Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
15 viewsMobility and Activity
Mobility and Activity
Uploaded by
neehoshiMobility refers to the ability to move freely and purposefully. There are different types of exercise including isotonic, isometric, and isokinetic. Exercise provides benefits like increased flexibility and bone density but impaired mobility can lead to complications. Nursing interventions include proper positioning, range of motion exercises, ambulation assistance, nutrition support, and skin care to prevent pressure injuries. Devices like pillows, mattresses, and walkers can also help support mobility.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- NDT by Dr. Rati.Document13 pagesNDT by Dr. Rati.Anup PednekarNo ratings yet
- Body Mechanics and Transferring PatientDocument57 pagesBody Mechanics and Transferring PatientRhenier S. Ilado100% (2)
- Assistive DevicesDocument30 pagesAssistive DevicesrlinaoNo ratings yet
- Computer Project 1: Assignment 1.1Document10 pagesComputer Project 1: Assignment 1.1Nelu TurcanuNo ratings yet
- Body Mechanics: Fundamental of Nursing IDocument55 pagesBody Mechanics: Fundamental of Nursing Irlinao100% (3)
- Skills 116 Finals ROM Assistive Devices PDFDocument64 pagesSkills 116 Finals ROM Assistive Devices PDFMae Arra Gilbao Lecobu-anNo ratings yet
- Chapter 2-Basic Care and ComfortDocument37 pagesChapter 2-Basic Care and ComfortWang Ming YaNo ratings yet
- Nursing RehabilitationDocument55 pagesNursing Rehabilitationnursereview100% (6)
- Ambulation With Crutches, Walker, Cane: PurposesDocument2 pagesAmbulation With Crutches, Walker, Cane: PurposesSienaNo ratings yet
- Assistive Devices For WalkingDocument4 pagesAssistive Devices For WalkingAbigail Mangaoang100% (1)
- HC - Transfer and AmbulationDocument14 pagesHC - Transfer and Ambulationblackangel07_angelie100% (2)
- AmbulationDocument18 pagesAmbulationDidik SusetiyantoNo ratings yet
- Assistive Devices For WalkingDocument4 pagesAssistive Devices For Walkingthomasfinley44No ratings yet
- Orthopedic NursingDocument154 pagesOrthopedic NursingTrisha Mae MarquezNo ratings yet
- Range of Motion ExerciseDocument8 pagesRange of Motion ExerciseAmit Martin83% (6)
- FUNDA REVIEW 2 Body MechanicsDocument27 pagesFUNDA REVIEW 2 Body Mechanicslovie dooNo ratings yet
- Body Mechanics: Efficient, Coordinated, and SafeDocument31 pagesBody Mechanics: Efficient, Coordinated, and SafeRhea Lyn LamosteNo ratings yet
- Positioning Transfers and Mobility N Uens Et Al 3Document18 pagesPositioning Transfers and Mobility N Uens Et Al 3Neurorestorasi RSPONNo ratings yet
- Follow These Rules For Safety and Comfort: Four-Point Crutch GaitDocument11 pagesFollow These Rules For Safety and Comfort: Four-Point Crutch Gaitnot your medz duranNo ratings yet
- GeriatricsDocument14 pagesGeriatricsParul ThakurNo ratings yet
- What Is Crutch WalkingDocument3 pagesWhat Is Crutch WalkingMANANNo ratings yet
- Balance ExercisesDocument24 pagesBalance ExercisesAvantika BirwalNo ratings yet
- PNF TechniquesDocument26 pagesPNF Techniquesabdul haseebNo ratings yet
- NSG126 - 4 - G - Skills - 4&5 - Checklists - SIGNAR, NIKITADocument7 pagesNSG126 - 4 - G - Skills - 4&5 - Checklists - SIGNAR, NIKITANikita SignarNo ratings yet
- CrutchDocument135 pagesCrutchYahia Tawfeek AlkilanyNo ratings yet
- CrutchesDocument11 pagesCrutchesAaron Roxas100% (1)
- TKR ProtocolDocument8 pagesTKR ProtocolSandeep SoniNo ratings yet
- Transfers - Mam BoomDocument25 pagesTransfers - Mam BoomRonald Estrada PajeNo ratings yet
- Basic Body MechanicsDocument83 pagesBasic Body MechanicsCyrille Aira AndresaNo ratings yet
- By DR Nshimiyimana Alexis Orthopedic Resident-UrDocument35 pagesBy DR Nshimiyimana Alexis Orthopedic Resident-UrNshimiyimana AlexisNo ratings yet
- Skills Mechanical Aids in WalkingDocument3 pagesSkills Mechanical Aids in WalkingEiichiro BertoNo ratings yet
- Mobility AidsDocument80 pagesMobility AidsVara100% (1)
