Professional Documents
Culture Documents
EAU Guidelines On Sexual and Reproductive Health 2022 - 2022 03 29 084141 - Megw (110 111)
EAU Guidelines On Sexual and Reproductive Health 2022 - 2022 03 29 084141 - Megw (110 111)
Uploaded by
CRISTH KIMBERLY ENEQUE DE LA CRUZOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
EAU Guidelines On Sexual and Reproductive Health 2022 - 2022 03 29 084141 - Megw (110 111)
EAU Guidelines On Sexual and Reproductive Health 2022 - 2022 03 29 084141 - Megw (110 111)
Uploaded by
CRISTH KIMBERLY ENEQUE DE LA CRUZCopyright:
Available Formats
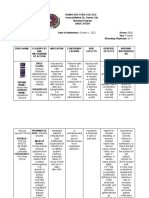
Figure 11: Treatment algorithm for Peyronie’s disease
Treatment of Peyronie’s disease
Discuss natural history of the disease
Reassure patient that Peyronie’s doesn’t lead to
any form of malignancy
Discuss current treatment modalities
Shared decision-making
Active disease Stable disease
(pain, deformity deterioration, (no pain, no deformity
progressive curvature) deterioration, stable penile
curvature)
Pain control (consider NSAIDs,
tadalafil or LI-ESWT) Patient desires active
Optional: Traction therapy, treatment
intralesional CCH or IFN-α2b
No ED ED
Response
Yes to ED
treatment
Palpable dorsal plaques Adequate penile Short penis
Non-calcified plaques length Severe curvature
Dorsal Curvature 30°-90° Absence of severe Complex deformities
No
Contraindications for curvature (hourglass, hinge)
surgery/patient does not Absence of complex
want surgery deformities
Intralesional Tunical shortening Tunical lengthening Penile
injection treatment: procedures procedures prosthesis
CCH or interferon
Residual
> 30°
curvature
Manual
modeling
Residual
> 30° < 30°
curvature
Tunical plication/ No additional
Plaque incision + straightening
grafting procedures
ED = erectile dysfunction; LI-ESWT = Low-intensity extracorporeal shockwave treatment; NSAIDs = non-
steroidal anti-inflammatory drugs; CCH = Collagenase Clostridium histolyticum; IFN-α2b = Interferon-α2b.
110 SEXUAL AND REPRODUCTIVE HEALTH - LIMITED UPDATE 2022
9. PRIAPISM
Evidence Acquisition and limitations
The Panel conducted systematic reviews on the medical and surgical management of ischaemic and non-
ischaemic priapism and a dedicated systematic review on the overall management of priapism related to sickle
cell disease. The results of these systematic reviews are presented below in the guidelines and the limitations
of the studies that were assessed are highlighted.
Most studies had the same limitations and methodological bias: lack of published protocols, retrospective and
usually single-arm design, lack of randomisation and blinding, incomplete outcome data, and selective reporting.
Additionally, most studies included small numbers of patients, reported non-standardised patient characteristics,
and had short (or even unreported) follow-up times and, in general, they reflected single-unit practices.
The definitions of priapism and outcomes (such as success and related complications) were inconsistent
across the literature and few of the trials met the clear definitions that were set by the Panel for use in the
systematic reviews. Hence, any attempt to draw clinically meaningful conclusions and offer evidence-based
guidance based on systematic assessment of the literature was a challenging task. These limitations highlight
the urgent need for clear and commonly accepted definitions of conditions and outcomes that should be used
by researchers in the future so that robust evidence can be developed to support relevant guidelines and
clinical practice recommendations.
The Panel acknowledged the evidence-related limitations, and in accordance with the GRADE approach
endorsed by the European Association of Urology Guidelines Office, also took into consideration the benefits/
harms balance and the patient ideals, views and preferences prior to finalising the relevant recommendations
(for/against, weak/strong).
Priapism is a persistent or prolonged erection in the absence of sexual stimulation that fails to subside. It can
be divided into ischaemic, non-ischaemic and stuttering priapism.
