Professional Documents
Culture Documents
Soket Prostesis
Soket Prostesis
Uploaded by
AnantaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Soket Prostesis
Soket Prostesis
Uploaded by
AnantaCopyright:
Available Formats
Case Report: Variably Compliant Transtibial Prosthetic Socket Fabricated Using Solid Freeform Fabrication
Bill Rogers, MS, Gordon Bosker, MEd, CPO, CPED, Mario Faustini, PhD, Gail Walden, MPH, Richard R. Neptune, PhD, Richard Crawford, PhD
ABSTRACT
Achieving and maintaining a comfortable t in a lower-limb prosthetic socket is an important goal to help ensure a successful rehabilitation. The purpose of this case study was to assess the performance of sockets with compliant features integrated into the socket wall to relieve in-socket pressure during transtibial amputee gait. Two sockets incorporating variably compliant areas over the bula head and distal tibia were fabricated for a transtibial amputee. The two sockets were designed with different levels of compliance and were compared with a third more conventional socket without compliant areas. All three sockets were otherwise geometrically identical and were aligned identically to eliminate in-socket pressure differences due to alignment. The three sockets were fabricated using selective laser sintering, a form of solid freeform fabrication. The in-socket pressure measurements were acquired during normal walking. Tekscan F-Socket pressure sensors were attached to the amputees residual limb rather than to the socket wall, which made it possible to measure pressures in the same location on the residual limb upon change of socket. A Vicon motion capture system was used to match in-socket pressures to the subjects gait cycle. The pressure measurements showed that the compliant socket peak pressures over the distal tibia and bula head were similar for the two compliance levels and nearly 50% and 30% lower than the conventional socket pressures, respectively. This case study showed that selective laser sintering manufactured sockets with variably compliant regions holds great promise for reducing contact pressure in sensitive regions of the residual limb. (J Prosthet Orthot. 2008;20:17.) KEY INDEXING TERMS: prosthetic socket, amputees, CAD, CAM, solid freeform fabrication
he most important aspect of a lower extremity transtibial prosthesis is the socket design. The socket introduces a new interface or a new joint between the human and the mechanical support system. The forces generated through the socket either by body weight or by gait
BILL ROGERS, MS, is afliated with the Department of Rehabilitation Medicine, The University of Texas Health Science Center at San Antonio, San Antonio, Texas. GORDON BOSKER, MED, CPO, CPED, is afliated with the Department of Rehabilitation Medicine, The University of Texas Health Science Center at San Antonio, San Antonio, Texas. MARIO FAUSTINI, PhD, is afliated with the Department of Mechanical Engineering, The University of Texas at Austin, Austin, Texas. GAIL WALDEN, MPH, is afliated with PM&R Service, South Texas Veterans Healthcare System, San Antonio, Texas. RICHARD R. NEPTUNE, PHD, is afliated with the Department of Mechanical Engineering, The University of Texas at Austin, Austin, Texas. RICHARD CRAWFORD, PHD, is afliated with the Department of Mechanical Engineering, The University of Texas at Austin, Austin, Texas. Supported by Veterans Administration grant no. A2755-r. Disclosure: The authors declare no conict of interest. Copyright 2007 American Academy of Orthotists and Prosthetists. Correspondence to: Bill Rogers, MS, Research Imaging Center, The University of Texas Health Science Center at San Antonio, 7703 Floyd Curl Drive, San Antonio, TX 78229; e-mail: rogers@ uthscsa.edu
Volume 20 Number 1 2008
have to be carried by the soft tissue of the residual limb, which when improperly loaded can lead to discomfort or skin breakdown. Ultimately, the design and t of the socket is what determines patient acceptance, comfort, suspension, and energy expenditure.1 Achieving and maintaining a comfortable and tissue-tolerant socket t remains a signicant clinical problem. This study explores the use of new manufacturing techniques to fabricate sockets with integrated compliant features specically designed to improve comfort and t of the prosthesis.
SOCKET DESIGN
There are two principal socket design strategies, and each is designed to distribute loads to pressure-tolerant tissues and relieve pressure on sensitive areas. The rst is the specic weight-bearing socket where loads are distributed over pressuretolerant areas of the residual limb such as the patella tendon, and pressure relief is provided over sensitive areas such as the bula head. The second principal design is the total surfacebearing socket with a gel-type liner. Here, the pressure is applied to the entire surface of the residual limb at a tolerable level. In this case, the method of relieving pressure is to provide liner materials that by their nature redistribute the weight-bearing areas by the ow of the material.2,3 An alternative solution is to locally modify the properties of the socket wall to provide pressure relief; however, very little work has been done in this area, especially in transtibial sockets.
CAD/CAM
Much effort has gone into the development of CAD/CAM systems for designing prosthetic sockets. However, a limita1
Rogers et al.
