Professional Documents
Culture Documents
Inferior Vena Cava Diameter
Inferior Vena Cava Diameter
Uploaded by
azizk83Copyright:
Available Formats
You might also like
- Scenarios For RevisionDocument16 pagesScenarios For RevisionJadon PunshonNo ratings yet
- PALS Study Guide: 2020 GuidelinesDocument3 pagesPALS Study Guide: 2020 GuidelinesVictoria Kidd100% (4)
- Pediatric Advanced Life Support: I. PALS System Approach AlgorithmDocument19 pagesPediatric Advanced Life Support: I. PALS System Approach AlgorithmIsabel Castillo100% (1)
- Advanced Trauma Life Support (Atls)Document44 pagesAdvanced Trauma Life Support (Atls)Danar Syahrial PradhiptaNo ratings yet
- Lyon 2005Document6 pagesLyon 2005azizk83No ratings yet
- Inferior Vena Cava Diameter and Collapsibility IndexDocument9 pagesInferior Vena Cava Diameter and Collapsibility IndexmalisalukmanNo ratings yet
- The Value of A Superior Vena Cava Collapsibility IndexDocument9 pagesThe Value of A Superior Vena Cava Collapsibility IndexmihaelamocanNo ratings yet
- Relacion Entre SvO y LactatoDocument9 pagesRelacion Entre SvO y LactatoMacros FitNo ratings yet
- Inferior Vena Cava Index in Edematous PatientsDocument4 pagesInferior Vena Cava Index in Edematous PatientsfillygogoNo ratings yet
- Doshi 2005Document6 pagesDoshi 2005Luba D'AndreaNo ratings yet
- Colapso de Vena CavaDocument9 pagesColapso de Vena CavaShirley castañedaNo ratings yet
- Prospective Assessment of The Rockall Risk Scoring System in Egyptian Patients With Upper Gastrointestinal BleedingDocument12 pagesProspective Assessment of The Rockall Risk Scoring System in Egyptian Patients With Upper Gastrointestinal BleedingsmallheartNo ratings yet
- Effect and Clinical Value of Coagulation Test On Adverse Reactions of Blood Transfusion in Patients With Major Bleeding in Ectopic PregnancyDocument5 pagesEffect and Clinical Value of Coagulation Test On Adverse Reactions of Blood Transfusion in Patients With Major Bleeding in Ectopic PregnancyRifky TaniyoNo ratings yet
- Cinahl 1Document9 pagesCinahl 1dhammo01No ratings yet
- NEJMcpc 2312731Document11 pagesNEJMcpc 2312731cehborrotoNo ratings yet
- TMP 4760Document6 pagesTMP 4760FrontiersNo ratings yet
- J Vet Emergen Crit Care - 2020 - Donati - Caudal Vena Cava Collapsibility Index As A Tool To Predict Fluid ResponsivenessDocument10 pagesJ Vet Emergen Crit Care - 2020 - Donati - Caudal Vena Cava Collapsibility Index As A Tool To Predict Fluid ResponsivenessJHON BAEZ SERRANONo ratings yet
- Sheikh Et Al 2020 - Meta-Analysis Utility of IVUS in PVIDocument10 pagesSheikh Et Al 2020 - Meta-Analysis Utility of IVUS in PVINobby MonicaNo ratings yet
- Vena Cava DonorDocument7 pagesVena Cava Donorazizk83No ratings yet
- Ijn2013 827459Document7 pagesIjn2013 827459dianaerlita97No ratings yet
- Bleeding and Infection With External Ventricular.8 PDFDocument11 pagesBleeding and Infection With External Ventricular.8 PDFAriel Aldo BravoNo ratings yet
- Informed Consent in Elective and Emergency LaparosDocument2 pagesInformed Consent in Elective and Emergency LaparosFadi NasrallahNo ratings yet
- Vol. 223, No. 4S2, October 2016 Scientific Poster Presentations: 2016 Clinical Congress E113Document1 pageVol. 223, No. 4S2, October 2016 Scientific Poster Presentations: 2016 Clinical Congress E113asfwegereNo ratings yet
- Saito 2015Document5 pagesSaito 2015didingNo ratings yet
- Echo Changes in Hypertensive Disorder of Pregnancy: Chaitra Shivananjiah, Ashwini Nayak, Asha SwarupDocument3 pagesEcho Changes in Hypertensive Disorder of Pregnancy: Chaitra Shivananjiah, Ashwini Nayak, Asha SwarupAlejandra PinillaNo ratings yet
- chengTEE SVC HypotensionDocument7 pageschengTEE SVC HypotensionthunderparthNo ratings yet
- Shoc IvcDocument12 pagesShoc Ivcsam smithNo ratings yet
- Inferior Vena Cava Diameter A Useful Method For EsDocument5 pagesInferior Vena Cava Diameter A Useful Method For EsmalisalukmanNo ratings yet
- Vena Cava ReanimacionDocument9 pagesVena Cava ReanimacionJuan Soto FarfanNo ratings yet
- Stroke Volume Variation For Prediction of Fluid Responsiveness in Patients Undergoing Gastrointestinal SurgeryDocument8 pagesStroke Volume Variation For Prediction of Fluid Responsiveness in Patients Undergoing Gastrointestinal SurgeryossinNo ratings yet
- Bedside Preload Assessment CVP, PLR and USG Guided JCCA Bali 2016Document36 pagesBedside Preload Assessment CVP, PLR and USG Guided JCCA Bali 2016Ari YudhaNo ratings yet
- Journal 36Document6 pagesJournal 36Muhammad FaisalNo ratings yet
- Oxfordshire Community Stroke Project Classification Poorly Differentiates Small Cortical and Subcortical InfarctsDocument9 pagesOxfordshire Community Stroke Project Classification Poorly Differentiates Small Cortical and Subcortical InfarctsSiti Ria RumaisaNo ratings yet
- 10.1097 01.ccm.0000474847.93776.f4Document2 pages10.1097 01.ccm.0000474847.93776.f4nermeen ahmedNo ratings yet
- Cranial Ultrasonography-2019Document4 pagesCranial Ultrasonography-2019Essam HassanNo ratings yet
- Koch 2016Document2 pagesKoch 2016Jocilene Dantas Torres NascimentoNo ratings yet
- Evaluation of Intraventricular Hemorrhage Assessment Methods For Predicting Outcome Following Intracerebral HemorrhageDocument8 pagesEvaluation of Intraventricular Hemorrhage Assessment Methods For Predicting Outcome Following Intracerebral HemorrhageNurul FajriNo ratings yet
- Inferior Vena Cava Diameter and Collapsibility IndDocument6 pagesInferior Vena Cava Diameter and Collapsibility Inddrmurad321No ratings yet
- Hasanin 2021Document8 pagesHasanin 2021Ammon10famNo ratings yet
- White-Coat Hypertension, As Defined by Ambulatory Blood Pressure Monitoring, and Subclinical Cardiac Organ Damage: A Meta-AnalysisDocument9 pagesWhite-Coat Hypertension, As Defined by Ambulatory Blood Pressure Monitoring, and Subclinical Cardiac Organ Damage: A Meta-AnalysisyuyunzilaNo ratings yet
