Professional Documents
Culture Documents
Common Laboratory and Diagnostic Tests
Common Laboratory and Diagnostic Tests
Uploaded by
Crazy Stranger0 ratings0% found this document useful (0 votes)
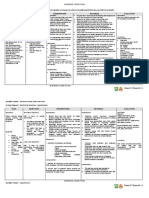
169 views8 pagesThe document provides information on various common laboratory and diagnostic tests, including:
1) Mantoux test and sputum examination to diagnose tuberculosis. Chest x-ray and bronchoscopy are also discussed.
2) Complete blood count, blood gases, and other blood tests to evaluate cardiovascular, hematologic, and renal function.
3) Electrocardiography, Holter monitoring, echocardiography and other cardiac tests like Doppler ultrasonography.
4) Tests for evaluating venous insufficiency and arterial blockages like plethysmography, arteriography, and venography.
Original Description:
Original Title
COMMON LABORATORY AND DIAGNOSTIC TESTS
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document provides information on various common laboratory and diagnostic tests, including:
1) Mantoux test and sputum examination to diagnose tuberculosis. Chest x-ray and bronchoscopy are also discussed.
2) Complete blood count, blood gases, and other blood tests to evaluate cardiovascular, hematologic, and renal function.
3) Electrocardiography, Holter monitoring, echocardiography and other cardiac tests like Doppler ultrasonography.
4) Tests for evaluating venous insufficiency and arterial blockages like plethysmography, arteriography, and venography.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
169 views8 pagesCommon Laboratory and Diagnostic Tests
Common Laboratory and Diagnostic Tests
Uploaded by
Crazy StrangerThe document provides information on various common laboratory and diagnostic tests, including:
1) Mantoux test and sputum examination to diagnose tuberculosis. Chest x-ray and bronchoscopy are also discussed.
2) Complete blood count, blood gases, and other blood tests to evaluate cardiovascular, hematologic, and renal function.
3) Electrocardiography, Holter monitoring, echocardiography and other cardiac tests like Doppler ultrasonography.
4) Tests for evaluating venous insufficiency and arterial blockages like plethysmography, arteriography, and venography.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 8
COMMON LABORATORY AND - + signifies exposure to
DIAGNOSTIC TESTS Mycobacterium tubercle
bacilli
GENERAL PRINCIPLES IN THE CARE OF - BCG immunization will have
CLIENTS UNDERGOING DIAGNOSTIC + result
TEST - RESULTS:
+ with indurations of
Prepare the client physically &
10 mm or more
psychosocially
HIV, indurations of 5
Provide privacy
mm is +
Provide adequate information
Chest X-ray
Take note of NPO
- Uses a very small dose of
Check written consent
ionizing radiation to produce
Assess for allergy to seafood & pictures of the inside of the
iodine chest.
Assess for history of claustrophobia - Used to evaluate the lungs,
Increase fluid intake heart and chest wall.
