Professional Documents
Culture Documents
Level 1 Nursing in Lpu
Level 1 Nursing in Lpu
Uploaded by
Britney TamuraOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Level 1 Nursing in Lpu
Level 1 Nursing in Lpu
Uploaded by
Britney TamuraCopyright:
Available Formats
NCM 109 REVIEWER
woman is pregnant; detectable in the blood or urine 1 to 2
A. Bleeding Disorder During the First days after implantation of the fertilized egg ( that is 10 days
Trimester of Pregnancy after ovulation)
Normal Values: Qualitative Urine and Blood
1.Abortion > the test is negative if client is not pregnant
Is a medical term for any interruption of a pregnancy before a > the test is positive if client is pregnant
fetus is viable (able to survive outside the uterus if born at
that time) Treatment and Management
termination of pregnancy before the age of viability (20 > Tissue passed from the vagina should be examined to
weeks or 5 mos) determine the source (fetal V/S H-Mole)
a procedure, either surgical or medical, to end a pregnancy > If remaining tissues are present – surgery or D & C
by removing the fetus and placenta from the uterus
A viable fetus is usually defined as a fetus of more than 20 Classification Of Spontaneous Abortion:
to 24 weeks of gestation or one that weighs at least 500 a.1. Threatened Abortion – pregnancy is jeopardized by
grams bleeding and cramping but the cervix is closed
A fetus born before this point is considered a miscarriage or
is termed as premature or immature birth Signs and Symptoms
Types: > Vaginal bleeding during the first 20 weeks of pregnancy
a. Spontaneous Abortion – termination of pregnancy after > Abdominal cramps may or may not accompany vaginal
the age of viability bleeding
> A miscarriage is an early miscarriage if it occurs before
week 16 of pregnancy and a late miscarriage if it occurs Treatment/Management
before weeks 16 and 20 > Complete Bed Rest (CBR) or pelvic rest for 24 to 48 hours-
> For the first 6 weeks (between 1st to 2nd month) of key intervention
pregnancy, the developing placenta is tentatively attached to > Abstaining from intercourse
the decidua of > Avoid douching
the uterus. > Avoid using tampons
During weeks 6 to 12 (2nd to 3rd month) of
pregnancy, the placenta is moderately attached 2. Imminent/ Inevitable Abortion
After week 12, the attachment is penetrating and deep – moderate bleeding, cramping, tissue protrudes from the
Bleeding before week 6 is rarely severe cervix (cervical dilatation)
Bleeding after week 12 can be profuse because the placenta Signs and Symptoms
is implanted so deeply. > low back pain or abdominal pain that is dull,
sharp, or cramping
Signs and symptoms: > vaginal bleeding, with or without abdominal
> Low back pain or abdominal pain that is dull, sharp, or cramps
cramping > tissue or clot – like material that passes from the
> Vaginal bleeding, with or without abdominal cramps vagina
> Tissue or clot – like material that passes from the vagina
TYPES
COMMON CAUSES A.2.1.Complete Abortion – all products of conception are
1. Abnormal fetal development due either to teratogenic expelled
factor (Any agent that can disturb the development of an A.2.2. Incomplete Abortion – placenta and membranes are
embryo or fetus.) or chromosomal aberration (changes retained
in chromosome number:gains or losses) Complication:
2.mmunologic factors > Infection-may also occur after a complete abortion
3.Implantation abnormalities * Escherrichia coli- organism responsible after miscarriage
4.Failure of the corpus luteum on the ovary to produce >spread from the rectum forward into the vagina
enough progesterone to maintain the decidua basalis *Group A streptococcus
5. Ingestion of alcoholic beverages during pregnancy
6. Urinary tract infection Management:
7. Systemic infections such as rubella, syphylis, poliomyelitis, > For complete abortion – emotional support
cytomegalovirus and toxoplasmosis for incomplete abortion – D & C – dilating the cervix and
scraping the lining of the uterus with an instrument called a
Signs and Test curette
1. Pelvic Exam – thinning of cervix (effacement) b. Habitual Abortion – three or more consecutive pregnancies
* Increased cervical dilatation result in abortion usually related to incompetent cervix
* Evidence of rupture membranes Other Possible Causes:
2. HCG – (qualitative and quantitative urine and blood) – > Defective spermatozoa
urine HCG test is a common method of determining if a
NCM 109 REVIEWER
Test to detect the cause: >Low blood pressure
1.X-ray or ultrasound of the uterus >Low body temperature
2. Transvaginal ultrasound >Little or no urine output
3.Blood test: >Troubled breathing
>Thrombophilia and thyroid function test Causes of Septic Abortion:
>Karyogram > The membranes surrounding the fetus have ruptured
>CBC to determine the degree of blood loss sometimes without detected
>WBC and differential to rule out infection >STD
Management: >IUD left in place during pregnancy
> Surgery for Habitual Abortion, if the cause is incompetent >Tissue from the fetus or placenta is left inside the uterus
cervix after a miscarriage or abortion
Temporary >Attempts were made to end the pregnancy, often illegally,
> McDonald Procedure by inserting tools, chemicals, or soaps into the uterus
> Temporary Circlage Long Term effects : Infertility Treatment: D & C
> Delivery: Normal Delivery Risks: Death of the fetus
Permanent
> Shirodkar procedure 1. Septicemia – is the presence of bacteria in the blood
> Delivery: C/S (bacteremia) and is often associated with severe disease.