- Sepsis-3: Jeffrey Ariesta PutraDocument35 pagesSepsis-3: Jeffrey Ariesta PutraMaria FernandezNo ratings yet
- Doppler Avf PPT JmajksnjaDocument53 pagesDoppler Avf PPT JmajksnjaraissaNo ratings yet
- Disfuncion Sistolica Ekg IngDocument13 pagesDisfuncion Sistolica Ekg IngEstreyita marNo ratings yet
- Superior Vena Cava Flow 2020Document6 pagesSuperior Vena Cava Flow 2020Betül DUMANNo ratings yet
- International Journal of CardiologyDocument7 pagesInternational Journal of CardiologySergio DiazNo ratings yet
- E1512 FullDocument16 pagesE1512 Fullamilkar morunoNo ratings yet
- Sat 8amct 9amet Acc16 Slides Partner 2aDocument40 pagesSat 8amct 9amet Acc16 Slides Partner 2anaimNo ratings yet
- Does The Central Venous Pressure Predict Fluid Responsiveness? An Updated Meta-Analysis and A Plea For Some Common SenseDocument8 pagesDoes The Central Venous Pressure Predict Fluid Responsiveness? An Updated Meta-Analysis and A Plea For Some Common SenseCris TianNo ratings yet
- Catheter Cardiovasc Interv 2021 May 27 Romeo FJDocument8 pagesCatheter Cardiovasc Interv 2021 May 27 Romeo FJFernando SousaNo ratings yet
- Invited Commentary - No Volume-Outcome Relationship For Opcabg (Plomondon Et Al)Document2 pagesInvited Commentary - No Volume-Outcome Relationship For Opcabg (Plomondon Et Al)fluid_man_brazilNo ratings yet
- 4595 7101 1 SMDocument7 pages4595 7101 1 SMNur Alifah Dina SNo ratings yet
- DTI Superposition PDFDocument7 pagesDTI Superposition PDFEtel SilvaNo ratings yet
- Sfad 156Document17 pagesSfad 156azizk83No ratings yet
- Risk Factors For Conversion During Laparoscopic Cholecystectomy - Experiences From A General Teaching HospitalDocument5 pagesRisk Factors For Conversion During Laparoscopic Cholecystectomy - Experiences From A General Teaching Hospitalskbaral86No ratings yet
- Sepsis NewDocument17 pagesSepsis Newapi-363606423No ratings yet
- Consice 2014 ACC AHA Guideline On Perioperative Cardiovascular EvaluationDocument48 pagesConsice 2014 ACC AHA Guideline On Perioperative Cardiovascular Evaluationmrezzu1No ratings yet
- ANMC Lab Body Fluid and CSF Normal ValuesDocument3 pagesANMC Lab Body Fluid and CSF Normal ValuesSaiNo ratings yet
- Journal Cardiac ArrestDocument6 pagesJournal Cardiac ArrestDavid Fransiskus SimarmataNo ratings yet
- BJOG - 2023 - MadarDocument10 pagesBJOG - 2023 - MadarOthny Jose Barboza RubioNo ratings yet
- Angina PostprandialDocument10 pagesAngina PostprandialJoaquín SosaNo ratings yet
- CARDIAC CATHETERIZATION LABORATORY AN INTRODUCTORY MANUAL, University of TennesseeDocument29 pagesCARDIAC CATHETERIZATION LABORATORY AN INTRODUCTORY MANUAL, University of TennesseeNavojit ChowdhuryNo ratings yet
- VPP y Vvci en Sepsis-2016Document20 pagesVPP y Vvci en Sepsis-2016Elsa AivarNo ratings yet
- Correlation of Platelet Count With Variceal Hemorrhage During Ligation in Hepatic Cirrhosis PatientsDocument4 pagesCorrelation of Platelet Count With Variceal Hemorrhage During Ligation in Hepatic Cirrhosis PatientsMasriyaniNo ratings yet
- Lyon 2005Document6 pagesLyon 2005azizk83No ratings yet
- The Potential Use of ABO Blood Group System For Risk Stratification of COVID-19Document6 pagesThe Potential Use of ABO Blood Group System For Risk Stratification of COVID-19azizk83No ratings yet
- ABO Blood Type Association With SARS CoV 2 Infection Mortality 2021Document7 pagesABO Blood Type Association With SARS CoV 2 Infection Mortality 2021azizk83No ratings yet
- Treatment of Autoimmune Disorders With A NeurotoxinDocument48 pagesTreatment of Autoimmune Disorders With A Neurotoxinazizk83No ratings yet
- The Protective Effect of O Blood Type Against SARS-CoV-2 InfectionDocument2 pagesThe Protective Effect of O Blood Type Against SARS-CoV-2 Infectionazizk83No ratings yet
- Jtad 12 0 en PDFDocument35 pagesJtad 12 0 en PDFazizk83No ratings yet
- An EU Programme of COVID-19 Convalescent PlasmaDocument14 pagesAn EU Programme of COVID-19 Convalescent Plasmaazizk83No ratings yet
- 1.4 Complications of Botulinum Toxin A Use in Facial Rejuvenation 1 PDFDocument10 pages1.4 Complications of Botulinum Toxin A Use in Facial Rejuvenation 1 PDFazizk83No ratings yet
- Fact Sheet Covid-19 Disease (Sars-Cov-2 Virus) : 9 February 2021, Version 8Document67 pagesFact Sheet Covid-19 Disease (Sars-Cov-2 Virus) : 9 February 2021, Version 8azizk83No ratings yet
- Long-Term Humoral Immune Response in Persons With Asymptomatic or Mild SARS-CoV-2 Infection, Vietnam February 2021Document5 pagesLong-Term Humoral Immune Response in Persons With Asymptomatic or Mild SARS-CoV-2 Infection, Vietnam February 2021azizk83No ratings yet
- Functional SARS CoV 2 Specific Immune MemoryDocument33 pagesFunctional SARS CoV 2 Specific Immune Memoryazizk83No ratings yet
- Presence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)Document12 pagesPresence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)azizk83No ratings yet
- Presence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)Document12 pagesPresence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)azizk83No ratings yet
- Estudo Prospectivo de Traumatismo CranioencefálicoDocument7 pagesEstudo Prospectivo de Traumatismo CranioencefálicoCamilaNo ratings yet
- Trauma Scoring Systems ExplainedDocument12 pagesTrauma Scoring Systems ExplainedputugunaNo ratings yet
- Crash Cart 2Document6 pagesCrash Cart 2deeptiNo ratings yet
- Adult Suspected Stroke Algorithm During COVID-19 Pandemic: Yes NoDocument1 pageAdult Suspected Stroke Algorithm During COVID-19 Pandemic: Yes NoAnabel VinuezaNo ratings yet
- CPG Abdominal TraumaDocument3 pagesCPG Abdominal TraumaHilmanNo ratings yet
- First Aid ManagementDocument69 pagesFirst Aid ManagementDandred AdrianoNo ratings yet
- Radiologic Technologists Knowledge On Basic Life SupportDocument3 pagesRadiologic Technologists Knowledge On Basic Life SupportIluminadaNo ratings yet
