Professional Documents
Culture Documents
Fneur 13 871187
Fneur 13 871187
Uploaded by
Yery AparicioOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fneur 13 871187
Fneur 13 871187
Uploaded by
Yery AparicioCopyright:
Available Formats
SYSTEMATIC REVIEW
published: 30 May 2022
doi: 10.3389/fneur.2022.871187
Medical Cannabis for the Treatment
of Migraine in Adults: A Review of the
Evidence
Babasola O. Okusanya 1 , Breanne E. Lott 1 , John Ehiri 1 , Jean McClelland 2 and
Cecilia Rosales 3*
1
Department of Health Promotion Sciences, Mel and Enid Zuckerman College of Public Health, University of Arizona, Tucson,
AZ, United States, 2 Health Sciences Library, University of Arizona, Tucson, AZ, United States, 3 Division of Public Health
Practice and Translational Research, Mel and Enid Zuckerman College of Public Health, University of Arizona, Phoenix, AZ,
United States
Background: Medical cannabis (MC) has been hypothesized as an alternative therapy
for migraines, given the undesirable side effects of current migraine medications. The
objective of this review was to assess the effectiveness and safety of MC in the treatment
of migraine in adults.
Methods: We searched PubMed, EMBASE, PsycINFO, CINAHL, and Web of
Science for eligible studies in adults aged 18 years and older. Two reviewers
independently screened studies for eligibility. A narrative synthesis of the included studies
Edited by: was conducted.
Milena De Felice,
The University of Sheffield,
Results: A total of 12 publications involving 1,980 participants in Italy and the
United Kingdom United States of America were included.
Reviewed by: Medical cannabis significantly reduced nausea and vomiting associated with migraine
Lanfranco Pellesi,
attacks after 6 months of use. Also, MC reduced the number of days of migraine after
Danish Headache Center,
Rigshospitalet, Denmark 30 days, and the frequency of migraine headaches per month. MC was 51% more
Ulises Coffeen, effective in reducing migraines than non-cannabis products. Compared to amitriptyline,
National Institute of Psychiatry Ramon
de la Fuente Muñiz (INPRFM), Mexico
MC aborted migraine headaches in some (11.6%) users and reduced migraine frequency.
*Correspondence:
While the use of MC for migraines was associated with the occurrence of medication
Cecilia Rosales overuse headaches (MOH), and the adverse events were mostly mild and occurred in
crosales@arizona.edu
43.75% of patients who used oral cannabinoid preparations.
Specialty section: Conclusions: There is promising evidence that MC may have a beneficial effect
This article was submitted to on the onset and duration of migraine headaches in adults. However, well-designed
Headache and Neurogenic Pain,
a section of the journal experimental studies that assess MC’s effectiveness and safety for treating migraine in
Frontiers in Neurology adults are needed to support this hypothesis.
Received: 08 February 2022
Keywords: migraine, headaches, medical marijuana, medical cannabis, cannabinoids
Accepted: 29 April 2022
Published: 30 May 2022
Citation:
Okusanya BO, Lott BE, Ehiri J,
HIGHLIGHTS
McClelland J and Rosales C (2022)
- High-quality research on medical cannabis (MC) for migraine treatment is lacking
Medical Cannabis for the Treatment of
Migraine in Adults: A Review of the - MC reduced migraine headaches per month from 10.4 to 4.6 at follow-up (p < 0.0001)
Evidence. Front. Neurol. 13:871187. - Medical cannabis aborted migraines in 11.6% of users
doi: 10.3389/fneur.2022.871187 - Like amitriptyline, medical cannabis use resulted in reduced migraine frequency (∼40%).
Frontiers in Neurology | www.frontiersin.org 1 May 2022 | Volume 13 | Article 871187
Okusanya et al. Medical Cannabis to Treat Migraine in Adults
BACKGROUND effects (3). Although surgical intervention for migraine has
been explored, the surgical risks and inconsistent patient
Migraine is a primary headache disorder and a clinical syndrome outcomes make it a less than desired treatment option. A
that is characterized by nausea and vomiting, photophobia, and recent study investigating the corrugator muscle’s resection with
phonophobia (1). Globally, migraine is a common disorder the trigeminal nerve’s zygomaticotemporal branch’s avulsion
and the second leading cause of disability in both males and eliminated migraine headaches in 47% of participants while 6.6%
females younger than 50 years (2). It is estimated that migraine of patients did not show any improvement after surgery (7).
affects 1 billion people worldwide and 37 million people in the Patient-reported relief of migraine symptoms (3) has fueled
United States, with a prevalence of 20.7 and 9.7% in females and recent interest in the use of MC for migraines. In a survey
males, respectively (3). of medical use of cannabis products in Germany, Austria, and
Headache associated with migraine is often unilateral and Switzerland, 10.2% of patients with migraine reported self-use
pulsatile (3) and is described as migraine without aura (1). of cannabis (10). Also, 35% of respondents reported using MC
Migraine with aura is migraine headaches with a set of symptoms for headaches/ migraine in another study (11). However, there
that result from cerebral dysfunction. The aura symptoms is limited compelling evidence of its effectiveness in treating
include visual, sensory, speech/language, motor, brainstem, and migraines. In addition to a lack of empirical evidence to support
retinal symptoms (1), with symptoms usually preceding the MC’s safe use for migraine, there is some evidence that long-term
headache by 20–30 min. Migraine is either episodic or chronic. or high-dose marijuana may pose health risks and exacerbate
Episodic migraines occur fewer than 15 days in a month, while headaches. One such documented risk is reversible cerebral
chronic migraine is present ≥15 days per month (3). Chronic vasoconstriction syndrome with a high dosage of CBD, leading
headaches have adverse effects on social relationships, job and to ischemic or hemorrhagic stroke (3) and neuroinflammation of
may cause family distress (4). the meninges, causing diminished analgesia (4).