- Hip Exercise Progressions EccentricDocument6 pagesHip Exercise Progressions EccentricLakshmi PrasannaNo ratings yet
- Knee PP Revision:: 1. Flexion (0 - 135)Document13 pagesKnee PP Revision:: 1. Flexion (0 - 135)senoNo ratings yet
- Topic 5 NCM 100 Skillsbody Mechanics Final LectureDocument22 pagesTopic 5 NCM 100 Skillsbody Mechanics Final LecturePearl IbisateNo ratings yet
- Assisting With Ambul at I OnDocument15 pagesAssisting With Ambul at I OnAndrew Isiah BonifacioNo ratings yet
- Range of MotionDocument36 pagesRange of Motiontrk_hussain100% (2)
- SLAB - Positioning ClientsDocument23 pagesSLAB - Positioning ClientsjosephNo ratings yet
- Safe Patient Handling - Sitting Up and TransferringDocument12 pagesSafe Patient Handling - Sitting Up and TransferringgrazeyjvNo ratings yet
- Self StretchDocument4 pagesSelf StretchHiba RiazNo ratings yet
- Assistive DevicesDocument4 pagesAssistive Devicesmiameyah375No ratings yet
- Chest Physiotherapy Walking Aids: Basic Technique in PhysiotherapyDocument28 pagesChest Physiotherapy Walking Aids: Basic Technique in PhysiotherapyDr.GK. Jeyakumar100% (1)
- Transfer and AmbulationDocument108 pagesTransfer and AmbulationGladys YaresNo ratings yet
- Pelvic Stabilization Hip StrengtheningDocument8 pagesPelvic Stabilization Hip StrengtheningAnonymous Gq5RQ6K3dmNo ratings yet
- Sushibala Assignment 02Document5 pagesSushibala Assignment 02Ananda NgangomNo ratings yet
- Activity Mobility ExerciseDocument27 pagesActivity Mobility ExerciseMary SutingcoNo ratings yet
- Assistivedevices 200430182946Document48 pagesAssistivedevices 200430182946Roni's Lifestyle LifeNo ratings yet
- Ambulation and Gait TrainingDocument36 pagesAmbulation and Gait Trainingakuphysio100% (1)
- Exercise, Ambulation: Nursing 125Document13 pagesExercise, Ambulation: Nursing 125omar kmr97No ratings yet
- Range of MotionDocument59 pagesRange of MotionIsrael Jiel Fedelicio100% (1)
- What Is Posture?: Phclab Phclab Phclab PhclabDocument8 pagesWhat Is Posture?: Phclab Phclab Phclab PhclabMaria Theresa UyNo ratings yet
- Assist With Client or Patient MovementDocument88 pagesAssist With Client or Patient Movementmihret gashayeNo ratings yet
- Walking CruthesDocument15 pagesWalking Cruthesanna Tanur100% (1)
- Lower Crossed SyndromeDocument11 pagesLower Crossed SyndromeJúnior Alvacir Camargo50% (2)
- Functional Re-Education BasicsDocument3 pagesFunctional Re-Education BasicsShreevidya IyerNo ratings yet
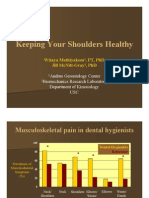
- Keeping Your Shoulders HealthyDocument38 pagesKeeping Your Shoulders Healthyxyz84No ratings yet
- CoordinationDocument73 pagesCoordinationHarsh RamiNo ratings yet
- Total Hip Replacement (THR) and Its RehabilitationDocument5 pagesTotal Hip Replacement (THR) and Its Rehabilitationfatimah.riazf16No ratings yet
- Assistive Devices - WalkerDocument51 pagesAssistive Devices - WalkerGrand Levi100% (1)
- Tips for Everyday Life and Sports With an Artificial Joint: Expert guidebook for dealing with a prosthesis for patients with a new hip or knee jointFrom EverandTips for Everyday Life and Sports With an Artificial Joint: Expert guidebook for dealing with a prosthesis for patients with a new hip or knee jointNo ratings yet
- Documentation System Focus ChartingDocument26 pagesDocumentation System Focus ChartingneehoshiNo ratings yet
- Perineal CareDocument2 pagesPerineal CareneehoshiNo ratings yet
- MCN LecDocument3 pagesMCN LecneehoshiNo ratings yet
- Case Analysis NOTESDocument5 pagesCase Analysis NOTESneehoshiNo ratings yet
- Virus ReviewerDocument6 pagesVirus ReviewerneehoshiNo ratings yet
- Asus T12C (X51C) Motherboard Schematic DiagramDocument94 pagesAsus T12C (X51C) Motherboard Schematic DiagramYblis100% (1)
- Lesson Plan Format (Acad)Document4 pagesLesson Plan Format (Acad)Aienna Lacaya MatabalanNo ratings yet
- Adriafil SummerDocument5 pagesAdriafil SummerTatu AradiNo ratings yet