9.1 Ischaemic (Low-Flow or Veno-Occlusive) Priapism
9.1.1 Epidemiology, aetiology, pathophysiology and Diagnosis
Ischaemic priapism is a persistent erection marked by rigidity of the corpora cavernosa and by little or no
cavernous arterial inflow [1304]. Ischaemic priapism is the most common subtype of priapism, accounting for
> 95% of all episodes [1304, 1305]. It presents as a painful rigid erection that is characterised clinically by absent
or reduced intracavernous arterial inflow, although proximally there is a compensated high velocity picture
with little flow distally [1306]. In ischaemic priapism, there are time-dependent metabolic alterations within the
corpus cavernosum progressively leading to hypoxia, hypercapnia, glucopenia and acidosis [1307, 1308].
Ischaemic priapism that lasts beyond 4 hours is similar to a compartment syndrome and characterised by the
development of ischaemia within the closed space of the corpora cavernosa, which severely compromises
the cavernosal circulation. Emergency medical intervention is required to minimise irreversible consequences,
such as smooth muscle necrosis, corporal fibrosis and the development of permanent erectile dysfunction (ED)
[1309, 1310]. The duration of ischaemic priapism represents the most significant predictor for the development
of ED. In this context, interventions beyond 48-72 hours of onset may help to relieve the erection and pain, but
have little clinical benefit in preventing long-term ED [1311].
Histological analysis of corporal smooth muscle biopsies shows that at 12 hours, there are features of
interstitial oedema, progressing to destruction of the sinusoidal endothelium, exposure of the basement
membrane and thrombocyte adherence by 24 hours. At 48 hours, thrombi in the sinusoidal spaces and smooth
muscle necrosis with fibroblast-like cell transformation are evident [1312]. This implies that by 48 hours there
appears to be smooth muscle necrosis and irreversibility of these ischaemic changes. A case-control study
comparing corporal biopsies from patients with priapism lasting 48-72 hours with control penile tissues
retrieved from autopsies demonstrated a significantly lower percentage of smooth muscle fibres, with an
increase in elastic fibres and collagen [1309, 1313].
No specific pathophysiological causes of ischaemic priapism can be identified in most cases [1304, 1314],
although the common aetiological factors include sickle cell disease (SCD), haematological dyscrasias,
neoplastic syndromes, and several pharmacological agents (e.g., intracavernosal PGE1 therapy) (Table 32).
Ischaemic priapism may occur (0.4-35%) after intracavernosal injection of erectogenic agents [585, 1304,
1309, 1315, 1316]. The risk is higher with papaverine-based combinations [1317], while the risk of priapism is
< 1% following prostaglandin E1 injection [1318].
SEXUAL AND REPRODUCTIVE HEALTH - LIMITED UPDATE 2022 111
You might also like
- Final NCP HerniaDocument5 pagesFinal NCP HerniaDenisse Shazz Mae Maret100% (2)
- Cyriax - Spine: by DR. Akshay A. Chougule (PT) Orthopaedic Manual TherapistDocument44 pagesCyriax - Spine: by DR. Akshay A. Chougule (PT) Orthopaedic Manual TherapistAishwarya Shah100% (1)
- Common Cases in Vascular SurgeryDocument72 pagesCommon Cases in Vascular Surgerynohazz100% (2)
- El Borno FusionDocument112 pagesEl Borno FusionneareastspineNo ratings yet
