Professional Documents
Culture Documents
Dimal Hema
Dimal Hema
Uploaded by
GioAndrew ReyesOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dimal Hema
Dimal Hema
Uploaded by
GioAndrew ReyesCopyright:
Available Formats
20
HEMATOLOGY 1 22
AUTOMATED BLOOD CELL ANALYSIS
GENERAL PRINCIPLES OF AUTOMATED BLOOD CELL ANALYSIS
ELECTRONIC IMPEDANCE
or low-voltage direct current (DC) resistance. Developed by Coulter in the 1950s. Most common methodology used.
RADIOFREQUENCY (RF)
or al- ternating current resistance, is a modification sometimes used in conjunction with DC electronic impedance.
DARKFIELD OPTICAL SCANNING
Introduced by Technicon Instruments Corporation in the 1960s.
OPTICAL SCATTER
Ortho Clinical Diagnostics followed with a laser-based optical instrument in the 1970s.
using both laser and non-laser light, is often employed in today’s hematology instrumentation.
PRINCIPAL INSTRUMENTS
COULTER PRINCIPLE
Detection and measurement of changes in electrical resistance produced by cells as they traverse a small aperture.
Blood cell suspension it is a solution that is composed of electrically conductive diluent
2 chambers filled with a conductive buffered electrolyte solutions separated by glass tube having a small aperture
Direct current is generated between the internal and external electrode
Aperture for RBC/platelet is smaller than the WBC aperture
(1) The cells that are suspended in an electrically conductive diluent (saline) and are pulled through the aperture (orifice with a glass
tube)
(2) In the counting chamber or transducer assembly, the low frequency electrical current is applied
(3) Electrical resistance between two electrodes or impedance in the current occurs as the cell passes through the sensing aperture
(4) This causes voltage pulses that are measurable
OTHER DEVICES
Oscilloscope
Screens or displays the pulses that are generated by the cell as they interrupt the current
The number of pulses is proportional to the number of cells counted
The height of the pulse is directly proportional to the volume of the cell
allows the discrimination and counting of cells of specific volumes to the use of threshold circuits
Histogram
Pulses are also collected and sorted according to their amplitude by pulse height analyzers
Data are plotted on a frequency distribution graph or volume distribution histogram
o Y-axis - relative number (no. of the cells)
o X -axis – channel number equivalent to the specific volume or femtoliter (fL)
It depicts the volume distribution of the cells counted
Pulse height is measured and categorized by pulse height analyzers;
256 channels for WBC and RBC analysis.
64 channels for platelet analysis
RADIOFREQUENCY
CHRISTIANA YSABEL RODRIGUEZ / 3Y1 – 4
Low-voltage DC impedance, may be used in conjunction with RF resistance, or resistance to a high voltage electromagnetic
current flowing between both electrodes simultaneously.
Alternating current resistance - A modification used in conjunction with DC electronic impedance
RFDC detection method
o Shows simultaneous use of direct current and radio frequency in one measurement system
o Conductivity – measured by high frequency is attenuated by nucleus or cytoplasm ratio, nuclear density, and
cytoplasmic granulation
Two different cell properties – to create two- dimensional distribution cytogram or scatter plot
o Low voltage DC impedance
o RF resistance
Cell distribution as clusters and concentration of cell type as number of dots can be seen
Cell internal structure density:
o Nucleus: cytoplasm ratio
o Nuclear density
o Cytoplasmic granulation
REAGENTS AND SUPPLIES
1. Electrolyte
✓ Bufferred isotonic salt solution that may contain one or more preservatives
✓ Must be particle free
✓ Used to dilute cells and to flush the instrument
2. Lysing Reagent
✓ A detergent solution
✓ Used to lyse erythrocytes by dissolving their stroma when leukocyte counts are to be performed
3. Cleaning agent
✓ Used at regular intervals to remove protein build up from the aperture tube and electrodes
4. Sample Container
✓ May range from small glass beakers to plastic vials manufactured for this purpose.
✓ Must be particle free and their internal surfaces do not react or attract cells.
