Professional Documents
Culture Documents
Diagnosis of Acute Rheumatic Fever: 2020 Updated Australian Criteria For ARF Diagnosis
Diagnosis of Acute Rheumatic Fever: 2020 Updated Australian Criteria For ARF Diagnosis
Uploaded by
Richard Ssenyondo0 ratings0% found this document useful (0 votes)
15 views3 pagesThis document provides updated criteria for diagnosing acute rheumatic fever in Australia. It lists the major and minor diagnostic manifestations. It also differentiates diagnostic criteria for high-risk versus low-risk groups. The document then provides treatment guidelines for managing acute rheumatic fever, including eradicating streptococcal infections, relieving pain, managing arthritis/chorea, and treating carditis complications. Disease-modifying corticosteroid treatments are also recommended for severe symptoms.
Original Description:
Original Title
ARF
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides updated criteria for diagnosing acute rheumatic fever in Australia. It lists the major and minor diagnostic manifestations. It also differentiates diagnostic criteria for high-risk versus low-risk groups. The document then provides treatment guidelines for managing acute rheumatic fever, including eradicating streptococcal infections, relieving pain, managing arthritis/chorea, and treating carditis complications. Disease-modifying corticosteroid treatments are also recommended for severe symptoms.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
15 views3 pagesDiagnosis of Acute Rheumatic Fever: 2020 Updated Australian Criteria For ARF Diagnosis
Diagnosis of Acute Rheumatic Fever: 2020 Updated Australian Criteria For ARF Diagnosis
Uploaded by
Richard SsenyondoThis document provides updated criteria for diagnosing acute rheumatic fever in Australia. It lists the major and minor diagnostic manifestations. It also differentiates diagnostic criteria for high-risk versus low-risk groups. The document then provides treatment guidelines for managing acute rheumatic fever, including eradicating streptococcal infections, relieving pain, managing arthritis/chorea, and treating carditis complications. Disease-modifying corticosteroid treatments are also recommended for severe symptoms.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 3
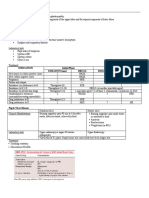
Diagnosis of acute rheumatic fever
2020 Updated Australian criteria for ARF diagnosis
HIGH-RISK GROUPS† LOW-RISK GROUPS
Definite initial 2 major manifestations + evidence of preceding Strep A infection, or
episode of ARF
1 major + 2 minor manifestations + evidence of preceding Strep A infection‡
Definite recurrent§ 2 major manifestations + evidence of preceding Strep A infection, or
episode of ARF
1 major + 2 minor manifestations + evidence of preceding Strep A infection‡,
in a patient with
a documented or
history of ARF 3 minor manifestations + evidence of a preceding Strep A infection‡
or RHD
Probable or A clinical presentation in which ARF is considered a likely diagnosis but falls
possible ARF short in meeting the criteria by either:
(first episode or
recurrence§) • one major or one minor manifestation, or
• no evidence of preceding Strep A infection (streptococcal titres within
normal limits or titres not measured)
Such cases should be further categorised according to the level of confidence
with which the diagnosis is made:
• Probable ARF (previously termed ‘probable: highly suspected’)
• Possible ARF (previously termed ‘probable: uncertain’)
Major Carditis (including subclinical Carditis (including subclinical evidence of
manifestations evidence of rheumatic valvulitis rheumatic valvulitis on echocardiogram)
on echocardiogram)
Polyarthritis¶
Polyarthritis¶ or aseptic
Sydenham chorea††
monoarthritis or polyarthralgia
Erythema marginatum‡‡
Sydenham chorea††
Subcutaneous nodules
Erythema marginatum‡‡
Subcutaneous nodules
Minor Fever§§ ≥38°C Fever ≥38.5°C
Manifestations
