Professional Documents
Culture Documents
Reference Card For Who Emergency Unit Form General
Reference Card For Who Emergency Unit Form General
Uploaded by
Gideon BahuleCopyright:
Available Formats
You might also like
- Maternity Care Guidelines - 24 November 2023Document266 pagesMaternity Care Guidelines - 24 November 2023KhodaniNo ratings yet
- Student Worksheet2023 PDFDocument2 pagesStudent Worksheet2023 PDFjj100% (1)
- Inpatient Oral Case PresentationDocument5 pagesInpatient Oral Case PresentationTemsegenNo ratings yet
- PAS Quick GuideDocument1 pagePAS Quick GuideTracyNo ratings yet
- Cardiac Exam Detailed Skill SheetDocument2 pagesCardiac Exam Detailed Skill SheetJp JardelezaNo ratings yet
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Assessing Neurologic FunctionsDocument10 pagesAssessing Neurologic FunctionsDenise DizonNo ratings yet
- Shock and Circulatory FailureDocument8 pagesShock and Circulatory FailureOktaviana Sari DewiNo ratings yet
- Review 2Document12 pagesReview 2Christine Rubio100% (1)
- Weekly Clinical Prep Packet 12 REVISEDDocument12 pagesWeekly Clinical Prep Packet 12 REVISEDMei SarteNo ratings yet
- An Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFDocument6 pagesAn Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFkatherine dayagNo ratings yet
- Suez Canal University/ Faculty of Nursing (Medical Surgical Nursing/ Clinical Assessment Sheet 2 Year 2020/2021)Document18 pagesSuez Canal University/ Faculty of Nursing (Medical Surgical Nursing/ Clinical Assessment Sheet 2 Year 2020/2021)طالب جامعة100% (1)
- H&PtemplateDocument2 pagesH&PtemplateScott OwenNo ratings yet
- Final Assessing Female and Male Genitourinary SystemDocument7 pagesFinal Assessing Female and Male Genitourinary SystemJo Marchianne PigarNo ratings yet
- Fluids and Electrolytes Lesson Outline For BBDocument14 pagesFluids and Electrolytes Lesson Outline For BBdlneisha61100% (1)
- NURS 225V Principles III Data Collection ToolDocument2 pagesNURS 225V Principles III Data Collection ToolKrisNo ratings yet
- Blood Sample Normal Panic Values For Abgs: Clinical SignificanceDocument7 pagesBlood Sample Normal Panic Values For Abgs: Clinical SignificancegeonarcisoNo ratings yet
- How To Present Cases (Short File) PDFDocument3 pagesHow To Present Cases (Short File) PDFAmjad SaudNo ratings yet
- Health History FormDocument1 pageHealth History Formapi-353679123No ratings yet
- Lab Workup: Practical Nursing Mohawk College 2014Document2 pagesLab Workup: Practical Nursing Mohawk College 2014Pawel PietruszczakNo ratings yet
- Area Technique Normal Findings Analysis and Interpretation A. SkullDocument7 pagesArea Technique Normal Findings Analysis and Interpretation A. Skullkingawesome21100% (1)
- Fluids Electrolytes and Acid Base ImbalancesDocument8 pagesFluids Electrolytes and Acid Base ImbalancesSamantha Bernardo UndaNo ratings yet
- Abdomenal Exam HandoutDocument5 pagesAbdomenal Exam HandoutNesma AdelNo ratings yet
- Communicable Diseases HandoutsDocument15 pagesCommunicable Diseases HandoutsLloyd LozanoNo ratings yet
- Pead 3 - Abdominal Pain and VommitingDocument22 pagesPead 3 - Abdominal Pain and Vommitingbbyes100% (1)
- ShockDocument9 pagesShockapocruNo ratings yet
- Cerebral Vascular Accident (Stroke)Document5 pagesCerebral Vascular Accident (Stroke)SN. CaRNo ratings yet
- Anatomical TermsDocument82 pagesAnatomical TermsRichelle Ann Gatchola EvangelistaNo ratings yet
- Fullsize SBAR Report SheetDocument2 pagesFullsize SBAR Report SheetMeg AqNo ratings yet
- Clinical SkilllllllllllllllDocument12 pagesClinical SkilllllllllllllllAlmira Putri100% (1)
- How To Treat: Septic ShockDocument6 pagesHow To Treat: Septic ShockmeeandsoeNo ratings yet
