Professional Documents
Culture Documents
Endocarditis Infecciosa
Endocarditis Infecciosa
Uploaded by
JOSECopyright:
Available Formats
You might also like
- 4 First Aid BFPDocument52 pages4 First Aid BFPJoyce FalladoNo ratings yet
- 17-Infective EndocarditisDocument17 pages17-Infective Endocarditisمصطفى محمد جواد كاظمNo ratings yet
- Robert So JR Batch 15 Taylors University 2018/2023Document6 pagesRobert So JR Batch 15 Taylors University 2018/2023Robert So Jr100% (1)
- Infective Endocarditis-2023Document40 pagesInfective Endocarditis-2023يزن الحارثيNo ratings yet
- Non Rheumatic EndocarditisDocument29 pagesNon Rheumatic EndocarditisSindhujaNo ratings yet
- F.05 The HeartDocument7 pagesF.05 The HeartPAUL ALINGKAYONNo ratings yet
- Infections and InflammationDocument10 pagesInfections and InflammationNarimèneNo ratings yet
- Pathology and Pathogenesis of Infective Endocarditis in Native Heart ValvesDocument8 pagesPathology and Pathogenesis of Infective Endocarditis in Native Heart ValvesIrina TănaseNo ratings yet
- Rheumatic Heart Disease: Infectious Diseases of The HeartDocument5 pagesRheumatic Heart Disease: Infectious Diseases of The HeartVoid LessNo ratings yet
- Endocardial PathologyDocument35 pagesEndocardial PathologyAsem AlhazmiNo ratings yet
- Infective EndocarditisDocument30 pagesInfective EndocarditisAlfrin Antony100% (3)
- Infective EndocarditisDocument4 pagesInfective EndocarditisXiang Yun TanNo ratings yet
- Heart BNHADocument13 pagesHeart BNHAX OloGyNo ratings yet
- Infective EndocarditisDocument3 pagesInfective EndocarditisAlfrin Antony80% (5)
- Infective EndocarditisDocument3 pagesInfective EndocarditisRechelle CabagingNo ratings yet
- Infective Endocarditis: PathogenesisDocument23 pagesInfective Endocarditis: PathogenesisSyauqie AlhasniNo ratings yet
- 2022 Pathogenesis, Diagnosis, Antimicrobial Therapy and Management of Infective Endocarditis, and Its ComplicationsDocument7 pages2022 Pathogenesis, Diagnosis, Antimicrobial Therapy and Management of Infective Endocarditis, and Its ComplicationsstedorasNo ratings yet
- Cardio-Vascular PathogyDocument54 pagesCardio-Vascular PathogyArleen MatincaNo ratings yet
- Endokarditis, Miokarditis Perikarditis: Blok KardiovaskularDocument31 pagesEndokarditis, Miokarditis Perikarditis: Blok KardiovaskularTiara RamliNo ratings yet
- Baliuag University College of Nursing Baliuag, BulacanDocument6 pagesBaliuag University College of Nursing Baliuag, Bulacanelmo_lalaNo ratings yet
- Rheumatic Heart DiseaseDocument4 pagesRheumatic Heart DiseaseAlfrin Antony100% (3)
- Most Commonly BacterialDocument2 pagesMost Commonly BacterialMaryam FadahNo ratings yet
- F.06 Diseases of The HeartDocument5 pagesF.06 Diseases of The HeartPAUL ALINGKAYONNo ratings yet
- Chapter 37 WorksheetDocument5 pagesChapter 37 Worksheetkristineconde89No ratings yet
- Dilated Cardiomyopathy Notes AtfDocument15 pagesDilated Cardiomyopathy Notes AtfSingha ChangsiriwatanaNo ratings yet
- Vasculitis by VinhDocument4 pagesVasculitis by VinhTovin NguyenNo ratings yet
- Patho - Rheumatic Heart DiseaseDocument26 pagesPatho - Rheumatic Heart DiseaseMahmoud hilmyNo ratings yet
- Cardiovascular Pathology - 020) Aortic Valve Stenosis and Regurgitation (Notes)Document13 pagesCardiovascular Pathology - 020) Aortic Valve Stenosis and Regurgitation (Notes)arga setyo adjiNo ratings yet
- Infective Endocarditis: Christine Joy F. Baquiran MED-3CDocument46 pagesInfective Endocarditis: Christine Joy F. Baquiran MED-3CAbigail SabinoNo ratings yet
- Pathology MRCS BDocument77 pagesPathology MRCS BHina MalikNo ratings yet
- EndicarditisDocument10 pagesEndicarditisAkarsh RamNo ratings yet
- Week 1Document7 pagesWeek 1Balkess NajemNo ratings yet
- Infective - EndocarditisDocument6 pagesInfective - EndocarditisHala AhmadNo ratings yet
- Rheumatic Fever & Infective EndocarditisDocument46 pagesRheumatic Fever & Infective EndocarditisMosab MasoudNo ratings yet
- Summer AssignmentDocument2 pagesSummer AssignmenttewetanNo ratings yet
- EndocarditisDocument35 pagesEndocarditisKatret ElnadaNo ratings yet
- Clinical Cases of Infectious Endocarditis in CatsDocument12 pagesClinical Cases of Infectious Endocarditis in CatsAna AldazNo ratings yet
- Boards - Gen PathDocument12 pagesBoards - Gen PathJoyce EbolNo ratings yet
- Valvular Heart DiseaseDocument8 pagesValvular Heart DiseaseHASNIZZAM BIN AHMAD AMIN -No ratings yet
- Valvular Heart DiseasesDocument29 pagesValvular Heart Diseasesbpt2No ratings yet
- Coronary Arteritis DDDocument6 pagesCoronary Arteritis DDvam buddhaNo ratings yet
- Seminar On Rhuematic Heart DiseaseDocument16 pagesSeminar On Rhuematic Heart Diseasenaga maniNo ratings yet
- Inflammatory Disorders A5Document5 pagesInflammatory Disorders A5FrancheskaNo ratings yet
- Arrhythmias - PrintingDocument5 pagesArrhythmias - Printingibrahim said faidNo ratings yet
- Multiple Organ Dysfunction SyndromeDocument4 pagesMultiple Organ Dysfunction SyndromeJenny SisonNo ratings yet
- Intracerebral Hemorrhage ICH Etiology, AtfDocument10 pagesIntracerebral Hemorrhage ICH Etiology, Atfsiti.220010019No ratings yet
- Ards PDFDocument20 pagesArds PDFRuki HartawanNo ratings yet
- 11.3 Chapter 23-Pt 2 Cardiovascular - Lecture - W13Document10 pages11.3 Chapter 23-Pt 2 Cardiovascular - Lecture - W13Hiba V.ANo ratings yet
- Katup Jantung: - Mempertahankan Aliran DGN Satu Arah Tetap - Membuka/Menutup PasifDocument24 pagesKatup Jantung: - Mempertahankan Aliran DGN Satu Arah Tetap - Membuka/Menutup PasifandreNo ratings yet
- Difference Between Rheumatic Heart Disease and Infective EndocarditisDocument7 pagesDifference Between Rheumatic Heart Disease and Infective Endocarditis<_>No ratings yet
- Rheumatic Heart Disease: Dr. Gehan Mohammed Dr. Abdelaty ShawkyDocument46 pagesRheumatic Heart Disease: Dr. Gehan Mohammed Dr. Abdelaty ShawkyimanNo ratings yet
