Professional Documents
Culture Documents
koay hui fern γδ t cells unveil invisible tumors
koay hui fern γδ t cells unveil invisible tumors
Uploaded by
Singh AditiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
koay hui fern γδ t cells unveil invisible tumors
koay hui fern γδ t cells unveil invisible tumors
Uploaded by
Singh AditiCopyright:
Available Formats
TREIMM 1992 No.
of Pages 3
Trends in
Immunology
Spotlight
γδ T cells unveil invisible are rare. Vδ1 cells are often enriched in
solid tumors, where they retain a cytotoxic
PD1, while no other lymphocyte popula-
tions differed between 2MWT and 2MMUT
tumors phenotype and are associated with a posi- cancers (Figure 1). Focusing on MMRd
1 2, tive prognosis [3]. It is largely unknown CRC, they found that these γδ T cells were
Hui-Fern Koay and Lydia Lynch * whether well-characterized inhibitory im- also enriched in the expression of NKRs. Im-
mune checkpoint molecules, including pro- portantly, although these intratumoral Vδ1/
Tumors can evade conventional grammed cell death protein 1 (PD1) and Vδ3 T cells were PD1+, they expressed cyto-
T cell recognition by rendering the CTLA4, which are essential for restraining toxicity markers, produced IFNγ, and could
HLA class I antigen presentation antitumor CD8+ αβ T cell function, are efficiently kill 2MMUT tumors in vitro. These
system defective. In a recent study, also relevant to, and/or expressed by, findings are in line with another recent
de Vries et al. reveal γδ T cells as intratumoral γδ T cells. study by the Hayday and Swanton laborato-
key contributors to the efficacy of ries showing that responses to ICB were
Immunogenic tumors that are well infiltrated associated with enriched Vδ1 transcripts in
immune checkpoint blockade (ICB)
with lymphocytes, especially T cells, are as- nonsmall cell lung cancer [9].
against HLA-I-silenced cancers,
sociated with improved prognosis. In turn,
highlighting a novel layer of sur-
immunotherapies targeting T cells are par- The study by de Vries et al. represents a new
veillance against immune escape ticularly effective in patients with mismatch level of understanding of the full potential of
by tumors. repair-deficient (MMRd) cancers, which both ICB and γδ T cells as anticancer agents
are rich in putative neoantigens recognized [8]. It raises many fundamental questions,
γδ T cells are evolutionary conserved by CD8+ T cells via HLA-I [4]. These tumor- and perhaps the overarching one revolves
T cells that straddle innate and adaptive infiltrating CD8+ T cells are often rendered around what γδ T cells see, and react to, in
immunity and have strong antitumor po- exhausted in the harsh tumor microenvi- MMRd 2MMUT tumors. Do they need their
tential. Intratumoral γδ T cell gene signa- ronment (TME), classically characterized T cell receptor (TCR) to recognize tumors,
tures have been shown to be a favorable by high expression of inhibitory check- and are neoantigen(s) involved? What we
prognostic indicator across many inde- point molecules [5]. ICB targeting PD1/ can conclude is that Vδ1/Vδ3 T cells are
pendent studies of solid tumors, including programmed death-ligand 1 and/or CTLA4 not engaging HLA-I, or the MHC-I-like mole-
colorectal cancer (CRC) [1,2]. γδ T cells blocks these inhibitory exhaustion path- cules CD1d or MR1 on tumors, given that
exert antitumor functions through degranu- ways, unleashing tumor-specific T cell re- the expression of these antigen-presenting
lation of cytotoxic factors, secretion of proin- sponses. However, MMRd cancers often molecules requires 2M. The authors pro-
flammatory cytokines, and transactivation lose HLA-I expression due to silencing posed that PD1+ Vδ1 T cells recognize tu-
of other antitumor immune cells. Unlike or mutating 2M (2MMUT) [6]. Despite this, mors by activating NKG2D or other NKRs
αβ T cells, γδ T cells are not restricted to 2MMUT tumors retain responsiveness to and their stress ligands on tumor cells. In-
HLA–peptide antigen complexes, and they ICB therapy [7]. This suggests that CD8+ deed, PD1+ Vδ1 cells kill tumors expressing
express natural killer/cytotoxicity receptors T cells are not the sole effectors in this con- NKG2D ligands MIC-A/B most effectively
(NKRs) that recognize stress antigens text and that other immune cells are able to [8]. Blockade of NKG2D reduced their ability
upregulated by many tumor types. Thus, recognize these tumors, which are ‘invisible’ to react against most, but not all tumors and
γδ T cells are rapidly gaining attention for to CD8 T cells. did not completely prevent killing of the tu-
their potential as excellent ‘universal donors’ mors. This itself raises further questions.
