Professional Documents
Culture Documents
Multitrauma Burn and Hi
Multitrauma Burn and Hi
Uploaded by
Harastha Khairi Afina0 ratings0% found this document useful (0 votes)
4 views8 pagesThis scenario involves the management of two trauma patients. The first is a 33-year-old male brought to the ED after being rescued from a house fire, who has significant burns to 30% of his total body surface area. The second is a 55-year-old male arriving from an altercation at a bar with a blunt head injury. Learners will be expected to recognize the need for airway management and fluid resuscitation in the burn patient, as well as treat potential complications including carbon monoxide poisoning and difficult ventilation requiring escharotomy. They will also need to identify and treat hypoglycemia in the head injury patient with a declining mental status. Management of both patients simultaneously tests crisis resource management and
Original Description:
Burn
Original Title
multitrauma-burn-and-hi
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis scenario involves the management of two trauma patients. The first is a 33-year-old male brought to the ED after being rescued from a house fire, who has significant burns to 30% of his total body surface area. The second is a 55-year-old male arriving from an altercation at a bar with a blunt head injury. Learners will be expected to recognize the need for airway management and fluid resuscitation in the burn patient, as well as treat potential complications including carbon monoxide poisoning and difficult ventilation requiring escharotomy. They will also need to identify and treat hypoglycemia in the head injury patient with a declining mental status. Management of both patients simultaneously tests crisis resource management and
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
4 views8 pagesMultitrauma Burn and Hi
Multitrauma Burn and Hi
Uploaded by
Harastha Khairi AfinaThis scenario involves the management of two trauma patients. The first is a 33-year-old male brought to the ED after being rescued from a house fire, who has significant burns to 30% of his total body surface area. The second is a 55-year-old male arriving from an altercation at a bar with a blunt head injury. Learners will be expected to recognize the need for airway management and fluid resuscitation in the burn patient, as well as treat potential complications including carbon monoxide poisoning and difficult ventilation requiring escharotomy. They will also need to identify and treat hypoglycemia in the head injury patient with a declining mental status. Management of both patients simultaneously tests crisis resource management and
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 8
Multi-trauma: Burn + Head Injury 1
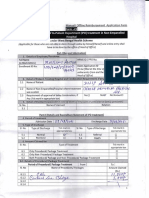
Section I: Scenario Demographics
Scenario Title: Multi-trauma Burn + Head Injury
Date of Development: 29/04/2016 (DD/MM/YYYY)
Target Learning Group: Juniors (PGY 1 – 2) Seniors (PGY ≥ 3) All Groups
Section II: Scenario Developers
Scenario Developer(s): Donika Orlich (adapted from “Two Patient Trauma” by Martin Kuuskne)
Affiliations/Institution(s): McMaster University
Contact E-mail (optional): Donika.orlich@medportal.ca
Section III: Curriculum Integration
Learning Goals & Objectives
EducationalCase
Goal:Summary:
To exposeBrief Summary
learners to a dualof Casecase
patient Progression and Major
which includes a severeEvents
burn patient
The case will begin with requiring
the arrival escharotomy.
of patient from a house fire who has 30%TBSA burns. The team will be
expected to recognize the1)
CRM Objectives: need for intubation
Demonstrates
References
and
resource fluid resuscitation.
utilization Afterfor
by calling successful intubation, a second
help appropriately,
Marx, J. A., Hockberger, R. S., Walls, R. M., & Adams, J. (2013). Rosen's emergency medicine: Concepts and clinical practice. St. Louis: Mosby.
patient will arrive from an altercation delegatingoutside a bar.needed
tasks when He appears to have apatients
and triaging blunt traumatic
appropriatelyhead injury after
Website: Trauma.org. Accessed May 2, 2016. Emergency Department Thoracotomy. http://www.trauma.org/index.php/main/article/361/
being repeatedly kicked. 2) TheCommunicates
team is expected to recognize
clearly hypoglycemia in the
with an inter-professional teamcontext
duringof handover
a minor head over
injury and provide immediatepatient glucose replacement. During the
care and during patient management management of the head injured patient,
the burn Objectives:
Medical patient will continue to by hypotensive.
