Professional Documents
Culture Documents
Peds General Profoma-1
Peds General Profoma-1
Uploaded by
Harikrishna Elangovan0 ratings0% found this document useful (0 votes)
10 views4 pagesCopyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
Download as pdf
0 ratings0% found this document useful (0 votes)
10 views4 pagesPeds General Profoma-1
Peds General Profoma-1
Uploaded by
Harikrishna ElangovanCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
Download as pdf
You are on page 1of 4
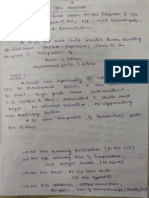
PRESENTATION OF PAEDIATRIC CASE.A PROTOCOL -Dr.C.NAGARAJAN ,
Prof.of.Paediatrics
1 Name ,Age, Sex---Name-( ,Cong. anomalies). Sex—sex linked disorders-eg.-
Haemophilia A,B, DMD, Vit. D resistant Rickets.( Age—completed years only)
2. Address—Epidemiology of diseases ( eg. Malaria, Kala azar, Filariasis ete.)
3. Informant—Mother, Father, Grandmother, Others whose reliabity is Good! Fair/ Poor
4. Complaints—i. Presenting complaint in patient’s/informant’s own words
1,2.3,4 ete. in ascending order Main complaint should be stressed.
5 History of presenting illness—Every complaint should be briefly elaborated in
medical terms, Nature, time of occurrence, progress/ course,precipitating, aggrevating &
relieving factors, possible aetiological factors, severity, frequency, diurnal& postural
variations, improvement with trt. etc. to be elaborated. Positive history first, Negative
history next
6. Past history — whether the patient has suffered from same type of illness in the past,
admitted, investigated & treated, nature of trt.. H/O. any related illness -eg. Portal
Hypertension—umbilical catheterization umb. sepsis to be elicited
7. Family History—Total no. of children in the family, Birth order of this child,
Consanguinous/ non- consanguinous parents, degree of consanguinity, other children
suffer from such illness.any congenital/ genetic disorders in the family. Pedigree chart to
be put(Autosomal Recessive inheritance common in consanguinity)
8.Antenatal history—Age of the mother at conception, AN visits, immunization
details,H/O ingestion of Abortifaecients,H/O X-ray exposure, H/O TORCH infection,
H/O systemic maternal illness -Diab,, HT, PIT, H/O Antithyroid, antiepileptic,
antidiabetic, anticancerous drugs, alcohol etc.
9. Natal—Delivery--FTND/ Preterm- Instrumental/ assisted/ LSCS delivery, cried well
after birth, resuscitation procedures,Breast feeding started -----hours after birth,
10. Postnatal—H/O breathing difficulty, feeding difficulty, cyanosis, scizures, jaundice...
umbilical sepsis,umb. vein catheterization, biood transfusion etc.
11.Developmental history—Developmental milestones- Gross motor, Fine motor,
Social& Adaptive, Speech -normal/ delayed. If delay +, nature of delay—expected
milestones, present status, devpt.al age to be elaborated—Refer Devpt.al milestones .
Delay is global or confined to one area- to be mentioned.
12.Diet( Nutrition) history—How long BF continued, weaning started when, diet menu,
calorie’ protein required/consumed, calorie gap/ protein gap, measures of bridging the
gap ete. In PEM case, history should be elaborate& complete.
13.Immunisation history--immunized as per age, Immunisation at various ages , last/
recent immunization, (UIP knowledge ~a must)
14. Socio-economic history—total members! total caring members, total monthly
income, per capita income, status—LIG, MIG, HIG.( Upper/ Upper middle/ Lower!
Lower middle/ High- Kuppusamy's scale-2007) Living in pucca house/ katcha-low
thatched roof, ventilation facilities, too many members in the family-overcrowding,
drinking water supply, sewage disposal etc., pet animals
15. Environmental history—Living in slum, sanitation& water supply, cattles ind
around, sewage disposal
16. Contact history—contact with TB, Leprosy, Exanthem or any other communicable
disease either in the family or in the neighbourhood—(to be mentioned in relevant cases
only.)
GENERAL EXAMINATION
Conscious, Alert, Active, Cooperative,Posture
_ Febrile’ Afebrile, comfortable/ Dyspnocic/ Tachypnoeic/ Toxic.
a) PICCLE—Pallor,leterus, Cyanosis, Clubbing, Lymphadenopathy, oEdema
~b) Anthropometry
1.Weight-—-----kgs
2.Height----- cms
3. Mid-arm circumference---—-cms(I-S years)
st circumference----cms (New-borns)
circumference----cms ( Micro/ Macrocephaly)
R un, Volume, Tension, Condition of the vessel wall, all
elt, any Radio-Radial /Radio- Femoral delay(.Rate per one min.)