The usual treatment modalities for migraine include In the State of Arizona, United States, MC use is
paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), predominantly (94%) for chronic pain, including migraines,
anti-emetics, and serotonin-receptor agonists -triptans (1, 3, 5). by MC cardholders (12). Given the increasing global interest
The effectiveness of these therapies varies due to individual in MC for the treatment of a wide range of ailments (13–15),
patient differences, and they equally have adverse side effects that and the proliferation of anecdotal information on the effect of
limit their duration of use (3, 5). To provide relief for patients cannabis on migraines in particular (3, 16, 17), it is important to
with chronic migraine, surgical management in the form of summarize the evidence regarding the effectiveness and safety
peripheral nerve decompression has been reported with some of MC for migraines. This systematic review’s objective was to
success. Although 47% of patients who had surgery reported assess the effectiveness and safety of MC in the treatment of
complete elimination of migraine, some people with chronic migraine in adults.
migraine did not have any benefits, despite the risks of surgical
exposure (6, 7). This has led both physicians and patients to
try dietary and herbal remedies, including the use of medical METHODS
cannabis (MC) for migraine treatment (4, 8, 9).
Cannabis, or marijuana as it is commonly referred to, has We searched the following electronic databases from inception
been used for centuries to treat several ailments. Anecdotal through November 19, 2020: PubMed; EMBASE; CINAHL;
client reports indicate benefits from marijuana or cannabidiol, PsycINFO; and Web of Science, in consultation with a
a constituent of MC (3). The cannabis plant contains more Medical Librarian (JM), for studies on medical marijuana and
than 100 cannabinoids, naturally occurring compounds, each migraine in adults ≥18 years. An updated search of PubMed,
with its own biological and medicinal properties. Two of these EMBASE, CINAHL, and PsycINFO was performed on 26
phytocannabinoids are 19 - tetrahydrocannabinol (19 -THC) January 2022. We included oral and inhalational routes of MC
and cannabidiol (CBD) (3). While 19 -THC has psychoactive administration. There were no language restrictions during the
properties, CBD does not (3). Instead, CBD causes sedation, search. Conference proceedings and abstracts returned in the
which makes it more studied as a potential medical therapy systematic search were screened with the same eligibility criteria
(3). Marijuana is classified by the relative proportion of its as peer-reviewed publications. The search strategies of the five
two constituents as cannabidiol (high CBD: low 19 -THC); databases are presented in Appendix 1.
intermediate (equal CBD: 19 -THC); 19 - tetrahydrocannabinol Studies were eligible for inclusion if they compared MC
(low CBD: high 19 -THC) (3). with any treatment or “Nothing”. The eligible studies included
Globally, disability due to migraine headaches is enormous, randomized controlled trials, controlled “Before and After”
yet the commonly used medical treatments for episodic or studies, case-control studies, cohort studies, cross-sectional
chronic migraines have disturbing short- and long-term adverse studies, case reports, or case series.
Two review authors (BO and BEL) independently screened
the literature search results in two successive rounds of title
Abbreviations: CBD, cannabidiol; MC, medical cannabis; MOH,
Medication overuse headaches; TGV, trigemino-vascular system; THC, 19 -
and then title/abstract review to identify potentially relevant
tetrahydrocannabinol; PRISMA, Preferred Reporting Items for Systematic Reviews studies. Full reports of potentially relevant studies were obtained
and Meta-Analyses; PROSPERO, Prospective Register of Systematic Reviews. for further assessment. We resolved disagreements through
Frontiers in Neurology | www.frontiersin.org 2 May 2022 | Volume 13 | Article 871187
Okusanya et al. Medical Cannabis to Treat Migraine in Adults
FIGURE 1 | PRISMA flowchart of study selection process.
consensus agreement within the review team and contacted with the International Prospective Register of Systematic Reviews
the third author when there was a disagreement between two (PROSPERO) before starting the review process.
authors on study eligibility. One review author extracted data
and checked it for accuracy by a second reviewer (BEL and BO).
RESULTS
Data were extracted for the following variables: study design,
sample size, location, population, treatment, control condition, Description of Included Studies
outcomes, and findings. A narrative synthesis was used to A total of 12 studies with 1,980 participants were included.
describe the included studies because of the included studies’ The included studies were seven peer-reviewed publications (19–
heterogeneity. The review was conducted following the Preferred 25) and five conference abstracts, including two case reports
Reporting Items for Systematic Reviews and Meta-Analysis (26, 27), one case series (28), one retrospective chart review (29),
(PRISMA) (18) (Figure 1). The review was exempt from ethics and one randomized control trial (30). The seven peer-reviewed
review, given that anonymized published data sources were used. publications were retrospective cohort study (22), retrospective
However, this review protocol was registered (CRD42019129923) analysis of medical charts of migraine patients who used MC
Frontiers in Neurology | www.frontiersin.org 3 May 2022 | Volume 13 | Article 871187
Okusanya et al. Medical Cannabis to Treat Migraine in Adults
TABLE 1 | Study characteristics, population, treatment, outcomes, and findings of included studies.
References Design Location Source type Population Treatment and control
Baraldi, et al. (22) Retrospective cohort study Italy Peer-reviewed publication 32 Oral cannabinoid preparations at maximum
daily dose of 1mL (25 drops) Control: None
Cuttler et al. (20) Review of Archival data on U. S. Peer-reviewed publication 653 Inhalational MC (smoking, vaping,
Strainprint application (App) concentrates, dab bubbler, dab portable)
Control: None
Dini et al. (26) Case report Italy Conference abstract Male, 48 years old Oral drop formulation with 6.5% THC and
8% CBD. Control: None
Gibson et al. (23) Cross sections online survey U.S. A Peer-reviewed publication 161 Topical, Flower CBD, Edible CBD,
concentrate CBD Control: None
Kesayan et al. (27) Case report U.S. Conference abstract Male, 38 years old 5 mg Dronabinol Control: None
Kuruvilla et al. (24) Cross section (social media) U.S. A Peer-reviewed publication 164 Cannabinoid derivatives or cannabinoids
survey Control: None
Lo Castro et al. (28) Case series Italy Conference abstract 18 Cannabis oil (5-8% THC and 7-12% CBD)
Control: None
Mechtler et al. (29) Retrospective chart review U.S. Conference abstract 316 Not specified
Nicolodi et al. (30) Randomized control trial Italy Conference abstract 79 Oral drop emulsion with 200 mg THC+CBD in
a 200 ml 50% fat emulsion, daily for
three months. Control: 25mg/day amitriptyline
Rhyne et al. (19) Retrospective chart review U.S. Peer-reviewed publication 121 Vaporized, edible, topical, and smoked
marijuana in varying doses and frequency.