- Research On Sustainable Development of Textile Industrial Clusters in The Process of GlobalizationDocument5 pagesResearch On Sustainable Development of Textile Industrial Clusters in The Process of GlobalizationSam AbdulNo ratings yet
- Science & Technology Current Affairs - Prelims 2019 PDFDocument171 pagesScience & Technology Current Affairs - Prelims 2019 PDFAditya KumarNo ratings yet
- BusDocument24 pagesBusSyed Noman AhmedNo ratings yet
- Methods?: Condoms Internal Condoms Sexually Transmissible Infections (Stis)Document25 pagesMethods?: Condoms Internal Condoms Sexually Transmissible Infections (Stis)Alecia R. CastilloNo ratings yet
- AHL Unit Removal For Pre 0305Document4 pagesAHL Unit Removal For Pre 0305Alex PioneerNo ratings yet
- Caudal Duplication Syndrome-Report of A CaseDocument4 pagesCaudal Duplication Syndrome-Report of A Casekhumaira1982No ratings yet
- CoEpower SVG AHF Price ListDocument2 pagesCoEpower SVG AHF Price ListChristian Huanca OscoNo ratings yet
- Ram Janm Bhumi Babri Masjid - Ayodhya BenchDocument251 pagesRam Janm Bhumi Babri Masjid - Ayodhya BenchNaresh KadyanNo ratings yet
- Makita 6910Document3 pagesMakita 6910El MacheteNo ratings yet
- Endovac BrochureDocument8 pagesEndovac BrochureGeorge MK100% (1)
- Straight DZR Brass Automatic Balancing Valve With Isolation Ball ValveDocument4 pagesStraight DZR Brass Automatic Balancing Valve With Isolation Ball ValveManuel Molina CamposNo ratings yet
- Campbeltown's Kilkerran Gun BatteryDocument2 pagesCampbeltown's Kilkerran Gun BatteryKintyre On RecordNo ratings yet
- Metabolizam SeceraDocument52 pagesMetabolizam SeceraAnel RedzepiNo ratings yet
- Raychem Molded PartsDocument28 pagesRaychem Molded PartsAMNo ratings yet
- Individual Development WorkoutDocument3 pagesIndividual Development WorkoutmichelleNo ratings yet
- Music Therapy When Death Is Imminent - A Phenomenological InquiryDocument32 pagesMusic Therapy When Death Is Imminent - A Phenomenological InquiryJuan Luis Köstner MartinoNo ratings yet
- 561566642977unit-3 - TextilesDocument11 pages561566642977unit-3 - TextilesGaganpreet Kaur Fashion DesigningNo ratings yet
- 5th Fancy BreadDocument7 pages5th Fancy BreadMera Funportal0% (1)
- Noise Computational Problem and Objective Type Questions For Quiz ShowDocument39 pagesNoise Computational Problem and Objective Type Questions For Quiz ShowJhasper ManagyoNo ratings yet
- Product Requirements Specification Process in ProdDocument12 pagesProduct Requirements Specification Process in ProdemmyNo ratings yet
- Chocolate From Cocoa - PPT 5.15Document21 pagesChocolate From Cocoa - PPT 5.15Sandhya ArulNo ratings yet
- Module 2 (People and The Earth's Ecosystem)Document11 pagesModule 2 (People and The Earth's Ecosystem)chris ian0% (2)
- Mobil - Welding Qa - QC and NDT Service - 20220927Document1 pageMobil - Welding Qa - QC and NDT Service - 20220927Wale OyeludeNo ratings yet
- ENV 107L.15 Assignment 1 Analysis of The Ecological Condition of A PondDocument4 pagesENV 107L.15 Assignment 1 Analysis of The Ecological Condition of A Pondsafwan shamsNo ratings yet
- CBSE Class 10 Revision WorksheetDocument13 pagesCBSE Class 10 Revision WorksheetEdward DevisNo ratings yet
- The Seven Spiritual Laws of Success BIZDocument7 pagesThe Seven Spiritual Laws of Success BIZDeac Roxana100% (2)
Mobility and Activity
Mobility and Activity
Uploaded by
neehoshi0 ratings0% found this document useful (0 votes)
15 views39 pagesMobility refers to the ability to move freely and purposefully. There are different types of exercise including isotonic, isometric, and isokinetic. Exercise provides benefits like increased flexibility and bone density but impaired mobility can lead to complications. Nursing interventions include proper positioning, range of motion exercises, ambulation assistance, nutrition support, and skin care to prevent pressure injuries. Devices like pillows, mattresses, and walkers can also help support mobility.