for adoptive cellular therapy in cancer, be- Building upon this, de Vries et al. [8] recently First, is PD1 a marker of exhaustion on
cause they would not elicit severe graft- reported that ICB worked more effec- intratumoral γδ T cells? If so, is the recogni-
versus-host disease and could recognize tively in patients with 2MMUT compared tion of stress ligands a strong enough signal
a wide variety of different tumor types, with ‘wild-type’ (2MWT) tumors (95% ver- to cause exhaustion on Vδ1/Vδ3 T cells? Of
eliminating the need for identifying tumor- sus 62% of patients, respectively, re- note, PD1+ Vδ1 T cells were more effective
specific (neo)antigens in advance [3]. In ceived clinical benefit) [8]. This led the killers than their PD1– counterparts, sug-
humans, there are three major γδ T cell sub- authors to investigate which immune gesting that PD1 + Vδ1 cells were not
sets denoted by T cell receptor usage and cells could infiltrate 2MMUT tumors. exhausted, but were instead activated
tissue tropism. In brief, Vδ2 cells are the Leveraging the Cancer Genome Atlas, or licensed to kill. However, their activity
most abundant subset found in peripheral they showed that several MMRd was associated with clinical benefit during
blood, while Vδ1 cells are more tissue resi- tumors with 2M mutations were enriched ICB, counter-intuitively indicating that
dent, as are Vδ3 cells, although the latter for Vδ1 and Vδ3 γδ T cells that expressed blocking PD1 on γδ T cells provided
Trends in Immunology, Month 2023, Vol. xx, No. xx 1
Trends in Immunology
B2MWT B2MMUT
?
Cancer cell
PD-1 ligands?
? Cancer
Cancer cell
Tumor PD1
cell associated VG1
neoantigens?
CD8+ αβT
TCR HLA-I
HLA-I PD1
?
? Tumor
associated NKR
neoantigens?
CD8+ αβT CD4 + ? VG1 CTLA4
αβT
VG1 γ γGG T
γGG T VG3 γ D + αβT
CD4
VG3
D + αβT
CD4
Trends in Immunology
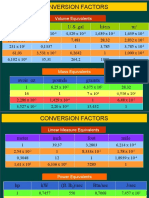
Figure 1. Proposed scenarios incorporating new clues on T cell recognition of HLA-I-presenting versus HLA-I-silenced tumors. B2M inactivation
(B2MMUT) occurs frequently in DNA mismatch repair-deficient (MMRd) colorectal cancers (CRCs), but it is unclear how B2MMUT tumors maintain reactivity to immune
checkpoint blockade (ICB). Vδ1 and Vδ3 γδ T cells infiltrate, and are activated in, B2MMUT MMRd CRC compared with their HLA-I-sufficient (B2MWT) counterparts.
These Vδ1 and Vδ3 γδT cells are PD1+ and respond to anti (α)-PD1 and α-CTLA4 antibody treatment, contributing to the efficacy of ICB therapy in B2MMUT MMRd
CRC [8]. Abbreviation: NKR, natural killer/cytotoxicity receptor.
enhanced function. Alternatively, perhaps Furthermore, is the TME as suppressive ‘off-the-shelf’ pan-cancer adoptive cellular
only PD1+ Vδ1 T cells recognize tumors for γδ T cells as it is for αβ T cells? Given immunotherapy, while, in turn, potentially
due to the co-expression of stress ligand that CD4+ αβ T cells can modulate ICB unveiling the identity of other tumor factors
receptors only on PD1+ cells, or even efficacy in MMRd 2M MUT CRC, under- that immune cells can see.
via PD1 ligands. Thus, how PD1 block- standing the weighted contribution and/or
ade affects γδ T cells warrants further interplay of antitumor Vδ1/Vδ3 T cells Acknowledgments
investigation. relative to other immune cells within the The authors are supported by NIAID grant R01AI134861
TME is crucial because these may be col- (to L.L.) and by L’Oréal UNESCO award (to H-F.K.).