- Chiropractic Soap Notes Ipad - Sample of A New Patient Soap NoteDocument3 pagesChiropractic Soap Notes Ipad - Sample of A New Patient Soap NoteKevinNo ratings yet
- GR 10 Biology - Tissues Organs and System of Living ThingDocument28 pagesGR 10 Biology - Tissues Organs and System of Living Thingapi-301141568No ratings yet
- 100 Concepts of Developmental and Gross AnatomyDocument246 pages100 Concepts of Developmental and Gross AnatomyAbd Samad100% (1)
- Week 7 ActivityDocument2 pagesWeek 7 ActivityDanny MannoNo ratings yet
- Low-Energy Extracorporeal Shock-Wave Treatment (ESWT) For Tendinitis of The SupraspinatusDocument4 pagesLow-Energy Extracorporeal Shock-Wave Treatment (ESWT) For Tendinitis of The SupraspinatusluizamgoNo ratings yet
- Techniques For Restoring Optimal Spinal Biomechanics To Alleviate Symptoms in Bertolotti Syndrome Illustrative CaseDocument10 pagesTechniques For Restoring Optimal Spinal Biomechanics To Alleviate Symptoms in Bertolotti Syndrome Illustrative CaseOscar Cayetano Herrera RodríguezNo ratings yet
- Abdominal Trauma Presentation NotesDocument14 pagesAbdominal Trauma Presentation NoteszaminazzNo ratings yet
- Hand and Wrist PathwayDocument2 pagesHand and Wrist PathwaydrsadafrafiNo ratings yet
- Cobb - Endoscopic Carpal Tunnel ReleaseDocument8 pagesCobb - Endoscopic Carpal Tunnel ReleaseJohnny WangNo ratings yet
- Ulnar Nerve NeuropathyDocument15 pagesUlnar Nerve NeuropathyDian Atillah IkhwaniNo ratings yet
- Approach To Articular and MSK DisordersDocument8 pagesApproach To Articular and MSK DisordersAiah AbenesNo ratings yet
- High Velocity Manipulation TechniquesDocument2 pagesHigh Velocity Manipulation TechniquesBhargavaNo ratings yet
- Fneur 11 603541Document7 pagesFneur 11 603541AnggitaNo ratings yet
- CE (Ra1) F (RK) PF1 (AJ SL RK) PN (P)Document4 pagesCE (Ra1) F (RK) PF1 (AJ SL RK) PN (P)karthik padmanathanNo ratings yet
- HKDJ 0401Document4 pagesHKDJ 0401Yiu Kai WongNo ratings yet
- 2020 浮针治疗非特异性下腰痛的多中心随机对照研究 杨青宇Document5 pages2020 浮针治疗非特异性下腰痛的多中心随机对照研究 杨青宇A CNo ratings yet
- Reseccion Endoscopica para Sindrome de BertolottiDocument6 pagesReseccion Endoscopica para Sindrome de BertolottiOscar Cayetano Herrera RodríguezNo ratings yet
- Management of A Case of Ventricular Bigeminy UsingDocument2 pagesManagement of A Case of Ventricular Bigeminy UsingAlfian AlfianNo ratings yet
- Limb Ischemia VascularDocument6 pagesLimb Ischemia Vascularalbadrimohammed1997No ratings yet
- Percutaneous US Guided Treatment of Shoulder Tendon CalcificationsDocument11 pagesPercutaneous US Guided Treatment of Shoulder Tendon Calcificationspepona89No ratings yet
- Clinical Portrait Pertinent DataDocument9 pagesClinical Portrait Pertinent DataGermin CesaNo ratings yet
- Inguinal Hernia Review PDFDocument4 pagesInguinal Hernia Review PDFSebastian SetiahardjaNo ratings yet
- Outline On Common Orthopaedic EmergenciesDocument15 pagesOutline On Common Orthopaedic EmergenciesBhaskar Borgohain100% (2)
- 6239 - Case Report - Closed Fracture of Right Femoral NeckDocument38 pages6239 - Case Report - Closed Fracture of Right Femoral NeckFitaNo ratings yet
- Chaudhry 2015 Basilar Invagination Preprint World Neurosurgery PDFDocument16 pagesChaudhry 2015 Basilar Invagination Preprint World Neurosurgery PDFSahibzada HaseebNo ratings yet