JPO Journal of Prosthetics and Orthotics
tion of commercially available prosthetic CAD systems is that they only represent the three-dimensional (3D) shape of the inner wall of the socket with limited ability to design features for pylon attachment. These CAD systems only design a pattern to be machined, which is all that is necessary for conventional fabrication. A promising alternative to conventional manufacturing is to use Solid Freeform Manufacturing (SFF) technologies, which are a class of technologies that can create 3D objects directly from a geometric database without specic tooling or human intervention.4 Objects are generally built in layers that are fused by a laser or a binder, or are created by extruded material. The SFF process used by this study is Selective Laser Sintering (SLS), in which components are built by material addition rather than by material removal using a directed laser beam that fuses powder particles in selected regions of space. The process begins by rst depositing a thin layer of powder into the part bed. The powder surface is rasterscanned with a laser beam in much the same way a picture is formed on a television screen by a set of horizontal lines. The intensity of the beam is modulated to melt the powder in the areas that dene the cross section of the part. Successive layers of powder are then deposited and scanned until the entire part is complete. In areas not irradiated, the powder remains loose and is removed once the part is completed. A variety of materials can be used in the process including metals, polymers, and wax. Historically, SFF has been used to make prototype parts for industry, which makes this fabrication technique a good match for use in prosthetics as each prosthetic socket is unique. The entire socket can be directly fabricated at once complete with trimlines and pylon attachment mounting features. Additional features also can be included such as variable compliance socket walls and integrated ttings. The SFF industry is largely service bureau based, which is a mode common with the prosthetics industry in many countries. There are several SFF techniques that have been used to directly fabricate prosthetic sockets under computer control thereby avoiding the intermediate step of pattern fabrication. The University of Texas at Austin (UTA) and The University of Texas Health Science Center at San Antonio (UTHSCSA) have collaborated to make a number of transtibial sockets using SLS.511 Stereolithography involves hardening a liquid photopolymer with a laser. This technique has been explored by Northwestern University12 and Freeman and Wontorcik13 to fabricate trial prosthetics sockets. Fused deposition modeling forms 3D shapes by extruding a bead of molten material through a nozzle. Fused deposition modeling has been used by Northwestern14,15, Lee,16 and Monash Universities17 to fabricate transtibial sockets. 3D printing is a method using gypsum or starch and a binder to form 3D parts in layers. Herbert et al.18 fabricated two prosthetic sockets using this method.
2
These systems could provide many benets including sockets with different mechanical properties in different areas of the socket.10,11,19 Thus, SFF is a promising technology to introduce compliant features in selective regions to reduce contact pressure. The idea is to assure proper rigidity of the socket in load-bearing areas while making the socket wall more exible over sensitive regions such as bony prominences. This can be achieved to a lesser degree with conventional fabrication with a exible inner socket and fenestrated rigid outer socket, though the conventional approach is labor intensive and expensive. With SFF, the cost of fabrication is related to the volume of the part rather than its complexity, so there is no cost penalty for a more sophisticated design. In addition, the freedom of design for parts fabricated with SFF technologies allows the exploration of potentially more elegant and efcient design solutions that would be otherwise prohibitively expensive or even impossible to manufacture using conventional methods. Early work at UTA and UTHSCSA in using SLS to produce a variably compliant socket resulted in a double-wall socket using cantilever compliant areas.7 This socket had a rigid outer wall and a thinner more exible inner wall. In addition, the inner wall had two hexagonal sets of triangular cantilever beams over the distal tibia and bula head. Some manual steps were required to trim the socket top. Quantitative gait analysis showed little difference between the subjects conventional socket and the cantilever compliant socket. This work led to the development of a spiral compliant area incorporating a diaphragm spring.11 Two sockets were fabricated using the spiral compliant areas and were tested on an amputee and compared with a socket without compliant areas.10 This initial test showed lowered socket pressures over the compliant areas. There was no period of acclimation for the sockets between the subjects conventional socket and the SFF manufactured sockets. The only measures taken were in-socket pressures that limited the ability to synchronize insocket pressure with the gait cycle. The purpose of this case study was to assess performance of sockets with compliant features integrated into the socket wall to relieve in-socket pressure during transtibial amputee gait. An important aspect of this study is limitation of the number of confounding variables by comparing sockets that are aligned identically and are otherwise geometrically identical. In addition, the subject was well acclimated to the socket design at the time of testing.
METHODS
The subject in this study was a 47-year-old male traumatic transtibial amputee. He weighed 85 kg, was 180 cm tall, and was judged a K4 ambulator. He had been an amputee for 5 years. He was recruited from the University Hospital prosthetic clinic. Informed consent was obtained following local institutional review board protocols.
