Professional Documents
Culture Documents
Yang2018 - Skizofrenia Referat
Yang2018 - Skizofrenia Referat
Uploaded by
Febelina IdjieOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Yang2018 - Skizofrenia Referat
Yang2018 - Skizofrenia Referat
Uploaded by
Febelina IdjieCopyright:
Available Formats
Polypharmacy and psychotropic drug loading in patients with schizophrenia in
Asian countries: The REAP-AP4 study
Shu-Yu Yang, PhD,1 Lian-Yu Chen, MD, PhD,1 Eunice Najoan, MD,2 Roy Abraham
Kallivayalil, MD,3 Kittisak Viboonma, MD,4 Ruzita Jamaluddin, MD,5 Afzal Javed,
MD,6 Duong Thi Quynh Hoa, MD,7 Hitoshi Iida, MD,8 Kang Sim, MD,9 Thiha Swe,
MD,10 Yan-Ling He, MD,11 Yongchon Park, MD,12 Helal Uddin Ahmed, MD,13
Angelo De Alwis, MD,14 Helen Fung-Kum Chiu, MD,15 Norman Sartorius, MD,
PhD,16 Chay-Hoon Tan, MD,17 Mian-Yoon Chong, MD, PhD,18 Naotaka Shinfuku,
Accepted Article
MD, PhD,19 Shih-Ku Lin, MD,1,20*
1
Taipei City Hospital and Psychiatric Center, Taipei, Taiwan, 2Mintoharjo Hospital,
Jakarta, Indonesia, 3Pushpagiri Institute of Medical Sciences, Tiruvalla, Kerala,
India, 4Suanprung Psychiatric Hospital, Chian Mai, Thailand, 5Department of
Psychiatry & Mental Health, Hospital Tuanku Fauziah, Kangar, Perlis, Malaysia, 6
Pakistan Psychiatric Research Centre, Fountain House, Lahore, Pakistan, 7Thanh
Hoa Provincial Psychiatric Hospital, Thanh Hoa, Vietnam, 8Department of
Psychiatry, Faculty of Medicine, Fukuoka University, Fukuoka, Japan, 9Institute of
Mental Health, Buangkok Green Medical Park, Singapore, 10 Department of Mental
Health, University of Medicine, Magway, Myanmar, 11Department of Psychiatric
Epidemiology, Shanghai Mental Health Center, Shanghai, China, 12Department of
Psychiatry, Hanyang University, Seoul, Korea, 13National Institute of Mental Health,
Dhaka, Bangladesh, 14National Institute of Mental Health, Angoda, Sri Lanka,
15
Department of Psychiatry, Chinese University of Hong Kong, Hong Kong SAR,
China, 16Association for the Improvement of Mental Health Programs, Geneva,
Switzerland, 17National University of Singapore, Singapore.18Chiayi Chang Gung
Memorial Hospital and School of Medicine, Chang Gung University, Chiayi, Taiwan,
19
School of Human Sciences, Seinan Gakuin University, Fukuoka, Japan,
20
Department of Psychiatry, School of Medicine, Taipei Medical University, Taipei,
Taiwan
*
Correspondence: Shih-Ku Lin, MD, Taipei City Hospital and Psychiatric Center
309 Songde Road, Taipei 110, Taiwan. E-mail: sklin@tpech.gov.tw
Tel: +88627263141
Running Title: Polypharmacy and PDL in REAP-AP4
This article has been accepted for publication and undergone full peer review but has not
been through the copyediting, typesetting, pagination and proofreading process, which
may lead to differences between this version and the Version of Record. Please cite this
article as doi: 10.1111/pcn.12676
This article is protected by copyright. All rights reserved.
Abstract
Aim: The aim of the present study was to survey the prevalence of antipsychotic
polypharmacy and combined medication use across 15 Asian countries and areas in
Accepted Article
2016.
Methods: By using the results from the fourth survey of Research on Asian
Prescription Patterns on antipsychotics (REAP-AP4), the rates of polypharmacy and
combined medication use in each country were analyzed. Daily medications
prescribed for the treatment of inpatients or outpatients with schizophrenia,
including antipsychotics, mood stabilizers, anxiolytics, hypnotics, and antiparkinson
agents, were collected. Fifteen countries from Asia participated in this study.
Results: A total of 3744 patients’ prescription form were examined. The prescription
patterns differed across these Asian countries, with the highest rate of polypharmacy
noted in Vietnam (59.1%) and the lowest in Myanmar (22.0%). Furthermore, the
highest rate and the lowest rate of combined use of mood stabilizers was China
(35.0%) and Bangladesh (1.0%), antidepressants South Korea (36.6%) and
Bangladesh (0%), anxiolytics Pakistan (55.7%) and Myanmar (8.5%), hypnotics
Japan (61.1%) and Myanmar and Sri Lanka (0%), and antiparkinson agents
Bangladesh (87.9%) and Vietnam (10.9%), respectively. The average psychotropic
drug loading of all patients was 2.01 ± 1.64, with the highest and lowest loadings
This article is protected by copyright. All rights reserved.
noted in Japan (4.13 ± 3.13) and Indonesia (1.16 ± 0.68), respectively.
Conclusion: Differences in psychiatrist training as well as the civil culture and
health insurance system of each country may have contributed to the differences in
Accepted Article
these rates. The concept of drug loading can be applied to other medical field.
Key words: antipsychotic loading, combined medication, polypharmacy,
psychotropic drug loading, schizophrenia
This article is protected by copyright. All rights reserved.
Introduction
The term polypharmacy is originally coined to refer to problems related to multiple
drug consumption and excessive drug use during treatment of a disease or disorder.1
Accepted Article
In the treatment of schizophrenia, polypharmacy usually refers to the simultaneous
use of two or more antipsychotic medications, and combined (adjunct) medications
as the use of mood stabilizers, antidepressants, anxiolytics, or hypnotics in addition
to single or multiple antipsychotics. Ideally, a clinician should administer
monotherapy of an antipsychotic to treat schizophrenia; however, some proportions
of patients respond to this treatment suboptimally.2 Thus, polypharmacy and
combined medications are frequently applied in clinical practice. The prevalence of
polypharmacy varies among countries: It is lower in North American countries, such
as the United States3-5 and Canada,6 and Europe such as United Kingdom,7 but higher
in Asian countries, such as Japan and Singapore.8, 9 Because it is expensive with
unproven efficacy and several side effects, the use of antipsychotic polypharmacy
used to be discouraged and avoided.10 However, recent data suggested that
antipsychotic polypharmacy and combined medications has been shown to be
helpful in some patients.11, 12
The Research on Asian Prescription Patterns (REAP) is an international
collaborative consortium for studying prescription patterns of psychotropic drugs
This article is protected by copyright. All rights reserved.
across countries. This consortium has conducted three surveys on antipsychotics
(REAP-AP1, -AP2, and -AP3 in 2001, 2004, and 2009, respectively) and two on
antidepressants (REAP-AD1 and -AD2 in 2004 and 2013, respectively;
Accepted Article
http://reap.asia/index.html). The rate of antipsychotic polypharmacy has been
reported in previous surveys.8, 13 The present study was the fourth REAP survey on
antipsychotics (REAP-AP4), and we report herein on the prevalence of
antipsychotic polypharmacy and combined medication use across 15 Asian countries
and areas.
