Professional Documents
Culture Documents
Wen 2023 Oi 230763 1689947066.86962
Wen 2023 Oi 230763 1689947066.86962
Uploaded by
JEAN GEMCopyright:
Available Formats
You might also like
- Elective 8 New Market Development ModuleDocument91 pagesElective 8 New Market Development Modulejulius80% (10)
- ABO AnalysisDocument38 pagesABO AnalysisMa Lyn Gabayeron75% (4)
- Roots & DerivsDocument17 pagesRoots & DerivsAbir Chowdhury100% (2)
- Prevalence of Tumor Genomic Alterations in Homologous Recombination Repair Genes Among Taiwanese Breast CancersDocument13 pagesPrevalence of Tumor Genomic Alterations in Homologous Recombination Repair Genes Among Taiwanese Breast Cancers郭竹瑩No ratings yet
- Godone 2018Document21 pagesGodone 2018Roberta GodoneNo ratings yet
- Rakha Et Al. 2006 Prognostic Markers in Triple Negative Breast CancerDocument8 pagesRakha Et Al. 2006 Prognostic Markers in Triple Negative Breast CancerdanishNo ratings yet
- Jamaoncology Mavaddat 2022 Oi 210095 1647458350.98716Document11 pagesJamaoncology Mavaddat 2022 Oi 210095 1647458350.98716Daira Gabriela Ormachea ArancibiaNo ratings yet
- 6880-Article Text-54409-3-10-20231020Document12 pages6880-Article Text-54409-3-10-20231020Selma Mutiara HaniNo ratings yet
- Breast Cancer in Indian Women Genetic Risk Factor and Predictive BiomarkerDocument14 pagesBreast Cancer in Indian Women Genetic Risk Factor and Predictive Biomarkermicrogmcapur2016No ratings yet
- Nejmoa 2105215Document12 pagesNejmoa 2105215cejigip953No ratings yet
- Impact of Breast Cancer Subtypes On Prognosis of Women With Operable Invasive Breast Cancer: A Population-Based Study Using SEER DatabaseDocument10 pagesImpact of Breast Cancer Subtypes On Prognosis of Women With Operable Invasive Breast Cancer: A Population-Based Study Using SEER DatabasesilviatengkerNo ratings yet
- 410-Article Text-1440-1-10-20211018Document7 pages410-Article Text-1440-1-10-20211018silviatengkerNo ratings yet
- Fertility Treatments and Invasive Epithelial Ovarian Cancer 2015 Fertility ADocument8 pagesFertility Treatments and Invasive Epithelial Ovarian Cancer 2015 Fertility Ajayeto4038No ratings yet
- Genetica 1Document9 pagesGenetica 1Jose Andres DiazNo ratings yet
- Kumar 2015Document5 pagesKumar 2015Isuploaded BlogspotcomNo ratings yet
- Centrosome-Related Genes, Genetic Variation, and Risk of Breast CancerDocument9 pagesCentrosome-Related Genes, Genetic Variation, and Risk of Breast CancerSari RiastiningsihNo ratings yet
- 10 1053@j Seminoncol 2016 10 001Document8 pages10 1053@j Seminoncol 2016 10 001rikudoutobiNo ratings yet
- Germline Breast Cancer SuspectibiliyDocument13 pagesGermline Breast Cancer SuspectibiliyDominick Dayton FinettiNo ratings yet
- 1 s2.0 S0893395222028435 MainDocument8 pages1 s2.0 S0893395222028435 MainSmit ShahNo ratings yet
- CA de MamaDocument106 pagesCA de MamaDamián López RangelNo ratings yet
- Naderi Et Al-2019-Molecular Genetics & Genomic Medicine PDFDocument7 pagesNaderi Et Al-2019-Molecular Genetics & Genomic Medicine PDFgeorgiaNo ratings yet
- Gulbahce 2016Document5 pagesGulbahce 2016Valir HusleNo ratings yet
- Advances in Screening, Diagnosis, and Treatment ofDocument7 pagesAdvances in Screening, Diagnosis, and Treatment ofBastomy EkaNo ratings yet
- The Genetics and Clinical Outcomes in 151 Cases OfDocument7 pagesThe Genetics and Clinical Outcomes in 151 Cases Ofzeni okta wiyantiNo ratings yet
- Complex Fibroadenoma and Breast Cancer RiskDocument15 pagesComplex Fibroadenoma and Breast Cancer RisktatianaNo ratings yet
- MTHFR/p53 Polymorphisms As Genetic Factors For Cervical Intraepithelial Neoplasia and Cervical Cancer in HPV-infected Mexican WomenDocument9 pagesMTHFR/p53 Polymorphisms As Genetic Factors For Cervical Intraepithelial Neoplasia and Cervical Cancer in HPV-infected Mexican WomenIrina Surco RodríguezNo ratings yet
- Journal Medicine: The New EnglandDocument11 pagesJournal Medicine: The New EnglandMohiuddin JishanNo ratings yet
- Ajol File Journals - 494 - Articles - 112408 - Submission - Proof - 112408 5833 311975 1 10 20150203Document5 pagesAjol File Journals - 494 - Articles - 112408 - Submission - Proof - 112408 5833 311975 1 10 20150203KeHuyDietNo ratings yet
- Prognostic Value of p53 Gene in Ovarian Cancer: - Maj Obstet 172 Rauf Dan Masadah Ginekol IndonesDocument5 pagesPrognostic Value of p53 Gene in Ovarian Cancer: - Maj Obstet 172 Rauf Dan Masadah Ginekol IndonesDini MedyaniNo ratings yet
- Germline Mutations in Predisposition Genes in Pediatric CancerDocument11 pagesGermline Mutations in Predisposition Genes in Pediatric CancerGuadalupeA.OsorioNo ratings yet
- Jurnal 1Document13 pagesJurnal 1Aqshal Ilham OktoriNo ratings yet
- Proof: Gynecologic OncologyDocument2 pagesProof: Gynecologic OncologyCamilaBurgosNo ratings yet
- Meijers Heijboer2001Document6 pagesMeijers Heijboer2001Market PlusNo ratings yet
- Advances in The Molecular Taxonomy of Breast CancerDocument7 pagesAdvances in The Molecular Taxonomy of Breast CancerbrendaNo ratings yet
- Fmolb 11 1394585Document18 pagesFmolb 11 1394585Rodrigo SierraNo ratings yet
- A Review of Triple-Negative Breast Cancer: Nick Patten. Last Light (Detail) - Oil On Canvas, 44" × 56"Document4 pagesA Review of Triple-Negative Breast Cancer: Nick Patten. Last Light (Detail) - Oil On Canvas, 44" × 56"Kritik KumarNo ratings yet
- Carcinoma: BRCA-Mutation-Associated Fallopian TubeDocument8 pagesCarcinoma: BRCA-Mutation-Associated Fallopian Tubew yNo ratings yet
- Expression of Mirnas and Pten in Endometrial Specimens Ranging From Histologically Normal To Hyperplasia and Endometrial AdenocarcinomaDocument9 pagesExpression of Mirnas and Pten in Endometrial Specimens Ranging From Histologically Normal To Hyperplasia and Endometrial AdenocarcinomaFerdina NidyasariNo ratings yet
- 2017 Article 52-2Document9 pages2017 Article 52-2Lorena RamosNo ratings yet
- Oncollogy 3Document9 pagesOncollogy 3AG LarikNo ratings yet
- Onkogenesis, Morfologi, Dan Modalitas Deteksi Dini Karsinoma ServiksDocument14 pagesOnkogenesis, Morfologi, Dan Modalitas Deteksi Dini Karsinoma ServiksJuschella SumakulNo ratings yet
- Cervical Cancer: Prevention, Diagnosis, and TherapeuticsDocument23 pagesCervical Cancer: Prevention, Diagnosis, and TherapeuticsranggadrNo ratings yet
- Diagnosing Hereditary Cancer Predisposition in MenDocument7 pagesDiagnosing Hereditary Cancer Predisposition in MenSaurabh SharmaNo ratings yet
- Safety and Efficacy of Pembrolizumab in Advanced, Programmed Death Ligand 1-Positive Cervical CancerDocument9 pagesSafety and Efficacy of Pembrolizumab in Advanced, Programmed Death Ligand 1-Positive Cervical CancerluizaNo ratings yet
- Atchley Et Al 2016 Clinical and Pathologic Characteristics of PatientsDocument7 pagesAtchley Et Al 2016 Clinical and Pathologic Characteristics of PatientsWojtek JanotaNo ratings yet
- NIH Public Access: Author ManuscriptDocument23 pagesNIH Public Access: Author ManuscriptGustavo IbarraNo ratings yet
- Cáncer OralDocument7 pagesCáncer OralValery MedinaNo ratings yet
- BRCA1 Gene Mutations in Breast Cancer Patients From Kerman Province, IranDocument6 pagesBRCA1 Gene Mutations in Breast Cancer Patients From Kerman Province, IranMohammed AladhraeiNo ratings yet
- Brjcancer00189 0144cDocument2 pagesBrjcancer00189 0144cZhangYixing EXOSNo ratings yet
- Matsuo 2018Document14 pagesMatsuo 2018Mahmudur Rahman27No ratings yet
- Molecular Diagnosis in Breast Cancer: Mini-Symposium: Breast PathologyDocument12 pagesMolecular Diagnosis in Breast Cancer: Mini-Symposium: Breast PathologyOber Van Gómez LópezNo ratings yet
- PJSS 66 3 Jul Sep 2011 3Document9 pagesPJSS 66 3 Jul Sep 2011 3Dwight AvelinoNo ratings yet
- MJZ 033Document10 pagesMJZ 033metrorespoNo ratings yet
- The Clinicopathological Features of Breast Carcinoma Cases in Adiwaniyah Province in IraqDocument11 pagesThe Clinicopathological Features of Breast Carcinoma Cases in Adiwaniyah Province in IraqCentral Asian StudiesNo ratings yet
- Editorial: Lung Cancer: Prevalent Trends & Emerging ConceptsDocument3 pagesEditorial: Lung Cancer: Prevalent Trends & Emerging Conceptsjeevan georgeNo ratings yet
- 1 s2.0 S003130251640365X MainDocument9 pages1 s2.0 S003130251640365X MainbrendaNo ratings yet
- Cytologic Patterns of Cervical Adenocarcinomas With Emphasis On Factors Associated With Underdiagnosis - Tumor DiathesisDocument9 pagesCytologic Patterns of Cervical Adenocarcinomas With Emphasis On Factors Associated With Underdiagnosis - Tumor Diathesisnakemi111No ratings yet