Volume 20 Number 1 2008
JPO Journal of Prosthetics and Orthotics
Variably Compliant Prosthetic Socket Fabricated Using SFF
SOCKET FABRICATION
The residual limb was cast using a berglass casting sock. The shape of the residual limb was digitized from the casting sock using a ShapeMaker 2000 scanner. A total surface bearing socket pattern was designed using GordoDesign prosthetic CAD software (GordoDesign. 1.1. 2002, University of Texas Health Science Center, San Antonio, TX). A foam pattern was milled using a Seattle SM2000 carver, and a check socket was fabricated for use with a Harmony VASS suspension system (Otto Bock, Minneapolis, MN, http://www. ottobockus.com). Once the socket was deemed suitable, the socket including trimline, wall thickness, location of pylon adapter, and location of compliant areas was output as a spline surface model in an IGES le (Initial Graphics Exchange Specication, IGES; http://www.eeel.nist.gov/iges/). The IGES le was imported into Rhinoceros (Rhino. 3.0. Robert McNeel and Associates, 2005, http://www.en.na. mcneel.com/.), a 3D CAD program, for nal socket design. Three sockets were designed from the same socket interior shape, and all incorporated the same pylon attachment tting for a European four-hole adapter. The rst socket was a conventional design except for a variation in socket wall thickness over the bula head and the distal tibia. The other two sockets had integrated variable compliance features over the bula head and distal tibia. The compliance was provided by an integrated diaphragm spring (Fig. 1).10 The thickness of the diaphragm spring was varied giving one socket more compliance than the other. The stiffness of the compliant areas was calculated by nite element modeling (FEM) using the I-deas (UGS, Plano, TX, http://www.ugs.com/) mechanical CAD software package. All values were obtained using FEM models of the compliant sites isolated from the socket; in other words, they are local, not taking into account the overall deformation of the socket. The boundary conditions were designed as follows: the surrounding surface of the detached compliant site was xed, and a dummy force (1 N) was applied at the center of the inner surface (where it should interface the limb/sock) of the compliant site, pointing outwards (to the outside of the socket). From the results of the FEM analysis, the displacement of the center of the compliant site was obtained, and the stiffness was calculated by dividing the force by the displacement (Table 1). The sockets were fabricated on a 3DSystems Vanguard HS SLS System (3D Systems, Valencia, CA, http://www.3dsystems.com/)
from Rilsan D80 polyamide powder (Arkema, France), a form of Nylon 11. The sockets with compliant areas required modication to work with the Harmony VASS system. Holes in the external diaphragm cover, which were used to remove excess powder after fabrication, were lled with epoxy putty to seal the sockets for vacuum (Fig. 2). The subjects prosthesis was assembled using the Harmony VASS system initially using the conventional socket without the sophisticated compliant areas. The subject was allowed to wear the socket for the following year and underwent regular evaluations to assure a proper t.
SOCKET EVALUATION
At the end of the year, a test session was scheduled to evaluate all three sockets via in-socket pressure measurements over the bula head and the distal tibia as well as kinematic and kinetic gait parameters. In-socket pressure measurements were taken using a Tekscan F-Scan Mobile system (Tekscan, Inc., South Boston, MA, http://www.tekscan. com/). This system utilizes F-Socket Mylar/resistive ink transducers that were attached to the residual limb. F-Socket transducers were trimmed to the appropriate size then calibrated using a at pressure bladder. To maintain the location of the sensors on the residual limb between tests, the sensors were attached directly to the residual limb rather than to the socket. This ensured that pressure measurements between the three sockets could be directly compared. To attach the sensors to the residual limb, the residual limb was wrapped in a shrink wrap plastic (Fig. 3). The plastic was gently heated to conform to the residual limb. The F-Socket sensors were then glued to the plastic around the residual limb. The regions of the distal tibia and bula head were marked on the sensors and photographed to aid in identifying those regions in the F-Scan analysis software. The subject walked using the socket without compliant features for about 5 minutes to condition the sensors. The F-Scan mobile system was used to capture three 30-second walks at a self-selected walking speed in a straight line. To dene the gait cycle and conrm that the overall walking mechanics were similar between sockets, a six-camera, four AMTI force plates (AMTI, Watertown, MA, http://www.amti.biz/), Vicon 370 3D Motion Analysis System (VICON Motion Systems, Tustin, CA, http://www.vicon.com/) was used. Reective markers were placed according to the Plug-In-Gait marker set. Ground reaction forces were obtained using AMTI force
Figure 1. CAD model of compliant socket showing inside, outside, and cross section.
Volume 20 Number 1 2008
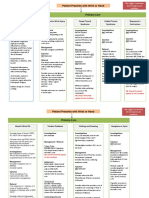
Rogers et al. Table 1. FEM calculated stiffness (kN/m)
JPO Journal of Prosthetics and Orthotics
Distal Tibia
Conventional socket Compliant socket 1 Compliant socket 2 194.4 79.5 58.4
Fibula Head (terminal stance)
112.3 27.2 19.8
location for all sockets, alignment was not affected. The data capture procedure was repeated for each of the two compliant sockets. At the end of the session, the F-Socket sensors were calibrated again to account for sensor drift.
RESULTS
The sockets with the variably compliant areas showed considerably less pressure over the distal tibia and bula head than the more conventional socket (Table 2 and Fig. 4 ). The maximum pressure over the distal tibia occurred during mid stance for all three sockets. The maximum pressure over the bula head occurred during terminal stance with the conventional socket (Table 2). With the compliant sockets, there were two small pressure peaks over the bula head during mid stance and terminal stance. There was an additional smaller pressure peak over the bula head during terminal swing with all three sockets. Vertical ground reaction forces were essentially the same for all sockets (Fig. 5). The cadence and walking speed increased with the compliant sockets. The increase was greatest with compliant socket 2, which had the most compliance (Table 3).