Methods
Design and participants
For data collection, this study used an online website-based data key-in system. The
research protocol can be accessed at http://reap.asia/reap_ap.html#reap_ap4. In brief,
data on the daily medications prescribed for treating inpatients or outpatients with
schizophrenia, including antipsychotics, mood stabilizers, antidepressants,
anxiolytics, hypnotics, and antiparkinson agents, and demographics were collected.
Fifteen Asian countries and areas, namely China, Hong Kong, Japan, South Korea,
Singapore, Taiwan (REAP-AP1–3), India, Thailand, Malaysia (REAP-AP3),
Bangladesh, Indonesia, Myanmar, Pakistan, Sri Lanka, and Vietnam, participated in
This article is protected by copyright. All rights reserved.
this study, which took place between March 1, 2016 and May 31, 2016. Because no
established definition of polypharmacy has been reported,14 here we referred to
polypharmacy as the use of two or more antipsychotics, and combined medications
Accepted Article
as the additional use of other psychotropic drugs in the treatment of schizophrenia.
The use of a long-acting injectable antipsychotic combined with the same drug in
oral form was considered monotherapy. The prevalence of antipsychotic
polypharmacy and combined medications of each psychotropic drug were analyzed.
Conventionally, a chlorpromazine equivalent is used to compare the therapeutic
dose of an antipsychotic.15-17 Because newer antipsychotics, such as iloperidone,
lurasidone, and paliperidone, do not have a chlorpromazine equivalent,18 the defined
daily dose (DDD) system is a useful and reliable tool for international drug
utilization studies19 for comparison with either other antipsychotics alone or
combined with other medications. Here, the antipsychotic loading index was
calculated using the sum of the prescribed daily dose (PDD) of each antipsychotic,
divided by its DDD to indicate the quantity of antipsychotic drugs received by a
patient. Accordingly, psychotropic drug loading (PDL) was used to represent the
medication quantity prescribed to treat a mental disorder. For schizophrenia,
psychotropic drugs comprise five pharmacological classes of drugs, namely
antipsychotics, mood stabilizers, antidepressants, anxiolytics, and hypnotics; these
This article is protected by copyright. All rights reserved.
drugs are administered to treat the core and peripheral schizophrenia symptoms,
such as delusions, hallucinations, agitated or aggressive behaviors, anxious or
depressive mood, and insomnia. PDL is the sum of each psychotropic drug’s PDD
Accepted Article
divided by its DDD in the five pharmacological classes. Based on the dose
information obtained from the Anatomical Therapeutic Chemical (ATC)
Classification System (i.e., the ATC/DDD Index 2016), DDD was considered to be
the assumed average maintenance dose per day for a drug used for its main
indication in an adult weighing 70 kg (https://www.whocc.no/atc_ddd_index/
[accessed 15 September 2016]).20 The ATC/DDD system is a tool used for
exchanging and comparing data on drug use at international, national, or local levels
and has become the gold standard for international drug utilization research. For
instance, if a patient receives a daily dose of aripiprazole 15 mg, valproic acid 750
mg, and lorazepam 2 mg, the PDL will be (15/15) +(750/1500) + (2/2.5) = 2.3. We
calculated the PDL of each enrolled patient and compared the results between
countries.
This REAP-AP4 study was approved by the Institutional Review Board (IRB)
of Taipei City Hospital (TCHIRB-10412128-E) for data collection in this hospital
and management of all data sets. For remaining regions, IRB approval was obtained
from individual study sites.
This article is protected by copyright. All rights reserved.
Statistical analyses
We used SPSS for Windows (version 20; IBM Corp., Armonk, NY, USA) for
Accepted Article
computing study data. Here, the samples are reported as numbers and percentages as
well as means ± standard deviations (SDs). A chi-square test was then used to
compare the four cohorts of the REAP-AP. Statistical significance was set at p <
0.05.
Results
In total, 3744 patients with schizophrenia (1950 inpatients, 1794 outpatients; 2200
men) were enrolled. The numbers and demographics of each country are presented
in Table 1, where countries are listed in order of the number of patients enrolled. The
mean age was 39.5 ± 13.1 years, with the oldest patients in Singapore (48.1 ± 13.7
years) and the youngest in Bangladesh (31.9 ± 11.0 years). The mean body weight
was 62.9 ± 13.8 kg, with highest patient weights in Hong Kong (71.8 ± 15.4 kg) and
the lowest in Bangladesh (52.2 ± 12.4 kg). The mean body mass index was 23.8 ±
4.6.
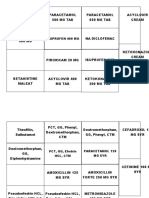
Table 2 shows the numbers and rates of antipsychotic polypharmacy and
This article is protected by copyright. All rights reserved.
combined medication use in each country, with the red and blue cells containing
more than and less than 1 SD, respectively. The antipsychotic polypharmacy rate
ranged from 22.0% (Myanmar) to 59.1% (Vietnam), with a mean rate of 42.2% ±
Accepted Article
12.0%. The mean number of antipsychotics used was 1.5 ± 0.6, with the highest
numbers obtained from Japan (1.8 ± 0.9) and the lowest numbers obtained from
Myanmar (1.2 ± 0.4). The most used antipsychotic was risperidone (36.9%),
followed by olanzapine (20.5%), clozapine (18.5%), haloperidol (15.5%),
chlorpromazine (8.4%), quetiapine (7.9%), aripiprazole (5.6%), and trifluoperazine
(4.0%).
Notably, there was a large variation in the rates of combined medication use
across countries. A comparison of the polypharmacy and drug loading between
inpatients and outpatients is outlined in Table 3.
Figure 1 illustrates the comparison of polypharmacy rates across countries,
from the REAP-AP1 to REAP-AP48, and Figure 2 depicts the comparison of PDL
and antipsychotic loading between the countries. The mean PDL of all patients was
2.01 ± 1.64, with the highest and lowest loadings occurring in Japan (4.1.3 ± 3.13)
and Indonesia (1.16 ± 0.68), respectively.
Discussion
This article is protected by copyright. All rights reserved.