Causes: Septicemia is a serious, life-threatening infection that
Nursing Management: get worse very quickly. It can arise from infections
throughout the body, including infections in the lungs,
>Check for signs of infection abdomen, and urinary tract
>Check for signs of labor Septicemia can rapidly lead to septic shock and death.
>Check for normal bleeding Septicemia associated with some organisms (germs) such as
meningogococci can lead to shock, adrenal collapse, and
c. Missed abortion disseminated intravascular coagulopathy, a condition called
– fetus dies; product of conception remain in uterus 4 weeks Waterhouse-Friderichsen syndrome
or longer; signs of pregnancy cease Signs and Symptoms:
Signs and Symptoms >Fever (sudden onset, often spiking)
>Scanty dark bleeding >Chills
>Negative pregnancy test >Toxic looking (looks acutely ill)
Management >Changes in mental state
>Induced labor – oxytocin/vaginal suppositories with >Irritable
prostaglandin hormone >Lethargic
>Vacuum extraction >Anxious
>Agitated
Infected/Septic Abortion >Unresponsive
– abortion associated with an infection inside a pregnant >comatose
woman’s uterus. Test that can confirm infection:
>Abortion may be spontaneous, which is referred to as >Blood culture
miscarriage. >Urine culture
>May also be an elective surgical or medical abortion, >CSF culture
meaning, the woman chose to terminate her pregnancy. >CBC
>Platelet count
Pathophysiology: A septic abortion can occur when bacteria >Clotting studies – Pt, PTT, fibrinogen levels
enter the uterus through the mucus plug. These bacteria can Complications:
be introduced by unclean tools used during an elective >Irreversible shock
abortion. The bacteria may also be those that normally live >Waterhouse-Friderichesen syndrome
in a woman’s vagina. If the woman has a sexually transmitted >Adult respiratory distress syndrome (ARDS)
disease (STD) such as chlamydia, the bacteria causing the STD Ectopic Pregnancy
can infect the uterus. If the infection reaches the > occurs when gestation is located outside the uterine
bloodstream, it is called sepsis cavity/tubal pregnancies
Signs and Symptoms: Causes:
>High fever, usually above 101 F >Fallopian tube damage often from infection-can block the
>Chills fertilized egg’s path to the uterus causing it to implant and
>Severe abdominal pain or cramping grow in the tube
>Prolonged or heavy vaginal bleeding >Surgery
>Foul-smelling vaginal discharge >Endometriosis
>backache >Smoking
If condition becomes serious, signs of shock may appear: >Previous ectopic pregnancy
These include: >Pelvic infection – chlamydia or gonorrhea
NCM 109 REVIEWER
>Fertility drugs that increase egg production
>Pelvic or abdominal surgery
Risks:
B. BLEEDING DISORDER DURING THE
>Can damage the fallopian tube SECOND TRIMESTER OF BLEEDING
Signs and Symptoms:
1. Hydatidiform Mole ( H-Mole)-
Normal signs of pregnancy - an abnormal proliferation and degeneration of the
Pain- first red flag sign trophoblastic villi
>Molar pregnancy
Other Signs and Symptoms: >Gestational Trophoblastic Disease
Vaginal spotting or bleeding >Bunch of Grapes
Dizziness or fainting (caused by blood loss) >Hydatid – means drop of water; mole – means spot
Low blood pressure (caused by blood loss) Types:
Lower back pain a.Partial Molar – pregnancy that includes an abnormal
embryo (a fertilized egg that has begun to grow) but does not
Unruptured Tubal Ruptured survive
>missed period >sudden sharp severe pain b.Complete Molar –pregnancy in which there is small cluster
> abdominal pain within >shoulder pain (indicative of clear blisters or pouches that don’t contain an embryo
3-5 weeks of intraperitoneal bleeding that Drug of choice: Methotrexate
> scant, dark brown extends to diaphragm and vaginal
> vague discomfort > + Cullen’s sign – bluish tinged Etiology: Unknown
Diagnostic Test:
>Urine pregnancy test Other Causes:
> If (+) pregnancy test – quantitative HCG test >Problems with the chromosome
>Pelvic exam >Problem with the nutrition – low protein intake
>Ultrasound >Problem with the ovaries and uterus
>Culdocentesis >Mole sometimes can develop from a placental tissue that is
Treatment: left behind in the uterus after a miscarriage or childbirth
>Vary depending on its size and location
>Injection of methotrexate Signs and Symptoms
>Surgery >(+) pregnancy test
>Laparoscopy >Symptoms for the first 3-4 months
>Uterus grow abnormally fast
Future Pregnancies: >End of 3rd month-woman will experience vaginal bleeding
ranging from scant spotting to excessive bleeding
>30% who have had ectopic pregnancy will have difficulty >Presence of hyperthyroidism (overproduction of thyroid
becoming pregnant again hormone) leads to:
>If the fallopian tube has been spared, the chances of a >Weight loss
future successful pregnancy are 60%. Even if one fallopian >Increase appetite
tube has been removed, the chances of having a successful >Intolerance to heat
pregnancy with the other tube can be greater than 40%.
