Professional Documents
Culture Documents
Implant Ology
Implant Ology
Uploaded by
Alireza MehryarCopyright:
Available Formats
You might also like
- Questions and Correct Answer Keys: MSCAA Practice Paper 2 November 2018Document36 pagesQuestions and Correct Answer Keys: MSCAA Practice Paper 2 November 2018Neelak100% (4)
- Cairo: Pilbeam's Mechanical Ventilation, 6th EditionDocument6 pagesCairo: Pilbeam's Mechanical Ventilation, 6th Editionفاتن المطيريNo ratings yet
- Test - Mark Klimek Yellow Book (KV) - QuizletDocument62 pagesTest - Mark Klimek Yellow Book (KV) - QuizletRonelyn Rachelle CabcabanNo ratings yet
- 11.dental Implants FNLDocument204 pages11.dental Implants FNLvsdeeps100% (3)
- Theme 7 - Partial Removable Skeletized Denture: Mandibular VarietiesDocument2 pagesTheme 7 - Partial Removable Skeletized Denture: Mandibular VarietiesShany SchwarzwaldNo ratings yet
- Septeper 2015 Recall 200 Sba Mrcog Part 1Document49 pagesSepteper 2015 Recall 200 Sba Mrcog Part 1VINOD GUPTA100% (2)
- Implant 2Document34 pagesImplant 2allakami777yousefNo ratings yet
- Dental Implants: by DR - Mahmoud Ahmed Elfarmawy Lecture of OMFS Faculty of Dentistry, SU, KantaraDocument34 pagesDental Implants: by DR - Mahmoud Ahmed Elfarmawy Lecture of OMFS Faculty of Dentistry, SU, KantaraMohammed TarekNo ratings yet
- ImplantDocument86 pagesImplantelle70503No ratings yet
- Imp 521Document149 pagesImp 521Mohamed KilaniNo ratings yet
- Dental ImplantsDocument49 pagesDental Implantsaay18bdsNo ratings yet
- Dental ImplantsDocument70 pagesDental ImplantsDENTALORG.COM100% (5)
- Module 7 2011 Tanima MannanDocument18 pagesModule 7 2011 Tanima MannandrarlenaphilipleeNo ratings yet
- O.surgery Lec11Document22 pagesO.surgery Lec11MohammedNo ratings yet
- 06 Success and Failure of ImplantsDocument28 pages06 Success and Failure of Implantsprostho booksNo ratings yet
- Risks and Complications of Orthodontic MiniscrewsDocument51 pagesRisks and Complications of Orthodontic MiniscrewsutokaNo ratings yet
- Caitlin Doede - Periodontology Study NotesDocument14 pagesCaitlin Doede - Periodontology Study Notesapi-347345383No ratings yet
- Dental Implant: Presented byDocument43 pagesDental Implant: Presented byade ismailNo ratings yet
- Micro Implant Anchorage in Orthodontics / Orthodontic Courses by Indian Dental AcademyDocument39 pagesMicro Implant Anchorage in Orthodontics / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Post Graduate Student: Dr. RahultiwariDocument158 pagesPost Graduate Student: Dr. RahultiwariVivek Sunil EdayathNo ratings yet
- 0verview of Dental ImplantologyDocument70 pages0verview of Dental ImplantologysabbyNo ratings yet
- ImpiantiDocument23 pagesImpiantisabbyNo ratings yet
- Screenshot 2022-12-22 at 6.21.43 PMDocument80 pagesScreenshot 2022-12-22 at 6.21.43 PMdr.teethdentalclinic2019No ratings yet
- Immediate Dental Implants and Bone Graft: Khalid S. Hassan and Adel S. AlaglDocument11 pagesImmediate Dental Implants and Bone Graft: Khalid S. Hassan and Adel S. AlaglAndria FadliNo ratings yet
- Temporary Anchorage Devices in Orthodont 970c9d2aDocument11 pagesTemporary Anchorage Devices in Orthodont 970c9d2aThang Nguyen TienNo ratings yet
- Indications For Dental ExtractionsDocument27 pagesIndications For Dental ExtractionsmidhunNo ratings yet
- TadsDocument27 pagesTadsshilpaNo ratings yet
- Bio-Materials in Implants: BY, DR - Siddarth SasDocument33 pagesBio-Materials in Implants: BY, DR - Siddarth SasNagappan Chockalingam100% (1)
- ImplantologyDocument212 pagesImplantologyGabriela Cocieru Motelica100% (1)
- DR Ghazy 2013 Implant Lectures For 4th Year StudentsDocument25 pagesDR Ghazy 2013 Implant Lectures For 4th Year StudentsMohamed Hamed GhazyNo ratings yet
- Dental Implantology: ImplantationDocument22 pagesDental Implantology: Implantationehab qasimNo ratings yet
- Review of Dental ImplantDocument10 pagesReview of Dental Implantmar100% (1)
- Dental ImplantsDocument34 pagesDental ImplantsMurielNo ratings yet
- NBDE Dental Boards Oral SurgeryDocument30 pagesNBDE Dental Boards Oral SurgeryJoyce Lim100% (1)
- The Future of ProsthodonticsDocument22 pagesThe Future of ProsthodonticsGoutham SunilNo ratings yet
- Lec1 - Bridge (Fixed Partial DentureDocument9 pagesLec1 - Bridge (Fixed Partial Dentureكاظم عبد الحسينNo ratings yet
- Temporary Anchorage Device (TAD's)Document121 pagesTemporary Anchorage Device (TAD's)Chandra Sekhar Reddy100% (3)
- Short ImplantsFrom EverandShort ImplantsBoyd J. TomasettiNo ratings yet
- IMPLANTOLOGY. Lec 4Document57 pagesIMPLANTOLOGY. Lec 4Moataz BellahNo ratings yet
- Oral ImplantologyDocument19 pagesOral ImplantologyKariim AhmadNo ratings yet
- Precision Attachments (2) PRDocument23 pagesPrecision Attachments (2) PRpriyaNo ratings yet
- Introduction To Dental Implantology: Dr. Nigam Sattar KhanDocument49 pagesIntroduction To Dental Implantology: Dr. Nigam Sattar KhanNigam SattarNo ratings yet
- SplintingDocument94 pagesSplintingsanthoshi_rani2006100% (3)
- IMPLANTOLOGI Compressed Compressed (1) - MinDocument122 pagesIMPLANTOLOGI Compressed Compressed (1) - MinNayafilahNo ratings yet
- (Dental Material) - Dental Implants (Lec18)Document6 pages(Dental Material) - Dental Implants (Lec18)DTM FHKNo ratings yet
- Dental Implants: Dr. D.M. Ajayi. August, 2017Document129 pagesDental Implants: Dr. D.M. Ajayi. August, 2017Kassim OboghenaNo ratings yet
- Biomaterials For Dental Implants Current and Future TrendsDocument34 pagesBiomaterials For Dental Implants Current and Future TrendsDeivyson Augusto100% (1)
- Surgical AP in Implant 21.07.09Document218 pagesSurgical AP in Implant 21.07.09Chokthanyawat100% (3)
- JHealthSpec1290-8553491 234534Document7 pagesJHealthSpec1290-8553491 234534Gabriela ZuritaNo ratings yet
- Orthodontics in 3 Millennia. Chapter 15: Skeletal Anchorage: Special ArticleDocument4 pagesOrthodontics in 3 Millennia. Chapter 15: Skeletal Anchorage: Special ArticleHARITHA H.PNo ratings yet
- Implant Guidelines For The Restorative DentistDocument165 pagesImplant Guidelines For The Restorative DentistRajab Lil'ronaldo67% (3)
- DENTAL ImplantDocument9 pagesDENTAL ImplantMohammed HassanNo ratings yet
- Implant Systems: Dr. Unjum Bashir, Dr. Manas Gupta, Dr. Ravish AhujaDocument7 pagesImplant Systems: Dr. Unjum Bashir, Dr. Manas Gupta, Dr. Ravish AhujaDr FarhatNo ratings yet
- Surgical Protocol: For Tidal Spiral Implant Systems TsiDocument13 pagesSurgical Protocol: For Tidal Spiral Implant Systems TsiRavi KumarNo ratings yet
- M Stimmelmayr, 2011Document6 pagesM Stimmelmayr, 2011aliserraristolNo ratings yet
- Implantology in Dental TechnologyDocument30 pagesImplantology in Dental TechnologyRufai HarunaNo ratings yet
- Jpis 51 100Document14 pagesJpis 51 100Veronica NatalieNo ratings yet
- Interlocking Nailining Minimally Invasive OsteosynthesisDocument28 pagesInterlocking Nailining Minimally Invasive Osteosynthesistvm1018No ratings yet
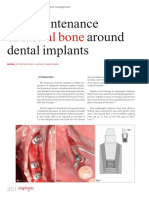
- Crestal Bone: The Maintenance of Around Dental ImplantsDocument5 pagesCrestal Bone: The Maintenance of Around Dental ImplantsJing XueNo ratings yet
- Role of Mini-Implants in OrthodonticsDocument9 pagesRole of Mini-Implants in OrthodonticsRonald WilfredNo ratings yet
- GTC 1 - Introduction To Fixed Prosthodontics (PPSG Lectures)Document52 pagesGTC 1 - Introduction To Fixed Prosthodontics (PPSG Lectures)rositadewiNo ratings yet
- ImplantDocument9 pagesImplantKhaled Abo ZaidNo ratings yet
- Tads - KomalDocument100 pagesTads - KomalRohini TondaNo ratings yet
- State of The Art: Fiona C. Goldizen,, Peter D. Sly,, and Luke D. KnibbsDocument15 pagesState of The Art: Fiona C. Goldizen,, Peter D. Sly,, and Luke D. KnibbsKarina Aguirre AlvarezNo ratings yet
- Welcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinDocument16 pagesWelcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinUmair MazharNo ratings yet
- India Immunization Chart 2010Document1 pageIndia Immunization Chart 2010Sarath Nageshwaran SujathaNo ratings yet
- Case Study ChoreaDocument18 pagesCase Study ChoreaKinjalNo ratings yet
- Antiplasmodial and Toxicological Properties of Cnidoscolus AconitifoliusDocument14 pagesAntiplasmodial and Toxicological Properties of Cnidoscolus AconitifoliusRuthNo ratings yet
- Induced Abortion and Risks That May Impact AdolescentsDocument29 pagesInduced Abortion and Risks That May Impact AdolescentsMichael RezaNo ratings yet
- Survival of Pediatric Patients After CPRDocument11 pagesSurvival of Pediatric Patients After CPRMaria Regina CamargoNo ratings yet
- 840 B2 Fire Rated Pu FoamDocument10 pages840 B2 Fire Rated Pu FoamJonathan Alexis Abarzua TorresNo ratings yet
- hs486 Document OSHA Recording Work-Related Injuries and IllnessesDocument13 pageshs486 Document OSHA Recording Work-Related Injuries and Illnessesfatmata koromaNo ratings yet
- SequiseZ 70000ON210156 2022 11 11Document19 pagesSequiseZ 70000ON210156 2022 11 11Vipul SinghNo ratings yet
- Icesu Updates Covid19 Confirmed Cases: Morbidity Week 13 January 1 - April 2, 2022Document15 pagesIcesu Updates Covid19 Confirmed Cases: Morbidity Week 13 January 1 - April 2, 2022Jeremae VentarNo ratings yet
- Ex - Cerebellar ExamDocument2 pagesEx - Cerebellar ExamssNo ratings yet
- Thyroid Gland An Diseases of Thyroid D Gland: Omc LectureDocument59 pagesThyroid Gland An Diseases of Thyroid D Gland: Omc LectureEdward MakemboNo ratings yet
- Essential Messages - 2023 CMDocument14 pagesEssential Messages - 2023 CMimran karimNo ratings yet
- Unani System of MedicineDocument18 pagesUnani System of MedicineManika RaiNo ratings yet
- Bab 7Document27 pagesBab 7bangarudaugtherNo ratings yet
- Abstract Book FinalDocument45 pagesAbstract Book Finalapi-200029530No ratings yet
- YökdilDocument195 pagesYökdilglisilsiklin antibiyotikNo ratings yet
- Risk Management PolicyDocument19 pagesRisk Management PolicySonukrishnaNo ratings yet
- Benda Asing Dalam Kornea Akibat Kurangnya Peralatan Keselamatan: Laporan KasusDocument6 pagesBenda Asing Dalam Kornea Akibat Kurangnya Peralatan Keselamatan: Laporan KasusRachmad SammuliaNo ratings yet
- Penn Yan CSD Reopening PlanDocument78 pagesPenn Yan CSD Reopening PlanNews 8 WROCNo ratings yet
- Body Fat & Hydration % Monitor Scale: EvaluationDocument8 pagesBody Fat & Hydration % Monitor Scale: EvaluationElkin MaldonadoNo ratings yet
- Vaccines Are Used To Chemically Neuter People, Drop Their IQ Points, Make Them Dumb, Dependant On Authority, Obediant SlavesDocument3 pagesVaccines Are Used To Chemically Neuter People, Drop Their IQ Points, Make Them Dumb, Dependant On Authority, Obediant Slavestesla2008No ratings yet
- What Is ECG?Document2 pagesWhat Is ECG?Lê Thanh HàNo ratings yet
- Home Economics and Food LiteracyDocument20 pagesHome Economics and Food LiteracyAllan Reuel DominicNo ratings yet
- Joy (Maternity Insurance Product) Prospectus Cum Sales LiteratureDocument23 pagesJoy (Maternity Insurance Product) Prospectus Cum Sales Literaturesanjay4u4allNo ratings yet
Implant Ology
Implant Ology
Uploaded by
Alireza MehryarOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Implant Ology
Implant Ology
Uploaded by
Alireza MehryarCopyright:
Available Formats
1.
Introduction, History of oral implantology
1-1. How can you summarize the possible success rate of modern implant treatments?
- 5 years success rate of oral implant is over 95% with mandible, 90% with maxilla
- response, healing ability, bone quality, smoking, diabetes etc.
- Long term success depends a lot on regular maintenance, oral hygiene, smoking, over loading etc.
1-2. What were the trends, and clinical trials with implants prior to the modern implantology?
Ancient times alloplastic material (gold, wood, animal teeth) in Egyptians, South Americans, Greeks
1st ~ 2nd century wrought iron implant
1647 (Duport) Teeth transplantation between patients
1756 (Hunter) first histological examination
1804 (Serre) Surgical preparation of tooth socket, warning about diseases transmission
1807 (Jourdan) First endosseal implant made from iron and later gold
19th century Alloplastic material (porcelain, platinum, silver, ivory, celluloid)
1891 (Znamesky) Implant made of caoutchouc (natural rubber) and porcelain
1-3. What was the first biocompatible alloy?
1929 (NewYork) Vitallium (Cr-Co-Mo 60% cobalt, 20% chromium, 5% molybdenum)
biocompatible, light weight, resistant to corrosion (used in dentistry and joint replacement)
1-4. What was the concept of sub-periosteal implants?
1943 (by Dahl) Sub-periosteal implant made using Vitallium
Make a flap, expose the bone
Apply the metal framework on the bone
Abutment project from this metal framework into the mouth
As muco-periosteal flap heals over the implant, they hold it securely in place
1-5. What were the causes of failure of sub-periosteal implants?
Framework must fit snugly (exact fit) over the bone, or implant will fail
rate of infection blood supply to the region
loading on the bone healing ability
No gingival seal Scar tissue formation
Exposed metal Operative stress
No quality control Few prosthetic options
-
Too little dense bone that can hold the implants
1-6. Who was the developer of the blade-cent implants?
1966 (Linkow) Titanium + endoosseal implant (pseudo-parodontium attachments)
1-7. -
Connective tissue around implant, that serves as a shock absorber
Fibro-osseointergration (PDL forming fibrotic attachments to the holes of the blade)
But this may cause implants to fail increased mobility
1-8. Who discovered, and published
1969 (Branemark) Titanium + screw type + direct implant bone attachment (osseointergration)
Requires - Bio-compatible material
- Atraumatic surgery
- Drilling in 47 degrees temp
- Precise adaptation of implant to bone
- Undisturbed, immobile healing phase
1-9. Since when do we reckon the modern implantology?
1969 (Branemark) modern implantology starts (Titanium + screw type + osseointergration)
1986 (Bosker) trans-mandibular implant
1952 first implants in Hungary sub-periosteal
1982 (Diakor) Bio-ceramic implants
1985 Screw type blade-vent implant
Today over 600 implant system available by 146 manufactures
1-10. What were the stages of the development of modern implantology?
Phase1 (1970-80) Pioneering, first clinical experience
Phase2 (1980-90) Systematic, fundamental researches. Planned clinical applications
Phase3 (1990-00) Clinical controls, randomized studies, extended clinical applications
Phase4 (2000+) Generally extended indications, GBR+bone grafting, increased demands, esthetic, functions.
Ed/Ju notes (eddieliuy@yahoo.com)
2. Classification of oral implants, according to the anatomic site. Endosteal implants
2-1. What is the meaning of an implant system
Specific implant + Surgical instruments + Prosthetic components
Different system to suite different implant system in different anatomical site and condition
Today, close to 600 system by at least 146 manufactures
Classified into Sub-periosteal(Ref:1-4), Intra-mucosal, trans-mandibular, trans-dental, endosteal
2-2. What is the intra-mucosal insert?
Non-reactive appliance that is fixed to the tissue-bone surface of a denture ( retention)
Consists of: 1. Base, 2. Cervix, 3. Head
Mushroom shaped titanium implants are embedded into the acrylic denture
Special burs create soft tissue receptor sites in the palatal tissue
Indication to retain a maxillary complete denture or RPD
2-3. What is the trans-mandibular implant?