The mean rate of antipsychotic polypharmacy in Asian countries was 42.2%
(although with considerable variation among the countries), indicating that
Accepted Article
polypharmacy is still widely prescribed for patients with schizophrenia in these
locations compared with Western countries.5-7
Compared with previous REAP-AP surveys8 (45.6% in 2001, 37.4% in 2004,
42.3% in 2009), the rate here showed no apparent significant change. However,
during the course of the four surveys, the rate has consistently decreased to 55.0%
from 78.1% in Japan (χ2 = 60.8, df = 3), to 52.6% from 70.3% in Singapore (χ2 =
22.9, df =3) and to 25.7% from 45.9% in India (χ2 = 24.9, df = 1; all p < 0.001). In
Japan, the use of high doses of antipsychotics and polypharmacy has been
conventionally prevalent.21, 22 To reduce the high rate of polypharmacy, psychotropic
dose equivalence has been suggested for dose standardization; in addition, the public
insurance reimbursement system, drug reduction program, and pharmacist
intervention policies have been revised to improve and prevent psychotropic
polypharmacy.23-25 Our results indicated that the rate of polypharmacy has reduced in
recent years in Japan; nevertheless, among the Asian countries included here, Japan
still has the highest average number of antipsychotic use (1.8 ± 0.9) and
antipsychotic loading (2.29 ± 1.79).
This article is protected by copyright. All rights reserved.
Notably, the rate of polypharmacy increased only in China, from 25.0% in 2001,
23.2% in 2006, and 35.7% in 2009, to 52.5% in 2016 (χ2 = 63.4, df = 3, p < 0.001).
In a series survey, the frequency of polypharmacy significantly increased from
Accepted Article
26.1% (2002) and 26.4% (2006) to 34.2% in 2012 (p < 0.001) in China.26 The data
analysis in that study revealed that polypharmacy-administered patients and their
families had lower satisfaction with treatment, higher mental quality of life, earlier
onset age, more side effects, and higher antipsychotic doses; the patients were also
more likely to receive first-generation antipsychotics, but less likely to receive
benzodiazepines.
The mean antipsychotic loading was 1.50 ± 1.15 in all patients, which was
approximately equal to chlorpromazine (DDD, 300 mg) 450 mg/day or risperidone
(DDD, 5 mg) 7.5 mg/day. After further stratification (Table 3), inpatients (n = 1950)
showed a significantly higher rate of polypharmacy (49.1%), higher antipsychotic
loading, and more psychotropic loading than did outpatients. These differences were
attributed to higher illness severity among inpatients. Whether a difference exists
between Asian and Western countries in antipsychotic loading should be
investigated in future studies.
The large differences in combined medication use observed among countries
are difficult to explain. For instance, in Bangladesh, only 1 of 99 (1%) patients was
This article is protected by copyright. All rights reserved.
prescribed mood stabilizers; by contrast, 25.8% and 35.0% of the patients in
Pakistan and China, respectively, were prescribed mood stabilizers. The rate of
antidepressant use was less than 5% in Indonesia, Vietnam, Japan, Myanmar, and
Accepted Article
Bangladesh, but was 23.4%, 25.8%, and 36.6% in Singapore, Hong Kong, and South
Korea, respectively. More than half of the patients in Pakistan (55.7%) and Korea
(54.2%) were receiving anxiolytics, whereas this rate was considerably smaller in
Myanmar (8.5%) and Sri Lanka (9.3%). However, the most notable difference was
observed for the use of hypnotics. In most countries, hypnotics were rarely
prescribed, but the rate of their use was 61.1% and 36.5% in Japan and Taiwan,
respectively. Nevertheless, our pooled combined medication use rates were lower
than those recently reported for 961 patients with schizophrenia from the Eastern
European region (anxiolytics, 70%; antidepressants, 42%; mood stabilizers, 27%).27
Some explanations to account for these differences among countries have been
proposed, such as training backgrounds, availability of drugs, and reimbursement
systems. Although no guidelines have been established for antipsychotic
polypharmacy or combined medications in the treatment of schizophrenia, a subset
of patients still require such unconventional pharmacotherapy.28 In a special
article,29 polypharmacy and high-dose antipsychotics were proposed. Additional
studies are warranted to elucidate the ideal rate of polypharmacy and combined
This article is protected by copyright. All rights reserved.
psychotropic drug use.
In this study, we created a PDL index to represent the medication burden on
patients with schizophrenia. In the treatment of schizophrenia, we considered each
Accepted Article
class of drug to have the same weighting, in terms of efficacy and side effects. This
is similar to the disease severity assessment of schizophrenia by Positive and
Negative Syndrome Scale,30 in which the item of delusion or hallucinatory behavior,
has the same weighting to the item of anxiety or depression. Notably, Japan had a
higher rate of polypharmacy (55.0%) and the highest index of antipsychotic loading
(2.29 ± 1.79) and PDL (4.06 ± 3.05); by contrast, Vietnam had the highest rate of
polypharmacy (59.1%) and lower antipsychotic loading (1.77 ± 0.96) and PDL (2.09
± 1.11). This example reveals that a high rate of polypharmacy does not necessarily
indicate a high burden of psychotropic drugs. Thus, when reviewing a prescription
pattern in the treatment of schizophrenia, the evaluation of antipsychotic
polypharmacy rate, antipsychotic loading index, and global PDL is crucial.
The PDL index may be applied to any other psychiatric disorder; the concept of
drug loading may be also applied to other diseases, such as hypertension and
diabetic mellitus, where polypharmacy or combined medication use is prevalent.
The main perspectives of the REAP are comparing the differences in
prescription patterns across Asian countries and contributing to the improvement of
This article is protected by copyright. All rights reserved.
psychotropic drug prescription quality in the Asian countries that participate in this
collaborative consortium. Similar to the conception of a quality indicator project,31,32
a set of indicators can be developed by using these comparisons; the exact positions
Accepted Article
of these indicators can then be learned by clinicians and health administrators to
obtain consistent results. Thus, according to the REAP-AP4 data related to
schizophrenia pharmacotherapy in Asian countries, we suggest the ideal rate of
antipsychotic polypharmacy could be around 30%; the approximate rates in
combination with mood stabilizers, antidepressants, anxiolytics, and hypnotics could
be 15%, 10%, 30%, and 10%, respectively; furthermore, the antipsychotic loading
and PDL could be approximately 1.5 and 2.0, respectively.
In conclusion, the differences in prescription patterns in the treatment of
schizophrenia among countries and fluctuations in the results among the
REAP-AP1–4 may attribute to the diverse training backgrounds of psychiatrists,
civil culture, availability and cost of drugs, patient characteristics, and the local
health care reimbursement system of each country. For a prescriber treating
schizophrenia, the golden rule should be an adequate dose of antipsychotic, reducing
polypharmacy and combined medication as much as possible. The results from all of
the REAP-AP studies provide a basis to compare individual clinicians and countries,
facilitating a more suitable and reasonable prescription pattern. It also offers an
This article is protected by copyright. All rights reserved.
indicator of change of practice due to changes in the education of psychiatry and
other mental health systems interventions.