1) Initiates appropriateThe team will
work-up and need to recognize
treatment the possibility
for suspected of CN
CO/CN poisoning
toxicity. The patient will also become more difficult to ventilate and will require an
2) Recognizes the potential for a difficult intubation and plans accordingly escharotomy.
3) Considers escharotomy in a difficult to ventilate burn patient and performs
the procedure
4) Recognizes hypoglycemia in the altered patient with HI and initiates
treatment
Section IV: Scenario Script
© 2015 EMSIMCASES.COM Page 1
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Multi-trauma: Burn + Head Injury 2
A. Clinical Vignette: To Read Aloud at Beginning of Case
Patient A: “You are working in a tertiary care ED. A 33 year old male has just been brought in by EMS after
being dragged out of a house fire. He has been unresponsive with EMS and has significant burns to his
chest, arm, and leg. The etiology of the fire is unclear, but the home was severely damaged.”
Midway through the case, Patient B will arrive with EMS:
Patient B: “55 year old male, repeatedly kicked during an altercation outside a bar. GCS 15 on arrival, but
just decreased to 13 in the ambulance bay, and he has become combative. C-spine collar applied
immediately. Lots of bruising to face/head, but no other obvious injuries. Patient denied other medical
history or allergies initially”.
B. Scenario Cast & Realism
Patients: Computerized Mannequin Realism: Conceptual
For both patients Mannequin Physical
Standardized Patient Select most Emotional/Experiential
Hybrid important Other:
Task Trainer dimension(s) N/A
Confederates Brief Description of Role
Paramedic To give HPI upon transfer of 2nd patient (as scripted above).
Nurse x2 To assist with cues to patient status, medication administration, etc. (One nurse per
patient will be required to run case smoothly)
C. Required Monitors
EKG Leads/Wires Temperature Probe Central Venous Line
NIBP Cuff Defibrillator Pads Capnography
Pulse Oximeter Arterial Line Other:
D. Required Equipment
Gloves Nasal Prongs Scalpel
Stethoscope Venturi Mask Tube Thoracostomy Kit
Defibrillator Non-Rebreather Mask Cricothyroidotomy Kit
IV Bags/Lines Bag Valve Mask Thoracotomy Kit
IV Push Medications Laryngoscope Central Line Kit
PO Tabs Video Assisted Laryngoscope Arterial Line Kit
Blood Products ET Tubes Other:
Intraosseous Set-up LMA Other:
E. Moulage
Patient A: Soot on face, singed eyebrows. Fake burns to chest/back, right arm/abdomen/leg
(circumferential to chest). C-collar in situ. (Note: can moulage burns with black garbage bag stuffed with
red bubble wrap and tissue paper so that students can “cut” for escharotomy)
Patient B: Bruising/contusions over face and head. Missing front tooth.
F. Approximate Timing
Set-Up: 5 min Scenario: 20 min Debriefing: 40 min
Section V: Patient Data and Baseline State- PATIENT A
© 2015 EMSIMCASES.COM Page 2
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Multi-trauma: Burn + Head Injury 3
A. Clinical Vignette: To Read Aloud at Beginning of Case
“You are working in a tertiary care ED. A 33 year old male has just been brought in by EMS after being
dragged out of a house fire. He has been unresponsive with EMS and has significant burns to his chest, arm,
and leg. The etiology of the fire is unclear, but the home was severely damaged. Last vitals: HR 120, BP
130/80, RR 30, O2 95% NRB. GCS 3 entire time with them, tolerating an oral airway.”
B. Patient Profile and History
Patient Name: Shawn Sherman Age: 33 Weight: 70
Gender: M F Code Status: Full
Chief Complaint: burns, aLOC
History of Presenting Illness: As above. Pulled from a house fire.