Implant fixed to symphysial border and transverses the mandible to attach to mandible
Consists of: 1. Baseplate, 2. Cortical screw, 3. Posts, 4. Superstructure (attach to denture)
Inserted via extra-oral incision (submandibular)
Indication sever mandibular alveolar atrophy
osteoporosis, parafunction (bruxism), fracture
2-4. What is the trans-dental implant?
Endodontic implant, similar to a prosthodontics implant in many ways
With additional purpose stabilize & preservation of teeth (instead of replacing lost teeth)
Push rigid post through tooth, and deep into bone
- Cementing implant to the intra-dental part of canal wall
- Aim to move fulcrum of a loose tooth deeper into jaw ( support, mobility)
- Needle shaped, mono-crystalline/sapphire/aluminum oxide
Indication broken apex or root resorption
2-5. How can we classify the endosteal implants?
According to their anatomical location & form
Extension 2D blade vent
3D disk form
Rotation-symmetric/root form cylinder
needle
screws (single part, two part)
2-6. What is the main indication of blade-type implants?
Blade vent wedge shape body (<1mm thickness), narrow neck connects to abutment
contain holes to allow retention (depends on width, not depth of implant)
More resistance to lateral & occlusal forces (c.f. to endosseous implant)
Less bone needs to be regenerated
Blade can be shaped (to avoid anatomical landmarks)
No epithelial invagination
Underlying bone always exposed during insertion (easier to find position)
Enough bone must be present
Full house bridge needs 4 implants
Indication In porous area (maxillary tuberosity)
For single tooth replacement (not for RPD)
2-7. Why the blade-vent implants are not used generally today in the clinical practice?
Pseudo-periodontium attachment (increased mobility)
Poor biomechanics
Limited prosthesis options
Difficult to prepare (vent must be very straight)
Difficult to remove bone resorption
2-8. What are the advantages of rotation-symmetric/root-form implants?
Precise preparation of implant bed good primary stability
Easy placement & removal
Minimum tissue damage
Ed/Ju notes (eddieliuy@yahoo.com)
Increase surface area in contact with bone
2-9. What type of rotation-symmetric implants do you know?
Needle implants mono-crystalline aluminum oxide implants for trans-dental fixation
Cylindrical implants press fit, smooth wall
Screw implants 30~500% greater surface area (better primary stability even in soft bone)
Root form implants (tapered shape like a root requires adequate width/depth of bone)
- Threaded screw like, turned into bone
- Press fit smooth wall, tapped into bone
2-10. How can you classify the screw-type implants?
one piece trans-gingival healing, allow immediate loading
two piece subgingival healing, open flap surgery later to attach abutment
Ed/Ju notes (eddieliuy@yahoo.com)
3. Indications and contraindications of implant rehabilitations
3-1. Which are the major indications for implant placement?
Indication is the Lack of contraindication , or benefit greater than risk
Brinkman s (1976) topography indication
Class1 one missing tooth (due to extraction or accident)
Class2 uni-bilateral distal edentulous arch
Class3 too many missing teeth within arch (the bridge will be too long)
Class4 complete edentulous (mainly in mandible)Too many missing teeth in the arch
Following trauma or tumor resections
In case of difficult swallowing and parafunction (bruxism)
Allergic to acrylic base plates, hypersensitive mucosa (cannot tolerate mucosa support)
Disease such as asthma, gastritis, epilepsy
Professions such as actors, singers, speakers
3-2. Which teeth are the most often replaces with implants?
Maxilla 1st premolar > 2nd premolar > molars (4>5>678) most important for mastication
central incisor > lateral incisor > canine (1>2>3) most important for esthetics
Mandible 1st molar > canine, premolar most important for mastication
3-3. How can contraindications be classified?
General contraindication
o Diseases or medical therapy that hinders wound healing (DM, lesion of bone metabolism, immune
suppression, antidepressant, anticoagulant, cytostatic treatment)
o General surgical contraindication (degree and severity of other systemic diseases according to ASA)
o Pregnancy (altered hormone may cause gingivitis)
o Psychological instability (panic syndrome, depression, paranoia, may have unrealistic expectation)
o Physical and mental retardation
o Alcoholism, heavy smoker
o Atypical facial pain of unknown origin (hard to decide if post-operative facial pain is due to implant)
o Age under 14 (uncompleted jaw development)
o Age (healthy elderly adult 70+ both men/women, osseointergration just as good as young)
Local contraindication (Ref:3-7)
3-4. How does diabetes influence our implant activities?
Proven study that DM patient s bone-implant connection is less strong
Reduced wound healing
Decreased immunity, increased infection risk
Untreated DM implant fail rate can be as high as 20% /5y
Well treated DM fail rate is about 6~7% /5y
3-5. Which type of osteoporosis may be a contraindication of implant placement?
Bone metabolic diseases
- Osteomalacia ratio of organic and inorganic components shift towards organic (imperfect mineralization)
- Osteoporosis progressive reduce in bone density due to age/menopause increase fracture risk
- Primary in postmenopausal women, or presenile men (old age)
(18% women above 40, and 8% men involved)
- Secondary consequences of another disease
(Cushing s, DM, renal disease, alcoholism, malignant hematological diseases)
- Primary is more dangerous in implant that secondary
3-6. How does smoking, alcoholism and drug abuse influence osseointergration?
Heavy smoker (>20cig/day) - failure doubled in smokers
Healing of peri-implant soft tissue is more difficult & more marginal bone loss
increase risk of peri-implatitis as nicotine inhibits capillary circulation
Chronic alcoholism associated with coagulopathy, thrombocytopenia cause direct bone marrow toxicity
Drug abuse drug that reduce blood flow osteoblast activity, osseointergration, failure rate
3-7. What local contraindications many hinder implant placement?
Radiation therapy within 5 years in the planned region
- success rate of implant is only 26.5% in first 5 years
- recommend to delay implant for 5 years until blood supply regenerates, + exceptional oral hygiene
Pathological condition of the local bone and soft tissue
Ed/Ju notes (eddieliuy@yahoo.com)
- Osteomyelitis, osteo-radio-necrosis, large cysts, granuloma, fibrous dysplasia, bone tumors
- Retained root
- leukoplakia, erosive lichen
- movable fibrotic ridge, papilloma, papillomatosis, fibroma, fibromatosis
Dysfunction that will overload the implant (e.g. deep bite)
Dental anomalies that have to be treated before implant placement
- Caries, bad oral hygiene, periodontitis, orthodontic anomalies
3-8. What do you know about titanium metallosis and allergy?
Cannot be detected as a toxic substance, or as causing allergy
Ed/Ju notes (eddieliuy@yahoo.com)
4. Diagnosis and treatment planning
4-1~4-4. What is the description of bone quality class, and what are the locations for it on the jaw
Class Composition Occurrence BIC
D1 - solid compact bone - Interforaminal area of ~ 80%
(good for - less blood supply than D2 atrophic mandible
implant)
D2 - Compact, porous cortical bone - interformainal and lateral ~70%
(best for - Hard, roughly granular spongious bone area of mandible
implant) - frontal area of maxilla
D3 - Thin porous compact bone - frontal area of maxilla < 50%
- Thin trabecular spongious bone - posterior region of
mandible
D4 - Thin trabecular spongious bone - premolar and molar ~ 25%
region of maxilla
4-5. Why do we need panoramic x-rays and template with metal sphere?
OPG (orthopantomogram)
Anatomical borders clearly visible
vertical bone dimensions measurable
low radiation dose
fast easy processing
Distortion of real dimensions (require template and sphere for better approximation)
- different magnification in vertical and horizontal direction
- dim image in frontal area compare to edge
- summation of anatomical structure (e.g. vertebral colum)
Implant template
- Transparent film with 1:1.25 magnification image of different size implant
- compare with OPG to determine size to be used
Metal sphere
- Acrylic resin base plate with metal balls, use equation to calculate real size
4-6. What are the situations when computer tomography is recommended?
Measuring accurate real dimensions (2~3mm thick sections in many directions can be analyzed)
- distance to anatomical structure (IAN, maxillary sinus, mental nerve)
- determines the accurate depth of implant
Measuring bone density (Hounsfield units)
- D1 (1300~600HU) - D3 (250~100HU)
- D2 (500~200HU) - D4 (100~500HU)
Can use with a CT template
Use of CBCT - 1/10 radiation dose of conventional CT, head/neck region takes 20sec, cost 20,000HUF
- can also take correct 3D localization of anatomical structure (hard and soft tissue)
- determine depth, position and angulation of implant in 3D
4-7. Why do we have to make surgical templates?
Accuracy of the implant placement
Drilling in the correct position and angulation
Minimize chance of failure and mistake
4-8. What can we examine using model analysis?
Diagnostic model (study cast of both jaw, mounted on mean value articulator)
- diagnostic setting of teeth
- determine optimal location of implants according to type of prosthesis
Ed/Ju notes (eddieliuy@yahoo.com)
5. General consideration of implant surgery
5-1. Regarding the way of healing, what kind of surgical protocols do you know?