Control: None
Stith et al. (21) Observational research U.S. Peer-reviewed publication 284 Cannabis flower Control: None
using Releaf Application
(App) data
Zhang et al. (25) Retrospective electronic U.S. A Peer-reviewed publication 150 Inhalation and orally ingested products Control:
chart review None
(19, 25) or analysis of MC Application (App) (20, 21) and online edible, and inhalational routes to administer MC products with
surveys (23, 24). The study selection process is shown in Figure 1. a mean monthly dose of 2.64 ounces (vaporized), 2.59 ounces
The included studies were presented at conferences or published (edible), 2.73 ounces (topical), and 1.59 ounces (smoked) (19).
from 2016 to 2021 and came from two countries, namely the
United States (19–21, 23–25, 27, 29) and Italy (22, 26, 28, 30). Indications for MC
The study characteristics are presented in Table 1. A total of three studies used daily MC for migraine prophylaxis
(24, 26, 27). An included study described prophylactic use every
day with an additional 200 mg dose permitted for acute pain
Routes and Dosage of Administration treatment in the event of headaches (30). Participants of three
Migraine sufferers, ranging in age from 18 to 89, were treated other studies used MC for the treatment of migraines (22, 23, 25).
with medical cannabis in various forms and doses (19). Oral In one study that assessed patients’ self-reported reasons for MC
drops of a THC and CBD formulation were administered in use, 90.9% of patients reported using medical marijuana both
three studies (26, 28, 30). Oral cannabinoid preparations up to preventively and for abortive migraine treatment (19).
a maximum of 1 ml daily were used in a study (22), while topical,
edible, and concentrate cannabinoids were used in two studies Relieving Effects of MC
(23, 24). Both inhalational and orally ingested products were The included studies measured migraine symptom relief
used by Zhang et al. (25) Dini et al. specified the formulation’s with either symptom frequency (19, 26, 28–30) or migraine
composition as 6.5% THC and 8% CBD but did not specify severity/intensity (20, 21, 27). The frequency was measured as
dosage or treatment frequency (26). Also, Lo Castro specified the number of days with headache per month (26) or the number
5–8% THC and 7–12% CBD in the MC oil in their study (28). of headache events in a specified period of 1–3 months (19, 28–
Conversely, Nicolodi et al. reported a 200-mg daily oral dosing 30). Migraine intensity was measured as perceived pain reduction
administered in a 200 ml 50% fat emulsion for 1 month but did using a Likert scale from 0 to 10 (27) or as the percent of pain
not specify the THC/CBD composition (30). Only one patient relief (30). See Table 1 for included studies’ characteristics.
received 5 mg dronabinol twice daily, without stating the route Two included studies reported data on pain freedom (abortion
of administration (27). An included study neither specified the of acute migraine headaches) (19, 28). Lo Castro reported a
dosage nor the route of MC use (29). While two studies used reduction of the number of days of migraine over 30 days of
inhalational routes to administer MC (20, 21); one with cannabis 0.86 (95% CI, 0.75–0.96) before and 0.75 (95% CI, 0.6–0.89)
flower (21), another included study used a combination of oral, after MC use (t-test p-value = 0.2039) (28). In contrast, Rhyne
Frontiers in Neurology | www.frontiersin.org 4 May 2022 | Volume 13 | Article 871187
Okusanya et al. Medical Cannabis to Treat Migraine in Adults
reported a reduction in the number of migraine headaches Adverse Events
per month; 10.4 at the initial visit and 4.6 at follow-up (p < The adverse events were mostly mild and occurred in 43.75%
0.0001), and the abortion of migraine headaches in 14 users of patients who used oral cannabinoid preparations (22). Also,
(11.6%) (19). MC significantly reduced nausea and vomiting tolerance to the effect of MC indicated by a significant increase
associated with migraine attacks after 6 months of use (p = in dose across time per cannabis use session (p = 0.001) has been
0.0057) (22). Although MC did not significantly change the reported (19) and this might lead to the use of higher dosages
number of migraine days after the 6th month (p = 0.1182), of MC.
it did change the acute medication consumption (p = 0.0006) The use of MC for migraines has been associated with the
and the number of days per month when at least one acute occurrence of medication overuse headaches (MOH), compared
medication was used for migraine (p = 0.0004) when compared with non-cannabis users (81 vs. 41%) (25). Also, current MC use
with baseline (22). for migraine is significantly associated with MOH [adjusted OR
A study reported MC relieved migraines more than non- = 6.3 (CI 3.56–11.1)] (25). The relationship between MC use and
cannabis products (75.82% vs. 51.01%) (23). Also, in participants MOH was further supported by a sensitivity analysis involving
who relied on non-cannabis products and cannabis therapy, MC only people who developed MOH after commencing the MC use
provided better relief (p < 0.001) (23), with sustained effect for migraines [OR = 2.6 (CI 1.52, 4.42)] (25).
