Professional Documents
Culture Documents
Physiatric Assessment
Physiatric Assessment
Uploaded by
Daniel Andry KurniawanCopyright:
Available Formats
You might also like
- Test Bank For Abnormal Psychology 5th Canadian Edition by BarlowDocument37 pagesTest Bank For Abnormal Psychology 5th Canadian Edition by BarlowNancy Medez100% (41)
- Ab Psy Test BankDocument155 pagesAb Psy Test BankGabrielle Anne AbadNo ratings yet
- Child Case History Taking PDFDocument6 pagesChild Case History Taking PDFSarika Varshney100% (4)
- Townsend Workbook Answers OnlyDocument25 pagesTownsend Workbook Answers OnlygioNo ratings yet
- Bioethics SyllabusDocument10 pagesBioethics Syllabusmei_15ph83% (6)
- AP Psych Practice Questions - Unit 1Document1 pageAP Psych Practice Questions - Unit 1dms727No ratings yet
- Overview of Pediatric Physical AssessmentDocument7 pagesOverview of Pediatric Physical AssessmentLloyd Jay Lin100% (1)
- PE1 1st Quarter Pre-TestDocument2 pagesPE1 1st Quarter Pre-TestJanine Bisenio-Betchayda100% (1)
- NCM 101 - Health Assessment SyllabusDocument2 pagesNCM 101 - Health Assessment SyllabusRA100% (3)
- Review of The Nursing ProcessDocument2 pagesReview of The Nursing Processmarkkkkkkkheeess100% (1)
- Guidelines Normal Assessment Day 1 Day 2: I. Mental StatusDocument7 pagesGuidelines Normal Assessment Day 1 Day 2: I. Mental StatusEllyn Rose Cardente ManiwangNo ratings yet
- Saint Francis of Assisi College College of NursingDocument4 pagesSaint Francis of Assisi College College of NursingCarolyn CalupitanNo ratings yet
- т2Document4 pagesт2Ploy SmileNo ratings yet
- Lecture Objectives & OutlinesDocument25 pagesLecture Objectives & OutlinesFelmerPolancoRodaNo ratings yet
- Modules 1-8 Answer To Guides QuestionsDocument15 pagesModules 1-8 Answer To Guides QuestionsBlackblight •No ratings yet
- Antisocial NcaDocument71 pagesAntisocial NcaCharisse CaydanNo ratings yet
- Patient Health History TakingDocument6 pagesPatient Health History Takingrose_roxasNo ratings yet
- Patient Assessment: 3Document6 pagesPatient Assessment: 3axmedfare138No ratings yet
- Guidelines Normal Assessment Day 1 Day 2: I. Mental StatusDocument7 pagesGuidelines Normal Assessment Day 1 Day 2: I. Mental StatusEllyn Rose Cardente ManiwangNo ratings yet
- Clinical Skills Study GuideDocument58 pagesClinical Skills Study GuideAngelica Mae Dela CruzNo ratings yet
- Oral - Internal 3rd YearDocument68 pagesOral - Internal 3rd Yearps886rd6chNo ratings yet
- Reporting Finals N3-ABDocument3 pagesReporting Finals N3-ABKrisia Mhel Buyagao MollejonNo ratings yet
- NCM 100 Course OutlineDocument3 pagesNCM 100 Course Outline배기숭100% (1)
- Behavioral Analysis:: Bipolar DisorderDocument2 pagesBehavioral Analysis:: Bipolar DisorderMary Angel Diaz AlejandroNo ratings yet
- BhhuOSaETLGYbjkmhHyxOQ - 3. Approach To The Sick Patient HandoutDocument5 pagesBhhuOSaETLGYbjkmhHyxOQ - 3. Approach To The Sick Patient HandoutStrahinja ŠkoboNo ratings yet
- Trial MCQ MHBS 4013Document15 pagesTrial MCQ MHBS 4013Muhammad ArifNo ratings yet
- Fundamentals of Nursing ContentDocument2 pagesFundamentals of Nursing ContentBasty BautistaNo ratings yet
- Aleli Q1 Lifestyle LPDocument3 pagesAleli Q1 Lifestyle LPMCarl F. ClycyNo ratings yet
- Specific Objectives Content Time Allotment Teaching Strategies Evaluative MeasuresDocument5 pagesSpecific Objectives Content Time Allotment Teaching Strategies Evaluative Measureslez2No ratings yet
- Examination of The Psychiatric Patient (Notes)Document3 pagesExamination of The Psychiatric Patient (Notes)Regine GlydelNo ratings yet