Early Signs:
High Risk Women: >Vesicles passed thru the vagina
>Age – 35 and 44 y/o >Hyperemesis gravidarum
>With PID – Pelvic Inflammatory Disease >Fundal height – rapidly increases
>Previous Ectopic Pregnancy >Vaginal bleeding (scant or profuse)
>Surgery on fallopian tube > Pre-eclampsia at about 12 weeks
>Infertility problems or medication to stimulate ovulation
Nursing Care: Serious Late Complications
>Vital Signs >Hyperthyroidism
>Administer IVF >Pulmonary embolus
>Monitor vaginal bleeding
>Monitor I&O Diagnosis:
> Prepare for Culdocentesis- > suspect until 3rd month or later if fetal heartbeat is
Result: to determine if clotting or non clotting present with bleeding and severe nausea and vomiting
>If clotting – negative for ectopic pregnancy >Physician will examine the woman’s abdomen feeling for
>If non – clotting – positive for ectopic pregnancy any strange humps or abnormalities in the uterus
> Culdocentesis- is a procedure in which peritoneal fluid is >Tubal pregnancy will be ruled out
obtained from the cul de sac of a female patient. It involves >Abnormally increased HCG level with vaginal bleeding; (-)
the introduction of a spinal needle through the vaginal wall FHB and unusually large uterus will indicate a molar
into the peritoneal space of the pouch of Douglas pregnancy
NCM 109 REVIEWER
Ultrasound – confirm no living fetus >Complete or partial previous would require a C/S
2. Avoid intercourse
Treatment 3. Limit or no travelling
4. Avoid pelvic exams/internal exams – can cause profuse
>often, the tissue is naturally expelled by the fourth month of bleeding
pregnancy. In some instances, the physician will give the Predisposing Factors
woman a drug called oxytocin to trigger the release of the >Old Age
mole that is not spontaneously aborted >Smoking
>If this does not happen, a vacuum aspiration can be >intake of alcoholic beverages
performed to remove the mole >history of placenta previa in the past pregnancy
1.D&C Surgical Management:C/S with blood transfusion based on
* woman is given anesthetic blood loss
* Cervix is dilated and the contents of the uterus is
gently sunctioned out. 2. Abruptio Placenta
* After the mole has been mostly removed, gentle
scraping of the uterus lining is usually performed. > Premature separation of the placenta from the
* If the woman is older and does not want any implantation site. It usually occurs after the 20th week of
more children, the uterus can be surgically removed pregnancy
(hysterectomy) instead of a vacuum aspiration because of the > Bleeding into the deciduas basalis (the layer between the
higher risk of cancerous moles in this age group placenta and myometrium) compresses and compromises
* Monitoring the patient for at least 2 months after the function of adjacent placenta
nthe end of a molar pregnancy for HCG level
Other Names:
C. BLEEDING DISORDERS DURING THE
>Premature Separation of Placenta
THIRD TRIMESTER OF PREGNANCY >Accidental Hemorrhage
>Ablatio Placenta
1. Placenta Previa >Placental Abruption
– occurs when the placenta is improperly implanted in the
lower uterine segment, sometimes covering the cervical os Signs and Symptoms:
Signs and Symptoms >Painful vaginal bleeding
>Severe abdominal pain
> Frank, bright red, painless vaginal bleeding >Concealed bleeding (retroplacental)
>Engagement (usually has not occurred) >Rigid abdomen
>Fetal distress >Couvelaire uterus (caused by bleeding into the
>Presentation (usually abnormal) – baby is breech or in myometrium)
transverse position >Dropping Coagulation factor ( a potential for DIC)
>Uterus measures larger than it should according to
gestational age Other Signs and Symptoms:
Types: >Uterine hypertonous
>Back pain
a.Partial Placenta Previa – a portion of the cervix is covered >Preterm labor
by the placenta >Hypovolemic shock
b.Complete Placental Previa/Total – cervical opening is >Non reassuring fetal heart trackings and fetal demise
completely covered
c.Marginal Placenta Previa – extends just to the edge of the Severe Cases
cervix >Maternal hypotension
>Uterine hypertonicity
Management >Fetal distress
1.Bed Rest >Death
>If the patient presents with mild bleeding before the fetal >Clotting abnormalities
lungs are mature Cause: unknown
2.Depending on the gestational age; steroid shots may be
given to help mature the baby’s lungs
3.If the bleeding cannot be controlled, an immediate cesarian
delivery is usually done regardless of the length of pregnancy
4.Near term, fetal lung maturity may be assessed by Predisposing Factors:
amniocentesis and the preferred method is C/S
>Some marginal previas can be delivered vaginally
NCM 109 REVIEWER
>Mechanical factors such as: abdominal trauma – car >Increased blood pressure, reading greater than 140/90
accident of fall mmHg or a significant increased in one or both pressures
>Sudden loss in uterine volume as occurs with rapid loss of >Protein in the urine – proteinuria
amniotic fluid or the delivery of a first twin >Edema – swelling of face and fingers
>Abnormally short umbilical cord Cause : unknown
>Hypertension
>Pre-eclampsia Predisposing Factors:
>Multiparity >Pre – existing HPN (increased BP) >PIH with previous
>Rupture of membranes more than 24H pregnancy
>Kidney disease >Mother’s age
Signs and Tests: younger than 20 or >Diabetes
older than 40
>During a physical examination, uterine tenderness and or >Multiple gestation (twins/triplets)
increased uterine tone may be noticed
>CBC – decreased hematocrit and hemoglobin and platelets Note:
>Prothrombin time test * PIH should be treated immediately since with sincreased
>Partial thromboplastin time test BP, there is also an increased in the resisitance of blood