after controlling for migraine severity (p = 0.03) (23). In an
online survey of MC users, there was an equivocal report of
the usefulness of MC on headaches with 39% (64/164) patients DISCUSSION
reporting MC as not effective at all (no change in headache days),
though 8.5% (14/164) reported MC to be very effective (50–100% There has been recent interest in using medical cannabis to
reduction in headache days) (24). treat many medical conditions, including migraines. The non-
The only included randomized control trial by Nicolodi response of all patients to commonly used medical treatments
et al. treated the control group with amitriptyline (30). (3), patient-reported relief of migraine symptoms with medical
In 79 migraine sufferers, THC+CBD treatment had a cannabis use, and biological plausibility for how MC may work
similar effect as amitriptyline (40.4% reduction in migraine to treat migraines have contributed to the increased interest. It is
attacks among the intervention group compared to a 40.1% also difficult to predict which patients will benefit from surgical
reduction in migraine attacks in the control group) (30). procedures for chronic migraine, with some patients showing no
Also, the use of 200 mg of cannabinoids as an adjuvant to improvement post-operation (6, 7). As the number of states in
patients on amitriptyline provided a further reduction of the United States approving marijuana for medical use continues
headache intensity to 43.5% among patients in the control to increase, likely, migraine sufferers may choose cannabis to
arm (30). relieve their pain. Therefore, this review was conducted to assess
In a 48-year-old patient with chronic migraine headaches, the beneficial effects and safety of MC in treating migraine
with previous pharmacotherapy treatment failure MC decreased in adults.
headache frequency from >20 days to 0–1 day per month (26). After searching five databases for eligible studies, we applied
Similarly, a 38–year-old had migraine pain intensity reduction, very liberal criteria to include published abstracts and seven
using a visual analog scale, from a 10/10 to 2/10 level following publications that reported the use of MC to treat migraines.
dronabinol treatment, and it remained effective for 3 years (27). The included publications were limited because they all used
In a case series of 18 patients, the number of days of analgesic use retrospective analysis of MC users’ data in prescription charts or
reduced from 1.83 (95% CI, 0.58- 3.07) at baseline to 0.85 (95% stored MC App data. Also, many of the clients had used or were
CI, 0.5–1.19) after 3 months (t-test p-value = 0.11889) (28). current users of cannabis at enrollment, so no true pre-treatment
Among 653 MC users, migraine severity was reduced in condition existed in one of the publications (19). Despite this, all
87.3% of men and 88.6% of women (20), with a migraine rating included publications showed some gradience toward symptom
reduction of 49.6% (p < 0.001) (20). relief of migraine headaches with reduced frequency and severity.
In a sub-group analysis of 284 (606 App sessions) MC users, However, of concern is the reported onset of tolerance to, and
Stith et al. reported symptom relief within 2 h (21). In another medication overuse headaches from MC after prolonged use, as
observational study involving 121 adult patients, the mean reported by Cuttler et al. and Zhang et al., respectively (20, 25).
number of migraines per month decreased significantly from 10.4 Since many people suffer migraine headaches for a long duration,
at the initial visit to 4.6 per month at follow-up (p < 0.0001) (19). there is a need for MC users and dispensaries to monitor the
In the Rhyne et al. study, the positive (abortion of headaches) development of tolerance to MC.
effects of MC were reported by 39.7% of patients, and negative This review’s major limitation is the paucity of high-quality
effects were reported by 11.6% of patients (19). The positive empirical studies on beneficial effects and safety of MC for
effect of aborting migraine headaches was reported by patients the treatment of migraines. We did not find well-conducted
vaporizing and smoking medical marijuana, probably due to the published prospective research on MC and migraine in adults in
fast absorption associated with those methods of delivery (19). the form of experimental studies. However, this review’s strength
The negative effects reported included somnolence (1.7%, n = is the comprehensive search of five major databases, which led
2) and difficulty controlling the timing and intensity of the dose to the identification of several conference abstracts and seven
(1.7%, n = 2) with edible cannabis use (19). publications that were not included in a previous MC review
Frontiers in Neurology | www.frontiersin.org 5 May 2022 | Volume 13 | Article 871187
Okusanya et al. Medical Cannabis to Treat Migraine in Adults
for headache disorders (31). The abstracts were presented at the interest in MC use to treat migraines, there is an urgent need to
2017–2019 conferences and included case reports and case series. implement well-designed studies to evaluate the effectiveness and
The evidence synthesized in this review demonstrates MC’s safety of medical marijuana for treating adults with migraines.
potential for both prophylactic and abortive treatment of
migraine. Cannabis use was associated with reduced headache DATA AVAILABILITY STATEMENT
frequency and pain intensity and had a similar effect to
standard medical care. Still, the paucity of studies on migraine The original contributions presented in the study are included
and medical cannabis and the lack of adequately powered in the article/Supplementary Materials, further inquiries can be
studies that compared current treatment modalities of migraine directed to the corresponding author.
with MC make it impossible to recommend MC to treat
migraine with confidence. Also, possible side effects of marijuana AUTHOR CONTRIBUTIONS
such as medication overuse headache, and especially, the
cerebral vasoconstriction syndrome that may lead to stroke CR and JE conceived the topic. BO wrote the draft protocol,
(3), demonstrate the need for rigorous experimental studies to performed eligibility screening, and wrote the draft discussion
evaluate MC’s effectiveness and safety for treating migraine in of the review. BL revised the draft protocol, performed
adults. Until more robust evidence exists on MC’s effectiveness eligibility screening, performed data extraction, and revised
and safety for migraine, healthcare providers and patients should the completed review. BL and BO drafted the results of the
carefully weigh considerations for potential improvements in completed review. JM collaborated in developing the search
quality of life associated with pain freedom and reduced pain strategy, performed the database search in March 2019 and
frequency with potential health risks of marijuana use for an updated search in November 2020, and revised the draft
migraine in adults. Users of MC for migraines should also be review. JE and CR revised the draft protocol and completed
aware of the potential to develop tolerance to MC, making them the review. All authors agreed to the contents of the review
need higher MC doses over time. for publication.
To ascertain if MC is safe and effective in treating migraine
in adults, future research should be experimental in design and FUNDING
enroll large numbers of participants. There is a need to investigate
the best route of administration of MC to achieve an adequate This systematic review was funded through a grant entitled
serum level with minimal side effects. The optimal dosage of MC Research and Evaluation Services awarded by the Arizona
to treat adults with migraine also needs to be determined since Department of Health Services (ADHS) under Contract Number
low-dose cannabinoids might be ineffective, while a high dosage ADHS12-017291. The content of this publication is solely that of
of cannabinoids might cause neuroinflammation, tolerance, and its authors and does not necessarily represent the official views
reduced analgesic effect (4). Equally, contemporary treatment of ADHS.
modalities of migraine should be compared with MC to prevent
migraines and for abortive emergency uses. There is a need to ACKNOWLEDGMENTS
explore CBD-only therapy for migraine as the psychoactive THC
component’s exclusion might make some difference in treatment Financial support for this work was provided by the Arizona
outcomes and pave new ways for both research and treatment Department of Health Services (AzDHS), Phoenix, Arizona,
with fewer legal restrictions. United States. AzDHS played no role in the study conception,
design, data collection, data analysis, data interpretation, or
CONCLUSION review writing.