- Ajith Kumar P MPT Cardiopulmonary SciencesDocument30 pagesAjith Kumar P MPT Cardiopulmonary SciencesSuhana JahangeerNo ratings yet
- Inflammation of Any Layer of Heart (Endo, Myo, Peri) : Damaging Valves, Muscles and /or Pericardial LiningsDocument15 pagesInflammation of Any Layer of Heart (Endo, Myo, Peri) : Damaging Valves, Muscles and /or Pericardial LiningsNur SetsuNo ratings yet
- Covid and Ebola MsDocument7 pagesCovid and Ebola MsAimee Rochelle MaesaNo ratings yet
- Infectious Disease of The HeartDocument3 pagesInfectious Disease of The HeartClaire GidoNo ratings yet
- MODULE 3 Disorders of Primary HemostasisDocument13 pagesMODULE 3 Disorders of Primary HemostasisLancer BlazeNo ratings yet
- Infective Endocarditis SAQ ChatGPTDocument2 pagesInfective Endocarditis SAQ ChatGPTGus LionsNo ratings yet
- Cvspa04 Ihd and MiDocument8 pagesCvspa04 Ihd and MiRobert So JrNo ratings yet
- P.20 Hemodynamic Disorders, Thromboembolic Disease, and Shock - Part 6 (Dr. Espiritu) (09-11-18)Document3 pagesP.20 Hemodynamic Disorders, Thromboembolic Disease, and Shock - Part 6 (Dr. Espiritu) (09-11-18)Raymund Dan AldabaNo ratings yet
- Thorn in the Flesh - How the Corona "Vaccine" Induced Spike Protein Causes Damage: (Author's Translation without Proofreading)From EverandThorn in the Flesh - How the Corona "Vaccine" Induced Spike Protein Causes Damage: (Author's Translation without Proofreading)No ratings yet
- Parotid Gland HistopathologyDocument32 pagesParotid Gland HistopathologyDrey Keesey CatzNo ratings yet
- 1 s2.0 S0894731723006223 MainDocument52 pages1 s2.0 S0894731723006223 Mainpaul00040No ratings yet
- (B-0270) Day Surgery Procedure UnitDocument22 pages(B-0270) Day Surgery Procedure UnitAhmad Gamal Elden MAhanyNo ratings yet
- Dr. YSR Aarogyasri Health Care TrustDocument23 pagesDr. YSR Aarogyasri Health Care Trusttatapudi mohanNo ratings yet
- Upper Gi BleedingDocument3 pagesUpper Gi BleedingJohiarra TabigneNo ratings yet
- Unusual Presentation of Recurrent Appendicitis - A Rare Case Report and Literature ReviewDocument4 pagesUnusual Presentation of Recurrent Appendicitis - A Rare Case Report and Literature ReviewMirachel AugustNo ratings yet
- RADSCIENCESDocument24 pagesRADSCIENCESYael Opeña AlipNo ratings yet
- Treatment ERSDDocument6 pagesTreatment ERSDAsep ArdiNo ratings yet
- Lista de Lucrari 3Document30 pagesLista de Lucrari 3Anonymous 0epuGwQTJNo ratings yet
- A Prospective Study On The Maternal Outcome in Cases of Previous One Cesarean SectionDocument6 pagesA Prospective Study On The Maternal Outcome in Cases of Previous One Cesarean SectionIJAR JOURNALNo ratings yet
- Subject: - Topics: Cholecystitis: Adult Health NursingDocument17 pagesSubject: - Topics: Cholecystitis: Adult Health NursingUzma KhanNo ratings yet
- LifePak 12 InstructionsDocument288 pagesLifePak 12 InstructionsthedrmikeNo ratings yet
- CPRDocument41 pagesCPRPreethi BNo ratings yet
- Open Access Atlas of Otolaryngology, Head & Neck Operative SurgeryDocument3 pagesOpen Access Atlas of Otolaryngology, Head & Neck Operative SurgeryMiggy GNo ratings yet
- Lesson PlanDocument22 pagesLesson PlanPramila AdhikariNo ratings yet
- Thoracic Segmental Spinal Anaesthesia/ General Anaesthesia For Laproscopy SurgeryDocument8 pagesThoracic Segmental Spinal Anaesthesia/ General Anaesthesia For Laproscopy SurgeryIJAR JOURNALNo ratings yet
- Case Study 55-3Document5 pagesCase Study 55-3jillNo ratings yet
- Biologic and Biophysical Technologies. FINALDocument28 pagesBiologic and Biophysical Technologies. FINALRafael Miguel MallillinNo ratings yet
- Science 9 1.4 Circulation of Blood in The BodyDocument13 pagesScience 9 1.4 Circulation of Blood in The BodyChad Kirsten Mier LustreNo ratings yet
- Dialysis Technician ResumeDocument6 pagesDialysis Technician Resumef5dbf38y100% (3)
- Incisive CT Produkt SpesifikacijoniDocument12 pagesIncisive CT Produkt SpesifikacijoniKaimiSuresh100% (1)
- March 21 MRIDocument2 pagesMarch 21 MRIBhavik ChavdaNo ratings yet
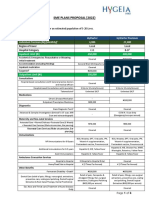
- Hygeia HMO SME Plans Proposal - 2022 - FinalDocument4 pagesHygeia HMO SME Plans Proposal - 2022 - FinalBanks C. GeorgeNo ratings yet
- Prevention of Infective Endocarditis AHA EditDocument17 pagesPrevention of Infective Endocarditis AHA EditDampee ReturnNo ratings yet
- Manual Lymphatic Drainage Versus Exercise in The Early PostoperativeDocument7 pagesManual Lymphatic Drainage Versus Exercise in The Early PostoperativeSofia Adão da FonsecaNo ratings yet
- Gastrostomy Feeding ProcedureDocument5 pagesGastrostomy Feeding ProcedureRohini RaiNo ratings yet
- Anesthesia 1Document55 pagesAnesthesia 1Mah ShawdNo ratings yet
- Most Requested Items/locations: Emergency Department Elevators Pedway Path Welcome CenterDocument2 pagesMost Requested Items/locations: Emergency Department Elevators Pedway Path Welcome CenterTERRENCENo ratings yet
- Barium Swallow Meal Follow-Through MealDocument2 pagesBarium Swallow Meal Follow-Through MealPervez Ahmad AhmadNo ratings yet
Endocarditis Infecciosa
Endocarditis Infecciosa
Uploaded by
JOSEOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Endocarditis Infecciosa
Endocarditis Infecciosa
Uploaded by
JOSECopyright:
Available Formats
Last edited: 3/21/2022
INFECTIVE ENDOCARDITIS
Infective Endocarditis Medical Editor: Gerard Jude Loyola
OUTLINE
I) MAIN HEADING IN IV) REVIEW QUESTIONS
II) CONTENT FORMATTING V) REFRENCES
III) APPENDIX
I) CAUSES (C) ABNORMAL VALVES
(A) DEFINITION
Endocarditis: inflammation of the endocardium
o Inflammation, damage or destruction of the
endocardium → forms microbial vegetations
Recall: The endocardium lines the ventricles and more
importantly, the valves of the heart
(B) TYPES OF INFECTIVE ENDOCARDITIS (IE) Figure 2. Causes of abnormal valves.