Past Medical History: Unknown Medications: Unknown
Allergies: None known.
Social History: Unknown
Family History: Unknown.
Review of Systems: CNS: Unable
HEENT: Unable
CVS: Unable
RESP: Unable
GI: Unable
GU: Unable
MSK: Unable INT: Unable
C. Baseline Simulator State and Physical Exam
No Monitor Display Monitor On, no data displayed Monitor on Standard Display
HR: 130/min BP: 90/70 RR: 30/min O2SAT: 95% NRB
Rhythm: sinus tach with T: 36.1 Co
Glucose: 6.1 mmol/L GCS: 3 (E 1 V 1 M1)
multiple PVCs
General Status: Unresponsive.
CNS: GCS 3. Pupils 3mm bilat, minimally reactive.
HEENT: No signs HI. Soot on face. Singed eyebrows.
CVS: Nil.
RESP: GAEB. No adventitious.
ABDO: Abdo soft, NT.
GU: Nil.
MSK: No signs trauma. Pelvis stable. SKIN: Burns to entire chest/back, R arm, R leg.
© 2015 EMSIMCASES.COM Page 3
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Multi-trauma: Burn + Head Injury 4
Section VI: Scenario Progression –Patient A
Scenario States, Modifiers and Triggers
Patient State Patient Status Learner Actions, Modifiers & Triggers to Move to Next State
1. Baseline State Unresponsive Learner Actions Modifiers
Rhythm: Sinus tach + with GCS 3. - 2 large bore IVs, bolus 2L Changes to patient condition based on
frequent PVCs - 100% O2, monitors learner action
HR: 130/min - Labs: VBG, carboxyHb, lactate, - 2L IVF HR 120, BP 120/80
BP: 90/70 coags, trop, G&S, INR
RR: 30/min - Check glucose: 6.3 Triggers
For progression to next state
O2SAT: 96 % NRB - Portable CXR/PXR
- Intubate 2. Intubation
T: 36.1oC - Full exposure re. TBSA
- 7 minutes 3. Critical VBG
- US FAST exam
2. Intubation Unchanged. Learner Actions Modifiers
HR: 120 - Push dose pressors at bedside - NE started BP 95/75
BP: 90/70 - Consider apneic oxygenation - Propofol used BP 60/30 (BP
RR: 30/min - Difficult airway cart 80/50 if NE started)
O2SAT: 93 % NRB - Surgical airway kit at bedside - Any other agent used BP 80/60
- Consider 1st look before
paralytic Triggers
- Anesthesia consult - Intubation complete
3. Critical VBG
**PATIENT B ARRIVES
3. Critical VBG Unchanged. Learner Actions Modifiers
HR: 100 - Ensure patient on 100% O2 - No hydroxycobalamin given 5 min
BP: 80/60 - Continue IVF to replace 3rd into state RN to prompt “isn’t
RR: 12/min vented space loses there some medicine you give when
O2SAT: 95% - Start vasopressor if not already people are in a fire?”