Monoarthralgia ¶¶
Polyarthralgia or aseptic monoarthritis¶¶
ESR ≥30 mm/h or CRP ≥30 mg/L ESR ≥60 mm/h or CRP ≥30 mg/L
Prolonged P-R interval on ECG †††
Prolonged P-R interval on ECG†††
. Risk groups for ARF
At high risk Living in an ARF-endemic setting†
Aboriginal and/or Torres Strait Islander peoples living in rural or remote
settings
Aboriginal and/or Torres Strait Islander peoples, and Māori and/or Pacific
Islander peoples living in metropolitan households affected by crowding and/
or lower socioeconomic status
Personal history of ARF/RHD and aged <40 years
May be at Family or household recent history of ARF/RHD
high risk
Household overcrowding (>2 people per bedroom) or low socioeconomic
status
Migrant or refugee from low- or middle-income country and their children
Additional Prior residence in a high ARF risk setting
considerations
Frequent or recent travel to a high ARF risk setting
which increase
risk Aged 5-20 years (the peak years for ARF)
Management of Acute Rheumatic Fever
INDICATION MEDICATION OPTIONS LISTED IN ORDER OF PREFERENCE
Eradication of inciting 1. Benzathine benzylpenicillin G (BPG) 1,200,000 units (child <20 kg: 600,000
units; ≥20 kg: 1,200,000 units) IMI single dose
streptococcal infection
Or
2. Phenoxymethylpenicillin 500 mg (child: 15 mg/kg up to 500 mg)
orally 12-hourly for 10 days
3. Penicillin hypersensitivity (non-severe): cefalexin 1 g (child: 25
mg/kg up to 1 g) orally, 12-hourly for 10 days
4. Immediate penicillin hypersensitivity: azithromycin 500 mg (child:
12 mg/kg up to 500 mg) orally daily for 5 days
Initial analgesia while awaiting Paracetamol 1000 mg (child 15 mg/kg) orally, 4-hourly up to a maximum of
diagnostic confirmation: 60 mg/kg/day or 4000 mg/day
mild- moderate pain
Initial analgesia while Tramadol immediate-release 50 to 100 mg (child 1 to 2 mg/kg) orally,
awaiting diagnostic 4-hourly up to a maximum of 400 mg/day
confirmation: severe pain
Symptomatic management of 1. Naproxen immediate-release 250-500 mg (child 10–20 mg/kg/day) orally
arthritis/arthralgia twice daily, up to a maximum of 1250 mg daily
after confirmation of ARF Or
diagnosis 2. Ibuprofen 200-400 mg (child 5-10 mg/kg) orally three times daily, up to a
maximum of 2400 mg daily
Or
3. Aspirin adults and children 50-60 mg/kg/day orally, in four to five divided
doses. Dose can be escalated up to a maximum of 80-100 mg/kg/day in
four to five divided doses.
Symptomatic management of 1. Carbamazepine 3.5 to 10 mg/kg per dose orally, twice daily
moderate to severe 2. Sodium valproate 7.5 to 10 mg/kg per dose orally, twice daily
chorea
Symptomatic management In addition to an anticonvulsant agent, consider adding corticosteroid:
of very severe chorea / Prednisone/prednisolone 1 to 2 mg/kg up to a maximum of 80 mg orally,
chorea paralytica once daily or in divided doses
Symptomatic management Paediatric dosing:
of carditis Furosemide (frusemide) 1 to 2 mg/kg orally as a single dose, then 0.5 to
1 mg/kg (to a maximum of 6 mg/kg) orally, 6- to 24-hourly
Spironolactone 1 to 3 mg/kg (initially) up to 100 mg orally, daily in 1 to 3
divided doses. Round dose to a multiple of 6.25 mg (a quarter of a 25 mg
tablet).
Enalapril 0.1 mg/kg orally, daily in 1 or 2 divided doses increased
gradually over 2 weeks to a maximum of 1 mg/kg orally, daily in 1 or
2 divided doses, other ACE inhibitors (captopril, lisinopril, ramipril,
perindopril)
Adult dosing:
Furosemide (frusemide) 20–40 mg oral or intravenous as a single dose
followed by 20–40 mg oral or intravenous 8–12 hourly. Ongoing dose
adjustment based on clinical progression and renal function.
Spironolactone may be added for patients having limited or no response
to loop diuretic, 12.5–25 mg spironolactone orally daily
Nitrate therapy may be added for patients having limited or no response
to diuretic therapy, whose systolic blood pressure is greater than 90
mmHg. Intravenous or topical glyceryl trinitrate may be used.