FLOW CYTOMETRY
combines fluid dynamics, optics, laser science, highspeed computers, and fluorochrome-conjugated monoclonal antibodies
(MAbs) that rapidly classify groups of cells in heterogeneous mixtures\
The principle of flow cytometry is based on cells being stained in suspension with an appropriate fluorochrome
An immunologic reagent, a dye that stains a specific component, or some other marker with specific reactivity.
Fluorescent dyes used in flow cytometry must bind or react specifically with the cellular component of interest (e.g.,
reticulocytes, peroxidase enzyme, DNA content).
PRINCIPLES OF FLOW CYTOMETRY
A suspension of stained cells is pressurized using gas and transported through plastic tubing to a flow chamber within the
instrument
In the flow chamber, the specimen is injected through a needle into a stream of physiologic saline called the sheath
The sheath and specimen both exit the flow chamber through a 75-µm orifice.
This laminar flow design confines the cells to the center of the saline sheath, with the cells moving in single file
The stained cells then pass through the laser beam
The laser activates the dye and the cell fluoresces
Although the fluorescence is emitted throughout a 360-degree circle, it is usually collected by optical sensors located 90
degrees relative to the laser beam.
The fluorescence information is then transmitted to a computer, which controls all decisions regarding data collection,
analysis, and cell sorting.
CELLULAR FEATURES MEASURED BY FLOW
CYTOMETRY
Cell size or volume
DNA content
CHRISTIANA YSABEL RODRIGUEZ / 3Y1 – 4
Cytoplasmic Granularity
Cell-surface antigens
Intracellular enzymes
RNA content
Emerging Clinical applications of Flow Cytometry
Detection of small populations of cells
Determination of cell surface phenomena
Evaluation of leukocyte function
Evaluation of intracellular metabolism
Cytogenetics
Semen analysis
Detection of autoantibodies
Measurement of cytotoxicity
Analysis of platelet function
ERRORS IN AUTOMATION
INSTRUMENTAL ERRORS:
Negative Errors - Excessive Lysis of RBC’s
Positive Errors
▪ Bubbles caused by shaking
CHRISTIANA YSABEL RODRIGUEZ / 3Y1 – 4
HISTOGRAM
Graphical representation of numerical data of different cell populations in a cell counter
Gives information on:
CHRISTIANA YSABEL RODRIGUEZ / 3Y1 – 4
o Average size of cell
o Distribution of size
X axis = volume of cell
Y axis = number of cells
Discriminators - separates the distribution curve for the volume
WBC Discriminator
Lower Discriminator = 30-60 fL
Upper Discriminator = fixed at 300 fL
RBC Discriminator
Lower Discriminator = 25-75 fL
Upper Discriminator = 200-250 fL
Platelet Discriminator
Lower Discriminator = 2-6 fL
Upper Discriminator 12-30 fL
Fixed discriminator 12 fL
RBC HISTOGRAM
Platelets have volume between 8-12 fL and counted between 2-25 fL
The value here in the figure is within the lower and upper discriminator
RBCs have volume 80-100 fL and are counted between 25- 250 fL
The value here in the figure is within the lower and upper discriminator
A platelet size distribution plot is produced using a threshold.
One fixed at 12 fL and the other two are allowed to hunt the upper and lower ends of the platelet population between certain
limits.
The lower platelet size threshold may move between 2-6 fL, the higher between 12 - 30 fL.
The importance of this different threshold is to distinguish the platelets from the small red blood cells that is located in the
upper end of the platelet population, and the debris at the lower end testing.
To distinguish their particular boundaries.
Microcytosis
Shift to the Left
Presence of microcytosis - smaller RBCs
Macrocytosis
Shift to the right
CHRISTIANA YSABEL RODRIGUEZ / 3Y1 – 4
More than the normal distribution
Macrocytosis
Dimorphic Population
There is a bimodal peak of the curve.
Two population of sizes of red blood cells.
WBC HISTOGRAM
Cells >35 fL - WBC in the WBC/Hb chamber
Lymphocytes = 35-90 Fl
MID cells = 90-160 fL
Refers to monocytes, basophil, and eosinophils
Neutrophils = 160-450 fL
Abnormal WBC Distribution Curve
When a particular parameter peaks
This diagram shows the different types of leucocytosis.