One stage (trans-gingival healing) Two stage (submerged healing + abutment install)
- Less surgical stress needed - Second operation needed
- Keratinized gingival - slower gingival healing
- More difficult gingival correction - Easy gingival correction
- GBR technique is more difficult - Easier GBR technique
- Good bone quality needed - Possible in poor bone quality
- Susceptible to infection - undisturbed healing
5-2. What are the surgical steps of implant placement?
(Example using a tapered 2.8-3.6mm implant with 4.2mm counter sink)
1. Flap design alveolar ridge, wassmund flap
2. Marking drill 2.3mm or 3.1mm round bur (Ref:5-3 for distance)
3. Pilot drill 2.2mm twist drill
4. Control measurements depth gauge, parallel gauge
drill guide (guide distance to adjacent implant)
5. Widening drill 2.8mm twist drill slowly increase size
Osteotom technique if needed in maxilla
6. Counter-sinking 4.2mm modified hole to fit the abutment
7. Threading depends on bone quality and implant design
8. Implant placement One stage or two stage technique
Insert with hand or rotary instrument
Apply torque to achieve primary stability
Placing healing screw if needed (for two stage technique)
5-3. What is the surgically positioned minimal distance, recommended between the implants and the implant tooth?
>3mm distance between 2 implants
>7mm distance between center of 2 implants
>1.5mm distance between implant and adjacent tooth
5-4. What is the meaning of primary stability of the implant?
Initial stability of implant maintained by cortical bone, or other hard tissue
Provide stability of implant, and chance for later osseointergration
Harder to establish in immediate implant placement
5-5. What is the purpose of the second operation in the two-stage protocol?
Expose the implant tip, and forming of gingiva-abutment connection
Ed/Ju notes (eddieliuy@yahoo.com)
6. The timing of implant placement
6-1. What are the possible times of implant placement after tooth loss?
Immediate Immediately after tooth removal
Delayed 4~8 weeks later Planned
Early 3~4 months later
Late completely healed jaw after 4~6 months Accidental
6-2. What are the advantages disadvantages of immediate implantation?
- Less surgical intervention - Primary stability difficult to achieve due to anatomical situation
- Shorter overall treatment time - Difficult adaptation of mucosa
- Optimal bone quantity - Local pathoses may influence wound healing
- Technique sensitive
If the space between bone and implant is <2mm, then complete bone healing can be expected if mucosa
properly adapted (using bone augmentation + GBR)
6-3. What are the advantages, disadvantages of delayed implantation? (4~8weeks)
- Nearly optimal quantity of bone - Primary stability is more difficult to achieve
- Easy mucosal adaptation - Longer overall treatment time
- Local pathoses have time to heal - Various degree of alveolar ridge atrophy
- Technique sensitive
6-4. What is the difference regarding the treatment plan, between the early and late implantation?
Early Planned treatment, with disease in mind (need to treat defect and heal wound before implant)
(e.g. inflammation, cysts or other extraction complications of molars)
Late Already edentulous for more than 4~6mth (in majority of cases of implant)
(edentulous patient wants a fixed prosthetic work)
6-5. What are the advantages, disadvantages of the late & early implantation?
- Good primary stability - longer treatment time
- healed soft tissue - atrophy of alveolar bone
Ed/Ju notes (eddieliuy@yahoo.com)
8. The role of implant surface in osseointergration
Titanium oxides
- responsible for biocompatibility of titanium (decisive role in formation of bone & Implant interface)
- 2~6 nanometer thick
- seven kinds of oxide layer can develop, TiO2 is the most thermodynamically stable
- bone & Implant interface: Ti / TiO2 / H2O / Ca2+ ion / glucose amyloglycane / serum protein / osteocytes
- purity of surface (any contaminant can lyse the Ti ions from implant surface negative biological effect)
Porosity of surface/thread shape/implant shape
- Macroretention, increase contact with bone
Surface coating
- Microretention, Aluminum oxide particle size of 75µm produce best result
8-1. What does it mean by macro and micro morphology of implant surface?
Macromorphology (establish mechanical contact with bone)
- biomechanically proper shape
- Implant volume
Micromorphology
(surface geometry of <100µm, accelerates osteoblast migration to surface)
- Surface coating
- Surface roughness
8-2. What does bone-implant contact (BIC) means?
BIC value percentage of implant surface in direct contact with bone (indicates the quality of surface contact)
Acceptable osseointergration Mandible average 40.7%
Maxilla average 37.2%
Circular cross section implants have higher BIC
High implant surface roughness leads to high BIC
- Addition of material Titanium plasma spray
coat with biomaterial (HA: non-resorbable, Tricalciumphosphate: resorbable)
roughening with crystalline TiO2 (produce new layer on top of original TiO2)
- Removal of material acid etching (HCl/H2SO4 need 4x torque to remove c.f. machined surface)
polishing
- Without material transport machined surface,
sand blasting
laser surface modification
- Combination methods SLA (Sandblasted-Large Grid-Acid etched)
8-3. What do you know about the titanium plasma spray method?
Increase surface roughness by addition of materials
Thickness 20~30µm, Roughness 20µm
8-4. What do you know about sandblasting?
Al2O3 or TiO2 sand blasting
Al2O3 can be 50 µm or 250 µm roughness
Pressurized air pushes Al2O3 to collide with implant in high speed
8-5. What do you know about the SLA surface?
Combined method using sandblasting (250 µm Al2O3) + Acid etching (HCl/H2SO4)
Used is Straumann ITI implant
8-6. Which methods may be applied to study the success of surface modification?
In vitro
XPS (X-ray photoelectron spectrometry) surface bombard with xray, measure kinetics of photoelectron
1~2nm study depth useful in detecting surface contaminants
SEM (Scanning electron microscope) best, most often used method for surface morphology
20x,100x,500x,1000x,2000x magnification compare morphology, detect contaminants
AFM (Atomic force microscopy) nanomorphological surface can be visualized
diagram with hillocks and dendritic structure visible concludes surface morphology
Histology and histomorphology examine histology of rabbit femur cross sections
BIC can be measured with micrometric occulator (express in %)
In vivo
Removal torque test implant on <1yo rabbit femur, kill 3mth later, remove with special torque meter
torque value recorded, and statistically analyzed
Ed/Ju notes (eddieliuy@yahoo.com)
9. Conditions of success1: Biocompatibility, osseointergration
9-1. What are the essential conditions of success of implantation?
Biocompatibility
Gingival seal
Optimal transmission of masticatory forces
9-2. What is the biocompatibility?
Characteristics that defines the connection of the implant and the neighboring tissue
Ability of device to perform the function its intended to do
Device should not make any undesirable local or systemic effects to the host
Non-toxic metals titanium, tantalum, zirconium, platinum, niobium
9-3. What is the biomechanical functional ability?
Characteristics of solidity and alterability of form, which enable the implant to transmit masticatory forces to the
bone, without damaging it
9-4/5/6. What are the bio-tolerant/bio-inert/bio-active materials?
Bio-tolerant materials (Increase mechanical property)
(steel alloy, Vitallium(Cr-Co-Mo), plastic materials)
Bio-inert materials
(tantalum, titanium, niobium, aluminum oxide ceramics, carbon compounds)
Bio-active materials (Increase biological property)
(bioglass, hydroxyapatite, tricalcium phosphate)
9-7. What is the most widely used titanium alloy?
Recommended for dental implant
- Commercially pure titanium (CP) (Ti 99.75%, Fe0.05%, O20.05%, N20.03%, C0.05%, H20.012%)
- Titanium alloys - Ti 6Al 4V (titanium + aluminum + vanadium) most widely used
- Ti 5Al 2.5Fe
- Ti 6Al 7Nb
Bone-implant interface - Bone/electrolyte
- Oxide layer (TiO2) responsible for stimulating osseointergration
- titanium body
9-8. What is the osseointergration?
1952 (Brånemark -Sweden) flow of blood in titanium implant chamber in rabbit bone
- Discover bone had integrated so complete with implant, and cannot remove
Healing process of bone and cellular reactions forming the implant-bone interface
- Direct structural and functional connection between implant
- A feature unique to titanium & hydroxyapatite
- When bone laid very close to implant, the TiO2 permanently fuses with bone
Stages: 1. Exudative/proliferative phase (day1-14)
- wound healing process
- water molecule bind to TiO2 layer by hydrogen bond
- Ca2+ & serum protein aggregate and form biofilm
- mesenchyme cell (from wall of BV) transformation into osteoblast
- collagen matrix deposition, blood vessels proliferation
2. Formation of reticular bone (week 2-6)
- formation of osteoid (reticular bone tissue)
3. Formation of lamellar bone and remodeling of peri-implant bone (week 6-18)
- osteoclast remodeling & osteoblast formation of lamellar bone
Ed/Ju notes (eddieliuy@yahoo.com)
9-9. What are the conditions of the development of osseointergration?
Atraumatic, aseptic operation
Bioinert or bioactive materials
Proper implant surface
Primary stability
Undisturbed (unloaded) healing
9-10. What are the bioactive materials used for?