Predisposes individuals to IE
Endocardial cells release prostacyclins (PGI2) and NO →
inhibits platelet aggregation
o Damage to endocardial cells results to inability to
release PGI2 and NO → cannot inhibit platelet
aggregation → platelets attach to exposed collagen in
damaged endocardium → platelet plug forms →
fibrin mesh stabilizes the platelet plug
Figure 1. Types of infective endocarditis.
(1) Causes of Damaged Heart Valves
(1) Acute Infective Endocarditis Table 2. Causes of abnormal heart valves.
Patients look really septic (really sick individuals) Causes Rationale
o Hypotensive, high fever, new heart failure symptoms
and septic emboli Rheumatic heart Excessive amounts of antibodies
disease that damage the endocardial lining
Due to a highly virulent pathogen: S. aureus
Pathogen damages the
(2) Subacute Infective Endocarditis History of
endocardium → fibrosis exposing
infective
the collagen, platelet plug forms,
Nonspecific symptoms: low-grade fever, dyspnea and endocarditis
etc.
fatiguability
More difficult to diagnose Patients with bicuspid aortic valve
Bicuspid aortic
Usually due to a low virulent pathogen: S. viridans form calcifications and very
valve
susceptible to IE
Table 1. Acute vs subacute IE (Harrison's).
Mitral valve Damage to the valve leaflets
Acute IE Subacute IE prolapse causing MV degeneration
S. aureus VSD, truncus arteriosus, TOF, etc
(sometimes) Congenital heart
S. aureus defects Underlying valvular damage
S. viridans
B-hemolytic increases the risk of IE
Enterococci
streptococci
Usual Etiology HACEK Very high risk for binding of
Pneumococci Prosthetic valves
Coagulase- pathogens, platelets and thrombin
Aerobic gram-
negative
negative bacilli
staph/strep
(prosthetic valves) NBTEs: non-bacterial thromboemboli
o Composed of platelets and fibrin
Low-grade fever
High-grade fever o Increases risk for bacterial infection
(rarely >39.4˚C)
(39.4-40˚C)
Manifestations Weight loss,
Acute/decompen-
abdominal
sated heart failure
symptoms, pleurisy
Rapid
Indolent, subtle,
Hematogenously
and non-specific
seeded
Course symptom
extracardiac sites
Rarely
Complications are
metastasizes
common
Prognosis Poor (if untreated) Better prognosis
Infective Endocarditis CARDIOVASCULAR PATHOLOGY: Note #23. 1 of 12
(2) S. viridans
(D) BACTEREMIA
Remember: most common cause of subacute IE
Gram positive bacteria
Part of the oral flora
o So any break in the normal barriers introduces the
bacteria in the bloodstream
Examples:
o Poor dentition
o Dental procedures (cleaning and root canal)
Subtypes of S. viridans
o S. mitis
o S. mutans
o S. oralis
o S. sanguinis
o S. milleri
o S. sopranus
(3) HACEK
Stands for Haemophilus spp, Aggregatibacter spp,
Cardiobacterium spp, Eikenella carodens and
Kingella spp
Gram negative rods
Causes subacute IE
Part of the oral flora
o Has similar mechanism of introduction to S. viridans
(4) Enterococcus
Part of the urogenitary tract
Causes of spread:
Figure 3. Bacterial and fungal organisms that can cause o UTI, specially pyelonephritis
infective endocarditis. Bacteria can enter the renal circulation
NBTEs increase the opportunity for bacterial infection, o Catheter, urinary stent and other urogenitary
multiply and colonize → form microbial vegetations procedures
leading to damaged valves Provides opportunity for the bacteria to enter
through a break in the integrity of the walls
(1) S. aureus
(5) Streptococcus gallolyticus
Remember: most common cause of acute IE
Gram-positive bacteria AKA Strep bovis
One of the few types of pathogens that can damage a Associated with the following:
healthy valve o Colorectal cancer
o Other bacteria commonly damage a compromised o Inflammatory bowel disease (ulcerative colitis or
valve Crohn’s disease)
(6) Staphylococcus epidermidis
Table 3. Common causes of S. aureus spread in the Gram positive bacteria
bloodstream.
Loves prosthetic valves and other prosthetic hardwares
Causes Rationale (AICD or pacemakers)
Remember that S. aureus is part of Prominent in the skin
the skin flora Can travel the bloodstream through a break in the skin
o Skin abscesses form a break o PIV, PICC line, CVC
Skin abscesses
in the skin → allowing spread
(7) Candida
of the bacteria in the
bloodstream Fungi
Not very common pathogen that can cause IE except for
Using dirty needles that increases
IV drug abuse risk of injecting bacteria in the immunocompromised patients (e.g. HIV, s/p transplant)
bloodstream o In immunocompromised individuals, neutrophils and
lymphocytes cannot clear Candida in the bloodstream
Example: Central venous
Catheters and
catheters
prosthetic
o Catheter is pushed through
hardware
the skin allowing the bacteria
introduction
to reach the bloodstream
Prosthetic heart
valves, AICD: automated implanted
pacemakers, cardioverter defibrillator
AICD
2 of 12 CARDIOVASCULAR PATHOLOGY: Note #23. Infective Endocarditis
II) CLINICAL FEATURES AND PHYSICAL EXAMINATION
(C) ↑VALVE DESTRUCTION
Figure 4. Pathophysiology of infective endocarditis.
Recap:
Inflammation of the endocardium from abnormal valve and
bacteremia Figure 6. Preference of heart valves in infective
o Exposure of the underlying collagen and formation of endocarditis.
platelet plug
Left-side is more commonly affected than right-
o Platelet plug stabilized by fibrin → NBTEs
side
o Bacteremia → pathogen sticks to NBTE in the surface →
o Recall: left side – mitral and aortic; right side –
infiltrates the NBTE → microbial vegetation
tricuspid and pulmonic valves
o Vegetations stimulate the immune system bringing
o Commonly affected valves arranged in order: (R)
neutrophils, macrophages, etc. → increases production of
mitral > aortic > (L) tricuspid > pulmonic
cytokines (IL-1, IL-6, TNF-⍺) EXCEPT for IV drug abusers with S. aureus
Summary: in which the tricuspid valve is preferred
NBTE formation • Mnemonic: TRI not doing drugs
Microbial vegetations
Immune response (1) Mitral Valve Destruction
(A) IMMUNE RESPONSE
Immune cells (macrophages and neutrophils) attack the
pathogens releasing ROS and proteases
o Microbes release proteases as well
Proteases and ROS start eroding both the valvular and
perivalvular tissue causing valve and perivalvular destruction
o One of the worst case scenarios
o Creates an opportunity for abscess formation and
prosthetic valve dysfunction
Vegetations may flick off becoming septic emboli
o Similar to clots in atrial fibrillation Figure 7. Acute left-sided heart failure symptoms from
o May be right-sided or left-sided (more common) aortic and mitral valve destruction.
