Professional Documents
Culture Documents
Stigma-Discrimination Complex Associated With Major Depressive Disorder
Stigma-Discrimination Complex Associated With Major Depressive Disorder
Uploaded by
Maria CamilaCopyright:
Available Formats
You might also like
- PESCI Recalls PDFDocument9 pagesPESCI Recalls PDFDanishNo ratings yet
- Essentials of Psychiatric Mental Health Nursing 7th Edition Townsend Test BankDocument15 pagesEssentials of Psychiatric Mental Health Nursing 7th Edition Townsend Test Bankkimberlymorriscntsoqmyjw100% (6)
- BIPOLAR - Mood Thermometer With Monitoring CardDocument6 pagesBIPOLAR - Mood Thermometer With Monitoring Cardathina karavolNo ratings yet
- Kessler 2005Document11 pagesKessler 2005mccg1478No ratings yet
- Behavioral Science Practice QuestionsDocument52 pagesBehavioral Science Practice QuestionsUsman KhanNo ratings yet
- Ajol File Journals - 75 - Articles - 155877 - Submission - Proof - 155877 889 406908 1 10 20170511Document6 pagesAjol File Journals - 75 - Articles - 155877 - Submission - Proof - 155877 889 406908 1 10 20170511Reni Tri AstutiNo ratings yet
- 1 s2.0 S2405844022012002 MainDocument16 pages1 s2.0 S2405844022012002 MainMythiliNo ratings yet
- Research Letter: Risk of Depression Among Patients With Acne in The U.K.: A Population-Based Cohort StudyDocument2 pagesResearch Letter: Risk of Depression Among Patients With Acne in The U.K.: A Population-Based Cohort StudyadhastriNo ratings yet
- An In-Depth Analysis of Machine Learning Approaches To Predict DepressionDocument12 pagesAn In-Depth Analysis of Machine Learning Approaches To Predict DepressionDilshan SonnadaraNo ratings yet
- A Study On Prevalence and Correlates of Depression Among Elderly Population of Rural South IndiaDocument4 pagesA Study On Prevalence and Correlates of Depression Among Elderly Population of Rural South Indiariska matokaNo ratings yet
- Journal of Affective Disorders ReportsDocument8 pagesJournal of Affective Disorders ReportsBAISHA BARETENo ratings yet
- Researching The Cultural Reaction On Mental Ill PatientsDocument8 pagesResearching The Cultural Reaction On Mental Ill Patientsmail9967No ratings yet
- Journal of Affective Disorders ReportsDocument10 pagesJournal of Affective Disorders ReportsAnnisa NurainiNo ratings yet
- Prevalence and Heritability of Body Dysmorphic Symptoms in Adolescents and Young Adults: A Population-Based Nationwide Twin StudyDocument8 pagesPrevalence and Heritability of Body Dysmorphic Symptoms in Adolescents and Young Adults: A Population-Based Nationwide Twin StudyCAMILLE HAMNo ratings yet
- Prevalence of Personality Disorders in The General Adult Population in Western Countries Systematic Review and Meta AnalysisDocument7 pagesPrevalence of Personality Disorders in The General Adult Population in Western Countries Systematic Review and Meta AnalysisFavio AndradeNo ratings yet
- Prevalence and Predictors of Depression Amongst ElderlyDocument4 pagesPrevalence and Predictors of Depression Amongst ElderlyDr.Wajid Habib (Doxxsab)No ratings yet
- 2018 Gemelos TDC y Heredabilidad DCQDocument8 pages2018 Gemelos TDC y Heredabilidad DCQIndiraNo ratings yet
- Assessment of Depression Among Older AdultsDocument9 pagesAssessment of Depression Among Older Adultsrani nauraNo ratings yet
- Admin, Ora 12 Ijnms 1921 Article 2 DeeptiDocument5 pagesAdmin, Ora 12 Ijnms 1921 Article 2 DeeptiPrinka PathaniaNo ratings yet
- Falls in The Elderly - SazlinaDocument6 pagesFalls in The Elderly - SazlinaKrishnanNo ratings yet
- DownDocument43 pagesDownAndrea LópezNo ratings yet
- Stigmatisation of People With Mental Illnesses Stigmatisation of People With Mental IllnessesDocument5 pagesStigmatisation of People With Mental Illnesses Stigmatisation of People With Mental Illnessessri endriyaniNo ratings yet
- Journal of Affective Disorders: Research PaperDocument6 pagesJournal of Affective Disorders: Research PaperjhuNo ratings yet
- Senior Seminar PaperDocument36 pagesSenior Seminar PaperKadiah KamaraNo ratings yet
- Does Loneliness Contribute To Mild Cognitive Impairment and DementiaDocument10 pagesDoes Loneliness Contribute To Mild Cognitive Impairment and Dementiamadalena limaNo ratings yet
- Major Depressive Disorder. NatureDocument20 pagesMajor Depressive Disorder. NatureMANUEL ALCIDES PUERTA BARRETO100% (1)
- Rajiv Gandhi University of Health Sciences, Bangalore, Karnataka Proforma For Registration of Subject For DissertationDocument16 pagesRajiv Gandhi University of Health Sciences, Bangalore, Karnataka Proforma For Registration of Subject For DissertationAngel SethNo ratings yet