- UCLA Fundamentals of Clinical Medicine Physical Exam Skills Checklist Student - GroupDocument5 pagesUCLA Fundamentals of Clinical Medicine Physical Exam Skills Checklist Student - GroupAmira AttyaNo ratings yet
- NRSG 2221 Skills Mastery 1 Skills ChecklistDocument2 pagesNRSG 2221 Skills Mastery 1 Skills ChecklistNi CaoNo ratings yet
- History and Physical Exam Skills List: Opening VisitDocument7 pagesHistory and Physical Exam Skills List: Opening VisitAnonymous Sfcml4GvZNo ratings yet
- 3west Brain SheetDocument2 pages3west Brain SheetVictoriaStoneHarrisNo ratings yet
- HistoryandPhysicalExamDocument105 pagesHistoryandPhysicalExamsilentscream0618No ratings yet
- This Study Resource Was: Student Name: - Section: - Date of Patient CareDocument2 pagesThis Study Resource Was: Student Name: - Section: - Date of Patient CareSashaNo ratings yet
- Complete Respiratory Examination Checklist 365Document5 pagesComplete Respiratory Examination Checklist 365mohammed alrubaiaanNo ratings yet
- Approach To Unconscious PatientsDocument5 pagesApproach To Unconscious PatientsMary Joyce Ajero LadimoNo ratings yet
- NCM112 LP1 Transes - RosalesDocument4 pagesNCM112 LP1 Transes - RosalesChristine CalleyNo ratings yet
- 6 Parts: o Mental Status o Cranial Nerves o Sensory Function o Motor Function o Cerebellar Function o Reflexes 1. Cranial NervesDocument3 pages6 Parts: o Mental Status o Cranial Nerves o Sensory Function o Motor Function o Cerebellar Function o Reflexes 1. Cranial NervesTaraKyleUyNo ratings yet
- F0826 International Standards For Neurological Classification of SCI Worksheet HGHDGDocument25 pagesF0826 International Standards For Neurological Classification of SCI Worksheet HGHDGreeves_cool100% (1)
- CASE 1 Neuro PDFDocument23 pagesCASE 1 Neuro PDFthe KLAWNo ratings yet
- Git HistoryDocument18 pagesGit HistoryAhmed SallamNo ratings yet
- Sepsis Quick Reference GuideDocument1 pageSepsis Quick Reference GuideRavin DebieNo ratings yet
- Nursing Management of The Perioperative PatientDocument16 pagesNursing Management of The Perioperative Patientashdmb217No ratings yet
- Abdominal Examination ProcedureDocument5 pagesAbdominal Examination ProcedureAnamul hossainNo ratings yet
- Primary Trauma CareDocument48 pagesPrimary Trauma CareKABERA RENENo ratings yet
- Script ECEDocument4 pagesScript ECESleepyHead ˋωˊNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- Manual of First Aid Professional English: Part 3—Case StudiesFrom EverandManual of First Aid Professional English: Part 3—Case StudiesNo ratings yet
- English in Urgent Care Medicine – Anglictina V Urgentní Medicíne: Textbook – UcebniceFrom EverandEnglish in Urgent Care Medicine – Anglictina V Urgentní Medicíne: Textbook – UcebniceNo ratings yet
- Leg Med (Abortion)Document3 pagesLeg Med (Abortion)julietNo ratings yet
- MTLB Debate PRODocument3 pagesMTLB Debate PRORHODA MAE CAPUTOLNo ratings yet
- Preeclampsia and EclampsiaDocument24 pagesPreeclampsia and EclampsiaLuisa SarangayNo ratings yet
- BHP Formula No 55 Refrence - Bioplasgen 20 Homeopathic Medicine For Skin DiseasesDocument2 pagesBHP Formula No 55 Refrence - Bioplasgen 20 Homeopathic Medicine For Skin DiseasesKazy Habibur RahmanNo ratings yet
- Ophthalmology - Diseases of CorneaDocument18 pagesOphthalmology - Diseases of CorneajbtcmdtjjvNo ratings yet
- Doh Programs First 1000 Days Ni BabyDocument65 pagesDoh Programs First 1000 Days Ni BabyjpnachorNo ratings yet
- Test Report:: Patient Name:Mr Bahu Anil Kumar Sahu Patient IDDocument1 pageTest Report:: Patient Name:Mr Bahu Anil Kumar Sahu Patient IDANILNo ratings yet
- Municipal Summary Monitoring of Incidence On Violence Against Children (Vac) During The Covid-19 PandemicDocument2 pagesMunicipal Summary Monitoring of Incidence On Violence Against Children (Vac) During The Covid-19 PandemicDann MarrNo ratings yet