MV is degenerated or chewed away → shortening of
Plasma cells produce antibodies (Ab) against the microbes
the MV → allows backflow of the blood → new MV
attacking bacterial antigens (Ag) → circulating Ab-Ag
regurgitation murmur
complexes (also called immune complexes) which deposit
Accumulated regurgitated blood flow back to the LV
throughout the body
→ overfilling of blood → blood accumulation in the
(B) ↑CYTOKINES left side of the heart → back up of blood in the lungs
→ pulmonary edema
Every time the ventricle contracts, accumulated
blood in the LV can be pushed to the left atrium →
↓stroke volume → ↓cardiac output → hypotension
→ cardiogenic shock
o Example: normal SV is 70 mL; in mitral
regurgitation, 50 mL is pushed to the aorta while
20 mL is pushed to the LA → decreased stroke
volume
(2) Aortic Valve Destruction
New aortic regurgitation
Pulmonary edema
Figure 5. Clinical manifestations from increased cytokines. Take Hypotension
note that this can occur at any valve. (3) Acute Left-Sided Heart Failure
IL-1, IL-6 and TNF-⍺
Due to involvement of aortic and/or mitral valves
o Stimulates the hypothalamus to release PGE2 →
Symptoms:
increases the body temperature → fever
o Shortness of breath due to pulmonary edema
o Stimulates the bone marrow to produce white blood cells
o Dyspnea on exertion
→ leukocytosis (CBC)
o Paroxysmal nocturnal dyspnea
“We need more help”
o Stimulates the liver to produce acute phase reactants
o Hypoxemia
(↑↑↑CRP and ↑↑ESR)
o Hypotension
Alerting the body of increased inflammation
o Cold extremities (ill-perfused extremities)
Very non-specific
o New aortic and/or mitral regurgitation
Infective Endocarditis CARDIOVASCULAR PATHOLOGY: Note #23. 3 of 12
(D) PERIVALVULAR DESTRUCTION (2) Left-Sided Emboli
Figure 8. Perivalvular destruction in native and prosthetic
valves.
Vegetation on the valve eats away the perivalvular tissue
leading to formation of annular abscess
o Perivalvular destruction → abscess
(1) Aortic Valve
Perivalvular destruction in the aortic valve produces
murmur due to inflammation and dilatation of the aorta
o Annular destruction may also involve the AV node
and the bundle system leading to AV blocks and Figure 10. Left-sided emboli causing a variety of clinical
manifestations.
bundle branch blocks
Flicking off pieces of the vegetations moving to the
(2) Mitral Valve systemic circulation going to different organs of the body
Perivalvular vegetations in the mitral valve can infiltrate (Table 3)
the pericardium → pericarditis ± pericardial effusion
Table 4. Effects of infiltration of vegetation to different organs
(3) Prosthetic Valves and blood vessels.
Perivalvular tissues should anchor the prosthetic valve Symptoms
o Destruction of the perivalvular tissue separates it from Organ/Vessels Complication or Clinical
the prosthetic valve leading to prosthetic valve Signs
dehiscence Acute ischemic Neural
Carotid system
Prosthetic valve dehiscence produce a leak into the stroke deficits,
ventricle leading to perivalvular leak dysarthria,
o Leads to prosthetic valve dysfunction ICH, subarachnoid gait
Brain and its preferences,
hemorrhage
(E) SEPTIC EMBOLI vessels sensory
Brain abscesses
deficits
(1) Right-Sided Emboli
Vessels of the Splinter hemorrhages
nailbeds (Figure 11)
Janeway lesions
Vessels to the
(Figure 12)
palms and
o Painless
soles
lesions
Discitis or spondylitis
→ osteomyelitis
Vertebrae o Destruction of Back pain
Figure 9. Right-sided emboli resulting to pulmonary embolism
and lung abscesses.
the discs and
vertebrae
Flicking off pieces of the vegetations in the tricuspid valve
→ moves to the pulmonary circulation → occludes blood Hot painful
Joint Tissue Septic arthritis
flow → pulmonary embolism tender joints
o Symptoms: Significant
Dyspnea Spleen and its Splenic infarct amount of
Increased sputum vessels Splenic abscess abdominal
Smaller emboli can pass through the capillaries and pain
infiltrate the lung tissue → lung abscesses Flank pain
• Small enough and can infiltrate to the lung Kidney vessels Renal infarct ↓urine output
tissue → lung abscesses ↑BUN or Cr
4 of 12 CARDIOVASCULAR PATHOLOGY: Note #23. Infective Endocarditis
Figure 11. Splinter hemorrhages. Figure 14. Roth spots [Arora et al, 2012].
Figure 15. Osler's nodes [Dermnet NZ].
Figure 12. Janeway lesions on the hypothenar eminence [Arora et Table 5. Summary of clinical findings in IE.
al, 2012].
Fever
(F) ↑IMMUNE COMPLEXES Leukocytosis
↑Cytokines
↑Acute phase reactants (CRP and
ESR)
L >>>>> R
o Mitral > Aortic > Tricuspid >
↑Valve Pulmonary
destruction MV or aortic valve regurgitation murmur
Pulmonary edema
Hypotension
Abscess
Aortic valve:
o Murmur
o AV blocks and bundle branch
↑Perivalvular blocks
destruction Mitral valve:
o Pericarditis ± pericardial effusion
Prosthetic valves:
o Prosthetic valve dehiscence →
prosthetic valve dysfunction
Figure 13. Increased immune complex deposition forming Right-sided
different clinical manifestations. o Pulmonary embolism
Immune complexes can be distributed to the systemic o Lung abscess
circulation and can be deposited to the following: Left-sided
o Pulp of the digits producing painful lesions called o Acute ischemic stroke
Osler’s nodes (Figure 15) o ICH, subarachnoid hemorrhage
Septic o Brain abscess
Mnemonic: Osler ouch! emboli
o Retina leading to hemorrhagic lesions called Roth o Splinter hemorrhage
spots (Figure 14) o Janeway lesions
o Discitis or spondylitis →
Symptom: Visual changes
osteomyelitis
o Glomerulus and glomerular tissue leading to their
o Septic arthritis
erosion once immune system attacks → leakage of o Splenic infarct, splenic abscess
blood (RBC) and plasma proteins (hematuria and o Renal infarct
proteinuria) → glomerulonephritis
Specific antibodies for Ab-Ag deposition process: Osler’s nodes
Immune Roth spots
rheumatoid factor (RF)
complexes Glomerulonephritis
Specific antibodies: Rheumatoid factor
Infective Endocarditis CARDIOVASCULAR PATHOLOGY: Note #23. 5 of 12
Purpose:
III) DIAGNOSIS o To prove that bacteremia is present
Looking for typical pathogens + Coxiella burnetii
(A) ECHOCARDIOGRAPHY o To narrow the antibiotics for specific pathogens
Three sets of blood culture is obtained
o Draw from different sites at different times
o Get a lot of blood to get a good number of potential
bacteria
o Aerobic, anaerobic and fungal cultures
o Remember that IE is an endovascular infection
meaning it’s continuous
Bacteremia is established when:
o ≥2 (+) blood cultures OR
o Persistently (+) blood cultures
(C) TESTS FOR SEPTIC EMBOLI
Figure 16. Diagnosis of IE with echocardiogram. Table 6. Tests for septic emboli.