- La Mellarin D2Document2 pagesLa Mellarin D2JESUS DAVID BOLA‹O JIMENEZNo ratings yet
- 3 PDFDocument24 pages3 PDFdindaNo ratings yet
- Biomarkers in Breast Cancer 2024: An Updated Consensus Statement by The Spanish Society of Medical Oncology and The Spanish Society of PathologyDocument17 pagesBiomarkers in Breast Cancer 2024: An Updated Consensus Statement by The Spanish Society of Medical Oncology and The Spanish Society of PathologyellyanaperwitasariNo ratings yet
- "OMIC" Tumor Markers For Breast Cancer: A ReviewDocument7 pages"OMIC" Tumor Markers For Breast Cancer: A ReviewwardaninurindahNo ratings yet
- Link ClassificationDocument12 pagesLink ClassificationluisalbertomendozapuNo ratings yet
- 2023 40668 Moesm3 EsmDocument3 pages2023 40668 Moesm3 EsmJEAN GEMNo ratings yet
- Project Muse 882910Document23 pagesProject Muse 882910JEAN GEMNo ratings yet
- The Impact of Translation Memory SegmentationDocument18 pagesThe Impact of Translation Memory SegmentationJEAN GEMNo ratings yet
- Proposal For A Translanguaging Space' in Interpreting StudiesDocument21 pagesProposal For A Translanguaging Space' in Interpreting StudiesJEAN GEMNo ratings yet
- Reflexology New Patient FormDocument7 pagesReflexology New Patient FormOana Iftimie100% (2)
- Chauhan / Gupta Homeophatic Principles and Practice of MedicineDocument10 pagesChauhan / Gupta Homeophatic Principles and Practice of Medicinems.anitha1980No ratings yet
- What Are CarbohydratesDocument7 pagesWhat Are CarbohydratesconstantinNo ratings yet
- Celiac Disease PathophysiologyDocument28 pagesCeliac Disease PathophysiologyIsmy HoiriyahNo ratings yet
- Home Remedies Using Mustard Seeds Prophet666Document2 pagesHome Remedies Using Mustard Seeds Prophet666Hussainz AliNo ratings yet
- tmp4946 TMPDocument27 pagestmp4946 TMPFrontiersNo ratings yet
- Electrical SafetyDocument3 pagesElectrical SafetyPerwez21No ratings yet
- Monitoring & Devices Used in ICU CCUDocument48 pagesMonitoring & Devices Used in ICU CCUProf. Ramsharan Mehta100% (1)
- Vamana Karma-Understanding Mode of ActionDocument12 pagesVamana Karma-Understanding Mode of ActionsmsmastiNo ratings yet
- Generalization and Stereotype in Counseling - Implication and Caution in Clinical Setting.Document15 pagesGeneralization and Stereotype in Counseling - Implication and Caution in Clinical Setting.Nishesh AcharyaNo ratings yet
- Module 3 - SociologyDocument74 pagesModule 3 - SociologyakshayaNo ratings yet
- Contingency Plan FormatDocument2 pagesContingency Plan FormatNagarajanNo ratings yet
- Chapter 10Document17 pagesChapter 10Bryle Dela TorreNo ratings yet
- Dezinfeqcia SterilizaciaDocument29 pagesDezinfeqcia SterilizaciaLuka KhvichiaNo ratings yet
- Radiology Abdomen InterpretationsDocument108 pagesRadiology Abdomen InterpretationsStudent100% (1)
- Arteritis TemporalisDocument5 pagesArteritis TemporalisbagasNo ratings yet
- Paul Saville For Mayor of Bristol 2016Document5 pagesPaul Saville For Mayor of Bristol 2016Paul SavilleNo ratings yet
- 114 247 1 SMDocument6 pages114 247 1 SMAzhar FauzanNo ratings yet
- Rule 1040 - Health and Safety CommitteeDocument10 pagesRule 1040 - Health and Safety Committeerobinrubina50% (2)
- SteraminDocument1 pageSteraminnodi79No ratings yet
- BiographyDocument7 pagesBiographyapi-348852766No ratings yet
- A Series of MCQ Type Online Practice Test On MANAGEMENT (22509) (Unit - IV)Document27 pagesA Series of MCQ Type Online Practice Test On MANAGEMENT (22509) (Unit - IV)S V67% (3)
- Dental IndicesDocument54 pagesDental IndicesrajshreeNo ratings yet
- Mater Maternity Booking Form V2 - March17 (Not For Record)Document1 pageMater Maternity Booking Form V2 - March17 (Not For Record)Oliver JanevNo ratings yet
- Book ItemDocument28 pagesBook ItemAnwesha PadhanNo ratings yet
- Induction Program ScriptDocument2 pagesInduction Program ScriptAl-var A AtibingNo ratings yet
- Descriptive Questions Asked in Previous Years IBPS PO Mains ExamDocument5 pagesDescriptive Questions Asked in Previous Years IBPS PO Mains ExamAnwesha SahooNo ratings yet
Wen 2023 Oi 230763 1689947066.86962
Wen 2023 Oi 230763 1689947066.86962
Uploaded by
JEAN GEMOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Wen 2023 Oi 230763 1689947066.86962
Wen 2023 Oi 230763 1689947066.86962
Uploaded by
JEAN GEMCopyright:
Available Formats
Original Investigation | Oncology
Prevalence and Landscape of Pathogenic or Likely Pathogenic Germline Variants
and Their Association With Somatic Phenotype in Unselected Chinese Patients
With Gynecologic Cancers
Hao Wen, MD; Qin Xu, PhD; Xiujie Sheng, PhD; Huawen Li, MD; Xipeng Wang, PhD, MD; Xiaohua Wu, PhD
Abstract Key Points
Question What is the prevalence and
IMPORTANCE Understanding germline and somatic status in patients with gynecologic cancers
landscape of pathologic or likely
could improve risk assessment and guide therapeutic decision-making.
pathologic (P/LP) germline variants, and
are they associated with somatic
OBJECTIVE To evaluate the prevalence and landscape of germline pathogenic or likely pathogenic
phenotype in unselected patients with
(P/LP) variants and explore whether these variants are associated with somatic phenotypes and
gynecologic cancers?
cancer risk in unselected patients with gynecologic cancers.
Findings This cross-sectional study of
DESIGN, SETTING, AND PARTICIPANTS This cross-sectional study retrospectively enrolled 1610 unselected patients with a
unselected patients in China with a gynecologic cancer, including ovarian, cervical, and endometrial, gynecologic cancer revealed a P/LP
who underwent tumor-normal sequencing using a 520-gene panel from October 1, 2017, through germline variant prevalence of 20.5%
May 31, 2021. for ovarian cancer, 13.4% for
endometrial cancer, and 6.4% for
EXPOSURE Germline variants in gynecologic cancers. cervical cancer, 95.1% of which were in
homologous recombination repair and
MAIN OUTCOMES AND MEASURES The P/LP germline variant rates in 62 cancer predisposition mismatch repair genes. These germline
genes were assessed using descriptive statistics. The associations of P/LP variant status with age, findings also revealed tumor lineage
somatic profiles, and cancer risk were also investigated using the Fisher exact test or Student t test. and gene-dependent associations with
the age of disease onset and somatic
RESULTS A total of 1610 women (median [IQR] age, 54 [47-62] years; 1201 [74.6%] with stage III-IV phenotype.
disease) were included (945 with ovarian cancer, 307 with endometrial cancer, and 358 with cervical
Meaning These findings highlight the
cancer). The prevalence of patients with P/LP variants was 20.5% (194 of 945) for ovarian cancer,
hereditary factor in cervical cancer,
13.4% (41 of 307) for endometrial cancer, and 6.4% (23 of 358) for cervical cancer; 95.1% of the
which has long been neglected and
germline findings (n = 252) were potentially actionable, mainly in homologous recombination repair
raises the importance of next-
(HRR) and mismatch repair genes. Chinese patients with endometrial cancer had a higher rate of
generation sequencing–based genetic
P/LP variants than a White population from The Cancer Genome Atlas (42 of 307 [13.7%] vs 24 of 367
testing with a large gene panel for
[6.5%]; P = .003). In endometrial and cervical cancers, the prevalence of P/LP variants was 12.7%
gynecologic cancers.
(30 of 237) and 4.8% (13 of 270), respectively, in patients diagnosed at age 45 years or older and
increased to 25.0% (9 of 36; P = .09) and 12.0% (10 of 83; P = .04), respectively, for those with an
onset age of less than 45 years. Mismatch repair P/LP variants were associated with a younger age at + Supplemental content
onset for ovarian cancer (46 vs 54 years; P = .02) and endometrial cancer (48 vs 57 years; P < .001), Author affiliations and article information are
while HRR P/LP variants were associated with a younger age at onset for cervical cancer (46 vs 52 listed at the end of this article.
years; P = .04). Carriers of HRR P/LP variants had more prevalent somatic TP53 variants and less
common somatic variants in oncogenic driver genes vs noncarriers. BRCA1/2 P/LP variants were also
associated with moderate risks for endometrial and cervical cancer.