ACE inhibitor is recommended in patients with moderate or severe left
ventricular systolic dysfunction, unless contraindicated
Digoxin 15 micrograms/kg orally, as a single dose, then 5 micrograms/kg
after 6 hours, then 3–5 micrograms/kg (adult: 125–250 micrograms) orally,
daily
Disease-modifying Prednisone/prednisolone 1 to 2 mg/kg up to a maximum of 80 mg orally,
(immunomodulatory) once daily or in divided doses
treatments
You might also like
- Pediatric Drug Dosage - All in One PDFDocument15 pagesPediatric Drug Dosage - All in One PDFHuang Hasjim33% (9)
- John Chambers, Sandeep S. Hothi, Camelia DemetrescuDocument269 pagesJohn Chambers, Sandeep S. Hothi, Camelia DemetrescuGianina CraiaNo ratings yet
- Hypertension in PregnancyDocument20 pagesHypertension in PregnancyFAMED RESIDENTS CESMED100% (1)
- FNCP Category and PrioritizationDocument8 pagesFNCP Category and PrioritizationJapeth John M. FloresNo ratings yet
- Final Haad (DOH) ExamDocument9 pagesFinal Haad (DOH) ExamsenthamizhselvanNo ratings yet
- Common Tropical Disease in ThailandDocument84 pagesCommon Tropical Disease in ThailandDr.Sathaporn KunnathumNo ratings yet
- ConnectorDocument4 pagesConnectoryetaung8No ratings yet
- Febrile SeizureDocument32 pagesFebrile SeizureShiva Valeska ArdhaniswariNo ratings yet
- 37 - Acute Rheumatic FeverDocument1 page37 - Acute Rheumatic FevernasibdinNo ratings yet
- Gestational HypertensionDocument30 pagesGestational Hypertensionarsalanahmadifar78No ratings yet
- Medicine OSCE - Common Diseases Ver1Document4 pagesMedicine OSCE - Common Diseases Ver1TrisNo ratings yet
- Anthelmintics: Antiparasitic Parasitic Worms HelminthsDocument9 pagesAnthelmintics: Antiparasitic Parasitic Worms HelminthsFredeluces, Lei Ann S.No ratings yet
- Pedia Drug StudyDocument11 pagesPedia Drug StudyPeetah PanNo ratings yet
- Weekly Drug CardsDocument43 pagesWeekly Drug CardsErica SanchezNo ratings yet
- Seizures/Epilepsy: Case PersentationDocument14 pagesSeizures/Epilepsy: Case PersentationAbdulmalik AliNo ratings yet
- File1 146 1714383Document366 pagesFile1 146 1714383Mutiara SazkiaNo ratings yet
- Tatalaksana Malaria Terkini Pada AnakDocument61 pagesTatalaksana Malaria Terkini Pada Anakretno adijayaNo ratings yet
- Dosis MimsDocument21 pagesDosis MimsYulia Putri CarlianaNo ratings yet
- General: Genetic Implications: Pronunciation: Maz Trade Name(s)Document7 pagesGeneral: Genetic Implications: Pronunciation: Maz Trade Name(s)jenm1228No ratings yet
- ASM Use Childhood Epilepsy PDFDocument7 pagesASM Use Childhood Epilepsy PDFIchrak GhachemNo ratings yet
- Group 5Document66 pagesGroup 5Cms CSUNo ratings yet
- Medication FlashcardsDocument10 pagesMedication FlashcardsSilvio PerezNo ratings yet
- Pediatric Drug Dosing GuidelinesDocument182 pagesPediatric Drug Dosing GuidelinesamiratolanNo ratings yet
- AzithromycinDocument4 pagesAzithromycinBrittany ClontzNo ratings yet
- Nephrotic SyndromeDocument6 pagesNephrotic SyndromeSanthosh KumarNo ratings yet
- Nephrotic Syndrome: BackgroundDocument7 pagesNephrotic Syndrome: BackgroundRiko JumattullahNo ratings yet
- 2021 Final - COVID 19 IN CHILDREN PROTOCOLDocument12 pages2021 Final - COVID 19 IN CHILDREN PROTOCOLSutirtha RoyNo ratings yet
- Drug Study Batch 1Document17 pagesDrug Study Batch 1John Philip M. Lacas RNNo ratings yet
- Drug Formulary Updated 2.12.09Document1,201 pagesDrug Formulary Updated 2.12.09மகெஷ்வாரென் தன்னிமலைNo ratings yet
- Nephrotic Syndrome in Children: Rahma Bagian Ilmu Kesehatan Anak Fkik UntadDocument11 pagesNephrotic Syndrome in Children: Rahma Bagian Ilmu Kesehatan Anak Fkik UntadSunaryo KRKNo ratings yet