Abdomen (IAPP) - Instruct client to remove
No abdominal Palpation if with tumor metals from chest because
(liver / kidneys) metals are radiopaque
Examination of abdomen, flex knees
Abdominal Sequence: RLQ, RUQ, Bronchoscopy and
LUQ & LLQ Bronchography
Examine chest in sitting/upright - Require insertion of
position bronchoscope
Stand behind when examining lymph - Uses premedication:
nodes/ thyroid Anticholinergic
Darken room for ophthalmoscopy Anxiolytics
Obtain C & S specimen before 1 st Topical Anesthetic
dose of antibiotic using sterile Spray
technique - Bronchography: uses
In examining female clients, female iodinated contrast medium
nurse must be in attendance then radiograph
- Post procedure:
RESPIRATORY SYSTEM NPO until reflexes
return
Mantoux Test (Skin Test) Side-lying position
- PPD (purified protein
derivative) is used Sputum Examination
- Administered by intradermal - The best time to collect:
injection morning upon awakening
- Interpretation is 48-72 hrs - Rinse mouth with plain water
post injection before collection
- AFB staining requires - Low RBC, hemoglobin &
collection for 3 consecutive hematocrit in anemia
mornings - Polycythemia (increased
RBC & hemoglobin) indicates
Lung Biopsy hypoxia
- After percutaneous needle - Elevated WBC indicates
lung biopsy, position patient infection
turning toward affected side - Neutropenia/ agranulocytosis
(low neutrophil count)
Arterial Blood Gas Analysis indicates low resistance to
- Assess ventilation & acid- infection
base balance - Eosinophilia (elevated
- Blood withdrawn from arterial eosinophil count) indicates
artery allergy or parasitism
- Allen’s test pre-collection
- Heparinized syringe is used Erythrocyte Sedimentation Rate
- Collected specimen is placed - It is elevated in inflammatory
in a container with ice conditions, e.g. Myocardial
infarction
Thoracentesis
- Pressure sensation is felt Blood Coagulation Studies
during the procedure - Prolonged PT, PTT, APTT
- Pneumothorax, needle is indicate bleeding tendencies
inserted in the 2nd & 3rd - PT is valuable in evaluating
intercostal space effectiveness of Coumadin
- Pleural effusion, needle is (therapeutic effect= 1.5-2)
inserted in the 7th or 8th ICS - PTT & APTT are used to
- Monitor for bleeding post evaluate effectiveness of
procedure Heparin (therapeutic
effect=2-2.5)
CARDIOVASCULAR AND
HEMATOLOGIC SYSTEM Blood Urea Nitrogen (BUN) and
Blood Uric Acid (BUA)
Complete Blood Count and
- The values are elevated
Erythrocyte Indices
when there is low renal
- Erythrocyte indices (MCV,
tissue perfusion due to
MCH & MCHC) are best
decreased cardiac output
indicators of anemia
- Increased MCV & MCH in
Blood Lipids
macrocytic anemia
- Serum cholesterol & serum
- Decreased MCV & MCH in
lipids
microcytic anemia
- Require NPO for 10-12 hours
- Decreased MCHC in severe
- Elevated levels increase risk
hypochromatic anemia
of atherosclerosis
CENTRAL VENOUS PRESSURE
Tropinin (CVP) MONITORING
- Elevated Troponin I & T are - Place 0 level/ base of the
best indicators of Myocardial water manometer at the right
infarction mid-axillary, 4th ICS
- Elevated CVP readings
Electrocardiography (ECG) indicate hypervolemia or right
- Elevated Troponin I & T are sided congestive heart failure
best indicators of Myocardial
infarction ECHOCARDIOGRAPHY
- MI: elevated ST, inverted T - Uses ultrasound to assess
wave, pathologic/ enlarged Q cardiac structures & mobility
wave
- Hypokalemia: prolonged DOPPLER ULTRASONOGRAPHY
QRS, elevated ST, short T - Permits assessment of
wave arterial and venous flow in
- Hyperkalemia: Prolonged the lower extremities with the
QRS, elevated ST, peaked T use of a probe moved over a
wave skin surface
- ECG machine
o Detects the patterns ULTRASONIC DUPLEX
of electrical impulse SCANNING