done
- Hydroxycobalamin 5mg IV Triggers
- ± Na thiosulfate 12.5g IV - Hydroxycobalamin given
- ± Call Poison Centre 4. Ventilator Alarming
4. Ventilator “High pressure” Learner Actions Modifiers
Alarming alarms on vent - Disconnect vent and attempt - Manual decompression no
HR: 110 and difficult to manual BVM change
BP: 90/50 vent or bag. - Consider US for PTX or needle - Escharotomy “improved ease of
RR: 12/min vented Nurse to help decompression ventilation”, O2 95%
O2SAT: 85% prompt re: vent - Manual decompression of chest
alarms for high - Escharotomy Triggers
pressure. - Escharotomy 5. Resolution
- No escharotomy by 20mins
END CASE
5. Resolution Patient Learner Actions
HR: 110 remains - Call ICU/Plastics ICU arrives to manage patient
BP: 100/50 unresponsive. - Call Poison Centre
RR: 12/min vented - ± Call for hyperbarics END CASE
O2SAT: 85%
© 2015 EMSIMCASES.COM Page 4
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Multi-trauma: Burn + Head Injury 5
Section VII: Supporting Documents, Laboratory Results, & Multimedia – Patient A
Laboratory Results
VBG pH: 6.98 PCO2: 28 PO2: 40 HCO3: 6 Lactate: 11
Carboxyhgb: 0.4
© 2015 EMSIMCASES.COM Page 5
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Multi-trauma: Burn + Head Injury 6
Section VIII: Patient Data and Baseline State - PATIENT B
A. Patient Profile and History
Patient Name: Michael Bissidy Age: 55 Weight: 150kg
Gender: M F Code Status: Unknown
Chief Complaint: Head injury
History of Presenting Illness: Patient involved in altercation outside a bar. Bystanders report the patient
was repeatedly kicked in the head/face after stabbing another person. Initially GCS 15 with EMS, but
decreased to GCS 13 as they pulled up to the hospital and became ++ agitated pulling out IV.
Past Medical History: Hypertension Medications: Hydrochlorothiazide
Dyslipidemia Atorvastatin
Diabetes Metformin
Insulin
Allergies: nil
Social History: unknown
Review of Systems: CNS: Initially complaining of headache to EMS. Now unable.
HEENT: “Face hurts”
CVS: No complaints.
RESP: No complaints.
GI: No complaints.
GU: No complaints.
MSK: No complaints. INT: No complaints.
B. Baseline Simulator State and Physical Exam
No Monitor Display Monitor On, no data displayed Monitor on Standard Display
HR: 90 /min BP: 120/80 RR: 20/min O2SAT: 99% RA
Rhythm: sinus T: 35.6 C
o
Glucose: 2.6 mmol/L GCS: 13 (E4 V4 M5)
General Status: Very large muscular/obese man. Combative. Swearing
CNS: Seems confused. ++ Agitated.
HEENT: Significant bruising over left orbit/jaw, bleeding nose, laceration to scalp with hematoma
(bleeding controlled)
CVS: Palpable, strong, tachycardic, pulse in all extremities. No murmurs. Normal heart sounds
RESP: GAEB, no adventitious sounds
ABDO: Normal
GU: Normal
MSK: No extremity deformities SKIN: Bruising/laceration to head & face
© 2015 EMSIMCASES.COM Page 6
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Multi-trauma: Burn + Head Injury 7
Section IX: Scenario Progression –Patient B
Scenario States, Modifiers and Triggers
Patient State Patient Status Learner Actions, Modifiers & Triggers to Move to Next State
1. Baseline State GCS – 13 Learner Actions Modifiers
Rhythm: NSR Seems - Call for security/back-up Changes to patient condition
HR: 110/min confused. - IM sedation based on learner action
BP: 120/78 - Monitor, full vitals - IM sedation -> settles over 1
RR: 20/min Patient is very - Establish IV access min
O2SAT: 99 % RA agitated, - Take history from EMS - If eFAST done negative
T: 35.6oC swearing and - Perform primary survey - If team decides needs imaging
trying to get off - Check sugar: 2.6 mmol/L radiology will ask who to
EMS stretcher - Replace glucose with D50 image first
and pull off his - Send trauma labs
c-spine collar. - ± eFAST Triggers
- Progress to secondary For progression to next state
Patient is survey - If cap sugar not checked by 5
collared. - Determine need for min 2. Seizure
further imaging (CT head, C- - If sugar replaced, primary
spine films) survey complete
3. Normal GCS
2. Seizure Patient has Learner Actions Modifiers
HR: 145 tonic/clonic - Check sugar: 2.6 mmol/L - If preparing to intubate, RN to
BP: 140/75 seizure. - Replace glucose with D50 ask: “should we check a sugar
RR: 12 - Arrange for CT head first?”