- Complications After AmputationDocument44 pagesComplications After AmputationGulzar AhmadNo ratings yet
- CHMP Post Authorisation Summary Positive Opinion Mounjaro II 07 - enDocument2 pagesCHMP Post Authorisation Summary Positive Opinion Mounjaro II 07 - enFRUNZANo ratings yet
- DR AK MedicineDocument1 pageDR AK MedicineShweta jainNo ratings yet
- NovoMix 30 FlexPen CM v15Document12 pagesNovoMix 30 FlexPen CM v15Nadia SalwaniNo ratings yet
- Vital SignsDocument5 pagesVital SignsFrances Kaye Sta. CruzNo ratings yet
- Neuromuscular and Other Diseases of The Chest WallDocument25 pagesNeuromuscular and Other Diseases of The Chest WallluckyNo ratings yet
- en Colitis TuberculosisDocument7 pagesen Colitis TuberculosisATIKA INDAH SARINo ratings yet
- Great Atlas of Dermatology IndexedDocument73 pagesGreat Atlas of Dermatology Indexedjohn pauloNo ratings yet
- CPH Lecture ReviewerDocument11 pagesCPH Lecture ReviewerAngel LadimNo ratings yet
- Pleural Effusion in A Patient With End-Stage Renal Disease - PMCDocument5 pagesPleural Effusion in A Patient With End-Stage Renal Disease - PMCCasemix rsudwaledNo ratings yet
- Noy 192Document10 pagesNoy 192Cleysser Antonio Custodio PolarNo ratings yet
- Exercises For Non Communicable DiseasesDocument32 pagesExercises For Non Communicable DiseasesParul ThakurNo ratings yet
- EPISODIC SOAP Note For UTIDocument40 pagesEPISODIC SOAP Note For UTIlagatduncan520No ratings yet
- Smile Dental ClinicDocument9 pagesSmile Dental ClinicADEA Group and PartnersNo ratings yet
- Case Study (Amit Mandal)Document7 pagesCase Study (Amit Mandal)Mukesh SelvanNo ratings yet
- What Are Normal Male Testosterone Levels by AgeDocument9 pagesWhat Are Normal Male Testosterone Levels by AgeMiltonNo ratings yet
- Efficacy of Erandamuladi Niruhabasti in Gridhasi A Case StudyDocument4 pagesEfficacy of Erandamuladi Niruhabasti in Gridhasi A Case StudyResearch ParkNo ratings yet
- ROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPDocument6 pagesROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPkimberly quitonNo ratings yet
- NCP Hyperbilirubinemia IIDocument4 pagesNCP Hyperbilirubinemia IISandyNo ratings yet
- Heat Illness Prevention ProgramDocument7 pagesHeat Illness Prevention ProgramSPIQCNo ratings yet
- Research 1Document22 pagesResearch 1Biplov RoyNo ratings yet
- Vocal Cord ParalysisDocument26 pagesVocal Cord ParalysisELIA RICHARDNo ratings yet
Reference Card For Who Emergency Unit Form General
Reference Card For Who Emergency Unit Form General
Uploaded by
Gideon BahuleOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Reference Card For Who Emergency Unit Form General
Reference Card For Who Emergency Unit Form General
Uploaded by
Gideon BahuleCopyright:
Available Formats
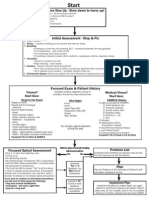
REFERENCE CARD FOR WHO EMERGENCY UNIT FORM: GENERAL
DATES/TIMES: Do not leave dates/times blank. Where unknown, write UNK
MASS CASUALTY: Check box if patient part of a mass casualty event
AGE: If age unknown, circle category: IN (infant) if appears <1 year of age, CH (child) if 1-18 years, or AD (adult)
OCCUPATION: Be as specific as possible (eg. farm laborer or farm manager instead of farming)
PATIENT RESIDENCE: Note if homeless, migrant worker, other
CHIEF COMPLAINT: Always in the patient’s own words
DEAD ON ARRIVAL: Use ONLY if NO signs of life on arrival
NORMAL VITAL SIGNS – FOR ALL: SpO2 >92% on RA, Temp 36˚C - 38˚C
Paediatric: *Record O2 saturation and amount/route of O2,
eg. 94% on 2L by NC
Adult: Pulse 60-100 bpm, RR 10-20, SPB >90
Pain score: Ask the patient to choose the face that best represents
the pain they are experiencing.