- Medico Legal Aspect of Stab Wound - Dilraj Singh ChouhanDocument16 pagesMedico Legal Aspect of Stab Wound - Dilraj Singh ChouhanDilraj Singh Th Det100% (2)
- Bahan ReferatDocument17 pagesBahan ReferatGisma CNo ratings yet
- ALS AlgorithmDocument22 pagesALS AlgorithmBookwormNo ratings yet
- Nur 111 Session 19 Sas 1Document6 pagesNur 111 Session 19 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- Neurosurgical Emergencies NeuroupdateDocument29 pagesNeurosurgical Emergencies NeuroupdateAdi SulistyantoNo ratings yet
- (NAI-HSE-014) FA AND MT FormDocument1 page(NAI-HSE-014) FA AND MT FormAnthony etienamNo ratings yet
- Philippine Pediatric Society in Cooperation With The Society of Pediatric Critical Care Medicine, PhilippinesDocument32 pagesPhilippine Pediatric Society in Cooperation With The Society of Pediatric Critical Care Medicine, PhilippinesShari TernolaNo ratings yet
- Chapter 7 - Dimension of Development - First Aid EducationDocument10 pagesChapter 7 - Dimension of Development - First Aid EducationAsh MooreNo ratings yet
- ACLSDocument26 pagesACLSrobmadereNo ratings yet
- Anesthetic Management of Non-Fasted Patients Requiring Emergency SurgeryDocument17 pagesAnesthetic Management of Non-Fasted Patients Requiring Emergency SurgeryBhi-An BatobalonosNo ratings yet
- CBD Doc MaffDocument6 pagesCBD Doc MaffRicky JalecoNo ratings yet
- Introduction To Emergency Nursing Concepts FinalDocument128 pagesIntroduction To Emergency Nursing Concepts FinalKarren FernandezNo ratings yet
- First Aid: By: Sem. Winmark S. PerdiganDocument18 pagesFirst Aid: By: Sem. Winmark S. PerdiganWinsley RazNo ratings yet
- Aneasth.2 - PHCP2Document11 pagesAneasth.2 - PHCP2أحمد أسامهNo ratings yet
- Basic First AidDocument55 pagesBasic First AidkurapotaNo ratings yet
- Hands On CPRDocument12 pagesHands On CPRMarites PangilinanNo ratings yet
- Nursing Pocket Card - Arterial Blood Gas (ABG) Analysis - September 2022Document3 pagesNursing Pocket Card - Arterial Blood Gas (ABG) Analysis - September 2022Mohammed FaragNo ratings yet
- HEMOTORAXDocument17 pagesHEMOTORAXmishponce12No ratings yet
- Chapter 21 Emergency and Disaster Nursing LEWISDocument22 pagesChapter 21 Emergency and Disaster Nursing LEWISMaythresha GonzalesNo ratings yet
Inferior Vena Cava Diameter
Inferior Vena Cava Diameter
Uploaded by
azizk83Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Inferior Vena Cava Diameter
Inferior Vena Cava Diameter
Uploaded by
azizk83Copyright:
Available Formats
ORIGINAL ARTICLE
Ultrasonography Measurement of Inferior Vena Cava
Diameter of Blood Donors As Predictors for Early Blood
Loss in Tertiary Hospital Northeastern, Malaysia
A W Shaik Farid*, F Mohd Hashairi*, N A R Nik Hisamuddin*, K S Chew*, A Rashidi**
*Department of Emergency Medicine, School of Medical Sciences, Universiti Sains Malaysia, 16150 Kubang Kerian, Kelantan,
Malaysia, **Academic Unit of Emergency Medicine, University Malaya Medical Center, Jalan Universiti, 59100, Kuala Lumpur,
Malaysia
SUMMARY Physical examination and vital sign in shock especially in
According to the class of hypovolaemic shock, a blood loss trauma patient were unreliable and masked by many other
less than 750 ml is not associated with the physiological factors. The blood pressure is an unreliable indicator of blood
changes. As a result it may cause a delay in fluid loss unless in the extreme shock1. The neurohormonal
resuscitation. We postulate inferior vena cava (IVC) diameter response is also inaccurate during hemorrhagic shock,
reduction in inspiration and expiration may resemble the especially in elderly due to cardiopulmonary status and
significant volume of blood loss in a healthy adult. We usage of drugs or medication2. Proper examination and
conducted a study to examine the changes of the IVC diagnosis in critically injured patient are difficult due to
diameter pre and post blood donation.The inferior vena cava inability to obtain any history pertaining to the injuries
diameter during inspiration (IVCi) and expiration (IVCe) were especially if the condition worsens. The intra abdominal
measured using ultrasound (GE HEALTH) in supine position injury which is characterized by abdominal tenderness,
before and after blood donation of 450 ml. Paired t-test and distension may not present in the early stage of the
Wilcoxin rank test were used to analyse the data. Forty two management3. Laboratory parameters were also unreliable
blood donors enrolled during the study period. The mean as the routine haemoglobin level does not change or
age of blood donors was 32.3 +/- 8.9 and mainly male blood decreases until after the mobilization of extra vascular fluid
donors. The mean IVCe of pre and post blood donation was into the blood vessels to compensate for blood loss4.
18.5 +/- 6.2 mm (95%CI 18.23, 18.74) and 16.6 +/- 6.6 mm
(95%CI 16.35, 16.76) respectively. Meanwhile, the mean IVCi Many studies have been done on the inferior vena cava (IVC)
of pre and post blood donation was 17.1 +/- 8.6 mm (95%CI diameter and have shown good correlation to the total blood
16.89,17.30) and 15.6 +/- 6.6 mm (95%CI 15.43,15.81) volume5. IVC diameter has a different diameter in various
respectively. The mean difference of IVCe pre and post places in human anatomy with no actual diameter recorded
blood donation was 1.9 +/- 0.5 mm (95%CI 1.75, 2.13) for the IVC. A larger study in India on cadavers showed that
(p<0.001). In contrast, the mean difference of IVCi pre and the average of the diameters differ at the different sites5-6. Our
post blood donation was 1.5 +/- 0.5 mm (95%CI 1.34, 1.68) study objective is to determine the changes of the inferior
(p<0.001). As a conclusion, the measurement of IVC vena cava diameter in blood donor as a simulated type 1
diameter by ultrasound can predict the volume of blood loss hypovolaemic shock with acute blood loss estimated about
in simulated type 1 hypovolaemia patient. 450ml per donor.