Calcium phosphate ceramics
- Bioglass (glass with <60% SiO2, also contains Na2O, CaO and P2O5)
- Hydroxyapatite Ca5(PO4)3OH non-resorbable
- Tricalium phosphate Ca3(PO4)2OH resorbable
Property highly bioactive, but mechanically weak (easily fracture)
Use - Filling up bony defects
- Augmentation of bone
- Coating of implant surface
Ed/Ju notes (eddieliuy@yahoo.com)
10. Conditions of success2 Gingival seal, progressive osseointergration
10-1. What are the technical possibilities of the surgical exposure of implants?
Made during 2nd stage technique to expose the implant for abutment connection after osteointegration
- Gingival former is placed after excision, and flap reconstructed to form peri-implant mucosa
Apical repositioning of the flap
Papilla regeneration techniques (P.Palacci)
Split finger techniques (Haessler, Kornmann)
H-shape flap (Hahn, Shahidi)
10-2. What are the morphologic parts of the gingival seal around implants?
1. Junctional epithelium (provide defense to bacteria for peri-implant tissue)
2. Basal lamina (part of junctional epi, adhere to implant surface by many hemidesmosome)
3. Collagen fibers (Run around the implant providing mechanical seal - stability of peri-implant tissue)
- originate from periosteum
- fiber runs parallel to machined surface, or directed towards micro-textured surface
10-3. What is the biologic width?
Constant vertical dimension of peri-implant soft tissue (periodontal for natural tooth)
- level of restoration will alter the biological width
- deeper restoration bacteria can accumulate deeper release toxin
biological width will move down ~2mm from level of restoration to compensate
Average value 2.04mm (Gargiulo1961) , 0.75-4.33mm range (Vacek1994) ~3mm
Biological width = SD + JE + CTA
PM/GM (Peri-implant mucosa margin / Gingiva margin)
Sulcus depth - tip of gingiva to depth of sulcus
aS (apical extension of sulcus)
Junctional epithelium - part of epithelium attached directly to implant/tooth
aJE (apical extension of junctional epithelium)
CT attachment - band of collagen attached to implant
BIC/BC (Bone-implant contact / Bone contact)
10-4. What are the possible clinical significances of the biologic width?
Is trans-gingival healing (1stage) better than submerged healing (2stage)?
- 1stage place implant supra-crestal, biological width immediately established less vertical bone loss
- 2stage place implant sub-crestal, biological width established only after 2nd stage more vertical bone loss
The distance recommended between submerged implant and CEJ of neighboring teeth is 3mm
Example: 11.5mm to IAN in mandible molar implant, need to retain as much bone as possible
1stage use 12mm implant, leave 2mm supra-crestal biological width immediately established, BIC is 10mm
2stage use 10mm implant, place at crestal level, after 2nd stage remodeling move BW down 2mm, BIC left is 8mm
10-5. What is progressive osseointergration?
Bone-implant contact increases by the physiological remodeling of bone
Proper loading allows BIC to increase from 53% to 74% by end of 1st year following insertion
Ed/Ju notes (eddieliuy@yahoo.com)
Stages Prosthetic loading Masticatory forces transmitted to bone
Bone resorption Formation of a cellular connective tissue matrix
Re-ossification starts
Completed ossification Bone remodeling
Keeping the bone in a physiological state
10-6. What is the clinical significance of progressive osseointergration?
Bone becomes more mature with the proper loading
The implant placed inhibits the atrophy of the edentulous alveolar ride
10-7. What are the conditions of long term maintenance of osseointergration?
Optimal gingival seal
Optimal transmission of masticatory forces
Ed/Ju notes (eddieliuy@yahoo.com)
11. Conditions of success3 Masticatory load transmission through implants
11-1. What factors influences the loading of oral implants?
Way of healing
Fibro-osseous healing transmission of compressive force undesirable
- Overload bone increase bone resorption
Osseous healing (Condition of osseointergration 3~6 months unloaded healing)
- Time of loading immediate/early/conventional
Bone properties
amount of peri-implant bone (minimum 1mm)
bone quality (D1~D4, BIC, distribution in the jaw)
progressive osseointergration (BIC increase with physiological remodeling of bone)
Implant material (Ref 11-8)
Cortical Titanium Tantalum Al2O3 Au-Pt Steel alloy Cobalt alloy
bone Ceramics alloy (Fe-Cr-Ni) (Co-Cr-Mo)
Tensile strength 30-60 600-1000 930 300 700-800 900-1500 900-1000
Elastic modulus ~20 120 180 350-400 100 200 250
Implant shape (Ref 11-9, 12)
Implant surface
- Macromorphology biomechanically proper shape, implant volume (threads, holes, hollows)
- Micromorphology Surface coating (plasma spray, bioactive material coat, sand blasting, acid etch)
- BIC stronger in rough surface than polished surface
- Roughened with fine granules better integration than coarse granules
- HCl/H2SO4 acid etched 4x higher removal torque needed than machined surface
- Microtextured surface allow bone formation on surface of implant
(machined polished surface, bone formed on surface of old bone)
Forces (Ref: 12)
Type: - Compressive force
- tensile force
- shear force
Direction - Horizontal force
- Vertical force (bending moment)
11-2. When can we load the implant, after insertion?
Immediate loading Loading in the initial stage of bone healing Within 72 hours
Early loading Physiological loading following initial osteogenesis About 3 weeks later
Conventional loading 3-6 months later
11-3. What are the advantages and disadvantages of immediate loading?
Immediate loading promotes the functional osteogenesis (Ledermann1979)
Functional bone remodeling
Allow temporary prosthesis on the implants
Shorter treatment time
Promote osteogenesis (Decreases bone resorption)
Increased aesthetics
- Total or partial lack of osteointegration (BIC decreased)
- Increase risk for rejection
Immediate loading is a therapeutic possibility that depends on complex biomechanical conditions
11-4. What is the value of micro-motion tolerated by the bone?
50 - 150 µm (at level of rough implant surface)
11-5. Which factors influence the immediate loading of endosteal implant?
masticatory forces
quality of bone
optimal load distribution - maximal implant surface
- splinting of implants together
- balanced occlusion
11-6. What is the primary stability of implants, and what is the importance of it?
Ed/Ju notes (eddieliuy@yahoo.com)
Fixation of implant in the bone during surgical placement
The insertion torque necessary for the success of immediate loading and primary stability is > 25 40 Ncm
11-7. What does it mean by early loading of endosteal implants?
Physiological loading following the initial phase of osteogenesis (about 3 weeks after implant placement)
Possibly for early loading achieved by modification of implant surface for accelerated osteointegration
Implant surface promoting early loading :
ITI, Nobel Biocare, 3i, Ankylos, Pitt-Easy, SLActive, Ti Unite, Osseotite, Puretex
11-8. Why do we not use aluminum implants?
Low tensile strength (300 N/mm2) with Very high elastic modulus (350-400 x103 N/mm2)
brittle, Not elastic, since a small strain (bending) will cause rapid increase in stress
quickly reach maximum tensile strength
Similar to glass, easily fractured
(NOTE: E-modulus the gradient of graph, tensile strength point when material break)
11-9. How about the ranking order of load-bearing characters of implants, according to their forms?
(Ref: 12)
Ed/Ju notes (eddieliuy@yahoo.com)
12. The fundamental biomechanics of oral implants
Mechanics solving the technical problem by physical laws
e.g. investigate prosthesis and connection to abutment
Biomechanics in vivo investigation of mechanical processes according to biological reaction
e.g. dynamic examination of BIC
Biomechanical role of the implant = the transmission of forces between the restoration and the jaws
o Aim for Mechanical solidity
o Proper transmission allow Prevention of inactivity and bone atrophy
Prevention of arising above the peak mechanical stress
Prevention of overloading of bone
Minimizing shearing stresses
12-1. What are the important physical elements and their description in biomechanics?
Force the physical strength of mechanical interactions of objects (1Newton ~ 0.1 kilopond kp)
Type: - Compressive, tensile, shear
direction: - Horizontal (concentrated on neck)
- compressive force act from opposite side as force
- tensile force act from same side as force
- Vertical (cause bending moments)
- parallel to tooth compressive force from below
- not parallel to tooth shear force (bending moments)
Bending moments scale of bending capacity of force, has direction, M=F.k (Nm)
Mechanical stress force over area, P=F/A (N/mm2)
Deformation elastic modulus,
Strength maximal stress-strain relationship object, without destroying it (point of destruction)
Isotropic substance physical property of substance (elastic modulus, light refraction, etc) are equal to the
different direction
Anisotropic substance homogeneity in all direction
12-2. Which investigative methods are useful in clinical practice?
Measure dynamic (biting) forces
- Dynamometer use to measure force between occlusal units
- scale , direction?, division of force?, dynamic measurements?
- Standardization?, reproducibility??
Measure bending moments
- torque wrench (with scale)
- indicates primary stability, but conjectural (guessing) calculations only
Periotest® method
- Test stability of implant, small metal rod, knock against implant
- value calculated using reflection
RFA - Resonance frequency analysis (by Osstell® instrument)
- vibration transmitted to implant by special transducer
- stability calculated based on interference analysis
Lab methods
Finite element analysis
- computer method with high accuracy
- dependent on input data (frequently uncertain)
- found that only upper 5mm of implant takes all the load
(wider diameter has better load distribution than longer implant)
Photoelasticity stress analysis
- direct modelling necessary
- result in raltive units
12-3. What are the most important biomechanical principles of implantology?