A review of three peer-reviewed publications and five gray SUPPLEMENTARY MATERIAL
literature sources (conference papers and posters) revealed that
there is some evidence for MC’s beneficial effect on treating The Supplementary Material for this article can be found
migraine in adults. However, further research is needed to assess online at: https://www.frontiersin.org/articles/10.3389/fneur.
effective dosing and safety critically. Mindful of the upsurge of 2022.871187/full#supplementary-material
REFERENCES analysis for the global burden of disease study 2016. Lancet. (2017) 390:1211–
59. doi: 10.1016/S0140-6736(17)32154-2
1. Arnold M. Headache Classification Committee of the International 3. Burch R. Migraine and Tension-Type Headache: Diagnosis and Treatment.
Headache Society (IHS) the international classification of headache Med Clin North Am. (2019) 103:215–33. doi: 10.1016/j.mcna.2018.10.003
disorders, 3rd edition. Cephalalgia. (2018) 38:1–211. doi: 10.1177/0333102417 4. Leimuranta P, Khiroug L, Giniatullin R. Emerging role of (Endo) cannabinoids
738202 in migraine. Front Pharmacol. (2018) 9:420. doi: 10.3389/fphar.2018.00420
2. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, 5. American Headache Society. The American Headache Society position
regional, and national incidence, prevalence, and years lived with disability statement on integrating new migraine treatments into clinical practice.
for 328 diseases and injuries for 195 countries, 1990-2016: a systematic Headache. (2019) 59:1–18. doi: 10.1111/head.13456
Frontiers in Neurology | www.frontiersin.org 6 May 2022 | Volume 13 | Article 871187
Okusanya et al. Medical Cannabis to Treat Migraine in Adults
6. Gfrerer L, Guyuron B. Surgical treatment of migraine headaches. Acta Neurol 22. Baraldi C, Lo Castro F, Negro A, Ferrari A, Cainazzo MM, Pani L, et al.
Belg. (2017) 117:27–32. doi: 10.1007/s13760-016-0731-1 Oral cannabinoid preparations for the treatment of chronic migraine: a
7. Jose A, Nagori SA, Roychoudhury A. Surgical management retrospective study. Pain Med. (2021) 23:396–402. doi: 10.1093/pm/pnab245
of migraine headache. J Craniofac Surg. (2018) 29:e106– 23. Gibson LP, Hitchcock LN, Bryan AD, Bidwell LC. Experience of migraine,
8. doi: 10.1097/SCS.0000000000004078 its severity, and perceived efficacy of treatments among cannabis users.
8. Rehman T, Ahmad S, Fatima Q. Effects of dietary supplementations and Complement Ther Med. (2021) 56:102619. doi: 10.1016/j.ctim.2020.
herbs on migraine - a systematic review. J Complement Integr Med. (2019) 102619
16. doi: 10.1515/jcim-2018-0143 24. Kuruvilla DE, Mehta A, Ravishankar N, Cowan RP. A
9. Fasinu PS, Phillips S, ElSohly MA, Walker LA. Current status and prospects patient perspective of complementary and integrative medicine
for cannabidiol preparations as new therapeutic agents. Pharmacotherapy Jul. (CIM) for migraine treatment: a social media survey. BMC
(2016) 36:781–96. doi: 10.1002/phar.1780 Complement Med Ther. (2021) 21:58. doi: 10.1186/s12906-021-0
10. Schnelle M GF, Reif M, Gorter RW. Results of a standardized survey on 3226-0
the medical use of cannabis products in the German-speaking areas. Forsch 25. Zhang N, Woldeamanuel YW. Medication overuse headache in patients with
Komplementarmed. (1999) 6(Suppl. 3):28–36. doi: 10.1159/000057154 chronic migraine using cannabis: a case-referent study. Headache. (2021)
11. Leung J, Chan G, Stjepanović D, Chung JYC, Hall W, Hammond D. Prevalence 61:1234–44. doi: 10.1111/head.14195
and self-reported reasons of cannabis use for medical purposes in USA 26. Dini E CM, De Luca C, Baldacci F, Gori S, Bonuccelli U. Chronic migraine
and Canada. Psychopharmacology. (2022). doi: 10.1007/s00213-021-06047-8. successfully treated with cannabinoids. J Headaches Pain. (2018) 186.
[Epub ahead of print]. 27. Kesayan T KN. Refractory migraine with face and ocular pain treated
12. (ADHS) ADoHS. Arizona Medical Marijuana Program October 2020 Monthly successfully with Dronabinol. Am Acad Pain Med. (2018).
Report. ADoHS (2020). 28. Lo Castro FBC, Cainazzo MM, Ferrari A, Pani L, Guerzoni S. Cannabis for
13. Eagleston LRM, Kalani NK, Patel RR, Flaten HK, Dunnick CA, Dellavalle RP. the treatment of refractory headaches: a case-series of 18 patients. Neurol Sci.
Cannabinoids in dermatology: a scoping review. Dermatol Online J. (2018) (2019) 40(Suppl. 2):S239.