- Gusti Muhammad Edy Muttaqin I4A012067 Pembimbing: Dr. Andri L. Tobing, SP - AnDocument25 pagesGusti Muhammad Edy Muttaqin I4A012067 Pembimbing: Dr. Andri L. Tobing, SP - AnBellato MauNo ratings yet
- Regional Anesthesia Technique For Post OP RehabDocument22 pagesRegional Anesthesia Technique For Post OP RehabBriantono Indroprasto WidodoNo ratings yet
- NCP NeuroDocument20 pagesNCP NeuroNica Gaborne Navarro100% (3)
- Adhesive CapsulitisDocument7 pagesAdhesive CapsulitisMariane GumbanNo ratings yet
- Because Ortho Is Cooler Than YouDocument35 pagesBecause Ortho Is Cooler Than YouMuhammad Haekal HasryNo ratings yet
- Damage Control in TraumaDocument5 pagesDamage Control in Traumavidro alifNo ratings yet
- Regis Chovvath AAOMPT Poster 2008Document1 pageRegis Chovvath AAOMPT Poster 2008smokey73No ratings yet
- Jospt 2009 3072 PDFDocument16 pagesJospt 2009 3072 PDFReissa Indah SNo ratings yet
- Bsn-Rs-Careplan 3-2Document12 pagesBsn-Rs-Careplan 3-2api-509646698No ratings yet
- How To Diagnose The PatientDocument3 pagesHow To Diagnose The PatientjohanNo ratings yet
- PRP No. 1 PDFDocument3 pagesPRP No. 1 PDFFrancisco Antonio Vicent PachecoNo ratings yet
- Hepatitis B VaccineDocument4 pagesHepatitis B VaccineShantal AbelloNo ratings yet
- Cyriax ConceptDocument30 pagesCyriax ConceptSarah Khawar ButtNo ratings yet
- Regional Anaesthesia: Anna WelbournDocument49 pagesRegional Anaesthesia: Anna WelbournAnna Welbourn100% (1)
- Journal Reading Acute Spinal Cord InjuryDocument14 pagesJournal Reading Acute Spinal Cord InjuryamandaNo ratings yet
- 09 Endoscopia Interventionala PDFDocument76 pages09 Endoscopia Interventionala PDFDark1oneNo ratings yet
- The Treatment of Chronic Coccydynia With PDFDocument7 pagesThe Treatment of Chronic Coccydynia With PDFRudolfGerNo ratings yet
- Week 1 Hip KneeDocument4 pagesWeek 1 Hip KneeEmma CannettiNo ratings yet
- Keya ChakrabartyDocument5 pagesKeya ChakrabartyKeya ChakrabartyNo ratings yet
- Chronic Pain SAQ'sDocument52 pagesChronic Pain SAQ'sNaser AhmedNo ratings yet
- Regis Leal AAOMPT Poster 2008Document1 pageRegis Leal AAOMPT Poster 2008smokey73No ratings yet
- NCL Alt. in Neuro System 2Document78 pagesNCL Alt. in Neuro System 2tavakol akbarimehmandostiNo ratings yet
- Ispub 8920Document8 pagesIspub 8920Metin AzaNo ratings yet
- Fluoroscopy Knee Cooled RF - Robin CorreaDocument41 pagesFluoroscopy Knee Cooled RF - Robin Correaandrzej.daszkiewiczNo ratings yet
- Defoort 2021Document5 pagesDefoort 2021OWL ANASNo ratings yet
- 2008 - Helminski - Daily Exercise Does Not Prevent Recurrence of Benign Paroxysmal Positional VertigoDocument6 pages2008 - Helminski - Daily Exercise Does Not Prevent Recurrence of Benign Paroxysmal Positional VertigoivanrouletNo ratings yet
- Sarimo 2011Document4 pagesSarimo 2011Pe T. ErNo ratings yet
- Vertical Talus. Surgical Technique Early Results of A New Method of Treatment For Idiopathic CongenitalDocument12 pagesVertical Talus. Surgical Technique Early Results of A New Method of Treatment For Idiopathic CongenitalChristian Jose MoralesNo ratings yet
- Acute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticeDocument54 pagesAcute Limb Ischemia Vs Critical Limb Ischemia: Clinical PracticeKiara GovenderNo ratings yet
- Hip Disorders SummaryDocument2 pagesHip Disorders SummarybhnsboshkashNo ratings yet
- Tendinitis Crónica Articulo en InglesDocument6 pagesTendinitis Crónica Articulo en IngleskarolndNo ratings yet