What then enables the infiltration and/or re- lectively required for optimal responses
activity of Vδ1/Vδ3 T cells toward MMRd [10] (Figure 1). Declaration of interests
2MMUT tumors, if not solely via NKG2D, or None declared by authors.
via HLA-I, CD1d, or MR1? Considering the Like many surprising and impactful studies,
1
Department of Microbiology and Immunology at the Peter
tissue tropism and observed enrichment of this one by de Vries et al. generates more Doherty Institute for Infection and Immunity, The University of
Vδ1/Vδ3 T cells within solid tumors, it is likely questions than answers, which warrants Melbourne, Melbourne, VIC, Australia
2
Department of Medicine, Brigham and Women’s Hospital,
that Vδ1/Vδ3 T cells were resident in normal follow-up because this may lead to new
Boston, Harvard Medical School, Boston, MA, USA
untransformed tissue. Many unidentified avenues for targeting γδ T cell biology
factors, from metabolites and nutrient avail- during ICB against solid tumors. It also *Correspondence:
llynch@bwh.harvard.edu (L. Lynch).
ability to tissue-associated molecules in the further spotlights a long-understudied and
https://doi.org/10.1016/j.it.2023.01.011
TME, may have then induced their infiltration perhaps underappreciated population of
and/or proliferation at the transformed site. T cells that offer striking potential as an © 2023 Elsevier Ltd. All rights reserved.
2 Trends in Immunology, Month 2023, Vol. xx, No. xx
Trends in Immunology
References 4. Le, D.T. et al. (2017) Mismatch repair deficiency predicts 8. de Vries, N.L. et al. (2023) γδ T cells are effectors of immu-
1. Meraviglia, S. et al. (2017) Distinctive features of tumor- response of solid tumors to PD-1 blockade. Science 357, notherapy in cancers with HLA class I defects. Nature 613,
infiltrating gammadelta T lymphocytes in human colorectal 409–413 743–750
cancer. Oncoimmunology 6, e1347742 5. Jiang, Y. et al. (2015) T-cell exhaustion in the tumor 9. Wu, Y. et al. (2022) A local human Vdelta1 T cell population
2. Gentles, A.J. et al. (2015) The prognostic landscape of microenvironment. Cell Death Dis. 6, e1792 is associated with survival in nonsmall-cell lung cancer.
genes and infiltrating immune cells across human cancers. 6. Grasso, C.S. et al. (2018) Genetic mechanisms of immune Nat. Cancer 3, 696–709
Nat. Med. 21, 938–945 evasion in colorectal cancer. Cancer Discov. 8, 730–749 10. Germano, G. et al. (2021) CD4 T cell-dependent rejection of
3. Mensurado, S. et al. (2023) The emerging roles of gammadelta 7. Middha, S. et al. Majority of B2M-mutant and -deficient beta-2 microglobulin null mismatch repair-deficient tumors.