CONCLUSIONS AND RELEVANCE This study delineates the landscape of germline P/LP variants in
Chinese women with gynecologic cancers. The findings highlight the hereditary factor in cervical
(continued)
Open Access. This is an open access article distributed under the terms of the CC-BY License.
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 1/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
JAMA Network Open | Oncology Germline Variants in Gynecologic Cancers Among Patients in China
Abstract (continued)
cancer that has long been neglected and suggest the importance of next-generation sequencing–
based genetic testing with a large gene panel for gynecologic cancers.
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437
Introduction
Cancers of the female genital tract include ovarian, corpus uteri (mainly endometrial), cervical, vulvar,
and vaginal tumors. These gynecologic tumors account for 15% to 20% of cancer-related deaths in
women worldwide,1-5 with cervical, uterine, and ovarian cancers being the 3 most prevalent. The
2022 cancer statistics for China reported increasing incidence rates for cancers of the cervix and
uterus and an increased mortality rate for cervical cancer during the past decade.6
Women harboring germline pathogenic/likely pathogenic (P/LP) variants have a higher risk of
developing cancers, including gynecologic cancers, and at an earlier age of onset. Approximately 10%
to 20% of ovarian cancers and 5% of endometrial cancers are inherited and attributable to
deleterious germline variants.7-12 Autosomal dominant germline variants in genes, including BRCA1
and BRCA2 and those involved in the mismatch repair (MMR) pathway, are associated with an
increased risk of developing hereditary breast and ovarian cancer syndrome and Lynch syndrome,
respectively.13 The lifetime risk of developing ovarian cancer is estimated at 1.5% for the general
population14 and significantly rises to 40% to 60% for BRCA1 and 11% to 30% for BRCA2 pathogenic
variant carriers.7 Individuals harboring a deleterious germline variant in 1 of the MMR genes have a
20% to 70% lifetime risk of developing endometrial cancer.15 In comparison, cervical cancer is more
sporadic and associated with genital infection with oncogenic types of human papillomavirus;
however, the risk of developing minimal deviation adenocarcinoma, a rare variant of cervical cancer,
increases in carriers of STK11 germline variants who have Peutz-Jeghers syndrome.
The use of next-generation sequencing (NGS) has contributed to our current understanding of
germline and somatic alterations involved in cancer development. Next-generation sequencing
enables the simultaneous detection of clinically relevant variants and other genomic signatures that
could guide therapy. With the improving turnaround time and cost-effectiveness of NGS, its
application in clinical practice has grown in the past decade. However, the need for multigene genetic
testing in gynecologic cancers remains limited due to the scarcity of clinically relevant genetic
markers. The European Society of Molecular Oncology Precision Medicine Working Group released
recommendations for the use of large NGS oncopanels for patients with metastatic cancers, including
ovarian and endometrial cancer.16 Understanding the germline and somatic status of these patients
could improve risk assessment and therapeutic management. Germline variants could shape the
somatic landscape,17,18 which could also affect tumor biology, development, and progression.19
In this study, we investigated the landscape of germline P/LP variants in cancer predisposition
genes in a large cohort of unselected Chinese women diagnosed with gynecologic cancers, including
ovarian, endometrial, and cervical. To better understand the mechanism underlying the
tumorigenesis of gynecologic cancers that develop in germline carriers, we also explored the
association of germline variants with somatic profiles and cancer risk.
Methods
Patients
This cross-sectional study included 1610 Chinese women diagnosed with gynecologic cancers who
submitted biological samples for genomic sequencing between October 1, 2017, and May 31, 2021. All
eligible patients provided paired white blood cells for sequencing in parallel with tumor samples,
including tumor biopsy, malignant pleural effusion, cerebrospinal fluid, or plasma. The study was
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 2/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
JAMA Network Open | Oncology Germline Variants in Gynecologic Cancers Among Patients in China
approved by the ethics committee of the Fudan University Shanghai Cancer Center. All patients
provided written informed consent to use their clinical information for research purposes. The study
followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)
reporting guideline.
Next-Generation Sequencing
Paired white blood cells and tumor samples were sequenced using a 520-gene panel (Burning Rock
Biotech), including 62 cancer predisposition genes (eTable 1 in Supplement 1). Details on NGS and the
data analysis are provided in the eMethods in Supplement 1.
Cancer Predisposition Analysis
The association between P/LP germline variants in certain genes and cancer was assessed using the
public gnomAD database20,21 as the reference control, which contains exome sequencing data from
125 748 unrelated individuals. The race and ethnicity–matched East Asian subset was included in this
analysis.
Statistical Analysis
The data analysis was performed using R, version 4.1.0 software (R Foundation for Statistical
Computing). Clinical characteristics were summarized as descriptive statistics. Fisher exact test and
paired 2-tailed Student t test were used to compare groups. Odds ratios (ORs) and corresponding
95% CIs were estimated by Fisher exact test. Statistical significance was defined as a 2-sided P < .05.
Results
Patient Characteristics
Of the 1610 women included in the study, 945 (58.7%) were diagnosed with ovarian cancer, 358
(22.2%) with cervical cancer, and 307 (19.1%) with endometrial cancer (eFigure 1 in Supplement 1).
Most women (1201 [74.6%]) had stage III to IV disease (Table 1). The cohort’s median age was 54
years (IQR, 47-62 years).
Germline P/LP Variants Across Gynecologic Cancers
A total of 265 germline P/LP variants were detected in 26 cancer predisposition genes from 258 of
the 1610 patients (16.0%) (Figure 1A; eTable 2 in Supplement 1). The prevalence was the highest in
Table 1. Clinical Characteristics of the Cohort
No. (%)
Clinical feature Overall (N = 1610) Ovarian (n = 945) Endometrial (n = 307) Cervical (n = 358) P value
Age, 54 (47-62) 54.0 (47-62) 57.0 (51-64) 51 (45-58)
median (IQR), y <.001
ND 151 (9.4) 112 (11.9) 34 (11.1) 5 (1.4)
Clinical stage
I 80 (5.0) 32 (3.4) 34 (11.1) 14 (3.9)
II 261 (16.2) 132 (14.0) 59 (19.2) 70 (19.6)
III 699 (43.4) 458 (48.5) 115 (37.5) 126 (35.2) <.001
IV 502 (31.2) 268 (28.4) 92 (30.0) 142 (39.7)
ND 68 (4.2) 55 (5.8) 7 (2.3) 6 (1.7)
MSI status
MSI-H 64 (4.0) 14 (1.5) 43 (14.0) 7 (2.0)
MSI-L 1 (0.1) 0 1 (0.3) 0
<.001 Abbreviations: MSI-H, high microsatellite instability;
MSS 1277 (79.3) 788 (83.4) 224 (73.0) 265 (74.0)
MSI-L, low microsatellite instability; MSS,
ND 268 (16.6) 143 (15.1) 39 (12.7) 86 (24.0)
microsatellite stable; ND, no data.
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 3/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
JAMA Network Open | Oncology Germline Variants in Gynecologic Cancers Among Patients in China
patients with ovarian cancer (20.5% [194 of 945]), followed by endometrial cancer (13.4% [41 of
307]) and cervical cancer (6.4% [23 of 358]). Among the 265 P/LP variants, most were frameshifts
(129 [48.7%]) and occurred in BRCA1 (118 [44.5%]) and BRCA2 (42 [15.8%]) (eTables 3 and 4 in
Supplement 1). Notably, 95.1% of these variants (n = 252) were potentially therapeutically actionable,
with a prevalence of 15.3% (n = 247) (Figure 1A), most of which were located in homologous
recombination repair (HRR) and MMR genes (Figure 1B). We found 77.0% of P/LP variants (n = 204)
in genes associated with the cancer type where they were identified, and 23.0% (n = 61) had no
canonical association with the cancer.
A total of 200 germline P/LP variants spanning 20 genes were detected in 194 patients with
ovarian cancer (eTables 2 and 4 in Supplement 1). Six patients (3.1%) harbored 2 heterozygous
variants in 2 genes. Most P/LP variants detected in ovarian cancer occurred in HRR genes (183
[91.5%]) (Figure 1B; eTable 3 in Supplement 1). Eight patients (4.1%) had P/LP variants located in
MMR genes. Fifteen P/LP variants (7.5%) were identified in genes that lack canonical association with
ovarian cancer.