- Consider other causes of
seizure/aLOC Triggers
- Glucose replaced 3. Normal
GCS
3. Normal GCS GCS 15 Learner Actions
HR: 90/min Patient alert - Send trauma labs
BP: 110/78 and oriented - ± eFAST END CASE PRN
RR: 18/min - Progress to secondary
O2SAT: 99 % survey
- Determine need for
further imaging (CT head, C-
spine films)
Section X: Supporting Documents, Laboratory Results, & Multimedia – Patient B
Laboratory Results - Patient B
Not available
© 2015 EMSIMCASES.COM Page 7
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Multi-trauma: Burn + Head Injury 8
Section XI: Debriefing Guide
Images (ECGs, CXRs, etc.)
Patient B – CXR General Debriefing Plan
Patient B – Normal Pelvic Xray
Individual Group With Video Without Video
Objectives
Educational Goal: To expose learners to a dual patient case which includes a severe burn
patient requiring escharotomy.
CRM Objectives: 1) Demonstrates resource utilization by calling for help appropriately,
delegating tasks when needed and triaging patients appropriately
2) Communicates clearly with an inter-professional team and taking and
giving effective handover
Medical Objectives: 1) Initiates appropriate work-up and treatment for suspected CO/CN
poisoning
2) Recognizes the potential for a difficult intubation and plans
accordingly PXR source:
3) Considers escharotomy in a difficult to ventilate burn patient and
http://radiopaedia.org/articles/pelvis-1
CXR source: performs the procedure
4) Recognizes hypoglycemia in the altered patient with HI and initiates
http://www.pharmacology2000.com/respiratory_a
nesthesiology/pulmonary_assessment/treatment
pulmonary_assessment2.htm Sample Questions for Debriefing
1. How was the decision made to split the team and resources? Do you think it was done well?
2. What was the team leader’s leadership style? Did it change when the second patient arrived?
3. What difficulties are faced when using resources for a trauma involving multiple patients?
4. What are the indications for an escharotomy?
Key Moments
1) Recognition that the team must be split to appropriately manage both patients.
2) Recognition of hypoglycemia as the cause for aLOC in patient B
3) Identification of CN as cause for persistent hypotension
4) Recognition of circumferential burns as the cause for high ventilator pressures
5) Decision to perform escharotomy
© 2015 EMSIMCASES.COM Page 8
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
You might also like
- UNBFAC Student Handbook enDocument32 pagesUNBFAC Student Handbook enOmed B.Mohamad HasanNo ratings yet
- DLR - Tips and TricksDocument9 pagesDLR - Tips and Tricksxvart3251No ratings yet
- Closing-The-Gap Action Plan - SycamoreDocument1 pageClosing-The-Gap Action Plan - Sycamoreapi-496518967No ratings yet
- Burn NCLEXDocument17 pagesBurn NCLEXMonica JubaneNo ratings yet
- U World - Questions and RatioDocument11 pagesU World - Questions and RatioCharisse TaylanNo ratings yet
- Cirurgia Plastica Queimados Livro2Document18 pagesCirurgia Plastica Queimados Livro2Joao FonsecaNo ratings yet
- CHApter 57Document18 pagesCHApter 572071317No ratings yet
- Emergency Nursing Exam and RatioDocument5 pagesEmergency Nursing Exam and RatioCharisse TaylanNo ratings yet
- NCM 120 Lec Disaster Triage ManagementDocument6 pagesNCM 120 Lec Disaster Triage ManagementHeist LadaoNo ratings yet