T cells in cancer immunotherapy. Nat. Rev. Clin. Oncol. colorectal carcinomas achieve clinical benefit from immune Cancer Discov. 11, 1844–1859
Published online January 9, 2023. https://doi.org/10.1038/ checkpoint inhibitor therapy and are microsatellite
s41571-022-00722-1 instability-high. JCO Precis. Oncol. 3, PO.18.00321
Trends in Immunology, Month 2023, Vol. xx, No. xx 3
You might also like
- Midpoints - Unleashing The POwer of The PlanetsDocument394 pagesMidpoints - Unleashing The POwer of The PlanetsAngela Gibson98% (104)
- Check List (Pre Entry) For Portable Grinding MachineDocument4 pagesCheck List (Pre Entry) For Portable Grinding MachineSufianul AtbarNo ratings yet
- 44 pdl1Document3 pages44 pdl1bawoji1763No ratings yet
- Fimmu 13 816005Document14 pagesFimmu 13 816005emmanuel AndemNo ratings yet
- IMP MDSCs Tregs y NKs BelloDocument11 pagesIMP MDSCs Tregs y NKs BelloLyanna StarkNo ratings yet
- Impact of Immunotherapy On CD4 T Cell Phenotypes ADocument21 pagesImpact of Immunotherapy On CD4 T Cell Phenotypes APatricia GomesNo ratings yet
- Inmunobiologia CA RenalDocument7 pagesInmunobiologia CA RenalDelia Lucia Escola GomezNo ratings yet
- γδ T Cells as Immuno-Oncology Treatments in the Era of Precision MedicineHarnessing the potential of the immune system to treat cancers has been the goal of many scientific investigations in the last few decades. Recent advances in cancer biology and immunology have allowed for cancer immunotherapy to become a reality. The premise of cancer immunotherapy is to stimulate the patient’s own immune system to attack and reject the malignant cells, sparing normal surrounding tissues.Document6 pagesγδ T Cells as Immuno-Oncology Treatments in the Era of Precision MedicineHarnessing the potential of the immune system to treat cancers has been the goal of many scientific investigations in the last few decades. Recent advances in cancer biology and immunology have allowed for cancer immunotherapy to become a reality. The premise of cancer immunotherapy is to stimulate the patient’s own immune system to attack and reject the malignant cells, sparing normal surrounding tissues.Bruce LennyNo ratings yet
- ImmunoDocument2 pagesImmunodiceNo ratings yet
- Antigen Presentation in Cancer - Insights Into Tumor Immunogenicity and Immune EvasionDocument15 pagesAntigen Presentation in Cancer - Insights Into Tumor Immunogenicity and Immune EvasionElton De SáNo ratings yet
- Reuwer Et AlDocument8 pagesReuwer Et AlCemal GürselNo ratings yet
- 30.defined Tumor Antigen-Specific T Cells Potentiate Personalized TCR-T Cell Therapy and Prediction of Immunotherapy ResponseDocument13 pages30.defined Tumor Antigen-Specific T Cells Potentiate Personalized TCR-T Cell Therapy and Prediction of Immunotherapy Responsezhe zhNo ratings yet
- Chimeric Antigen Receptor Engineered Human Gamma DDocument12 pagesChimeric Antigen Receptor Engineered Human Gamma Dedwin tjandraNo ratings yet
- Avances en Nuevas Estrategias de Vacunas para La Inmunoterapia y Prevención Del Cáncer JAY A. BERZOFSKY 2004Document11 pagesAvances en Nuevas Estrategias de Vacunas para La Inmunoterapia y Prevención Del Cáncer JAY A. BERZOFSKY 2004Ramiro J. Rodriguez GarciaNo ratings yet
- NEJMe 2400203Document2 pagesNEJMe 2400203sazzad suvroNo ratings yet
- A CD40 Agonist and PD-1 Antagonist Antibody Reprogram The Microenvironment of Nonimmunogenic Tumors To Allow T-cell-Mediated Anticancer ActivityDocument16 pagesA CD40 Agonist and PD-1 Antagonist Antibody Reprogram The Microenvironment of Nonimmunogenic Tumors To Allow T-cell-Mediated Anticancer ActivitySoumya PoddarNo ratings yet