1. Optimal load distribution (Ref: 12-4)
2. Tensionless (precise) fit
Imprecise fit of denture will develop permanent stress
May cause - dislocation of abutments
Ed/Ju notes (eddieliuy@yahoo.com)
- unfavorable bone remodeling
- braking of prosthesis
3. Decrease horizontal forces & bending moment (Ref: 12-6)
4. Force (stress) breaking effect (Ref: 12-8)
12-4. What is the importance of the mechanical stress distribution in peri-implant bone?
The proper implant loading on the bone providing bone remodeling
Proper loading will increase bone-implant contact (Progressive osteointegration) (Ref10-5)
BIC increase from 53% to 74% by end of 1st year following insertion
Prevent alveolar bone resorption and increase bone formation
To achieve optimal load distribution
a. Maximal implant supported surface
placing more implants Anterior region 1 implant replace 1 tooth
Molar region 2 implants replace 1 tooth
2
Extension of implant surface (Axisymmetric A~r l, P=F/A)
- radius of implant (r) effectively decrease stress, Optimal radius depends on bone dimension
- length of implant (l) limited decrease in stress highest stress located in neck region (5mm)
- surface roughness increase surface area (BIC) of osseointergration
- macromorphology (threads, holes, hollows)
- micromorphology (surface roughness, surface coating)
b. Splinting of implants with a fixed prosthesis
c. Balanced articulation
d. Avoid rigid connection between implant and natural teeth need precision attachment with micromovements
(e.g. screw joint retention, telescopic coping, internal pin with axial movement)
12-5. What is the difference between natural teeth and implants in view of biomechanical behavior?
Natural teeth
- Periodontal tissues Visco-elastic biomechanical behavior (sharpey fibers + fluids in periodontal space)
- Physiological mobility of teeth Axially 10-50µm, laterally 500µm
- Forces are prolonged in time
Endosteal implants
- Fibro-osteointegration (fibrous capsule) Transmission of the compressive forces are undesirable
- Osteointegration Bony healing, direct bone-implant connection, simpler than periodontium
Compressive, tensile and shearing stresses are directly transmitted to bone
In optimal case implants-neighbouring tissues have an equal elastic modulus
In reality bone and implant have different elastic modulus (Ref 11-1)
Bone 15~30, Ti 120, Al2O3 350, CoCr alloy 225 (103 N/mm2)
Masticatory forces - Molar/premolar 200~880N
- full denture 77~196N
- Max value on implant 412N
- horizontal component 20N
12-6. What is the role of bending moment, and what are the possibilities to decrease it?
Bending moment Elevated stress around the implant
Necessary to know the forces + center of rotation for calculation
- Centre of rotation - Close to the border of the neck and middle third of the implant, or
- other part of the implant or
- out of the implant, somewhere in the bone?? (so hard to determine)
- site determined by - jaw anatomy
- quality, the ratio of compact and trabecular bone
- type of prosthesis
- forces - scale is measurable
- the division on the abutment and directions are presumable only
Possible bending forces
Ed/Ju notes (eddieliuy@yahoo.com)
1. inclinated cusp surfaces transform the load to lateral forces
2. the force creates torque around the other abutments
3. the prosthesis follows the bended dental arch
4. rigid splinting of abutments (implants and natural teeth) torque arises
Possibilities to decrease horizontal forces and bending moment
Decrease horizontal force (horizontally directed force)
1. Create canine guidance when replacing lateral teeth
2. Make flat cusps
3. decrease height of the supra-structure
Decrease bending moment (vertically directed force)
4. Reducing the width of the masticatory surface
5. Rigid splinting of implants
6. Avoid cantilever whenever possible
12-7. How can implant geometry influence long-term implant success?
The shape of the implants
extended (Blade) - effective bone utilization
- doubtful direct bone-implant contact surface
- peak stresses in the neck portion of the implant
stepped shape - neck region = moderate stress
- other parts = peak stress
cylindrical implant - straight-cylindrical shape neck region = higher stress
other parts = equal stress
screw (threaded) - stresses are more equal compared to cylindrical
implant - high stress in neck region
- direction of loading is determinant
- low rising of thread is favorable (especially in compact bone)
- rounded quadrangular thread profile is favorable
- high profile depth in trabecular bone
12-8. What theories are the stress breakers based on? What is the function and clinical importance of stress breakers?
Theory: Replacing the role of periodontium in absorbing masticatory forces
Function: An elastic element between the implant and the abutment
To prolong in time and absorb sudden, shock-like forces directed on the jaw
To biomechanically harmonies osseointegrated implants and natural teeth
Plastics or rubber stress breakers
- Fatigue, Plague accumulation need to change often
- MDI® implant rubber O-ring
- Adoro-Ivoclar composite masticatory surface
- IMZ®, Flexiroot®, SIS® IMP plastic masticatory surface
12-9. What is the biomechanical difference between cylindrical and screw type implants?
The screw type implants
o Its critical to load the bone in compression while minimising the shear forces
Compressive and tensile stress
o Stresses are more equal
o Direction of loading is determinant
The cylindrical implant
o Deriving its support through shear stress applied to the implant
Straight or stepped shaped
Ed/Ju notes (eddieliuy@yahoo.com)
12-10. What do the terms reactive and therapeutic biomechanics mean?
Reactive biomechanics
- Inter-alveolar space grow as a consequence of the atrophy of alveolar
process following loss of teeth
- Due to altered morphology of the jaws, the implant can only be placed in a
biomechanical unfavorable position
- Due to these conditions, implants are subjected to a high bending moment
when the restoration is in place
Therapeutic biomechanics (solve problem produced by reactive biomechanics)
- Bending moment effecting final restoration can be by biomechanical thinking upon implant planning
- by determining the position and direction of the implants and by a deliberate planning of articulation
Degree inclination of cusp may influence bending movement
- Increased inclination of cusp by 10% will increase torque by 30%
vestibule-oral and vertical placement of implant may influence bending moment
- upper molar implant move 1mm buccally torque by ~15%
move 1mm apically torque by ~5%
Angle of implant placement relative to direction of force also influences bending moment.
- 10 degree difference in axis increases torque by about 5%
Ed/Ju notes (eddieliuy@yahoo.com)
13. The fundamentals of implant prosthodontics 1
13-1. What is the surgical and prosthetic role of healing abutments?
Implant component place during 2nd stage surgery (only for two stage technique)
use to guide periodontal soft tissue healing prior to definitive prosthetic restoration
typical cylindrical design
Used in anterior region to form peri-implant gingiva for esthetic reasons
Usually NOT used in molar region (no esthetic demand)
13-2. What are the characteristics of the one-piece abutment?
Abutment implant component, serves as support or retention for dental prosthesis
Requirements mechanical stability
proper form for retention of superstructure
tight seal between implant and abutment
retrievability
One piece - Direct attachment to implant
- Non-rotational stable(rely on conical connection only)
- should NOT be used for solo crown rotational risk
- Only straight form
- connection to prosthesis - normal conical/tapered shape abutment
- abutments for O-ring/ball retention
- abutment for screw-retained restoration
Two piece - implant, then retain with a screw
- Rotational stable (conical + hexagonal, octagonal form) can be used for crown and bridge
- Can be straight or angulated (more widely used)
- more complex structure
- esthetic problem with mini screw
13-3. How to provide rotation stability of implant abutment?
Types:
Conical, tapered connection widely used in both one piece and two piece abutment, 6 degree angle
very solid connection, no micro gap, no bacteria, no peri-implantitis risk
Good conical seal, but insufficient rotational stability (rely on friction)
hexagon, octagon formations Only for two piece abutment, press in and screw retained
internal/External, hexagon/octagon true rotational stability
other mechanical retentions
conical-tapered Internal - octagon External octagon
connection formations formation
One piece & two piece ITI-Straumann SynOcta
Ed/Ju notes (eddieliuy@yahoo.com)
13-4. How can the divergence of implant be prosthetically corrected?
Upper anterior region - shape of alveolar ridge cause implant to be placed in diverging position
Straight abutment
Slight grinding to make 10~15degree angulation allowed
screw retained easier to adapt cemented
(since screw retained can use shorter abutment than cemented)
Two piece angulated abutment to correct this
can change angulation (usually 15~25 degree, no more than 30drgree)
due to mechanical problem, buccal portion of prosthetic shoulder
is high up (esthetic problem in marginal region)
13-5. What are the characteristics of the zirconia abutments?
- Very esthetic important in anterior region
- Individually shaped using CAD/CAM
- Not as strong as titanium, but sufficient for anterior teeth, mechanically stiff
- Very strong surface-surface contact,
But if not precisely fit (i.e. with debris) can fracture under load
13-6. What is the basic difference in taking impressions, between the conventional and implant prosthodontics?