Accepted Article
Limitations
This study had several limitations: the convenient sampling method may have
incurred selection bias, patients underwent antipsychotic switching and dose
tapering, the numbers of patients enrolled from each country varied, no stratification
of illness severity was performed, and the ethnic diversity of the sample.
Nevertheless, the comparison of the four surveys may approximate trends of
antipsychotic polypharmacy and combined medications in the treatment of patients
with schizophrenia across Asian countries. Future research should employ a more
precise study design, and also investigate the effects of prescription patterns on
bipolar disorder or other minor psychiatric disorders, particularly by comparing
them with results from Western countries.
Acknowledgements
The authors thank Mr. Da-Yi Tsai for internet server maintenance and Mr. Yan-Lung
Chiou for assistance of data management. The authors are grateful to the following
This article is protected by copyright. All rights reserved.
clinicians involved in the data collection: Mekhala Sarkar in Bangladesh; Hao Wei
and Weifu Cai in China; Adarsh Tripathi, Ajit Avasthi, Sandeep Grover, Amitava
Dan and Arshad Hussain in India; Andi J Tanra, Elmeida Effendy, Margarita
Accepted Article
Maramis, Khamelia Malik, Isa Multazam, Santi Yuliani, Widodo Sarjana and Metta
Desvini in Indonesia; Toshiya Inada, Hiroaki Kawasaki, Kentaro Kira, Yuma Ogushi,
Shigenobu Kanba, Takahiro Kato, Hiroaki Kubo, Hironori Kuga, Nobutomo
Yamamoto, Futoshi Shintani, Hajime Iwatsuki, Hideki Horikawa and Mina
Sato-Kasai in Japan; Min-Soo Lee, Seon-Cheol Park and Yong-Chon Park in Korea;
Chee Kok Yoon, Loi-Fei Chin, Chee-Hoong Moey, Yee-Tieng Lee, Aida Mohd Arif,
Siong-Teck Wong, Syarifah Hafizah Wan Kassim, Selvasingam Ratnasingam and
Siti Salwa Ramly in Malaysia; Wing Aung Myint, Tin Oo, Bo Bo Nyan, Sun Lin,
Nyan Win Kyaw in Myanmar; M. Munir Hamirani, Imtiaz Dogar and Mazhar Malik
in Pakistan; Ee-Heok Kua and Johnson Fam in Singapore; Samudra Kathiarachchi,
Dulshika Wass and Thilini Rajapakse in Sri Lanka; Chi-Fa Hung, Tsung-Ming Hu,
Chih-Ken Chen, Wen-Chen Ouyang in Taiwan; Pichet Udomratn, Nopporn
Tantirangsee and Pairoj Sareedenchai in Thailand; Tran Van Cuong, La Duc Cuong,
Bui The Khanh, Nguyen Doan Phuong, Ngo Van Vinh, Ly Tran Tinh, Trinh Tat
Thang, Lam Tu Trung, Doan Hong Quang, Duong Thi Quynh Hoa, Trinh Van An
and Cao Tien Duc in Vietnam. We acknowledge Wallace Academic Editing
This article is protected by copyright. All rights reserved.
(www.editing.tw) for editing this manuscript.
DISCLOSURES STATEMENT
Accepted Article
This work was supported by Taipei City Government (10501-62-012). The authors
declare no conflict of interest in reporting this study.
AUTHOR CONTRIBUTIONS
N.S., M.Y.C., S.Y.Y., C.H.T., N.S., and S.K.L. designed the REAP-AP4 study and
wrote the protocol. L.Y.C., E.N., R.A.K., K.V., R.J., A.J., D.T.Q.H., H.I., K.S., T.S.,
Y.L.H., Y.P., H.U.A., A.D.A., H.F.K.C., recruited participants in different countries,
and S.Y.Y., and S.K.L. performed the statistical analyses and drafted the manuscript.
This article is protected by copyright. All rights reserved.
References
1. Friend DG. Polypharmacy; multiple-ingredient and shotgun prescriptions.
The New England journal of medicine 1959; 260: 1015-10188.
2. Kane JM, Correll CU. Past and present progress in the pharmacologic
treatment of schizophrenia. The Journal of clinical psychiatry 2010; 71:
Accepted Article
1115-1124.
3. Correll CU, Shaikh L, Gallego JA et al. Antipsychotic polypharmacy: a
survey study of prescriber attitudes, knowledge and behavior. Schizophrenia
research 2011; 131: 58-62.
4. Mojtabai R, Olfson M. National trends in psychotropic medication
polypharmacy in office-based psychiatry. Archives of general psychiatry
2010; 67: 26-36.
5. Fisher MD, Reilly K, Isenberg K, Villa KF. Antipsychotic patterns of use in
patients with schizophrenia: polypharmacy versus monotherapy. BMC
psychiatry 2014; 14: 341.
6. Procyshyn RM, Honer WG, Wu TK et al. Persistent antipsychotic
polypharmacy and excessive dosing in the community psychiatric treatment
setting: a review of medication profiles in 435 Canadian outpatients. The
Journal of clinical psychiatry 2010; 71: 566-573.
7. Kadra G, Stewart R, Shetty H et al. Predictors of long-term (>/=6months)
antipsychotic polypharmacy prescribing in secondary mental healthcare.
Schizophrenia research 2016; 174: 106-112.
8. Xiang YT, Wang CY, Si TM et al. Antipsychotic polypharmacy in inpatients
with schizophrenia in Asia (2001-2009). Pharmacopsychiatry 2012; 45:
7-12.
9. Ito C, Kubota Y, Sato M. A prospective survey on drug choice for
prescriptions for admitted patients with schizophrenia. Psychiatry and
clinical neurosciences 1999; 53 Suppl: S35-40.
10. Stahl SM. Antipsychotic polypharmacy, Part 1: Therapeutic option or dirty
little secret? The Journal of clinical psychiatry 1999; 60: 425-426.
11. Correll CU, Rummel-Kluge C, Corves C, Kane JM, Leucht S. Antipsychotic
combinations vs monotherapy in schizophrenia: a meta-analysis of
randomized controlled trials. Schizophrenia bulletin 2009; 35: 443-57.
12. Stahl SM. Antipsychotic polypharmacy: never say never, but never say
always. Acta psychiatrica Scandinavica 2012; 125: 349-351.
13. Sim K, Su A, Fujii S et al. Antipsychotic polypharmacy in patients with
schizophrenia: a multicentre comparative study in East Asia. British journal
of clinical pharmacology 2004; 58: 178-183.
This article is protected by copyright. All rights reserved.