KEY WORDS:
Ultrasound, Inferior Vena Cava diameter, hypovolaemic shock MATERIALS AND METHODS
A prospective study was conducted on normal healthy blood
donors who came to the blood bank for blood donations. A
INTRODUCTION study was carried out in a university hospital which is a
Shock is a clinical condition that can arise from multiple tertiary centre. Blood donors were identified by the blood
etiologies such as trauma, dehydration, excessive fluid bank staff and all necessary tests were done according to the
extraction post dialysis, burns, ruptured ectopic tubal blood bank criteria. Once donors were eligible for blood
pregnancy and many others. In trauma for example, it’s donations, the donors then included into the study and
very difficult to determine the amount of blood loss since written consent was taken from them. Inclusion criteria are
there is no tool to assess the ongoing blood loss contrast to similar to the blood donors in university hospital which
any open wound or soaked gauze which we can approximate include adult donor age 18 to 55 years old, weight more than
the blood loss1. Seriously injured patient or with altered 45kg, no any medical illness and able to understand and to
sensorium combine with lack of history will lead to give informed consent. Exclusion criteria’s include patient
irregularity of the physical examination and laboratory requires rehydration immediately during or post donation,
evaluation. All these unreliability leads to potentially previous surgery or delivery or received blood transfusion
misdiagnosed and inappropriate resuscitation. within 6 months, donor who is pregnant and breast feeding,
This article was accepted: 18 December 2013
Corresponding Author: Mohd Hashairi Hj Fauzi, Emergency Medicine Department, School of Medical Sciences, 16150 Kubang Kerian, Kelantan, Malaysia
Email: hashairi@kk.usm.my
Med J Malaysia Vol 68 No 6 December 2013 465
Original Article
Table I: Socio-demographic characteristic of respondents Table II: Inferior Vena Cava mean distribution and standard
deviation.
Socio-demographic Respondents
Variables ( N = 42 ) Variable Mean(sd)
Age (mean + sd ) 32.33 (9.20) (mm)
Sex Pre
Male 42 (100%) IVCi 18.49 (0.81)
Female 0 (0%) IVCe 17.10 (0.67)
Race Post
Malay 87.7% IVCi 16.55 (0.65)
Chinese 2.8% IVCe 15.62 (0.60)
Indian 9.5% Difference
IVCi 1.94 (0.60)
IVCe 1.51 (0.54)
Table III: Paired T test for IVC expiration
Mean (95%CI) t df p value
pre IVCe-post IVCe 1.94 (1.74,2.12) 20.7 41 <0.001
Table IV: Wilcoxon Signed Ranks Test for IVC during inspiration.
Mean Rank z p value
pre IVCi-post IVCi 21.50 -5.65a <0.001
a = based on positive rank
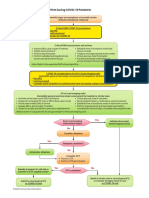
donor with high risk behaviour such as multiple sex partners diameter is measured 2cm from the junction of the right
or sharing needles and sex worker. atrium inlet, measuring the anterior and posterior wall of
IVC wall are well seen parallel to each other (Figure 2). The
Each ultrasound examinations were performed by the single measurement taken during donor had a deep inspiration
researcher who is familiar with ultrasound. The researcher (IVCi) and on full expiration (IVCe). Upon visualization of
was trained in the principle of the abdominal ultrasound and the IVC, the image was frozen and using cine loop the
particularly IVC with hands on demonstration and maximal IVC diameter and the minimal IVC diameter is
measurement validation by a Consultant Radiologist in identified and recorded. No technical adjustment done to the
Radiology Department, Universiti Hospital with more than ultrasound machine and the patient’s position to get the pre
25 years experience. Using the Spearmen’s rank correlation donation and post donation IVC measurement, in an
coefficient, there was a significant, positive and excellent attempt to exclude the cofactors. Measurement taken before
correlation between the researcher and the radiologist score the blood donation and repeat just after the blood donation.
(σ =0. 903, p<0.001). Subsequently the researcher performed
independent ultrasound measurement of inferior vena cava Statistical analysis
on the blood donors who agreed to participate in this study. The data recorded from ultrasound examination which
includes demographic, vital sign before and after donation
The ultrasound measurement was carried out once donor was were compiled and analysed using SPSS 18.0.1 which was
in a comfortable position on the blood donation bed in a licensed to School of Medicine, Universiti Sains Malaysia. The
supine position. The first measurements of the inferior vena aim of this study was to evaluate the changes of the IVC
cava were done during inspiration and expiration before the diameter in blood donors in correlation with the type 1
blood donation. Three readings were taken on each hypovolemia. Paired t-test and Wilcoxon Signed Rank test
inspiration and expiration and the average value were are used to analyse the statistical significance of the mean
calculated. The second measurements were done values of the IVC during inspiration and expiration. P values
immediately after the completion of blood donation. The less than 0.05 is considered to be significant.
similar three readings during inspiration and expiration
taken post blood donation and average value calculated.
RESULTS
The ultrasound measurement evaluation of the inferior vena There were 42 donors who fulfilled the inclusion criteria
cava was performed with a portable ultrasound Micro during the study time and had an ultrasound of the inferior
Convex GE LOGIQ BOOK, GE Health Care Service, USA. A 3.0 vena cava diameter performed at the time of blood donation.
- 5.0 MHz curvilinear probe was used. The same model All donors included in the study. Data from 42 donors were
ultrasound was used for training, hands on demonstration submitted for analysis. All donors were male with mean age
and validation by the researcher and a radiologist. The 32.3 years (range, 21-54) (Table 1). Mean IVCe measurement
probe with B mode scan placed longitudinally over the before blood donation was 18.49mm (95%CI 18.23,18.74)
subxyphoid area and adjusted till able to see the IVC meeting and after blood donation was 16.55mm (95%CI 16.35,16.76).
the right atrium inlet (Figure 1). The inferior vena cava is The mean IVCi before blood donation was 17.09mm (95%CI
identified with colour Doppler setting. Inferior vena cava 16.89,17.30) and after blood donation was 15.62mm (95%CI
466 Med J Malaysia Vol 68 No 6 December 2013
Ultrasonography Measurement of Inferior Vena Cava Diameter of Blood Donors
Fig. 2 : Inferior vena measurement measure 2cm from the right
atrium.
associated with decrease venous content and metabolic
acidosis10. Hypovolemic shock usually presents with some
physiological changes in large amount of blood loss11. Early
management of shock is to restore the intravascular fluid
volume, sufficient enough to reverse the hypo perfusion and
limit regional hypo perfusion, maintaining adequate oxygen
Fig. 1 : The position of probe on donor’s epigastric region. carrying capacity so that tissue oxygen delivery meets the
critical tissue oxygen demands and limiting ongoing blood
loss12.