- Acute Rheumatic Fever and Rheumatic Heart Disease: Ria NovaDocument36 pagesAcute Rheumatic Fever and Rheumatic Heart Disease: Ria NovaaisyahNo ratings yet
- Anti Parasites Blok 3.2Document46 pagesAnti Parasites Blok 3.2Alda Herlen Kalkarina BangunNo ratings yet
- AcetaminophenDocument3 pagesAcetaminophenShaira Tan100% (1)
- IMCI TECHNICAL UPDATES: The KEY To Your Success!! Pls..... Read.. Read.. Read.Document10 pagesIMCI TECHNICAL UPDATES: The KEY To Your Success!! Pls..... Read.. Read.. Read.Kim RamosNo ratings yet
- MALARIA Tatalaksana Dewasa PWT PBG 2019Document34 pagesMALARIA Tatalaksana Dewasa PWT PBG 2019roniNo ratings yet
- Therapeutic:: Brand Name: PLASIL ClassificationsDocument5 pagesTherapeutic:: Brand Name: PLASIL ClassificationsAbby MontealegreNo ratings yet
- Furosemide Mims EngDocument17 pagesFurosemide Mims EngNur Ilmi SofiahNo ratings yet
- MalariaDocument38 pagesMalariaMehroze FatimaNo ratings yet
- Dr. Anati Purwakanthi, MSC Departemen Farmakologi Fkik UnjaDocument40 pagesDr. Anati Purwakanthi, MSC Departemen Farmakologi Fkik Unjaanes tiraNo ratings yet
- Infectious Disease - BoardsDocument8 pagesInfectious Disease - BoardsSoojung NamNo ratings yet
- Adult: PO HTN As Conventional Tab or Oral Soln: Initial: 40-80 MG Bid. Usual Range: 160Document3 pagesAdult: PO HTN As Conventional Tab or Oral Soln: Initial: 40-80 MG Bid. Usual Range: 160berliana agustinNo ratings yet
- Malaria Is A Disease Caused by Parasites of The Genus PlasmodiumDocument4 pagesMalaria Is A Disease Caused by Parasites of The Genus PlasmodiumDungani AllanNo ratings yet
- Integrated Management of Childhood IllnessesDocument30 pagesIntegrated Management of Childhood IllnessesKen Rex BarcelonNo ratings yet
- AIIMS Issues New Guidelines For Treatment of CovidDocument7 pagesAIIMS Issues New Guidelines For Treatment of Covidsenthil kumarNo ratings yet
- Medications: Medication Name Generic/Trade Classification Pregnancy CategoryDocument8 pagesMedications: Medication Name Generic/Trade Classification Pregnancy CategoryapalestiNo ratings yet
- National Malaria Drug PolicyDocument22 pagesNational Malaria Drug Policydocsaurabh777No ratings yet
- Lecture 11. Acute and Chronic Glomerulonephritis, Pediatric HypertensionDocument30 pagesLecture 11. Acute and Chronic Glomerulonephritis, Pediatric HypertensionkrisnadewirahadiNo ratings yet
- Tuberculosis Treatment Guide & Patient InformationDocument4 pagesTuberculosis Treatment Guide & Patient InformationShila LupiyatamaNo ratings yet
- Nephrotic Syndrome in Children: Nama: Anjaya Pratama Putra Kelas: 4aDocument11 pagesNephrotic Syndrome in Children: Nama: Anjaya Pratama Putra Kelas: 4aSunaryo KRKNo ratings yet
- Drug StudyDocument9 pagesDrug StudyChristine PunsalanNo ratings yet
- Approach To Acute GastroenteritisDocument15 pagesApproach To Acute GastroenteritisMelissa TisadoNo ratings yet
- Community Cheat CodeDocument19 pagesCommunity Cheat Codeeuphrosyne92No ratings yet
- College of Nursing: Pharmacology Drug StudyDocument2 pagesCollege of Nursing: Pharmacology Drug StudyChristine Pialan SalimbagatNo ratings yet
- Albendazole - Drug Information PDFDocument7 pagesAlbendazole - Drug Information PDFjjjkkNo ratings yet
- Drug StudDocument31 pagesDrug StudTwisted FlameNo ratings yet
- 5 Drug RecomendDocument4 pages5 Drug RecomendNama ManaNo ratings yet
- Treatment Protocol Against Covid 19 From WWW - Ippocrateorg.orgDocument4 pagesTreatment Protocol Against Covid 19 From WWW - Ippocrateorg.orgJohnuri MoraNo ratings yet