Original Description:
Original Title
MOBILITY AND ACTIVITY
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentMobility refers to the ability to move freely and purposefully. There are different types of exercise including isotonic, isometric, and isokinetic. Exercise provides benefits like increased flexibility and bone density but impaired mobility can lead to complications. Nursing interventions include proper positioning, range of motion exercises, ambulation assistance, nutrition support, and skin care to prevent pressure injuries. Devices like pillows, mattresses, and walkers can also help support mobility.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
15 views39 pagesMobility and Activity
Mobility and Activity
Uploaded by
neehoshiMobility refers to the ability to move freely and purposefully. There are different types of exercise including isotonic, isometric, and isokinetic. Exercise provides benefits like increased flexibility and bone density but impaired mobility can lead to complications. Nursing interventions include proper positioning, range of motion exercises, ambulation assistance, nutrition support, and skin care to prevent pressure injuries. Devices like pillows, mattresses, and walkers can also help support mobility.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 39
MOBILITY AND ACTIVITY
Mobility - The ability to move freely, easily, rhythmically
and purposefully
Range of Motion - The ROM of the joint is the maximum
movement that is possible for that joint.
Exercise - A type of physical activity defined as a planned,
structure and repetitive bodily movement done to improve
or maintain one or more components of physical fitness .
Types of Exercise
ISOTONIC - Dynamic exercise in which the muscle
shortens to produce contraction and movement
Ex. Running, walking, swimming, cycling
ISOMETRIC - Are those in which there is a change in
muscle tension but NO CHANGE in muscle length Tensing,
extending and pressing exercises
ISOKINETIC - Involves muscle contraction or tension
against a resistance
Aerobic exercise activity during which the amount of
oxygen taken into the body is greater than that used to
perform the activity.
Benefits of Exercise
Increases joint flexibility, tone and ROM
Bone density is maintained
Increases cardiac output and perfusion
Prevents pooling of secretions in the lungs
Improves appetite and facilitate peristalsis
Elevates the metabolic rate
Prevents stasis of urine
Produces a sense of well-being
IMPAIRED PHYSICAL MOBILITY
Complications of IMMOBILITY
1. Contractures, atrophy and stiffness
2. Foot drop
3. DVT
4. Hypostatic pneumonia
5. Pressure ulcers, skin breakdown, reduced skin turgor
6. Muscle atrophy
7. osteoporosis
8. dependent edema
9. urine stasis
10. constipation
ASSESSMENT
1. Assess patient’s ability to move
2. Assess muscle tone, strength
3. Assess joint movement and positioning
Nursing Interventions
1. Position properly to prevent contractures
Place trochanter roll from the iliac crest to the mid-
thigh to prevent EXTERNAL rotation
Place patient on wheelchair 90 degrees with the foot
resting flat on the floor/foot rest
Place foot board or high-heeled shoes to prevent foot
drop
Nursing Interventions
2. Maintain muscle strength and joint
mobility
Perform passive ROME
Perform assistive ROME
Perform active ROME
Move the joints three times TID
Nursing Interventions
3. Promote independent mobility
Warn patient of the orthostatic hypotension
when suddenly standing upright.
4. Assist patient with transfer
Assess patient’s ability to participate
Position yourself in front of the patient
Lock the wheelchair or the bed wheel
Use devices such as transfer boards, sliding
boards, trapeze and sheets
Assist patient with transfer
In general, the equipments are placed on the
side of the STRONGER , UNAFFECTED
body part .