TREATING PROVIDER ASSESSMENT Date and time of first assessment of patient by medical provider at current facility
Primary Survey
Airway: Normal (NML) •OPA/NPA=oro-/naso-pharyngeal airway •LMA=laryngeal mask
•Patent (speaking normally) airway •BVM=bag valve mask •ETT=endotracheal tube
•NO signs of obstruction, stridor or angioedema •TTP=tenderness to palpation
Breathing: NML Abnormal •NC=nasal cannula •NRB=non-rebreather mask •BVM=bag valve
• Effort normal •Distant breath sounds •Crepitation •Rhonchi mask •CPAP/BiPAP=continuous or bi-level positive airway pressure
•Wheezing • Enter N/A for spontaneous RR if
• Sounds clear •Ventilator=mechanical ventilation
sedated, paralyzed or on ventilator
Circulation: NML Abnormal Access: Document location (loc) and size
•Warm & dry •JVD (jugular venous distention) •IV=peripheral intravenous •CVL=central venous line
•Pulse strong & •Prolonged capillary refill (>3 sec) •IO=intraosseous
symmetric (upper & •IVF (intravenous fluids): •NS=normal saline) •LR=Lactated
lower extremities) Ringer’s •Other (write name)
Disability: NML Abnormal •Blood glucose (RBG): Normal >3.5 mmol/L
•Alert (A) •Oriented to •Responds only to Verbal (V), Pain (P), or is •Antiepileptic (eg. diazepam, phenytoin, etc.)
person/place/time Unconscious (U) •Others: list (eg. sedation medications for agitation,
•Moves all extremities •Motor or sensory deficit (note location) antihypertensives for hypertensive emergency, etc.)
•Pupil Size: normal, large, or pinpoint
•Pupil Reactivity: Reactive (NML/brisk), slow, fixed, nonreactive (NR)
REVIEW OF SYSTEMS (If patients do not have any of these symptoms, mark NML)
General: Fever, chills, night sweats, fatigue, weight loss Female Reproductive: Vaginal bleeding, vaginal discharge,
Head/Ears/Eyes/Nose/Throat (HEENT): Vision changes, discharge abnormal menses, pelvic pain
(eye/ear), pain (eye/ear), nose bleeds, mucosal lesions, difficulty If pregnant – Decreased fetal movement, contractions, leakage of
swallowing, drooling, sore throat, dental problem, facial swelling fluid
Respiratory: Difficulty breathing, cough, sputum production, bloody Male Reproductive: Penile discharge, testicular pain, penile pain,
sputum, wheezing priapism
Cardiovascular (CV): Chest pain, chest tightness, palpitations, Skin: Rash, itching, jaundice, ulcers
orthopnea, edema Musculoskeletal (MSK): Myalgia, joint pain/swelling
Gastrointestinal (GI): Anorexia, abdominal pain, nausea, vomiting, Hematologic (Heme): Lymphadenopathy, easy bruising
vomiting blood, diarrhea, blood in stool, black/tarry stool Neurologic (Neuro): Headache, syncope, focal weakness,
Genitourinary: Urination (difficulty, pain, frequency, blood), numbness, dizziness, lightheadedness, speech problems, balance
incontinence, flank pain, genital lesions problems
Psychiatric: Hallucination, agitation, homicidal thoughts, suicidal
thoughts, depression, anxiety
Pediatric specific: Unable to feed, decreased activity, decreased urine,
vomiting everything, convulsions, excessive irritability
***NOTE: if more than one calendar is used in your setting by clinical providers and recorded as such on this form, all dates must be converted to
Gregorian calendar and times converted to 24-hour format by data clerk before it is entered into registry.***
To be used as a reference for completing the general emergency unit form.