Increased neutrophil = neutrophilia
Increased lymphocyte = lymphocytosis
MID cells is difficult to detect or distinguish when there is a presence of leukocytosis
WBC distribution of that particular curve are all distributed in the same region.
It cannot be distinguished whether there is an increase in monocyte, basophil or eosinophil.
all three cells could be the reason of the increase of that particular parameter.
CHRISTIANA YSABEL RODRIGUEZ / 3Y1 – 4
WBC Scatterplot
X axis = side scatter and will detect the granularity of the cell
The more it is going to the right, the more granular
Y axis = forward scatter that will reflect the size of the cell.
Going upward, the larger the size
Interpretation:
Lymphocytes (red) – smaller and less granular
smaller in have few internal components or granules than the monocyte (yellow) and granulocyte (purple).
Granulocyte (purple)
most granular population and have the most side scatter, and appear farthest to the right of the scatter plot.
CALIBRATION
Calibrate every morning before running tests
To ensure readings from an instrument are consistent with other measurements
To determine accuracy of the Instrument readings
To establish reliability of the instrument
Determines the accuracy and precision of the analyzers
“Tuning” of the instrument
Basophil-Lobularity (BASO) Channel
cells are treated with a reagent containing a nonionic surfactant in an acidic solution.
Basophils are particularly resistant to lysis in this temperature-controlled reaction, whereas RBCs and platelets lyse and other
leukocytes (nonbasophils) are stripped of their cytoplasm.
Laser optics, using the same two-angle (2 to 3 degrees and 5 to 15 degrees) forward scattering system of the RBC/platelet
channel, is used to analyze the treated cells.
High-angle scatter (proportional to nuclear complexity) is plotted on the x-axis, and low-angle scatter (proportional to cell
volume) is plotted on the y-axis.
Basophils fall above a horizontal threshold on the cytogram. The stripped nuclei fall below the basophils, with segmented cells to
the right and mononuclear cells to the left along the x-axis. Blast cells uniquely cluster below the mononuclear cells.
The nucleated RBC method is based on the physical charac- teristics of volume and density of the nucleated RBC nuclei.
These characteristics allow counting in both WBC channels on the ADVIA 2120, and algorithms are applied to determine the
absolute number and percentage of nucleated RBCs.
Information from the PEROX and BASO channels is used to generate differential morphology flags indicating the possible
presence of reactive lymphocytes, blasts, left shift, immature granulo- cytes, nucleated RBCs, or large platelets or platelet
clumps.
SPECIMEN LIMITATION
CHRISTIANA YSABEL RODRIGUEZ / 3Y1 – 4
Limitations resulting from inherent specimen problems include those related to the presence of cold agglutinins,
icterus, and lipemia.
Cold agglutinins manifest as a classic pattern of increased MCV (often greater than 130 fL), markedly decreased RBC
count, and increased MCHC (often greater than 40 g/dL).
Careful examination of the histograms or cytograms from the instruments may yield clues to this abnormality.
Icterus and lipemia directly affect hemoglobin measurements and related indices.