>Fibrinogen level test vessels. This may hinder blood flow in many different organ
>Ultrasound systems in an expectant
Other Problems:
Treatment and Management: >Occurrence of placental abruptio
>IVF > Fetal problems such as intrauterine growth restriction (poor
>Blood Transfusion fetal growth) and stillbirth
>Check for presence of shock and fetal distress
>Emergency C/S – for fetal distress or maternal bleeding Signs and Symptoms: may experience symptoms differently
Immature fetus with small placental separation – >Increased BP
hospitalization – for observation – release after several days >Proteinuria
if no evidence of progressing abruption occurs >Edema on face and fingers
If mature fetus – vaginal delivery if maternal and fetal >Sudden weight gain
distress is minimal >Blurring or double vision
C/S – to protect the mother and child >Nausea and vomiting
>Right sided upper abdominal pain or pain around the
General Nursing Care stomach
>Infuse IVF, prepare to administer blood >Decreased urine output
>Type and cross match blood components (PRBC) >Changes in liver or kidney function test
>Monitor FHR
>Insert foley catheter Diagnosis:
>Measure blood loss – count pads >BP assessment
>Report signs and symptoms of DIC >Urine testing
>Monitor V/S >Assessment of edema
>Strict I & O >Frequent weight measurement
>Eye examination to check for retinal changes
Pregnancy Induced Hypertension >Liver and kidney function test
> A form of increased blood pressure in pregnancy >Blood clotting tests
> Also called toxemia or pre – eclampsia
> Eclampsia is a severe form of PIH accompanied with Treatment:
seizures Goal: to prevent the condition from becoming worse and to
> HELLP Syndrome – Hemolysis with Elevated Liver Enzymes prevent other complications
and Decreased Platelet Counts- is a complication of severe 1. Bed rest – either at home or in the hospital
pre-eclampsia or eclampsia 2.Magnesium Sulfate (MgSO4) – drug of choice
Action: CNS Depressant/ Anti Convulsive Drug
Signs and Symptoms of HELLP Syndrome: Route: IM/IV
> Breakdown of RBC Site: 1st dose – IV; 2nd dose – buttocks
> Changes in the liver
> Decreased platelets (cells found in the blood that are Nursing Considerations:
needed to help the blood to clot in order to control bleeding) >Consider the rights in giving medications
>Check the expiration date of the medication
>Check for proper color of the medication
> Check the patient’s BP before and after giving of
THREE PRIMARY CHARACTERISTICS: medication
> Insert foley catheter as per doctor’s order
NCM 109 REVIEWER
Occurs when there is excess fluid of more than 2,000ml or an
GENERAL NURSING CARE: amniotic fluid index above 24 cm.
P – PROMOTE BED REST Normal volume at term: 500 to 1000 ml
> Prevent convulsion by nursing measures: seizure Effects on Pregnancy:
precautions Can cause fetal malpresentation due to the additional uterine
*Quiet and calm environment space and can allow the fetus to turn on a transverse lie
Can lead to premature rupture of the membranes from the
E - NSURE HIGH PROTEIN INTAKE ( 1 G/KG/DAY) increased pressure that can lead to risks for infection,
A – NTIHYPERTENSIVE DRUG : HYDRALIZE proplapsed cordand preterm birth
C - NS DEPRESSANT (MGSO4) ANTICONVULSANT DRUG
E – VALUATE PHYSICAL PARAMETERS FOR MAGNESIUM Normal Process during Pregnancy:
SULFATE TOXICITY > Amniotic fluid is formed by a combination of the cells of the
amniotic membrane and from fetal urine
B – BP decreased t is evacuated by being swallowed by the fetus, absorbed
U – urine output decreased across the intestinal membrane into the fetal bloodstream
R – RR less than 12/min and transferred across the placenta
P – patellar reflex absent With polyhydramnios, accumulation of amniotic fluid
suggests difficulty with the fetus’s ability to swallow or
Olygohydramnios absorb fluid
Refers to a pregnancy with less than the average amount of
amniotic fluid. Causes of inability to swallow fluids:
Part of the volume of amniotic fluid is formed by the addition Anencephalic
of fetal urine, this reduced amount of fluid is usually caused Fetus with tracheoesophageal fistula with stenosis
by a bladder or renal disorder in the fetus that is interfering Fetus with intestinal obstruction
with voiding Occurs among infant with diabetic mother
Another cause: due to growth restriction of the fetus, he/she
is not voiding as much as usual Assessment/Diagnosis:
Physical Assessment: Inspection- rapid enlargement of the
Diagnosis: uterus
1.Physical Assessment: Inspection: suspected during Difficulty to palpate fetal parts because the uterus is
pregnancy if the uterus fails to meet its expected growth rate unusually tense
2.Ultrasound – pockets of amniotic fluid are less than average Difficulty in auscultating the FHR due to the depth of the
Effects on the fetus after birth: increased amount of fluid surrounding the fetus
Muscles are weak due to cramped space during pregnancy Woman may have extreme shortness of breath due to
Lungs fail to develop that can lead to hypoplastic lungs- pushing up of the uterus against her diaphragm
difficulty of breathing
Potter syndrome- distorted features of the face Therapeutic Management:
Nursing Consideration: Hospitalization or home care
> Careful inspection among infants at birth to rule out kidney Goal:
disease and compromised lung development a.For adequate rest
b.For further evaluation
Polyhydramnios C. Amniocentesis – to remove excess some of the extra fluid
Occurs when there is excess fluid of more than 2,000ml or an D. .Tocolytics- to prevent or halt preterm labor
amniotic fluid index above 24 cm. If preterm rupture of the membranes occurs:
Normal volume at term: 500 to 1000 ml E. Membranes can be “Needled” (insertion of a thin needle
Effects on Pregnancy: vaginally to pierce them) to slow, control the release of fluid
Can cause fetal malpresentation due to the additional uterine and to prevent proplapsed cord during labor
space and can allow the fetus to turn on a transverse lie
Can lead to premature rupture of the membranes from the Postterm Pregnancy
increased pressure that can lead to risks for infection, > A term pregnancy is 38 to 42 weeks
proplapsed cordand preterm birth Any pregnancy that extends this period is postterm
Normal Process during Pregnancy: Causes:
> Amniotic fluid is formed by a combination of the cells of the 1. Women who have long menstrual cycle
amniotic membrane and from fetal urine 40 to 45 days: they do not ovulate on day 14 which is the
normal period
They ovulate 14 days from the end of their cycle, or on day
26 or 31, children will be considered “late” by 12 to 17 days
2. Women who are receiving high dose of salicylates for their
severe sinus headaches or rheumatoid arthritis- this
Polyhydramnios interferes with the synthesis of prostaglandin
NCM 109 REVIEWER
3.Myometrial quiescence-uterus that does not respond to 6.Immediately report signs of ruptured membranes9sudden
normal labor stimulation gush of fluid from the vagina) or vaginal bleeding
7.Report signs of urinary tract infections or vaginal infection
Danger to the fetus: (burning or frequency of urination, vaginal itching or pain)
1.Meconium aspiration 8.Keep appointments for prenatal care.
2.Macrosomia 9.Empty bladder to prevent pressure on the uterus
3.Lack of growth-placenta is functioning for only 40-42 10.Lie down on your left or right side to encourage blood
weeks-exposes the fetus to decreased blood perfusion, return to the fetus
oxygen, fluid and nutrients
Signs and Symptoms:
Management: persistent, dull, and low backache
Biophysical profile- to evaluate the placental perfusion and vaginal spotting
amount of amniotic fluid present; Feeling of pelvic pressure
if normal, it is assumed miscalculation occurs Abdominal tightenin
If abnormal result or physical examination or biparietal Menstrual-like cramping
diameter on ultrasound result the fetus is in term size, labor Increased vaginal discharge
will be induced Uterine contractions
Intestinal cramping
How to induce labor: Diagnosis:
1.Prostaglandin gel or misoprostol (Cytotec) –applied to the Analyzing changes in the length of the cervix by ultrasound
vagina to initiate uterine contraction followed by an oxytocin Analysis of vaginal mucus for the presence of fetal
infusion fibronectin, a protein produced by trophoblast cells
2.If oxytocin is ineffective, C/S is performed * If this is present in vaginal mucus, preterm labor occurs,
Nursing Consideration during the labor process: labor will not occur if the protein is absent for at least 14
1.Monitor FHR, V/S days
After Birth:
1.Assess newborn for meconium aspiration Therapeutic Management:
>Establish and maintain patent airway 1.Medical attempts can be made to stop preterm labor if:
2.Assess for polycythemia – due to decreased oxygenation in a.The fetal membranes have not ruptures
the final weeks b.No fetal distress
>hematocrit may be elevated due to polycythemia and c.No evidence of bleeding
dehydration that leads to lowered circulating plasma level. d.Cervix is not dilated more than 4 to 5 cm
3.Asess for hypoglycemia-because fetus had to use stores of e.Effacement is not more than 50%
glycogen for nourishment in the final weeks of intrauterine 2.If in preterm labor:
life a.Admission in the hospital
b.Bed rest – to relieve the pressure of the fetus in the cervix
Care of the Woman: c.Monitoring the uterine contractions
Allow woman to stay a longer period of time with her d.IVF therapy-to keep the woman well hydrated
newborn and let her or assist her in providing appropriate e.Vaginal and cervical cultures and a clean catch urine
interventions to her newborn sample- to rule out infection
Preterm Labor Drug Administration:
Labor that occurs before the end of week 37 of gestation (9 1.Tocolytic drugs- an agent to halt labor
months) >Terbutaline-drug of choice
Danger: *carries a “black box” warning- should not be used for over
Infant is immature 48 to 72 hours
Assessment: *Reason: could cause serious maternal heart problems and
> Any pregnant woman having persistent uterine death
contractions, mild and widely spaced should be considered to *should not be used in out patient or home setting-requires
be in labor, if contractions have caused cervical effacement constant professional assessment
or dilatation over 1 cm 2.Magnesium Sulfate-used traditionally to treat pre
eclampsia and prevent eclamptic seizures, can also be used
Measures on How to Prevent Preterm Labor: *recent research does not support this as tocolytic agent
1.Remain on bed rest except to use on bathroom. 3.Corticosteroid
2.Drink 8 to 10 glasses of fluids daily > bethamethasone- to promote the formation of lung
3.Keep mentally active by reading or working on a project to surfactant to prevent respiratory distress syndrome among
prevent boredom newborn
4.Avoid activities that could stimulate labor
5. Consult your primary care giver whether sexual relations Fetal Assessment: if woman is sent home:
should be restricted 1.Advice woman to keep herself well hydrated
2.Maintain adequate nutrition
NCM 109 REVIEWER
3.Mainatin bed rest and avoid strenuous activities
4.Advice the woman to have a record of daily” kick” count or
“count to 10” test of her baby’s movements inside her
womb.