- 3 Hypertension in PregnancyDocument36 pages3 Hypertension in PregnancySwee WaiNo ratings yet
- Cardiology Doses: WhiteknightloveDocument3 pagesCardiology Doses: WhiteknightloveSelim TarekNo ratings yet
- Course Task 10Document29 pagesCourse Task 10Katrina AballaNo ratings yet
- AIIMS Issues New Guidelines For Treatment of Covid-19 Cases: (Enter Post Title Here)Document7 pagesAIIMS Issues New Guidelines For Treatment of Covid-19 Cases: (Enter Post Title Here)senthil kumarNo ratings yet
- Sample NCP in Format Color CodedDocument4 pagesSample NCP in Format Color CodedinsadauNo ratings yet
- Pathophysiology of Type 1 DiabetesDocument14 pagesPathophysiology of Type 1 DiabetesBoNo ratings yet
- Final Online Exam Guideline CBTDocument105 pagesFinal Online Exam Guideline CBTfaisalaminwani121No ratings yet
- Verbatim: Ministry of Health Directorate of Public Counselling Services and Training UnitDocument12 pagesVerbatim: Ministry of Health Directorate of Public Counselling Services and Training Unitfredrick kaheha100% (1)
- IvdpDocument2 pagesIvdpSubramanya RaoNo ratings yet
- Breast CancerDocument23 pagesBreast CancerCiocan AlexandraNo ratings yet
- Ch7 To Post On JUMPDocument50 pagesCh7 To Post On JUMPidkNo ratings yet
- Laboratory Rules and Regulation: Brief History of SiwesDocument12 pagesLaboratory Rules and Regulation: Brief History of Siwesgolden abidemNo ratings yet
- WHO Is Peter DaszakDocument170 pagesWHO Is Peter Daszakjb_uspuNo ratings yet
- Disorders of The Nose and Paranasal SinusesDocument50 pagesDisorders of The Nose and Paranasal Sinusesphew1234567890No ratings yet
- Alpha Dent Implants Online Book Customers Reviews and Clinical CasesDocument32 pagesAlpha Dent Implants Online Book Customers Reviews and Clinical CasesAlphaDentNo ratings yet
- (123doc) - Funggal-SinusitisDocument58 pages(123doc) - Funggal-SinusitisUchiha MandaizanNo ratings yet
- Curriculum Vitae DR SumitDocument3 pagesCurriculum Vitae DR SumitdrsumitpuriNo ratings yet
- O@g Maternal and Fetal Mesures ContentDocument22 pagesO@g Maternal and Fetal Mesures Contentjeya maniNo ratings yet
- Hematology CLL, ММ tableDocument4 pagesHematology CLL, ММ tableShur .ENo ratings yet
- Pharma 4 QDocument1 pagePharma 4 QMARIA PAULINA AMANTENo ratings yet
- Developmental Disabilities in Infancy & Childhood: Neurodevelopmental PediatricianDocument75 pagesDevelopmental Disabilities in Infancy & Childhood: Neurodevelopmental PediatricianCarol Rombaoa Serdenia100% (1)
- Cholecystitis Case StudyDocument7 pagesCholecystitis Case StudyElle MongeNo ratings yet
- Recording A 12-Lead Electrocardiogram (ECG)Document4 pagesRecording A 12-Lead Electrocardiogram (ECG)brianNo ratings yet
- Standards of Care in Diabetes - 2023Document12 pagesStandards of Care in Diabetes - 2023Menethil Terenas ElijiahNo ratings yet
- Urine Glucose TestDocument6 pagesUrine Glucose TestSelim HanNo ratings yet
- ACEM PostersDocument2 pagesACEM PostersDr.KHAJA SHAFIUDDINNo ratings yet
- 2nd Year AntidoteDocument100 pages2nd Year Antidoteshafeeque TNo ratings yet
- Comparison RepertoryDocument3 pagesComparison RepertorySuhasSkyNo ratings yet
- NEQAS - AnswersDocument6 pagesNEQAS - AnswerssandheeaNo ratings yet
- Oet Granular FeverDocument7 pagesOet Granular FeverSajal ShresthaNo ratings yet
- Class 11 - Physical EducationDocument4 pagesClass 11 - Physical EducationRishit BaranwalNo ratings yet
- Activity #1 (PT)Document2 pagesActivity #1 (PT)Ashley AgustinNo ratings yet