Professional Documents
Culture Documents
Pneumothorax
Pneumothorax
Uploaded by
Andrei MurariuOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pneumothorax
Pneumothorax
Uploaded by
Andrei MurariuCopyright:
Available Formats
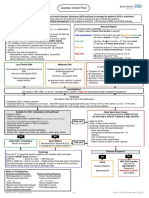
Emergency Department NUH
Pneumothorax
This pathway is only for management of spontaneous pneumothorax ie not related to trauma
Primary pneumothorax = no underlying lung disease
Secondary pneumothorax = underlying lung disease (eg COPD, asthma, TB, malignancy, age > 50 years and
significant smoking history, evidence of underlying lung disease on exam or CXR)
Contraindications to needle aspiration Technique Safe Triangle
· Signs of tension pneumothorax Staff must be competent or supervised by person Between lateral edges of pectoralis major
· Haemodynamically unstable competent in procedure and latissimus dorsi, above the 5th
· Bilateral pneumothoraces intercostal space and below the base of
· Previous pneumothorax within last 2 BEWARE BULLAE the axilla
weeks
· Complete NatSIP checklist & document consent
· Anticoagulated - await INR unless
· Aseptic technique
emergency
· Site: Safe triangle (unless contraindicated eg
· Ventilated patient
extensive scarring – then use 2nd space anteriorly)
· Aspiration: 14 – 16 G cannula, stop when no more
air can be aspirated or 2.5 L aspirated
· Drain: 8 -14 Fr, take care when inserting dilator;
aim drain upwards
· Immediate repeat CXR
Primary Pneumothorax Secondary Pneumothorax
No DIB DIB DIB No DIB No DIB
AND AND / OR AND / OR AND AND
< 2cm rim of air on CXR > 2 cm rim of air on CXR > 2 cm rim of air on CXR 1 – 2 cm rim of air on < 1 cm rim of air on CXR
(measure at level of hilum) (unless senior decision to CXR
observe only)
Put onto high flow oxygen unless COPD) in which case given oxygen to target sats to 88-92%
Contraindications to Contraindications to
Yes Yes
needle aspiration? needle aspiration?
No No
Consider needle aspiration Consider needle aspiration
(50% success rate) (50% success rate)
Aspiration adequate? Aspiration adequate?
breathing improved, rim < 2 cm No breathing improved, rim < 1 cm
No
(do not repeat aspiration unless (do not repeat aspiration unless
technical difficulties) technical difficulties)
Yes
Admit CDU
Insert Seldinger Chest Drain Yes
Prescribe O2
Complete procedure checklist
PRN analgesia
Check CXR after insertion
Observe 2 hours
Is patient suitable for discharge?
Remains asymptomatic for 2 hours Secondary Pneumothorax: Admit
Refer to Medical reg bleep 4627
Yes
Discharge Primary Pneumothorax with chest drain: Admit to CDU
Refer to Chest clinic
· Complete OPA referral form including patient contact · Observe for bubbling every hour – document when stops
phone number · Observe for 4 hours from when bubbling in drain stops
· Print discharge letter for notes · Repeat CXR at 4 hours from when bubbling stops, prior to removing drain
· If CXR normal and no DIB, remove drain and observe for further 1 hour
Ensure patient has the following: · Discharge with advice and chest clinic OPA
· Copy of GP letter
· Patient advice leaflet Refer to Medical SpR if:
· Bubbling persists for more than 4 hours
Discharge advice (Give patient advice sheet):
· Persisting DIB
· Return immediately if breathless or chest pain
· Bubbling restarts within 4 hours of stopping
· Avoid diving – for life
· Persisting pneumothorax on check CXR
· Avoid air travel until further advice in chest clinic
· Surgical emphysema
DO NOT CLAMP DRAIN
EM Network Guideline Group v6 July 2018 [review July 2021]
Emergency Department NUH
Pneumothorax
Lead Author
Consultant Emergency Medicine
Co-Authors / Collaborators
Consultant Respiratory Medicine
Reference Documents
Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline
2010. Thorax 2010; 65 (Suppl 2):ii18-ii31. doi:10.1136/thx.2010.136986
Pleural procedures and thoracic ultrasound: British Thoracic Society pleural disease guideline 2010.