15.43,15.81) (Table II). The difference of IVCe before and after
blood donation was 1.94mm (95%CI 1.75,2.13) yielding a In this study, volunteer blood donors had been chosen as the
p<0.001 (Table III). The difference of IVCi before and after models for trauma patients because the amount of blood
blood donation was 1.51mm (95%CI 1.34,1.68) yielding a withdrawn from the body in this controlled environment was
p<0.001 (Table IV). The mean duration for the blood 450ml. It occurs over a brief period and stimulates class 1
donations is 5 min 26 seconds. No blood donors suffered haemorrhage in the trauma related blood loss. IVC diameter
from complications of blood donation.No patient excluded varies from one individual to another but there are no studies
from the study. to confirm such finding. IVC is a very good compliance vessel
with the distensibility property influenced by the total body
water and phases of respiration13. The change in the IVC
DISCUSSION diameter is crucial in determining the blood loss or the
Ultrasound has now become an integral part of emergency ongoing blood loss. The early detection of the changes of the
medicine and acute critical care. It is routinely used in many diameter would allow an EP to start early appropriate fluid
ED and trauma centre7. In view of the fast expanding of the therapy. This study shared the same finding by the Lyon et al
ultrasound usage and easily available modalities with no from Medical College of Georgia8. His study revealed a
radiation involvement, ultrasound has a potential to develop positive correlation between IVC diameter and intravascular
as an early blood loss detector8. Ultrasound has become an volume that has been retrospectively investigated using
essential tool as a noninvasive and sensitive diagnostic computed tomography (CT) scan which shows flattened
modality; especially in the part of the emergency physicians inferior vena cava in massive haemorrhagic patients with
(EP) practice particularly in the ED setting8,9,10. intra abdomen injury14.
Vital signs are the first clinical parameters taken during any This study showed that there was a significant correlation
trauma cases and the most reliable tool till now in between both changes in IVC on inspiration (IVCi) and IVC
resuscitating a trauma victim. These vital signs such as blood on expiration (IVCe) during the blood donation. The mean
pressure and heart rate are unreliable during condition such diameter of the IVCe of 18.5mm before blood donation was
as trauma and these indicators are not consistent with the slightly bigger than a study carried out by Lyon et al about
acute blood loss unless the shock is irreversible4. 17.4mm and Ando et al 16.7mm8,15. In another study by
Quantification of occult blood loss is difficult in cases such as Sefidbakht et al, the measured IVCe was far smaller
intra abdominal bleeding and unrevealed bleeding for compared to our finding. The IVCe is more accurate and
example long bone fractures. appropriate measurement for trauma related hypovolaemia
comparison to IVCi in trauma patient for evaluating for
Shock is defined as circulatory insufficiency that creates an potential haemorrhage. Both IVCe and IVCi measurement
imbalance between tissue oxygen supply and oxygen would be unreliable if certain pathological conditions were
demand which results in global tissue hypo perfusion and found in trauma patient such as abnormal acid base
Med J Malaysia Vol 68 No 6 December 2013 467
Original Article
balance, severe pain, anxiety and other factors which cause REFERENCES
patient to forcefully breathe or irregular respiration that 1. Wo CC, Shoemaker WC, Appel PL, Bishop MH, Kram HB, Hardin E.
Unreliability of blood pressure and heart rate to evaluate cardiac output
would lead to alteration in IVC diameter13.
in emergency resuscitation and critical illness. Crit Care MED 1993 Feb; 21
(2): 218-23.
Besides that, a serial measurement was also applicable to 2. Benedict CR, Grahame-Smith DG. Plasma noradrenaline and adrenaline
further assess the on ongoing blood loss and easily done at concentrations and dopamine-beta-hydroxylase activity in patients with
shock due to septicaemia, trauma and haemorrhage. Q J Med 1978
bedside without any radiation hazards. Direct measurement Jan;47(185): 1-20.
of the fluid status via central venous pressure is not readily 3. Scalea TM, Holman M, Fuortes M, et al. Central venous blood oxygen
appropriate in trauma patient and the invasive procedure is saturation: an early, accurate measurement of volume during
haemorrhage. J Trauma1988 Jun; 28 (6): 725-32.
not suitable as a routine assessment18, 19. The early detection
4. Carey LC, Lowery BD, Cloutier CT. Haemorrhagic shock. Curr Probl Surg
of acute blood loss is becoming more important for diagnostic 1971 Jan: 3-48.
purpose especially with the development of the newer 5. Yanagawa Y, Sakamoto T, Okada Y. Hypovolemic shock evaluated by
portable ultrasound device. Yet, in real practice, trauma cases sonographic measurement of the inferior vena cava during resuscitation
in trauma patients. J Trauma 2007 Dec; 63 (6): 1245-8.
will be managed according to Advanced Trauma Life Support 6. Sharma D, Deshmukh A, Raina VK. Surgical anatomy of retrohepatic
(ATLS) Guidelines whereby the IVC measurement by inferior vena cava and hepatic veins: a quantitative assessment. Indian J
ultrasound will be performed after completing primary & Gastroenterol 2001 Jul-Aug; 20(4): 136-9.
7. Melanson SWH, M. The emerging role of bedside ultrasonography in
secondary survey20. At this point, the ultrasound may help to
trauma care. Emerg MED Clin North Am 1998; 16 (1): 165-89.
determine the fluid status of the patient either to detect 8. Lyon M, Blaivas M, Brannam L. Sonographic measurement of the inferior
volume loss or monitor the body response to fluid therapy. vena cava as a marker of blood loss. Am J Emerg MED 2005 Jan; 23(1): 45-
50.
9. Chan SS. Emergency bedside ultrasound to detect pneumothorax. Acad
Emerg Med2 003 Jan; 10(1): 91-4.
LIMITATIONS 10. Judith E, Gabor D, Stephen J. Textbook of Emergency Medicine: A
There were limitations in this study. Firstly, ultrasonographic Comprehensive Study Guide (6th ed). McGraw Hills, 2004.