www.who/int/emergencycare
MEDICAL HISTORY
Past Medical History Immunization: Ask if up to Family History
•DM •COPD •HTN •Psych •Renal disease •Other (list conditions not date. Review card if •Early death
noted, eg. heart disease, stroke, asthma, sickle cell, active cancer, available. •Known heart disease
HIV/AIDS) Safe at home: Ask about •Cancer
Medication: include anticoagulants, rx medications, traditional violence in the home •Epilepsy
medicines, herbs and supplements
Normal Exam (Check NML only if NO abnormal findings as below are present)
General: Well-developed, well-nourished, awake, alert Respiratory: Nml effort, nml breath sounds
Neuro/Psychiatric: Oriented X3, CN intact, no focal weakness or Abdominal: Soft and non-tender, bowel sounds nml
sensory deficits. Nml mood and affect, nml behavior, nml thought Pelvis/GU/Rectal: External genitals nml, no costovertebral angle
content (CVA) tenderness
HEENT: Normocephalic, atraumatic. Eyes - Pupils equal and reactive, MSK: Range of motion nml
extra ocular movements intact, conjunctivae normal Skin: Warm, intact, capillary refill ≤3 sec
Neck: Trachea midline, neck supple, ROM nml Lymph: No lymphadenopathy
Cardiac: Nml rate and rhythm, strong pulses, nml sounds
Abnormal Exam Findings (Always specify right or left when needed to clarify abnormal finding)
General: Distressed, malnourished (if suspect obtain MUAC), Respiratory: Absent breath sounds, decreased breath sounds,
diaphoretic, uncooperative, sedated, lethargic crackles, wheezes
Neuro/Psychiatric: Neuro - Disoriented, CN deficit, focal sensory or Abdominal: Distension, tenderness, rebound, guarding, ascites,
motor deficit, abnormal gait or coordination, tremors, seizure activity, hepatomegaly, splenomegaly, mass
Kernig/Brudzinski sign, abnormal rectal tone. Psych- Suicidal, Pelvis/GU/Rectal: Penile discharge, testicular mass or
depressed, homicidal, delusional, agitated, hallucinating, abnormal tenderness, CVA tenderness, vaginal bleeding or discharge,
speech cervical motion tenderness, adnexal tenderness, blood or dark
HEENT: Dry mucus membranes, tonsillar exudate, abnormal stool on rectal exam
fontanelle, ear discharge, oral lesions, facial swelling. Eyes - If pregnant - No fetal heart rate
Conjunctiva pale, peri-orbital lesion, abnormal ocular movements, MSK: Joint swelling, decreased ROM or strength, scoliosis,
scleral jaundice, eye discharge, pupils unequal and/or slow or non- kyphosis, spine tenderness
reactive Skin: Rash, lesion, ulcer, pustules, bruising, petechiae, poor
Neck: Neck stiffness, JVD, carotid bruit, neck mass, tracheal deviation turgor, capillary refill > 3 seconds
Cardiac: Distant heart sounds, systolic or diastolic murmur, S3 or S4 Lymph: Adenopathy (head, cervical, supraclavicular, axillary or
gallop, friction rub, irregular pulse inguinal), lymphedema
DIAGNOSTICS INTERVENTIONS (if no interventions, write NONE)
Fluids/Medications: list Blood product type (eg. PRBC, platelets)
and number of units, write medication name/dose in appropriate
category if applicable (eg. Opioid Analgesia: Morphine 4 mg)
•Other: Vasopressors, post-intubation gtt, etc.
Procedures: list number of attempts, location, and outcome for
UPT: Urine pregnancy test
each procedure, if applicable
ECG: Electrocardiogram
•Other: Diagnostic peritoneal lavage, regional block, central line
Other: List study name (eg. lactate, amylase, lipase, PT/INR, PTT, CK,
placement (if not noted in “Circulation” section), suprapubic
CK MB, cultures [blood, CSF or urine]) and result
catheterization, cricothyroidotomy, foreign body removal, etc.
Imaging: Specify type (XR, CT, U/S), location and results. If study
needed but not available, write this in other.