Thorax 2010; 65 (Suppl 2):ii61-ii76. doi:10.1136/thx.2010.137026
EM Network Guideline Group v6 July 2018 [review July 2021]
You might also like
- DR Breath by Carl Stough PDFDocument128 pagesDR Breath by Carl Stough PDFJuan Vizán86% (7)
- Reading Test #32 (Thursday) - MergedDocument28 pagesReading Test #32 (Thursday) - MergedPiper Parker0% (1)
- Med Surg Notes 3Document6 pagesMed Surg Notes 3Ivy NguyenNo ratings yet
- Emphysema Case Study E3Document28 pagesEmphysema Case Study E3scarletsky1975% (8)
- Respiratory Diseases Chapter From Nelson Textbook of PediatricsDocument312 pagesRespiratory Diseases Chapter From Nelson Textbook of PediatricsMilan Andrejevic100% (1)
- Pneumothorax Part ADocument4 pagesPneumothorax Part ASoji0% (1)
- PPP Reading Test 11 Part A TextsDocument4 pagesPPP Reading Test 11 Part A TextsDaniah Marwan Dawood DAWOODNo ratings yet
- Medical Surgical Nursing Module 14Document31 pagesMedical Surgical Nursing Module 14weissNo ratings yet
- Assessment: Suctioning An Adult Patient With An Artificial AirwayDocument2 pagesAssessment: Suctioning An Adult Patient With An Artificial Airwayeunike FriciliaNo ratings yet
- Table of Comparison On Cardiopulmonary Resuscitation For Adul1Document1 pageTable of Comparison On Cardiopulmonary Resuscitation For Adul1Luigi GeduqueNo ratings yet
- AiepiDocument12 pagesAiepiRenzo Iván Marín DávalosNo ratings yet
- Non Invasive VentilationDocument58 pagesNon Invasive VentilationsachinNo ratings yet
- Lung Recruitment in General AnesthesiaDocument2 pagesLung Recruitment in General AnesthesiaIda SutawanNo ratings yet
- Medical Surgical Nursing Module 17Document31 pagesMedical Surgical Nursing Module 17weissNo ratings yet
- Uued Coivd 19mgmt Guide For Publication 9 - 15 - 2020Document29 pagesUued Coivd 19mgmt Guide For Publication 9 - 15 - 2020JorgeNo ratings yet
- Apa3 Cicv FinalDocument1 pageApa3 Cicv FinalRhany Ariesti IndryaniNo ratings yet
- Comprehensive Life Support Tutorial Case 1: Question/Action Information Note/Reference TipsDocument3 pagesComprehensive Life Support Tutorial Case 1: Question/Action Information Note/Reference Tipshyukkie minnieNo ratings yet
- Lung - PathophysiologyDocument66 pagesLung - PathophysiologyjmosserNo ratings yet
- Emergency Department Bronchiolitis Care Guideline: Inclusion CriteriaDocument3 pagesEmergency Department Bronchiolitis Care Guideline: Inclusion CriteriaPatricia KoikyNo ratings yet
- Spontaneous Pneumothorax - Management Feb15Document12 pagesSpontaneous Pneumothorax - Management Feb15samuelNo ratings yet
- PneumothoraxDocument45 pagesPneumothoraxLuknut Nuttamon NukaeowNo ratings yet
- Als2010 NewDocument185 pagesAls2010 NewMuhammad JazibNo ratings yet
- Mechanical VentilationDocument27 pagesMechanical VentilationAnne CamilleNo ratings yet
- Nursing Care Plan Thyroid CancerDocument2 pagesNursing Care Plan Thyroid CancerKathleen DimacaliNo ratings yet
- Spiro Me TryDocument13 pagesSpiro Me TryfatimaabedulkhalikturkeyNo ratings yet
- Application HFOV in NICU - Lily RundjanDocument43 pagesApplication HFOV in NICU - Lily Rundjandiah ayu pitalokaNo ratings yet
- ICU One Pager ARDS v1.1Document1 pageICU One Pager ARDS v1.1Michael LevitNo ratings yet
- Bronchiolitis: See AlsoDocument6 pagesBronchiolitis: See AlsoJuleides De LeonNo ratings yet