DISCUSSION
The goal of this case study was to assess the performance of sockets with compliant features integrated into the socket wall to relieve in-socket pressure during transtibial amputee gait. An important part of the study was to compare sockets that were geometrically identical except for the compliant areas. This approach limited the number of variables to be managed. Also, being able to switch sockets without changing the alignment was as important to avoid the confounding inuence of alignment on in-socket pressure. The compliant sockets showed considerably less pressure over the distal tibia and bula head than the more conventional socket. The pressures from the two variably compliant sockets were so close as to be indistinguishable. As can be seen from Table 1, the calculated stiffness of the two compliant sockets is much less than the conventional socket. Also the difference in stiffness between the two compliant sockets is relatively small. Previous work showed a difference in in-socket pressures with two compliant sockets.10 The earlier work utilized Duraform PA, a type of Nylon-12 (3D Systems), rather than the Nylon-11 used here. A difference in material properties between the two materials may account for the differences observed. In this study, the compliant sockets
Table 2. Peak in-socket pressure (KPa)
Figure 2. Assembled prostheses, compliant SLS socket on right.
Figure 3. Tekscan sensor placement on residual limb.
plates embedded into the gait lab oor. The subject walked at his self selected speed through the motion capture area. Enough trials were taken to get ve clear hits on a force plate for each foot. At the same time, F-Scan in-socket pressures were captured so that they could be synchronized with the gait cycle. The socket was then replaced with one of the compliant sockets. Because the pylon attachment was in the same
4
Distal Tibia (mid stance)
Conventional socket Compliant socket 1 Compliant socket 2 177.8 88.4 97.9
Fibula Head (terminal stance)
97.4 33.9 25.9
Volume 20 Number 1 2008
JPO Journal of Prosthetics and Orthotics
Variably Compliant Prosthetic Socket Fabricated Using SFF
Figure 4. In-socket pressures over distal tibia and bula head.
Figure 5. Normalized vertical ground reaction forces. Table 3. Cadence, stride length, and walking speed
Cadence Stride Walking (steps/min) Length (m) Speed (m/s)
Conventional socket Compliant socket 1 Compliant socket 2 96.8 101.0 105.0 1.38 1.35 1.41 1.12 1.14 1.23
used a stiffness of less than half the stiffness of the conventional socket. Future tests should use a wider range of socket compliance by using a greater variation in the stiffness of the diaphragm spring including stiffness values closer to that of a conventional socket. All the pressure measurements were taken during one session, so relative measurements of pressure between sockets were valid. However, quantifying the absolute value of the in-socket pressure was difcult because of specic issues with the F-Socket sensors. The sensors were calibrated using a at pressure bladder, and it has been reported that the sensor output is affected by the curvature of the surface they are
Volume 20 Number 1 2008
attached to,20 with areas of higher curvature reporting higher pressures. As the residual limb has a highly contoured surface, the absolute value of the pressure is likely smaller than was recorded. It should be noted that over the distal tibia, the peak pressure measured in compliant socket 2 was higher than the stiffer compliant socket 1. The difference may be due to the slightly higher cadence and walking speed observed during the compliant socket 2 trials. The difference is small and may also be due to the limitations of the accuracy of the F-Scan system. There was a slight increase in cadence and walking speed with the compliant sockets (Table 3). It might be expected that the faster cadence and walking speed measured with the compliant sockets would result in higher ground reaction forces though the measured ground reaction forces were essentially identical (Fig. 5). It may be that the cushioning effect of the compliant sockets mitigated any increase in pressure due to an increase in walking speed. All sockets showed a small pressure peak over the bula head during terminal swing. The small peak occurred in the
5
Rogers et al.
JPO Journal of Prosthetics and Orthotics
proximal end of the sensor region dened for the bula head, and the peaks during stance occurred in a more distal location. This suggests that some pistoning of the residual limb within the socket was occurring. Apparently there was enough motion in the socket for the bula head to contact the proximal end of the relief area during swing. The appearance of the compliant sockets is unattractive. The bulbous covers over the compliant regions are cosmetically challenging. It should be possible to lower the prole and blend the compliant regions into the socket. For these sockets to be clinically acceptable a more suitable cosmetic appearance will be necessary. The subject had complained about discomfort in the area of the bula head with the long-term conventional SLS socket. He felt that the SLS compliant socket 2, which was designed to have more compliance, was most comfortable and relieved the discomfort. The increased comfort may account for the increased walking speed observed. The inability to predict socket pressures via modeling is a clear limitation of this study. Calculated stiffness values alone will not predict the level of compliance and pressure relief for the site. Compliant features with the same stiffness could lead to different pressure-relieving outcomes due to other factors such as the location of the compliant feature on the socket, and even more importantly, the interaction with the tissues that will contact the feature (how bony is the site or how much soft fat or muscle will be in contact with the feature or with the areas surrounding the compliant feature to where the peak pressures will be redistributed once the feature starts to deform). An initial attempt at studying the response of the entire system (compliant socket residual limb) was done in a previous case study.11 This study used computed tomography data of the patient while wearing a prosthetic socket, which is not done in a normal clinical situation. In conclusion, this case study showed that the SLS manufactured sockets with the variably compliant regions were successful in reducing pressures in sensitive regions of the residual limb. Future work will address the long-term durability of the compliant sockets, improvements in cosmetic appearance, and the evaluation of a large number of subjects.