ASSESSMENT AND PLAN (include summary and differential diagnosis AND plan for imaging, pain meds, consults)
CONSULT Document service, name, time of call AND time of arrival with any recommendations
REASSESSMENT: Time, vitals and clinical condition
DISPOSITION Write date and time of ED departure, updated vital signs (VS), check box for destination
Checklist Completion: Use WHO medical emergency checklist to verify tasks have been completed
DIAGNOSIS: List all diagnoses
Admit or Transfer: Write Discharge: Confirm that plan including Death: Specify cause of death, but DO NOT WRITE cardiac or
the name of the follow-up care was discussed with the respiratory failure/arrest. Instead, use precise terms such as
accepting provider for all patient. “pneumonia” or “organophosphate poisoning” or “suicide.”
handovers.
Document all providers engaged in the patient’s care including through shift handovers.
***NOTE: if more than one calendar is used in your setting by clinical providers and recorded as such on this form, all dates must be converted to
Gregorian calendar and times converted to 24-hour format by data clerk before it is entered into registry.***
To be used as a reference for completing the general emergency unit form.
www.who/int/emergencycare
You might also like
- Maternity Care Guidelines - 24 November 2023Document266 pagesMaternity Care Guidelines - 24 November 2023KhodaniNo ratings yet
- Student Worksheet2023 PDFDocument2 pagesStudent Worksheet2023 PDFjj100% (1)
- Inpatient Oral Case PresentationDocument5 pagesInpatient Oral Case PresentationTemsegenNo ratings yet
- PAS Quick GuideDocument1 pagePAS Quick GuideTracyNo ratings yet
- Cardiac Exam Detailed Skill SheetDocument2 pagesCardiac Exam Detailed Skill SheetJp JardelezaNo ratings yet
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Assessing Neurologic FunctionsDocument10 pagesAssessing Neurologic FunctionsDenise DizonNo ratings yet
- Shock and Circulatory FailureDocument8 pagesShock and Circulatory FailureOktaviana Sari DewiNo ratings yet
- Review 2Document12 pagesReview 2Christine Rubio100% (1)
- Weekly Clinical Prep Packet 12 REVISEDDocument12 pagesWeekly Clinical Prep Packet 12 REVISEDMei SarteNo ratings yet
- An Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFDocument6 pagesAn Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFkatherine dayagNo ratings yet
- Suez Canal University/ Faculty of Nursing (Medical Surgical Nursing/ Clinical Assessment Sheet 2 Year 2020/2021)Document18 pagesSuez Canal University/ Faculty of Nursing (Medical Surgical Nursing/ Clinical Assessment Sheet 2 Year 2020/2021)طالب جامعة100% (1)
- H&PtemplateDocument2 pagesH&PtemplateScott OwenNo ratings yet
- Final Assessing Female and Male Genitourinary SystemDocument7 pagesFinal Assessing Female and Male Genitourinary SystemJo Marchianne PigarNo ratings yet
- Fluids and Electrolytes Lesson Outline For BBDocument14 pagesFluids and Electrolytes Lesson Outline For BBdlneisha61100% (1)
- NURS 225V Principles III Data Collection ToolDocument2 pagesNURS 225V Principles III Data Collection ToolKrisNo ratings yet
- Blood Sample Normal Panic Values For Abgs: Clinical SignificanceDocument7 pagesBlood Sample Normal Panic Values For Abgs: Clinical SignificancegeonarcisoNo ratings yet
- How To Present Cases (Short File) PDFDocument3 pagesHow To Present Cases (Short File) PDFAmjad SaudNo ratings yet
- Health History FormDocument1 pageHealth History Formapi-353679123No ratings yet
- Lab Workup: Practical Nursing Mohawk College 2014Document2 pagesLab Workup: Practical Nursing Mohawk College 2014Pawel PietruszczakNo ratings yet