- Pulmo Case Simulation-TEAM Yellow-Blue - 01-04-21Document35 pagesPulmo Case Simulation-TEAM Yellow-Blue - 01-04-21Jolaine ValloNo ratings yet
- 5 Advanced Resu PDFDocument22 pages5 Advanced Resu PDFBeatrice Joy TombocNo ratings yet
- OxygenationDocument3 pagesOxygenationFritz MirandaNo ratings yet
- 10.5 Tracheostomies - Clinical Procedures For Safer Patient CareDocument31 pages10.5 Tracheostomies - Clinical Procedures For Safer Patient CareMeg AqNo ratings yet
- TSCUH Trachy Bed Head PDFDocument4 pagesTSCUH Trachy Bed Head PDFTudistef Analize SanatateNo ratings yet
- Respi Hema NotesDocument16 pagesRespi Hema NotesLucky GomezNo ratings yet
- Potential Conflicts of InterestDocument8 pagesPotential Conflicts of InterestLina GuerraNo ratings yet
- Excess or Deficit in Oxygenation And/or Carbon Dioxide Elimination at The Alveolar-Capillary MembraneDocument6 pagesExcess or Deficit in Oxygenation And/or Carbon Dioxide Elimination at The Alveolar-Capillary MembraneHazel MiraranNo ratings yet
- Non Invasive Positive Pressure Ventilation (NIPPV)Document39 pagesNon Invasive Positive Pressure Ventilation (NIPPV)api-3820606100% (1)
- Detresa Respiratorie NeonatalaDocument2 pagesDetresa Respiratorie NeonatalaAndrada CatrinoiuNo ratings yet
- Niv Vizag FinalDocument56 pagesNiv Vizag FinalPrakash PratimaNo ratings yet
- Anaesthetics NotesDocument15 pagesAnaesthetics NotesnaNo ratings yet
- RahpoDocument3 pagesRahpoassouma16052002No ratings yet
- PP Lung VolumesDocument30 pagesPP Lung VolumesAdam PrabowoNo ratings yet
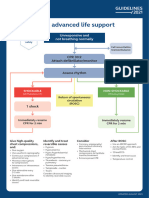
- Adult Advanced Life Support Algorithm 2021 Aug 2023Document1 pageAdult Advanced Life Support Algorithm 2021 Aug 2023cknihilnewNo ratings yet
- Presentasi Code Blue IGDDocument16 pagesPresentasi Code Blue IGDIgd Pondok TjandraNo ratings yet
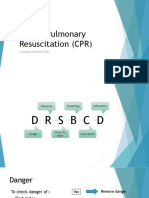
- CPR Guideline 2022Document12 pagesCPR Guideline 2022Wyndham WooNo ratings yet
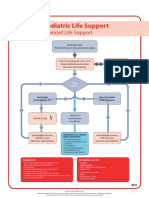
- PalsDocument1 pagePalslordroentgenNo ratings yet
- NCP CroupDocument3 pagesNCP Croupaurezea100% (3)
- S T A R T: Imple Riage ND Apid ReatmentDocument17 pagesS T A R T: Imple Riage ND Apid ReatmentNavine NavNo ratings yet
- BLS Healthcare Provider AlgorithmDocument7 pagesBLS Healthcare Provider AlgorithmyuniNo ratings yet
- Pneumothorax: Algorithm: Queen's Dect: KGH BleepDocument2 pagesPneumothorax: Algorithm: Queen's Dect: KGH BleepRachmi Merrina0% (1)
- Anesthesia For Laparoscopic SurgeryDocument14 pagesAnesthesia For Laparoscopic Surgeryhendrik taufikNo ratings yet
- Dean - Diagnostic 1 PDFDocument3 pagesDean - Diagnostic 1 PDFSophia GoNo ratings yet
- Poster 10 PALS 01 01 ENG V20100927 PDFDocument1 pagePoster 10 PALS 01 01 ENG V20100927 PDFAndy XiaoNo ratings yet
- NIV and HFNCDocument16 pagesNIV and HFNCMarceline GarciaNo ratings yet
- Respiratory Cram 6Document1 pageRespiratory Cram 6gwendolyn henryNo ratings yet
- Body CT - Chest HRCTDocument5 pagesBody CT - Chest HRCTKelum BuddhikaNo ratings yet
- Recovery Room Transfer Sheet44Document1 pageRecovery Room Transfer Sheet44Dr. Sumit Kumbhar0% (1)
- ABC AcuteCareDocument1 pageABC AcuteCareparkerNo ratings yet
- Triptico RCPDocument2 pagesTriptico RCPDenia Anguamea CalderónNo ratings yet
- 14.PNEUMOTHORAX + IC TubeDocument8 pages14.PNEUMOTHORAX + IC TubeLankeshwaraNo ratings yet
- 4-5 MV For COPD & AsthmaDocument45 pages4-5 MV For COPD & AsthmasalwafathiNo ratings yet