24. doi: 10.5070/D3246040706 29. Mechtler LBV, Hart P, McVige J, Saikali N. Medical cannabis for chronic
14. Stetten N, Pomeranz J, Moorhouse M, Yurasek A, Blue AV. The level of migraine: a retrospective review. Neurology. (2019) 92.
evidence of medical marijuana use for treating disabilities: a scoping review. 30. Nicolodi M SV, Torrini A. Therapeutic use of cannabinoids- dose findings,
Disabil Rehabil. (2020) 42:1190–201. doi: 10.1080/09638288.2018.1523952 effects and pilot data of effects in chronic migraine and cluster headaches. Eur
15. Hoch E, Niemann D, von Keller R, et al. How effective and J Neurol. (2017) 24:287. doi: 10.1111/ene.13367
safe is medical cannabis as a treatment of mental disorders? 31. Lochte BC, Beletsky A, Samuel NK, Grant I. The Use of Cannabis
A systematic review. Eur Arch Psychiatry Clin Neurosci. (2019) for Headache Disorders. Cannabis Cannabinoid Res. (2017)
269:87–105. doi: 10.1007/s00406-019-00984-4 2:61–71. doi: 10.1089/can.2016.0033
16. Baron EP, Lucas P, Eades J, Hogue O. Patterns of medicinal cannabis use, strain
analysis, and substitution effect among patients with migraine, headache, Conflict of Interest: The authors declare that the research was conducted in the
arthritis, and chronic pain in a medicinal cannabis cohort. J Headache Pain. absence of any commercial or financial relationships that could be construed as a
(2018) 19:37. doi: 10.1186/s10194-018-0862-2 potential conflict of interest.
17. Tauchen J. Natural products and their (semi-)synthetic forms in treatment
of migraine: history and current status. Curr Med Chem. (2019) 27:3784– Publisher’s Note: All claims expressed in this article are solely those of the authors
808. doi: 10.2174/0929867326666190125155947 and do not necessarily represent those of their affiliated organizations, or those of
18. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for
the publisher, the editors and the reviewers. Any product that may be evaluated in
systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009)
this article, or claim that may be made by its manufacturer, is not guaranteed or
339:b2535. doi: 10.1136/bmj.b2535
19. Rhyne DN, Anderson SL, Gedde M, Borgelt LM. Effects of medical marijuana endorsed by the publisher.
on migraine headache frequency in an adult population. Pharmacotherapy.
(2016) 36:505–10. doi: 10.1002/phar.1673 Copyright © 2022 Okusanya, Lott, Ehiri, McClelland and Rosales. This is an open-
20. Cuttler C, Spradlin A, Cleveland MJ, Craft RM. Short- and long-term access article distributed under the terms of the Creative Commons Attribution
effects of cannabis on headache and migraine. J Pain. (2020) 21:722– License (CC BY). The use, distribution or reproduction in other forums is permitted,
30. doi: 10.1016/j.jpain.2019.11.001 provided the original author(s) and the copyright owner(s) are credited and that the
21. Stith SS, Diviant JP, Brockelman F, Keeling K, Hall B, Lucern S, Vigil JM. original publication in this journal is cited, in accordance with accepted academic
Alleviative effects of Cannabis flower on migraine and headache. J Integr Med. practice. No use, distribution or reproduction is permitted which does not comply
(2020) 18:416–24. doi: 10.1016/j.joim.2020.07.004 with these terms.
Frontiers in Neurology | www.frontiersin.org 7 May 2022 | Volume 13 | Article 871187
You might also like
- Maintanance and Repairof Shipword MachineryDocument58 pagesMaintanance and Repairof Shipword MachineryBahtera Adi50% (2)
- What Makes Great ArtDocument45 pagesWhat Makes Great Artsaba100% (1)
- Evaluation of Green Light Exposure On Laurent MartinDocument13 pagesEvaluation of Green Light Exposure On Laurent MartinYunita Christiani BiyangNo ratings yet
- Charles 2017Document9 pagesCharles 2017Aldebaran LadoNo ratings yet
- Inbound 1186825581313765270Document16 pagesInbound 1186825581313765270NylNo ratings yet
- 47 Migraine and Its Psychiatric ComorbiditiesDocument9 pages47 Migraine and Its Psychiatric ComorbiditiesElizabeth Mautino CaceresNo ratings yet
- Chronic Migraine Pathophysiology and Treatment: A Review of Current PerspectivesDocument15 pagesChronic Migraine Pathophysiology and Treatment: A Review of Current PerspectivesJorge ZegarraNo ratings yet
- The Combined Effect of AcupuncDocument7 pagesThe Combined Effect of AcupuncnsanbaNo ratings yet
- 9.1 An Approach To Identifying Headache Patients That Require Neuroimaging (Curr, Inst and Pedagogy 2019)Document6 pages9.1 An Approach To Identifying Headache Patients That Require Neuroimaging (Curr, Inst and Pedagogy 2019)Katherine RodríguezNo ratings yet
- VSC Poster ProjectDocument1 pageVSC Poster ProjectluckyNo ratings yet
- Cognitive Effects of Migraine TreatmentDocument27 pagesCognitive Effects of Migraine TreatmentRenju KuriakoseNo ratings yet
- Aapm 08 06 81688Document6 pagesAapm 08 06 81688Asti DwiningsihNo ratings yet
- Arnadottir & Sigurdardottir, 2013 - Is Craniosacral Therapy Effective For Migrane - Tested With HIT - QuestionnaireDocument4 pagesArnadottir & Sigurdardottir, 2013 - Is Craniosacral Therapy Effective For Migrane - Tested With HIT - QuestionnaireFlávio GuimarãesNo ratings yet
- J Pharep 2017 02 019Document8 pagesJ Pharep 2017 02 019Daniel Garcia del PinoNo ratings yet