11. Cocchi MN, Kimlin E, Walsh M, Donnino MW. Identification and
examination was carried out by a single operator. Therefore
resuscitation of the trauma patient in shock. Emerg MED Clin North Am
the results of this study may be questionable. Multiple 2007 Aug; 25 (3): 623-42, vii.
operators with good training and validation are necessary to 12. Falk JL, O'Brien JF, Kerr R. Fluid resuscitation in traumatic hemorrhagic
perform a bigger study in view of producing more reliable shock. Crit Care Clin1992 Apr; 8 (2): 323-40.
13. Kusaba T, Yamaguchi K, Oda H. Echography of the inferior vena cava for
results. Secondly, the sample of this study was rather small. estimating fluid removal from patients undergoing hemodialysis. Nippon
We need a larger number of donors as a sample, and then it Jinzo Gakkai Shi 1996 Mar; 38(3): 119-23.
is comparable or even better compared to other designed 14. Jeffrey RB, Jr., Federle MP. The collapsed inferior vena cava: CT evidence of
hypovolemia. AJR Am J Roentgenol 1988 Feb; 150 (2): 431-2.
studies. With a larger sample, we also believe that we can
15. Ando Y, Yanagiba S, Asano Y. The inferior vena cava diameter as a marker
produce the average inferior vena cava diameter to the of dry weight in chronic hemodialyzed patients. Artif Organs 1995 Dec; 19
population of blood donors in Kelantan and subsequently the (12): 1237-42.
average diameter of Malaysian inferior vena cava diameter. 16. Tetsuka T, Ando Y, Ono S, Asano Y. Change in inferior vena caval diameter
detected by ultrasonography during and after hemodialysis. Asaio J 1995
Jan-Mar; 41(1): 105-10.
17. Kusaba T, Yamaguchi K, Oda H, Harada T. Echography of inferior vena
CONCLUSION cava for estimating fluid removed from patients undergoing hemodialysis.
Nippon Jinzo Gakkai Shi 1994 Aug; 36(8): 914-20.
The early detection of acute blood loss is becoming very
18. Carr BG, Dean AJ, Everett WW, Ku BS, Mark DG, Okusanya O, Horan AD,
challenging and more important for diagnostic and Gracias VH. Intensivist bedside ultrasound (INBU) for volume assessment
management purposes. There were two clinical implications in the intensive care unit: a pilot study. J Trauma 2007 Sep; 63(3): 495-500.
of this study. First, the IVC diameter changes in this simulated 19. Mirvis SE, Shanmuganathan K, Erb R. Diffuse small-bowel ischemia in
hypotensive adults after blunt trauma (shock bowel): CT findings and
type 1 shock can be used to detect a volume loss even when clinical significance. AJR Am J Roentgenol 1994 Dec; 163 (6): 1375-9.
the blood pressure still remains normal. Secondly, it’s given 20. Advanced Trauma Life Support for Doctors. Student Course Manual. (8th
an information of normal values of IVC diameter among our Ed.) American College of Surgeons. 2008
populations as a guide for future research.
ACKNOWLEDGEMENTS
The authors wish to express their deep gratitude to Universiti
Sains Malaysia for supporting this study by granting the
Short Term Grant number 304/PPSP/6131622. Author also
feels the deepest gratitude for the support of the HUSM Blood
Bank and our fantastic blood donors.
468 Med J Malaysia Vol 68 No 6 December 2013
You might also like
- Scenarios For RevisionDocument16 pagesScenarios For RevisionJadon PunshonNo ratings yet
- PALS Study Guide: 2020 GuidelinesDocument3 pagesPALS Study Guide: 2020 GuidelinesVictoria Kidd100% (4)
- Pediatric Advanced Life Support: I. PALS System Approach AlgorithmDocument19 pagesPediatric Advanced Life Support: I. PALS System Approach AlgorithmIsabel Castillo100% (1)
- Advanced Trauma Life Support (Atls)Document44 pagesAdvanced Trauma Life Support (Atls)Danar Syahrial PradhiptaNo ratings yet
- Lyon 2005Document6 pagesLyon 2005azizk83No ratings yet
- Inferior Vena Cava Diameter and Collapsibility IndexDocument9 pagesInferior Vena Cava Diameter and Collapsibility IndexmalisalukmanNo ratings yet
- The Value of A Superior Vena Cava Collapsibility IndexDocument9 pagesThe Value of A Superior Vena Cava Collapsibility IndexmihaelamocanNo ratings yet
- Relacion Entre SvO y LactatoDocument9 pagesRelacion Entre SvO y LactatoMacros FitNo ratings yet
- Inferior Vena Cava Index in Edematous PatientsDocument4 pagesInferior Vena Cava Index in Edematous PatientsfillygogoNo ratings yet
- Doshi 2005Document6 pagesDoshi 2005Luba D'AndreaNo ratings yet
- Colapso de Vena CavaDocument9 pagesColapso de Vena CavaShirley castañedaNo ratings yet
- Prospective Assessment of The Rockall Risk Scoring System in Egyptian Patients With Upper Gastrointestinal BleedingDocument12 pagesProspective Assessment of The Rockall Risk Scoring System in Egyptian Patients With Upper Gastrointestinal BleedingsmallheartNo ratings yet
- Effect and Clinical Value of Coagulation Test On Adverse Reactions of Blood Transfusion in Patients With Major Bleeding in Ectopic PregnancyDocument5 pagesEffect and Clinical Value of Coagulation Test On Adverse Reactions of Blood Transfusion in Patients With Major Bleeding in Ectopic PregnancyRifky TaniyoNo ratings yet
- Cinahl 1Document9 pagesCinahl 1dhammo01No ratings yet
- NEJMcpc 2312731Document11 pagesNEJMcpc 2312731cehborrotoNo ratings yet
- TMP 4760Document6 pagesTMP 4760FrontiersNo ratings yet
- J Vet Emergen Crit Care - 2020 - Donati - Caudal Vena Cava Collapsibility Index As A Tool To Predict Fluid ResponsivenessDocument10 pagesJ Vet Emergen Crit Care - 2020 - Donati - Caudal Vena Cava Collapsibility Index As A Tool To Predict Fluid ResponsivenessJHON BAEZ SERRANONo ratings yet
- Sheikh Et Al 2020 - Meta-Analysis Utility of IVUS in PVIDocument10 pagesSheikh Et Al 2020 - Meta-Analysis Utility of IVUS in PVINobby MonicaNo ratings yet