UL lying/ sitting posture
mminal/ abdomino-thoracic, regular’ irregular
n necessary)
ook for the following. Ifeverything is normal, say no
LH ¢ad—Micro/Macrocephaly, AF/ PF, Flat occiput, Frontal bossing
2.Hair-Sparse, Alopacia —areata/ totalis, Hypopigmentation
“3 Ears----Low- set earsASOM/CSOM, Pre-auricular sinus, skin tags.
4, Eyes—Upward/ downward slant, Hypertelorism, Epicanthie folds, Cataract, Proptosis,
Nystagmus, Vit. A def signs. Ptosis,Periorbital oedema, sunken eyes, KF ring.
S.Face—Mangoloid , Haemolytic, Coarse facies of Cretin, MPS, Cushingoid,
6. Nose—Depressed bridge , Upturned nostrils
7.Mouth—Microstomia, Large tongue, Ariboflavinosis, Aphthous ulcer, Dental caries,
Malocclusion,, Protruding teeth, Cleft Lip/ Palate, Facial palsy, High-arched palate,
‘Micro/ Macro / Retro gnathia
8, Neck—Webbing, Torticollis, Short neck , Low hairline
9. Chest—Widely placed nipples’ supernumery nipples, Gynaecomastia, Pectus
Excavatum/ Carinatum, Ricketty rosary/ Scorbutic. rosary
10. Abd—Umb. Hernia, Ing. Hernia
11. Genitalia—Hydrocele, Micropenis, Hypospadias, Chordae, Cryptorchidism,
Ambiguous Genitalia
12. Skeletal—Upper limb— Proximal shortening, Simian crease, Cleinodactyly.
Polydactyly, Syndactyly. Lower limb—Genu valgus, varus,, CTEV, Club foot.
Kyphosis, Scoliosis, Kyphoscoliosis, Gibbus
‘Skin—Macule, Papule, Vesicle,, Pustule, Wheal, Petechiae,
ra,Eechymosis,Hypo/ Hyperpimentation, Scabies, Mangolian blue
giomas, Telengiectasia, Spider Naevus, Salmon patch, Portwine stain,
marginatuny nodosum, Café-au-lait spots
eous Markers (CNS cases only )
ait spots-->Smm &>6 no. in prepubertal /.> 15mm8&>6 in no. in post-
freckling,
mented patches -2mm diameter, 2 or more
nodules- Hamartomas in iris,
‘more neurofibromas’ | plexiform (Neurofibroma):
hagreen patches,
macule,Sub- ungual fibroma,
Adenoma sebaceum (Tuberous sclerosis);,
9. Pilo-nidal sinus,/ dimp
occulta);
10. ,Capillary haemangioma (Sturge-weber);,
11. Telengiectasia( Ataxia Telengiectasia)
le, Tuft of hair in sacral area ( Spina bifida’ Spina bifida
AE RCC Re I AC a A
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (898)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Null 8Document48 pagesNull 8Harikrishna ElangovanNo ratings yet
- Obs Osce TotalDocument18 pagesObs Osce TotalHarikrishna ElangovanNo ratings yet
- Og 1 1Document21 pagesOg 1 1Harikrishna ElangovanNo ratings yet
- Image To PDF 20240318 12.42.34Document16 pagesImage To PDF 20240318 12.42.34Harikrishna ElangovanNo ratings yet
- Fever With SM - UNIV 4Document6 pagesFever With SM - UNIV 4Harikrishna ElangovanNo ratings yet
- Hearing AidDocument24 pagesHearing AidHarikrishna ElangovanNo ratings yet
- CP Univ Case 7Document9 pagesCP Univ Case 7Harikrishna ElangovanNo ratings yet
- UitgDocument26 pagesUitgHarikrishna ElangovanNo ratings yet
- BreechDocument35 pagesBreechHarikrishna ElangovanNo ratings yet
- CP Univ Case-1Document9 pagesCP Univ Case-1Harikrishna ElangovanNo ratings yet
- Newborn CaseDocument7 pagesNewborn CaseHarikrishna ElangovanNo ratings yet
- Ariyur, Puducherry. Ph.0413-2644435, 2644482 Department of Pathology Cell Injury OSPE Charts (Competency: 2.8)Document5 pagesAriyur, Puducherry. Ph.0413-2644435, 2644482 Department of Pathology Cell Injury OSPE Charts (Competency: 2.8)Harikrishna ElangovanNo ratings yet
- Paed. Vaccines 1Document21 pagesPaed. Vaccines 1Harikrishna ElangovanNo ratings yet
- Paed DrugsDocument26 pagesPaed DrugsHarikrishna ElangovanNo ratings yet