Professional Documents
Culture Documents
Ehad 488
Ehad 488
Uploaded by
Jorge ZúnigaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ehad 488
Ehad 488
Uploaded by
Jorge ZúnigaCopyright:
Available Formats
European Heart Journal (2023) 00, 1–3 VIEWPOINT
https://doi.org/10.1093/eurheartj/ehad488 Heart failure and cardiomyopathies
REVIV(E)ing the ischaemic paradigm in heart
failure: STICHes are needed
Downloaded from https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehad488/7234447 by guest on 06 August 2023
1,2,3
Luis E. Rohde * and John J.V. McMurray1,2,3
1
Medical School, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil; 2Cardiovascular Division, Hospital de Clínicas de Porto Alegre and Hospital Moinhos de Vento, Porto
Alegre, Brazil; and 3British Heart Foundation Cardiovascular Research Centre, School of Cardiovascular and Metabolic Health at the University of Glasgow, Glasgow, UK
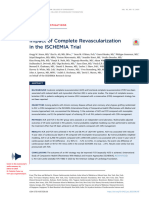
Graphical Abstract
REVIV(E)ing the ischaemic paradigm in heart failure: STICHes are needed
STICH(ES) & REVIVED-BCIS2 REVIVED-BCIS2 Trial STICH(ES) Trial
Trials asked a similar question Sample size 700 1212
Does revascularization of patients with CAD and left Year of enrolment 2013–2020 2002–2007
ventricular dysfunction improve clinical outcomes?
Mode of revascularization Percutaneous Surgical
NYHA class III-IV 26% 37%
Main findings were conflicting
Angina pectoris 33% 64%
CABG reduced all-cause mortality in STICHES
after extended follow-up Previous MI 53% 77%
PCI did not reduce all-cause mortality or HF
LVEF 27% 27% (CABG); 28% (medical)
hospitalization in REVIVED-BCIS2
Left main disease 13.6% 2.6%
Several possible explanations Three-vessel CAD 40% 60%
Patient profile, mode of revascularization, sample Medical therapy
size and follow-up were different in each trial
Beta blockers 91% 85%
CAD might be a “bystander” rather than cause
of systolic dysfunction in some patients ACEi or ARBs 84% 90%
Mineralocorticoid antagonist 49% 46%
What advice to patients?
What is to come? ICD 21% 2.4%*
Both PCI and CABG continue to be important Primary outcome All-cause death or HF hospitalization All-cause death
treatments for symptomatic myocardial ischaemia
Mortality rate in GDMT group 33% over 41 months 41% over 56 months †
CABG has a specific indication in selected
patients to improve outcomes in HF Deaths in GDMT group 115 244 †
STICH-3 will compare PCI & CABG Follow-up, median 3.4 years 4.7 years † & 9.3 years ‡
Critical comparison between REVIVED-BCIS2 and STICH(ES) trials. NYHA, New York Heart Association; MI, myocardial infarction; LVEF, left ventricu-
lar ejection fraction; CAD, coronary artery disease; ACEi, angiotensin converting enzyme inhibitor; ARBs, angiotensin receptor blockers; ICD, implan-
table cardio-defibrillator; HF, heart failure; GDMT, guideline directed medical therapy. *Only baseline ICD was reported. †Based on the 2011
publication. ‡Based on the extended follow-up 2016 publication.
* Corresponding author. Tel: + 55 51 33598342, Email: rohde.le@gmail.com
© The Author(s) 2023. Published by Oxford University Press on behalf of the European Society of Cardiology. All rights reserved. For permissions, please e-mail: journals.permissions@oup.com
2 Viewpoint
Over recent decades, heart failure with reduced ejection fraction evaluated in sub-studies of REVIVED and STICHES.8,9 At face value,
(HFrEF) has been transformed from a highly lethal disorder with a short findings from both trials do not support the concept that using pre-
life expectancy to a more chronic condition with much-improved qual- sumed myocardial viability to guide myocardial revascularization leads
ity and quantity of life.1 Most of these successful therapies modulate to better outcomes in ischaemic cardiomyopathy. In STICHES, the
homeostatic systems that are deleteriously activated after an index insult presence of viable myocardium was associated with improvement in
to the heart. Despite unquestionable benefits, our therapeutic actions LV systolic function, but such improvement was not related to long-
are primarily restricted to ameliorating the secondary consequences of term survival. The opposite was observed in REVIVED where dysfunc-
reduced cardiac contractility. However, therapeutic strategies aimed at tional viable myocardial did not predict LV recovery. However, the
Downloaded from https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehad488/7234447 by guest on 06 August 2023
preventing recurrent direct myocardial injury, e.g. due to further coron- presence of greater scar burden seemed to identify patients with re-
ary artery occlusion, should also be a priority. Moreover, in patients with duced likelihood of improvement LV function (and improvement in
severe obstructive coronary artery disease (CAD), chronic myocardial LVEF was a predictor of better outcome). It is important to note
hypoperfusion may cause or exacerbate left ventricular (LV) systolic dys- that both these subs-studies were small, and their results are unreliable.