CHRISTIANA YSABEL RODRIGUEZ / 3Y1 – 4
You might also like
- CASINO by Nicholas PileggiDocument238 pagesCASINO by Nicholas PileggiPutipufNo ratings yet
- Hematology UnitDocument8 pagesHematology UnitMary CabalceNo ratings yet
- Three Dual Polarized 2.4GHz Microstrip Patch Antennas For Active Antenna and In-Band Full Duplex ApplicationsDocument4 pagesThree Dual Polarized 2.4GHz Microstrip Patch Antennas For Active Antenna and In-Band Full Duplex Applicationssanthosh kNo ratings yet
- CELTA Tip: Language Analysis Assignment - Elt PlanningDocument6 pagesCELTA Tip: Language Analysis Assignment - Elt PlanningTeddy BroughtonNo ratings yet
- By Dr. Richa SharmaDocument51 pagesBy Dr. Richa SharmaTrần Thanh ViệnNo ratings yet
- Hematology AutomationDocument117 pagesHematology AutomationRico EdureseNo ratings yet
- HEMATOLOGYDocument7 pagesHEMATOLOGYGioAndrew ReyesNo ratings yet
- 11auto Unit Cell Counting Instruments HandoutDocument15 pages11auto Unit Cell Counting Instruments HandoutyoraikarNo ratings yet
- Module 2 Key Concepts 2Document4 pagesModule 2 Key Concepts 2Pauline Louise S. DURANNo ratings yet
- Chapt 8 Cell Counting AutomationDocument44 pagesChapt 8 Cell Counting Automationnasirex.14No ratings yet
- Quiz2 NoteseditDocument33 pagesQuiz2 NoteseditEricka GenoveNo ratings yet
- Medical MysteriesDocument82 pagesMedical MysteriesSai Kumar KonukuNo ratings yet
- Automation in HaematologyDocument67 pagesAutomation in Haematologyk11a1r18No ratings yet
- SG 8 CH 15 InstrumentationDocument5 pagesSG 8 CH 15 InstrumentationwerfsdsfNo ratings yet
- Complete Blood Counts and ExaminationDocument63 pagesComplete Blood Counts and Examinationzarairahad486No ratings yet
- Chapter 11Document35 pagesChapter 11elleNo ratings yet
- Bismillah..a.yuli FlowcytometriDocument40 pagesBismillah..a.yuli FlowcytometriYuli RohmaNo ratings yet
- DR Preeti Mansukhani - CBC 5 Parts - 2017Document56 pagesDR Preeti Mansukhani - CBC 5 Parts - 2017Silence T-jmNo ratings yet
- Equ28-01 Sysmex XE2100 Op SOPDocument16 pagesEqu28-01 Sysmex XE2100 Op SOPWasim AkramNo ratings yet
- Using Hematology Instrument Data To TroubleshootDocument82 pagesUsing Hematology Instrument Data To Troubleshootuber6791No ratings yet
- 4 - Hematology UnitDocument16 pages4 - Hematology UnitMary CabalceNo ratings yet
- Electrical Impedance: Hematology AnalyzerDocument2 pagesElectrical Impedance: Hematology AnalyzerAzura JKNo ratings yet
- Haematology Analyzer: Automated Cell Counting InstrumentationDocument33 pagesHaematology Analyzer: Automated Cell Counting InstrumentationLisa Virya100% (1)
- Week 17 - Instrumentation in HematologyDocument54 pagesWeek 17 - Instrumentation in HematologyMarie Anthonette SolimanNo ratings yet
- Automated Cell Counting Instrumentation and Point of CareDocument78 pagesAutomated Cell Counting Instrumentation and Point of CareThea ConcepcionNo ratings yet
- Instruments in HaemDocument26 pagesInstruments in HaemZeeshan Yousuf0% (1)
- Hematology AnalyzerDocument29 pagesHematology AnalyzerMac Kevin MandapNo ratings yet
- Automated Counters3Document14 pagesAutomated Counters3Jacky SharmaNo ratings yet
- Automation in Haematology 5-1Document50 pagesAutomation in Haematology 5-1Raphael AnajeNo ratings yet
- HLG Automata 150428233016 Conversion Gate02Document111 pagesHLG Automata 150428233016 Conversion Gate02Starks Gazer100% (1)
- Point of Care Testing: Microhematocrit Centrifuge Conductometric MethodDocument4 pagesPoint of Care Testing: Microhematocrit Centrifuge Conductometric MethodJean BelciñaNo ratings yet