- Research and Treatment Approaches To Depression: Cite This PaperDocument10 pagesResearch and Treatment Approaches To Depression: Cite This PaperSnehaNo ratings yet
- Suicide-Specific Mortality Amo 2Document12 pagesSuicide-Specific Mortality Amo 2I AM xbananaxNo ratings yet
- The Side Effects of Sick Leave Are PsychDocument33 pagesThe Side Effects of Sick Leave Are PsychthefrankoneNo ratings yet
- The Presence of Behavioural and Psychological Symptoms and Progression To Dementia in The Cognitively Impaired Older PopulationDocument11 pagesThe Presence of Behavioural and Psychological Symptoms and Progression To Dementia in The Cognitively Impaired Older PopulationCeci_SunshineNo ratings yet
- Borderline Personality Disorder in The Elderly. Valdivieso (2018)Document5 pagesBorderline Personality Disorder in The Elderly. Valdivieso (2018)pasandy.jrNo ratings yet
- Póster INNS 2020 Urazan J. C.Document1 pagePóster INNS 2020 Urazan J. C.jcurazanNo ratings yet
- A Study To Assess of Knowledge and Perception of Women Regarding Premenstrual Dysphoric Disorder and Its Impact On Daily Routine WorkDocument3 pagesA Study To Assess of Knowledge and Perception of Women Regarding Premenstrual Dysphoric Disorder and Its Impact On Daily Routine WorkInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Depression Research Paper PDFDocument8 pagesDepression Research Paper PDFgz9g97ha100% (1)
- Overview of Generalized Anxiety DisorderDocument6 pagesOverview of Generalized Anxiety Disordernandaas887No ratings yet
- Perceived Stress and Mild Cognitive Impairment Among 32,715 Community-Dwelling Older Adults Across Six Low-And Middle-Income CountriesDocument9 pagesPerceived Stress and Mild Cognitive Impairment Among 32,715 Community-Dwelling Older Adults Across Six Low-And Middle-Income CountriesIshani SharmaNo ratings yet
- Prevalencia de Dementcia PDFDocument15 pagesPrevalencia de Dementcia PDFdanielaNo ratings yet
- B MJ Sedgwick Cross Sectional StudiesDocument3 pagesB MJ Sedgwick Cross Sectional StudiesSaurabh MundadaNo ratings yet
- OH Honlap Felveteli Eredmenyek Gyorsstat 20180208Document2 pagesOH Honlap Felveteli Eredmenyek Gyorsstat 20180208LPATI12No ratings yet
- Estimate of Dementia PrevalenceDocument10 pagesEstimate of Dementia Prevalenceaxl___No ratings yet
- 2017 Grace Y. Lim Prevalence of Depression in The Community From 30 Countries Between 1994 and 2014Document10 pages2017 Grace Y. Lim Prevalence of Depression in The Community From 30 Countries Between 1994 and 2014adni halianieNo ratings yet
- Music and DepressionDocument6 pagesMusic and DepressiongabrielavlahopolNo ratings yet
- Major Depressive Disorder and Difference Between Genders: Dzevad Sabic, Adela Sabic, Amila Bacic-BecirovicDocument4 pagesMajor Depressive Disorder and Difference Between Genders: Dzevad Sabic, Adela Sabic, Amila Bacic-BecirovicDzevad SabicNo ratings yet
- Due Dec 3 - Mini CogDocument2 pagesDue Dec 3 - Mini Cogchuckydoll1989No ratings yet
- Gender and Social Mental HealthDocument17 pagesGender and Social Mental HealthMiEtaineNo ratings yet
- 1 s2.0 S0747563219303425 MainDocument6 pages1 s2.0 S0747563219303425 MainSAFWA BATOOL NAQVINo ratings yet
- Characterization by Gender of Frailty SyDocument12 pagesCharacterization by Gender of Frailty SygianellaNo ratings yet
- Identifying Depression On Twitter: Moin Nadeem, Mike Horn., Glen Coppersmith, PHD, University ofDocument9 pagesIdentifying Depression On Twitter: Moin Nadeem, Mike Horn., Glen Coppersmith, PHD, University ofAnanya SaikiaNo ratings yet
- Diferencias Entre Depresión Crónica y No Crónica Revisión Sistemática e Implicaciones para El TratamientoDocument13 pagesDiferencias Entre Depresión Crónica y No Crónica Revisión Sistemática e Implicaciones para El TratamientoIVAN ALVAREZNo ratings yet
- Positive Traits in The Bipolar Spectrum: The Space Between Madness and GeniusDocument15 pagesPositive Traits in The Bipolar Spectrum: The Space Between Madness and GeniusVinícius BranquinhoNo ratings yet
- Repensando Depresion Con Los RcDOCS 2023Document16 pagesRepensando Depresion Con Los RcDOCS 2023Psiquiatria Clinica ProyectarteNo ratings yet
- Anxiety-Depressive Disorders in The General Population During A Period of Confinement in MoroccoDocument9 pagesAnxiety-Depressive Disorders in The General Population During A Period of Confinement in MoroccoIJAR JOURNALNo ratings yet
- Neurology, Psychiatry and Brain Research: B.A. Pramesona, S. TaneepanichskulDocument6 pagesNeurology, Psychiatry and Brain Research: B.A. Pramesona, S. TaneepanichskulMutiara Anak NegeriNo ratings yet
- Jamapsychiatry Ruscio 2017 Oi 170004Document11 pagesJamapsychiatry Ruscio 2017 Oi 170004Koas aningNo ratings yet