function (hibernating myocardium), and this might be reversible with res- Unfortunately, most other clinical studies that tried to address the role
toration of coronary blood flow.2 The logical extension of this of viability-guided revascularization have used nonrandomized designs,
conceptual framework, if correct, is that diagnosis and treatment of heterogenous protocols, and different imaging techniques. The incon-
CAD should be central to the management of patients with HFrEF. sistent results in these reports highlight the uncertainty around the def-
Surprisingly, however, few randomized clinical trials have evaluated the inition and quantification of myocardial viability and whether attempting
efficacy and safety of coronary revascularization in patients with HFrEF. to assess myocardial viability is worthwhile in clinical practice.
The Surgical Treatment for Ischaemic Heart Failure (STICH) trial was Clinicians now face the difficult task of reconciling these two apparently
designed to evaluate the role of cardiac surgery in the treatment of pa- conflicting trial outcomes and confusing findings related to myocardial via-
tients with CAD and LV systolic dysfunction. One of the central hy- bility and deciding what to advise their patients. In comparing these trials,
potheses of STICH was that coronary artery bypass surgery (CABG) we need to consider the patients enrolled, their background treatment,
and medical therapy would reduce overall mortality compared to med- the randomized intervention used, and the size and power of the
ical therapy alone. In 2011, the initial results of STICH showed that the trial (Graphical Abstract). Although the eligibility criteria for both trials
primary outcome—the rate of death from any cause—occurred in 244 were similar—extensive CAD associated with severe systolic dysfunc-
of 602 patients (41%) in the medical-therapy group and 218 of 610 pa- tion—the participants enrolled had different clinical profiles. Most
tients (36%) in the CABG group, representing a 14% non-significant STICH patients had symptomatic CAD, previous myocardial infarction,
relative risk reduction over a median follow-up of 56 months.3 Based and three-vessel disease, while the participants in REVIVED had asymp-
in part on the results of STICH, international heart failure (HF) guide- tomatic or mildly symptomatic CAD and two-vessel disease. Although pa-
lines in 2013 made only a weak recommendation supporting CABG tients were selected to be at high risk of acute coronary occlusion (as well
in HF patients with severe systolic dysfunction.4 Five years later, the as having potentially hypoperfused but viable myocardium), it is worth re-
publication of the extended follow-up study (STICHES) rekindled inter- membering that the contribution of coronary events to adverse outcomes
est in coronary revascularization as a treatment for HFrEF patients. even in patients with HFrEF is small. Effective pharmacological therapies
Over a median follow-up of 9.8 years, CABG reduced rates of death preventing plaque rupture (rosuvastatin)10 and thrombosis (rivaroxa-
from any cause, death from cardiovascular causes, and the rates of ban)11 had little if any impact on HF outcomes, particularly death, sudden
the combined endpoint of death from any cause or hospitalization death, and HF hospitalization (which constitute most adverse events in pa-
for cardiovascular causes significantly.5 Although much more time tients with HFrEF).