- New QuantitiesDocument6 pagesNew Quantities20100117 Bùi Thùy VyNo ratings yet
- Prinsip Sysmex Hematology AnalyzerDocument5 pagesPrinsip Sysmex Hematology AnalyzerLince Wijoyo100% (1)
- Comparison of The Leukocyte Differentiation PDFDocument8 pagesComparison of The Leukocyte Differentiation PDFDyah LaksmiNo ratings yet
- Flow CytometryDocument7 pagesFlow CytometryWNo ratings yet
- Automated Hematology Analyzer: Presenter: DR - KeerthyDocument95 pagesAutomated Hematology Analyzer: Presenter: DR - KeerthyadiNo ratings yet
- Sysmex XS-1000i Automated Hematology AnalyzerDocument3 pagesSysmex XS-1000i Automated Hematology AnalyzerAdi Subagio0% (1)
- Complete Basic Flow Cytometry Principles ManualDocument37 pagesComplete Basic Flow Cytometry Principles ManualcandiddreamsNo ratings yet
- 2 Thursday MorningDocument4 pages2 Thursday MorningEricka GenoveNo ratings yet
- 11 - Hematology Analyzers - Cell CountersDocument19 pages11 - Hematology Analyzers - Cell CountersMohamed YousifNo ratings yet
- XN 3000 VS BeckmanDocument8 pagesXN 3000 VS BeckmanZied FehriNo ratings yet
- Interpretation of HistogramDocument92 pagesInterpretation of HistogramJagu ShahNo ratings yet
- Complete Blood Count - Student'sDocument20 pagesComplete Blood Count - Student'sAnastasia100% (1)
- Basic HematologyDocument89 pagesBasic Hematologydrafq2000No ratings yet
- Manual of Basic Hematology Techniques For ResidentsDocument35 pagesManual of Basic Hematology Techniques For Residentsksoft appsNo ratings yet
- Presentation On Full Blood Count by Group EightDocument15 pagesPresentation On Full Blood Count by Group Eightmaxwell amponsahNo ratings yet
- Evaluation of The Performance of The Sysmex XT-200Document11 pagesEvaluation of The Performance of The Sysmex XT-200Игорь БеняNo ratings yet
- Int J Lab Hematology - 2007 - ZANDECKI - Spurious Counts and Spurious Results On Haematology Analysers A Review Part IDocument17 pagesInt J Lab Hematology - 2007 - ZANDECKI - Spurious Counts and Spurious Results On Haematology Analysers A Review Part IYangnuu TitusNo ratings yet
- FINAL Automated-HematologyDocument67 pagesFINAL Automated-HematologyDineshprakash GovindhrajNo ratings yet
- RT-7600 Hematology AnalyzerDocument86 pagesRT-7600 Hematology AnalyzerJesus100% (1)
- Presentation On Full Blood Count by Group EightDocument15 pagesPresentation On Full Blood Count by Group Eightmaxwell amponsahNo ratings yet
- Automated Cell Counting InstrumentationDocument33 pagesAutomated Cell Counting InstrumentationCecille Ann100% (1)
- Peripheral Blood Smear and HistologyDocument26 pagesPeripheral Blood Smear and Histologystudent2013100% (1)
- ZP11 Xxi 63Document8 pagesZP11 Xxi 63Jai CarungayNo ratings yet
- Flow Cytometry: Meroj A. JasemDocument58 pagesFlow Cytometry: Meroj A. Jasemahmad100% (1)
- Tech Note Swelab Alfa Plus Analyzer Procedures For Optimized System Performance Tns 33228 2Document8 pagesTech Note Swelab Alfa Plus Analyzer Procedures For Optimized System Performance Tns 33228 2Tholkappiyan Rajamanickam100% (1)
- Accurasi Perhitungan PlateletDocument68 pagesAccurasi Perhitungan PlateletMaria Yosefina HeraNo ratings yet
- Flow CytometryDocument6 pagesFlow Cytometrytanweer_elevenNo ratings yet
- Sysmex ScattergramsDocument7 pagesSysmex ScattergramsRuxandra Mesaros100% (1)
- 6-Principles of Automated Haematology AnalyzerDocument27 pages6-Principles of Automated Haematology AnalyzerWasana MendisNo ratings yet
- Lab EquipmentDocument2 pagesLab EquipmentTaseenHaqueNo ratings yet