- Review of Related Literature OutlineDocument1 pageReview of Related Literature Outlineangela_nehNo ratings yet
- Pscyhe - Collantes - Module 1Document10 pagesPscyhe - Collantes - Module 1Eller Tacud CollantesNo ratings yet
- Psyceh - Collantes - Module 4.-UpdatedDocument14 pagesPsyceh - Collantes - Module 4.-UpdatedEller Tacud CollantesNo ratings yet
- Instructions: Select The Most Appropriate ResponseDocument3 pagesInstructions: Select The Most Appropriate ResponseJodi-Ann RobertsNo ratings yet
- Mapeh 1st QuarterDocument5 pagesMapeh 1st QuarterNunag Mary AnnNo ratings yet
- Template Psychosocial AssessmentDocument3 pagesTemplate Psychosocial AssessmentMark ApeladasNo ratings yet
- I. Vital InformationDocument7 pagesI. Vital InformationAlecNo ratings yet
- Acute Gastroenteritis With Severe DehydrationDocument22 pagesAcute Gastroenteritis With Severe DehydrationCess Dunwan100% (1)
- Abpsy ReviewerDocument15 pagesAbpsy ReviewerMARIE ROSE L. FUNTANARNo ratings yet
- Pe Summative TestDocument2 pagesPe Summative TestErica DelapenaNo ratings yet
- Abnormal Psychology 6th Edition Nolen Hoeksema Solutions ManualDocument35 pagesAbnormal Psychology 6th Edition Nolen Hoeksema Solutions Manualuncutresortpxb0k3100% (44)
- NURS124 OxygenationDocument11 pagesNURS124 Oxygenationmarie100% (4)
- RSPT 324 - Gen. PathologyDocument5 pagesRSPT 324 - Gen. PathologyNestor BalboaNo ratings yet
- 24 Sample TestDocument1 page24 Sample TestIvy Marie ToyonganNo ratings yet
- Gordon's Functional Health Pattern FormDocument6 pagesGordon's Functional Health Pattern FormMichael Bon MargajaNo ratings yet
- Abnormal Psychology TESTDocument6 pagesAbnormal Psychology TESTShiela maeNo ratings yet
- Immobility: 1. Scientific Knowledge BaseDocument3 pagesImmobility: 1. Scientific Knowledge BaseJharaNo ratings yet
- Psyche SupplementDocument51 pagesPsyche SupplementAchilles YbarraNo ratings yet
- OLD MidtermsDocument55 pagesOLD MidtermsCee JayNo ratings yet
- Adolescent History and Physical Examination FormDocument10 pagesAdolescent History and Physical Examination Formjosephtimbol123No ratings yet
- Guide of Experimental AnimalsDocument339 pagesGuide of Experimental Animalsmifta huljannahNo ratings yet
- College of Our Lady of Mt. Carmel (Pampanga) : Course SyllabusDocument4 pagesCollege of Our Lady of Mt. Carmel (Pampanga) : Course Syllabus;'SiLeNt';No ratings yet
- 2023 Health Assessment Exam 1 NotesDocument3 pages2023 Health Assessment Exam 1 NotesbaileyalexisjonesNo ratings yet
- Pe1 Midterm ExamDocument2 pagesPe1 Midterm ExamKris TelNo ratings yet
- Gen Psych Outline 1Document7 pagesGen Psych Outline 1Brittany NicoleNo ratings yet
- University of The CordillerasDocument2 pagesUniversity of The Cordillerasmj Canilang100% (1)
- PG 1 !4050Document30 pagesPG 1 !4050Dr.Parikshit Mahimkar MD (Hom.)No ratings yet
- FC 105 - Outline Scope PrelimsDocument6 pagesFC 105 - Outline Scope PrelimsSally SomintacNo ratings yet
Physiatric Assessment
Physiatric Assessment
Uploaded by
Daniel Andry KurniawanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Physiatric Assessment
Physiatric Assessment
Uploaded by
Daniel Andry KurniawanCopyright:
Available Formats
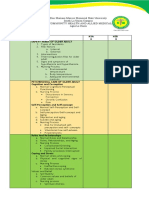
I.
PATIENT HISTORY
1. Chief report of symptoms.
a. OLDCART.
2. History of present illness.
3. History of past illness.
4. Functional history.
a. Communication.
b. Bathing.
c. Dressing.
d. Toileting.
e. Transferring.
f. Going to toilet.
g. Eating & drinking.
5. Personal history.
a. Psychological & psychiatric history.
b. Diet.
c. Drinking, smoking and drug.