A total of 42 germline P/LP variants spanning 18 genes were detected in 41 patients with
endometrial cancer (eTables 2 and 4 in Supplement 1). One patient harbored 2 heterozygous variants
in EGFR and MSH2. In addition to canonical Lynch syndrome–associated MMR genes (17 [40.5%]),
P/LP variants in HRR genes, which are not canonically associated with endometrial cancer, also
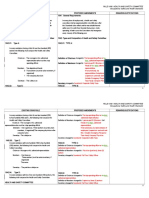
Figure 1. Prevalence of Germline Pathogenic/Likely Pathogenic (P/LP) Variants Across Gynecologic Cancers
A Prevalence of overall and therapeutically actionable germline variants B Germline P/LP variant rates according to genes
25
TP53 1 1 Other genes
Variant class
SDHA 2 2 SDH family
Germline variation rate, %
20 Actionable
Nonactionable EGFR 1 1
Tyrosine kinase
15 RET 2 1 1
NTHL1 1 1
10 NBN 1 1
Other DDR
MSH3 2 2
5
MUTYH 6 3 2 1
PMS2 1 1
0
Total OV EC CC MLH1 4 2 2
MMR
MSH6 7 1 6
C Distribution of different 2-hit events among germline carriers of different genes MSH2 14 4 9 1 Proportion, %
Biallelic status Germ+ LOH_germ+ Somatic_germ+ FANCL 1 1
9
OV EC CC RAD51B 2 2 6
P < .001 P = .002 P = .07 CHEK2 2 1 1 3
100 100 100
BARD1 2 1 1
80 80 80 RAD54L 4 2 2
PALB2 4 2 2
Non-BRCA HRR
60 60 60 ATM
Percentage
Percentage
Percentage
4 2 1 1
FANCI 5 2 3
Penetrance
40 40 40 BRIP1 6 5 1 High
FANCA 8 3 1 4 Moderate
Low/uncertain
20 20 20 RAD51C 10 7 2 1
RAD51D 15 14 1
0 0 0 BRCA2 42 36 2 4
BRCA1/2
rs
rs
rs
BRCA1
Ot R
Ot R
CA 2
R
Ot R
CA 2
R
CA 2
R
118 110 4 4
BR 1/
M
HR
M
BR 1/
BR 1/
HR
HR
he
he
he
M
M
n- CA
n- CA
n- CA
No BR
No BR
No BR
Total OV EC CC Association with
cancer
Therapeutic actionable genes are shown in boldface in panel B. The penetrance of genes heterozygosity; MMR, mismatch repair; OV, ovarian cancer; SDH, succinate
was adopted from Srinivasan et al.18 CC indicates cervical cancer; DDR, DNA damage dehydrogenase.
response; EC, endometrial cancer; HRR, homologous recombination repair; LOH, loss of
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 4/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
JAMA Network Open | Oncology Germline Variants in Gynecologic Cancers Among Patients in China
represented 47.6% of germline findings in endometrial cancer (n = 20) (Figure 1B; eTable 3 in
Supplement 1).
We identified 23 germline P/LP variants spanning 14 genes from 23 patients with cervical cancer
(eTables 2 and 4 in Supplement 1). The HRR variants comprised 86.9% of all germline findings
(n = 20) in cervical cancer. BRCA1, BRCA2, and FANCA were the top 3 commonly altered genes, the
P/LP variants of which were detected in 4 patients (17.4%) each (Figure 1B; eTable 3 in Supplement 1).
The prevalence of P/LP variants was 8.5% (18 of 212) in squamous cervical cancer and 4.4% (3 of 68)
in adenocarcinoma cervical cancer. The difference was not significant.
Next, we investigated the distribution of 2-hit events (also referred to as biallelic inactivation)
in carriers of different P/LP variants (Figure 1C). In ovarian cancer, 69.6% (78 of 112) of BRCA1/2
germline-variant tumors had 2-hit events, 94.9% (74 of 78) of which were via loss of heterozygosity
(LOH). Similarly, 48.5% (16 of 33) of the ovarian cancers harboring non-BRCA HRR P/LP variants had
2-hit events solely via LOH. In contrast, 60.0% (3 of 5) of MMR germline-variant ovarian cancers
presented with 2-hit events only by acquiring second somatic variants. The 2-hit rates in both HRR
and MMR P/LP variants were significantly higher than that in the background of benign germline
variants (HRR: 64.8% vs 20.3% [P < .001]; MMR: 60.0% vs 17.2% [P < .001]) (eFigure 2 in
Supplement 1). In endometrial cancer, 2-hit events were seen in 83.3% (10 of 12) of MMR germline-
variant tumors mainly through a second somatic variant (90.0% [9 of 10]) and only in 16.7% (2 of 12)
of the tumors carrying non-BRCA HRR P/LP variants via either mechanism (Figure 1C). Notably, none
of the 5 germline carriers of BRCA1/2 P/LP variants had 2-hit events, suggesting that these variants
might be incidental findings. The enrichment of 2-hit events in P/LP variants was only significant for
MMR (83.3% [10 of 12] vs 13.1% [11 of 84]; P < .001) but not for HRR genes (11.8% [2 of 17] vs 17.7%
[47 of 265], P > .99) (eFigure 2 in Supplement 1). In cervical cancer, we also identified LOH in 28.6%
(2 of 7) of BRCA1/2 and 11.1% (1 of 9) of non-BRCA HRR germline-variant tumors. The 2-hit rate for
BRCA P/LP variants was numerically higher than the background (28.6% [2 of 7] vs 14.5% [43 of 297];
P = .33) (eFigure 2 in Supplement 1). The difference was not significant, which may be due to the
small sample size. The 1 patient with cervical cancer harboring an MMR (MSH2) LP variant acquired a
second somatic variant, conferring a 100% 2-hit rate compared with that of 9.9% in the background
(P = .02).
Comparison of the Rate of Germline P/LP Variants Between Different Populations
We further compared the prevalence of germline P/LP variants between this study’s cohort and the
White population from The Cancer Genome Atlas (TCGA) research network.22 The overall rate of P/LP
variants, based on the 53 overlapping genes between panels, was similar in ovarian cancer between
cohorts, but the BRCA2 P/LP variants were less frequent (36 of 945 [3.8%] vs 27 of 348 [7.8%];
P = .005) in our cohort than in TCGA (eFigure 3 in Supplement 1). Our endometrial cancer cohort had
a significantly higher overall rate (42 of 307 [13.7%] vs 24 of 367 [6.5%]; P = .003) and more
common P/LP variants in non-BRCA HRR genes (14 of 307 [4.6%] vs 6 of 367 [1.6%]; P = .04) than
the TCGA data set. Patients with cervical cancer had comparable germline prevalence across genes
between cohorts.
Association Between Age and Status of Germline P/LP Variants
Patients with endometrial cancer and cervical cancer who were younger had a higher prevalence of
P/LP variants. Specifically, the prevalence was 25.0% (9 of 36) in patients with early-onset (defined
as age at diagnosis <45 years) endometrial cancer vs 12.7% (30 of 237) in those diagnosed at 45 years
or older (P = .09). In cervical cancer, the prevalence was 12.0% (10 of 83) in patients with early onset
and 4.8% (13 of 270) in those diagnosed at 45 years or older (P = .04) (Figure 2A). In contrast, the
prevalence of P/LP variants was independent of age in ovarian cancer.
We stratified the cohort according to the status of P/LP variants in different gene sets.
Compared with noncarriers, carriers of MMR P/LP variants were younger at onset of ovarian cancer
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 5/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
JAMA Network Open | Oncology Germline Variants in Gynecologic Cancers Among Patients in China
(46 vs 54 years; P = .02) and endometrial cancer (48 vs 57 years; P < .001), while those with HRR
P/LP variants were younger at onset of cervical cancer (46 vs 52 years; P = .04) (Figure 2B).
We further stratified the cohort according to the biallelic status of the P/LP variants. No
significant difference was observed in age at onset among patients with different statuses for HRR
variants in ovarian, endometrial, or cervical cancer (Figure 2C). Harboring MMR P/LP variants with
2-hit events was significantly associated with early onset in endometrial cancer, and a similar but
nonsignificant result was seen in ovarian cancer (Figure 2D). The only patient with cervical cancer
who harbored an MMR LP variant had a 2-hit event and was diagnosed at age 42 years. Of note, this
analysis is limited by the small sample size, especially those with 2-hit events.
Distinct Somatic Variant Profiles and Signatures in Carriers of Germline P/LP Variants
We also compared the somatic landscape and signatures of women who were carriers vs noncarriers
of germline P/LP variants. Tumors that developed in carriers of HRR P/LP variants harbored more
Figure 2. Association Between Age at Diagnosis and Germline Variant Status Across Gynecologic Cancer Types
A Distribution of germline carriers according to age at onset in years B Comparison of age between carriers of germline P/LP variants in different genes vs noncarriers
25 .64
.57 >.99
.28
.02 .001
100
.04
.99 .58
20
Germline variation rate, %
80
15
60
Age, y
10
40
5
20
0 0
<45 ≥45 <45 ≥45 <45 ≥45
–
–
rs
rs
R
rs
R
R
rm
rm
rm
HR
HR
HR
M
he
he
he
M
Ge
Ge
Ge
M
M
Ot
Ot
Ot
OV EC CC
OV EC CC
C Comparison of age among germline noncarriers for HRR variants D Comparison of age among germline noncarriers for MMR variants
.12 .28 .80
.37 >.99
.24 .26 .002
.45 .06
100 100
.21 .51 .29
.79 .29
80 80
60 60
Age, y
Age, y
40 40
20 20
0 0
–
–
+
+
t
it
it
rm
rm
rm
rm
rm
rm
Hi
Hi
Hi
Hi
rm
rm
rm
rm
rm
H
H
2-
2-
2-
2-
2-
2-
Ge
Ge
Ge
Ge
Ge
Ge
Ge
Ge
Ge
Ge
Ge
OV EC CC OV EC CC
In panel B, vertical white lines represent 95% CIs, individual dots are abnormal values, value for those entries. CC indicates cervical cancer; EC, endometrial cancer; germ–,
and the width of the shape represents the frequency of the value. In panels C and D, the germline noncarriers; germ+, germline carriers without 2-hit events; HHR, homologous
upper and lower bounds of the boxes are the upper and lower quartiles, whiskers recombination repair; MMR, mismatch repair; OV, ovarian cancer; P/LP, pathogenic/likely
represent 95% CIs, the center lines are the medians, and individual dots are abnormal pathogenic.
values beyond the 95% CIs. In panel D, the single horizontal lines represent only a single
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 6/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
JAMA Network Open | Oncology Germline Variants in Gynecologic Cancers Among Patients in China
prevalent somatic TP53 variants, regardless of cancer type, and generally had fewer variants in driver
genes (eg, PTEN, KRAS, and ERBB2 in ovarian cancer and ARID1A in both ovarian and endometrial
cancer). The MMR germline carriers with endometrial cancer had more somatic MMR variants, while
those with ovarian cancer harbored more common variants in driver genes, including KRAS, ARID1A,
and PTEN (Figure 3A).