LABOR THAT CANNOT BE HALTED
Membranes have ruptured-point of no return
Effacement is more than 50%
Cervical dilatation is more than 3 to 4 cm
Management:
> If fetus is very immature, C/S – to reduce pressure on the
fetal head and reduce the possibility of subdural or
intrventricular hemorrhage from a vaginal birth
What to expect:
Missed abortion – when the fetus dies before 20 weeks of
gestation and is not aborted spontaneously
Fetal death – occurs after 20 weeks of gestation and may be
used when labor does not begin within 48H of death
Signs and Symptoms:
Painless spotting
Uterine contractions with cervical effacement and dilatation
Fetus is born lifeless and emaciated
Dx:
> (-) fetal movement
> (-) FHB
> Uterine growth ceases
> Uterine size decrease
> Fetal heart movement cannot be visualized by UTZ
> X-ray detected by the appearance of intravascular or intra
abdominal fetal gas (Robert’s sign)
Management:
1.Induced labor- combination of misoprostol(Cytotec) applied
to the vagina to effect cervical ripening and oxytocin
administration to begin uterine contraction
2.Bllod studies: test for DIC
J. Rh Incompatibility
> Occurs when an Rh-negative mother (one negative for a D
antigen or one with a dd genotype0 carries a fetus with an Rh
positive blood type (DD or Dd genotype)
For this to happen:
> The father of the child must either be homozygous (DD) or
heterozygous (Dd) Rh positive
If the father of the child is homozygous (DD) for the factor,
100% of the couple’s children will be Rh positive (Dd)
If the father is heterozygous for the trait, 50% of their
children can be Rh positive (Dd)
People who have Rh-positive blood have a protein factor
(the D antigen) that Rh – negative people do not, when an Rh
–positive fetus begins to grow inside an Rh-negative mother
who is sensitized, her body reacts by forming antibodies
against the invading substance-the fetus.
You might also like
- UW Ped Clerkship Final Exam From CLIPP CasesDocument4 pagesUW Ped Clerkship Final Exam From CLIPP CasesJoe ConeNo ratings yet
- High Risk PregnancyDocument10 pagesHigh Risk PregnancyRoy Mujeres CabueñasNo ratings yet
- AbortionDocument121 pagesAbortionSindhu JojoNo ratings yet
- Abortion SeminarDocument16 pagesAbortion SeminarAjit M Prasad Prasad100% (2)
- Week 3 Care of The Woman Experiencing A Sudden Pregnancy ComplicationsDocument68 pagesWeek 3 Care of The Woman Experiencing A Sudden Pregnancy ComplicationsWendell Mark B FernandezNo ratings yet
- NCM 109 (PRELIMS) - Lesson 3Document17 pagesNCM 109 (PRELIMS) - Lesson 3nianNo ratings yet
- COMPLETE DISCUSSION NCM 109 LEC-WEEK 3 CARE GiVEN TO A MOTHER WITH SUDDEN COMPLICATIONS OF PREGNANCY WITH Recorded DiscussionDocument79 pagesCOMPLETE DISCUSSION NCM 109 LEC-WEEK 3 CARE GiVEN TO A MOTHER WITH SUDDEN COMPLICATIONS OF PREGNANCY WITH Recorded DiscussionMa. Isabel A. EnriquezNo ratings yet
- Sudden Pregnancy Complication 082852Document163 pagesSudden Pregnancy Complication 082852ian.tenorio001No ratings yet
- Abortion HandoutDocument3 pagesAbortion HandoutShena Mie Adis ValleceraNo ratings yet
- MCN NotesDocument20 pagesMCN NotesLiamLexus JavierNo ratings yet
- 109 Bleeding Disorder To DIC NotesDocument7 pages109 Bleeding Disorder To DIC NotesAngel MoncadaNo ratings yet
- Lesson 6 NCMDocument10 pagesLesson 6 NCMjohn michael cantilNo ratings yet
- High Risk of PregnancyDocument16 pagesHigh Risk of PregnancyGeraldine PatayanNo ratings yet
- High Risk PregnancyDocument104 pagesHigh Risk PregnancyNovelyn PuaNo ratings yet
- Bleeding in Early PregnancyDocument20 pagesBleeding in Early Pregnancynanapet80No ratings yet
- A 3.1 Sudden Pregnancy Complications PDFDocument47 pagesA 3.1 Sudden Pregnancy Complications PDFCamille Joy BaliliNo ratings yet
- Spontaneous Abortion (Miscarriage) Definition:: SyndromeDocument9 pagesSpontaneous Abortion (Miscarriage) Definition:: SyndromeSridevi DevarajNo ratings yet
- Abortion SolenyDocument123 pagesAbortion SolenyAyalewNo ratings yet
- AbortionDocument35 pagesAbortionZahida Aida Ida Paramore100% (1)
- Abortion TypesDocument19 pagesAbortion TypesFany MaldoNo ratings yet
- MCN Midterm HandoutDocument14 pagesMCN Midterm HandoutmerisdumpNo ratings yet