- 2022 DCQ en Gemelos Suecia TDC y SuicidioDocument9 pages2022 DCQ en Gemelos Suecia TDC y SuicidioIndiraNo ratings yet
- Depression and Genes 99Document12 pagesDepression and Genes 99Rayan BotanyNo ratings yet
- Depreesion PredictionDocument11 pagesDepreesion PredictionYunitaYunitaRahmaNo ratings yet
- Lehtinen 1994Document4 pagesLehtinen 1994HARINI KNo ratings yet
- DepressionDocument16 pagesDepressionLEONARDO ANTONIO CASTILLO ZEGARRA100% (1)
- Brasil, Campeão Mundial de DepressãoDocument16 pagesBrasil, Campeão Mundial de DepressãoValéria AlmeidaNo ratings yet
- Polygenic Risk Scores Derived From Varying DefinitionsDocument9 pagesPolygenic Risk Scores Derived From Varying DefinitionsFelipe Neira DíazNo ratings yet
- Struggling Striving Surviving: Living with Borderline Personality DisorderFrom EverandStruggling Striving Surviving: Living with Borderline Personality DisorderNo ratings yet
- Depression Among Teenagers in Trinidad and TobagoDocument16 pagesDepression Among Teenagers in Trinidad and TobagoLori-Ann JacobsNo ratings yet
- Cala Component CDocument4 pagesCala Component CSancho KanyamaNo ratings yet
- Chapter 4 ResearchDocument11 pagesChapter 4 Researchsunshinemauricio1No ratings yet
- Depresion in The ElderlyDocument9 pagesDepresion in The ElderlyGuzman RubenNo ratings yet
- Written Report - Mental HealthDocument2 pagesWritten Report - Mental HealthJonalyn SalvateraNo ratings yet
- Helping Students Manage Emotions - REBT As A Mental Health Educational CurriculumDocument13 pagesHelping Students Manage Emotions - REBT As A Mental Health Educational CurriculumDalila VicenteNo ratings yet
- Geri Assess Tools ArticleDocument9 pagesGeri Assess Tools ArticleThesmith FamNo ratings yet
- Introduction, ROL (Aayushi Pillai)Document7 pagesIntroduction, ROL (Aayushi Pillai)Aayushi PillaiNo ratings yet
- Psychiatry Reporting - Classification in PsychiatryDocument13 pagesPsychiatry Reporting - Classification in PsychiatryJyl Yan SelasorNo ratings yet
- Music TherapyDocument16 pagesMusic TherapyJFFNo ratings yet
- Sample QuestionsDocument19 pagesSample Questionsjeallynasala02No ratings yet
- B-Complex Vitamins - Benefits, Side Effects and DosageDocument11 pagesB-Complex Vitamins - Benefits, Side Effects and DosageMohammed shamiul Shahid100% (1)
- Ots 1990Document38 pagesOts 1990Lau PalermoNo ratings yet
- E.1 Depression PowerPoint 20151Document38 pagesE.1 Depression PowerPoint 20151Ptrc Lbr LpNo ratings yet
- Article SCL 10Document21 pagesArticle SCL 10Erlina RatmayantiNo ratings yet
- Vagal Nerve Stimulation For Treatment Resistant DepressionDocument14 pagesVagal Nerve Stimulation For Treatment Resistant DepressionCTAFDocuments100% (1)
- Prevention and Treatment of Systemic Glucocorticoid Side EffectsDocument10 pagesPrevention and Treatment of Systemic Glucocorticoid Side EffectsMahmoud DiaaNo ratings yet
- Depresión (Dos Semanas)Document3 pagesDepresión (Dos Semanas)AcdaNo ratings yet
- Yoga and Counseling ExperienceDocument7 pagesYoga and Counseling ExperienceWilliamArugaNo ratings yet
- Electroconvulsive Therapy Ect FormDocument5 pagesElectroconvulsive Therapy Ect FormRoshita G PillaiNo ratings yet
- MentalHealthIssuesCOVID 19NIMHANSDocument177 pagesMentalHealthIssuesCOVID 19NIMHANSYanti HarjonoNo ratings yet
- Lewinsohn 1975Document3 pagesLewinsohn 1975serenadenightNo ratings yet
- A Study of Depression and Anxiety in Cancer Patients PDFDocument34 pagesA Study of Depression and Anxiety in Cancer Patients PDFIrdha Nasta KurniaNo ratings yet
- Listing of DSM-5 Diagnoses and New ICD-10-CM Codes: As Ordered in The DSM-5 ClassificationDocument2 pagesListing of DSM-5 Diagnoses and New ICD-10-CM Codes: As Ordered in The DSM-5 ClassificationFitria Ning RositaNo ratings yet
- Ambient PM2.5 Caused Depressive-Like Responses Through Nrf2NLRP3 Signaling Pathway Modulating InflammationDocument11 pagesAmbient PM2.5 Caused Depressive-Like Responses Through Nrf2NLRP3 Signaling Pathway Modulating InflammationNNo ratings yet
- The Application of Cognitive Behaviour Therapy (CBT) For Depression: A Case Study of Iranian FemaleDocument8 pagesThe Application of Cognitive Behaviour Therapy (CBT) For Depression: A Case Study of Iranian FemaleHanilah RamliNo ratings yet
Stigma-Discrimination Complex Associated With Major Depressive Disorder
Stigma-Discrimination Complex Associated With Major Depressive Disorder
Uploaded by
Maria CamilaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Stigma-Discrimination Complex Associated With Major Depressive Disorder
Stigma-Discrimination Complex Associated With Major Depressive Disorder
Uploaded by
Maria CamilaCopyright:
Available Formats
Rev. Fac. Med. 2019 Vol. 67 No.