Impression coping:
- Usually cannot take an impression directly over abutment (compare to conventional)
- commercially available or custom fabricated component, connected to an abutment or directly to implant
- for transferring the implant location or relationship with other implants in the arch, to the lab
- Impression can be taken:
At abutment/implant level
With closed/open tray technique
13-7. How can you describe the impressions on implant and abutment level?
- abutment level
(impression recording position of abutment)
coping attached to abutment
impression taken directly over coping with special tray
- Implant level
(impression recording position of implant)
use of abutment analogue during impression
dental lab selects the right abutment to fit implant
13-8. What is the difference between impression techniques with closed or open tray?
- close tray technique
impression made directly over coping
- open tray technique
impression made on coping with screw attached
Special tray prepared with holes (open tray)
After impression, screw released to remove impression with coping
Lab equipment
Abutment analogue
E
The other end allows impression to be taken
Use with implant level impression
- Impression taken with the position of the implant
- allow abutment to be selected in the lab
Laboratory copings
Metal or plastic coping used in lab to build up prosthetic work
Allow wax up directly on the coping
Produce precise attachment
(Plastic coping ONLY used in lab
- since unable to sterilize for oral use)
Ed/Ju notes (eddieliuy@yahoo.com)
14. The fundamentals of implant prosthodontics 2
14-1. What are the nomenclatures of implant prosthesis?
(way of fixation) (type of support)
Fixed partial denture - cemented - tooth-implant
- implant
- Screw - tooth-implant
- implant
Removable partial denture Overdenture - implant
- Mucosa
- Implant mucosa
Prosthesis type Partial arch coverage Full arch coverage
Removable Implant supported RPD Implant supported overdenture
Implant-tissue supported RPD Implant-tissue supported overdentre
Fixed Implant FPD Implant FCD
14-2. What are the types of fixed implant restorations?
Extension
Full house bridge -
Partial bridge -
Solo crown - due to rotational stability, should ONLY use two piece abutment
Way of fixation
Cemented
Screw retained
Type of support
Purely Implant
Tooth-implant
14-3/4. What are the advantages & disadvantages of cemented implant prosthesis?
passive suprastructure
conventional laboratory work easy impression, easy lab work
easy completing procedure only cementation required
good esthetics no screw holes
no retrievability, difficult correction if fractured ceramic, periodontal disease require damaging the prosthesis
(temporary cement instead of permanent can be used to overcome problem)
larger abutment, extended inter-maxilla space needed
for cement to hold bridge/abutment at least 5~6mm crown length of abutment needed
inter-maxilla space minimum is 8mm, (if less can be a problem)
long standing edentulous often have inter-maxillary space, due to opposing tooth elongation
14-5/6. What are the advantages & disadvantages of screw-retained implant prosthesis?
more widely used
shorter superstructure less inter-maxillary space needed, can use very small & short abutment
divergence easily corrected small/short abutment allow easy correction
- straight abutment 10~15 degree correction allowed
- angulated abutment 15~25 degree angulation available
easy retrievability if more than 2~3 implant, prefer to make screw retained then cemented
expensive but preferable if patient can afford
precise lab work needed ability of technician
difficult completing procedure need to screw in prosthesis
esthetic problem of screw holes need to cover with composite cement (clip)
Precise fit needed AVOID in tooth-implant supported cases!!
Ed/Ju notes (eddieliuy@yahoo.com)
14-7. What are the types of removable implant restorations?
These are all Overdenture
Type of support
- implant
- implant mucosa
Type of retention
- Bar retainer
- Telescopic retainer
- Implant (Ball attachment)
bar-retained, implant and mucosa supported , overdenture
- improve upper lip profile (extended buccal soft tissue base plate)
- better oral hygiene
- better phonetic ability
- bar should be parallel with inter-condylar axis
- bar can be extended if more implant available (increased implant support)
Implant retained, mucosa supported overdenture
- use of ball-attachment or telescopic retainer
- completely mucosa supported (extended base plate)
- implant of ball retainer needs to be parallel with each other
- retention via matrix (plastic cap to attach to retainer)
- can be changed if worn out (i.e. reduce retention)
Locator® abutment & Locator® component (matrix)
- - (inner & outer retention)
- Use by ITI, 3i, Noble Biocare, Lifecore
- ®
Cantilever effect of tooth-implant supported fixed prosthesis
- Study found NO different in tooth+implant or purely implant supported cases
- But we still prefer purely implant supported
- After many years, Caries or perio problem of natural abutment can cause moment rotation
- Implant will be steady forever (osseointergration ankylosis to bone)
Cantilever effect will eventually develop cause bridge/ceramic fracture, or bone resorption
Ed/Ju notes (eddieliuy@yahoo.com)
You might also like
- Questions and Correct Answer Keys: MSCAA Practice Paper 2 November 2018Document36 pagesQuestions and Correct Answer Keys: MSCAA Practice Paper 2 November 2018Neelak100% (4)
- Cairo: Pilbeam's Mechanical Ventilation, 6th EditionDocument6 pagesCairo: Pilbeam's Mechanical Ventilation, 6th Editionفاتن المطيريNo ratings yet
- Test - Mark Klimek Yellow Book (KV) - QuizletDocument62 pagesTest - Mark Klimek Yellow Book (KV) - QuizletRonelyn Rachelle CabcabanNo ratings yet
- 11.dental Implants FNLDocument204 pages11.dental Implants FNLvsdeeps100% (3)
- Theme 7 - Partial Removable Skeletized Denture: Mandibular VarietiesDocument2 pagesTheme 7 - Partial Removable Skeletized Denture: Mandibular VarietiesShany SchwarzwaldNo ratings yet
- Septeper 2015 Recall 200 Sba Mrcog Part 1Document49 pagesSepteper 2015 Recall 200 Sba Mrcog Part 1VINOD GUPTA100% (2)
- Implant 2Document34 pagesImplant 2allakami777yousefNo ratings yet
- Dental Implants: by DR - Mahmoud Ahmed Elfarmawy Lecture of OMFS Faculty of Dentistry, SU, KantaraDocument34 pagesDental Implants: by DR - Mahmoud Ahmed Elfarmawy Lecture of OMFS Faculty of Dentistry, SU, KantaraMohammed TarekNo ratings yet
- ImplantDocument86 pagesImplantelle70503No ratings yet
- Imp 521Document149 pagesImp 521Mohamed KilaniNo ratings yet
- Dental ImplantsDocument49 pagesDental Implantsaay18bdsNo ratings yet
- Dental ImplantsDocument70 pagesDental ImplantsDENTALORG.COM100% (5)
- Module 7 2011 Tanima MannanDocument18 pagesModule 7 2011 Tanima MannandrarlenaphilipleeNo ratings yet
- O.surgery Lec11Document22 pagesO.surgery Lec11MohammedNo ratings yet
- 06 Success and Failure of ImplantsDocument28 pages06 Success and Failure of Implantsprostho booksNo ratings yet
- Risks and Complications of Orthodontic MiniscrewsDocument51 pagesRisks and Complications of Orthodontic MiniscrewsutokaNo ratings yet
- Caitlin Doede - Periodontology Study NotesDocument14 pagesCaitlin Doede - Periodontology Study Notesapi-347345383No ratings yet
- Dental Implant: Presented byDocument43 pagesDental Implant: Presented byade ismailNo ratings yet
- Micro Implant Anchorage in Orthodontics / Orthodontic Courses by Indian Dental AcademyDocument39 pagesMicro Implant Anchorage in Orthodontics / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Post Graduate Student: Dr. RahultiwariDocument158 pagesPost Graduate Student: Dr. RahultiwariVivek Sunil EdayathNo ratings yet
- 0verview of Dental ImplantologyDocument70 pages0verview of Dental ImplantologysabbyNo ratings yet
- ImpiantiDocument23 pagesImpiantisabbyNo ratings yet
- Screenshot 2022-12-22 at 6.21.43 PMDocument80 pagesScreenshot 2022-12-22 at 6.21.43 PMdr.teethdentalclinic2019No ratings yet