- 2 Nursing Care of The Pregnant Client Gestational ConditionDocument120 pages2 Nursing Care of The Pregnant Client Gestational ConditionjustinjareddNo ratings yet
- 2.2 NCM 109 - Complications During Pregnancy, Labor and Delivery and Postpartum PeriodsDocument10 pages2.2 NCM 109 - Complications During Pregnancy, Labor and Delivery and Postpartum PeriodsSittie Haneen TabaraNo ratings yet
- Types of AbortionDocument2 pagesTypes of AbortionMaako MonteverdeNo ratings yet
- A Woman Who Develops A Complication of PregnancyDocument24 pagesA Woman Who Develops A Complication of PregnancyLady Jane CaguladaNo ratings yet
- Obsandgyne Tables 200pagesDocument221 pagesObsandgyne Tables 200pagesRashed ShatnawiNo ratings yet
- Ectopic Pregnancy (m104)Document13 pagesEctopic Pregnancy (m104)Alphine DalgoNo ratings yet
- Abortion Part 2Document13 pagesAbortion Part 2Silver ShadowNo ratings yet
- Nle - High-Risk PregnancyDocument113 pagesNle - High-Risk Pregnancytachycardia01No ratings yet
- Bleeding in PregnancyDocument28 pagesBleeding in PregnancyNurul AnnisaniNo ratings yet
- Miscarriage (Abortion) : (Adhesions Inside The Uterine Cavity)Document10 pagesMiscarriage (Abortion) : (Adhesions Inside The Uterine Cavity)Rashed Shatnawi100% (1)
- Abortion: TH THDocument36 pagesAbortion: TH THdimly100% (1)
- Abortion (Miscarrage)Document46 pagesAbortion (Miscarrage)escalatorNo ratings yet
- Bleeding During PregnancyDocument41 pagesBleeding During PregnancyMustafa SHawkiNo ratings yet
- AbortionDocument62 pagesAbortionRaj KumarNo ratings yet
- AbortionDocument35 pagesAbortionHoney May Rollan VicenteNo ratings yet
- MiscarriageDocument38 pagesMiscarriagezianab aliNo ratings yet
- High-Risks-Of-Pregnancies - JillDocument13 pagesHigh-Risks-Of-Pregnancies - JillMaureline DominarNo ratings yet
- 14 AbortionDocument28 pages14 Abortionputz_grilla007No ratings yet
- Book Picture Patient PictureDocument22 pagesBook Picture Patient PictureAnsiya K ANo ratings yet
- A.1 AbortionDocument47 pagesA.1 AbortionRiza Mae Follero DanteNo ratings yet
- Module For Abnormal OB 1 - 120227Document129 pagesModule For Abnormal OB 1 - 120227Elizabeth MadejaNo ratings yet
- NCM 102 OB Abnormal 2Document113 pagesNCM 102 OB Abnormal 2Maria Garcia Pimentel Vanguardia IINo ratings yet
- Abortion II ND Yr MSC NursingDocument121 pagesAbortion II ND Yr MSC Nursingesthereugenia100% (2)
- Abortion: DEFINITION-Abortion Is The Separation Partial orDocument77 pagesAbortion: DEFINITION-Abortion Is The Separation Partial orPadmaNo ratings yet
- High Risk PregnancyDocument12 pagesHigh Risk Pregnancyggrrk7100% (2)
- Chapter 21Document69 pagesChapter 212082194No ratings yet
- AbortionDocument33 pagesAbortionAbdi Ñãśìr Møhàmèď ŚàĺàhNo ratings yet
- M3 - ReviewerDocument8 pagesM3 - ReviewerKristine KimNo ratings yet
- AbortionDocument22 pagesAbortionwindows3123100% (2)
- 5 - Abortion or MiscarriageDocument43 pages5 - Abortion or Miscarriageasifdawar2011No ratings yet
- Causes of Spontaneous Abortion 2Document23 pagesCauses of Spontaneous Abortion 2kenNo ratings yet
- 1 AbortionDocument60 pages1 AbortionDrMohammad KhadrawyNo ratings yet
- AbortionDocument32 pagesAbortionKirandeep Parmar100% (1)
- Early Pregnancy BleedingDocument23 pagesEarly Pregnancy Bleedingdafac7777No ratings yet
- Show Note - MCH High RiskDocument145 pagesShow Note - MCH High RiskHoneylouAzOpondaNo ratings yet
- Handouts of Complications of PostnatalDocument12 pagesHandouts of Complications of PostnatalAshish GuptaNo ratings yet
- Cmca2 (Prelim) 2Document16 pagesCmca2 (Prelim) 2NOEL YRIGONNo ratings yet
- It's Not Just a Heavy Period; The Miscarriage HandbookFrom EverandIt's Not Just a Heavy Period; The Miscarriage HandbookRating: 2 out of 5 stars2/5 (1)
- Getting Pregnant Faster: Step-By-Step Guide To Achieving PregnancyFrom EverandGetting Pregnant Faster: Step-By-Step Guide To Achieving PregnancyNo ratings yet
- Ovarian Cysts, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandOvarian Cysts, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 3 out of 5 stars3/5 (2)
- Week 8 NIPDocument25 pagesWeek 8 NIPBritney TamuraNo ratings yet
- Age Stratification 1Document6 pagesAge Stratification 1Britney TamuraNo ratings yet