Transthoracic Echocardiogram (TTE) Assess for presence of infarct,
o Looking at different views: subxiphoid, parasternal Brain MRI abscess or bleeds
long axis, short axis, apical, etc. o For patients with altered mental
o Provides a global visualization of the heart status
o However, it’s difficult to have a good look at the AV
and MV using this Spinal MRI Assess for discitis, osteomyelitis or
spinal cord abscess
Transesophageal Echocardiogram (TEE)
o High specificity and sensitivity (>90%) Splenic UTS
o Probe is swallowed allowing visualization of the or CT of Assess for splenic infarcts or
posterior aspect of the heart abdomen abscesses
and pelvis
o Another advantage is the visualization of other
complications such as ring abscesses
Can show renal vascular emboli
Look for the following: Look for signs of AKI:
o Vegetations Renal UTS o Basic metabolic panel (BMP) -
o New or worse regurgitation murmur ↑BUN, ↑Cr
Using Color Doppler o ↓urine output
o Prosthetic valve dehiscence
Physical Splinter hemorrhages and Janeway
Prosthetic valve rocking back and forth with
Exam lesions
perivalvular leak
o Perivalvular abscess (ring abscess)
CXR: opacities or abnormal nodular
More common in aortic than mitral valve Chest Xray vision → proceed to CT scan
or CT Scan CT: look for pulmonary emboli or
abscesses
Figure 17. Mitral valve vegetation shown on echocardiogram
[Cabell et al, 2003].
(B) BLOOD CULTURES
Figure 19. Diagnostic tests and imaging for septic emboli in IE.
Figure 18. Diagnosis of IE with blood cultures.
6 of 12 CARDIOVASCULAR PATHOLOGY: Note #23. Infective Endocarditis
(F) NON-INFECTIVE ENDOCARDITIS
(D) TESTS FOR IMMUNE COMPLEXES
Table 7. Tests for immune complexes.
Urinalysis (+) RBC casts, protein
with Look for signs of AKI:
microscopy o ↑BUN, ↑Cr, ↓urine output
Fundoscopy Check for presence of lesions
(hemorrhages) on the retina
Physical
Examination Osler’s nodes
Rheumatoid
Factor Positive RF
Figure 22. Non-infective endocarditis.
(1) Marantic Endocarditis
Pancreatic carcinoma
o Tumor produce cytokines that stimulate clot formation
→ microclots spread to the valves
o Microclots are non-septic emboli
(2) Libman-Sacks Endocarditis
Endocarditis from SLE (systemic lupus erythematosus)
o Body produces a lot of auto-Abs that increase
Figure 20. Diagnostic tests for immune complexes in IE. inflammation → increases activity of microthrombi
that form on the heart valves
(E) MODIFIED DUKE’S CRITERIA
Establishes the diagnosis of infective endocarditis when (3) Diagnosis
the following conditions are met: Manifestations:
o Two major criteria o Low-grade fevers
o One major criterium + three minor criteria o Little vegetations on the valves (on Echo)
o Five minor criteria o Valve dysfunction leading to heart murmurs
o (-) blood cultures
(1) Major Criteria
o Does not improve on antibiotics
(+) Echo findings It does not always mean non-infective
o Vegetations, murmur, PV dehiscence, abscess endocarditis; it may also mean IE that needs
(+) Blood culture surgery
o ≥2 (+) tests OR persistently (+) tests; AND (i) Biopsy
o Typical pathogens
o EXCEPT for Coxiella burnetii For confirmation
Does not need to meet the aforementioned
circumstances (ii) Look for underlying condition
More important
(2) Minor Criteria
CT of the abdomen or MRCP = pancreatic tumors
(+) Fever (≥38˚C or ≥100.4˚F) (+) SLE antibodies
(+) Predisposing factors:
o Factors for abnormal valves and/or bacteremia
IV) TREATMENT
(+) Septic emboli
(+) Immune phenomenon (A) ANTIBIOTICS
(+) Blood cultures not meeting major criteria
o <2 positive cultures or not persistently positive To clear the infection that causes problems such as
septic emboli, vegetations, etc.
Patients are sometimes hemodynamically unstable,
especially patients with acute IE, where cardiogenic
shock can occur
o Immediately start on empiric antibiotics after taking
the blood cultures
o On subacute IE, it’s possible to hold off the
antibiotics after taking the blood cultures unless they
are not as hemodynamically stable as possible
Figure 21. Modified Duke's criteria.
Infective Endocarditis CARDIOVASCULAR PATHOLOGY: Note #23. 7 of 12
(1) Empiric Antibiotics
Table 8. Summary of empiric Abx used in native and prosthetic
Depends upon the valve affected valve IE.
When blood cultures come back positive, narrow the
types of antibiotics depending the type of pathogens Prosthetic
Native Valve IE
Valve IE
(i) Native Valve IE Acute S. aureus (MSSA or MRSA)
Patho- S. epidermidis,
S. viridans,
gens Sub- S. viridans,
HACEK,
acute HACEK,
Enterococci
Enterococci
Vancomycin +
Vancomycin +
Cefepime +
Acute Cefazolin/
Gentamicin ±
Nafcillin
Rifampin
Abx Vancomycin +
Vancomycin + Ampicillin-
Sub- Ampicillin- Sulbactam (or
Figure 23. Antibiotics used in native valve IE.
acute Sulbactam (or Ceftriaxone) +
Vegetations on the mitral, aortic, tricuspid or pulmonary Ceftriaxone) Gentamicin ±
valves Rifampin
Establish whether acute or subacute
Acute IE (B) SURGERY
o S. aureus: either MSSA or MRSA
Vancomycin + Cefazolin/Nafcillin (β-lactam)
• Vancomycin: for MRSA
• Cefazolin/Nafcillin: augments effect of
vancomycin covering MISA
MSSA: Methicillin-susceptible S. aureus
MRSA: Methicillin-resistant S. aureus
Subacute IE
o S. viridans, HACEK, Enterococcus
Vancomycin + Ampicillin-Sulbactam (or
Ceftriaxone)
• Vancomycin: for gram-positive bacteria
• Ampicillin-Sulbactam: covers HACEK and
Enterococci
• Ceftriaxone to replace Ampicillin-Sulbactam if Figure 25. Indications for surgery in IE.
there is penicillin allergy Valve repair or valve replacement
(ii) Prosthetic Valve IE o Depending on the cardiothoracic surgeon’s opinion
(1) Indications
(+) Acute left-sided heart failure
o Mitral regurgitation or aortic regurgitation
o Pulmonary edema
o Cardiogenic shock
(+) Prosthetic valve dehiscence
o Can lead to acute LHF
(+) Perivalvular abscess
o Abx cannot adequately clear the infections
Figure 24. Antibiotics used in prosthetic valve IE. (-) Improvement on IV Abx
(+) Pathogens that cannot be cleared with antibiotics
Acute IE o Candida species
o S. aureus: either MSSA or MRSA Need IV antifungals (amphotericin B and/or
Vancomycin + Cefepime (β-lactam) + caspofungin)
Gentamicin ± Rifampin o S. aureus
• Cefepime is much more superior than
cefazolin/nafcillin in prosthetic valve IE Recurrent septic emboli
• Gentamicin is IMPORTANT for prosthetic o Resistant to antibiotics
valve IE o Led to brain abscesses, hemorrhages, mycotic
o Covers Staph species aneurysms, splenic abscess, renal infarcts, discitis
• Rifampin can cause bacterial resistance to
other Abx so this should be added later on
(after 1 week)
Subacute IE
o S. epidermidis, S. viridans, HACEK, Enterococcus
Recall that S. epidermidis love prosthetic hardware
Vancomycin + Ampicillin-Sulbactam (or
Ceftriaxone) + Gentamicin ± Rifampin
8 of 12 CARDIOVASCULAR PATHOLOGY: Note #23. Infective Endocarditis
V) ENDOCARDITIS PROPHYLAXIS
Figure 26. Endocarditis prophylaxis.