14. Freudenreich O, Goff DC. Polypharmacy in schizophrenia: a fuzzy concept.
The Journal of clinical psychiatry 2003; 64: 1132; author reply 1132-1133.
15. Davis JM. Dose equivalence of the antipsychotic drugs. Journal of
psychiatric research 1974; 11: 65-69.
16. Woods SW. Chlorpromazine equivalent doses for the newer atypical
Accepted Article
antipsychotics. The Journal of clinical psychiatry 2003; 64: 663-667.
17. Leucht S, Samara M, Heres S, Patel MX, Woods SW, Davis JM. Dose
equivalents for second-generation antipsychotics: the minimum effective
dose method. Schizophrenia bulletin 2014; 40: 314-326.
18. Leucht S, Samara M, Heres S et al. Dose Equivalents for Second-Generation
Antipsychotic Drugs: The Classical Mean Dose Method. Schizophrenia
bulletin 2015; 41: 1397-1402.
19. Nose M, Tansella M, Thornicroft G et al. Is the Defined Daily Dose system a
reliable tool for standardizing antipsychotic dosages? International clinical
psychopharmacology 2008; 23: 287-290.
20. WHO Collaborating Centre for Drug Statistics Methodology AciwD, 2016.
Oslo, Norway 2015.
21. Takei N, Inagaki A, group J-r. Polypharmacy for psychiatric treatments in
Japan. Lancet 2002; 360: 647.
22. Shinfuku M, Uchida H, Tsutsumi C et al. How psychotropic polypharmacy
in schizophrenia begins: a longitudinal perspective. Pharmacopsychiatry
2012; 45: 133-137.
23. Inada T, Inagaki A. Psychotropic dose equivalence in Japan. Psychiatry and
clinical neurosciences 2015; 69: 440-447.
24. Hashimoto Y, Tensho M. Effect of pharmacist intervention on physician
prescribing in patients with chronic schizophrenia: a descriptive pre/post
study. BMC health services research 2016; 16: 150.
25. Yamanouchi Y, Sukegawa T, Inagaki A et al. Evaluation of the individual
safe correction of antipsychotic agent polypharmacy in Japanese patients
with chronic schizophrenia: validation of safe corrections for antipsychotic
polypharmacy and the high-dose method. The international journal of
neuropsychopharmacology 2014; 18.
26. Li Q, Xiang YT, Su YA et al. Antipsychotic polypharmacy in schizophrenia
patients in China and its association with treatment satisfaction and quality
of life: findings of the third national survey on use of psychotropic
medications in China. The Australian and New Zealand journal of psychiatry
2015; 49: 129-136.
27. Szkultecka-Debek M, Miernik K, Stelmachowski J et al. Treatment patterns
This article is protected by copyright. All rights reserved.
of schizophrenia based on the data from seven Central and Eastern European
Countries. Psychiatria Danubina 2016; 28: 234-242.
28. Stahl SM. Emerging guidelines for the use of antipsychotic polypharmacy.
Rev Psiquiatr Salud Ment 2013; 6:97-100
29. Moore BA, Morrissette DA, Meyer JM, Stahl SM. Drug information update.
Accepted Article
Unconventional treatment strategies for schizophrenia: polypharmacy and
heroic dosing. BJPsych Bull 2017, 41:164-168.30. Kay SR, Fiszbein A,
Opler LA. The positive and negative syndrome scale (PANSS) for
schizophrenia. Schizophrenia bulletin 1987; 13: 261-276.
31. Arah OA, Westert GP, Hurst J, Klazinga NS. A conceptual framework for the
OECD Health Care Quality Indicators Project. International journal for
quality in health care 2006; 18 Suppl 1: 5-13.
32. Carinci F, Van Gool K, Mainz J et al. Towards actionable international
comparisons of health system performance: expert revision of the OECD
framework and quality indicators. International journal for quality in health
care 2015; 27: 137-146
This article is protected by copyright. All rights reserved.
Figuure legends
Figuure 1. Compparison of polypharmaccy rates from
m the REAP
P-AP1 to REAP-AP4.
Accepted Article
This article is protected by copyright. All rights reserved.
Figuure 2. Compparison of psychotropic
p c drug loadiing betweenn countries; red bar
indiicates antipssychotic loaading and bllue bar indicates combined medicaations
loadding.
Accepted Article
This article is protected by copyright. All rights reserved.
Accepted Article
Table 1. Patient number and demographics in each country
South Sri Hong
Indonesia India Taiwan Thailand Malaysia Pakistan Vietnam Japan Singapore Myanmar China Bangladesh Total
n(%) Korea Lanka Kong
n= 581 479 403 322 305 298 274 229 171 164 160 131 99 97 31 3744
gender
Male 370 319 182 212 157 168 184 140 64 107 104 59 58 58 18 2200
( 63.7 ) ( 66.6 ) ( 45.2 ) ( 65.8 ) ( 51.5 ) ( 56.4 ) ( 67.2 ) ( 61.1 ) ( 37.4 ) ( 65.2 ) ( 65 ) ( 45 ) ( 58.6 ) ( 59.8 ) ( 58.1 ) ( 58.8 )
Female 211 160 221 110 148 130 90 89 107 57 56 72 41 39 13 1544
( 36.3 ) ( 33.4 ) ( 54.8 ) ( 34.2 ) ( 48.5 ) ( 43.6 ) ( 32.8 ) ( 38.9 ) ( 62.6 ) ( 34.8 ) ( 35 ) ( 55 ) ( 41.4 ) ( 40.2 ) ( 41.9 ) ( 41.2 )
Age
mean 34.9 36 47.6 39.3 39.3 36.9 38.7 46.5 48.1 37.6 39.7 40.5 31.9 40.4 38.8 39.5
SD 11.3 11.7 11.7 12.3 12.3 11.9 12 14.4 13.7 11.2 16.4 12.5 11.0 13.3 13.9 13.1
Body weight
mean 60.5 64.4 64.9 63.3 67.1 66.3 57.3 64.1 62.5 56.7 67.9 66.7 52.2 57.8 71.8 62.9
SD 12.8 11.9 15.5 13.2 16.5 13.6 10.1 14.2 13.9 10.1 13.0 13.2 12.4 10.2 15.4 13.8
BMI
mean 23.1 24.1 24.8 23.7 25.3 25.2 21.9 23.9 24.7 21.8 24.1 24.2 22.0 22.9 26.3 23.8
SD 4.7 4.4 4.9 4.5 5.1 5.2 3.5 4.3 5.0 3.6 3.8 3.8 4.0 3.4 5.5 4.6
This article is protected by copyright. All rights reserved.