- Vena Cava DonorDocument7 pagesVena Cava Donorazizk83No ratings yet
- Ijn2013 827459Document7 pagesIjn2013 827459dianaerlita97No ratings yet
- Bleeding and Infection With External Ventricular.8 PDFDocument11 pagesBleeding and Infection With External Ventricular.8 PDFAriel Aldo BravoNo ratings yet
- Informed Consent in Elective and Emergency LaparosDocument2 pagesInformed Consent in Elective and Emergency LaparosFadi NasrallahNo ratings yet
- Vol. 223, No. 4S2, October 2016 Scientific Poster Presentations: 2016 Clinical Congress E113Document1 pageVol. 223, No. 4S2, October 2016 Scientific Poster Presentations: 2016 Clinical Congress E113asfwegereNo ratings yet
- Saito 2015Document5 pagesSaito 2015didingNo ratings yet
- Echo Changes in Hypertensive Disorder of Pregnancy: Chaitra Shivananjiah, Ashwini Nayak, Asha SwarupDocument3 pagesEcho Changes in Hypertensive Disorder of Pregnancy: Chaitra Shivananjiah, Ashwini Nayak, Asha SwarupAlejandra PinillaNo ratings yet
- chengTEE SVC HypotensionDocument7 pageschengTEE SVC HypotensionthunderparthNo ratings yet
- Shoc IvcDocument12 pagesShoc Ivcsam smithNo ratings yet
- Inferior Vena Cava Diameter A Useful Method For EsDocument5 pagesInferior Vena Cava Diameter A Useful Method For EsmalisalukmanNo ratings yet
- Vena Cava ReanimacionDocument9 pagesVena Cava ReanimacionJuan Soto FarfanNo ratings yet
- Stroke Volume Variation For Prediction of Fluid Responsiveness in Patients Undergoing Gastrointestinal SurgeryDocument8 pagesStroke Volume Variation For Prediction of Fluid Responsiveness in Patients Undergoing Gastrointestinal SurgeryossinNo ratings yet
- Bedside Preload Assessment CVP, PLR and USG Guided JCCA Bali 2016Document36 pagesBedside Preload Assessment CVP, PLR and USG Guided JCCA Bali 2016Ari YudhaNo ratings yet
- Journal 36Document6 pagesJournal 36Muhammad FaisalNo ratings yet
- Oxfordshire Community Stroke Project Classification Poorly Differentiates Small Cortical and Subcortical InfarctsDocument9 pagesOxfordshire Community Stroke Project Classification Poorly Differentiates Small Cortical and Subcortical InfarctsSiti Ria RumaisaNo ratings yet
- 10.1097 01.ccm.0000474847.93776.f4Document2 pages10.1097 01.ccm.0000474847.93776.f4nermeen ahmedNo ratings yet
- Cranial Ultrasonography-2019Document4 pagesCranial Ultrasonography-2019Essam HassanNo ratings yet
- Koch 2016Document2 pagesKoch 2016Jocilene Dantas Torres NascimentoNo ratings yet
- Evaluation of Intraventricular Hemorrhage Assessment Methods For Predicting Outcome Following Intracerebral HemorrhageDocument8 pagesEvaluation of Intraventricular Hemorrhage Assessment Methods For Predicting Outcome Following Intracerebral HemorrhageNurul FajriNo ratings yet
- Inferior Vena Cava Diameter and Collapsibility IndDocument6 pagesInferior Vena Cava Diameter and Collapsibility Inddrmurad321No ratings yet
- Hasanin 2021Document8 pagesHasanin 2021Ammon10famNo ratings yet
- White-Coat Hypertension, As Defined by Ambulatory Blood Pressure Monitoring, and Subclinical Cardiac Organ Damage: A Meta-AnalysisDocument9 pagesWhite-Coat Hypertension, As Defined by Ambulatory Blood Pressure Monitoring, and Subclinical Cardiac Organ Damage: A Meta-AnalysisyuyunzilaNo ratings yet
- Sepsis-3: Jeffrey Ariesta PutraDocument35 pagesSepsis-3: Jeffrey Ariesta PutraMaria FernandezNo ratings yet
- Doppler Avf PPT JmajksnjaDocument53 pagesDoppler Avf PPT JmajksnjaraissaNo ratings yet
- Disfuncion Sistolica Ekg IngDocument13 pagesDisfuncion Sistolica Ekg IngEstreyita marNo ratings yet
- Superior Vena Cava Flow 2020Document6 pagesSuperior Vena Cava Flow 2020Betül DUMANNo ratings yet
- International Journal of CardiologyDocument7 pagesInternational Journal of CardiologySergio DiazNo ratings yet
- E1512 FullDocument16 pagesE1512 Fullamilkar morunoNo ratings yet
- Sat 8amct 9amet Acc16 Slides Partner 2aDocument40 pagesSat 8amct 9amet Acc16 Slides Partner 2anaimNo ratings yet
- Does The Central Venous Pressure Predict Fluid Responsiveness? An Updated Meta-Analysis and A Plea For Some Common SenseDocument8 pagesDoes The Central Venous Pressure Predict Fluid Responsiveness? An Updated Meta-Analysis and A Plea For Some Common SenseCris TianNo ratings yet
- Catheter Cardiovasc Interv 2021 May 27 Romeo FJDocument8 pagesCatheter Cardiovasc Interv 2021 May 27 Romeo FJFernando SousaNo ratings yet
- Invited Commentary - No Volume-Outcome Relationship For Opcabg (Plomondon Et Al)Document2 pagesInvited Commentary - No Volume-Outcome Relationship For Opcabg (Plomondon Et Al)fluid_man_brazilNo ratings yet
- 4595 7101 1 SMDocument7 pages4595 7101 1 SMNur Alifah Dina SNo ratings yet
- DTI Superposition PDFDocument7 pagesDTI Superposition PDFEtel SilvaNo ratings yet
- Sfad 156Document17 pagesSfad 156azizk83No ratings yet
- Risk Factors For Conversion During Laparoscopic Cholecystectomy - Experiences From A General Teaching HospitalDocument5 pagesRisk Factors For Conversion During Laparoscopic Cholecystectomy - Experiences From A General Teaching Hospitalskbaral86No ratings yet
- Sepsis NewDocument17 pagesSepsis Newapi-363606423No ratings yet
- Consice 2014 ACC AHA Guideline On Perioperative Cardiovascular EvaluationDocument48 pagesConsice 2014 ACC AHA Guideline On Perioperative Cardiovascular Evaluationmrezzu1No ratings yet
- ANMC Lab Body Fluid and CSF Normal ValuesDocument3 pagesANMC Lab Body Fluid and CSF Normal ValuesSaiNo ratings yet
- Journal Cardiac ArrestDocument6 pagesJournal Cardiac ArrestDavid Fransiskus SimarmataNo ratings yet
- BJOG - 2023 - MadarDocument10 pagesBJOG - 2023 - MadarOthny Jose Barboza RubioNo ratings yet
- Angina PostprandialDocument10 pagesAngina PostprandialJoaquín SosaNo ratings yet