- 1a PDFDocument10 pages1a PDFAndrea Il MiodoNo ratings yet
- 2021 in Search of An Ideal CAR-T Cell Antigen TargetDocument8 pages2021 in Search of An Ideal CAR-T Cell Antigen TargetTMU d151109004No ratings yet
- Cell Proliferation - 2019 - Zhao - PD 1 PD L1 Blockade Rescue Exhausted CD8 T Cells in Gastrointestinal Stromal TumoursDocument10 pagesCell Proliferation - 2019 - Zhao - PD 1 PD L1 Blockade Rescue Exhausted CD8 T Cells in Gastrointestinal Stromal TumoursAnu ShaNo ratings yet
- Fonc 08 00086Document14 pagesFonc 08 00086Siska HarapanNo ratings yet
- Immune Checkpointtargeted Therapy Cancer and Autoimmune Diseases Represent Two Sides of The Same CoinDocument4 pagesImmune Checkpointtargeted Therapy Cancer and Autoimmune Diseases Represent Two Sides of The Same Coinpratiwi eka rahmawatiNo ratings yet
- 7 Cancer Immunotherapy Etc-2020Document32 pages7 Cancer Immunotherapy Etc-2020Syifa KhairunnisaNo ratings yet
- (14796821 - Endocrine-Related Cancer) Considerations For Cancer Immunotherapy Biomarker Research During COVID-19Document8 pages(14796821 - Endocrine-Related Cancer) Considerations For Cancer Immunotherapy Biomarker Research During COVID-19Betül SulubulutNo ratings yet
- A Game Changer in Cancer TreatmentDocument11 pagesA Game Changer in Cancer TreatmentŞeyma YılmazNo ratings yet
- IMPORTANTE MDSCs en El Nicho TumoralDocument10 pagesIMPORTANTE MDSCs en El Nicho TumoralLyanna StarkNo ratings yet
- Artigo ImunologiaDocument13 pagesArtigo ImunologiapaulamonteiromedNo ratings yet
- Pi Is 1535610821006103Document4 pagesPi Is 1535610821006103maulvi.labe12No ratings yet
- J Exp Med-2010-Xie-651-67Document21 pagesJ Exp Med-2010-Xie-651-67tahsaliNo ratings yet
- 18 JL 7Document15 pages18 JL 7Irma SihotangNo ratings yet
- 2 - Celulas T Gama DeltaDocument8 pages2 - Celulas T Gama DeltaDan RyuNo ratings yet
- Ijms 23 14412Document11 pagesIjms 23 14412Dhivya l.sNo ratings yet
- 2014 - MesenchymalDocument18 pages2014 - MesenchymalMiguel ÁngelNo ratings yet
- 1 s2.0 S0959804921002215 MainDocument10 pages1 s2.0 S0959804921002215 MainGUO YUNo ratings yet
- Nri 1936 ArtigoDocument13 pagesNri 1936 ArtigoGlauce L TrevisanNo ratings yet
- 2021-Review-Tumour Neoantigen Mimicry by Microbial Species in Cancer ImmunotherapyDocument11 pages2021-Review-Tumour Neoantigen Mimicry by Microbial Species in Cancer ImmunotherapyCristian Felipe Sandoval QuiñonezNo ratings yet
- 2020 - Tun - HL ImmunotherapyDocument10 pages2020 - Tun - HL ImmunotherapyMiguel ÁngelNo ratings yet
- 1 s2.0 S2352304222002239 MainDocument33 pages1 s2.0 S2352304222002239 MainAnu ShaNo ratings yet
- Ecancermedicalscience 2014 Article 441Document15 pagesEcancermedicalscience 2014 Article 441YulianaNo ratings yet
- PHD Thesis Dendritic CellsDocument5 pagesPHD Thesis Dendritic Cellsashleyjonesmobile100% (1)
- 4728 FullDocument15 pages4728 FullMounikaGoruganthuNo ratings yet
- Nej Mo A 2308917Document14 pagesNej Mo A 2308917mnf6bb2tckNo ratings yet
- The Article On MicrobalsDocument29 pagesThe Article On Microbalsrangesh aravindNo ratings yet
- Jones PA Et Al. 2019 Epigetnic Therapy in Immune-OncologyDocument11 pagesJones PA Et Al. 2019 Epigetnic Therapy in Immune-OncologyJasmyn KimNo ratings yet
- 10 1016@j Thorsurg 2020 01 006Document8 pages10 1016@j Thorsurg 2020 01 006entannabilakasdyNo ratings yet
- Immune Response and Immunotherapy in Chronic Lymphocytic LeukemiaDocument25 pagesImmune Response and Immunotherapy in Chronic Lymphocytic Leukemiakj185No ratings yet