For people who are high-risk (cardiac conditions) and are
undergoing specific procedures
(1) Indications
(i) Cardiac Conditions
History of IE
Prosthetic valve
Congenital heart defects
s/p Heart transplant with associated valvulopathy
(ii) Procedures
Any simple dental procedure
o Cleaning
o Root canal
Incision and drainage (I&D) of skin or musculoskeletal
abscess
Respiratory tract incision or biopsy
Insertion of cardiac prosthetic hardware (AICD,
pacemakers, etc)
(2) Antibiotic Prophylaxis
PO (per orem): amoxicillin
o Most common
o 30-60 mins prior the procedure
IV or IM: ampicillin
Penicillin allergy: azithromycin or clindamycin
Infective Endocarditis CARDIOVASCULAR PATHOLOGY: Note #23. 9 of 12
VI) APPENDIX
Table 23-9 Summary
Acute Infective Endocarditis Subacute Infective Endocarditis
Patients are really septic (hypotensive, high Non-specific symptoms: low-grade fever,
fever, new heart failure symptoms, septic dyspnea, fatiguability
Definition emboli) Due to S. viridans (most common), HACEK,
Due to S. aureus Enterococci, S. gallolyticus, S.
epidermidis, Candida
Bacteremia
o S. aureus
Skin abscesses, IV drug abuse,
prosthetic hardwires
o S. viridans
Abnormal Valves Dental procedures, poor dentition
o Rheumatic heart disease o HACEK
o Hx of IE Dental procedures, poor dentition
Causes o Bicuspid aortic valve o Enterococci
o Mitral valve prolapse UTI (pyelonephritis), catheters and
o Congenital heart defects other urogenitary procedures
o Prosthetic valves o S. gallolyticus
Colorectal cancers, IBD
o S. epidermidis
Loves prosthetic hardwares; skin flora
o Candida
Immunocompromised patients
↑Cytokines Septic Emboli
o Fever o Pulmonary embolism (right-sided)
o Leukocytosis o Lung abscess (right-sided)
Acute Heart Failure Symptoms o Acute ischemic stroke
o Shortness of breath due to pulmonary o ICH/SAH
edema o Abscess
o Dyspnea on exertion o Splinter hemorrhages
o Paroxysmal nocturnal dyspnea o Janeway’s lesions
o Orthopnea o Discitis → Osteomyelitis
Clinical Manifestations o Hypoxemia o Septic arthritis
and PE o Hypotension o Splenic infarct → splenic abscess
o Cold extremities o Renal infarct
o New aortic and/or mitral regurgitation ↑Immune Complexes
o Left side >>>>> Right side o Glomerulonephritis = hematuria and
↑Perivalvular Destruction proteinuria
o Murmur o Osler nodes
o AV blocks and BBB o Roth spots
o Pericarditis +/- pericardial effusion o (+) Rheumatoid factor
o Perivalvular dehiscence → perivalvular
dysfunction
Tests for Immune Complexes
o Urinalysis with microscopy
o Fundoscopy
o PE
Echocardiogram o Rheumatoid factor
o Vegetations Modified Duke’s Criteria
o New or worse regurgitation murmur o Two major criteria
o Prosthetic valve dehiscence o One major criterium + three minor criteria
o Perivalvular abscesses o Five minor criteria
Blood Cultures o Major criteria
o Two positive cultures (+) Echo findings
Diagnosis o Persistently positive BCx (+) Blood culture
Tests for Septic Emboli o Minor criteria
o Brain MRI (+) Fever
o Spinal MRI (+) Predisposing factors (abnormal
o Splenic UTS or CTAP valves and/or bacteremia)
o Renal UTS (+) Septic emboli
o PE (+) Immune phenomenon
o CXR or CT scan (+) Blood cultures not meeting the
major criteria
10 of 12 CARDIOVASCULAR PATHOLOGY: Note #23. Infective Endocarditis
Marantic Endocarditis Libmann-Sacks Endocarditis
Differentials o (+) Advanced malignancy such as o (+) SLE
pancreatic carcinoma
Clinical Features
o Low grade fevers
o Little vegetations
o Heart murmurs
o (-) Blood cultures
o Does not improve on Abx
Diagnosis
o Biopsy
o Look for underlying condition
Empiric Antibiotics
o Native valve IE
o Native valve IE Vancomycin + ampicillin-sulbactam
Vancomycin + cefazolin/nafcillin (or ceftriaxone)
o Prosthetic valve IE o Prosthetic valve IE
Vancomycin + cefepime + gentamicin Vancomycin + ampicillin-sulbactam
+/- rifampin (or ceftriaxone) + gentamicin +/-
rifampin
Treatment
Surgery
o Valve repair or valve replacement
o Indications:
(+) Acute LHF
(+) PV dehiscence
(+) PV abscess
(-) Improvement on IV Abx
(+) Pathogens that cannot be cleared with Abx
Recurrent septic emboli
Cardiac Conditions
o History of IE
o PV
o Congenital heart defects
o s/p Heart transplant with assoc. valvulopathy
Procedures
Prophylaxis o Dental procedures
o I&D
o Respiratory tract incision or biopsy
o Insertion of cardiac prosthetic hardware
Abx Prophylaxis
o PO: amoxicillin
o IV: ampicillin
o Penicillin allergy: azithromycin/clindamycin
Infective Endocarditis CARDIOVASCULAR PATHOLOGY: Note #23. 11 of 12
VII) REVIEW QUESTIONS VIII) REFRENCES
1) Which of the following is NOT a pathogen for
● Jameson, J. L., & Loscalzo, J. (2015). Harrison's principles of
subacute endocarditis? internal medicine (19th edition.). New York: McGraw Hill Education.
a) S. aureus ● Le T. First Aid for the USMLE Step 1 2020. 30th anniversary
b) S. viridans edition: McGraw Hill; 2020.
● Papadakis MA, McPhee SJ, Rabow MW. Current Medical
c) Klebsiella Diagnosis & Treatment 2018. New York: McGraw-Hill Education;
d) Haemophilius 2017.
● Sabatine MS. Pocket Medicine: the Massachusetts General
2) The following are causes of damaged heart valves Hospital Handbook of Internal Medicine. Philadelphia: Wolters
EXCEPT: Kluwer; 2020.
a) Infective endocarditis three years ago ● Williams DA. Pance Prep Pearls. Middletown, DE: Kindle Direct
Publishing Platform; 2020.
b) Mitral valve regurgitation
c) Tetralogy of Fallot
d) Prosthetic valves
3) The following can cause spread of S. aureus into the
bloodstream which may cause IE?
a) Dental cleaning
b) IV drug abuse
c) Colorectal cancer
d) Pyelonephritis
4) Which of the following is TRUE about S. aureus?
a) One of the pathogens that can damage healthy
valves
b) Gram-positive
c) Most common bacteria causing IE on IV drug
abusers
d) All of the above
5) Which is a clinical manifestation caused by
increased immune complexes?
a) Janeway lesions
b) Roth spots
c) Regurgitation murmur
d) Shortness of breath
6) What diagnostic tests should you order if a patient
with IE presented with altered mental status?
a) MRI of the brain
b) CT scan
c) Physical exam is okay
d) None of the above
7) A 58/F patient with history of IE, presented with
fever. Her spinal MRI revealed abscesses on the
vertebral discs. Upon fundoscopy, you observed
small hemorrhages in the retina. You ordered blood
cultures but only one of the cultures are positive. Her
echo findings showed vegetations and perivalvular
abscesses. Will you establish IE as diagnosis?
a) Yes, it met the Duke’s criteria.
b) No, I will order more tests.