4: 531-2 531
LETTER TO THE EDITOR
DOI: http://dx.doi.org/10.15446/revfacmed.v67n4.72529
Stigma-discrimination complex associated
with major depressive disorder
Complejo estigma-discriminación relacionado con el trastorno depresivo mayor
Received: 30/05/2018. Accepted: 12/08/2018.
Adalberto Campo-Arias1 • Edwin Herazo2 • Guillermo Augusto Ceballos-Ospino3
1
Universidad del Magdalena - Faculty of Health Sciences - Medical Program - Santa Marta - Colombia.
2
Instituto de Investigación del Comportamiento Humano - Director’s Office - Bogotá D.C. - Colombia.
3
Universidad del Magdalena - Faculty of Health Sciences - Psychology Program - Santa Marta - Colombia.
Corresponding author: Adalberto Campo-Arias. Programa de Medicina, Facultad de Ciencias de la Salud, Universidad del Magdalena. Carrera 32
No 22-08. Phone: +57 5 4381000, ext.: 1338. Santa Marta. Colombia. Email: acampoa@unimagdalena.edu.co.
Dear Editor: used in the search were “estigma hacia la depresión”, “estigma de la
depresión”, “estigma contra la depresión” and “escala de estigma
Throughout history, the stigma-discrimination complex (SDC) has relacionado con la depresión” (stigma towards depression, stigma of
been associated with serious mental disorders such as those on the depression, stigma against depression, and depression-related stigma
spectrum of schizophrenia, where symptoms, side effects and impaired scale). A descriptive analysis of identified research on the perception
social functioning are difficult to conceal. (1) For its part, SDC related component was carried out and, given the dimensional nature of
to major depressive disorder (MDD) is a growing phenomenon even the scale, the frequency of response of each item was analyzed
though its clinical characteristics are easy to hide or are less evident without considering the total score due to the lack of a cut-off point
in the social sphere (2,3); in these cases, said association may have to categorize high perceived SDC towards the MDD. (6)
more negative effects on people’s lives than the disorder itself. (4,5) Three studies showed the prevalence of SDC-MDD (perceived
Consequently, the Depression Stigma Scale (DSS) was designed stigma) with the use of DSS. The first study was Cook & Wang (7),
to quantify the relationship between SDC and MDD (SDC-MDD). who assessed SDC-MDD in 2 987 adults aged 18-74 years (51%
This is a Likert scale consisting of two subscales with nine items men); the second was Coppens et al. (8), which evaluated 4 011
each. The first addresses the issue of attitude towards people who adults aged 18 or over (45.8% male) from four European countries;
meet criteria for MDD, i.e. perceived stigma, and the second, the the third was Subramanian et al. (9), who researched SDC-MDD
anticipated attitude for MDD, i.e. personal stigma or self-stigma. (6) in 607 adults aged 18 to 65 (50.9% male). The three investigations
In order to know the prevalence of SDC-MDD (perceived stigma) found that between 3.2% and 89.4% (mean 30.7%) of the participants
among the general population, a review of original research works that agreed with at least one of the nine items suggestive of perceived
used the DSS was carried out between 2005 and 2017. The key words stigma (Table 1). (7-9)
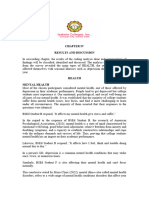
Table 1. Percentage of agreement for the scale items about stigma related to depression - perceived stigma.
Study Cook & Wang (7) Coppens et al. (8) Subramanian et al. (9)
Country
Item Canada Germany Hungary Ireland Portugal Singapore
People with depression could overcome it if they wanted to 17.0% 20.1% 60.4% 18.5% 42.4% 89.4%
Depression is a sign of weakness 9.8% 25.9% 46.0% 18.6% 33.3% 50.8%
Depression is not a real medical condition 8.5% 14.7% 27.8% 16.5% 25.8% 38.5%
People with depression are dangerous 21.5% 28.6% 35.3% 14.9% 35.5% 35.8%
It is best to avoid people with depression if you do not
3.2% 13.7% 20.3% 8.2% 24.6% 10.6%
want to get depressed
People with depression are unpredictable 45.9% 36.5% 46.2% 38.0% 70.0% 62.5%
If I were depressed, I wouldn't tell anyone 13.6% 25.2% 22.5% 21.1% 27.8% 20.4%
I wouldn't hire someone if I knew they'd been
22.1% 24.3% 17.1% 20.3% 9.2% 45.3%
depressed
I wouldn't vote for a politician if I knew s/he'd been
39.5% 41.3% 34.1% 30.3% 20.3% -
depressed
Source: Own elaboration.