generation and - Localizes site of vascular
conduction through obstruction
the heart - Evaluates degree of
o translates that narrowing & the amount of
information into vascular reflux
recorded patterns - Detects deep vein
(waveform on cardiac thrombosis
monitor or calibrated
paper) PLETHYSMOGRAPHY
- Evaluates venous
Holter Monitoring insufficiency
- Continuous ECG monitoring,
24-H period ARTERIOGRAPHY AND
- Instruct to record activities & VENOGRAPHY
any unusual sensation - Assess for allergy to seafood
experienced & iodine before the
- May remove device only procedure
during bathing
- Continued even during TRENDELENBURG TEST
asleep - Done to detect leg
varicosities
GASTROINTESTINAL SYSTEM - Care post procedure is the
same as post upper GI series
CARCINOEMBRYONIC ANTIGEN
(CEA) UPPER GI ENDOSCOPY
- Elevated levels indicate
- NPO for 6 to 8 hours
presence of colorectal cancer
- Remove dentures
- Gag reflex is depressed with
D-XYLOSE ABSORPTION TEST local anesthetic
- Indicates presence of - Post procedure, side lying
malabsorption disorders position & NPO until gag
reflex returns
FECAL ANALYSIS
- Guaiac stool exam (Fecal LOWER GI ENDOSCOPY
occult blood test/ FOBT) PROCTOSIGMOIDOSCOPY
No red meats, poultry o NPO for 6-8 hours
for 3 days o Laxative the night
Withhold iron,
before the test
steriods, NSAID’s for
o Placed in knee
48 hours
chest/lateral position
- For detection of ova &
during the procedure
parasites, send fresh, warm
o Post procedure,
stool specimen to laboratory
assess for perforation
& vagal stimulation
UPPER GI SERIES/ BARIUM
COLONOSCOPY
SWALLOW
o Preparation is the
- NPO for 6 to 8 hours
same as
- Barium Sulfate is
proctosigmoidoscopy
administered orally
o Place in side-lying
- X-rays are taken in standing
position with knees
& supine position
flexed
- Laxatives & fluids are given
o Post procedure, same
after procedure
as
proctosigmoidoscopy
LOWER GI SERIES / BARIUM
ENEMA
- Preparation for the test ULTRASOUND OF THE
includes: ABDOMEN, LIVER, GALL
NPO for 6 to 8 hours BLADDER & PANCREAS
Laxative the night - NPO for 8-12 hours
before the procedure - Laxative the night before the
Cleansing enema in test
the morning of the HEPATO-BILIARY AND PANCREATIC
test SYSTEM
LIVER BIOPSY GLYCOSYLATED HEMOGLOBIN /
- Vitamin K injection prior the HGBA1C
procedure if PT is prolonged - The most accurate indicator
- During procedure: left lateral of diabetes mellitus
position - Reflects glucose levels for
- Instruct to exhale deeply, the past 3-4 months
hold breath for 5 – 10
seconds during needle Thyroid Function test:T3, T4 and
insertion RAIU(Radioactive Iodine Uptake)
- Post procedure: right side - Increased in hyperthyroidism
lying for 4 hours - Decreased in hypothyroidism
PARACENTESIS THYROID SCAN
- Check vital signs - Helps determine whether the
- Empty bladder prior to tumor is benign or malignant
procedure
- Place in upright or sitting FINE NEEDLE BIOPSY
position - Is done to confirm
- Post procedure: monitor for malignancy
hypovolemic shock &
peritonitis VANILLYLMANDELIC ACID (VMA)
TEST
ENDOSCOPIC RETROGRADE - Done to detect
CHOLANGIOPANCREATOGRAPH pheochromocytoma
Y (ERCP) - VMA is the metabolite of
- ERCP is a procedure that epinephrine
enables your physician to - 24-hour urine specimen
examine the pancreatic and - Avoid in 24H: coffee, tea,
bile ducts. chocolate, banana, vanilla &
- Involves upper GI endoscopy aspirin
for contrast medium - Elevated:
- Assess allergy to seafood & pheochromocytoma – a
iodine tumor in the adrenal medulla
- Post procedure: NPO until
gag reflex returns & turn to GENITO-UNRINARY SYSTEM
sides
ROUTINE URINALYSIS
- Collect in the morning upon
ULTRASOUND OF THE GALL
awakening
BLADDER
- Cleanse external genitals
- The most Definitive test to
with soap & water
detect gallstones.