had been necessary to unequivocally demonstrate the difference be- Any difference in outcome between the two trials probably cannot
tween treatment groups, the magnitude of benefit was not trivial— be explained by concomitant medical therapy which was similar in each
only 14 patients needed surgery to avoid one death. study. Although use of device therapy was lower than expected in both
Recently, a second trial clouded the picture once again. The studies, it was much better in REVIVED than STICH which may have
Revascularization for Ischaemic Ventricular Dysfunction (REVIVED) trial reduced the background mortality rate in the former trial. Regarding
tested a similar hypothesis to the STICH trial. The REVIVED investigators the randomized intervention, incomplete revascularization has historic-
hypothesized that revascularization with percutaneous coronary interven- ally been the Achilles heel of percutaneous intervention, although the
tion (PCI) in addition to optimal medical therapy, as compared with opti- completeness of revascularization was reported to be high in the PCI
mal medical therapy alone, would improve event-free survival (and ejection group in REVIVED. Similarly, the durability of revascularization with ar-
fraction) in patients with severe ischaemic LV systolic dysfunction and terial grafting is superior compared to percutaneous intervention.
myocardial viability confirmed by cardiac imaging. Unfortunately, neither Bypass surgery also seems to offer greater protection against myocar-
of these benefits was demonstrated. Over a median of 41 months, the dial infarction than PCI, and prevention of further ischaemic injury
rate of the primary outcome—death from any cause or hospitalization might have resulted in greater protection in STICH than REVIVED.
for HF—was similar between groups, occurring in 129 of 347 patients The clinical profile of the participants and the potential advantages of
(37%) in the PCI group and 134 of 353 patients (38%) in the surgery plus the larger sample size and longer follow-up may have led
optimal-medical-therapy group. Left ventricular ejection fraction increased to the difference in outcome between the two trials. Due to the low
in both groups but did not differ meaningfully by treatment assignment.6 rate of coronary events in patients with HFrEF alluded to above, it
Central to one of the hypothesized benefits of coronary revascular- would be necessary to follow a large number of patients for a longer
ization is the existence of significant amounts of viable but dysfunctional time before the benefit of an effective treatment could be identified.
myocardium in patients with HFrEF and CAD, that this can be accurate- Another subtle but fundamentally important question is how much
ly identified and quantified, and that it is reversible after improvement in the patient’s CAD in each trial was contributing to their ventricular
coronary perfusion.7 The association between myocardial viability and dysfunction, HF symptoms, or both? From a practical perspective,
LV recovery, and between viability and prognosis, has also been we should consider that the historical delineation of ischaemic vs.
Viewpoint 3
non-ischaemic cardiomyopathy may not be as simple as previously Novartis. J.M. reports payments through Glasgow University from
thought. Was CAD patho-physiologically linked to myocardial hypoperfu- work on clinical trials, consulting and other activities from: Amgen,
sion and systolic dysfunction or essentially a ‘bystander’ with respect to AstraZeneca, Bayer, Cardurion, Cytokinetics, GSK, KBP Biosciences,
ventricular function (e.g. stenosed vessels supply predominantly scar tissue and Novartis. Personal consultancy fees from: Alnylam Pharma.,
or stenosed vessels that do not truly cause myocardial ischaemia)? Did the Bayer, BMS, George Clinical PTY Ltd., Ionis Pharma., Novartis,
patients in STICH, with more severe and symptomatic CAD, have more Regeneron Pharma., and River 2 Renal Corporation. J.M. reports per-
‘recoverable’ myocardium? It is not possible to answer all these questions sonal lecture fees from Abbott, Alkem Metabolics, Astra Zeneca,
from the data available, but it could be crucial to explaining the different Blue Ocean Scientific Solutions Ltd., Boehringer Ingelheim, Canadian
Downloaded from https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehad488/7234447 by guest on 06 August 2023
outcomes between the two trials. Medical and Surgical Knowledge, Emcure Pharma. Ltd., Eris
Finally, neither STICH nor REVIVED had sufficient statistical power to Lifesciences, European Academy of CME, Hikma Pharmaceuticals,
detect more than a large effect of treatment on mortality. This was espe- Imagica health, Intas Pharma, J.B. Chemicals & Pharma. Ltd., Lupin
cially true of REVIVED, which was much smaller than STICH with many Pharma, Medscape/Heart.Org, ProAdWise Communications,
fewer deaths (115 vs. 244) in the respective medical therapy groups. The Radcliffe Cardiology, Sun Pharma., The Corpus, Translation Research
apparent mortality reduction in the extended follow-up of STICHES, Group, and Translational Medicine Academy. J.M. is a director of
with a corresponding increase in the number of deaths over time, lends sup- Global Clinical Trial Partners Ltd.