532 Stigma and depressive disorder: 531-2
These findings suggest that about one third of the general population 5. Campo-Arias A, Oviedo HC, Herazo E. Estigma: barrera de acceso
has SDC-MDD at different degrees or levels, in other words, they a servicios en salud mental. Rev Colomb Psiquiatr. 2014;43(3):162-7.
have a negative attitude towards people who meet the MDD criteria. http://doi.org/f2tf2t.
In general, SDC represents a barrier to access to mental health 6. Griffiths KM, Christensen H, Jorm AF, Evans K, Groves C. Effect of
services (4) and reduces the likelihood of seeking help and adherence web-based depression literacy and cognitive-behavioural therapy inter-
to treatment plans (10-12), even more so if SDC-MDD is found in ventions on stigmatising attitudes to depression: Randomised controlled
trial. Br J Psychiatry. 2004;185:342-9. http://doi.org/c89xw7.
health professionals. (13,14)
SDC-MDD seems to be frequent, so new research is required to 7. Cook TM, Wang J. Descriptive epidemiology of stigma against depression
provide more information on the phenomenon and, based on it, take in a general population sample in Alberta. BMC Psychiatry. 2010;10:29.
http://doi.org/b5wv85.https://doi.org/10.1186/1471-244X-10-29.
effective actions for its reduction in different contexts and levels.
(15,16) 8. Coppens E, Van Audenhove C, Scheerder G, Arensman E, Coffey
C, Costa S, et al. Public attitudes toward depression and help-seeking
in four European countries baseline survey prior to the OSPI-Europe
Conflicts of interest intervention. J Affect Disord. 2013;150(2):320-9. http://doi.org/f47v8c.
None stated by the authors. 9. Subramaniam M, Abdin E, Picco L, Pang S, Shafie S, Vaingankar
JA, et al. Stigma towards people with mental disorders and its compo-
nents-a perspective from multi-ethnic Singapore. Epidemiol Psychiatr
Funding Sci. 2016;26(4):371-82. http://doi.org/gbpmjh.
10. Conner KO, Copeland VC, Grote NK, Koeske G, Rosen D, Rey-
This research was financially supported by Universidad del Magdalena
nolds CF, et al. Mental health treatment seeking among older adults
and Instituto de Investigación del Comportamiento Humano. with depression: the impact of stigma and race. Am J Geriat Psychiatry.
2010;18(6):531-43. http://doi.org/ftjkfb.
Acknowledgements 11. Picco L, Abdin E, Pang S, Vaingankar JA, Jeyagurunathan A, Chong
SA, et al. Association between recognition and help-seeking preferences
None stated by the authors. and stigma towards people with mental illness. Epidemiol Psychiatr Sci.
2018;27(1):84-93. http://doi.org/gctzmf.
References 12. Gulliver A, Griffiths KM, Christensen H. Perceived barriers and
facilitators to mental health help-seeking in young people: a systematic
1. Yap MB, Mackinnon A, Reavley N, Jorm AF. The measurement pro- review. BMC Psychiatry. 2010;10:113. http://doi.org/b246pr.
perties of stigmatizing attitudes towards mental disorders: Results from
13. Reavley NJ, Mackinnon AJ, Morgan AJ, Jorm AF. Stigmatising atti-
two community surveys. Int J Method Psychiatr Res. 2014;23(1):49-61.
tudes towards people with mental disorders: A comparison of Australian
http://doi.org/f53x8q. health professionals with the general community. Aust N Z J Psychiatry.
2. Aromaa E, Tolvanen A, Tuulari J, Wahlbeck K. Predictors of stigmati- 2014;48(5):433-41. http://doi.org/c8qw.
zing attitudes towards people with mental disorders in a general population 14. Roja-Vistorte AO, Silva-Ribeiro W, Jaen D, Jorge MR, Evans-Lasko
in Finland. Nord J Psychiatry. 2011;65(2):125-32. http://doi.org/ddtw9c. S, Mari JJ. Stigmatizing attitudes of primary care professionals towards
3. Dietrich S, Mergl R, Rummel-Kluge C. Personal and perceived stigma- people with mental disorders: a systematic review. Int J Psychiatr Med.
tization of depression: A comparison of data from the general population, 2018;53(4):317-38. http://doi.org/c8qz.
participants of a depression congress and job placement officers in 15. Finkelstein J, Lapshin O. Reducing depression stigma using a web-based
Germany. Psychiatry Res. 2014;220(1-2):598-603. http://doi.org/f6q2sg. program. Int J Med Inform. 2007;76(10):726-34. http://doi.org/cgczkb.
4. Simmons LA, Yang NY, Wu Q, Bush HM, Crofford LJ. Public and 16. Quinn N, Knifton L, Goldie I, Van Bortel T, Dowds J, Lasalvia A, et
personal depression stigma in a rural American female sample. Arch al. Nature and impact of European anti-stigma depression programmes.
Psychiatr Nurs. 2015;29(6):407-12. http://doi.org/f724k9. Health Prom Int. 2013;29(3):403-13. http://doi.org/f6q6wd.