3. Baars EC, Geertzen JH. Literature review of the possible advantages of silicon liner socket use in trans-tibial prostheses. Prosthet Orthot Int 2005;29:2737. 4. Beaman JJ, Bourell DL, Crawford RH, et al. Solid Freeform Fabrication: A New Direction in Manufacturing. Norwell, MA: Kluwer Academic Publishers; 1997. 5. Rogers W, Crawford RH, Beaman JJ, et al. Fabrication of prosthetic sockets by selective laser sintering. In: Bourell DL, Beaman JJ, Crawford RH, et al., eds. Solid Freeform Fabrication Symposium. Austin, TX: University of Texas; 1991: 158 163. 6. Rogers W, Crawford RH, Faulkner VF, et al. Fabrication of an integrated prosthetic socket using solid freeform fabrication. In: Zupko JP, ed. Seventh World Congress of the International Society for Prosthetics and Orthotics. Chicago, IL: International Society for Prosthetics and Orthotics; 1992:23. 7. Rogers B, Stephens S, Gitter A, et al. Double-wall, transtibial prosthetic socket fabricated using selective laser sintering: a case study. J Prosthet Orthot 2000;12:97100. 8. Stephens S, Crawford R, Rogers W, et al. Manufacture of compliant prosthesis sockets using selective laser sintering. In: Bourell DL, Beaman JJ, Crawford RH, et al. Eleventh Freeform Fabrication Symposium. Austin, TX: University of Texas; 2000: 565577. 9. Rogers B, Gitter A, Bosker G, et al. Clinical evaluation of prosthetic sockets manufactured by selective laser sintering. In: Bourell DL, Beaman JJ, Crawford RH, et al. Twelfth Freeform Fabrication Symposium. Austin, TX: University of Texas; 2001: 505512. 10. Faustini MC, Crawford RH, Neptune RR, et al. Design and analysis of orthogonally compliant features for local contact pressure relief in transtibial prostheses. J Biomech Eng 2005; 127:946 951. 11. Faustini MC, Neptune RR, Crawford RH. The quasi-static response of compliant prosthetic sockets for transtibial amputees using nite element methods. Med Eng Phys 2006;28:114 121. 12. Rovick J, et al. Computer-aided manufacturing in prosthetics: various possibilities using industrial equipment. In: Zupko JP, ed. Seventh World Congress of the International Society for Prosthetics and Orthotics. Chicago, IL: International Society for Prosthetics and Orthotics; 1992:22. 13. Freeman D, Wontorcik L. Stereolithography and prosthetic test socket manufacture: a cost/benet analysis. J Prosthet Orthot 1998;10:1720. 14. Rovick J. An additive fabrication technique for the computeraided manufacturing of sockets. In: Zupko JP, ed. Seventh World Congress of the International Society for Prosthetics and Orthotics. Chicago, IL: International Society for Prosthetics and Orthotics; 1992:24. 15. Northwestern University. Squirt Shape Enters New Phase of Development. 2003 http://www.medschool.northwestern.edu/ depts/repoc/sections/research/projects/cadcam/index.html.
Volume 20 Number 1 2008
ACKNOWLEDGMENTS
Thanks to the Andrew J. Gitter Research Center at the South Texas Veterans Healthcare System and the Laboratory for Freeform Fabrication at the University of Texas, Austin whose technical resources were key to this study. Thanks to Alberto Portillo for assistance with processing the data. We recognize Nicolas Walsh, MD for his continued support of this research.
REFERENCES
1. Fergason J, Smith DG. Socket considerations for the patient with a transtibial amputation. Clin Orthop Relat Res 1999;361: 76 84. 2. Edwards ML. Below knee prosthetic socket designs and suspension systems. Phys Med Rehabil Clin N Am 2000;11:585593. 6
JPO Journal of Prosthetics and Orthotics
Variably Compliant Prosthetic Socket Fabricated Using SFF 18. Herbert N, Simpson D, Spence WD, Ion WJ. A preliminary investigation into the development of 3-D printing of prosthetic sockets. J Rehabil Res Dev 2005;42:141146. 19. Smith DG, Burgess EM. The use of CAD/CAM technology in prosthetics and orthotics current clinical models and a view to the future. J Rehabil Res Dev 2001;38:327334. 20. Ferguson-Pell M, et al. Evaluation of a sensor for low interface pressure applications. Med Eng Phys 2000;22:657 663.