- Pattern and Categorisation of Neurosurgical Emergencies: Conference ProceedingDocument3 pagesPattern and Categorisation of Neurosurgical Emergencies: Conference ProceedingarshadNo ratings yet
- Tumor Lysis Syndrome1Document7 pagesTumor Lysis Syndrome1czalesky66No ratings yet
- MGT 489 Final Exam Submission Document: Section: 18 Student Name: Samrin HassanDocument8 pagesMGT 489 Final Exam Submission Document: Section: 18 Student Name: Samrin HassanSamrin HassanNo ratings yet
- PBL Shock Ko BaiDocument11 pagesPBL Shock Ko BaiHaronsHutchSabellinaNo ratings yet
- Burns Open: Christoph Wallner, Peter Kern, Norbert Teig, Marcus Lehnhardt, Björn BehrDocument4 pagesBurns Open: Christoph Wallner, Peter Kern, Norbert Teig, Marcus Lehnhardt, Björn BehrferaNo ratings yet
- Quemaduras Parte 2Document8 pagesQuemaduras Parte 2maxifamous6No ratings yet
- 48 Art IngDocument6 pages48 Art IngEmily YuliethNo ratings yet
- BURNS - Surgery Trans2Document9 pagesBURNS - Surgery Trans2JAMPTNo ratings yet
- Trauma 2018 BMJDocument8 pagesTrauma 2018 BMJLuis JaraNo ratings yet
- 12Document13 pages12Tyson Easo JonesNo ratings yet
- A Critical Updated of The Assessmente and Acute Management If Patients With Severe BurnsDocument27 pagesA Critical Updated of The Assessmente and Acute Management If Patients With Severe BurnsCarlos Javier SolorzaNo ratings yet
- Wound Management 2017Document9 pagesWound Management 2017Carlos DNo ratings yet
- EMERGENCY RESPONSE AND RESCUE PLAN Burn InjuryDocument2 pagesEMERGENCY RESPONSE AND RESCUE PLAN Burn InjuryHutomo 75No ratings yet
- Disaster Risk Reduction Management LectureDocument19 pagesDisaster Risk Reduction Management LectureJames Joseph ObispoNo ratings yet
- Hyperbaric Oxygen Therapy For A Pediatric Electrical BurnDocument3 pagesHyperbaric Oxygen Therapy For A Pediatric Electrical Burnsarah iriamanaNo ratings yet
- Classic HyperthermiaDocument10 pagesClassic HyperthermiaoalabdulhadiNo ratings yet
- Jurnal CombusDocument4 pagesJurnal CombusnikitagustiNo ratings yet
- Critical Care Set UpDocument33 pagesCritical Care Set UpSam TullyNo ratings yet
- Lesson Plan TRIAGEDocument8 pagesLesson Plan TRIAGEDebasree sahaNo ratings yet
- Initial Management of A Major BurnDocument3 pagesInitial Management of A Major BurnSandy GaresNo ratings yet
- Ursing ARE LAN: Short Term Goal: Independent Intervention: Independent InterventionDocument2 pagesUrsing ARE LAN: Short Term Goal: Independent Intervention: Independent InterventionGiselle EstoquiaNo ratings yet
- Chapter 57Document10 pagesChapter 572071317No ratings yet
- Impact of Nursing Rehabilitation Program On Minimizing Post - Burn Joint ContractureDocument15 pagesImpact of Nursing Rehabilitation Program On Minimizing Post - Burn Joint ContractureIJAR JOURNALNo ratings yet
- Critical Care Management of Patients With Severe Burns and InhalationalDocument5 pagesCritical Care Management of Patients With Severe Burns and Inhalationaljorge saavedra chiraNo ratings yet
- Management Luka BakarDocument24 pagesManagement Luka BakarVega CandraNo ratings yet
- Principles of Hospital Disaster PlanningDocument6 pagesPrinciples of Hospital Disaster PlanningArdaNo ratings yet
- Venturina NCPSDocument5 pagesVenturina NCPSYsabelle VenturinaNo ratings yet
- Burns - Surgery Trans1Document3 pagesBurns - Surgery Trans1JAMPTNo ratings yet