port to the view that the original trial was underpowered. Notably, viability
sub-studies were even more underpowered for treatment effect on clinical References
events. From this perspective, we cannot conclude that the findings of 1. Vaduganathan M, Claggett BL, Jhund PS, Cunningham JW, Pedro Ferreira J, Zannad F,
STICH and REVIVED are truly different, and longer follow-up of et al. Estimating lifetime benefits of comprehensive disease-modifying pharmacological
REVIVED with accrual of more deaths is necessary to get a better assess- therapies in patients with heart failure with reduced ejection fraction: a comparative
analysis of three randomised controlled trials. Lancet 2020;396:121–8. https://doi.org/
ment of whether the two interventions resulted in different outcomes. 10.1016/S0140-6736(20)30748-0
So, what is the current role of coronary revascularization in patients 2. Kloner RA. Stunned and hibernation myocardium. Where are we nearly 4
with HFrEF? First, both percutaneous and surgical coronary revasculariza- decades later? J Am Heart Assoc 2020;9:e015502. https://doi.org/10.1161/JAHA.119.
015502
tion continue to be important treatments for symptomatic myocardial is-
3. Velasquez EJ, Lee KL, Deja MA, Jain A, Sopko G, Marchenko A, et al. Coronary-artery
chaemia i.e. angina pectoris. However, the role of percutaneous coronary bypass surgery in patients with left ventricular dysfunction. N Engl J Med 2011;364:
revascularization as a treatment for HF per se, to reduce the risk of death 1607–16. https://doi.org/10.1056/NEJMoa1100356
and HF hospitalization, is unproven. Even in current guidelines, surgical 4. Yancy C, Jessup M, Boskurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA
guideline for the management of heart failure. A report of the American College of
coronary revascularization has a limited and specific indication to improve Cardiology Foundation/American Heart Association task force on practice guidelines.
mortality in HF only in carefully selected individuals (e.g. young non-frail Circulation 2013;128:e240–327. https:doi.org/10.1161/CIR.0b013e31829e8776
patients with few comorbid conditions).12 A recent meta-analysis of ran- 5. Velasquez EJ, Lee KL, Jones RH, Al-Khalidi HR, Hill JA, Panza JA, et al. Coronary-artery
domized clinical trials of revascularization strategies in HF supports this bypass surgery in patients with left ventricular dysfunction. N Engl J Med 2016;374:
1511–20. https://doi.org/10.1056/NEJMoa1602001
recommendation but suggest lack of statistical robustness.13 So, overall, 6. Perera D, Clayton T, O’Kane PD, Greenwood JP, Weerackody R, Ryan M, et al.
the ischaemic paradigm remains alive in HF, and REVIVED has not changed Percutaneous revascularization for ischemic left ventricular dysfunction. N Engl J Med
the cautious recommendations based upon STICHES. At present, the role 2022;387:1351–60. https://doi.org/10.1056/NEJMoa2206606
7. Ryan M, Morgan H, Chiribiri A, Nagel E, Cleland J, Perera D. Myocardial viability testing:
of pre-treatment evaluation of myocardial viability and hibernation in guid-
all STICHed up, or about to be REVIVED? Eur Heart J 2022;43:118–26. https://doi.org/
ing treatment and predicting benefit from myocardial revascularization 10.1093/eurheartj/ehab729
can be neither convincingly affirmed nor refuted, and this should remain 8. Panza JA, Ellis AM, Al-Khalidi HR, Holly TA, Berman DS, Oh JK, et al. Myocardial viability
a key area of research.14 Unquestionably, we need further trials to give and long-term outcomes in ischemic cardiomyopathy. N Engl J Med 2019;381:739–48.
https://doi.org/10.1056/NEJMoa1807365
more definitive answers about how to identify patients who might benefit 9. Effect of myocardial viability, percutaneous coronary intervention and functional recov-
from coronary revascularization and how coronary revascularization is ery on clinical outcomes in the REVIVED-BCIS2 randomized trial. Presented by Divaka
best performed. An international consortium (STICH-3) has recently in- Perera at the American College of Cardiology Annual Scientific Session (ACC.23/
WCC), New Orleans, LA, March 4, 2023.
itiated a randomized clinical trial (NCT05761067) to determine whether
10. Kjekshus J, Apetrei E, Barrios V, Böhm M, Cleland JG, Cornel JH, et al. Rosuvastatin in
CABG is superior to PCI in terms of all-cause mortality in patients with older patients with systolic heart failure. N Engl J Med 2007;357:2248–61. https://doi.
severe CAD and LV systolic dysfunction.15 Unfortunately, however, org/10.1056/NEJMoa0706201
STICH-3 does not have a medically treated group, and there is no pre- 11. Zannad F, Anker SD, Byra WM, Cleland JGF, Fu M, Gheorghiade M, et al.