- Discard the first flow of urine,
ENDOCRINE SYSTEM collect the midstream, then
discard the last flow
- Label properly & send Permits better
immediately to labs transmission of high
frequency sound
24 – HOUR URINE COLLECTION (ultrasound)
- Discard the first voided urine
- Collect specimen thereafter RENAL BIOPSY
- Include the last voided - Check coagulation studies
specimen - Placed in prone position
- If a specimen was discarded, - Post procedure: placed in
restart the collection the supine with small pillow or
following day rolled towel under the
posterior lumbar area
CREATININE CLEARANCE
- Best indicator of glomerular NERVOUS SYSTEM
function
CAT SCAN
- Requires 24-H urine
- Assess for allergy to seafood
specimen collection
& iodine (if done with
- Low: renal function
contrast medium)
impairment
- Assess for claustrophobia
- Remove metallic items from
KUB
hair
- Plain Xray of the kidneys,
Ureters & bladder
ELECTROENCEPHALOGRAPHY
- Laxative is administered the
(EEG)
night before
- Provide hair shampoo prior
to procedure
INTRAVENOUS PYELOGRAM - Avoid caffeine,
(IVP) / EXCRETORY UROGRAM anticonvulsants, & stimulants
- An x-ray examination of the for at least 24 hours prior to
kidneys, ureters and urinary procedure
bladder that uses iodinated
contrast material injected into
ELECTROMYOGRAPHY (EMG) &
veins.
NERVE CONDUCTION VELOCITY
- Assess allergy to seafood
(NCV)
and iodine
- Done to diagnose
- Administer laxative
neuromuscular disorders
- Dangerous Complication:
- Electrode needles will be
Anaphylactic Shock
inserted into the muscle with
mild discomfort
ULTRASOUND OF THE KIDNEYS,
URETERS, BLADDER
LUMBAR PUNCTURE
- Distend the bladder by giving
- Placed in lateral, knee-chest
2 glasses of water
position
- Instruct to withhold voiding
- Label specimen - Denominator indicates
- Post procedure: placed in flat distance at which the normal
position for 6-8 hours to eye can read letters
prevent spinal headache - 20/200 means legal
- Spinal headache is due to blindness
leakage of CSF thru the dural - 20/30 or greater means
hole. myopia/nearsightedness
- 20/15 or less means
MYELOGRAPHY hyperopia /farsightedness
- Detects vertebral disk
diseases & spinal cord TONOMETRY
tumors - Indirectly measures
- Contrast medium is intraocular pressure (IOP)
administered thru lumbar - 25 mmHg & above means
puncture glaucoma
MAGNETIC RESONANCE OPTHALMOSCOPY
IMAGING (MRI) - Examines the fundus, interior
- Obtain history of metal of the eyes
implants & artificial cardiac - May diagnose retinal
pacemaker detachment & papilledema /
- Assess for claustrophobia choked disk
- Drum-like or knocking sound
TUNING FORK TESTS
MUSCULOSKELETAL SYSTEM RINNE’S TEST
BONE X-RAY o Compares air
- To detect bone fracture conduction from bone
conduction
BONE SCAN o Vibrating tuning fork
- Instruct client to void is placed against the
immediately prior to mastoid process
procedure to prevent irritation (behind the ear) then
of the bladder by 2 inches from the
radioisotope opening of the ear
canal
EYES AND EARS o Valuable in the
diagnosis of
SNELLEN’S TEST otosclerosis,
- Tests visual acuity conductive hearing