- Area Technique Normal Findings Analysis and Interpretation A. SkullDocument7 pagesArea Technique Normal Findings Analysis and Interpretation A. Skullkingawesome21100% (1)
- Fluids Electrolytes and Acid Base ImbalancesDocument8 pagesFluids Electrolytes and Acid Base ImbalancesSamantha Bernardo UndaNo ratings yet
- Abdomenal Exam HandoutDocument5 pagesAbdomenal Exam HandoutNesma AdelNo ratings yet
- Communicable Diseases HandoutsDocument15 pagesCommunicable Diseases HandoutsLloyd LozanoNo ratings yet
- Pead 3 - Abdominal Pain and VommitingDocument22 pagesPead 3 - Abdominal Pain and Vommitingbbyes100% (1)
- ShockDocument9 pagesShockapocruNo ratings yet
- Cerebral Vascular Accident (Stroke)Document5 pagesCerebral Vascular Accident (Stroke)SN. CaRNo ratings yet
- Anatomical TermsDocument82 pagesAnatomical TermsRichelle Ann Gatchola EvangelistaNo ratings yet
- Fullsize SBAR Report SheetDocument2 pagesFullsize SBAR Report SheetMeg AqNo ratings yet
- Clinical SkilllllllllllllllDocument12 pagesClinical SkilllllllllllllllAlmira Putri100% (1)
- How To Treat: Septic ShockDocument6 pagesHow To Treat: Septic ShockmeeandsoeNo ratings yet
- UCLA Fundamentals of Clinical Medicine Physical Exam Skills Checklist Student - GroupDocument5 pagesUCLA Fundamentals of Clinical Medicine Physical Exam Skills Checklist Student - GroupAmira AttyaNo ratings yet
- NRSG 2221 Skills Mastery 1 Skills ChecklistDocument2 pagesNRSG 2221 Skills Mastery 1 Skills ChecklistNi CaoNo ratings yet
- History and Physical Exam Skills List: Opening VisitDocument7 pagesHistory and Physical Exam Skills List: Opening VisitAnonymous Sfcml4GvZNo ratings yet
- 3west Brain SheetDocument2 pages3west Brain SheetVictoriaStoneHarrisNo ratings yet
- HistoryandPhysicalExamDocument105 pagesHistoryandPhysicalExamsilentscream0618No ratings yet
- This Study Resource Was: Student Name: - Section: - Date of Patient CareDocument2 pagesThis Study Resource Was: Student Name: - Section: - Date of Patient CareSashaNo ratings yet
- Complete Respiratory Examination Checklist 365Document5 pagesComplete Respiratory Examination Checklist 365mohammed alrubaiaanNo ratings yet
- Approach To Unconscious PatientsDocument5 pagesApproach To Unconscious PatientsMary Joyce Ajero LadimoNo ratings yet
- NCM112 LP1 Transes - RosalesDocument4 pagesNCM112 LP1 Transes - RosalesChristine CalleyNo ratings yet
- 6 Parts: o Mental Status o Cranial Nerves o Sensory Function o Motor Function o Cerebellar Function o Reflexes 1. Cranial NervesDocument3 pages6 Parts: o Mental Status o Cranial Nerves o Sensory Function o Motor Function o Cerebellar Function o Reflexes 1. Cranial NervesTaraKyleUyNo ratings yet
- F0826 International Standards For Neurological Classification of SCI Worksheet HGHDGDocument25 pagesF0826 International Standards For Neurological Classification of SCI Worksheet HGHDGreeves_cool100% (1)
- CASE 1 Neuro PDFDocument23 pagesCASE 1 Neuro PDFthe KLAWNo ratings yet
- Git HistoryDocument18 pagesGit HistoryAhmed SallamNo ratings yet
- Sepsis Quick Reference GuideDocument1 pageSepsis Quick Reference GuideRavin DebieNo ratings yet
- Nursing Management of The Perioperative PatientDocument16 pagesNursing Management of The Perioperative Patientashdmb217No ratings yet
- Abdominal Examination ProcedureDocument5 pagesAbdominal Examination ProcedureAnamul hossainNo ratings yet
- Primary Trauma CareDocument48 pagesPrimary Trauma CareKABERA RENENo ratings yet
- Script ECEDocument4 pagesScript ECESleepyHead ˋωˊNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- Manual of First Aid Professional English: Part 3—Case StudiesFrom EverandManual of First Aid Professional English: Part 3—Case StudiesNo ratings yet