Nurses assist the patient to move
TOWARDS the stronger side
In moving the patient, move to the direction
FACING the nurse
Nursing Interventions
5. Assist patient to prepare for ambulation
Exercise such as quadriceps setting, gluteal
setting and arm push ups
Use rubber ball for hand exercise
6. Assist patient in crutch ambulation
Measure correct crutch length
LYING DOWN
Measure from the Anterior Axillary Fold to the
HEEL of the foot then
Nursing Interventions
Add 1 inch (Kozier)
Add 2 inches (Brunner and Suddarth)
STANDING
(Kozier) - Mark a distance of 2 inches to the side from
the tip of the toe (first mark), 6 inches is marked
(second mark) ahead from the first Measure 2 inches
below the axilla to the second mark
Measure correct crutch length
STANDING (Kozier) Make sure that the shoulder-rest
of the crutch is at least 1- 2 inches below the axilla
Assist patient in crutch ambulation
Measure correct crutch length - Utilizing
the patient’s HEIGHT
Height MINUS 40 cm or 16 inches
Hand piece should allow 20-30 degrees
elbow flexion
Nursing Interventions
Assist patient in crutch GAIT
A. 4 point gait
B. three-point gait
C. two point gait
D. swing to gait
E. swing through gait
GAIT
4-point gait - Safest gait
Requires weight bearing on both legs
Move RIGHT crutch ahead (6 inches) Move LEFT foot
forward at the level of the RIGHT crutch Move the
LEFT crutch forward Move the RIGHT foot forward
GAIT
3-point gait - Requires weight bearing on the
UNAFECTED leg
Move BOTH crutches and the WEAKER LEG forward
Move the STRONGER leg forward
2-point gait - Faster than 4-point
Requires more balance
Partial bearing on BOTH legs
Move the LEFT crutch and RIGHT foot FORWARD
together
Move the RIGHT crutch and LEFT foot forward together
Swing-to gait
Swing-to gait - Usually used by client with
paralysis of both legs
Prolonged use results in atrophy of unused
muscle Move BOTH crutches together
Lift body weight by the arms and swing to
the crutches (at the level)
Swing-through gait
Swing-through gait - Move BOTH crutches
together Lift body weight by the arms and
swing forward, ahead of the crutches
(beyond the level)
Assist patient in ambulation with
a walker
Correct height of the walker must allow a
20-30 degrees of elbow flexion.
Assist patient in ambulation with
a cane
Assist patient in ambulation with a cane
Correct cane measurement:
With elbow flexion of 30 degrees, measure
the length from the HAND to 6 inches
lateral to the tip of the 5 th toe.
Nursing Interventions
IMPROVE MOBILITY
Active and passive exercises
Assistive exercise
Nursing Interventions
IMPROVE TISSUE PERFUSION
Exercise and repositioning are the most important
activities : AVOID MASSAGE ON THE REDDENED
AREAS
Nursing Interventions IMPROVE
NUTRITIONAL STATUS
HIGH protein , HIGH vitamin C diet Measure body
weight Assess hemoglobin and albumin
Nursing Interventions REDUCE FRICTION AND
SHEAR
Lift and not drag patient Prevent the presence of
wrinkles and creases on bed sheets.
Nursing Interventions to REDUCE IRRITATING
MOISTURE
Adhere to a meticulous skin care
Promptly clean and dry the soiled areas
Use mild soap and water
Lotion may be applied
AVOID powders (cause dryness)
Positions
Fowler’s Position - The Sitting position
Fowler’s Position (Low Fowler’s, Semi-fowler’s, High
Fowler’s
Orthopneic position The client sits in chair or bed,
with an over-bed table.
Dorsal Recumbent . Back-lying position, with head
and shoulders SLIGHTLY elevated
Prone The client lies on the abdomen with the head
usually turned to one side.
Positions
Lateral . Side-lying position
Sims – (Semi-prone position )
Support Devices
Pillows.
Mattresses
Suspension or heel guard boot.
Hand roll.
Abduction pillow.
Support Devices
Pillows The Slipp® Patient Mover
Support Devices
Suspension boot Heel guard
Support Devices
FootBoard Chair Bed
Support Devices
TROCHANTER
ROLLTROCHANTER
TTROLL Trochanter Rol
TRANSFER TRANSFER BELTBELT
.