- Normal result 20/20 loss
- Numerator indicates distance RINNE’S TEST FINDINGS
of the client from the chart - Normal: air
conduction is better
than bone conduction
-
Conductive hearing
loss: bone conduction
is better than air
conduction
- Sensorineural hearing
loss: result is the
same as normal
result
WEBER TEST
- The rounded tip of the
handle of vibrating
tuning fork is placed
in the center of the
client’s head
- Valuable in the
diagnosis of
Meniere’s Disease,
sensorineural hearing
loss
WEBER TEST FINDINGS
- Normal: tone is
perceived in the
center of the clent’s
head or equally in
both ears
- Conductive Hearing
loss: tone is heard
better in the poor ear
- Sensorineural hearing
loss: tone is heard
better in the good ear
AUDIOMETRY
- Single most important
diagnostic test in detecting
hearing loss
- May be pure tone or speech
audiometry
- Critical level of loudness is
30 decibels
You might also like
- High Sensitivity CRP - IMMULITE and IMMULITE 1000 - Rev 06 DXDCM 09017fe980297730-1538194293759Document36 pagesHigh Sensitivity CRP - IMMULITE and IMMULITE 1000 - Rev 06 DXDCM 09017fe980297730-1538194293759Deqsa Corporativo0% (1)
- NCM 118L/ 119L (Related Learning Experience) Day 3-ActivityDocument4 pagesNCM 118L/ 119L (Related Learning Experience) Day 3-ActivityNicole Villanueva, BSN - Level 3ANo ratings yet
- Waiters Postpartal Hemorrhage PDFDocument1 pageWaiters Postpartal Hemorrhage PDFmp1757No ratings yet
- HiPath Xpressions Compact V3.0 Installation Administration GuideDocument194 pagesHiPath Xpressions Compact V3.0 Installation Administration GuideenjoythedocsNo ratings yet
- File: Chapter 03 - Consolidations - Subsequent To The Date of Acquisition Multiple ChoiceDocument58 pagesFile: Chapter 03 - Consolidations - Subsequent To The Date of Acquisition Multiple Choicejana ayoubNo ratings yet
- Project An Monitoring Tool 1Document3 pagesProject An Monitoring Tool 1Rames Ely GJ100% (2)
- Unit 8Document3 pagesUnit 804Cabanting, Mark Louie G.No ratings yet
- Chem123 Lab Phlebotomy-FinalsDocument6 pagesChem123 Lab Phlebotomy-Finalssaculala0291pamNo ratings yet
- Acute Kidney Injury W/ Hyperkalemia NCPDocument5 pagesAcute Kidney Injury W/ Hyperkalemia NCPMyrvic Ortiz La OrdenNo ratings yet
- A Case Presentation On Viral Pneumonia: Sr. Saraswati RoyDocument29 pagesA Case Presentation On Viral Pneumonia: Sr. Saraswati RoyjyotiangelNo ratings yet
- Ct7 Fluid, Electrolyte ImbalanceDocument9 pagesCt7 Fluid, Electrolyte ImbalanceAlondra VelascoNo ratings yet
- NCP TableDocument6 pagesNCP TableShivani SrivastavaNo ratings yet
- NCM-112 Midterms BATCH 2023 College of Nursing-Adamson UniversityDocument13 pagesNCM-112 Midterms BATCH 2023 College of Nursing-Adamson UniversityjoanneNo ratings yet
- Ctni/Ck-Mb/Myo/D-D/Nt-Probnp Rapid Quantitative Test: Intended Use Storage and StabilityDocument2 pagesCtni/Ck-Mb/Myo/D-D/Nt-Probnp Rapid Quantitative Test: Intended Use Storage and StabilityTrần Thanh ViệnNo ratings yet
- AnesthesiaDocument8 pagesAnesthesiaYavani KulasinghamNo ratings yet
- Trauma: HX and PE (Adults) : For The EMS Providers, (Prior To Patient'sDocument3 pagesTrauma: HX and PE (Adults) : For The EMS Providers, (Prior To Patient'sJustine CastilloNo ratings yet