- English in Urgent Care Medicine – Anglictina V Urgentní Medicíne: Textbook – UcebniceFrom EverandEnglish in Urgent Care Medicine – Anglictina V Urgentní Medicíne: Textbook – UcebniceNo ratings yet
- Leg Med (Abortion)Document3 pagesLeg Med (Abortion)julietNo ratings yet
- MTLB Debate PRODocument3 pagesMTLB Debate PRORHODA MAE CAPUTOLNo ratings yet
- Preeclampsia and EclampsiaDocument24 pagesPreeclampsia and EclampsiaLuisa SarangayNo ratings yet
- BHP Formula No 55 Refrence - Bioplasgen 20 Homeopathic Medicine For Skin DiseasesDocument2 pagesBHP Formula No 55 Refrence - Bioplasgen 20 Homeopathic Medicine For Skin DiseasesKazy Habibur RahmanNo ratings yet
- Ophthalmology - Diseases of CorneaDocument18 pagesOphthalmology - Diseases of CorneajbtcmdtjjvNo ratings yet
- Doh Programs First 1000 Days Ni BabyDocument65 pagesDoh Programs First 1000 Days Ni BabyjpnachorNo ratings yet
- Test Report:: Patient Name:Mr Bahu Anil Kumar Sahu Patient IDDocument1 pageTest Report:: Patient Name:Mr Bahu Anil Kumar Sahu Patient IDANILNo ratings yet
- Municipal Summary Monitoring of Incidence On Violence Against Children (Vac) During The Covid-19 PandemicDocument2 pagesMunicipal Summary Monitoring of Incidence On Violence Against Children (Vac) During The Covid-19 PandemicDann MarrNo ratings yet
- Complications After AmputationDocument44 pagesComplications After AmputationGulzar AhmadNo ratings yet
- CHMP Post Authorisation Summary Positive Opinion Mounjaro II 07 - enDocument2 pagesCHMP Post Authorisation Summary Positive Opinion Mounjaro II 07 - enFRUNZANo ratings yet
- DR AK MedicineDocument1 pageDR AK MedicineShweta jainNo ratings yet
- NovoMix 30 FlexPen CM v15Document12 pagesNovoMix 30 FlexPen CM v15Nadia SalwaniNo ratings yet
- Vital SignsDocument5 pagesVital SignsFrances Kaye Sta. CruzNo ratings yet
- Neuromuscular and Other Diseases of The Chest WallDocument25 pagesNeuromuscular and Other Diseases of The Chest WallluckyNo ratings yet
- en Colitis TuberculosisDocument7 pagesen Colitis TuberculosisATIKA INDAH SARINo ratings yet
- Great Atlas of Dermatology IndexedDocument73 pagesGreat Atlas of Dermatology Indexedjohn pauloNo ratings yet
- CPH Lecture ReviewerDocument11 pagesCPH Lecture ReviewerAngel LadimNo ratings yet
- Pleural Effusion in A Patient With End-Stage Renal Disease - PMCDocument5 pagesPleural Effusion in A Patient With End-Stage Renal Disease - PMCCasemix rsudwaledNo ratings yet
- Noy 192Document10 pagesNoy 192Cleysser Antonio Custodio PolarNo ratings yet
- Exercises For Non Communicable DiseasesDocument32 pagesExercises For Non Communicable DiseasesParul ThakurNo ratings yet
- EPISODIC SOAP Note For UTIDocument40 pagesEPISODIC SOAP Note For UTIlagatduncan520No ratings yet
- Smile Dental ClinicDocument9 pagesSmile Dental ClinicADEA Group and PartnersNo ratings yet
- Case Study (Amit Mandal)Document7 pagesCase Study (Amit Mandal)Mukesh SelvanNo ratings yet
- What Are Normal Male Testosterone Levels by AgeDocument9 pagesWhat Are Normal Male Testosterone Levels by AgeMiltonNo ratings yet
- Efficacy of Erandamuladi Niruhabasti in Gridhasi A Case StudyDocument4 pagesEfficacy of Erandamuladi Niruhabasti in Gridhasi A Case StudyResearch ParkNo ratings yet
- ROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPDocument6 pagesROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPkimberly quitonNo ratings yet
- NCP Hyperbilirubinemia IIDocument4 pagesNCP Hyperbilirubinemia IISandyNo ratings yet
- Heat Illness Prevention ProgramDocument7 pagesHeat Illness Prevention ProgramSPIQCNo ratings yet
- Research 1Document22 pagesResearch 1Biplov RoyNo ratings yet
- Vocal Cord ParalysisDocument26 pagesVocal Cord ParalysisELIA RICHARDNo ratings yet