- The Use of Cannabis For Headache DisordersDocument11 pagesThe Use of Cannabis For Headache DisordersNazmi ZegarraNo ratings yet
- Headache 2: SeriesDocument9 pagesHeadache 2: SeriesAzam alausyNo ratings yet
- PDF 3961Document7 pagesPDF 3961MohammadHossein NazariNo ratings yet
- Klan Et Al 2023 Behavioral Treatment For Migraine Prophylaxis in Adults Moderator Analysis of A Randomized ControlledDocument11 pagesKlan Et Al 2023 Behavioral Treatment For Migraine Prophylaxis in Adults Moderator Analysis of A Randomized ControlledyennyNo ratings yet
- Manejo de La Migraña Crónica. Review 2022Document19 pagesManejo de La Migraña Crónica. Review 2022Edwin Fabian Paz UrbanoNo ratings yet
- MetoclopramideDocument6 pagesMetoclopramideRahmi Nurul HNo ratings yet
- Aian 22 286Document5 pagesAian 22 286gloriaNo ratings yet
- Pharmacogenetics in Primary Headache DisordersDocument27 pagesPharmacogenetics in Primary Headache DisordersJorge ZegarraNo ratings yet
- Diener May 2024 New Migraine Drugs A Critical Appraisal of The Reason Why The Majority of Migraine Patients Do NotDocument8 pagesDiener May 2024 New Migraine Drugs A Critical Appraisal of The Reason Why The Majority of Migraine Patients Do NotrenatoNo ratings yet
- Lasmiditan Migraña PerimenstrualDocument9 pagesLasmiditan Migraña Perimenstrualcepdep orgNo ratings yet
- Jackson2017 Article TricyclicAndTetracyclicAntidepDocument8 pagesJackson2017 Article TricyclicAndTetracyclicAntidepAndreas NatanNo ratings yet
- A Review of Herbal Therapy in Multiple SclerosisDocument16 pagesA Review of Herbal Therapy in Multiple Sclerosissorin.morosan64No ratings yet
- Acm 2009 0376Document10 pagesAcm 2009 0376Dr Tanu GogoiNo ratings yet
- Low-Dose Ketamine Does Not Improve Migraine in The Emergency Department A Randomized Placebo-Controlled TrialDocument9 pagesLow-Dose Ketamine Does Not Improve Migraine in The Emergency Department A Randomized Placebo-Controlled TrialRiza FirdausNo ratings yet
- MigraineDocument6 pagesMigraineNatália CândidoNo ratings yet
- Fneur 14 1160204Document9 pagesFneur 14 1160204tafazzal.eduNo ratings yet
- Altered Functional Connectivity of Amygdala Underlying The Neuromechanism of Migraine PathogenesisDocument8 pagesAltered Functional Connectivity of Amygdala Underlying The Neuromechanism of Migraine PathogenesisRizal Sven VollfiedNo ratings yet
- Primary Headache DisordersDocument12 pagesPrimary Headache DisordersririsNo ratings yet
- 2017 - Millstine Et Al - Complementary and Integrative Medicine in The Management of HeadacheDocument11 pages2017 - Millstine Et Al - Complementary and Integrative Medicine in The Management of HeadacheLélia FigueiredoNo ratings yet
- Fneur 11 570335Document9 pagesFneur 11 570335AudryaNo ratings yet
- Long Term Efficacy of Intranasal - EsketamineDocument14 pagesLong Term Efficacy of Intranasal - EsketamineCasey KaneNo ratings yet
- Characterizing Opioid Use in A US Population With MigraineDocument12 pagesCharacterizing Opioid Use in A US Population With MigraineVagner PinheiroNo ratings yet
- The Association Between Migraine and Physical Exercise: Reviewarticle Open AccessDocument9 pagesThe Association Between Migraine and Physical Exercise: Reviewarticle Open AccessAyashopia AyaNo ratings yet
- Brain Sciences: The Role of Adenosine Signaling in Headache: A ReviewDocument20 pagesBrain Sciences: The Role of Adenosine Signaling in Headache: A ReviewMarlyNationTVNo ratings yet
- Trend Watch: Treatment of Migraine and The Role of Psychiatric MedicationsDocument3 pagesTrend Watch: Treatment of Migraine and The Role of Psychiatric MedicationsCharbel Rodrigo Gonzalez SosaNo ratings yet
- Cannabis Based Medicines and Medical Cannabis For Chronic Neuropathic PainDocument14 pagesCannabis Based Medicines and Medical Cannabis For Chronic Neuropathic PainRocio BeteluNo ratings yet
- Chen 2021Document13 pagesChen 2021Aitor UzkudunNo ratings yet
- Treatment-Resistant Schizophrenia: Genetic and Neuroimaging CorrelatesDocument16 pagesTreatment-Resistant Schizophrenia: Genetic and Neuroimaging CorrelatesBianca CaterinalisendraNo ratings yet
- Intradermal Mesotherapy Versus Intravenous DexketoDocument9 pagesIntradermal Mesotherapy Versus Intravenous DexketoMetin SabuncuNo ratings yet
- Meyers 2019 Treatment Patterns and Characteristics of Patients With Migraine in Japan A Retrospective Analysis of Health Insurance Claims DataDocument17 pagesMeyers 2019 Treatment Patterns and Characteristics of Patients With Migraine in Japan A Retrospective Analysis of Health Insurance Claims DataSatra Azmia HerlandaNo ratings yet
- Cognitive Behavioral Therapy For Chronic Insomnia: A Systematic Review and Meta-AnalysisDocument16 pagesCognitive Behavioral Therapy For Chronic Insomnia: A Systematic Review and Meta-AnalysisLiezer Hernandez PinoNo ratings yet
- Ketamine NNTDocument8 pagesKetamine NNTBrent AllieNo ratings yet
- Eptinezumab in Episodic Migraine: A Randomized, Double-Blind, Placebo-Controlled Study (PROMISE-1)Document14 pagesEptinezumab in Episodic Migraine: A Randomized, Double-Blind, Placebo-Controlled Study (PROMISE-1)JUAN MANUEL CERON ALVARADONo ratings yet