COMMANDER HF Investigators. Rivaroxaban in patients with heart failure, sinus
defined viability protocol or viability eligibility criteria. It seems remarkable rhythm, and coronary disease. N Engl J Med 2018;379:1332–42. https://doi.org/10.
that in 2023, we do not have a robust and clear answer to such important 1056/NEJMoa1808848
questions about the intersection between the two most important pro- 12. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021
blems we encounter in modern cardiology. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure:
developed by the task force for the diagnosis and treatment of acute and chronic
heart failure of the European Society of Cardiology (ESC) with the special contribu-
tion of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2021;42:
Supplementary data 3599–726. https:doi.org/10.1093/eurheartj/ehab368
13. Iaconelli A, Pellicori P, Dolce P, Busti M, Ruggio A, Aspromonte N, et al. Coronary re-
Supplementary data are not available at European Heart Journal online. vascularization for heart failure with coronary artery disease: a systematic review and
meta-analysis of randomized trials. Eur J Heart Fail 2023. https://doi.org/10.1002/ejhf.
2911
Declaration 14. Liga R, Colli A, Taggart DP, Boden WE, De Caterina R. Myocardial revascularization in
patients with ischemic cardiomyopathy: for whom and how. J Am Heart Assoc 2023;12:
Disclosure of Interest e026943. https://doi.org/10.1161/JAHA.122.026943
15. Clinicaltrials.gov. The CABG or PCI in Patients With Ischemic Cardiomyopathy
L.E.R. has received consulting or personal lecture fees from Aché, (STICH) 3.0 International Trial Consortium. https://www.clinicaltrials.gov/ct2/show/
AstraZeneca, Bayer, Boehringer Ingelheim, Merck Serono, and NCT05761067. (1 July 2023, date last accessed).
You might also like
- Kirklin Barratt-Boyes - Cardiac Surgery 2013Document2,059 pagesKirklin Barratt-Boyes - Cardiac Surgery 2013Nilutpal Dhar100% (13)
- Mashaba FilesDocument1,268 pagesMashaba FilesGugu TeoNo ratings yet
- Original Research Abstract AFCC ASMIHA 2019Document82 pagesOriginal Research Abstract AFCC ASMIHA 2019Program Studi Kardiologi100% (1)
- The Circulatory System BookletDocument30 pagesThe Circulatory System BookletTroy CampbellNo ratings yet
- Perera Et Al 2023 Arrhythmia and Death Following Percutaneous Revascularization in Ischemic Left VentricularDocument10 pagesPerera Et Al 2023 Arrhythmia and Death Following Percutaneous Revascularization in Ischemic Left VentriculardiegoiglesiasNo ratings yet
- Bleeding and Ischemic Risks of Ticagrelor Monotherapy After Coronary InterventionsDocument14 pagesBleeding and Ischemic Risks of Ticagrelor Monotherapy After Coronary InterventionsKardiologi ManadoNo ratings yet
- To Stent or Not To Stent in Ischemic Heart Failure - The REVIVED-BCIS2 Trial - AmDocument2 pagesTo Stent or Not To Stent in Ischemic Heart Failure - The REVIVED-BCIS2 Trial - AmHand SanitizerNo ratings yet
- LM LagiDocument4 pagesLM LagiJicko Street HooligansNo ratings yet
- AmiloidozaDocument9 pagesAmiloidozame1921No ratings yet
- Diagnostics: Cardiac Resynchronization Therapy in Non-Ischemic Cardiomyopathy: Role of Multimodality ImagingDocument15 pagesDiagnostics: Cardiac Resynchronization Therapy in Non-Ischemic Cardiomyopathy: Role of Multimodality Imagingmarsim92No ratings yet
- CardiologyDocument7 pagesCardiologyEmanuela SîrbuNo ratings yet
- Nejmoa 2206606Document10 pagesNejmoa 2206606dipan diratuNo ratings yet