Accepted Article
Table 2. Antipsychotic polypharmacy and combined medications
South Sri Hong
Indonesia India Taiwan Thailand Malaysia Pakistan Vietnam Japan Singapore Myanmar China Bangladesh Total
Korea Lanka Kong
N 581 479 403 322 305 298 274 229 171 164 160 131 99 97 31 3744
Polypharmacy (More than 1 antipsychotic)
N 234 123 109 175 132 154 162 126 90 36 84 60 45 41 9 1580
% (40.3) (25.7) (27.0) (54.3) (43.3) (51.7) (59.1) (55.0) (52.6) (22.0) (52.5) (45.8) (45.5) (42.3) (29.0) (42.2±12.0)
Number of Antipsychotic used
mean 1.4 1.3 1.3 1.7 1.5 1.6 1.6 1.8 1.6 1.2 1.6 1.6 1.5 1.5 1.3 1.5
SD 0.6 0.5 0.5 0.7 0.6 0.8 0.5 0.9 0.6 0.4 0.6 0.8 0.5 0.6 0.5 0.6
Antipsychotic loading (Sum of each antipsychotic’s PDD/DDD)
mean 1.00 1.33 1.39 1.39 1.43 1.79 1.79 2.29 1.47 1.14 1.79 1.92 2.17 1.81 1.44 1.50
SD 0.64 0.92 0.97 1.19 1.07 1.47 1.02 1.79 0.99 0.55 0.95 1.74 1.01 1.34 0.75 1.15
Mood stabilizer used
N 44 34 54 63 18 77 37 69 30 16 56 11 1 7 6 523
% (7.6) (7.1) (13.4) (19.6) (5.9) (25.8) (13.5) (30.1) (17.5) (9.8) (35.0) (8.4) (1.0) (7.2) (19.4) (14.0±9.7)
Antidepressant used
N 24 73 51 62 21 56 12 6 40 5 29 48 0 13 8 448
% (4.1) (15.2) (12.7) (19.3) (6.9) (18.8) (4.4) (2.6) (23.4) (3.0) (18.1) (36.6) 0 (13.4) (25.8) (12.0±10.3)
Anxiolytics used
N 92 151 157 99 49 166 42 73 53 14 24 71 39 9 5 1044
% (15.8) (31.5) (39.0) (30.7) (16.1) (55.7) (15.3) (31.9) (31.0) (8.5) (15.0) (54.2) (39.4) (9.3) (16.1) (27.9±15.2)
Hypnotics used
N 1 7 147 10 1 21 0 140 10 0 4 2 4 0 1 348
% (0.2) (1.5) (36.5) (3.1) (0.3) (7.0) 0 (61.1) (5.8) 0 (2.5) (1.5) (4.0) 0 (3.2) (9.3±17.2)
Antiparkinsonian drug used
N 224 180 154 272 116 207 30 90 69 99 49 65 87 33 13 1688
% (38.6) (37.6) (38.2) (84.5) (38.0) (69.5) (10.9) (39.3) (40.4) (60.4) (30.6) (49.6) (87.9) (34.0) (41.9) (45.1±20.6)
Note: Red and blue cells contain more than and less than 1 SD, respectively.
This article is protected by copyright. All rights reserved.
Accepted Article
Table 3. Comparison of polypharmacy and drug loading between inpatients and outpatient
Inpatient Outpatient P value
Count 1950 1794
Polypharmacy N (%) 957 (49.1) 623 (34.7) < 0.001
Antipsychotic loading mean (SD) 1.72 (1.24) 1.27 (1.01) < 0.001
Psychotropic drug loading mean (SD) 2.29 (1.79 ) 1.70 (1.40) < 0.001
This article is protected by copyright. All rights reserved.
You might also like
- ADHD OaplDocument145 pagesADHD Oaplminiloup05No ratings yet
- Inada, 2015Document8 pagesInada, 2015Khumaira SantaNo ratings yet
- Antipsychotic Medication Prescribing Trends in A Tertiary Care HospitalDocument4 pagesAntipsychotic Medication Prescribing Trends in A Tertiary Care HospitalSilfa NataliaNo ratings yet
- Patterns and Frequency of Atypical Antipsychotic Prescribing in Psychiatric Medical Centers: A Cross-Sectional National SurveyDocument9 pagesPatterns and Frequency of Atypical Antipsychotic Prescribing in Psychiatric Medical Centers: A Cross-Sectional National Surveymiron_ghiuNo ratings yet
- Pone 0267808Document22 pagesPone 0267808patowilliamsNo ratings yet
- Off-Label Use of Sodium Valproate For SchizophreniaDocument7 pagesOff-Label Use of Sodium Valproate For SchizophreniaHaya GrinvaldNo ratings yet
- Antipsychotic Polypharmacy in Psychotic DisorderDocument10 pagesAntipsychotic Polypharmacy in Psychotic DisorderFiarry FikarisNo ratings yet
- Efficacy and Safety of Paliperidone Palmitate Eca ADocument14 pagesEfficacy and Safety of Paliperidone Palmitate Eca AMaria Fernanda AbrahamNo ratings yet
- Meta-Analysis 1Document9 pagesMeta-Analysis 1blessing OjoneNo ratings yet
- BarbuiDocument8 pagesBarbuirinaldiapt08No ratings yet
- Evaluation of Anti-Psychotics Prescribing Pattern Using Who Indicators in A Tertiary Care HospitalDocument14 pagesEvaluation of Anti-Psychotics Prescribing Pattern Using Who Indicators in A Tertiary Care HospitalInternational Journal of Innovative Science and Research Technology100% (1)
- Pi Is 0025712514000893Document32 pagesPi Is 0025712514000893Christoph HockNo ratings yet
- Antipsychotic PolypharmacyDocument10 pagesAntipsychotic PolypharmacymarcoNo ratings yet
- NDT 45697 Efficacy of Second Generation Antipsychotics in Patients at 061813Document8 pagesNDT 45697 Efficacy of Second Generation Antipsychotics in Patients at 061813twahyuningsih_16No ratings yet
- Provisional: Pharmacotherapy of Anxiety Disorders: Current and Emerging Treatment OptionsDocument73 pagesProvisional: Pharmacotherapy of Anxiety Disorders: Current and Emerging Treatment OptionsDewi NofiantiNo ratings yet
- Integrative Literature Review FinalDocument17 pagesIntegrative Literature Review Finalapi-355221395No ratings yet
- Clinician Guidelines For The Treatment of Psychiatric Disorders With Nutraceuticals and Phytoceuticals The World Federation of Societies of BiologicaDocument34 pagesClinician Guidelines For The Treatment of Psychiatric Disorders With Nutraceuticals and Phytoceuticals The World Federation of Societies of Biologicapatrick.arnonNo ratings yet
- Chapter 12Document59 pagesChapter 12Alif riadiNo ratings yet
- Atypical Antipsychotic Augmentation in Major Depressive DisorderDocument13 pagesAtypical Antipsychotic Augmentation in Major Depressive DisorderrantiNo ratings yet