Germline P/LP variants in MMR genes (MLH1, MSH2, MSH6, and PMS2) were detected in 28.6%
(4 of 14), 20.9% (9 of 43), and 14.3% (1 of 7) of high microsatellite instability (MSI-H) ovarian,
endometrial, and cervical cancer, respectively (Figure 3B). Further analyses showed that 100% (3 of
3) of the biallelic inactivated ovarian cancers that developed in carriers of MMR P/LP variants had an
MSI-H phenotype, while the proportion was 80.0% (8 of 10) in endometrial cancer. On the other
hand, 1 of the 3 (33.3%) ovarian cancers and 1 of the 4 (25.0%) endometrial cancers that developed
in carriers of MMR P/LP variants but retained the somatic heterozygosity of the germline-variant
Figure 3. Association of Germline Pathogenic/Likely Pathogenic (P/LP) Variants With Somatic Profiles and Signatures
A Comparison of somatic variation rates between noncarriers and carriers of germline P/LP variants in different gene sets
Proportion
OV EC CC 0.25
TP53 TP53 TP53 0.50
RB1 RNF43 TERT 0.75
PTEN PTEN STK11 1.00
PIK3CA PIK3R1 RICTOR
P value
NF1 PIK3CA RB1 P < .05
MYC NF1 PTEN
Somatic variation
Somatic variation
Somatic variation
KRAS MSH6 PIK3CA
FGFR3 MSH2 MYC
ERBB2 KRAS KRAS
CDK12 FGFR2 FBXW7
CCNE1 FBXW7 ERBB2
CCND2 ERBB2 BAP1
BRCA1 CTNNB1 ATRX
BRAF ATM ARID1A
ARID1A ARID1A AKT1
Germ– HRR MMR Others Germ– HRR MMR Others Germ– HRR MMR Others
B Distribution of germline P/LP variants in MSI-H vs MSS tumors C Biallelic status of MMR germline P/LP variants and MSI phenotype
MMR status MMR germ+ Non-MMR germ+ Germ–
OV EC
100
N=2
N=3
80 2-hit
P < .001 P < .001
2-hit MSI-H
MSI-H
P < .001
Percentage
60 N=8
40 N=2
Germ+
N=3 MSS
MSS
20 N=1 Germ+
N=1
Biallelic status MSI status Biallelic status MSI status
0
MSI-H MSS MSI-H MSS MSI-H MSS
OV EC CC
MSI status
CC indicates cervical cancer; EC, endometrial cancer; germ–, germline noncarriers; germ+, germline carriers without 2-hit events; HRR, homologous recombination repair; MMR,
mismatch repair; MSI, microsatellite instable; MSI-H, high microsatellite instability; MSS, microsatellite stable; OV, ovarian cancer.
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 7/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
JAMA Network Open | Oncology Germline Variants in Gynecologic Cancers Among Patients in China
allele exhibited an MSI-H status (Figure 3C). Only 1 patient with cervical cancer harbored an MMR LP
variant, and her tumor showed biallelic inactivation and an MSI-H status. The median tissue tumor
mutational burden was generally higher in carriers of MMR P/LP variants but comparable in carriers of
other germline variants compared with noncarriers across gynecologic cancer types (eFigure 4 in
Supplement 1).
Association of Germline P/LP Variants and Cancer Risk
We further investigated whether our germline findings were associated with an increased cancer risk
using an East Asian population without cancer from gnomAD as the reference. In addition to well-
known cancer-gene associations, we also identified that P/LP variants in BRCA1 (OR, 5.47; 95% CI,
1.42-17.17; P = .008) and FANCI (OR, 5.53; 95% CI, 1.03-19.47; P = .02) were associated with
endometrial cancer. The P/LP variants in BRCA1 (OR, 4.92; 95% CI, 1.22-14.68; P = .01) and BRCA2
(OR, 4.46; 95% CI, 1.11-13.14; P = .02) were associated with cervical cancer (Table 2).
Discussion
In this cross-sectional study, we evaluated the prevalence and landscape of germline P/LP variants in
unselected Chinese women with gynecologic cancers. Our results revealed a prevalence of 12.5%
(202 of 1610) for germline carriers of variants in genes consistent with known tumor phenotypes and
a prevalence of 3.7% (60 of 1610) for those with variants that are not known to be associated with
the cancer. Cervical cancer has been thought to be a sporadic disease associated with genital
infection of human papillomavirus and has little to do with rare inheritable variants. Our study
identified a spectrum of deleterious germline variants, with a prevalence of 6.4% in cervical cancer.
Most of these germline findings were in HRR genes, especially BRCA1/2. Interestingly, we found an
association of HRR P/LP variants with earlier onset of cervical cancer, which often indicates an
underlying inherited predisposition to cancer. Somatic biallelic inactivation observed in some of
these HRR variants and the moderate cervical cancer risk of BRCA1/2 P/LP variants further support
that at least some of these germline findings may be driving events in cervical cancer. Nevertheless,
the lower rate of biallelic inactivation (18.7%) compared with ovarian cancer (65.0%) also suggests
that most of these P/LP variants may be incidental findings. Besides, a deleterious MSH2 variant was
identified in 1 patient with cervical cancer with a 2-hit event and MSI-H status, suggesting a role of
this variant in the tumorigenesis of this case. Our results underscore the necessity of investigating
Table 2. Cancer Predisposition of Germline Mutated Genes
Gene Cancer altered, No. Cancer total, No. Control altered, No. Control total, No. Odds ratio (95% CI) P value
Ovarian cancer
BRCA1 110 945 21 9163 57.26 (35.47-96.28) <.001
BRCA2 36 945 23 9097 15.61 (8.96-27.74) <.001
MLH1 2 945 0 9012 ⬁ (1.79-⬁) .009
MSH2 4 945 3 9102 12.89 (2.18-88.04) .002
RAD51C 7 945 16 8796 4.09 (1.42-10.55) .005
RAD51D 14 945 19 8854 6.99 (3.23-14.75) <.001
Endometrial cancer
MSH2 9 307 3 9102 91.61 (22.66-526.57) <.001
MSH6 6 307 10 9152 18.20 (5.40-55.61) <.001
MLH1 2 307 0 9012 ⬁ (5.52-⬁) .001
BRCA1 4 307 21 9163 5.74 (1.42-17.17) .008
FANCI 3 307 16 8990 5.53 (1.03-19.47) .02
Cervical cancer
BRCA1 4 358 21 9163 4.92 (1.22-14.68) .01
BRCA2 4 358 23 9097 4.46 (1.11-13.14) .02
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 8/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
JAMA Network Open | Oncology Germline Variants in Gynecologic Cancers Among Patients in China
inheritable factors in cervical cancer, which has long been neglected. Such studies may help to define
a subgroup of patients with cervical cancer with distinctive molecular and clinicopathologic features
who may benefit the most from germline testing.
For endometrial cancer, our study found a prevalence of HRR P/LP variants of 6.2%, comprising
one-half of the germline findings in this disease. Notably, only a small proportion of these HRR
variants occurred in BRCA1/2, with a prevalence of 2.0%. Previous studies also identified pathogenic
BRCA1/2 germline variants in 0.5% to 1.4% of patients with endometrial cancer.23,24 Based on the
distinct clinicopathologic, molecular, and survival features of germline BRCA1/2 variant carriers,
another study suggested that endometrial cancer should be considered as one of the BRCA1/2-
associated hereditary breast and ovarian cancer syndromes.25 A recent study reported a 2 to 3-fold
increased risk for endometrial cancer in BRCA1/2 variant carriers.26 We also observed that P/LP
variants in BRCA1 and FANCI were associated with a moderate risk for endometrial cancer, though a
low rate of biallelic inactivation was observed. These results suggest potential involvement of
pathogenic HRR germline variants in endometrial cancer development, which merits further
investigation.
US Food and Drug Administration–approved targeted agents for managing gynecologic cancer
remain limited.27,28 We found potential druggable germline variants in 15.3% of our cohort,
comprising 95.1% of all germline findings. The majority of these variants were in HRR and MMR
genes, suggesting therapeutic opportunities for poly(ADP-ribose) polymerase inhibitors and
pembrolizumab. Moreover, prophylactic removal of both ovaries and fallopian tubes
(salpingo-oophorectomy) and/or the uterus (hysterectomy) in BRCA1/2 carriers is recognized as the
most effective method for decreasing ovarian and endometrial cancer risk.29 Despite the substantial
clinical relevance of germline findings in gynecologic cancer for therapeutic decision-making, genetic
counseling, and intervention, current clinical guidelines only recommend germline testing for
selected patients based on pathologic features of the tumor, onset age, and family history of cancer.
The American Society of Clinical Oncology has recently recommended offering germline testing for
women with epithelial ovarian cancer regardless of clinical features or family history.30 Germline
testing of MMR genes is only recommended for patients with endometrial cancer whose tumors are
MMR deficient or MSI-H, who have a family history of Lynch syndrome–related cancer, or who
possess significant clinical characteristics for Lynch syndrome.31 Patients with cervical cancer are not
referred for germline testing in the clinic. Notably, a large proportion of the clinically actionable
germline findings stemming from our unselected cohort would have been missed if guideline-based
genetic testing were offered. Despite the uncertain pathogenicity of some of these variants,
identifying these germline findings could also benefit patients by providing implications for risk-
reducing interventions and cancer surveillance and prevention measures in at-risk families.32
Emerging evidence suggests that germline variants, in addition to increasing cancer risk, also
influence tumor progression by shaping the landscape of somatic alterations in cancer.17,18 Our study
reveals some distinctive genomic features in cancers developing in carriers of pathogenic germline
variants. Tumors in carriers of pathogenic HRR variants harbored more TP53 variants than
noncarriers, consistent with the finding that the loss of TP53 function is associated with higher
homologous recombination deficiency status.33 We also found that carriers of pathogenic HRR
variants harbored fewer somatic variants in oncogenic driver genes than noncarriers. Consistently,
Srinivasan et al18 recently showed the acquisition of fewer somatic oncogenic drivers as one of the
hallmarks for tumors in carriers of germline variants in high-penetrance genes. Pathogenic germline
variants can also increase the likelihood of somatic biallelic inactivation in the same gene or somatic
alterations in the same pathway.18,34 Concordantly, we found that endometrial cancer developing in
carriers of pathogenic MMR variants had higher somatic variant rates in the MMR genes. In contrast,
MMR germline carriers with ovarian cancer showed higher somatic variant rates in oncogenic driver
genes, suggesting a heterogeneous etiology of tumorigenesis mediated by MMR germline variants
in endometrial cancer. Alternatively, these oncogenic variants may be just passenger events, given
the higher mutation burden in these tumors.