- MKSAP Questions: Intern ReportDocument37 pagesMKSAP Questions: Intern Reportfidelurtecho4881No ratings yet
- Diagnostic and Laboratory ExaminationsDocument19 pagesDiagnostic and Laboratory Examinationsgeng gengNo ratings yet
- Basic Laboratory InvestigationsDocument65 pagesBasic Laboratory InvestigationsMadhan PrabhuNo ratings yet
- Advanced Cardiovascular Life SupportDocument43 pagesAdvanced Cardiovascular Life SupportGeraldine Marie SalvoNo ratings yet
- 05.monitoring Hemodinamik AG SHANGRILLA SBY 2018Document65 pages05.monitoring Hemodinamik AG SHANGRILLA SBY 2018syafeiNo ratings yet
- The Acutely Ill Patient: Key InvestigationsDocument300 pagesThe Acutely Ill Patient: Key Investigationsjames.a.blairNo ratings yet
- Monitoring Intra Operatif: Mindi Widayani NRP 122.022.1115 FK UPN "Veteran" JakartaDocument21 pagesMonitoring Intra Operatif: Mindi Widayani NRP 122.022.1115 FK UPN "Veteran" Jakartaputri wulandariNo ratings yet
- Preop Conference AnesthesiaDocument33 pagesPreop Conference AnesthesiaBhi-An BatobalonosNo ratings yet
- NCP - PreeclampsiaDocument3 pagesNCP - PreeclampsiaRap De la Cruz50% (2)
- 9 - Role of Non InvasiveDocument46 pages9 - Role of Non InvasiveHavara Kausar AkbarNo ratings yet
- 2nd - NCPDocument3 pages2nd - NCPjoidaNo ratings yet
- Acs - 12.01.2022Document41 pagesAcs - 12.01.2022SabariNo ratings yet
- Risk For IneffectiveDocument6 pagesRisk For IneffectiveAce FabrigasNo ratings yet
- Acute Respiratory Failure Type Ii, Cap HR: de La Salle Health Sciences Institute College of Nursing Nursing Case PlanDocument9 pagesAcute Respiratory Failure Type Ii, Cap HR: de La Salle Health Sciences Institute College of Nursing Nursing Case PlanLuigi ArenasNo ratings yet
- ECMO Monitoring - PediatrikDocument24 pagesECMO Monitoring - PediatrikIsran IsRanNo ratings yet
- COVID19 Hospitalized Requiring Treatment Diagnostic NotesDocument2 pagesCOVID19 Hospitalized Requiring Treatment Diagnostic NotesYazid HimeurNo ratings yet
- Respiratory Term 2Document13 pagesRespiratory Term 2Abegail QuintoNo ratings yet
- Week - 7 Rle 312Document5 pagesWeek - 7 Rle 312VAL ASHLIE ACEBARNo ratings yet
- Selective B2-Adrenergic Agonists:: Mode of ActionDocument9 pagesSelective B2-Adrenergic Agonists:: Mode of ActionAda JoraimiNo ratings yet
- Golden Period Septic ChildDocument32 pagesGolden Period Septic ChildcallNo ratings yet
- Appendix A Nursing Management TablesDocument27 pagesAppendix A Nursing Management Tablesba.ramirez11No ratings yet
- Preoperative AssessmentDocument2 pagesPreoperative AssessmentTom MallinsonNo ratings yet
- Aldrette Score (Nitasha Best) (Discharge Criteria From Pacu)Document72 pagesAldrette Score (Nitasha Best) (Discharge Criteria From Pacu)Parvathy R NairNo ratings yet
- Cu 7Document6 pagesCu 7VALERIANO TRISHANo ratings yet
- Cerebrospinal Fluid LectureDocument5 pagesCerebrospinal Fluid LectureColene MoresNo ratings yet
- NCPDocument2 pagesNCPJulianne MagtunaoNo ratings yet
- Urinary Infection Care PlanDocument2 pagesUrinary Infection Care PlanmysterioushumaneNo ratings yet