8) Aside from vancomycin, what antibiotics will you
prescribe for a septic IE patient with prosthetic
valves?
a) Cefazolin
b) Ampicillin-Sulbactam
c) Gentamicin
d) B and C
9) What antibiotic prophylaxis is prescribed PO if the
patient has no allergies?
a) Ampicillin
b) Amoxicillin
c) Clindamycin
12 of 12 CARDIOVASCULAR PATHOLOGY: Note #23. Infective Endocarditis
You might also like
- 4 First Aid BFPDocument52 pages4 First Aid BFPJoyce FalladoNo ratings yet
- 17-Infective EndocarditisDocument17 pages17-Infective Endocarditisمصطفى محمد جواد كاظمNo ratings yet
- Robert So JR Batch 15 Taylors University 2018/2023Document6 pagesRobert So JR Batch 15 Taylors University 2018/2023Robert So Jr100% (1)
- Infective Endocarditis-2023Document40 pagesInfective Endocarditis-2023يزن الحارثيNo ratings yet
- Non Rheumatic EndocarditisDocument29 pagesNon Rheumatic EndocarditisSindhujaNo ratings yet
- F.05 The HeartDocument7 pagesF.05 The HeartPAUL ALINGKAYONNo ratings yet
- Infections and InflammationDocument10 pagesInfections and InflammationNarimèneNo ratings yet
- Pathology and Pathogenesis of Infective Endocarditis in Native Heart ValvesDocument8 pagesPathology and Pathogenesis of Infective Endocarditis in Native Heart ValvesIrina TănaseNo ratings yet
- Rheumatic Heart Disease: Infectious Diseases of The HeartDocument5 pagesRheumatic Heart Disease: Infectious Diseases of The HeartVoid LessNo ratings yet
- Endocardial PathologyDocument35 pagesEndocardial PathologyAsem AlhazmiNo ratings yet
- Infective EndocarditisDocument30 pagesInfective EndocarditisAlfrin Antony100% (3)
- Infective EndocarditisDocument4 pagesInfective EndocarditisXiang Yun TanNo ratings yet
- Heart BNHADocument13 pagesHeart BNHAX OloGyNo ratings yet
- Infective EndocarditisDocument3 pagesInfective EndocarditisAlfrin Antony80% (5)
- Infective EndocarditisDocument3 pagesInfective EndocarditisRechelle CabagingNo ratings yet
- Infective Endocarditis: PathogenesisDocument23 pagesInfective Endocarditis: PathogenesisSyauqie AlhasniNo ratings yet
- 2022 Pathogenesis, Diagnosis, Antimicrobial Therapy and Management of Infective Endocarditis, and Its ComplicationsDocument7 pages2022 Pathogenesis, Diagnosis, Antimicrobial Therapy and Management of Infective Endocarditis, and Its ComplicationsstedorasNo ratings yet
- Cardio-Vascular PathogyDocument54 pagesCardio-Vascular PathogyArleen MatincaNo ratings yet
- Endokarditis, Miokarditis Perikarditis: Blok KardiovaskularDocument31 pagesEndokarditis, Miokarditis Perikarditis: Blok KardiovaskularTiara RamliNo ratings yet
- Baliuag University College of Nursing Baliuag, BulacanDocument6 pagesBaliuag University College of Nursing Baliuag, Bulacanelmo_lalaNo ratings yet
- Rheumatic Heart DiseaseDocument4 pagesRheumatic Heart DiseaseAlfrin Antony100% (3)
- Most Commonly BacterialDocument2 pagesMost Commonly BacterialMaryam FadahNo ratings yet
- F.06 Diseases of The HeartDocument5 pagesF.06 Diseases of The HeartPAUL ALINGKAYONNo ratings yet
- Chapter 37 WorksheetDocument5 pagesChapter 37 Worksheetkristineconde89No ratings yet
- Dilated Cardiomyopathy Notes AtfDocument15 pagesDilated Cardiomyopathy Notes AtfSingha ChangsiriwatanaNo ratings yet
- Vasculitis by VinhDocument4 pagesVasculitis by VinhTovin NguyenNo ratings yet
- Patho - Rheumatic Heart DiseaseDocument26 pagesPatho - Rheumatic Heart DiseaseMahmoud hilmyNo ratings yet
- Cardiovascular Pathology - 020) Aortic Valve Stenosis and Regurgitation (Notes)Document13 pagesCardiovascular Pathology - 020) Aortic Valve Stenosis and Regurgitation (Notes)arga setyo adjiNo ratings yet
- Infective Endocarditis: Christine Joy F. Baquiran MED-3CDocument46 pagesInfective Endocarditis: Christine Joy F. Baquiran MED-3CAbigail SabinoNo ratings yet
- Pathology MRCS BDocument77 pagesPathology MRCS BHina MalikNo ratings yet
- EndicarditisDocument10 pagesEndicarditisAkarsh RamNo ratings yet
- Week 1Document7 pagesWeek 1Balkess NajemNo ratings yet
- Infective - EndocarditisDocument6 pagesInfective - EndocarditisHala AhmadNo ratings yet
- Rheumatic Fever & Infective EndocarditisDocument46 pagesRheumatic Fever & Infective EndocarditisMosab MasoudNo ratings yet
- Summer AssignmentDocument2 pagesSummer AssignmenttewetanNo ratings yet
- EndocarditisDocument35 pagesEndocarditisKatret ElnadaNo ratings yet
- Clinical Cases of Infectious Endocarditis in CatsDocument12 pagesClinical Cases of Infectious Endocarditis in CatsAna AldazNo ratings yet
- Boards - Gen PathDocument12 pagesBoards - Gen PathJoyce EbolNo ratings yet
- Valvular Heart DiseaseDocument8 pagesValvular Heart DiseaseHASNIZZAM BIN AHMAD AMIN -No ratings yet
- Valvular Heart DiseasesDocument29 pagesValvular Heart Diseasesbpt2No ratings yet
- Coronary Arteritis DDDocument6 pagesCoronary Arteritis DDvam buddhaNo ratings yet
- Seminar On Rhuematic Heart DiseaseDocument16 pagesSeminar On Rhuematic Heart Diseasenaga maniNo ratings yet
- Inflammatory Disorders A5Document5 pagesInflammatory Disorders A5FrancheskaNo ratings yet
- Arrhythmias - PrintingDocument5 pagesArrhythmias - Printingibrahim said faidNo ratings yet
- Multiple Organ Dysfunction SyndromeDocument4 pagesMultiple Organ Dysfunction SyndromeJenny SisonNo ratings yet
- Intracerebral Hemorrhage ICH Etiology, AtfDocument10 pagesIntracerebral Hemorrhage ICH Etiology, Atfsiti.220010019No ratings yet
- Ards PDFDocument20 pagesArds PDFRuki HartawanNo ratings yet
- 11.3 Chapter 23-Pt 2 Cardiovascular - Lecture - W13Document10 pages11.3 Chapter 23-Pt 2 Cardiovascular - Lecture - W13Hiba V.ANo ratings yet