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 9/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
JAMA Network Open | Oncology Germline Variants in Gynecologic Cancers Among Patients in China
Limitations
This study had several limitations. The clinical significance of P/LP germline variants identified in our
cohort lacks further validation, especially those without biallelic inactivation. Moreover, the targeted
panel used in the study did not allow for the accurate determination of LOH status via a segment-
based approach. Alternatively, we roughly estimated LOH status based on the mutation allele
frequency (ⱖ60%), assuming the tumor cell proportion to be 20% or greater (eMethods in
Supplement 1). We had assessed this surrogate’s accuracy by using samples with a known LOH status
determined by the standard segment-based approach. The cutoff of 60% resulted in a sensitivity of
65% and a specificity of 95%. Therefore, the LOH events may have been largely underestimated in
our study. Moreover, the sample size for cervical cancer was small, which attenuates the strength of
our findings on the associations of germline variants with age at onset and cancer risk.
Conclusions
This study delineates the landscape of germline P/LP variants in cancer predisposition genes and
reveals distinct somatic profiles in carriers of germline variants among unselected Chinese women
with gynecologic cancers. The findings raise the importance of universal NGS-based genetic testing
with a large gene panel as part of gynecologic cancer screening and diagnosis. Genetic testing could
improve risk assessment, bring more opportunities for cancer prevention and early detection, and
guide therapeutic decision-making.
ARTICLE INFORMATION
Accepted for Publication: June 12, 2023.
Published: July 31, 2023. doi:10.1001/jamanetworkopen.2023.26437
Open Access: This is an open access article distributed under the terms of the CC-BY License. © 2023 Wen H et al.
JAMA Network Open.
Corresponding Authors: Xiaohua Wu, PhD, Department of Gynecologic Oncology, Fudan University Shanghai
Cancer Center, 270 Dong-An Rd, Xuhui District, Shanghai 200032, China (wu.xh@fudan.edu.cn); Xipeng Wang,
PhD, MD, Department of Obstetrics and Gynecology, Xinhua Hospital Affiliated to Shanghai Jiao Tong University
School of Medicine, 1665 Kongjiang Rd, Yangpu District, Shanghai 200092, China (wangxipeng@
xinhuamed.com.cn).
Author Affiliations: Department of Gynecologic Oncology, Fudan University Shanghai Cancer Center, Shanghai,
China (Wen, Wu); Department of Oncology, Shanghai Medical College, Fudan University, Shanghai, China (Wen,
Wu); Clinical Oncology School of Fujian Medical University, Fujian Cancer Hospital, Fuzhou, China (Xu); Department
of Gynecology, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, China (Sheng);
Department of Gynecology, Zhuhai People’s Hospital (Zhuhai Hospital Affiliated with Jinan University), Zhuhai,
China (Li); Department of Obstetrics and Gynecology, Xinhua Hospital Affiliated to Shanghai JiaoTong University
School of Medicine, Shanghai, China (Wang).
Author Contributions: Dr Wen had full access to all of the data in the study and takes responsibility for the
integrity of the data and the accuracy of the data analysis. Drs Wen, Xu, and Sheng contributed equally to
this work.
Concept and design: Wen, Wang, Wu.
Acquisition, analysis, or interpretation of data: Wen, Xu, Sheng, Li.
Drafting of the manuscript: Wen, Xu.
Critical review of the manuscript for important intellectual content: Sheng, Li, Wang, Wu.
Statistical analysis: Wen, Xu.
Administrative, technical, or material support: Sheng, Li.
Supervision: Wang, Wu.
Conflict of Interest Disclosures: None reported.
Data Sharing Statement: See Supplement 2.
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 10/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
JAMA Network Open | Oncology Germline Variants in Gynecologic Cancers Among Patients in China
Additional Contributions: The authors thank Fei Zhao, PhD, Lin Shao, PhD, and Jing Wang, MD, from Burning Rock
Biotech for their help in data analysis and manuscript editing. These individuals were not compensated for their
contributions.
REFERENCES
1. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115-132. doi:10.
3322/caac.21338
2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7-34. doi:10.3322/caac.21551
3. Jiang X, Tang H, Chen T. Epidemiology of gynecologic cancers in China. J Gynecol Oncol. 2018;29(1):e7. doi:10.
3802/jgo.2018.29.e7
4. Hicks-Courant K, Melamed A, Worley MJ Jr, Kim YB, Schorge JO, Rauh-Hain JA. Trends in place of death among
patients with gynecologic cancer in the United States. Obstet Gynecol. 2018;131(6):1111-1120. doi:10.1097/AOG.
0000000000002614
5. Torre LA, Islami F, Siegel RL, Ward EM, Jemal A. Global cancer in women: burden and trends. Cancer Epidemiol
Biomarkers Prev. 2017;26(4):444-457. doi:10.1158/1055-9965.EPI-16-0858
6. Zheng R, Zhang S, Zeng H, et al. Cancer incidence and mortality in China, 2016. J Natl Cancer Cent. 2022;22
(1):1-9. doi:10.1016/j.jncc.2022.02.002
7. Ford D, Easton DF, Stratton M, et al; the Breast Cancer Linkage Consortium. Genetic heterogeneity and
penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. Am J Hum Genet. 1998;62(3):
676-689. doi:10.1086/301749
8. Lynch HT, Casey MJ, Snyder CL, et al. Hereditary ovarian carcinoma: heterogeneity, molecular genetics,
pathology, and management. Mol Oncol. 2009;3(2):97-137. doi:10.1016/j.molonc.2009.02.004
9. Holman LL, Lu KH. Genetic risk and gynecologic cancers. Hematol Oncol Clin North Am. 2012;26(1):13-29. doi:
10.1016/j.hoc.2011.11.003
10. Morice P, Leary A, Creutzberg C, Abu-Rustum N, Darai E. Endometrial cancer. Lancet. 2016;387(10023):
1094-1108. doi:10.1016/S0140-6736(15)00130-0
11. Luna C, Balcacer P, Castillo P, Huang M, Alessandrino F. Endometrial cancer from early to advanced-stage
disease: an update for radiologists. Abdom Radiol (NY). 2021;46(11):5325-5336. doi:10.1007/s00261-021-03220-7
12. Kast K, Rhiem K, Wappenschmidt B, et al; German Consortium for Hereditary Breast and Ovarian Cancer
(GC-HBOC). Prevalence of BRCA1/2 germline mutations in 21 401 families with breast and ovarian cancer. J Med
Genet. 2016;53(7):465-471. doi:10.1136/jmedgenet-2015-103672
13. Kuchenbaecker KB, Hopper JL, Barnes DR, et al; BRCA1 and BRCA2 Cohort Consortium. Risks of breast,
ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA. 2017;317(23):2402-2416.
doi:10.1001/jama.2017.7112
14. Eccles DM, Balmaña J, Clune J, et al. Selecting patients with ovarian cancer for germline BRCA mutation
testing: findings from guidelines and a systematic literature review. Adv Ther. 2016;33(2):129-150. doi:10.1007/
s12325-016-0281-1
15. Ring KL, Bruegl AS, Allen BA, et al. Germline multi-gene hereditary cancer panel testing in an unselected
endometrial cancer cohort. Mod Pathol. 2016;29(11):1381-1389. doi:10.1038/modpathol.2016.135
16. Mosele F, Remon J, Mateo J, et al. Recommendations for the use of next-generation sequencing (NGS) for
patients with metastatic cancers: a report from the ESMO Precision Medicine Working Group. Ann Oncol. 2020;31
(11):1491-1505. doi:10.1016/j.annonc.2020.07.014
17. Chanock SJ. How the germline informs the somatic landscape. Nat Genet. 2021;53(11):1523-1525. doi:10.1038/
s41588-021-00960-6
18. Srinivasan P, Bandlamudi C, Jonsson P, et al. The context-specific role of germline pathogenicity in
tumorigenesis. Nat Genet. 2021;53(11):1577-1585. doi:10.1038/s41588-021-00949-1
19. Chatrath A, Ratan A, Dutta A. Germline variants that affect tumor progression. Trends Genet. 2021;37(5):
433-443. doi:10.1016/j.tig.2020.10.005
20. Lek M, Karczewski KJ, Minikel EV, et al; Exome Aggregation Consortium. Analysis of protein-coding genetic
variation in 60,706 humans. Nature. 2016;536(7616):285-291. doi:10.1038/nature19057
21. gnomAD. Broad Institute. Accessed April 1, 2023. https://gnomad.broadinstitute.org/
22. Huang KL, Mashl RJ, Wu Y, et al; Cancer Genome Atlas Research Network. Pathogenic germline variants in
10,389 adult cancers. Cell. 2018;173(2):355-370.e14. doi:10.1016/j.cell.2018.03.039
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 11/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
JAMA Network Open | Oncology Germline Variants in Gynecologic Cancers Among Patients in China
23. Spurdle AB, Bowman MA, Shamsani J, Kirk J. Endometrial cancer gene panels: clinical diagnostic vs research
germline DNA testing. Mod Pathol. 2017;30(8):1048-1068. doi:10.1038/modpathol.2017.20
24. Smith ES, Da Cruz Paula A, Cadoo KA, et al. Endometrial cancers in BRCA1 or BRCA2 germline mutation
carriers: assessment of homologous recombination DNA repair defects. JCO Precis Oncol. Published online August
29, 2019. doi:10.1200/PO.19.00103
25. de Jonge MM, Ritterhouse LL, de Kroon CD, et al; HEBON Group. Germline BRCA-associated endometrial
carcinoma is a distinct clinicopathologic entity. Clin Cancer Res. 2019;25(24):7517-7526. doi:10.1158/1078-0432.