OVER BED TABLE
.
STRETCHER
STRETCHER
Wheelchair
You might also like
- NDT by Dr. Rati.Document13 pagesNDT by Dr. Rati.Anup PednekarNo ratings yet
- Body Mechanics and Transferring PatientDocument57 pagesBody Mechanics and Transferring PatientRhenier S. Ilado100% (2)
- Assistive DevicesDocument30 pagesAssistive DevicesrlinaoNo ratings yet
- Computer Project 1: Assignment 1.1Document10 pagesComputer Project 1: Assignment 1.1Nelu TurcanuNo ratings yet
- Body Mechanics: Fundamental of Nursing IDocument55 pagesBody Mechanics: Fundamental of Nursing Irlinao100% (3)
- Skills 116 Finals ROM Assistive Devices PDFDocument64 pagesSkills 116 Finals ROM Assistive Devices PDFMae Arra Gilbao Lecobu-anNo ratings yet
- Chapter 2-Basic Care and ComfortDocument37 pagesChapter 2-Basic Care and ComfortWang Ming YaNo ratings yet
- Nursing RehabilitationDocument55 pagesNursing Rehabilitationnursereview100% (6)
- Ambulation With Crutches, Walker, Cane: PurposesDocument2 pagesAmbulation With Crutches, Walker, Cane: PurposesSienaNo ratings yet
- Assistive Devices For WalkingDocument4 pagesAssistive Devices For WalkingAbigail Mangaoang100% (1)
- HC - Transfer and AmbulationDocument14 pagesHC - Transfer and Ambulationblackangel07_angelie100% (2)
- AmbulationDocument18 pagesAmbulationDidik SusetiyantoNo ratings yet
- Assistive Devices For WalkingDocument4 pagesAssistive Devices For Walkingthomasfinley44No ratings yet
- Orthopedic NursingDocument154 pagesOrthopedic NursingTrisha Mae MarquezNo ratings yet
- Range of Motion ExerciseDocument8 pagesRange of Motion ExerciseAmit Martin83% (6)
- FUNDA REVIEW 2 Body MechanicsDocument27 pagesFUNDA REVIEW 2 Body Mechanicslovie dooNo ratings yet
- Body Mechanics: Efficient, Coordinated, and SafeDocument31 pagesBody Mechanics: Efficient, Coordinated, and SafeRhea Lyn LamosteNo ratings yet
- Positioning Transfers and Mobility N Uens Et Al 3Document18 pagesPositioning Transfers and Mobility N Uens Et Al 3Neurorestorasi RSPONNo ratings yet
- Follow These Rules For Safety and Comfort: Four-Point Crutch GaitDocument11 pagesFollow These Rules For Safety and Comfort: Four-Point Crutch Gaitnot your medz duranNo ratings yet
- GeriatricsDocument14 pagesGeriatricsParul ThakurNo ratings yet
- What Is Crutch WalkingDocument3 pagesWhat Is Crutch WalkingMANANNo ratings yet
- Balance ExercisesDocument24 pagesBalance ExercisesAvantika BirwalNo ratings yet
- PNF TechniquesDocument26 pagesPNF Techniquesabdul haseebNo ratings yet
- NSG126 - 4 - G - Skills - 4&5 - Checklists - SIGNAR, NIKITADocument7 pagesNSG126 - 4 - G - Skills - 4&5 - Checklists - SIGNAR, NIKITANikita SignarNo ratings yet
- CrutchDocument135 pagesCrutchYahia Tawfeek AlkilanyNo ratings yet
- CrutchesDocument11 pagesCrutchesAaron Roxas100% (1)
- TKR ProtocolDocument8 pagesTKR ProtocolSandeep SoniNo ratings yet
- Transfers - Mam BoomDocument25 pagesTransfers - Mam BoomRonald Estrada PajeNo ratings yet
- Basic Body MechanicsDocument83 pagesBasic Body MechanicsCyrille Aira AndresaNo ratings yet
- By DR Nshimiyimana Alexis Orthopedic Resident-UrDocument35 pagesBy DR Nshimiyimana Alexis Orthopedic Resident-UrNshimiyimana AlexisNo ratings yet
- Skills Mechanical Aids in WalkingDocument3 pagesSkills Mechanical Aids in WalkingEiichiro BertoNo ratings yet
- Mobility AidsDocument80 pagesMobility AidsVara100% (1)
- Hip Exercise Progressions EccentricDocument6 pagesHip Exercise Progressions EccentricLakshmi PrasannaNo ratings yet