- T Cells With A Single Tumor Antigen Specific T Cell Receptor Can Be Generated in Vitro From Clinically Relevant Stem Cell SourcesDocument13 pagesT Cells With A Single Tumor Antigen Specific T Cell Receptor Can Be Generated in Vitro From Clinically Relevant Stem Cell SourcesGraha NaturNo ratings yet
- 1 s2.0 S221138352100099X MainDocument14 pages1 s2.0 S221138352100099X Mainsara.madkour99No ratings yet
- Car-T Cells TherapyDocument7 pagesCar-T Cells TherapydrbrevathiNo ratings yet
- Paper 4 - Developement of A Bispecific Antibody Targeting PD-L1 and TIGIT With Optimal CytotocityDocument11 pagesPaper 4 - Developement of A Bispecific Antibody Targeting PD-L1 and TIGIT With Optimal CytotocityChauPhuongNo ratings yet
- Virus-Specific Memory T Cells Populate Tumors and Can Be Repurposed For Tumor ImmunotherapyDocument9 pagesVirus-Specific Memory T Cells Populate Tumors and Can Be Repurposed For Tumor ImmunotherapyNaima LeeNo ratings yet
- Paper 1 - PD1 Blockade Enhances ICAM1-Directed CAR T Therapeutic Efficacy in Advanced Thyroid CancerDocument14 pagesPaper 1 - PD1 Blockade Enhances ICAM1-Directed CAR T Therapeutic Efficacy in Advanced Thyroid CancerChauPhuongNo ratings yet
- Cancers: Dendritic Cell-Based and Other Vaccination Strategies For Pediatric CancerDocument19 pagesCancers: Dendritic Cell-Based and Other Vaccination Strategies For Pediatric CancerFrendy Ahmad AfandiNo ratings yet
- CD40-STING-PDL1 BlockDocument15 pagesCD40-STING-PDL1 Blockmpl12345678No ratings yet
- Targeting Neoantigens For Cancer Immunotherapy: Yong-Chen Lu and Paul F. RobbinsDocument6 pagesTargeting Neoantigens For Cancer Immunotherapy: Yong-Chen Lu and Paul F. RobbinsRoni ArmandaNo ratings yet
- HHS Public Access: Cell-Intrinsic Barriers of T Cell-Based ImmunotherapyDocument24 pagesHHS Public Access: Cell-Intrinsic Barriers of T Cell-Based Immunotherapyro111111No ratings yet
- Car-T Cell Receptors (7758)Document8 pagesCar-T Cell Receptors (7758)Saradha PellatiNo ratings yet
- CD19-targeted Chimeric Antigen Receptor T-Cell Therapy For ALLDocument8 pagesCD19-targeted Chimeric Antigen Receptor T-Cell Therapy For ALLella.mbtNo ratings yet
- 1 s2.0 S0304383522000052 MainDocument12 pages1 s2.0 S0304383522000052 MainJavi MontañoNo ratings yet
- 7 Tumor ImmunityDocument51 pages7 Tumor ImmunityNanda SalmasNo ratings yet
- Regulatory T Cells - A Potential Target in Cancer ImmunotherapyDocument12 pagesRegulatory T Cells - A Potential Target in Cancer Immunotherapymedp7060No ratings yet
- T Cells in Health and DiseaseDocument50 pagesT Cells in Health and Diseaseygilad9139No ratings yet
- Fast Facts: CAR T-Cell Therapy: Insight into current and future applicationsFrom EverandFast Facts: CAR T-Cell Therapy: Insight into current and future applicationsNo ratings yet
- Bradley Clara Mathematical Responses To The HoleDocument10 pagesBradley Clara Mathematical Responses To The HoleSingh AditiNo ratings yet
- Managing Floods-01Document15 pagesManaging Floods-01Singh AditiNo ratings yet
- Rain Fury & Roads-01Document14 pagesRain Fury & Roads-01Singh AditiNo ratings yet
- Katti Et Al-2022-Nature Reviews CancerDocument21 pagesKatti Et Al-2022-Nature Reviews CancerSingh AditiNo ratings yet
- LECTURE 1. PUMPS and FANS.Document21 pagesLECTURE 1. PUMPS and FANS.RocsNo ratings yet
- CLS Aipmt-19-20 XIII Che Study-Package-3 Level-1 Chapter-15 PDFDocument40 pagesCLS Aipmt-19-20 XIII Che Study-Package-3 Level-1 Chapter-15 PDFThavasimariselvam N100% (1)
- Borrowing Costs PDFDocument9 pagesBorrowing Costs PDFanjcabsNo ratings yet