- Blood Ceslls CounterDocument21 pagesBlood Ceslls Countermohammed alolfeNo ratings yet
- 00027634-B RCC Wiring DiagramDocument50 pages00027634-B RCC Wiring DiagramKarikalan JayNo ratings yet
- Sigma MALDI Calibration KitDocument4 pagesSigma MALDI Calibration KitRamona Neka TamoNo ratings yet
- Soalan Psikologi Pengujian Dan PengukuranDocument11 pagesSoalan Psikologi Pengujian Dan PengukuranmisxcheaNo ratings yet
- History: The History of The Hospitality Industry Dates All The WayDocument10 pagesHistory: The History of The Hospitality Industry Dates All The WaySAKET TYAGINo ratings yet
- Instruction Book Manual de Instrucciones Livre D'InstructionsDocument79 pagesInstruction Book Manual de Instrucciones Livre D'InstructionsWilfrido RosadoNo ratings yet
- RelativityDocument9 pagesRelativity0hitk0No ratings yet
- Ngspice ManualDocument592 pagesNgspice ManualRommel Joshua OrtegaNo ratings yet
- Name: - ClassDocument4 pagesName: - ClassGumbNo ratings yet
- Combustion Products From Ventilation Controlled Fires - Thesis PDFDocument321 pagesCombustion Products From Ventilation Controlled Fires - Thesis PDFYuri SanchezNo ratings yet
- Order Flow AnalysisDocument6 pagesOrder Flow AnalysisSumit SinghNo ratings yet
- Mfx2550 Field Engineering ManualDocument415 pagesMfx2550 Field Engineering ManualJoeNo ratings yet
- Form 5 ElectrolysisDocument2 pagesForm 5 ElectrolysisgrimyNo ratings yet
- Group Medical Insurance - 2020-21Document2 pagesGroup Medical Insurance - 2020-21Vilaz VijiNo ratings yet
- A J-Protein Co-Chaperone Recruits BiP To Monomerize IRE1 and Repress The Unfolded Protein ResponseDocument27 pagesA J-Protein Co-Chaperone Recruits BiP To Monomerize IRE1 and Repress The Unfolded Protein ResponseLefan YuNo ratings yet
- Topic 7 Basic Concepts of Urban Drainage: (Urban Stormwater Management Manual For Malaysia) MasmaDocument29 pagesTopic 7 Basic Concepts of Urban Drainage: (Urban Stormwater Management Manual For Malaysia) MasmaAzhar SabriNo ratings yet
- Carasuc Form 2 GalleryDocument2 pagesCarasuc Form 2 GalleryJohn Henry TampoyNo ratings yet
- Making Salts NotesDocument17 pagesMaking Salts NotesLola AdegbonmireNo ratings yet
- He Va Grass Roller 63 82 Spare PartsDocument48 pagesHe Va Grass Roller 63 82 Spare PartstotcsabNo ratings yet
- IoT - Internet of Things Based Energy Management For Smart HomeDocument4 pagesIoT - Internet of Things Based Energy Management For Smart HomeEditor IJTSRDNo ratings yet
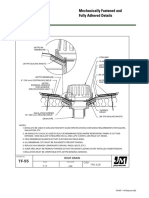
- JM Mechanically Fastened and Adhered Details UltraGard TPO Roof Drain New Construction Detail Drawing B18270Document1 pageJM Mechanically Fastened and Adhered Details UltraGard TPO Roof Drain New Construction Detail Drawing B18270michael jan tubongbanuaNo ratings yet
- Investing in GPS Guidance Systems?Document10 pagesInvesting in GPS Guidance Systems?Koert OosterhuisNo ratings yet
- RS232Document29 pagesRS232Pravish Sainath100% (1)
- Key Performance IndicatorsDocument27 pagesKey Performance IndicatorsZiad NayyerNo ratings yet
- Mfe Getting StartedDocument50 pagesMfe Getting StartedDinesh KNo ratings yet
- Synchro Studio 8: Getting Started and What's New in Version 8Document35 pagesSynchro Studio 8: Getting Started and What's New in Version 8Fernando Luis FerrerNo ratings yet
- Economics SBADocument24 pagesEconomics SBAJamol benjaminNo ratings yet
- MicroZed-3.3 Operators Manual SW v9.00Document64 pagesMicroZed-3.3 Operators Manual SW v9.00Emeka Pius Oramunwa100% (1)