- RCP TripticoDocument2 pagesRCP Tripticoqg4r5srcnpNo ratings yet
- Hypertension: Hypertensive Emergency Hypertensive UrgencyDocument2 pagesHypertension: Hypertensive Emergency Hypertensive UrgencyAndrei MurariuNo ratings yet
- AsthmaDocument2 pagesAsthmaAndrei MurariuNo ratings yet
- Chest PainDocument5 pagesChest PainAndrei MurariuNo ratings yet
- Physiotherapeutic Management of Patients With Pregnancy-Related Pelvic Girdle PainDocument24 pagesPhysiotherapeutic Management of Patients With Pregnancy-Related Pelvic Girdle PainAndrei MurariuNo ratings yet
- Oxygen DeliveryDocument6 pagesOxygen Deliveryyourdirtysocks100% (1)
- 03 NCP 5 Pulmonary Tuberculosis LalitDocument17 pages03 NCP 5 Pulmonary Tuberculosis Lalitamit100% (2)
- Respiratory - Circulatory SystemDocument3 pagesRespiratory - Circulatory SystemClaude PeñaNo ratings yet
- Body PlathyDocument13 pagesBody PlathyWayanWahyuSemaraPutraNo ratings yet
- Negative Effects of SmokingDocument19 pagesNegative Effects of SmokingAnafemolyn NingascaNo ratings yet
- Worksheet ADocument3 pagesWorksheet AM Riel Cim AlbancesNo ratings yet
- GOLD Pocket 2017Document34 pagesGOLD Pocket 2017Giovanni MisseriNo ratings yet
- 1.chronic Illness Overview and COPDDocument12 pages1.chronic Illness Overview and COPDOmar IzzoNo ratings yet
- Covid - 19 NCPDocument4 pagesCovid - 19 NCPKrisianne Mae Lorenzo FranciscoNo ratings yet
- Question Bank X 202324 BiologyDocument9 pagesQuestion Bank X 202324 Biologyvaibhav4gameNo ratings yet
- 01 1 PDFDocument8 pages01 1 PDFpravikumar1989No ratings yet
- Critical Care Nursing A Holistic ApproachDocument84 pagesCritical Care Nursing A Holistic ApproachMildred GamboaNo ratings yet
- Respiratory Function TestDocument7 pagesRespiratory Function TestMarivic DianoNo ratings yet
- Predisposing Factors Disease Precipitating Factors: LegendDocument3 pagesPredisposing Factors Disease Precipitating Factors: LegendSOPHIA LOISE TEJANO FULACHENo ratings yet
- Airway-Anatomy: Maj Yuvraj Issar Resident Oral & Maxillofacial SurgeryDocument83 pagesAirway-Anatomy: Maj Yuvraj Issar Resident Oral & Maxillofacial SurgeryBhanu PraseedhaNo ratings yet
- Exercise Science and The VocalistDocument10 pagesExercise Science and The VocalistVoz UGM100% (1)
- Worksheet - Week 6 - ANSWERSDocument6 pagesWorksheet - Week 6 - ANSWERSstudent4007No ratings yet
- NCP - Or-Rotation 2Document12 pagesNCP - Or-Rotation 2Vian RiveraNo ratings yet
- Thoracocentesis: Nadja E. SigristDocument4 pagesThoracocentesis: Nadja E. SigristDwi AnaNo ratings yet
- PSLE Science 2020 Booklet ADocument16 pagesPSLE Science 2020 Booklet Asgdogman1212No ratings yet
- Wheezing From PCODocument23 pagesWheezing From PCOShan KaiNo ratings yet
- EXAM 3 20210405 C11 NUR310G.C Health Assessment PDFDocument37 pagesEXAM 3 20210405 C11 NUR310G.C Health Assessment PDFCeciliaNo ratings yet
- Vocabulary Listening Speaking Reading WritingDocument9 pagesVocabulary Listening Speaking Reading Writingnimat rasyidNo ratings yet
- Respiratory SystemhjhuDocument23 pagesRespiratory SystemhjhuSara ANo ratings yet
- MTV1000 - PNEUMACARE (Eng) PDFDocument2 pagesMTV1000 - PNEUMACARE (Eng) PDFNhật LongNo ratings yet
- Breathing - Herbert M. SheltonDocument1 pageBreathing - Herbert M. Sheltonraweater75% (4)
- Avian and Exotic Animal AnesthesiaDocument46 pagesAvian and Exotic Animal AnesthesiaManecas TianeNo ratings yet