- Immediate Dental Implants and Bone Graft: Khalid S. Hassan and Adel S. AlaglDocument11 pagesImmediate Dental Implants and Bone Graft: Khalid S. Hassan and Adel S. AlaglAndria FadliNo ratings yet
- Temporary Anchorage Devices in Orthodont 970c9d2aDocument11 pagesTemporary Anchorage Devices in Orthodont 970c9d2aThang Nguyen TienNo ratings yet
- Indications For Dental ExtractionsDocument27 pagesIndications For Dental ExtractionsmidhunNo ratings yet
- TadsDocument27 pagesTadsshilpaNo ratings yet
- Bio-Materials in Implants: BY, DR - Siddarth SasDocument33 pagesBio-Materials in Implants: BY, DR - Siddarth SasNagappan Chockalingam100% (1)
- ImplantologyDocument212 pagesImplantologyGabriela Cocieru Motelica100% (1)
- DR Ghazy 2013 Implant Lectures For 4th Year StudentsDocument25 pagesDR Ghazy 2013 Implant Lectures For 4th Year StudentsMohamed Hamed GhazyNo ratings yet
- Dental Implantology: ImplantationDocument22 pagesDental Implantology: Implantationehab qasimNo ratings yet
- Review of Dental ImplantDocument10 pagesReview of Dental Implantmar100% (1)
- Dental ImplantsDocument34 pagesDental ImplantsMurielNo ratings yet
- NBDE Dental Boards Oral SurgeryDocument30 pagesNBDE Dental Boards Oral SurgeryJoyce Lim100% (1)
- The Future of ProsthodonticsDocument22 pagesThe Future of ProsthodonticsGoutham SunilNo ratings yet
- Lec1 - Bridge (Fixed Partial DentureDocument9 pagesLec1 - Bridge (Fixed Partial Dentureكاظم عبد الحسينNo ratings yet
- Temporary Anchorage Device (TAD's)Document121 pagesTemporary Anchorage Device (TAD's)Chandra Sekhar Reddy100% (3)
- Short ImplantsFrom EverandShort ImplantsBoyd J. TomasettiNo ratings yet
- IMPLANTOLOGY. Lec 4Document57 pagesIMPLANTOLOGY. Lec 4Moataz BellahNo ratings yet
- Oral ImplantologyDocument19 pagesOral ImplantologyKariim AhmadNo ratings yet
- Precision Attachments (2) PRDocument23 pagesPrecision Attachments (2) PRpriyaNo ratings yet
- Introduction To Dental Implantology: Dr. Nigam Sattar KhanDocument49 pagesIntroduction To Dental Implantology: Dr. Nigam Sattar KhanNigam SattarNo ratings yet
- SplintingDocument94 pagesSplintingsanthoshi_rani2006100% (3)
- IMPLANTOLOGI Compressed Compressed (1) - MinDocument122 pagesIMPLANTOLOGI Compressed Compressed (1) - MinNayafilahNo ratings yet
- (Dental Material) - Dental Implants (Lec18)Document6 pages(Dental Material) - Dental Implants (Lec18)DTM FHKNo ratings yet
- Dental Implants: Dr. D.M. Ajayi. August, 2017Document129 pagesDental Implants: Dr. D.M. Ajayi. August, 2017Kassim OboghenaNo ratings yet
- Biomaterials For Dental Implants Current and Future TrendsDocument34 pagesBiomaterials For Dental Implants Current and Future TrendsDeivyson Augusto100% (1)
- Surgical AP in Implant 21.07.09Document218 pagesSurgical AP in Implant 21.07.09Chokthanyawat100% (3)
- JHealthSpec1290-8553491 234534Document7 pagesJHealthSpec1290-8553491 234534Gabriela ZuritaNo ratings yet
- Orthodontics in 3 Millennia. Chapter 15: Skeletal Anchorage: Special ArticleDocument4 pagesOrthodontics in 3 Millennia. Chapter 15: Skeletal Anchorage: Special ArticleHARITHA H.PNo ratings yet
- Implant Guidelines For The Restorative DentistDocument165 pagesImplant Guidelines For The Restorative DentistRajab Lil'ronaldo67% (3)
- DENTAL ImplantDocument9 pagesDENTAL ImplantMohammed HassanNo ratings yet
- Implant Systems: Dr. Unjum Bashir, Dr. Manas Gupta, Dr. Ravish AhujaDocument7 pagesImplant Systems: Dr. Unjum Bashir, Dr. Manas Gupta, Dr. Ravish AhujaDr FarhatNo ratings yet
- Surgical Protocol: For Tidal Spiral Implant Systems TsiDocument13 pagesSurgical Protocol: For Tidal Spiral Implant Systems TsiRavi KumarNo ratings yet
- M Stimmelmayr, 2011Document6 pagesM Stimmelmayr, 2011aliserraristolNo ratings yet
- Implantology in Dental TechnologyDocument30 pagesImplantology in Dental TechnologyRufai HarunaNo ratings yet
- Jpis 51 100Document14 pagesJpis 51 100Veronica NatalieNo ratings yet
- Interlocking Nailining Minimally Invasive OsteosynthesisDocument28 pagesInterlocking Nailining Minimally Invasive Osteosynthesistvm1018No ratings yet
- Crestal Bone: The Maintenance of Around Dental ImplantsDocument5 pagesCrestal Bone: The Maintenance of Around Dental ImplantsJing XueNo ratings yet
- Role of Mini-Implants in OrthodonticsDocument9 pagesRole of Mini-Implants in OrthodonticsRonald WilfredNo ratings yet
- GTC 1 - Introduction To Fixed Prosthodontics (PPSG Lectures)Document52 pagesGTC 1 - Introduction To Fixed Prosthodontics (PPSG Lectures)rositadewiNo ratings yet
- ImplantDocument9 pagesImplantKhaled Abo ZaidNo ratings yet
- Tads - KomalDocument100 pagesTads - KomalRohini TondaNo ratings yet
- State of The Art: Fiona C. Goldizen,, Peter D. Sly,, and Luke D. KnibbsDocument15 pagesState of The Art: Fiona C. Goldizen,, Peter D. Sly,, and Luke D. KnibbsKarina Aguirre AlvarezNo ratings yet
- Welcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinDocument16 pagesWelcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinUmair MazharNo ratings yet
- India Immunization Chart 2010Document1 pageIndia Immunization Chart 2010Sarath Nageshwaran SujathaNo ratings yet
- Case Study ChoreaDocument18 pagesCase Study ChoreaKinjalNo ratings yet
- Antiplasmodial and Toxicological Properties of Cnidoscolus AconitifoliusDocument14 pagesAntiplasmodial and Toxicological Properties of Cnidoscolus AconitifoliusRuthNo ratings yet
- Induced Abortion and Risks That May Impact AdolescentsDocument29 pagesInduced Abortion and Risks That May Impact AdolescentsMichael RezaNo ratings yet
- Survival of Pediatric Patients After CPRDocument11 pagesSurvival of Pediatric Patients After CPRMaria Regina CamargoNo ratings yet
- 840 B2 Fire Rated Pu FoamDocument10 pages840 B2 Fire Rated Pu FoamJonathan Alexis Abarzua TorresNo ratings yet
- hs486 Document OSHA Recording Work-Related Injuries and IllnessesDocument13 pageshs486 Document OSHA Recording Work-Related Injuries and Illnessesfatmata koromaNo ratings yet
- SequiseZ 70000ON210156 2022 11 11Document19 pagesSequiseZ 70000ON210156 2022 11 11Vipul SinghNo ratings yet
- Icesu Updates Covid19 Confirmed Cases: Morbidity Week 13 January 1 - April 2, 2022Document15 pagesIcesu Updates Covid19 Confirmed Cases: Morbidity Week 13 January 1 - April 2, 2022Jeremae VentarNo ratings yet
- Ex - Cerebellar ExamDocument2 pagesEx - Cerebellar ExamssNo ratings yet
- Thyroid Gland An Diseases of Thyroid D Gland: Omc LectureDocument59 pagesThyroid Gland An Diseases of Thyroid D Gland: Omc LectureEdward MakemboNo ratings yet
- Essential Messages - 2023 CMDocument14 pagesEssential Messages - 2023 CMimran karimNo ratings yet
- Unani System of MedicineDocument18 pagesUnani System of MedicineManika RaiNo ratings yet
- Bab 7Document27 pagesBab 7bangarudaugtherNo ratings yet
- Abstract Book FinalDocument45 pagesAbstract Book Finalapi-200029530No ratings yet
- YökdilDocument195 pagesYökdilglisilsiklin antibiyotikNo ratings yet
- Risk Management PolicyDocument19 pagesRisk Management PolicySonukrishnaNo ratings yet
- Benda Asing Dalam Kornea Akibat Kurangnya Peralatan Keselamatan: Laporan KasusDocument6 pagesBenda Asing Dalam Kornea Akibat Kurangnya Peralatan Keselamatan: Laporan KasusRachmad SammuliaNo ratings yet
- Penn Yan CSD Reopening PlanDocument78 pagesPenn Yan CSD Reopening PlanNews 8 WROCNo ratings yet
- Body Fat & Hydration % Monitor Scale: EvaluationDocument8 pagesBody Fat & Hydration % Monitor Scale: EvaluationElkin MaldonadoNo ratings yet
- Vaccines Are Used To Chemically Neuter People, Drop Their IQ Points, Make Them Dumb, Dependant On Authority, Obediant SlavesDocument3 pagesVaccines Are Used To Chemically Neuter People, Drop Their IQ Points, Make Them Dumb, Dependant On Authority, Obediant Slavestesla2008No ratings yet
- What Is ECG?Document2 pagesWhat Is ECG?Lê Thanh HàNo ratings yet
- Home Economics and Food LiteracyDocument20 pagesHome Economics and Food LiteracyAllan Reuel DominicNo ratings yet
- Joy (Maternity Insurance Product) Prospectus Cum Sales LiteratureDocument23 pagesJoy (Maternity Insurance Product) Prospectus Cum Sales Literaturesanjay4u4allNo ratings yet