- GRSS - FINAL LIST - 1 June 2011 - 2Document26 pagesGRSS - FINAL LIST - 1 June 2011 - 2Robel TadesseNo ratings yet
- Poultry Anatomy and PhysiologyDocument40 pagesPoultry Anatomy and PhysiologyMamtaNo ratings yet
- Craftsman Snowblower ManualDocument64 pagesCraftsman Snowblower ManualKevinNo ratings yet
- Introduction To Histology: Preparation of Tissue For Histology Dr. OkoloDocument38 pagesIntroduction To Histology: Preparation of Tissue For Histology Dr. OkoloAbiola NerdNo ratings yet
- Gestational Trophoblastic DiseaseDocument4 pagesGestational Trophoblastic DiseasePrincess PlateroNo ratings yet
- Uasa Year 1Document10 pagesUasa Year 1vatsalkrishnasamyNo ratings yet
- Spec Sheet Scania R730la4x2mnaDocument4 pagesSpec Sheet Scania R730la4x2mnaRoman PopulikNo ratings yet
- Object-Oriented Programming, C++ and Power System SimulationDocument10 pagesObject-Oriented Programming, C++ and Power System SimulationjasonkinNo ratings yet
- Conversion Factors: in FT U.S. Gal Liters MDocument8 pagesConversion Factors: in FT U.S. Gal Liters MSamuel MahendraNo ratings yet
- BSC 116 SyllabusDocument8 pagesBSC 116 SyllabussahanchemNo ratings yet
- ComputerDocument104 pagesComputerPhadadosty Owusu KwadwoNo ratings yet
- Garden Staff Position Description 2015Document1 pageGarden Staff Position Description 2015congressheightsontheriseNo ratings yet
- The 10 Biggest Business Trends For 2021 Everyone Must Be Ready ForDocument1 pageThe 10 Biggest Business Trends For 2021 Everyone Must Be Ready ForJUAN SEBASTIAN ARTEAGA MUÑOZNo ratings yet
- Wastewater Treatment: D. Jim Livingston Asst. Prof. of ChemistryDocument22 pagesWastewater Treatment: D. Jim Livingston Asst. Prof. of ChemistryJim LivingstonNo ratings yet
- Introduction To FEX and Cisco Nexus CommandsDocument29 pagesIntroduction To FEX and Cisco Nexus CommandsNagarajanNo ratings yet
- REPORTDocument6 pagesREPORTrachana singhNo ratings yet
- Development of A Topical Gel Containing A Dipeptidyl Peptidase-4 Inhibitor For Wound Healing ApplicationsDocument15 pagesDevelopment of A Topical Gel Containing A Dipeptidyl Peptidase-4 Inhibitor For Wound Healing ApplicationsGlobal Research and Development ServicesNo ratings yet
- Drilling Intersects Significant Coal Seams at TCM Coal Project, Kalimantan, Indonesia HighlightsDocument6 pagesDrilling Intersects Significant Coal Seams at TCM Coal Project, Kalimantan, Indonesia HighlightsgancanNo ratings yet
- Preliminary Observations On The Effects of Milk Fortification and Heating On Microstructure and Physical Properties of Stirred YogurtDocument10 pagesPreliminary Observations On The Effects of Milk Fortification and Heating On Microstructure and Physical Properties of Stirred Yogurt伊利亚斯尼亚佐夫No ratings yet
- CHALLENGES IN IMPLEMENTING A NEW SIGNALLING SYSTEM TO REPLACE AN EXISTING SIGNALLING SYSTEM WHILE MAINTAINING NORMAL TRAIN SERVICE-good ReferenceDocument47 pagesCHALLENGES IN IMPLEMENTING A NEW SIGNALLING SYSTEM TO REPLACE AN EXISTING SIGNALLING SYSTEM WHILE MAINTAINING NORMAL TRAIN SERVICE-good ReferencePulin ChaudhariNo ratings yet
- Si47 1971 Frenic Lift Loader Im WebDocument128 pagesSi47 1971 Frenic Lift Loader Im WebLogic EngineeringNo ratings yet
- Fartlek - WikipediaDocument7 pagesFartlek - Wikipediamohan raoNo ratings yet
- Msds Hydrogen PeroxideDocument2 pagesMsds Hydrogen PeroxideSlamet Ar100% (1)
- HP 100 Series Rack v142: Key Features and BenefitsDocument2 pagesHP 100 Series Rack v142: Key Features and Benefitsevangelista7940No ratings yet
- Fs p611 Sparkplug Ijb-222027-EnDocument2 pagesFs p611 Sparkplug Ijb-222027-EnwaltsdavinNo ratings yet