6. Social history.
7. Vocational history.
a. Vocational ADL.
b. Avocational ADL.
8. Family history.
II. PHYSICAL EXAMINATION
1. Vital sign & general appearance.
2. Head-to-toe examination.
3. Musculoskeletal:
a. Inspection.
b. Palpation.
c. Muscle strength testing.
d. ROM assessment.
e. Joint stability.
III. NEUROLOGIC EXAMINATION
1. Level of consciousness:
a. Orientasi & Memori.
b. Konsentrasi & Kalkulasi.
c. Intelegensi baca & tulis.
d. Tilikan diri.
e. Coping & Stressor.
2. Cranial nerves.
3. Physiologic and pathologic reflexes.
4. Motoric & sensoric examination.
5. Equilibrium examination.
IV. FUNCTIONAL STATUS EXAMINATION
V. SUMMARY
You might also like
- Test Bank For Abnormal Psychology 5th Canadian Edition by BarlowDocument37 pagesTest Bank For Abnormal Psychology 5th Canadian Edition by BarlowNancy Medez100% (41)
- Ab Psy Test BankDocument155 pagesAb Psy Test BankGabrielle Anne AbadNo ratings yet
- Child Case History Taking PDFDocument6 pagesChild Case History Taking PDFSarika Varshney100% (4)
- Townsend Workbook Answers OnlyDocument25 pagesTownsend Workbook Answers OnlygioNo ratings yet
- Bioethics SyllabusDocument10 pagesBioethics Syllabusmei_15ph83% (6)
- AP Psych Practice Questions - Unit 1Document1 pageAP Psych Practice Questions - Unit 1dms727No ratings yet
- Overview of Pediatric Physical AssessmentDocument7 pagesOverview of Pediatric Physical AssessmentLloyd Jay Lin100% (1)
- PE1 1st Quarter Pre-TestDocument2 pagesPE1 1st Quarter Pre-TestJanine Bisenio-Betchayda100% (1)
- NCM 101 - Health Assessment SyllabusDocument2 pagesNCM 101 - Health Assessment SyllabusRA100% (3)
- Review of The Nursing ProcessDocument2 pagesReview of The Nursing Processmarkkkkkkkheeess100% (1)
- Guidelines Normal Assessment Day 1 Day 2: I. Mental StatusDocument7 pagesGuidelines Normal Assessment Day 1 Day 2: I. Mental StatusEllyn Rose Cardente ManiwangNo ratings yet
- Saint Francis of Assisi College College of NursingDocument4 pagesSaint Francis of Assisi College College of NursingCarolyn CalupitanNo ratings yet
- т2Document4 pagesт2Ploy SmileNo ratings yet
- Lecture Objectives & OutlinesDocument25 pagesLecture Objectives & OutlinesFelmerPolancoRodaNo ratings yet
- Modules 1-8 Answer To Guides QuestionsDocument15 pagesModules 1-8 Answer To Guides QuestionsBlackblight •No ratings yet
- Antisocial NcaDocument71 pagesAntisocial NcaCharisse CaydanNo ratings yet
- Patient Health History TakingDocument6 pagesPatient Health History Takingrose_roxasNo ratings yet
- Patient Assessment: 3Document6 pagesPatient Assessment: 3axmedfare138No ratings yet
- Guidelines Normal Assessment Day 1 Day 2: I. Mental StatusDocument7 pagesGuidelines Normal Assessment Day 1 Day 2: I. Mental StatusEllyn Rose Cardente ManiwangNo ratings yet
- Clinical Skills Study GuideDocument58 pagesClinical Skills Study GuideAngelica Mae Dela CruzNo ratings yet
- Oral - Internal 3rd YearDocument68 pagesOral - Internal 3rd Yearps886rd6chNo ratings yet
- Reporting Finals N3-ABDocument3 pagesReporting Finals N3-ABKrisia Mhel Buyagao MollejonNo ratings yet
- NCM 100 Course OutlineDocument3 pagesNCM 100 Course Outline배기숭100% (1)
- Behavioral Analysis:: Bipolar DisorderDocument2 pagesBehavioral Analysis:: Bipolar DisorderMary Angel Diaz AlejandroNo ratings yet
- BhhuOSaETLGYbjkmhHyxOQ - 3. Approach To The Sick Patient HandoutDocument5 pagesBhhuOSaETLGYbjkmhHyxOQ - 3. Approach To The Sick Patient HandoutStrahinja ŠkoboNo ratings yet
- Trial MCQ MHBS 4013Document15 pagesTrial MCQ MHBS 4013Muhammad ArifNo ratings yet