CCR-19-0848
26. de Jonge MM, de Kroon CD, Jenner DJ, et al; Hebon Group. Endometrial cancer risk in women with germline
BRCA1 or BRCA2 mutations: multicenter cohort study. J Natl Cancer Inst. 2021;113(9):1203-1211. doi:10.1093/
jnci/djab036
27. Wang Q, Peng H, Qi X, Wu M, Zhao X. Targeted therapies in gynecological cancers: a comprehensive review of
clinical evidence. Signal Transduct Target Ther. 2020;5(1):137. doi:10.1038/s41392-020-0199-6
28. Lightfoot M, Montemorano L, Bixel K. PARP inhibitors in gynecologic cancers: what is the next big
development? Curr Oncol Rep. 2020;22(3):29. doi:10.1007/s11912-020-0873-4
29. Finch A, Beiner M, Lubinski J, et al; Hereditary Ovarian Cancer Clinical Study Group. Salpingo-oophorectomy
and the risk of ovarian, fallopian tube, and peritoneal cancers in women with a BRCA1 or BRCA2 mutation. JAMA.
2006;296(2):185-192. doi:10.1001/jama.296.2.185
30. Konstantinopoulos PA, Norquist B, Lacchetti C, et al. Germline and somatic tumor testing in epithelial ovarian
cancer: ASCO guideline. J Clin Oncol. 2020;38(11):1222-1245. doi:10.1200/JCO.19.02960
31. Koh WJ, Abu-Rustum NR, Bean S, et al. Uterine neoplasms, version 1.2018, NCCN Clinical Practice Guidelines in
Oncology. J Natl Compr Canc Netw. 2018;16(2):170-199. doi:10.6004/jnccn.2018.0006
32. Subbiah V, Kurzrock R. Universal germline and tumor genomic testing needed to win the war against cancer:
genomics is the diagnosis. J Clin Oncol. 2023;41(17):3100-3103. doi:10.1200/JCO.22.02833
33. Knijnenburg TA, Wang L, Zimmermann MT, et al; Cancer Genome Atlas Research Network. Genomic and
molecular landscape of DNA damage repair deficiency across The Cancer Genome Atlas. Cell Rep. 2018;23(1):239-
254.e6. doi:10.1016/j.celrep.2018.03.076
34. Kanchi KL, Johnson KJ, Lu C, et al. Integrated analysis of germline and somatic variants in ovarian cancer. Nat
Commun. 2014;5:3156. doi:10.1038/ncomms4156
SUPPLEMENT 1.
eMethods.
eReferences.
eFigure 1. Flow Diagram Illustrating the Cohort and Study Design
eFigure 2. Comparison of 2-Hit Events for P/LP Variants vs Benign Variants
eFigure 3. Comparison of the Germline P/LP Variant Rates Between Different Populations
eFigure 4. Comparison of TMB Between Noncarriers (Germ–) and Carriers of Germline P/LP Variants in Different
Gene Sets
eTable 1. List of 62 Cancer-Predisposition Genes Included in the OncoScreen Plus Panel
eTable 2. Detailed Information of Germline Pathogenic/Likely Pathogenic Variants Detected in the Cohort
eTable 3. Distribution of Germline Pathogenic/Likely Pathogenic Variants Detected in the Cohort According to
Genes and the Related Signaling Pathways
eTable 4. Distribution of Germline Pathogenic/Likely Pathogenic Variants Detected from the Cohort According to
Variant Type
SUPPLEMENT 2.
Data Sharing Statement
JAMA Network Open. 2023;6(7):e2326437. doi:10.1001/jamanetworkopen.2023.26437 (Reprinted) July 31, 2023 12/12
Downloaded From: https://jamanetwork.com/ on 08/29/2023
You might also like
- Elective 8 New Market Development ModuleDocument91 pagesElective 8 New Market Development Modulejulius80% (10)
- ABO AnalysisDocument38 pagesABO AnalysisMa Lyn Gabayeron75% (4)
- Roots & DerivsDocument17 pagesRoots & DerivsAbir Chowdhury100% (2)
- Prevalence of Tumor Genomic Alterations in Homologous Recombination Repair Genes Among Taiwanese Breast CancersDocument13 pagesPrevalence of Tumor Genomic Alterations in Homologous Recombination Repair Genes Among Taiwanese Breast Cancers郭竹瑩No ratings yet
- Godone 2018Document21 pagesGodone 2018Roberta GodoneNo ratings yet
- Rakha Et Al. 2006 Prognostic Markers in Triple Negative Breast CancerDocument8 pagesRakha Et Al. 2006 Prognostic Markers in Triple Negative Breast CancerdanishNo ratings yet
- Jamaoncology Mavaddat 2022 Oi 210095 1647458350.98716Document11 pagesJamaoncology Mavaddat 2022 Oi 210095 1647458350.98716Daira Gabriela Ormachea ArancibiaNo ratings yet
- 6880-Article Text-54409-3-10-20231020Document12 pages6880-Article Text-54409-3-10-20231020Selma Mutiara HaniNo ratings yet
- Breast Cancer in Indian Women Genetic Risk Factor and Predictive BiomarkerDocument14 pagesBreast Cancer in Indian Women Genetic Risk Factor and Predictive Biomarkermicrogmcapur2016No ratings yet
- Nejmoa 2105215Document12 pagesNejmoa 2105215cejigip953No ratings yet
- Impact of Breast Cancer Subtypes On Prognosis of Women With Operable Invasive Breast Cancer: A Population-Based Study Using SEER DatabaseDocument10 pagesImpact of Breast Cancer Subtypes On Prognosis of Women With Operable Invasive Breast Cancer: A Population-Based Study Using SEER DatabasesilviatengkerNo ratings yet
- 410-Article Text-1440-1-10-20211018Document7 pages410-Article Text-1440-1-10-20211018silviatengkerNo ratings yet
- Fertility Treatments and Invasive Epithelial Ovarian Cancer 2015 Fertility ADocument8 pagesFertility Treatments and Invasive Epithelial Ovarian Cancer 2015 Fertility Ajayeto4038No ratings yet
- Genetica 1Document9 pagesGenetica 1Jose Andres DiazNo ratings yet
- Kumar 2015Document5 pagesKumar 2015Isuploaded BlogspotcomNo ratings yet
- Centrosome-Related Genes, Genetic Variation, and Risk of Breast CancerDocument9 pagesCentrosome-Related Genes, Genetic Variation, and Risk of Breast CancerSari RiastiningsihNo ratings yet
- 10 1053@j Seminoncol 2016 10 001Document8 pages10 1053@j Seminoncol 2016 10 001rikudoutobiNo ratings yet
- Germline Breast Cancer SuspectibiliyDocument13 pagesGermline Breast Cancer SuspectibiliyDominick Dayton FinettiNo ratings yet
- 1 s2.0 S0893395222028435 MainDocument8 pages1 s2.0 S0893395222028435 MainSmit ShahNo ratings yet
- CA de MamaDocument106 pagesCA de MamaDamián López RangelNo ratings yet
- Naderi Et Al-2019-Molecular Genetics & Genomic Medicine PDFDocument7 pagesNaderi Et Al-2019-Molecular Genetics & Genomic Medicine PDFgeorgiaNo ratings yet
- Gulbahce 2016Document5 pagesGulbahce 2016Valir HusleNo ratings yet
- Advances in Screening, Diagnosis, and Treatment ofDocument7 pagesAdvances in Screening, Diagnosis, and Treatment ofBastomy EkaNo ratings yet
- The Genetics and Clinical Outcomes in 151 Cases OfDocument7 pagesThe Genetics and Clinical Outcomes in 151 Cases Ofzeni okta wiyantiNo ratings yet
- Complex Fibroadenoma and Breast Cancer RiskDocument15 pagesComplex Fibroadenoma and Breast Cancer RisktatianaNo ratings yet
- MTHFR/p53 Polymorphisms As Genetic Factors For Cervical Intraepithelial Neoplasia and Cervical Cancer in HPV-infected Mexican WomenDocument9 pagesMTHFR/p53 Polymorphisms As Genetic Factors For Cervical Intraepithelial Neoplasia and Cervical Cancer in HPV-infected Mexican WomenIrina Surco RodríguezNo ratings yet
- Journal Medicine: The New EnglandDocument11 pagesJournal Medicine: The New EnglandMohiuddin JishanNo ratings yet
- Ajol File Journals - 494 - Articles - 112408 - Submission - Proof - 112408 5833 311975 1 10 20150203Document5 pagesAjol File Journals - 494 - Articles - 112408 - Submission - Proof - 112408 5833 311975 1 10 20150203KeHuyDietNo ratings yet
- Prognostic Value of p53 Gene in Ovarian Cancer: - Maj Obstet 172 Rauf Dan Masadah Ginekol IndonesDocument5 pagesPrognostic Value of p53 Gene in Ovarian Cancer: - Maj Obstet 172 Rauf Dan Masadah Ginekol IndonesDini MedyaniNo ratings yet
- Germline Mutations in Predisposition Genes in Pediatric CancerDocument11 pagesGermline Mutations in Predisposition Genes in Pediatric CancerGuadalupeA.OsorioNo ratings yet
- Jurnal 1Document13 pagesJurnal 1Aqshal Ilham OktoriNo ratings yet
- Proof: Gynecologic OncologyDocument2 pagesProof: Gynecologic OncologyCamilaBurgosNo ratings yet
- Meijers Heijboer2001Document6 pagesMeijers Heijboer2001Market PlusNo ratings yet