- Role of Magnesium Supplementation in The Treatment of Depression: A Randomized Clinical TrialDocument15 pagesRole of Magnesium Supplementation in The Treatment of Depression: A Randomized Clinical Trialvenkat mechNo ratings yet
- NeurologiaDocument216 pagesNeurologiaPietro BracagliaNo ratings yet
- Gengibre Agudo e Enxaqueca Laís Bhering 2019Document9 pagesGengibre Agudo e Enxaqueca Laís Bhering 2019alicebarcelosbartolskiNo ratings yet
- Treatment of Depression in CADDocument15 pagesTreatment of Depression in CADjordanbadangayonNo ratings yet
- Fibromyalgia and Its New Lessons For Neuropsychiatry (2019) PDFDocument10 pagesFibromyalgia and Its New Lessons For Neuropsychiatry (2019) PDFBecados PsiquiatriaNo ratings yet
- Monti 2020Document8 pagesMonti 2020Ian MannNo ratings yet
- Fnins 13 00038Document21 pagesFnins 13 00038peludosainzNo ratings yet
- Antiseizure Medications For EpilepsyDocument13 pagesAntiseizure Medications For EpilepsyJorge CastilloNo ratings yet
- Abram Hoffer, Linus Pauling, James Greenblatt - Functional Psychiatry For Treatment of Anxiety-Psychiatry Redefined (2024)Document16 pagesAbram Hoffer, Linus Pauling, James Greenblatt - Functional Psychiatry For Treatment of Anxiety-Psychiatry Redefined (2024)Alina BreazuNo ratings yet
- Migraine and The Scope of HomeopathyDocument6 pagesMigraine and The Scope of HomeopathyDiego RodriguezNo ratings yet
- Fpsyt 12 584416Document10 pagesFpsyt 12 584416JuliaNo ratings yet
- Morbid Anxiety As A Risk Factor in Patients With Somatic Diseases A Review of Recent FindingsDocument9 pagesMorbid Anxiety As A Risk Factor in Patients With Somatic Diseases A Review of Recent FindingsAdelina AndritoiNo ratings yet
- British J Pharmacology - 2021 - ZobdehDocument20 pagesBritish J Pharmacology - 2021 - ZobdehRenju KuriakoseNo ratings yet
- Migraine Integrated Approaches To Clinical ManagementDocument14 pagesMigraine Integrated Approaches To Clinical ManagementJOHN ROMERO CEVALLOSNo ratings yet
- Migraine: The Definitive Guide to Understanding and Managing Severe HeadachesFrom EverandMigraine: The Definitive Guide to Understanding and Managing Severe HeadachesNo ratings yet
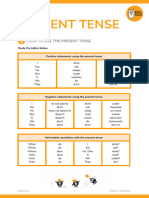
- (TV) Present TenseDocument8 pages(TV) Present TenseDe Aparicio DenisseNo ratings yet
- TUGAS INDIVIDU - 3-01 - 18 - Manajemen Keuangan - Mind Map CH 15Document1 pageTUGAS INDIVIDU - 3-01 - 18 - Manajemen Keuangan - Mind Map CH 15Ni Made Indah MeliawatiNo ratings yet
- EBS Full ReportDocument74 pagesEBS Full ReportEd SalangaNo ratings yet
- Northern SnakeheadDocument2 pagesNorthern SnakeheadrkarlinNo ratings yet
- Reviewer For CriminologyDocument6 pagesReviewer For CriminologyJoemar LucasNo ratings yet
- Embroidery Assistant: User Instruction GuideDocument92 pagesEmbroidery Assistant: User Instruction GuideAhlia Waqas AnjumNo ratings yet
- How Deep Is Your LoveDocument1 pageHow Deep Is Your LoveJanina JaworskiNo ratings yet
- Gravimetric Determination of Barium SulfateDocument3 pagesGravimetric Determination of Barium SulfateArmiee InfiniteNo ratings yet
- Media and Information Literacy Is Defined As An Access To InformationDocument2 pagesMedia and Information Literacy Is Defined As An Access To InformationmarvinNo ratings yet
- DCDC Exam BlueprintDocument2 pagesDCDC Exam BlueprintfarshathNo ratings yet
- Three-Phase Induction MotorsDocument36 pagesThree-Phase Induction MotorsCARMEN DIMITRIUNo ratings yet
- Vine-Vpdc Report As of Feb. 3, 2022Document9 pagesVine-Vpdc Report As of Feb. 3, 2022Elbert Ryan OcampoNo ratings yet
- Ca3 Week1 ModuleDocument16 pagesCa3 Week1 ModuleKate Serrano ManlutacNo ratings yet
- There's No Pill For This - IntroductionDocument4 pagesThere's No Pill For This - IntroductionChelsea Green PublishingNo ratings yet
- Test Report Quadplexer 4in1outDocument8 pagesTest Report Quadplexer 4in1outHagniAryaGunadiNo ratings yet
- DSM Mixing Tower SkyCiv ReportDocument484 pagesDSM Mixing Tower SkyCiv Reportmincho4104No ratings yet
- How The Leopard Got His Spots by Rudyard KiplingDocument4 pagesHow The Leopard Got His Spots by Rudyard KiplingProxten DsilvaNo ratings yet
- Gut DecontaminationDocument17 pagesGut DecontaminationRaju NiraulaNo ratings yet
- Assignment 2Document7 pagesAssignment 2suresh avaduthaNo ratings yet
- Chapter 7 - Cognitive DevelopmentDocument3 pagesChapter 7 - Cognitive DevelopmentmizbigspendaNo ratings yet
- Samsung Brittle Fracture Evaluation - Additional Scope P23-0105-R3Document5 pagesSamsung Brittle Fracture Evaluation - Additional Scope P23-0105-R3Vipin NairNo ratings yet
- Math InterventionDocument6 pagesMath InterventionPAOLO R. ALARDENo ratings yet
- Result Phase III - A, B - Lot (23!03!2024)Document15 pagesResult Phase III - A, B - Lot (23!03!2024)xxxlordimpalerxxxNo ratings yet
- 24 Solar TermsDocument98 pages24 Solar TermsWei Yu LowNo ratings yet
- Bob Fitts - Highest PlaceDocument2 pagesBob Fitts - Highest PlaceJosé Miguel Baute Rosado100% (1)
- Oil Pressure Transmission PT2509Document3 pagesOil Pressure Transmission PT2509Trisna TeaNo ratings yet
- 1 Notes and HW On Even Odd and NeitherDocument3 pages1 Notes and HW On Even Odd and NeitherAlin LyndaNo ratings yet
- Emami Limited: Sales ManagementDocument12 pagesEmami Limited: Sales ManagementSANYUJ ZADGAONKARNo ratings yet