- Fundamentals of Nursing ContentDocument2 pagesFundamentals of Nursing ContentBasty BautistaNo ratings yet
- Aleli Q1 Lifestyle LPDocument3 pagesAleli Q1 Lifestyle LPMCarl F. ClycyNo ratings yet
- Specific Objectives Content Time Allotment Teaching Strategies Evaluative MeasuresDocument5 pagesSpecific Objectives Content Time Allotment Teaching Strategies Evaluative Measureslez2No ratings yet
- Examination of The Psychiatric Patient (Notes)Document3 pagesExamination of The Psychiatric Patient (Notes)Regine GlydelNo ratings yet
- Review of Related Literature OutlineDocument1 pageReview of Related Literature Outlineangela_nehNo ratings yet
- Pscyhe - Collantes - Module 1Document10 pagesPscyhe - Collantes - Module 1Eller Tacud CollantesNo ratings yet
- Psyceh - Collantes - Module 4.-UpdatedDocument14 pagesPsyceh - Collantes - Module 4.-UpdatedEller Tacud CollantesNo ratings yet
- Instructions: Select The Most Appropriate ResponseDocument3 pagesInstructions: Select The Most Appropriate ResponseJodi-Ann RobertsNo ratings yet
- Mapeh 1st QuarterDocument5 pagesMapeh 1st QuarterNunag Mary AnnNo ratings yet
- Template Psychosocial AssessmentDocument3 pagesTemplate Psychosocial AssessmentMark ApeladasNo ratings yet
- I. Vital InformationDocument7 pagesI. Vital InformationAlecNo ratings yet
- Acute Gastroenteritis With Severe DehydrationDocument22 pagesAcute Gastroenteritis With Severe DehydrationCess Dunwan100% (1)
- Abpsy ReviewerDocument15 pagesAbpsy ReviewerMARIE ROSE L. FUNTANARNo ratings yet
- Pe Summative TestDocument2 pagesPe Summative TestErica DelapenaNo ratings yet
- Abnormal Psychology 6th Edition Nolen Hoeksema Solutions ManualDocument35 pagesAbnormal Psychology 6th Edition Nolen Hoeksema Solutions Manualuncutresortpxb0k3100% (44)
- NURS124 OxygenationDocument11 pagesNURS124 Oxygenationmarie100% (4)
- RSPT 324 - Gen. PathologyDocument5 pagesRSPT 324 - Gen. PathologyNestor BalboaNo ratings yet
- 24 Sample TestDocument1 page24 Sample TestIvy Marie ToyonganNo ratings yet
- Gordon's Functional Health Pattern FormDocument6 pagesGordon's Functional Health Pattern FormMichael Bon MargajaNo ratings yet
- Abnormal Psychology TESTDocument6 pagesAbnormal Psychology TESTShiela maeNo ratings yet
- Immobility: 1. Scientific Knowledge BaseDocument3 pagesImmobility: 1. Scientific Knowledge BaseJharaNo ratings yet
- Psyche SupplementDocument51 pagesPsyche SupplementAchilles YbarraNo ratings yet
- OLD MidtermsDocument55 pagesOLD MidtermsCee JayNo ratings yet
- Adolescent History and Physical Examination FormDocument10 pagesAdolescent History and Physical Examination Formjosephtimbol123No ratings yet
- Guide of Experimental AnimalsDocument339 pagesGuide of Experimental Animalsmifta huljannahNo ratings yet
- College of Our Lady of Mt. Carmel (Pampanga) : Course SyllabusDocument4 pagesCollege of Our Lady of Mt. Carmel (Pampanga) : Course Syllabus;'SiLeNt';No ratings yet
- 2023 Health Assessment Exam 1 NotesDocument3 pages2023 Health Assessment Exam 1 NotesbaileyalexisjonesNo ratings yet
- Pe1 Midterm ExamDocument2 pagesPe1 Midterm ExamKris TelNo ratings yet
- Gen Psych Outline 1Document7 pagesGen Psych Outline 1Brittany NicoleNo ratings yet
- University of The CordillerasDocument2 pagesUniversity of The Cordillerasmj Canilang100% (1)
- PG 1 !4050Document30 pagesPG 1 !4050Dr.Parikshit Mahimkar MD (Hom.)No ratings yet
- FC 105 - Outline Scope PrelimsDocument6 pagesFC 105 - Outline Scope PrelimsSally SomintacNo ratings yet