- 2 HistoryDocument33 pages2 HistoryBritney TamuraNo ratings yet
- Example 1Document1 pageExample 1Britney TamuraNo ratings yet
- WEEK-5 LectureDocument3 pagesWEEK-5 LectureBritney TamuraNo ratings yet
- WEEK-4 - LectureDocument2 pagesWEEK-4 - LectureBritney TamuraNo ratings yet
- Administration of Blood TransfusionDocument1 pageAdministration of Blood TransfusionBritney TamuraNo ratings yet
- Ortho Case StudyDocument28 pagesOrtho Case StudyBritney TamuraNo ratings yet
- (Current Topics in Behavioral Neurosciences 15) Ilias Kazanis (Auth.), Catherine Belzung, Peter Wigmore (Eds.) - Neurogenesis and Neural Plasticity-Springer-Verlag Berlin Heidelberg (2013) PDFDocument402 pages(Current Topics in Behavioral Neurosciences 15) Ilias Kazanis (Auth.), Catherine Belzung, Peter Wigmore (Eds.) - Neurogenesis and Neural Plasticity-Springer-Verlag Berlin Heidelberg (2013) PDFdupuytren100% (2)
- HormonesDocument25 pagesHormonesapi-309893409No ratings yet
- IB Biology Topic 6 - Human Physiology Revision SheetDocument1 pageIB Biology Topic 6 - Human Physiology Revision SheetLexieNo ratings yet
- Introduction To MicrobiologyDocument51 pagesIntroduction To MicrobiologyGabz GabbyNo ratings yet
- Prometric Sample For DentistryDocument43 pagesPrometric Sample For DentistryAlvin RamirezNo ratings yet
- SuctionNing ProacessDocument24 pagesSuctionNing Proacesspop lopNo ratings yet
- Hiv 101Document33 pagesHiv 101Hend Al-RamahiNo ratings yet
- Lapsus Fraktur Neck FemurDocument32 pagesLapsus Fraktur Neck FemurZóélkårnåín PhåntómhívéNo ratings yet
- Rogerian Argument Essay - Drew GoellerDocument8 pagesRogerian Argument Essay - Drew Goellerapi-610224452No ratings yet
- Eight Types of DementiaDocument4 pagesEight Types of DementiaShradha AlkaNo ratings yet
- Blood Bank ProjectDocument10 pagesBlood Bank ProjectH0001437267% (3)
- NCP Ineffective Airway ClearanceDocument1 pageNCP Ineffective Airway ClearanceLucky RiusNo ratings yet
- Preaxial Polydactyly (New)Document19 pagesPreaxial Polydactyly (New)Ilham Dwiretya MuktieNo ratings yet
- Bethesda SystemDocument186 pagesBethesda SystemJoyce Pardo FernandezNo ratings yet
- 1NUR8 ABRIO Summative AssessmentDocument3 pages1NUR8 ABRIO Summative AssessmentKYRA CHEYENNE NICHOLLE ABRIO100% (1)
- Neurostimulation Treatment of Chronic PainDocument9 pagesNeurostimulation Treatment of Chronic PainTannov SiregarNo ratings yet
- Epidemiology of Malaria, Clinical Features, Treatment and Its ControlDocument157 pagesEpidemiology of Malaria, Clinical Features, Treatment and Its ControlJ Nuchin100% (2)
- Epidemiology of Cutaneous Melanoma in Germany and Worldwide: Claus Garbe Andreas BlumDocument11 pagesEpidemiology of Cutaneous Melanoma in Germany and Worldwide: Claus Garbe Andreas BlumGabriela AgrigNo ratings yet
- NursingDocument98 pagesNursingLAWRENCE MARI SANTELLA0% (1)
- Ophtha TMC Lec3Document16 pagesOphtha TMC Lec3Anonymous ic2CDkFNo ratings yet
- Treatment MGRDocument12 pagesTreatment MGRMod AntbugNo ratings yet
- Sciencefairreserchpaper LogankushnerDocument5 pagesSciencefairreserchpaper Logankushnerapi-347582278No ratings yet
- Immediate Care of The NewbornDocument3 pagesImmediate Care of The NewbornAngelee OngchuaNo ratings yet
- Thesis OphthalmologyDocument7 pagesThesis OphthalmologyJames Heller100% (2)
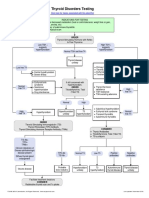
- Thyroid Disorders Testing AlgorithmDocument1 pageThyroid Disorders Testing AlgorithmRezi HelperNo ratings yet
- Measuring Other Conditions in Oral EpidemiologyDocument7 pagesMeasuring Other Conditions in Oral EpidemiologyAl Azizul HakimNo ratings yet
- Translating The A1C Assay Into Estimated Average Glucose ValuesDocument6 pagesTranslating The A1C Assay Into Estimated Average Glucose ValuesFaryalBalochNo ratings yet
- Kidney Stone Detection Using Image Processing and Convolutional Neural NetworksDocument5 pagesKidney Stone Detection Using Image Processing and Convolutional Neural NetworksInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Case Report: Management of Pit Viper Envenoming Without AntivenomDocument3 pagesCase Report: Management of Pit Viper Envenoming Without AntivenomNavin BhattNo ratings yet