- CARDIAC CATHETERIZATION LABORATORY AN INTRODUCTORY MANUAL, University of TennesseeDocument29 pagesCARDIAC CATHETERIZATION LABORATORY AN INTRODUCTORY MANUAL, University of TennesseeNavojit ChowdhuryNo ratings yet
- VPP y Vvci en Sepsis-2016Document20 pagesVPP y Vvci en Sepsis-2016Elsa AivarNo ratings yet
- Correlation of Platelet Count With Variceal Hemorrhage During Ligation in Hepatic Cirrhosis PatientsDocument4 pagesCorrelation of Platelet Count With Variceal Hemorrhage During Ligation in Hepatic Cirrhosis PatientsMasriyaniNo ratings yet
- Lyon 2005Document6 pagesLyon 2005azizk83No ratings yet
- The Potential Use of ABO Blood Group System For Risk Stratification of COVID-19Document6 pagesThe Potential Use of ABO Blood Group System For Risk Stratification of COVID-19azizk83No ratings yet
- ABO Blood Type Association With SARS CoV 2 Infection Mortality 2021Document7 pagesABO Blood Type Association With SARS CoV 2 Infection Mortality 2021azizk83No ratings yet
- Treatment of Autoimmune Disorders With A NeurotoxinDocument48 pagesTreatment of Autoimmune Disorders With A Neurotoxinazizk83No ratings yet
- The Protective Effect of O Blood Type Against SARS-CoV-2 InfectionDocument2 pagesThe Protective Effect of O Blood Type Against SARS-CoV-2 Infectionazizk83No ratings yet
- Jtad 12 0 en PDFDocument35 pagesJtad 12 0 en PDFazizk83No ratings yet
- An EU Programme of COVID-19 Convalescent PlasmaDocument14 pagesAn EU Programme of COVID-19 Convalescent Plasmaazizk83No ratings yet
- 1.4 Complications of Botulinum Toxin A Use in Facial Rejuvenation 1 PDFDocument10 pages1.4 Complications of Botulinum Toxin A Use in Facial Rejuvenation 1 PDFazizk83No ratings yet
- Fact Sheet Covid-19 Disease (Sars-Cov-2 Virus) : 9 February 2021, Version 8Document67 pagesFact Sheet Covid-19 Disease (Sars-Cov-2 Virus) : 9 February 2021, Version 8azizk83No ratings yet
- Long-Term Humoral Immune Response in Persons With Asymptomatic or Mild SARS-CoV-2 Infection, Vietnam February 2021Document5 pagesLong-Term Humoral Immune Response in Persons With Asymptomatic or Mild SARS-CoV-2 Infection, Vietnam February 2021azizk83No ratings yet
- Functional SARS CoV 2 Specific Immune MemoryDocument33 pagesFunctional SARS CoV 2 Specific Immune Memoryazizk83No ratings yet
- Presence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)Document12 pagesPresence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)azizk83No ratings yet
- Presence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)Document12 pagesPresence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)azizk83No ratings yet
- Estudo Prospectivo de Traumatismo CranioencefálicoDocument7 pagesEstudo Prospectivo de Traumatismo CranioencefálicoCamilaNo ratings yet
- Trauma Scoring Systems ExplainedDocument12 pagesTrauma Scoring Systems ExplainedputugunaNo ratings yet
- Crash Cart 2Document6 pagesCrash Cart 2deeptiNo ratings yet
- Adult Suspected Stroke Algorithm During COVID-19 Pandemic: Yes NoDocument1 pageAdult Suspected Stroke Algorithm During COVID-19 Pandemic: Yes NoAnabel VinuezaNo ratings yet
- CPG Abdominal TraumaDocument3 pagesCPG Abdominal TraumaHilmanNo ratings yet
- First Aid ManagementDocument69 pagesFirst Aid ManagementDandred AdrianoNo ratings yet
- Radiologic Technologists Knowledge On Basic Life SupportDocument3 pagesRadiologic Technologists Knowledge On Basic Life SupportIluminadaNo ratings yet
- Medico Legal Aspect of Stab Wound - Dilraj Singh ChouhanDocument16 pagesMedico Legal Aspect of Stab Wound - Dilraj Singh ChouhanDilraj Singh Th Det100% (2)
- Bahan ReferatDocument17 pagesBahan ReferatGisma CNo ratings yet
- ALS AlgorithmDocument22 pagesALS AlgorithmBookwormNo ratings yet
- Nur 111 Session 19 Sas 1Document6 pagesNur 111 Session 19 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- Neurosurgical Emergencies NeuroupdateDocument29 pagesNeurosurgical Emergencies NeuroupdateAdi SulistyantoNo ratings yet
- (NAI-HSE-014) FA AND MT FormDocument1 page(NAI-HSE-014) FA AND MT FormAnthony etienamNo ratings yet
- Philippine Pediatric Society in Cooperation With The Society of Pediatric Critical Care Medicine, PhilippinesDocument32 pagesPhilippine Pediatric Society in Cooperation With The Society of Pediatric Critical Care Medicine, PhilippinesShari TernolaNo ratings yet
- Chapter 7 - Dimension of Development - First Aid EducationDocument10 pagesChapter 7 - Dimension of Development - First Aid EducationAsh MooreNo ratings yet
- ACLSDocument26 pagesACLSrobmadereNo ratings yet
- Anesthetic Management of Non-Fasted Patients Requiring Emergency SurgeryDocument17 pagesAnesthetic Management of Non-Fasted Patients Requiring Emergency SurgeryBhi-An BatobalonosNo ratings yet
- CBD Doc MaffDocument6 pagesCBD Doc MaffRicky JalecoNo ratings yet
- Introduction To Emergency Nursing Concepts FinalDocument128 pagesIntroduction To Emergency Nursing Concepts FinalKarren FernandezNo ratings yet
- First Aid: By: Sem. Winmark S. PerdiganDocument18 pagesFirst Aid: By: Sem. Winmark S. PerdiganWinsley RazNo ratings yet
- Aneasth.2 - PHCP2Document11 pagesAneasth.2 - PHCP2أحمد أسامهNo ratings yet
- Basic First AidDocument55 pagesBasic First AidkurapotaNo ratings yet
- Hands On CPRDocument12 pagesHands On CPRMarites PangilinanNo ratings yet
- Nursing Pocket Card - Arterial Blood Gas (ABG) Analysis - September 2022Document3 pagesNursing Pocket Card - Arterial Blood Gas (ABG) Analysis - September 2022Mohammed FaragNo ratings yet
- HEMOTORAXDocument17 pagesHEMOTORAXmishponce12No ratings yet
- Chapter 21 Emergency and Disaster Nursing LEWISDocument22 pagesChapter 21 Emergency and Disaster Nursing LEWISMaythresha GonzalesNo ratings yet