You might also like
- PESCI Recalls PDFDocument9 pagesPESCI Recalls PDFDanishNo ratings yet
- Essentials of Psychiatric Mental Health Nursing 7th Edition Townsend Test BankDocument15 pagesEssentials of Psychiatric Mental Health Nursing 7th Edition Townsend Test Bankkimberlymorriscntsoqmyjw100% (6)
- BIPOLAR - Mood Thermometer With Monitoring CardDocument6 pagesBIPOLAR - Mood Thermometer With Monitoring Cardathina karavolNo ratings yet
- Kessler 2005Document11 pagesKessler 2005mccg1478No ratings yet
- Behavioral Science Practice QuestionsDocument52 pagesBehavioral Science Practice QuestionsUsman KhanNo ratings yet
- Ajol File Journals - 75 - Articles - 155877 - Submission - Proof - 155877 889 406908 1 10 20170511Document6 pagesAjol File Journals - 75 - Articles - 155877 - Submission - Proof - 155877 889 406908 1 10 20170511Reni Tri AstutiNo ratings yet
- 1 s2.0 S2405844022012002 MainDocument16 pages1 s2.0 S2405844022012002 MainMythiliNo ratings yet
- Research Letter: Risk of Depression Among Patients With Acne in The U.K.: A Population-Based Cohort StudyDocument2 pagesResearch Letter: Risk of Depression Among Patients With Acne in The U.K.: A Population-Based Cohort StudyadhastriNo ratings yet
- An In-Depth Analysis of Machine Learning Approaches To Predict DepressionDocument12 pagesAn In-Depth Analysis of Machine Learning Approaches To Predict DepressionDilshan SonnadaraNo ratings yet
- A Study On Prevalence and Correlates of Depression Among Elderly Population of Rural South IndiaDocument4 pagesA Study On Prevalence and Correlates of Depression Among Elderly Population of Rural South Indiariska matokaNo ratings yet
- Journal of Affective Disorders ReportsDocument8 pagesJournal of Affective Disorders ReportsBAISHA BARETENo ratings yet
- Researching The Cultural Reaction On Mental Ill PatientsDocument8 pagesResearching The Cultural Reaction On Mental Ill Patientsmail9967No ratings yet
- Journal of Affective Disorders ReportsDocument10 pagesJournal of Affective Disorders ReportsAnnisa NurainiNo ratings yet
- Prevalence and Heritability of Body Dysmorphic Symptoms in Adolescents and Young Adults: A Population-Based Nationwide Twin StudyDocument8 pagesPrevalence and Heritability of Body Dysmorphic Symptoms in Adolescents and Young Adults: A Population-Based Nationwide Twin StudyCAMILLE HAMNo ratings yet
- Prevalence of Personality Disorders in The General Adult Population in Western Countries Systematic Review and Meta AnalysisDocument7 pagesPrevalence of Personality Disorders in The General Adult Population in Western Countries Systematic Review and Meta AnalysisFavio AndradeNo ratings yet
- Prevalence and Predictors of Depression Amongst ElderlyDocument4 pagesPrevalence and Predictors of Depression Amongst ElderlyDr.Wajid Habib (Doxxsab)No ratings yet
- 2018 Gemelos TDC y Heredabilidad DCQDocument8 pages2018 Gemelos TDC y Heredabilidad DCQIndiraNo ratings yet
- Assessment of Depression Among Older AdultsDocument9 pagesAssessment of Depression Among Older Adultsrani nauraNo ratings yet
- Admin, Ora 12 Ijnms 1921 Article 2 DeeptiDocument5 pagesAdmin, Ora 12 Ijnms 1921 Article 2 DeeptiPrinka PathaniaNo ratings yet
- Falls in The Elderly - SazlinaDocument6 pagesFalls in The Elderly - SazlinaKrishnanNo ratings yet
- DownDocument43 pagesDownAndrea LópezNo ratings yet
- Stigmatisation of People With Mental Illnesses Stigmatisation of People With Mental IllnessesDocument5 pagesStigmatisation of People With Mental Illnesses Stigmatisation of People With Mental Illnessessri endriyaniNo ratings yet
- Journal of Affective Disorders: Research PaperDocument6 pagesJournal of Affective Disorders: Research PaperjhuNo ratings yet
- Senior Seminar PaperDocument36 pagesSenior Seminar PaperKadiah KamaraNo ratings yet
- Does Loneliness Contribute To Mild Cognitive Impairment and DementiaDocument10 pagesDoes Loneliness Contribute To Mild Cognitive Impairment and Dementiamadalena limaNo ratings yet
- Major Depressive Disorder. NatureDocument20 pagesMajor Depressive Disorder. NatureMANUEL ALCIDES PUERTA BARRETO100% (1)
- Rajiv Gandhi University of Health Sciences, Bangalore, Karnataka Proforma For Registration of Subject For DissertationDocument16 pagesRajiv Gandhi University of Health Sciences, Bangalore, Karnataka Proforma For Registration of Subject For DissertationAngel SethNo ratings yet