- The Hybrid Coronary Approach For Optimal Revascularization: JACC Review Topic of The WeekDocument13 pagesThe Hybrid Coronary Approach For Optimal Revascularization: JACC Review Topic of The WeekAhmad FauzanNo ratings yet
- Beta-Blockers in Asymptomatic Coronary Artery Disease: No Benefit or No Evidence?Document3 pagesBeta-Blockers in Asymptomatic Coronary Artery Disease: No Benefit or No Evidence?Yolanda Karoline PasaribuNo ratings yet
- Stone Et Al 2023 Impact of Complete Revascularization in The Ischemia TrialDocument14 pagesStone Et Al 2023 Impact of Complete Revascularization in The Ischemia TrialKardiologi ManadoNo ratings yet
- Jamacardiology Perera 2023 Oi 230054 1696866153.86277Document8 pagesJamacardiology Perera 2023 Oi 230054 1696866153.86277Omar MedinaNo ratings yet
- Revascularization in Stable Coronary Artery Disease Review BMJDocument17 pagesRevascularization in Stable Coronary Artery Disease Review BMJucicardiocovid ocgnNo ratings yet
- 998 FullDocument7 pages998 FullsilviaNo ratings yet
- Multivessel CADDocument4 pagesMultivessel CADJohn HetharieNo ratings yet
- Revascularizar ICC No Mejora PronosticoDocument10 pagesRevascularizar ICC No Mejora Pronosticokaren mendoza rodriguezNo ratings yet
- Revived Bcis2 TrialDocument10 pagesRevived Bcis2 TrialSundaresan SankarNo ratings yet
- Lancet CABG in Patients With Diabetes and Multivessel Diseas (Commento 10 Marzo)Document2 pagesLancet CABG in Patients With Diabetes and Multivessel Diseas (Commento 10 Marzo)Mr. LNo ratings yet
- Clinical Implications of Complete LeftSided Reverse Remodeling With Cardiac Resynchronization Therapy.Document9 pagesClinical Implications of Complete LeftSided Reverse Remodeling With Cardiac Resynchronization Therapy.Kevin Padilla OlivoNo ratings yet
- 10.1136@heartjnl 2020 316605Document6 pages10.1136@heartjnl 2020 316605KEERTIMAAN JOSHINo ratings yet
- Article - Surgical Management of Infective Endocarditis - Early Predictors of Short-Term Morbidity and MortalityDocument6 pagesArticle - Surgical Management of Infective Endocarditis - Early Predictors of Short-Term Morbidity and Mortalityfluid_man_brazilNo ratings yet
- Comparison of Left Bundle Branch Area Pacing and BiventricularDocument14 pagesComparison of Left Bundle Branch Area Pacing and BiventricularRomán Wagner Thomas Esteli ChávezNo ratings yet
- Keywords:-STS Score, MACE, CABGDocument6 pagesKeywords:-STS Score, MACE, CABGInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 1 s2.0 S0735109722052615 MainDocument13 pages1 s2.0 S0735109722052615 MainMurat MukharyamovNo ratings yet
- Jurnal Kardio3Document8 pagesJurnal Kardio3Andi SusiloNo ratings yet
- Jamacardiology Watanabe 2022 Oi 210085 1648745334.74675Document11 pagesJamacardiology Watanabe 2022 Oi 210085 1648745334.74675anamunaier.18No ratings yet
- Shankar Et Al 2022 A Clinical Update On Vasoactive Medication in The Management of Cardiogenic ShockDocument11 pagesShankar Et Al 2022 A Clinical Update On Vasoactive Medication in The Management of Cardiogenic ShockNguyen SuNo ratings yet
- Perioperative Hemodynamic Monitoring and GDT Concepts in TraumaDocument427 pagesPerioperative Hemodynamic Monitoring and GDT Concepts in TraumaHendy MasjayantoNo ratings yet
- Predictores CLDocument10 pagesPredictores CLAlejandra Olivares VargasNo ratings yet
- Contrast-Induced Acute Kidney Injury After Primary Percutaneous Coronary Intervention: Results From The HORIZONS-AMI SubstudyDocument9 pagesContrast-Induced Acute Kidney Injury After Primary Percutaneous Coronary Intervention: Results From The HORIZONS-AMI SubstudysarahNo ratings yet