16. Lee P, Tan KC, Tam KF, Lye SL. Biomechanical evaluation of prosthetic sockets fabricated using fused depository method. In: Goh JCH, Lee PVS, ed. Fourth Asian Symposium on Biomedical Materials. Singapore: The Institute of Materials Research and Engineering; 1998. 17. Monash University. Digital manipulation of prosthesis data for the introduction of advanced manufacturing techniques. 2002 http://rehabtech.eng.monash.edu.au/cadcam/INFO/details.htm.
Anatomy & Human Movement
NEW
By Nigel Palastrange, MA, BA, MCSP, DMS, DipTP Derek Field: Grad Dip Phys, FCSP, DipTP, SRP Rogert W. Soames, BSc, PhD
With over 25,000 copies sold, this book has established itself as a core textbook for students. All illustrations have been redrawn to meet the needs of students today along with a new design and layout to make studying anatomy easier. The upper and lower limbs have been divided into the bones, muscles, joints, and nerve and blood supply, and the book also covers the skin, trunk, neck, head, viscera and nervous system in a comprehensive way. The musculoskeletal structures are presented as a living dynamic system and is a must-buy for all students of physiotherapy, osteopathy, chiropractic, occupational therapists as well as sports scientists, kinesiologists and podiatrists.
MEMBERS: $65 NONMEMBERS : $75
ORDER TODAY! Call 301-617-7805
Volume 20 Number 1 2008
You might also like
- DSUS VELYS Robot Product BrochureDocument10 pagesDSUS VELYS Robot Product BrochureKBTXNo ratings yet
- Manual Book Forklift ToyotaDocument12 pagesManual Book Forklift ToyotaAnanta60% (5)
- Global Top 100 Manufacturers of Orthopedic & Prosthetic Devices: A Thorough Analysis of The Technologies and TrendsDocument4 pagesGlobal Top 100 Manufacturers of Orthopedic & Prosthetic Devices: A Thorough Analysis of The Technologies and Trendsriya jain0% (1)
- Above-Knee Fitting and Alignment Tehniques PDFDocument18 pagesAbove-Knee Fitting and Alignment Tehniques PDFsunsrayNo ratings yet
- Production of NuggetDocument10 pagesProduction of NuggetNur AishaNo ratings yet
- Reservoir CouplingDocument39 pagesReservoir CouplingGigih Adi PambudiNo ratings yet
- American Academy of Orthotists & ProsthetistsDocument14 pagesAmerican Academy of Orthotists & ProsthetistsAndres UlloaNo ratings yet
- ThirdDocument24 pagesThirdtinap_15No ratings yet
- Ispo-Who Training GuidelinesDocument59 pagesIspo-Who Training GuidelinesAlfionita WikaNo ratings yet
- PMR Role in Congenital Limb Deficient 2Document42 pagesPMR Role in Congenital Limb Deficient 2virginiaNo ratings yet
- Design of A Prosthesis For Running in Composite MaterialsDocument12 pagesDesign of A Prosthesis For Running in Composite MaterialsginkenoNo ratings yet
- Introduction To Prosthetic & OrthoticDocument63 pagesIntroduction To Prosthetic & OrthoticHassan Saifullah Khan AlisherzaiNo ratings yet
- P&O Elementary MathematicsDocument22 pagesP&O Elementary MathematicsrrutayisireNo ratings yet
- How To Make A Prosthetic LimbDocument6 pagesHow To Make A Prosthetic LimbMatt LawallNo ratings yet
- Large Medium ExternalfixatorsDocument42 pagesLarge Medium ExternalfixatorsZulfadli Salleh0% (1)
- Orthotics Consensus Conference ReportDocument354 pagesOrthotics Consensus Conference ReportAlec joshua RapadaNo ratings yet
- The Application of Supra - Malleolar Orthosis (SMO) in Iraq: Design and Fabrication ApproachDocument13 pagesThe Application of Supra - Malleolar Orthosis (SMO) in Iraq: Design and Fabrication ApproachucssNo ratings yet
- Modelling and Analysis of A Prosthetic Runner BladeDocument11 pagesModelling and Analysis of A Prosthetic Runner BladeIJRASETPublicationsNo ratings yet
- Hand and Wrist PathwayDocument2 pagesHand and Wrist PathwaydrsadafrafiNo ratings yet
- Bs. in P&O India. Syllabus 2010Document58 pagesBs. in P&O India. Syllabus 2010Priscila Arriagada PulgarNo ratings yet
- Admission: Post Graduate Entrance Test (Pget) - 2019Document15 pagesAdmission: Post Graduate Entrance Test (Pget) - 2019deepanshi vashishthaNo ratings yet