- Nursing Care Plan (Bronchiectasis)Document4 pagesNursing Care Plan (Bronchiectasis)Leah QuiñanolaNo ratings yet
- Trans PMLS 1 - Batch 2 and 3.Document23 pagesTrans PMLS 1 - Batch 2 and 3.leexxjannelapatNo ratings yet
- Sedation For Icu Patients PresentationDocument8 pagesSedation For Icu Patients Presentationapi-736869233No ratings yet
- Homologous Blood Trasfusion Practice ShortsDocument23 pagesHomologous Blood Trasfusion Practice ShortsdrprasadingleyNo ratings yet
- Cerebrospinal Fluid - AUBFDocument9 pagesCerebrospinal Fluid - AUBFMitch IbayNo ratings yet
- Laboratory Examinations: Allen's Test Normal Finding: Hand Quickly BecomesDocument9 pagesLaboratory Examinations: Allen's Test Normal Finding: Hand Quickly BecomesShane GumaponNo ratings yet
- Diving Medical CertificateDocument2 pagesDiving Medical Certificatesuarti ningsihNo ratings yet
- Compiled High Yield Questions and Recalls For Board ExamDocument48 pagesCompiled High Yield Questions and Recalls For Board Examqnx6696m7fNo ratings yet
- Complex Care Concept MapDocument6 pagesComplex Care Concept Mapapi-740628337No ratings yet
- Cme: Dengue Fever: by Nur ShafikaDocument47 pagesCme: Dengue Fever: by Nur ShafikaSyuk IdhamNo ratings yet
- Pcol 2 PrelimsDocument6 pagesPcol 2 PrelimsMa. Andrea Julie AcasoNo ratings yet
- Nursing Care Management of Systematic Lupus ErythematosusDocument53 pagesNursing Care Management of Systematic Lupus ErythematosusDana Marie LeanoNo ratings yet
- 林奕廷 - perioperative management of TSSDocument15 pages林奕廷 - perioperative management of TSS林奕廷No ratings yet
- Esai EMDocument3 pagesEsai EMAdelia Putri WirandaniNo ratings yet
- Pulmonary EmbolismDocument2 pagesPulmonary EmbolismAnjana BasilNo ratings yet
- Acute Chest SyndromeDocument28 pagesAcute Chest SyndromeJohn OkidiNo ratings yet
- Contora, Isah TblrenalDocument7 pagesContora, Isah TblrenalisahNo ratings yet
- 3Document6 pages3Amjad SaudNo ratings yet
- Pneumonia Case StudyDocument8 pagesPneumonia Case StudyAlin Dragos100% (1)
- SLEEPDocument13 pagesSLEEPCrazy StrangerNo ratings yet
- HYGIENEDocument6 pagesHYGIENECrazy StrangerNo ratings yet
- Monitoring and Measuring Intake and OutputDocument2 pagesMonitoring and Measuring Intake and OutputCrazy StrangerNo ratings yet
- Fecal EliminationDocument13 pagesFecal EliminationCrazy StrangerNo ratings yet
- Implenting and EvaluationDocument2 pagesImplenting and EvaluationCrazy StrangerNo ratings yet
- PLANNINGDocument3 pagesPLANNINGCrazy StrangerNo ratings yet
- Callista RoyDocument2 pagesCallista RoyCrazy StrangerNo ratings yet
- ASSESSINGDocument3 pagesASSESSINGCrazy StrangerNo ratings yet
- Margaret Newman and Rosemarie Rizzo-ParseDocument2 pagesMargaret Newman and Rosemarie Rizzo-ParseCrazy StrangerNo ratings yet
- Jean WatsonDocument1 pageJean WatsonCrazy StrangerNo ratings yet
- Lydia HallDocument1 pageLydia HallCrazy StrangerNo ratings yet
- TissuesDocument6 pagesTissuesCrazy StrangerNo ratings yet
- Respiratory SystemDocument7 pagesRespiratory SystemCrazy StrangerNo ratings yet
- Dorothy JohnsonDocument2 pagesDorothy JohnsonCrazy StrangerNo ratings yet