- Challenges in Anaesthesia and Pain Management For Burn InjuriesDocument13 pagesChallenges in Anaesthesia and Pain Management For Burn InjuriesArif Setyo WibowoNo ratings yet
- Pediatric Septic ShockDocument6 pagesPediatric Septic ShockSugi DenyNo ratings yet
- Content Woundcare Effective Skin and Wound Management of Non-Complex Burns BestPracticeGuidelinesDocument28 pagesContent Woundcare Effective Skin and Wound Management of Non-Complex Burns BestPracticeGuidelinesBayu Pratama PutraNo ratings yet
- Acute Respiratory Distress: Section I: Scenario DemographicsDocument6 pagesAcute Respiratory Distress: Section I: Scenario DemographicsharasthaNo ratings yet
- 4.nursing Management in DisasterDocument15 pages4.nursing Management in Disastersari arie lestariNo ratings yet
- Essentials of Hyperbaric Oxygen Therapy: 2019 ReviewDocument4 pagesEssentials of Hyperbaric Oxygen Therapy: 2019 ReviewMahipal Reddy NimmalaNo ratings yet
- Hospital Response To A Major Incident: Initial Considerations and Longer Term EffectsDocument5 pagesHospital Response To A Major Incident: Initial Considerations and Longer Term EffectsMinaz PatelNo ratings yet
- COVID-19 Pandemic Mental Health Risks Among Anesthesiologists: It Is Not Only BurnoutDocument3 pagesCOVID-19 Pandemic Mental Health Risks Among Anesthesiologists: It Is Not Only BurnoutCristhian AndresNo ratings yet
- Case Study, Chapter 73, Terrorism, Mass Casualty, and Disaster NursingDocument1 pageCase Study, Chapter 73, Terrorism, Mass Casualty, and Disaster Nursingclyde i amNo ratings yet
- Chapter 56 Preoperative and Postoperative CareDocument6 pagesChapter 56 Preoperative and Postoperative CareReymon RodriguezNo ratings yet
- Clinical Casuality ManagementDocument6 pagesClinical Casuality ManagementswathiprasadNo ratings yet
- Celulas MesenquimalesDocument6 pagesCelulas MesenquimalesDIOGENESNo ratings yet
- 2018 - 06 - 18 BMJ The Trauma CallDocument8 pages2018 - 06 - 18 BMJ The Trauma CallBeaulah HunidzariraNo ratings yet
- Management of The Patient With A Burn InjuryDocument43 pagesManagement of The Patient With A Burn InjuryAshraf HusseinNo ratings yet
- Comprehensive Care Plan TemplateDocument4 pagesComprehensive Care Plan Templateapi-572974227No ratings yet
- Scientific Analysis Goal: Goal:: Subjective CuesDocument2 pagesScientific Analysis Goal: Goal:: Subjective CuesChloie Marie RosalejosNo ratings yet
- Burn Injury: General Surgery Department, FKUI/RSCM, Jakarta, Indonesia, May 2011Document8 pagesBurn Injury: General Surgery Department, FKUI/RSCM, Jakarta, Indonesia, May 2011DeVi K. NinGsihNo ratings yet
- NCP Stab Wound (Artillo)Document7 pagesNCP Stab Wound (Artillo)Al TheóNo ratings yet
- Evaluation of Emotional Excitation During Standardized Endotracheal Intubation in Simulated Conditionsannals of Intensive CareDocument8 pagesEvaluation of Emotional Excitation During Standardized Endotracheal Intubation in Simulated Conditionsannals of Intensive CareRoberto SanchezNo ratings yet
- Acute Burn Care.41Document20 pagesAcute Burn Care.41Gabrielle Fávaro HolandaNo ratings yet
- Chinese Nursing Research: Research Progress in Disaster Nursing Competency Framework of Nurses in ChinaDocument4 pagesChinese Nursing Research: Research Progress in Disaster Nursing Competency Framework of Nurses in ChinaSyahrizal FahmiantoNo ratings yet