- Clinical Symptom Score of The Japanese Orthopaedic Association PDFDocument3 pagesClinical Symptom Score of The Japanese Orthopaedic Association PDFJoanne NgimNo ratings yet
- Prosthetic Knee JointsDocument20 pagesProsthetic Knee JointsAlfred JacksonNo ratings yet
- Foot and Ankle Clinics Volume A Refined Classification SystemDocument17 pagesFoot and Ankle Clinics Volume A Refined Classification SystemRicardo CastilloNo ratings yet
- Rotational Flap Closure of 1st and 5nth Met HeadDocument8 pagesRotational Flap Closure of 1st and 5nth Met HeadleahbayNo ratings yet
- ProsthesisDocument2 pagesProsthesislisasmith2000012No ratings yet
- Prosthesis For Symes AmputationDocument24 pagesProsthesis For Symes AmputationSHAIK SHABEENANo ratings yet
- BionicDocument33 pagesBionicperepu jyotirmayiNo ratings yet
- Myoelectric ControlDocument15 pagesMyoelectric ControlAbdullah AhmedNo ratings yet
- 01-Hypro-Oss Clinical Assessment 2012 enDocument14 pages01-Hypro-Oss Clinical Assessment 2012 enPaulus LagadanNo ratings yet
- The Journal of Bangladesh Orthopaedic Society (JBOS)Document118 pagesThe Journal of Bangladesh Orthopaedic Society (JBOS)Roman Popescu100% (1)
- Gates ThesisDocument95 pagesGates Thesisforlogin018No ratings yet
- Overview of Knee Dis ArticulationDocument30 pagesOverview of Knee Dis ArticulationNitin RananavareNo ratings yet
- Exocad Prosthetic Components Libraries enDocument22 pagesExocad Prosthetic Components Libraries enAlex BushNo ratings yet
- Gpe - 017.1 - Orthopaedic ExaminationDocument3 pagesGpe - 017.1 - Orthopaedic ExaminationImiey Eleena HanumNo ratings yet
- The Neglected ClubfootDocument3 pagesThe Neglected ClubfootAngelica Mercado SirotNo ratings yet
- Uka Failure Mechanisms Vs TKRDocument7 pagesUka Failure Mechanisms Vs TKRapi-267962692100% (1)
- ORTHOPEDICSDocument7 pagesORTHOPEDICSMohsin JahNo ratings yet
- Recommendations For Blood Collection, Processing and Reporting of Coagulation AssaysDocument22 pagesRecommendations For Blood Collection, Processing and Reporting of Coagulation AssaysHaizel HoughtonNo ratings yet
- Distraction OsteogenesisDocument30 pagesDistraction OsteogenesisMohd ZahiNo ratings yet
- Steeper Prosthetic Best Practice GuidelinesDocument67 pagesSteeper Prosthetic Best Practice GuidelinesMohammed Al-shamiriNo ratings yet
- 2002, Vol.33, Issues 1, Treatment of Complex FracturesDocument280 pages2002, Vol.33, Issues 1, Treatment of Complex FracturesSitthikorn StrikerrNo ratings yet
- ProsthesisDocument52 pagesProsthesisVijay MgNo ratings yet
- Shoulder Arthroplasty WIC - Dr. LSDocument56 pagesShoulder Arthroplasty WIC - Dr. LSDifitasari Cipta Perdana100% (1)
- Secur-Fit Advanced: Surgical TechniqueDocument28 pagesSecur-Fit Advanced: Surgical TechniqueX ComNo ratings yet
- ATTUNE S+ Master Content Deck DSUS - JRC - 0517 - 2142Document82 pagesATTUNE S+ Master Content Deck DSUS - JRC - 0517 - 2142medtechy100% (1)
- OSTEOPOROSISDocument39 pagesOSTEOPOROSISHapsari Wibawani 'winda'No ratings yet
- NPWT RENASYS and PICO Clinical GuidelinesDocument78 pagesNPWT RENASYS and PICO Clinical GuidelinesAgung GinanjarNo ratings yet
- Corail Surgical Technique Revision 1 PDFDocument20 pagesCorail Surgical Technique Revision 1 PDFKaustubh KeskarNo ratings yet
- Pilon Fractures Preventing ComplicationsDocument12 pagesPilon Fractures Preventing ComplicationsjojoNo ratings yet
- Final PGP PGO PGASLP - MSC - PO CET 2018 Information Brochure 1Document52 pagesFinal PGP PGO PGASLP - MSC - PO CET 2018 Information Brochure 1Subhashree Sahoo0% (1)
- 501k StrykerDocument12 pages501k StrykerFrancisco100% (1)
- Prostehtics For Transtibial AmputeesDocument13 pagesProstehtics For Transtibial Amputeesaufar syehanNo ratings yet
- Skeletal System: By: Ella Dela Cruz:)Document11 pagesSkeletal System: By: Ella Dela Cruz:)EllaDelaCruzNo ratings yet
- Pilot Study of The Wrist Orthosis Design ProcessDocument7 pagesPilot Study of The Wrist Orthosis Design ProcessRobert PetersonNo ratings yet
- Double GlovingDocument24 pagesDouble GlovingCarlos Rios100% (1)