- Knee PP Revision:: 1. Flexion (0 - 135)Document13 pagesKnee PP Revision:: 1. Flexion (0 - 135)senoNo ratings yet
- Topic 5 NCM 100 Skillsbody Mechanics Final LectureDocument22 pagesTopic 5 NCM 100 Skillsbody Mechanics Final LecturePearl IbisateNo ratings yet
- Assisting With Ambul at I OnDocument15 pagesAssisting With Ambul at I OnAndrew Isiah BonifacioNo ratings yet
- Range of MotionDocument36 pagesRange of Motiontrk_hussain100% (2)
- SLAB - Positioning ClientsDocument23 pagesSLAB - Positioning ClientsjosephNo ratings yet
- Safe Patient Handling - Sitting Up and TransferringDocument12 pagesSafe Patient Handling - Sitting Up and TransferringgrazeyjvNo ratings yet
- Self StretchDocument4 pagesSelf StretchHiba RiazNo ratings yet
- Assistive DevicesDocument4 pagesAssistive Devicesmiameyah375No ratings yet
- Chest Physiotherapy Walking Aids: Basic Technique in PhysiotherapyDocument28 pagesChest Physiotherapy Walking Aids: Basic Technique in PhysiotherapyDr.GK. Jeyakumar100% (1)
- Transfer and AmbulationDocument108 pagesTransfer and AmbulationGladys YaresNo ratings yet
- Pelvic Stabilization Hip StrengtheningDocument8 pagesPelvic Stabilization Hip StrengtheningAnonymous Gq5RQ6K3dmNo ratings yet
- Sushibala Assignment 02Document5 pagesSushibala Assignment 02Ananda NgangomNo ratings yet
- Activity Mobility ExerciseDocument27 pagesActivity Mobility ExerciseMary SutingcoNo ratings yet
- Assistivedevices 200430182946Document48 pagesAssistivedevices 200430182946Roni's Lifestyle LifeNo ratings yet
- Ambulation and Gait TrainingDocument36 pagesAmbulation and Gait Trainingakuphysio100% (1)
- Exercise, Ambulation: Nursing 125Document13 pagesExercise, Ambulation: Nursing 125omar kmr97No ratings yet
- Range of MotionDocument59 pagesRange of MotionIsrael Jiel Fedelicio100% (1)
- What Is Posture?: Phclab Phclab Phclab PhclabDocument8 pagesWhat Is Posture?: Phclab Phclab Phclab PhclabMaria Theresa UyNo ratings yet
- Assist With Client or Patient MovementDocument88 pagesAssist With Client or Patient Movementmihret gashayeNo ratings yet
- Walking CruthesDocument15 pagesWalking Cruthesanna Tanur100% (1)
- Lower Crossed SyndromeDocument11 pagesLower Crossed SyndromeJúnior Alvacir Camargo50% (2)
- Functional Re-Education BasicsDocument3 pagesFunctional Re-Education BasicsShreevidya IyerNo ratings yet
- Keeping Your Shoulders HealthyDocument38 pagesKeeping Your Shoulders Healthyxyz84No ratings yet
- CoordinationDocument73 pagesCoordinationHarsh RamiNo ratings yet
- Total Hip Replacement (THR) and Its RehabilitationDocument5 pagesTotal Hip Replacement (THR) and Its Rehabilitationfatimah.riazf16No ratings yet
- Assistive Devices - WalkerDocument51 pagesAssistive Devices - WalkerGrand Levi100% (1)
- Tips for Everyday Life and Sports With an Artificial Joint: Expert guidebook for dealing with a prosthesis for patients with a new hip or knee jointFrom EverandTips for Everyday Life and Sports With an Artificial Joint: Expert guidebook for dealing with a prosthesis for patients with a new hip or knee jointNo ratings yet
- Documentation System Focus ChartingDocument26 pagesDocumentation System Focus ChartingneehoshiNo ratings yet
- Perineal CareDocument2 pagesPerineal CareneehoshiNo ratings yet
- MCN LecDocument3 pagesMCN LecneehoshiNo ratings yet
- Case Analysis NOTESDocument5 pagesCase Analysis NOTESneehoshiNo ratings yet
- Virus ReviewerDocument6 pagesVirus ReviewerneehoshiNo ratings yet
- Asus T12C (X51C) Motherboard Schematic DiagramDocument94 pagesAsus T12C (X51C) Motherboard Schematic DiagramYblis100% (1)