- 2022 Velagelati LVEF PCI Vs CABGDocument8 pages2022 Velagelati LVEF PCI Vs CABGTheresia Sri RezekiNo ratings yet
- Ehac 811Document3 pagesEhac 811Rositaka1991No ratings yet
- International Journal of Cardiology: SciencedirectDocument8 pagesInternational Journal of Cardiology: SciencedirectsarahNo ratings yet
- Jaha 120 019114Document28 pagesJaha 120 019114Andi Tiara S. AdamNo ratings yet
- Original Investigation: ImportanceDocument9 pagesOriginal Investigation: ImportancesarahNo ratings yet
- Freedom TrialDocument34 pagesFreedom TrialDaniela DíazNo ratings yet
- Kuno 2020Document2 pagesKuno 2020Dr. RajibNo ratings yet
- Completeness of Revascularisation in Acute Coronary Syndrome Patients With MultiDocument13 pagesCompleteness of Revascularisation in Acute Coronary Syndrome Patients With MultiDhiraj Kr GauravNo ratings yet
- Jurnal InternalDocument10 pagesJurnal InternalseptikusumaNo ratings yet
- Thrombectomy in Extensive Stroke May Not Be Beneficial and Is Associated With Increased Risk For HemorrhageDocument9 pagesThrombectomy in Extensive Stroke May Not Be Beneficial and Is Associated With Increased Risk For HemorrhageAlex LüttichNo ratings yet
- Cartlidge Timothy Role of Percutaneous CoronaryDocument7 pagesCartlidge Timothy Role of Percutaneous Coronarybruno baileyNo ratings yet
- Tutorial ElectrocardiogramaDocument6 pagesTutorial ElectrocardiogramakodagaNo ratings yet
- Voskoboinik2020 ABC SCOREDocument9 pagesVoskoboinik2020 ABC SCOREVallejo Romo Alberto CristianNo ratings yet
- Acs 07 04 506Document10 pagesAcs 07 04 506Mohammed ThabtNo ratings yet
- Use of Lipid-, Blood Pressure-, and Glucose-Lowering PharmacotherapyDocument15 pagesUse of Lipid-, Blood Pressure-, and Glucose-Lowering PharmacotherapyTuan NguyenNo ratings yet
- Optimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionDocument7 pagesOptimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionsarahNo ratings yet
- Nej Me 2210183Document2 pagesNej Me 2210183lakshminivas PingaliNo ratings yet
- Biological Variation of Cardiac Markers in Patients With Aortic Valve StenosisDocument7 pagesBiological Variation of Cardiac Markers in Patients With Aortic Valve StenosisAstridApriliaSimanjuntakNo ratings yet
- Anestesi 5Document7 pagesAnestesi 5Dina RyantiNo ratings yet
- De Baat 2021Document7 pagesDe Baat 2021Dhan RamadhanNo ratings yet
- Packer 2019Document14 pagesPacker 2019Renata D GNo ratings yet
- Coronary Revascularization For Heart Failure With Coronary Artery DiseaseDocument11 pagesCoronary Revascularization For Heart Failure With Coronary Artery DiseasediegoiglesiasNo ratings yet
- Van Der Schaar Et Al 2022 Reduced Heart Failure and Mortality in Patients Receiving Statin Therapy Before Initial AcuteDocument13 pagesVan Der Schaar Et Al 2022 Reduced Heart Failure and Mortality in Patients Receiving Statin Therapy Before Initial AcuteRizky AisNo ratings yet
- Antithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextDocument12 pagesAntithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextenviNo ratings yet
- Relation of Ejection Fraction and Inducible Ventricular Tachycardia To Mode of Death in Patients With Coronary Artery DiseaseDocument7 pagesRelation of Ejection Fraction and Inducible Ventricular Tachycardia To Mode of Death in Patients With Coronary Artery Diseaseapi-26169291No ratings yet
- Use of Chads and Cha Ds - Vasc Scores To Predict Prognosis After StrokeDocument7 pagesUse of Chads and Cha Ds - Vasc Scores To Predict Prognosis After Strokealexander alanNo ratings yet