- Research and Treatment Approaches To Depression: Cite This PaperDocument10 pagesResearch and Treatment Approaches To Depression: Cite This PaperSnehaNo ratings yet
- Suicide-Specific Mortality Amo 2Document12 pagesSuicide-Specific Mortality Amo 2I AM xbananaxNo ratings yet
- The Side Effects of Sick Leave Are PsychDocument33 pagesThe Side Effects of Sick Leave Are PsychthefrankoneNo ratings yet
- The Presence of Behavioural and Psychological Symptoms and Progression To Dementia in The Cognitively Impaired Older PopulationDocument11 pagesThe Presence of Behavioural and Psychological Symptoms and Progression To Dementia in The Cognitively Impaired Older PopulationCeci_SunshineNo ratings yet
- Borderline Personality Disorder in The Elderly. Valdivieso (2018)Document5 pagesBorderline Personality Disorder in The Elderly. Valdivieso (2018)pasandy.jrNo ratings yet
- Póster INNS 2020 Urazan J. C.Document1 pagePóster INNS 2020 Urazan J. C.jcurazanNo ratings yet
- A Study To Assess of Knowledge and Perception of Women Regarding Premenstrual Dysphoric Disorder and Its Impact On Daily Routine WorkDocument3 pagesA Study To Assess of Knowledge and Perception of Women Regarding Premenstrual Dysphoric Disorder and Its Impact On Daily Routine WorkInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Depression Research Paper PDFDocument8 pagesDepression Research Paper PDFgz9g97ha100% (1)
- Overview of Generalized Anxiety DisorderDocument6 pagesOverview of Generalized Anxiety Disordernandaas887No ratings yet
- Perceived Stress and Mild Cognitive Impairment Among 32,715 Community-Dwelling Older Adults Across Six Low-And Middle-Income CountriesDocument9 pagesPerceived Stress and Mild Cognitive Impairment Among 32,715 Community-Dwelling Older Adults Across Six Low-And Middle-Income CountriesIshani SharmaNo ratings yet
- Prevalencia de Dementcia PDFDocument15 pagesPrevalencia de Dementcia PDFdanielaNo ratings yet
- B MJ Sedgwick Cross Sectional StudiesDocument3 pagesB MJ Sedgwick Cross Sectional StudiesSaurabh MundadaNo ratings yet
- OH Honlap Felveteli Eredmenyek Gyorsstat 20180208Document2 pagesOH Honlap Felveteli Eredmenyek Gyorsstat 20180208LPATI12No ratings yet
- Estimate of Dementia PrevalenceDocument10 pagesEstimate of Dementia Prevalenceaxl___No ratings yet
- 2017 Grace Y. Lim Prevalence of Depression in The Community From 30 Countries Between 1994 and 2014Document10 pages2017 Grace Y. Lim Prevalence of Depression in The Community From 30 Countries Between 1994 and 2014adni halianieNo ratings yet
- Music and DepressionDocument6 pagesMusic and DepressiongabrielavlahopolNo ratings yet
- Major Depressive Disorder and Difference Between Genders: Dzevad Sabic, Adela Sabic, Amila Bacic-BecirovicDocument4 pagesMajor Depressive Disorder and Difference Between Genders: Dzevad Sabic, Adela Sabic, Amila Bacic-BecirovicDzevad SabicNo ratings yet
- Due Dec 3 - Mini CogDocument2 pagesDue Dec 3 - Mini Cogchuckydoll1989No ratings yet
- Gender and Social Mental HealthDocument17 pagesGender and Social Mental HealthMiEtaineNo ratings yet
- 1 s2.0 S0747563219303425 MainDocument6 pages1 s2.0 S0747563219303425 MainSAFWA BATOOL NAQVINo ratings yet
- Characterization by Gender of Frailty SyDocument12 pagesCharacterization by Gender of Frailty SygianellaNo ratings yet
- Identifying Depression On Twitter: Moin Nadeem, Mike Horn., Glen Coppersmith, PHD, University ofDocument9 pagesIdentifying Depression On Twitter: Moin Nadeem, Mike Horn., Glen Coppersmith, PHD, University ofAnanya SaikiaNo ratings yet
- Diferencias Entre Depresión Crónica y No Crónica Revisión Sistemática e Implicaciones para El TratamientoDocument13 pagesDiferencias Entre Depresión Crónica y No Crónica Revisión Sistemática e Implicaciones para El TratamientoIVAN ALVAREZNo ratings yet
- Positive Traits in The Bipolar Spectrum: The Space Between Madness and GeniusDocument15 pagesPositive Traits in The Bipolar Spectrum: The Space Between Madness and GeniusVinícius BranquinhoNo ratings yet
- Repensando Depresion Con Los RcDOCS 2023Document16 pagesRepensando Depresion Con Los RcDOCS 2023Psiquiatria Clinica ProyectarteNo ratings yet
- Anxiety-Depressive Disorders in The General Population During A Period of Confinement in MoroccoDocument9 pagesAnxiety-Depressive Disorders in The General Population During A Period of Confinement in MoroccoIJAR JOURNALNo ratings yet
- Neurology, Psychiatry and Brain Research: B.A. Pramesona, S. TaneepanichskulDocument6 pagesNeurology, Psychiatry and Brain Research: B.A. Pramesona, S. TaneepanichskulMutiara Anak NegeriNo ratings yet