- Lesson Plan Format (Acad)Document4 pagesLesson Plan Format (Acad)Aienna Lacaya MatabalanNo ratings yet
- Adriafil SummerDocument5 pagesAdriafil SummerTatu AradiNo ratings yet
- Research On Sustainable Development of Textile Industrial Clusters in The Process of GlobalizationDocument5 pagesResearch On Sustainable Development of Textile Industrial Clusters in The Process of GlobalizationSam AbdulNo ratings yet
- Science & Technology Current Affairs - Prelims 2019 PDFDocument171 pagesScience & Technology Current Affairs - Prelims 2019 PDFAditya KumarNo ratings yet
- BusDocument24 pagesBusSyed Noman AhmedNo ratings yet
- Methods?: Condoms Internal Condoms Sexually Transmissible Infections (Stis)Document25 pagesMethods?: Condoms Internal Condoms Sexually Transmissible Infections (Stis)Alecia R. CastilloNo ratings yet
- AHL Unit Removal For Pre 0305Document4 pagesAHL Unit Removal For Pre 0305Alex PioneerNo ratings yet
- Caudal Duplication Syndrome-Report of A CaseDocument4 pagesCaudal Duplication Syndrome-Report of A Casekhumaira1982No ratings yet
- CoEpower SVG AHF Price ListDocument2 pagesCoEpower SVG AHF Price ListChristian Huanca OscoNo ratings yet
- Ram Janm Bhumi Babri Masjid - Ayodhya BenchDocument251 pagesRam Janm Bhumi Babri Masjid - Ayodhya BenchNaresh KadyanNo ratings yet
- Makita 6910Document3 pagesMakita 6910El MacheteNo ratings yet
- Endovac BrochureDocument8 pagesEndovac BrochureGeorge MK100% (1)
- Straight DZR Brass Automatic Balancing Valve With Isolation Ball ValveDocument4 pagesStraight DZR Brass Automatic Balancing Valve With Isolation Ball ValveManuel Molina CamposNo ratings yet
- Campbeltown's Kilkerran Gun BatteryDocument2 pagesCampbeltown's Kilkerran Gun BatteryKintyre On RecordNo ratings yet
- Metabolizam SeceraDocument52 pagesMetabolizam SeceraAnel RedzepiNo ratings yet
- Raychem Molded PartsDocument28 pagesRaychem Molded PartsAMNo ratings yet
- Individual Development WorkoutDocument3 pagesIndividual Development WorkoutmichelleNo ratings yet
- Music Therapy When Death Is Imminent - A Phenomenological InquiryDocument32 pagesMusic Therapy When Death Is Imminent - A Phenomenological InquiryJuan Luis Köstner MartinoNo ratings yet
- 561566642977unit-3 - TextilesDocument11 pages561566642977unit-3 - TextilesGaganpreet Kaur Fashion DesigningNo ratings yet
- 5th Fancy BreadDocument7 pages5th Fancy BreadMera Funportal0% (1)
- Noise Computational Problem and Objective Type Questions For Quiz ShowDocument39 pagesNoise Computational Problem and Objective Type Questions For Quiz ShowJhasper ManagyoNo ratings yet
- Product Requirements Specification Process in ProdDocument12 pagesProduct Requirements Specification Process in ProdemmyNo ratings yet
- Chocolate From Cocoa - PPT 5.15Document21 pagesChocolate From Cocoa - PPT 5.15Sandhya ArulNo ratings yet
- Module 2 (People and The Earth's Ecosystem)Document11 pagesModule 2 (People and The Earth's Ecosystem)chris ian0% (2)
- Mobil - Welding Qa - QC and NDT Service - 20220927Document1 pageMobil - Welding Qa - QC and NDT Service - 20220927Wale OyeludeNo ratings yet
- ENV 107L.15 Assignment 1 Analysis of The Ecological Condition of A PondDocument4 pagesENV 107L.15 Assignment 1 Analysis of The Ecological Condition of A Pondsafwan shamsNo ratings yet
- CBSE Class 10 Revision WorksheetDocument13 pagesCBSE Class 10 Revision WorksheetEdward DevisNo ratings yet
- The Seven Spiritual Laws of Success BIZDocument7 pagesThe Seven Spiritual Laws of Success BIZDeac Roxana100% (2)