- Versys Fiber Metal Taper Hip Prosthesis Surgical TechniqueDocument16 pagesVersys Fiber Metal Taper Hip Prosthesis Surgical TechniqueSaumil ShahNo ratings yet
- Knee Disarticulation: A Whirlwind TourDocument39 pagesKnee Disarticulation: A Whirlwind TourRifka AnnisaNo ratings yet
- Clemens Attinger 10 Angiosomes and Wound Care in The Diabetic FootDocument26 pagesClemens Attinger 10 Angiosomes and Wound Care in The Diabetic FootDorin DvornicNo ratings yet
- Actures - In.adults.8e Booksmedicos - Org Parte4 PDFDocument1 pageActures - In.adults.8e Booksmedicos - Org Parte4 PDFeladioNo ratings yet
- Amvex Intermittent Vacuum Regulator Manual PDFDocument4 pagesAmvex Intermittent Vacuum Regulator Manual PDFPeter ayalaNo ratings yet
- Patient-Specific Bone Implants Using Subtractive Rapid PrototypingDocument12 pagesPatient-Specific Bone Implants Using Subtractive Rapid PrototypingsreeshpsNo ratings yet
- Epoxy Resins (Overview)Document11 pagesEpoxy Resins (Overview)gogana93No ratings yet
- Refrigeration and Heat PumpDocument21 pagesRefrigeration and Heat PumpAnantaNo ratings yet
- Daftar Harga Prosthesis April 2011 - Kuspito Prosthetic OrthoticDocument1 pageDaftar Harga Prosthesis April 2011 - Kuspito Prosthetic OrthoticAnantaNo ratings yet
- Windows Tips+Document135 pagesWindows Tips+AnantaNo ratings yet
- FGHBNJMKDocument2 pagesFGHBNJMKNIMANo ratings yet
- Exercise # 1: General TermDocument5 pagesExercise # 1: General TermNikhil RajNo ratings yet
- MarkDocument17 pagesMarkMutaawe MMarkNo ratings yet
- The Child SeducersDocument422 pagesThe Child SeducersurgesfromhellNo ratings yet
- Getting Started With MDMDocument22 pagesGetting Started With MDMdesijnk100% (2)
- Laboratory Report 1.1.1 Measurements and UncertaintyDocument7 pagesLaboratory Report 1.1.1 Measurements and UncertaintyalfieqdeguzmanNo ratings yet
- Bhupathiraju Ravi SanjayvarmaDocument2 pagesBhupathiraju Ravi SanjayvarmaramyaNo ratings yet
- Questions and Solutions Wit - 1665247828131Document5 pagesQuestions and Solutions Wit - 1665247828131ManishNo ratings yet
- MATH4512 2022spring HW3SolutionDocument9 pagesMATH4512 2022spring HW3SolutionMNo ratings yet
- Ict Literacy Skills Development Training of TrainersDocument3 pagesIct Literacy Skills Development Training of TrainersAmir M. Villas100% (2)
- Outline SOC 210Document7 pagesOutline SOC 210AnjNo ratings yet
- Freedom Notes Class 11Document2 pagesFreedom Notes Class 11vsurendar159No ratings yet
- BSBRSK501 Student Assessment Tasks V1.0Document46 pagesBSBRSK501 Student Assessment Tasks V1.0Ricka Mhel Garcia0% (1)
- 15 - Error Message ListDocument5 pages15 - Error Message ListZak zsNo ratings yet
- Lesson Plan WavefrontDocument6 pagesLesson Plan Wavefrontafifahyuliani100% (1)
- (Prof. Dr. Dr. H.C Dietrich H. Welte, Dr. Brian HoDocument554 pages(Prof. Dr. Dr. H.C Dietrich H. Welte, Dr. Brian HoGabi LeventeNo ratings yet
- DOW UF Case Study For High Turbid WaterDocument5 pagesDOW UF Case Study For High Turbid WaterWendyNo ratings yet
- Digital Technology Essay (Marked)Document3 pagesDigital Technology Essay (Marked)MeganSouthernNo ratings yet
- Reiki and ArchangDocument29 pagesReiki and Archangbbddd75% (4)
- Evolving Training PolicyDocument9 pagesEvolving Training PolicySandeep_Khanna_1620No ratings yet
- What Illusions Teach Us PDFDocument4 pagesWhat Illusions Teach Us PDFDr JoseNo ratings yet
- CV Nurul Rachma PutriDocument2 pagesCV Nurul Rachma PutrispongeraputNo ratings yet
- CNF Lesson 3 Bio Autobio MemoirDocument18 pagesCNF Lesson 3 Bio Autobio MemoirRJ OnsanaNo ratings yet
- Understanding Operations ManagementDocument26 pagesUnderstanding Operations ManagementlapogkNo ratings yet
- Whole Brain Teaching: Long DivisionDocument4 pagesWhole Brain Teaching: Long DivisionChris BiffleNo ratings yet
- Đề thi (chính thức)Document7 pagesĐề thi (chính thức)Mai VũNo ratings yet
- Teaching by Principles #1-GMPDocument3 pagesTeaching by Principles #1-GMPGerman MartinezNo ratings yet
- Research QuestionDocument6 pagesResearch QuestionAlfian Ardhiyana PutraNo ratings yet