- Imogen KingDocument1 pageImogen KingCrazy StrangerNo ratings yet
- Female Reproductive SystemDocument7 pagesFemale Reproductive SystemCrazy StrangerNo ratings yet
- 099CYUT5512017 001卵礫石Document212 pages099CYUT5512017 001卵礫石ruizhou04 wuNo ratings yet
- CTEKS 12-14 X 50 HGSDocument2 pagesCTEKS 12-14 X 50 HGSPT SHS Garasi GempolNo ratings yet
- Pressure Vessel Plates, Alloy Steel, High-Strength, Quenched and TemperedDocument3 pagesPressure Vessel Plates, Alloy Steel, High-Strength, Quenched and TemperedRoland CepedaNo ratings yet
- Adolescent Development and Teaching Reflection - CDocument2 pagesAdolescent Development and Teaching Reflection - Capi-374467245No ratings yet
- What Is Code-Switching? Language AlternationDocument35 pagesWhat Is Code-Switching? Language AlternationCao hảiNo ratings yet
- Report (Sculpture Materials)Document32 pagesReport (Sculpture Materials)triziasisonNo ratings yet
- OSB Error HandlingDocument45 pagesOSB Error Handlingabhishek_acharya_13100% (1)
- What If Everyone Were: The Same?Document9 pagesWhat If Everyone Were: The Same?Eddie FongNo ratings yet
- CompanyDocument2 pagesCompanyhusse fokNo ratings yet
- Divisional Public School & College Faisalabad: Class: XDocument2 pagesDivisional Public School & College Faisalabad: Class: XMubashra RazaNo ratings yet
- The Impact of Organizational Justice On Employee's Job Satisfaction: The Malaysian Companies PerspectivesDocument8 pagesThe Impact of Organizational Justice On Employee's Job Satisfaction: The Malaysian Companies PerspectivesNaim NordinNo ratings yet
- K12 - CC - Catalog - 2013-2014 LouisianaDocument34 pagesK12 - CC - Catalog - 2013-2014 LouisianaElizabeth KahnNo ratings yet
- Aspen Tree Art Lesson PlanDocument3 pagesAspen Tree Art Lesson Planapi-563439476No ratings yet
- Misusing Company TimeDocument9 pagesMisusing Company TimeMadakiwe NyashadzasheNo ratings yet
- Phys - Exam - May 2014-ZagazigDocument8 pagesPhys - Exam - May 2014-ZagazigWael ElsawyNo ratings yet
- Abstract The History and Principles of Trauma-Informed Practice in Social WorkDocument20 pagesAbstract The History and Principles of Trauma-Informed Practice in Social WorkHany A Aziz100% (1)
- Minolta Ep4000Document392 pagesMinolta Ep4000kostas_san50% (2)
- Estelle DarcyDocument1 pageEstelle DarcyTasnim Ben AmmarNo ratings yet
- OverviewDocument346 pagesOverviewarnaldospbrNo ratings yet
- Nitrogrn - Gate Valve Data SheetDocument2 pagesNitrogrn - Gate Valve Data SheetHabib ur rahmanNo ratings yet
- Monday Tuesday Wednesday Thursday Friday: GRADES 1 To 12 Daily Lesson LogDocument7 pagesMonday Tuesday Wednesday Thursday Friday: GRADES 1 To 12 Daily Lesson LogKatrina Baldas Kew-isNo ratings yet
- Eposter For Art & Science of Patient PreparationDocument50 pagesEposter For Art & Science of Patient PreparationdrsmritiNo ratings yet
- Shaibu Amana DavidDocument44 pagesShaibu Amana DavidEsauNo ratings yet
- 4058 - Bunnings Store Map - Canberra Airport ACT 4058 - PFO - WebDocument2 pages4058 - Bunnings Store Map - Canberra Airport ACT 4058 - PFO - WebplaywellmusicNo ratings yet
- G59 Control PanelDocument2 pagesG59 Control PanelKiliardt ScmidtNo ratings yet