- En V27n4a04Document4 pagesEn V27n4a04Rodrigo AbreuNo ratings yet
- Role of Exercise Treadmill Testing in The Assessment of Coronary Microvascular Disease - LopezDocument10 pagesRole of Exercise Treadmill Testing in The Assessment of Coronary Microvascular Disease - LopezM. PurnomoNo ratings yet
- Cardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesFrom EverandCardiac Sarcoidosis: Key Concepts in Pathogenesis, Disease Management, and Interesting CasesNo ratings yet
- NSG 6001 Final Exam 1 - Question and AnswersDocument49 pagesNSG 6001 Final Exam 1 - Question and AnswersDAVIDNo ratings yet
- Abel Wakai Diagnosis and Management of Patients WithDocument2 pagesAbel Wakai Diagnosis and Management of Patients WithJuliaNo ratings yet
- Atenolol: Atenolol Is A Beta Blocker MedicationDocument6 pagesAtenolol: Atenolol Is A Beta Blocker MedicationAbdelrhman AboodaNo ratings yet
- 21 GMS Bedah JantungDocument140 pages21 GMS Bedah JantungNuravif SetianingrumNo ratings yet
- From Clinical Data To RWE - DOAC For Secondary Stroke Prevention in AF PatientsDocument7 pagesFrom Clinical Data To RWE - DOAC For Secondary Stroke Prevention in AF PatientsYunita Christiani BiyangNo ratings yet
- Emergency Protocols Book FinalDocument137 pagesEmergency Protocols Book Finalsilverbat91No ratings yet
- TAPSE AgainDocument8 pagesTAPSE Againomotola ajayiNo ratings yet
- 1700 MCQ Revised VersionDocument485 pages1700 MCQ Revised VersionLu YaNo ratings yet
- Lemus Rangel 2010Document2 pagesLemus Rangel 2010audiNo ratings yet
- Acute Pericarditis PDFDocument14 pagesAcute Pericarditis PDFMila CcasaniNo ratings yet
- 16 Vascular Diseases of Nervous System-QDocument24 pages16 Vascular Diseases of Nervous System-QAdi PomeranzNo ratings yet
- Form 3 Chapter 2Document9 pagesForm 3 Chapter 2Mariana AhmadNo ratings yet
- What Is A Brain AVM?: Symptoms and Bleeding Diagnosis and TreatmentDocument5 pagesWhat Is A Brain AVM?: Symptoms and Bleeding Diagnosis and Treatmentrita mulyanaNo ratings yet
- Santi-Total Thesis Title - Upto June 2017Document37 pagesSanti-Total Thesis Title - Upto June 2017SRIKANTA MAJINo ratings yet
- St. Paul University PhilippinesDocument4 pagesSt. Paul University PhilippinesAshley DayagNo ratings yet
- Special Circumstances GuidelinesDocument19 pagesSpecial Circumstances GuidelinesRayNo ratings yet
- CA CardiovascularDocument10 pagesCA CardiovascularNina OaipNo ratings yet
- Congestive Heart FailureDocument74 pagesCongestive Heart FailureNiharikaNo ratings yet
- Cardiac Arrest VF/Pulseless VT Learning Station ChecklistDocument5 pagesCardiac Arrest VF/Pulseless VT Learning Station ChecklistMaryam FadahNo ratings yet
- APK Cardiology - Pulmonology (Without Answers)Document14 pagesAPK Cardiology - Pulmonology (Without Answers)sereNo ratings yet
- Maximal Pre-Excitation Based Algorithm For Localization of Manifest Accessory Pathways in AdultsDocument10 pagesMaximal Pre-Excitation Based Algorithm For Localization of Manifest Accessory Pathways in AdultsFredy TandriNo ratings yet
- Eyal Herzog (Editor) - Pulmonary Embolism-Springer (2021)Document288 pagesEyal Herzog (Editor) - Pulmonary Embolism-Springer (2021)Frederico PóvoaNo ratings yet
- CPR 2Document3 pagesCPR 2Baebee Lou100% (1)
- DiltiazemDocument4 pagesDiltiazemRichard MoralesNo ratings yet
- 3 Nursing Care PlanDocument6 pages3 Nursing Care PlanJeyser T. GamutiaNo ratings yet
- Angina PectorisDocument3 pagesAngina PectorisKhalid Mahmud Arifin100% (2)
- CNV Codman EnterpriseDocument8 pagesCNV Codman EnterpriseneureportNo ratings yet