- Emergent Conditions (Triage and CPR)Document4 pagesEmergent Conditions (Triage and CPR)mikErlhNo ratings yet
- NCM 106 Rle Module 2Document26 pagesNCM 106 Rle Module 2Esmareldah Henry SirueNo ratings yet
- Single Visit EndodonticsDocument5 pagesSingle Visit EndodonticsSreena VenugopalanNo ratings yet
- NCP Disturbed Sleep PatternDocument2 pagesNCP Disturbed Sleep Patterncharmaine3469% (13)
- 1.0 Responsibilities and Emergency OrganisationDocument7 pages1.0 Responsibilities and Emergency OrganisationKL PetrachkovNo ratings yet
- Img 20210502 0001Document4 pagesImg 20210502 0001anirbanpwd76No ratings yet
- Practices That Promote Comprehensive School Safety: ArticleDocument10 pagesPractices That Promote Comprehensive School Safety: ArticleOyam MendozaNo ratings yet
- Sai Khelo IndiaDocument7 pagesSai Khelo IndiaPiyush kumarNo ratings yet
- Reading & Writing Week 7Document17 pagesReading & Writing Week 7Joseph ChristianNo ratings yet
- Intelligence Testing: Aachal P. TaywadeDocument30 pagesIntelligence Testing: Aachal P. TaywadeJohn Lexter Rosales100% (1)
- PYC3705 Merged NotesDocument56 pagesPYC3705 Merged Notesjadie leeNo ratings yet
- A Study On Grivence Management in Improving Employees in A Privete EnterpriseDocument52 pagesA Study On Grivence Management in Improving Employees in A Privete Enterpriseavinash bulusuNo ratings yet
- 4.employee Motivation ProjectDocument53 pages4.employee Motivation ProjectAdeel AhmadNo ratings yet
- NURS 6512 Advanced Health Assessment FInal ExamDocument19 pagesNURS 6512 Advanced Health Assessment FInal ExamtroillerdrippyNo ratings yet
- Evaluation One Elementary1 JanuaryDocument8 pagesEvaluation One Elementary1 JanuaryCarlos MinanoNo ratings yet
- Ch2 P1 Utilitarianism SVDocument21 pagesCh2 P1 Utilitarianism SVK57 PHAN QUOC THANHNo ratings yet
- Maternity MOH 333 PDFDocument4 pagesMaternity MOH 333 PDFMajivaNo ratings yet
- Clean Form Planche ProgramDocument7 pagesClean Form Planche ProgramAbderrahman TalebNo ratings yet
- Narrative Review of The LiteratureDocument5 pagesNarrative Review of The Literature우즈무즈No ratings yet
- Senior High School Department: Caldwell Adventist AcademyDocument3 pagesSenior High School Department: Caldwell Adventist Academyrosanie remotinNo ratings yet
- Journey of Adulthood 8th Edition Ebook PDFDocument61 pagesJourney of Adulthood 8th Edition Ebook PDFhenrietta.hallquist413100% (52)
- ICU Manual - Nodrm by Prem KumarDocument865 pagesICU Manual - Nodrm by Prem Kumarssipon118No ratings yet
- Tibial and Femur FactrueDocument25 pagesTibial and Femur Factruesingireddi1revathiNo ratings yet
- Company ProfileDocument5 pagesCompany ProfileJongabantu NgcuthusheNo ratings yet
- Beckman Price List 2017xlsxDocument12 pagesBeckman Price List 2017xlsxSkymedicalairEngenhariaMedicaNo ratings yet
- Brain Break GameDocument2 pagesBrain Break GameManisha MishraNo ratings yet
- LESSON EXEMPLAR IN TleDocument2 pagesLESSON EXEMPLAR IN TleChe'che Inabangan Icawalo100% (3)
- 4.double Standard of MoralityDocument12 pages4.double Standard of MoralityIvy DumadaraNo ratings yet
- Project Report: Feed The Future India Triangular Training Program OnDocument66 pagesProject Report: Feed The Future India Triangular Training Program OnSourav GhoshNo ratings yet
- Standard For Dried Floral Parts: Cloves CXS 344-2021Document5 pagesStandard For Dried Floral Parts: Cloves CXS 344-2021KHALIDNo ratings yet