- Red Flag: MSK Services Pathway - Hand PathologyDocument10 pagesRed Flag: MSK Services Pathway - Hand PathologyMuhammed ElgasimNo ratings yet
- Image-guided Intra- and Extra-articular Musculoskeletal Interventions: An Illustrated Practical GuideFrom EverandImage-guided Intra- and Extra-articular Musculoskeletal Interventions: An Illustrated Practical GuideMarina ObradovNo ratings yet
- Kode IcdDocument6 pagesKode Icderi rahmayaniNo ratings yet
- Module 2 HeredityDocument18 pagesModule 2 Heredityailyn costalesNo ratings yet
- Biology Paper 6 November October 2008 IGCSE Question Paper QPDocument12 pagesBiology Paper 6 November October 2008 IGCSE Question Paper QPStevo4975% (4)
- 1 Year Puc Practical Examination: Subject: Biology (36) Question PaperDocument3 pages1 Year Puc Practical Examination: Subject: Biology (36) Question PaperChetan JavaliNo ratings yet
- Cell Cycle Worksheet 2Document4 pagesCell Cycle Worksheet 2Rodolf Jones RaboNo ratings yet
- General Biology Lab Manual - F2016 PDFDocument114 pagesGeneral Biology Lab Manual - F2016 PDFDuncan ComptonNo ratings yet
- Grassland Landscape ManagementDocument22 pagesGrassland Landscape ManagementAr Deepika RajaNo ratings yet
- Assessment Diagnosis Scientific Reason Planning Intervention Rational E EvaluationDocument2 pagesAssessment Diagnosis Scientific Reason Planning Intervention Rational E EvaluationCamille VirayNo ratings yet
- Histology Is The Study of TissuesDocument87 pagesHistology Is The Study of TissuesElena ArvanitiNo ratings yet
- Rajkumar Class 11 Unit 1Document21 pagesRajkumar Class 11 Unit 1asuhassNo ratings yet
- E10q4w5 Capslet 1Document5 pagesE10q4w5 Capslet 1MattNo ratings yet
- Honors+Onion+Root+Mitosis+Lab VirtualDocument5 pagesHonors+Onion+Root+Mitosis+Lab VirtualSwarra MudgalkarNo ratings yet
- BT224 Lec2 Cells OrgansDocument57 pagesBT224 Lec2 Cells OrgansMukul SuryawanshiNo ratings yet
- Poner en Práctica: Ejercicio 1. Completa Las Oraciones Con oDocument2 pagesPoner en Práctica: Ejercicio 1. Completa Las Oraciones Con oDIEGONo ratings yet
- Bicentennial ManDocument2 pagesBicentennial ManBubbles InojalesNo ratings yet
- Tissue Repair 2016Document16 pagesTissue Repair 2016Luis AndradeNo ratings yet
- Science Sample Paper Class-8 (2013 - 14) : (1x3 3) I. Very Short Answer QuestionsDocument3 pagesScience Sample Paper Class-8 (2013 - 14) : (1x3 3) I. Very Short Answer QuestionsTechnical GamingNo ratings yet
- 10 Science Mid Term PaperDocument6 pages10 Science Mid Term PaperAnishika100% (1)
- Suvarna 2015Document7 pagesSuvarna 2015Lívia MeloNo ratings yet
- Effectiveness of Guava 1Document16 pagesEffectiveness of Guava 1Arellano Reyson100% (1)
- A Very Big LionDocument4 pagesA Very Big LionCholifatur RohmahNo ratings yet
- 2.01 Medical Term PrefixesDocument60 pages2.01 Medical Term PrefixesNicholas FerroniNo ratings yet
- Arthroscopy of The Temporomandibular JointDocument44 pagesArthroscopy of The Temporomandibular JointDencyclopediaNo ratings yet
- Grp.2 DNA REPLICATION EMERALDDocument48 pagesGrp.2 DNA REPLICATION EMERALDLinda Ann BacunadorNo ratings yet
- Speciation PolyploidyDocument3 pagesSpeciation PolyploidySen dokNo ratings yet
- Importanceof CarbohydratesDocument3 pagesImportanceof CarbohydratescraigNo ratings yet
- Adrenergic ReceptorsDocument9 pagesAdrenergic Receptorsrababmohsin110100% (1)