- Katup Jantung: - Mempertahankan Aliran DGN Satu Arah Tetap - Membuka/Menutup PasifDocument24 pagesKatup Jantung: - Mempertahankan Aliran DGN Satu Arah Tetap - Membuka/Menutup PasifandreNo ratings yet
- Difference Between Rheumatic Heart Disease and Infective EndocarditisDocument7 pagesDifference Between Rheumatic Heart Disease and Infective Endocarditis<_>No ratings yet
- Rheumatic Heart Disease: Dr. Gehan Mohammed Dr. Abdelaty ShawkyDocument46 pagesRheumatic Heart Disease: Dr. Gehan Mohammed Dr. Abdelaty ShawkyimanNo ratings yet
- Ajith Kumar P MPT Cardiopulmonary SciencesDocument30 pagesAjith Kumar P MPT Cardiopulmonary SciencesSuhana JahangeerNo ratings yet
- Inflammation of Any Layer of Heart (Endo, Myo, Peri) : Damaging Valves, Muscles and /or Pericardial LiningsDocument15 pagesInflammation of Any Layer of Heart (Endo, Myo, Peri) : Damaging Valves, Muscles and /or Pericardial LiningsNur SetsuNo ratings yet
- Covid and Ebola MsDocument7 pagesCovid and Ebola MsAimee Rochelle MaesaNo ratings yet
- Infectious Disease of The HeartDocument3 pagesInfectious Disease of The HeartClaire GidoNo ratings yet
- MODULE 3 Disorders of Primary HemostasisDocument13 pagesMODULE 3 Disorders of Primary HemostasisLancer BlazeNo ratings yet
- Infective Endocarditis SAQ ChatGPTDocument2 pagesInfective Endocarditis SAQ ChatGPTGus LionsNo ratings yet
- Cvspa04 Ihd and MiDocument8 pagesCvspa04 Ihd and MiRobert So JrNo ratings yet
- P.20 Hemodynamic Disorders, Thromboembolic Disease, and Shock - Part 6 (Dr. Espiritu) (09-11-18)Document3 pagesP.20 Hemodynamic Disorders, Thromboembolic Disease, and Shock - Part 6 (Dr. Espiritu) (09-11-18)Raymund Dan AldabaNo ratings yet
- Thorn in the Flesh - How the Corona "Vaccine" Induced Spike Protein Causes Damage: (Author's Translation without Proofreading)From EverandThorn in the Flesh - How the Corona "Vaccine" Induced Spike Protein Causes Damage: (Author's Translation without Proofreading)No ratings yet
- Parotid Gland HistopathologyDocument32 pagesParotid Gland HistopathologyDrey Keesey CatzNo ratings yet
- 1 s2.0 S0894731723006223 MainDocument52 pages1 s2.0 S0894731723006223 Mainpaul00040No ratings yet
- (B-0270) Day Surgery Procedure UnitDocument22 pages(B-0270) Day Surgery Procedure UnitAhmad Gamal Elden MAhanyNo ratings yet
- Dr. YSR Aarogyasri Health Care TrustDocument23 pagesDr. YSR Aarogyasri Health Care Trusttatapudi mohanNo ratings yet
- Upper Gi BleedingDocument3 pagesUpper Gi BleedingJohiarra TabigneNo ratings yet
- Unusual Presentation of Recurrent Appendicitis - A Rare Case Report and Literature ReviewDocument4 pagesUnusual Presentation of Recurrent Appendicitis - A Rare Case Report and Literature ReviewMirachel AugustNo ratings yet
- RADSCIENCESDocument24 pagesRADSCIENCESYael Opeña AlipNo ratings yet
- Treatment ERSDDocument6 pagesTreatment ERSDAsep ArdiNo ratings yet
- Lista de Lucrari 3Document30 pagesLista de Lucrari 3Anonymous 0epuGwQTJNo ratings yet
- A Prospective Study On The Maternal Outcome in Cases of Previous One Cesarean SectionDocument6 pagesA Prospective Study On The Maternal Outcome in Cases of Previous One Cesarean SectionIJAR JOURNALNo ratings yet
- Subject: - Topics: Cholecystitis: Adult Health NursingDocument17 pagesSubject: - Topics: Cholecystitis: Adult Health NursingUzma KhanNo ratings yet
- LifePak 12 InstructionsDocument288 pagesLifePak 12 InstructionsthedrmikeNo ratings yet
- CPRDocument41 pagesCPRPreethi BNo ratings yet
- Open Access Atlas of Otolaryngology, Head & Neck Operative SurgeryDocument3 pagesOpen Access Atlas of Otolaryngology, Head & Neck Operative SurgeryMiggy GNo ratings yet
- Lesson PlanDocument22 pagesLesson PlanPramila AdhikariNo ratings yet
- Thoracic Segmental Spinal Anaesthesia/ General Anaesthesia For Laproscopy SurgeryDocument8 pagesThoracic Segmental Spinal Anaesthesia/ General Anaesthesia For Laproscopy SurgeryIJAR JOURNALNo ratings yet
- Case Study 55-3Document5 pagesCase Study 55-3jillNo ratings yet
- Biologic and Biophysical Technologies. FINALDocument28 pagesBiologic and Biophysical Technologies. FINALRafael Miguel MallillinNo ratings yet
- Science 9 1.4 Circulation of Blood in The BodyDocument13 pagesScience 9 1.4 Circulation of Blood in The BodyChad Kirsten Mier LustreNo ratings yet
- Dialysis Technician ResumeDocument6 pagesDialysis Technician Resumef5dbf38y100% (3)
- Incisive CT Produkt SpesifikacijoniDocument12 pagesIncisive CT Produkt SpesifikacijoniKaimiSuresh100% (1)
- March 21 MRIDocument2 pagesMarch 21 MRIBhavik ChavdaNo ratings yet
- Hygeia HMO SME Plans Proposal - 2022 - FinalDocument4 pagesHygeia HMO SME Plans Proposal - 2022 - FinalBanks C. GeorgeNo ratings yet
- Prevention of Infective Endocarditis AHA EditDocument17 pagesPrevention of Infective Endocarditis AHA EditDampee ReturnNo ratings yet
- Manual Lymphatic Drainage Versus Exercise in The Early PostoperativeDocument7 pagesManual Lymphatic Drainage Versus Exercise in The Early PostoperativeSofia Adão da FonsecaNo ratings yet
- Gastrostomy Feeding ProcedureDocument5 pagesGastrostomy Feeding ProcedureRohini RaiNo ratings yet
- Anesthesia 1Document55 pagesAnesthesia 1Mah ShawdNo ratings yet
- Most Requested Items/locations: Emergency Department Elevators Pedway Path Welcome CenterDocument2 pagesMost Requested Items/locations: Emergency Department Elevators Pedway Path Welcome CenterTERRENCENo ratings yet
- Barium Swallow Meal Follow-Through MealDocument2 pagesBarium Swallow Meal Follow-Through MealPervez Ahmad AhmadNo ratings yet