- Alpha-Dihydroergocryptine vs. Pramipexole As Adjunct Symptomatic Treatment of Idiopathic Parkinson'sDocument9 pagesAlpha-Dihydroergocryptine vs. Pramipexole As Adjunct Symptomatic Treatment of Idiopathic Parkinson'sRizka Leonita FahmyNo ratings yet
- Mahatme M S Et. Al., 2018Document6 pagesMahatme M S Et. Al., 2018kaniNo ratings yet
- Panss ScoreDocument8 pagesPanss ScoretriaclaresiaNo ratings yet
- Prescription Patterns of Patients Diagnosed With Schizophrenia in Mental Hospitals in Tashkent/Uzbekistan and in Four German CitiesDocument7 pagesPrescription Patterns of Patients Diagnosed With Schizophrenia in Mental Hospitals in Tashkent/Uzbekistan and in Four German CitiesRina YemimaNo ratings yet
- Antipsychotic Use in Children and Adolescents A.13Document7 pagesAntipsychotic Use in Children and Adolescents A.13jacopo pruccoliNo ratings yet
- Medi-100-E27653Document7 pagesMedi-100-E27653Rika TriwardianiNo ratings yet
- Earitcle - Practice Parameters For The Psychological and Behavioaral Treatment of InsomniaDocument5 pagesEaritcle - Practice Parameters For The Psychological and Behavioaral Treatment of InsomniaRichard SiahaanNo ratings yet
- Appi Focus 16407Document10 pagesAppi Focus 16407MARIALEJ PEREZ MONTALVANNo ratings yet
- Morbidity Profile and Prescribing Patterns Among Outpatients in A Teaching Hospital in Western NepalDocument7 pagesMorbidity Profile and Prescribing Patterns Among Outpatients in A Teaching Hospital in Western Nepalpolosan123No ratings yet
- Clinical Medicine Insights: PediatricsDocument14 pagesClinical Medicine Insights: PediatricsferegodocNo ratings yet
- Ijmrhs Vol 4 Issue 3Document263 pagesIjmrhs Vol 4 Issue 3editorijmrhsNo ratings yet
- Usr 6403928586398Document3 pagesUsr 6403928586398Rodrigo SosaNo ratings yet
- J Eurpsy 2007 03 002Document11 pagesJ Eurpsy 2007 03 002xhdrv7nvdrNo ratings yet
- J Ajem 2020 07 013Document21 pagesJ Ajem 2020 07 013Athea 88No ratings yet
- Comparative e Cacy and Acceptability of Antimanic Drugs in Acute Mania: A Multiple-Treatments Meta-AnalysisDocument10 pagesComparative e Cacy and Acceptability of Antimanic Drugs in Acute Mania: A Multiple-Treatments Meta-AnalysisCarolina PradoNo ratings yet
- Psychotic Disorders Induced by Antiepileptic Drugs in People With EpilepsyDocument11 pagesPsychotic Disorders Induced by Antiepileptic Drugs in People With EpilepsyShadrackNo ratings yet
- Pharmacologic Treatment of Attention Deficit-Hyperactivity DisorderDocument7 pagesPharmacologic Treatment of Attention Deficit-Hyperactivity DisorderSusana Maria Ribero BalagueraNo ratings yet
- Tdah - ReviewDocument7 pagesTdah - ReviewFábio Yutani KosekiNo ratings yet
- Analysis of The Prescription Pattern of Psychotropics I 2022 Medical JournalDocument6 pagesAnalysis of The Prescription Pattern of Psychotropics I 2022 Medical JournalAnisha RanaNo ratings yet
- REF4 - Evaluation of Drug Utilization and Analysis of AntiEpileptic DrugsDocument7 pagesREF4 - Evaluation of Drug Utilization and Analysis of AntiEpileptic DrugsJorge Ropero VegaNo ratings yet
- Sleep Medicine: Judith A. Owens, Carol L. Rosen, Jodi A. Mindell, Hal L. KirchnerDocument9 pagesSleep Medicine: Judith A. Owens, Carol L. Rosen, Jodi A. Mindell, Hal L. KirchnerHernán MarínNo ratings yet
- Psychiatric Drugs in Children and Adolescents: Basic Pharmacology and Practical ApplicationsDocument540 pagesPsychiatric Drugs in Children and Adolescents: Basic Pharmacology and Practical ApplicationsRey Jerly Duran BenitoNo ratings yet
- Paliperidona Revision 18 PagsDocument19 pagesPaliperidona Revision 18 PagsRodrigo SosaNo ratings yet
- Clinical Characteristics of Agitated Psychotic Patients Treated With An Oral Antipsychotics Attended in The Emergency Room Setting: NATURA StudyDocument8 pagesClinical Characteristics of Agitated Psychotic Patients Treated With An Oral Antipsychotics Attended in The Emergency Room Setting: NATURA StudyMaria Niña Beatrice DelaCruzNo ratings yet
- Herbal Medicine Treatment For Children With Autism Spectrum Disorder: A Systematic ReviewDocument14 pagesHerbal Medicine Treatment For Children With Autism Spectrum Disorder: A Systematic ReviewMaximiliano QMCNo ratings yet
- Schizophrenia Treatment & ManagementDocument16 pagesSchizophrenia Treatment & ManagementDimas Januar100% (2)
- Aripiprazol Versus Quetiapine in Treatment of Non-Affective Acute Psychosis: A Double-Blind, Randomized - Controlled Clinical TrialDocument4 pagesAripiprazol Versus Quetiapine in Treatment of Non-Affective Acute Psychosis: A Double-Blind, Randomized - Controlled Clinical TrialAsti DwiningsihNo ratings yet
- Matej Stuhec Antipsychotic Treatment in ElderlyDocument6 pagesMatej Stuhec Antipsychotic Treatment in Elderlymagocita.martinNo ratings yet
- Current Practices, Experiences, and Views in Clinical HypnosisDocument43 pagesCurrent Practices, Experiences, and Views in Clinical HypnosisJoBPNo ratings yet
- Presentation RTA, DM, Rheumatoid ArthritisDocument26 pagesPresentation RTA, DM, Rheumatoid ArthritisShah MohammedNo ratings yet
- Sci 2013 9 (10s) :60-62) - (ISSN: 1545-1003)Document3 pagesSci 2013 9 (10s) :60-62) - (ISSN: 1545-1003)Muhammad Ziaur RahmanNo ratings yet
- An Association Between Incontinence and Antipsychotic Drugs - A Systematic ReviewDocument9 pagesAn Association Between Incontinence and Antipsychotic Drugs - A Systematic ReviewchaconcarpiotatianaNo ratings yet
