahdi ZakeriNo ratings yet
- Đề thi thử Anh ĐK 3Document5 pagesĐề thi thử Anh ĐK 3Duc NguyenNo ratings yet
- Belmont MANUAL OP ClestaIICM HolderType-EnDocument24 pagesBelmont MANUAL OP ClestaIICM HolderType-EnAzzamNo ratings yet
- HTTP WWW - Styleitaliano.org Stamp Technique CommunityDocument11 pagesHTTP WWW - Styleitaliano.org Stamp Technique CommunityAmee PatelNo ratings yet
- Esthetic Correction of Gummy Smile by Gingivectomy Using Diode LaserDocument5 pagesEsthetic Correction of Gummy Smile by Gingivectomy Using Diode LaserlindaNo ratings yet
- Blue Assured Individual Health PlanDocument5 pagesBlue Assured Individual Health PlanahsanNo ratings yet
- Exam Hilla 1122Document4 pagesExam Hilla 1122zainNo ratings yet
- Marzouk Password RemovedDocument487 pagesMarzouk Password RemovedKeerthiga NagarajanNo ratings yet
- VOCABULARY Daily RoutineDocument3 pagesVOCABULARY Daily Routinecristylersam7No ratings yet
- Divisi Go List Product GSK Per 1 April 2022 Harga: NO Kode Produk Deskripsi SatuanDocument2 pagesDivisi Go List Product GSK Per 1 April 2022 Harga: NO Kode Produk Deskripsi Satuanmispa hendriNo ratings yet
- SOP For MoH Dental Clinics - Management of Periodontal Conditions in Primary Oral Healthcare ClinicsDocument23 pagesSOP For MoH Dental Clinics - Management of Periodontal Conditions in Primary Oral Healthcare ClinicsSu Min LaiNo ratings yet
- Your Total Rewards at Newyork-PresbyterianDocument20 pagesYour Total Rewards at Newyork-PresbyterianweiweiahNo ratings yet
- Standard Operating Procedure: Transition To RecoveryDocument38 pagesStandard Operating Procedure: Transition To RecoveryArjun KanjariaNo ratings yet