- Advances in The Molecular Taxonomy of Breast CancerDocument7 pagesAdvances in The Molecular Taxonomy of Breast CancerbrendaNo ratings yet
- Fmolb 11 1394585Document18 pagesFmolb 11 1394585Rodrigo SierraNo ratings yet
- A Review of Triple-Negative Breast Cancer: Nick Patten. Last Light (Detail) - Oil On Canvas, 44" × 56"Document4 pagesA Review of Triple-Negative Breast Cancer: Nick Patten. Last Light (Detail) - Oil On Canvas, 44" × 56"Kritik KumarNo ratings yet
- Carcinoma: BRCA-Mutation-Associated Fallopian TubeDocument8 pagesCarcinoma: BRCA-Mutation-Associated Fallopian Tubew yNo ratings yet
- Expression of Mirnas and Pten in Endometrial Specimens Ranging From Histologically Normal To Hyperplasia and Endometrial AdenocarcinomaDocument9 pagesExpression of Mirnas and Pten in Endometrial Specimens Ranging From Histologically Normal To Hyperplasia and Endometrial AdenocarcinomaFerdina NidyasariNo ratings yet
- 2017 Article 52-2Document9 pages2017 Article 52-2Lorena RamosNo ratings yet
- Oncollogy 3Document9 pagesOncollogy 3AG LarikNo ratings yet
- Onkogenesis, Morfologi, Dan Modalitas Deteksi Dini Karsinoma ServiksDocument14 pagesOnkogenesis, Morfologi, Dan Modalitas Deteksi Dini Karsinoma ServiksJuschella SumakulNo ratings yet
- Cervical Cancer: Prevention, Diagnosis, and TherapeuticsDocument23 pagesCervical Cancer: Prevention, Diagnosis, and TherapeuticsranggadrNo ratings yet
- Diagnosing Hereditary Cancer Predisposition in MenDocument7 pagesDiagnosing Hereditary Cancer Predisposition in MenSaurabh SharmaNo ratings yet
- Safety and Efficacy of Pembrolizumab in Advanced, Programmed Death Ligand 1-Positive Cervical CancerDocument9 pagesSafety and Efficacy of Pembrolizumab in Advanced, Programmed Death Ligand 1-Positive Cervical CancerluizaNo ratings yet
- Atchley Et Al 2016 Clinical and Pathologic Characteristics of PatientsDocument7 pagesAtchley Et Al 2016 Clinical and Pathologic Characteristics of PatientsWojtek JanotaNo ratings yet
- NIH Public Access: Author ManuscriptDocument23 pagesNIH Public Access: Author ManuscriptGustavo IbarraNo ratings yet
- Cáncer OralDocument7 pagesCáncer OralValery MedinaNo ratings yet
- BRCA1 Gene Mutations in Breast Cancer Patients From Kerman Province, IranDocument6 pagesBRCA1 Gene Mutations in Breast Cancer Patients From Kerman Province, IranMohammed AladhraeiNo ratings yet
- Brjcancer00189 0144cDocument2 pagesBrjcancer00189 0144cZhangYixing EXOSNo ratings yet
- Matsuo 2018Document14 pagesMatsuo 2018Mahmudur Rahman27No ratings yet
- Molecular Diagnosis in Breast Cancer: Mini-Symposium: Breast PathologyDocument12 pagesMolecular Diagnosis in Breast Cancer: Mini-Symposium: Breast PathologyOber Van Gómez LópezNo ratings yet
- PJSS 66 3 Jul Sep 2011 3Document9 pagesPJSS 66 3 Jul Sep 2011 3Dwight AvelinoNo ratings yet
- MJZ 033Document10 pagesMJZ 033metrorespoNo ratings yet
- The Clinicopathological Features of Breast Carcinoma Cases in Adiwaniyah Province in IraqDocument11 pagesThe Clinicopathological Features of Breast Carcinoma Cases in Adiwaniyah Province in IraqCentral Asian StudiesNo ratings yet
- Editorial: Lung Cancer: Prevalent Trends & Emerging ConceptsDocument3 pagesEditorial: Lung Cancer: Prevalent Trends & Emerging Conceptsjeevan georgeNo ratings yet
- 1 s2.0 S003130251640365X MainDocument9 pages1 s2.0 S003130251640365X MainbrendaNo ratings yet
- Cytologic Patterns of Cervical Adenocarcinomas With Emphasis On Factors Associated With Underdiagnosis - Tumor DiathesisDocument9 pagesCytologic Patterns of Cervical Adenocarcinomas With Emphasis On Factors Associated With Underdiagnosis - Tumor Diathesisnakemi111No ratings yet
- La Mellarin D2Document2 pagesLa Mellarin D2JESUS DAVID BOLA‹O JIMENEZNo ratings yet
- 3 PDFDocument24 pages3 PDFdindaNo ratings yet
- Biomarkers in Breast Cancer 2024: An Updated Consensus Statement by The Spanish Society of Medical Oncology and The Spanish Society of PathologyDocument17 pagesBiomarkers in Breast Cancer 2024: An Updated Consensus Statement by The Spanish Society of Medical Oncology and The Spanish Society of PathologyellyanaperwitasariNo ratings yet
- "OMIC" Tumor Markers For Breast Cancer: A ReviewDocument7 pages"OMIC" Tumor Markers For Breast Cancer: A ReviewwardaninurindahNo ratings yet
- Link ClassificationDocument12 pagesLink ClassificationluisalbertomendozapuNo ratings yet
- 2023 40668 Moesm3 EsmDocument3 pages2023 40668 Moesm3 EsmJEAN GEMNo ratings yet
- Project Muse 882910Document23 pagesProject Muse 882910JEAN GEMNo ratings yet
- The Impact of Translation Memory SegmentationDocument18 pagesThe Impact of Translation Memory SegmentationJEAN GEMNo ratings yet
- Proposal For A Translanguaging Space' in Interpreting StudiesDocument21 pagesProposal For A Translanguaging Space' in Interpreting StudiesJEAN GEMNo ratings yet
- Reflexology New Patient FormDocument7 pagesReflexology New Patient FormOana Iftimie100% (2)
- Chauhan / Gupta Homeophatic Principles and Practice of MedicineDocument10 pagesChauhan / Gupta Homeophatic Principles and Practice of Medicinems.anitha1980No ratings yet
- What Are CarbohydratesDocument7 pagesWhat Are CarbohydratesconstantinNo ratings yet
- Celiac Disease PathophysiologyDocument28 pagesCeliac Disease PathophysiologyIsmy HoiriyahNo ratings yet
- Home Remedies Using Mustard Seeds Prophet666Document2 pagesHome Remedies Using Mustard Seeds Prophet666Hussainz AliNo ratings yet
- tmp4946 TMPDocument27 pagestmp4946 TMPFrontiersNo ratings yet
- Electrical SafetyDocument3 pagesElectrical SafetyPerwez21No ratings yet
- Monitoring & Devices Used in ICU CCUDocument48 pagesMonitoring & Devices Used in ICU CCUProf. Ramsharan Mehta100% (1)
- Vamana Karma-Understanding Mode of ActionDocument12 pagesVamana Karma-Understanding Mode of ActionsmsmastiNo ratings yet
- Generalization and Stereotype in Counseling - Implication and Caution in Clinical Setting.Document15 pagesGeneralization and Stereotype in Counseling - Implication and Caution in Clinical Setting.Nishesh AcharyaNo ratings yet
- Module 3 - SociologyDocument74 pagesModule 3 - SociologyakshayaNo ratings yet
- Contingency Plan FormatDocument2 pagesContingency Plan FormatNagarajanNo ratings yet
- Chapter 10Document17 pagesChapter 10Bryle Dela TorreNo ratings yet
- Dezinfeqcia SterilizaciaDocument29 pagesDezinfeqcia SterilizaciaLuka KhvichiaNo ratings yet
- Radiology Abdomen InterpretationsDocument108 pagesRadiology Abdomen InterpretationsStudent100% (1)
- Arteritis TemporalisDocument5 pagesArteritis TemporalisbagasNo ratings yet
- Paul Saville For Mayor of Bristol 2016Document5 pagesPaul Saville For Mayor of Bristol 2016Paul SavilleNo ratings yet
- 114 247 1 SMDocument6 pages114 247 1 SMAzhar FauzanNo ratings yet
- Rule 1040 - Health and Safety CommitteeDocument10 pagesRule 1040 - Health and Safety Committeerobinrubina50% (2)
- SteraminDocument1 pageSteraminnodi79No ratings yet
- BiographyDocument7 pagesBiographyapi-348852766No ratings yet
- A Series of MCQ Type Online Practice Test On MANAGEMENT (22509) (Unit - IV)Document27 pagesA Series of MCQ Type Online Practice Test On MANAGEMENT (22509) (Unit - IV)S V67% (3)
- Dental IndicesDocument54 pagesDental IndicesrajshreeNo ratings yet
- Mater Maternity Booking Form V2 - March17 (Not For Record)Document1 pageMater Maternity Booking Form V2 - March17 (Not For Record)Oliver JanevNo ratings yet
- Book ItemDocument28 pagesBook ItemAnwesha PadhanNo ratings yet
- Induction Program ScriptDocument2 pagesInduction Program ScriptAl-var A AtibingNo ratings yet
- Descriptive Questions Asked in Previous Years IBPS PO Mains ExamDocument5 pagesDescriptive Questions Asked in Previous Years IBPS PO Mains ExamAnwesha SahooNo ratings yet