- Hipnose e AVCDocument8 pagesHipnose e AVCTransf ArquivosNo ratings yet
- Aripiprazol LAI Vs Paliperidona LAI in SKDocument10 pagesAripiprazol LAI Vs Paliperidona LAI in SKRobert MovileanuNo ratings yet
- 2017-Ugo Chukwu-International Journal of Medicine and PharmacyDocument10 pages2017-Ugo Chukwu-International Journal of Medicine and PharmacyNurettin AbacıoğluNo ratings yet
- Gajjar B M Et. Al., 2016Document6 pagesGajjar B M Et. Al., 2016kaniNo ratings yet
- 2021 Grupo 1 Metanálise AntidepressivosDocument14 pages2021 Grupo 1 Metanálise AntidepressivosAmanda NelvoNo ratings yet
- Long-Term Stimulant Treatment Affects Brain Dopamine Transporter Level in Patients With Attention Deficit Hyperactive DisorderDocument6 pagesLong-Term Stimulant Treatment Affects Brain Dopamine Transporter Level in Patients With Attention Deficit Hyperactive DisorderpriyaNo ratings yet
- Initial Severity Jama PDFDocument8 pagesInitial Severity Jama PDFnoeanisaNo ratings yet
- Initial Severity of Schizophrenia and Efficacy of Antipsychotics Participant-Level Meta-Analysis of 6 Placebo-Controlled StudiesDocument8 pagesInitial Severity of Schizophrenia and Efficacy of Antipsychotics Participant-Level Meta-Analysis of 6 Placebo-Controlled StudieseviantiNo ratings yet
- Medication Errors Associated With Look-alike/Sound-alike Drugs: A Brief ReviewDocument8 pagesMedication Errors Associated With Look-alike/Sound-alike Drugs: A Brief Reviewsabbo morsNo ratings yet
- 01 Drug Absorption (Notes - Q A) AtfDocument2 pages01 Drug Absorption (Notes - Q A) Atfemaannoor972No ratings yet
- Daftar Nama Obat Di Farmasi Klinik Ibnu SinaDocument5 pagesDaftar Nama Obat Di Farmasi Klinik Ibnu SinaAfifa RahmahNo ratings yet
- Pentingnya Pemberian Imunisasi DPT Pada Anak Difteri Dan PertusisDocument30 pagesPentingnya Pemberian Imunisasi DPT Pada Anak Difteri Dan Pertusisrevi rillianiNo ratings yet
- Drug Study PediaDocument3 pagesDrug Study PediaDanica Kate GalleonNo ratings yet
- ParacetamolDocument2 pagesParacetamolKristine YoungNo ratings yet
- Pharmacy and Therapeutics Committee: APOLLOJAMES, M. Pharm., (PH.D), Asst - Prof, Dept of Pharmacy PracticeDocument39 pagesPharmacy and Therapeutics Committee: APOLLOJAMES, M. Pharm., (PH.D), Asst - Prof, Dept of Pharmacy PracticeSuresh ThanneruNo ratings yet
- Pharmacology Pharmacokinetics and Pharmacodynamics - PPT - Dr. Maulana Antian Empitu (Airlangga Medical Faculty)Document59 pagesPharmacology Pharmacokinetics and Pharmacodynamics - PPT - Dr. Maulana Antian Empitu (Airlangga Medical Faculty)rizkyyunitaa15No ratings yet
- Multimodal Analgesia Techniques and Postoperative RehabilitationDocument18 pagesMultimodal Analgesia Techniques and Postoperative RehabilitationJazmín PrósperoNo ratings yet
- Insulin Injection PDFDocument6 pagesInsulin Injection PDFAulia mulidaNo ratings yet
- The American Psychiatric Publishing Textbook of PsDocument3 pagesThe American Psychiatric Publishing Textbook of Ps!R_I_A!No ratings yet
- Abaloparatide (Tymlos) For OsteoporosisDocument2 pagesAbaloparatide (Tymlos) For Osteoporosishossein kasiriNo ratings yet
- Medicines For BaguioDocument3 pagesMedicines For BaguioMaielyne Keith DalilisNo ratings yet
- Inn Dci ListDocument80 pagesInn Dci ListPapa Sissao SeckNo ratings yet
- THE Check Principle Applied in Pharmacology: Remember To Take Your Tagamet With Meals!Document35 pagesTHE Check Principle Applied in Pharmacology: Remember To Take Your Tagamet With Meals!helloaNo ratings yet
- Crash Cart Check ListDocument2 pagesCrash Cart Check Listkim reyesNo ratings yet
- Practice Standard: Safe Prescribing of Opioids and SedativesDocument4 pagesPractice Standard: Safe Prescribing of Opioids and SedativesSteve GreenNo ratings yet
- CLARITHROMYCINDocument3 pagesCLARITHROMYCINCay SevillaNo ratings yet
- Lisinopril (Prinvil, Zestril) Fosinopril (Monopril) Ramapril (Altace)Document1 pageLisinopril (Prinvil, Zestril) Fosinopril (Monopril) Ramapril (Altace)vigNo ratings yet
- COMPRE - MODULE 3 (Practice of Pharmacy) : Attempt ReviewDocument39 pagesCOMPRE - MODULE 3 (Practice of Pharmacy) : Attempt ReviewLance RafaelNo ratings yet
- Simvastatin 20 MG Paracetamol 500 MG Tab Paracetamol 650 MG Tab Acyclovir CreamDocument7 pagesSimvastatin 20 MG Paracetamol 500 MG Tab Paracetamol 650 MG Tab Acyclovir CreamtdshyenNo ratings yet
- DrugStudy CelecoxibDocument2 pagesDrugStudy CelecoxibLegendXNo ratings yet
- P2 (1) - Kowski AB, Et Al. Epilepsy Behav - 2016 Jan 54150-7.Document8 pagesP2 (1) - Kowski AB, Et Al. Epilepsy Behav - 2016 Jan 54150-7.li chenNo ratings yet
- Pepcid AC - Group1 - AnalysisDocument2 pagesPepcid AC - Group1 - AnalysisRini RafiNo ratings yet
- USFDA Guidance For Industry - PSURDocument50 pagesUSFDA Guidance For Industry - PSURErshad Shafi AhmedNo ratings yet
- India: Drug Regulatory Framework & New InitiativesDocument16 pagesIndia: Drug Regulatory Framework & New InitiativesRajesh RanganathanNo ratings yet
- Drug Interactions of Antianginal Drugs..Document40 pagesDrug Interactions of Antianginal Drugs..Kamal SikandarNo ratings yet
- Beneficiary Details: COVID-19Document1 pageBeneficiary Details: COVID-19THAMIZHAZHAHAN SNo ratings yet
- Drug StudyDocument4 pagesDrug StudyMelvin D. RamosNo ratings yet
- Drugs Not To Take With LDNDocument10 pagesDrugs Not To Take With LDNbktangoNo ratings yet