- Jamapsychiatry Ruscio 2017 Oi 170004Document11 pagesJamapsychiatry Ruscio 2017 Oi 170004Koas aningNo ratings yet
- 2022 DCQ en Gemelos Suecia TDC y SuicidioDocument9 pages2022 DCQ en Gemelos Suecia TDC y SuicidioIndiraNo ratings yet
- Depression and Genes 99Document12 pagesDepression and Genes 99Rayan BotanyNo ratings yet
- Depreesion PredictionDocument11 pagesDepreesion PredictionYunitaYunitaRahmaNo ratings yet
- Lehtinen 1994Document4 pagesLehtinen 1994HARINI KNo ratings yet
- DepressionDocument16 pagesDepressionLEONARDO ANTONIO CASTILLO ZEGARRA100% (1)
- Brasil, Campeão Mundial de DepressãoDocument16 pagesBrasil, Campeão Mundial de DepressãoValéria AlmeidaNo ratings yet
- Polygenic Risk Scores Derived From Varying DefinitionsDocument9 pagesPolygenic Risk Scores Derived From Varying DefinitionsFelipe Neira DíazNo ratings yet
- Struggling Striving Surviving: Living with Borderline Personality DisorderFrom EverandStruggling Striving Surviving: Living with Borderline Personality DisorderNo ratings yet
- Depression Among Teenagers in Trinidad and TobagoDocument16 pagesDepression Among Teenagers in Trinidad and TobagoLori-Ann JacobsNo ratings yet
- Cala Component CDocument4 pagesCala Component CSancho KanyamaNo ratings yet
- Chapter 4 ResearchDocument11 pagesChapter 4 Researchsunshinemauricio1No ratings yet
- Depresion in The ElderlyDocument9 pagesDepresion in The ElderlyGuzman RubenNo ratings yet
- Written Report - Mental HealthDocument2 pagesWritten Report - Mental HealthJonalyn SalvateraNo ratings yet
- Helping Students Manage Emotions - REBT As A Mental Health Educational CurriculumDocument13 pagesHelping Students Manage Emotions - REBT As A Mental Health Educational CurriculumDalila VicenteNo ratings yet
- Geri Assess Tools ArticleDocument9 pagesGeri Assess Tools ArticleThesmith FamNo ratings yet
- Introduction, ROL (Aayushi Pillai)Document7 pagesIntroduction, ROL (Aayushi Pillai)Aayushi PillaiNo ratings yet
- Psychiatry Reporting - Classification in PsychiatryDocument13 pagesPsychiatry Reporting - Classification in PsychiatryJyl Yan SelasorNo ratings yet
- Music TherapyDocument16 pagesMusic TherapyJFFNo ratings yet
- Sample QuestionsDocument19 pagesSample Questionsjeallynasala02No ratings yet
- B-Complex Vitamins - Benefits, Side Effects and DosageDocument11 pagesB-Complex Vitamins - Benefits, Side Effects and DosageMohammed shamiul Shahid100% (1)
- Ots 1990Document38 pagesOts 1990Lau PalermoNo ratings yet
- E.1 Depression PowerPoint 20151Document38 pagesE.1 Depression PowerPoint 20151Ptrc Lbr LpNo ratings yet
- Article SCL 10Document21 pagesArticle SCL 10Erlina RatmayantiNo ratings yet
- Vagal Nerve Stimulation For Treatment Resistant DepressionDocument14 pagesVagal Nerve Stimulation For Treatment Resistant DepressionCTAFDocuments100% (1)
- Prevention and Treatment of Systemic Glucocorticoid Side EffectsDocument10 pagesPrevention and Treatment of Systemic Glucocorticoid Side EffectsMahmoud DiaaNo ratings yet
- Depresión (Dos Semanas)Document3 pagesDepresión (Dos Semanas)AcdaNo ratings yet
- Yoga and Counseling ExperienceDocument7 pagesYoga and Counseling ExperienceWilliamArugaNo ratings yet
- Electroconvulsive Therapy Ect FormDocument5 pagesElectroconvulsive Therapy Ect FormRoshita G PillaiNo ratings yet
- MentalHealthIssuesCOVID 19NIMHANSDocument177 pagesMentalHealthIssuesCOVID 19NIMHANSYanti HarjonoNo ratings yet
- Lewinsohn 1975Document3 pagesLewinsohn 1975serenadenightNo ratings yet
- A Study of Depression and Anxiety in Cancer Patients PDFDocument34 pagesA Study of Depression and Anxiety in Cancer Patients PDFIrdha Nasta KurniaNo ratings yet
- Listing of DSM-5 Diagnoses and New ICD-10-CM Codes: As Ordered in The DSM-5 ClassificationDocument2 pagesListing of DSM-5 Diagnoses and New ICD-10-CM Codes: As Ordered in The DSM-5 ClassificationFitria Ning RositaNo ratings yet
- Ambient PM2.5 Caused Depressive-Like Responses Through Nrf2NLRP3 Signaling Pathway Modulating InflammationDocument11 pagesAmbient PM2.5 Caused Depressive-Like Responses Through Nrf2NLRP3 Signaling Pathway Modulating InflammationNNo ratings yet
- The Application of Cognitive Behaviour Therapy (CBT) For Depression: A Case Study of Iranian FemaleDocument8 pagesThe Application of Cognitive Behaviour Therapy (CBT) For Depression: A Case Study of Iranian FemaleHanilah RamliNo ratings yet